NSN008 Case Study: Chronic Health Conditions Analysis
VerifiedAdded on 2022/10/02
|17
|5119
|16
Case Study
AI Summary
This case study provides a critical analysis of the complex care needs of a patient, Mr. M, suffering from multiple chronic health conditions including cardiovascular disease, type-2 diabetes, and chronic kidney disease. The essay examines the patient's symptoms, diagnostic data, and the interrelationships between these diseases. It explores the impact on the patient's physical, social, psychological, financial, and spiritual well-being, as well as the challenges faced by caregivers and the community. The analysis applies a conceptual model to address the complexity of patient care, emphasizing the need for holistic care, collaborative approaches, and the application of ethical, socially inclusive, and culturally appropriate practices. The study highlights the role of nursing care, emphasizing the importance of clinical reasoning, addressing treatment burdens, and delivering holistic care to improve patient outcomes. The case study also discusses the importance of mobile-based healthcare infrastructure to improve service delivery in chronic situations.
Summative Essay
Critical analysis of complex care needs of
patient with chronic health conditions
: A case study analysis
Critical analysis of complex care needs of
patient with chronic health conditions
: A case study analysis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Diseases extending over 3 months requiring continuous medical care, that limits routine activities of
patient are considered as chronic diseases (Goodman, Posner, Huang, Parekh, & Koh, 2013).
Cardiovascular disease, type-2-diabetes and kidney disease are the three chronic illnesses affecting
Mr M (patient) in the case study. He had myocardial infarction 5 years before, following which he
suffers from increased dyspnoea, leg oedema, frequent cough, venous-leg-ulcer, diaphoretic-skin,
ventricular-hypertrophy (left), pulmonary-oedema and high blood-pressure (BP). He has abnormal
kidney functioning wherein Serum test detected high blood K+ level 6.3 mmol/L, lower HCO3
level 15 mmol/L, higher creatinine level 390 μmmol/L, very low eGFR 12 mL/min/1.73m2 and
very low Hb 98 g/L. Increased HbA1C 7.5% underlines the cause of type-2 diabetes. Through
critical evaluation of complex care needs using Conceptual-model, ethical principles in health-care
have been applied using socially inclusive, culturally appropriate practices. The present case study
analyses the chronic illnesses and their impact on physical, social, psychological, financial and
spiritual aspects of patient and his carers, family and community.
Disease Symptoms
Symptoms refer to the subjective evidences, feelings or physical abnormalities indicating a body’s
shift from homeostasis due to a disease or illness. Chronic-Heart-Diseases (CCD), Diabetes mellitus
and Chronic-Kidney-Diseases (CKD) are often interrelated and the causative reasons behind the
other, as discussed below.
Symptoms – Cardiovascular Disease
The patient, shows symptoms suggesting that he suffers from cardiovascular illnesses. A
myocardial infarction, is a major symptom that his heart is not functioning normally. Heart attacks,
are medical emergencies occurring due to blocked flow of blood to heart, causing cardiovascular
tissue damage for lack of oxygen (Quah, Yap, Cheah, Ng, Goh, et al., 2014). Symptoms include,
Diseases extending over 3 months requiring continuous medical care, that limits routine activities of
patient are considered as chronic diseases (Goodman, Posner, Huang, Parekh, & Koh, 2013).
Cardiovascular disease, type-2-diabetes and kidney disease are the three chronic illnesses affecting
Mr M (patient) in the case study. He had myocardial infarction 5 years before, following which he
suffers from increased dyspnoea, leg oedema, frequent cough, venous-leg-ulcer, diaphoretic-skin,
ventricular-hypertrophy (left), pulmonary-oedema and high blood-pressure (BP). He has abnormal
kidney functioning wherein Serum test detected high blood K+ level 6.3 mmol/L, lower HCO3
level 15 mmol/L, higher creatinine level 390 μmmol/L, very low eGFR 12 mL/min/1.73m2 and
very low Hb 98 g/L. Increased HbA1C 7.5% underlines the cause of type-2 diabetes. Through
critical evaluation of complex care needs using Conceptual-model, ethical principles in health-care
have been applied using socially inclusive, culturally appropriate practices. The present case study
analyses the chronic illnesses and their impact on physical, social, psychological, financial and
spiritual aspects of patient and his carers, family and community.
Disease Symptoms
Symptoms refer to the subjective evidences, feelings or physical abnormalities indicating a body’s
shift from homeostasis due to a disease or illness. Chronic-Heart-Diseases (CCD), Diabetes mellitus
and Chronic-Kidney-Diseases (CKD) are often interrelated and the causative reasons behind the
other, as discussed below.
Symptoms – Cardiovascular Disease
The patient, shows symptoms suggesting that he suffers from cardiovascular illnesses. A
myocardial infarction, is a major symptom that his heart is not functioning normally. Heart attacks,
are medical emergencies occurring due to blocked flow of blood to heart, causing cardiovascular
tissue damage for lack of oxygen (Quah, Yap, Cheah, Ng, Goh, et al., 2014). Symptoms include,
abnormal heart-beat, anxiety, fatigue, bloating, appetite loss and tight pain in chest, shoulder, neck
or arm. Symptoms drawn from patient’s Objective Data, with diaphoretic skin and high respiratory
rate of 34 breath/min (normal range – 12 to 20 breath/min) suggest anxiety and hypertension
(Javaheri, Javaheri, & Javaheri 2013). Heart murmur (turbulent blood flow through problematic
heart-valve) is another symptom (Schnabel, Rienstra, Sullivan, Sun, Moser, et al., 2013). Venous
leg ulcers are caused by heart failures by blood pooling in leg veins (Vlajinac, Marinkovic,
Maksimovic, & Radak, 2014).
Subjective data on increased dyspnoea and cough suggests abnormal lung functioning in relation to
cardiac abnormalities. Leg oedema detected in the patient is caused by heart failure, with fluids
beginning to collect in lower legs. Physical examination data shows very high BP 162/106 mmHg
(normal range 120/80mmHg), which may lead to Heart murmur and Heart arrests in future.
Oxygen-saturation% is less 88% (94-100%), being a causal reason of pulmonary-heart disease.
Diagnostic studies show, left-ventricular-hypertrophy causing enlarged ventricular walls sue to high
BP and abnormal heart functioning.
Type-2 Diabetes mellitus also leads to heart attacks. Pulmonary oedema is another symptom caused
by heart congestions failing to pump blood, leading to fluid storage in alveoli (Marcinkiewicz-
Siemion, Ponikwicka, Szpakowicz, Musiał, & Kamiński, 2013). Kidney disorders also cause heart
problems, as endocrine system functions harder for increasing the kidney blood supply. This causes
the heart to pump hard, increasing pressure leading to Chronic-cardiovascular-diseases (CCD)
("Heart disease & chronic kidney disease (CKD)", 2019). All aforementioned symptoms suggest
that patient suffers from chronic-cardiovascular-disease.
Symptoms – Kidney Disease
Since the heart and kidneys function together, the failure to pump blood in a normal manner, may
cause pressure build ups in major vein which is connected to the kidneys, leading to blockage and
lesser O2 supply to kidneys ("Heart disease & chronic kidney disease (CKD)", 2019). Symptoms of
or arm. Symptoms drawn from patient’s Objective Data, with diaphoretic skin and high respiratory
rate of 34 breath/min (normal range – 12 to 20 breath/min) suggest anxiety and hypertension
(Javaheri, Javaheri, & Javaheri 2013). Heart murmur (turbulent blood flow through problematic
heart-valve) is another symptom (Schnabel, Rienstra, Sullivan, Sun, Moser, et al., 2013). Venous
leg ulcers are caused by heart failures by blood pooling in leg veins (Vlajinac, Marinkovic,
Maksimovic, & Radak, 2014).
Subjective data on increased dyspnoea and cough suggests abnormal lung functioning in relation to
cardiac abnormalities. Leg oedema detected in the patient is caused by heart failure, with fluids
beginning to collect in lower legs. Physical examination data shows very high BP 162/106 mmHg
(normal range 120/80mmHg), which may lead to Heart murmur and Heart arrests in future.
Oxygen-saturation% is less 88% (94-100%), being a causal reason of pulmonary-heart disease.
Diagnostic studies show, left-ventricular-hypertrophy causing enlarged ventricular walls sue to high
BP and abnormal heart functioning.
Type-2 Diabetes mellitus also leads to heart attacks. Pulmonary oedema is another symptom caused
by heart congestions failing to pump blood, leading to fluid storage in alveoli (Marcinkiewicz-
Siemion, Ponikwicka, Szpakowicz, Musiał, & Kamiński, 2013). Kidney disorders also cause heart
problems, as endocrine system functions harder for increasing the kidney blood supply. This causes
the heart to pump hard, increasing pressure leading to Chronic-cardiovascular-diseases (CCD)
("Heart disease & chronic kidney disease (CKD)", 2019). All aforementioned symptoms suggest
that patient suffers from chronic-cardiovascular-disease.
Symptoms – Kidney Disease
Since the heart and kidneys function together, the failure to pump blood in a normal manner, may
cause pressure build ups in major vein which is connected to the kidneys, leading to blockage and
lesser O2 supply to kidneys ("Heart disease & chronic kidney disease (CKD)", 2019). Symptoms of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CKD are indicative of poor-appetite, breathlessness, leg/hand oedema, tiredness, insomnia, and
increased-urination, blood in urine, itchy-skin, muscle-cramp, headache, erectile-dysfunction and
weight-loss ("Chronic kidney disease - Symptoms", 2019).
From Diagnostic data, Mr M has HbA1C 7.5%, which is higher than normal range 4-5.6%,
indicating high chances of developing Diabetes Mellitus (Florkowski, 2013). Furthermore Diabetes,
results in higher blood sugar level damaging blood vessels in heart and the kidneys, causing CKD
and CCD. High HbA1C value is thus a potent causal sign of CKD. Even though the Physical tests
of Urinalysis suggest the patient has a moreover right urine composition, with pH 6.8 (normal-range
7), SG 1.020 (normal-range 1.002 – 1.020), and no glucose, blood and ketone, diagnostic serum-
creatinine tests showcase a different picture.
The patient has high Serum K+ level 6.3 mmol/L (normal-range 3.5-5.0); low HCO3 15 mmol/L
(normal-range 22 - 28 mmol/L); very high Urea 22.7 mmol/L (normal-range 2.5 to 7.1 mmol/L);
very high Creatinine 390 μmmol/L (normal-range 60 to 110 μmmol/L) and a very low eGFR 12
mL/min/1.73m2 (90 mL/min/1.73m2), all being causative signs of CKD (Rule, Bailey, Lieske,
Peyser, & Turner, 2013).
Symptoms – Type – 2 Diabetes
A high HbA1C value (7.5%) as noticed in the Diagnostic tests of the patient is a potent symptom of
Diabetes. With test result value of HbA1C 6-6.4% pre-diabetes is indicated. However, with HbA1C
value ≥ 6.5% Type-2 Diabetes is indicated ("HbA1c Test for Diabetes - Diagnosis, Target HbA1c,
Home Tests", 2019). There are also certain early signs which can help detect Type-2 Diabetes,
namely, highly-frequent-urination, thirst, hunger, tiredness, blurred-vision, slow-healing of wounds,
numbness in feet or hands, dark-skin patches, itchy yeast-infections. An early detection of Type-2
Diabetes can prevent CCD and CKD (Herman, Ye, Griffin, Simmons, Davies, et al., 2015).
The patient also showed symptoms of leg oedema, in his subjective data, which is also a symptom
of diabetes. This is caused due to factors like kidney and heart problems, venous insufficiency, poor
increased-urination, blood in urine, itchy-skin, muscle-cramp, headache, erectile-dysfunction and
weight-loss ("Chronic kidney disease - Symptoms", 2019).
From Diagnostic data, Mr M has HbA1C 7.5%, which is higher than normal range 4-5.6%,
indicating high chances of developing Diabetes Mellitus (Florkowski, 2013). Furthermore Diabetes,
results in higher blood sugar level damaging blood vessels in heart and the kidneys, causing CKD
and CCD. High HbA1C value is thus a potent causal sign of CKD. Even though the Physical tests
of Urinalysis suggest the patient has a moreover right urine composition, with pH 6.8 (normal-range
7), SG 1.020 (normal-range 1.002 – 1.020), and no glucose, blood and ketone, diagnostic serum-
creatinine tests showcase a different picture.
The patient has high Serum K+ level 6.3 mmol/L (normal-range 3.5-5.0); low HCO3 15 mmol/L
(normal-range 22 - 28 mmol/L); very high Urea 22.7 mmol/L (normal-range 2.5 to 7.1 mmol/L);
very high Creatinine 390 μmmol/L (normal-range 60 to 110 μmmol/L) and a very low eGFR 12
mL/min/1.73m2 (90 mL/min/1.73m2), all being causative signs of CKD (Rule, Bailey, Lieske,
Peyser, & Turner, 2013).
Symptoms – Type – 2 Diabetes
A high HbA1C value (7.5%) as noticed in the Diagnostic tests of the patient is a potent symptom of
Diabetes. With test result value of HbA1C 6-6.4% pre-diabetes is indicated. However, with HbA1C
value ≥ 6.5% Type-2 Diabetes is indicated ("HbA1c Test for Diabetes - Diagnosis, Target HbA1c,
Home Tests", 2019). There are also certain early signs which can help detect Type-2 Diabetes,
namely, highly-frequent-urination, thirst, hunger, tiredness, blurred-vision, slow-healing of wounds,
numbness in feet or hands, dark-skin patches, itchy yeast-infections. An early detection of Type-2
Diabetes can prevent CCD and CKD (Herman, Ye, Griffin, Simmons, Davies, et al., 2015).
The patient also showed symptoms of leg oedema, in his subjective data, which is also a symptom
of diabetes. This is caused due to factors like kidney and heart problems, venous insufficiency, poor
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
circulation and obesity. The Objective data of Mr M showcases him to have venous ulcer in left
ankle, which is yet another symptom of diabetes caused by factors of venous insufficiency,
peripheral-arterial-occlusive-disease or peripheral neuropathy ("Prevention and Treatment of Leg
and Foot Ulcers in Diabetes Mellitus", 2019).
All these symptoms in the patient Mr M, suggest an interrelationship between the three chronic
diseases detected in him, namely Chronic-Cardiovascular-Disease (CCD), Chronic-Kidney-Disease
(CKD) and Type-2 Diabetes (Chin, Wrolstad, Bakris, Chertow, de Zeeuw, et al., 2014). Diabetes
increases blood-sugar level, damaging the blood vessels of the kidney and the heart. Furthermore,
CKDs’ causes damaged kidney to release more renin, which creates abnormality in blood pressure,
leading to increased CCDs.
Complexity – Patient care
Patient need and Service requirement – Multiple-Chronic-Condition (MCC) Patient
Figure: Conceptual Model addressing complexity in MCC patient-care
(Source: Grembowski, Schaefer, Johnson, Fischer, Moore, et al., 2014).
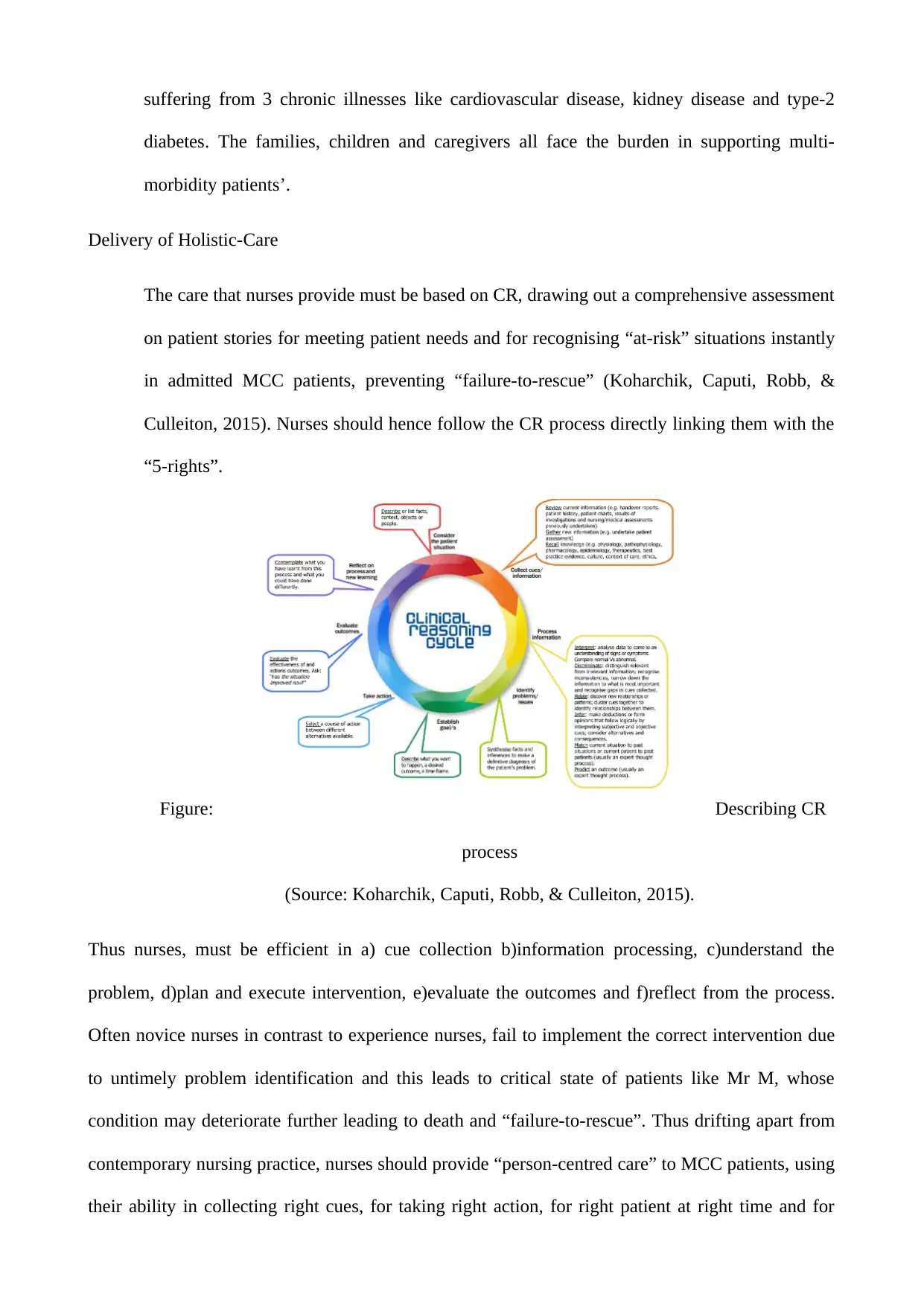
The Conceptual-model delves into the inherent complexity in delivery of patient care assessing the
needs and requirement of the patients, addressing the challenges faced by MCC patient. The
Conceptual-Model thereby serves as a guideline in patient care and research in the arena
(Grembowski, et al., 2014). Complexity as defined by the model, addresses the gap existing
between the patients’ requirements and the healthcare practices revolving around multiple
considerations affecting MCC patient needs and several contextual factors which influence the
service delivery. Processes of healthcare and outcomes are reframed by the Conceptual-model
ankle, which is yet another symptom of diabetes caused by factors of venous insufficiency,
peripheral-arterial-occlusive-disease or peripheral neuropathy ("Prevention and Treatment of Leg
and Foot Ulcers in Diabetes Mellitus", 2019).
All these symptoms in the patient Mr M, suggest an interrelationship between the three chronic
diseases detected in him, namely Chronic-Cardiovascular-Disease (CCD), Chronic-Kidney-Disease
(CKD) and Type-2 Diabetes (Chin, Wrolstad, Bakris, Chertow, de Zeeuw, et al., 2014). Diabetes
increases blood-sugar level, damaging the blood vessels of the kidney and the heart. Furthermore,
CKDs’ causes damaged kidney to release more renin, which creates abnormality in blood pressure,
leading to increased CCDs.
Complexity – Patient care
Patient need and Service requirement – Multiple-Chronic-Condition (MCC) Patient
Figure: Conceptual Model addressing complexity in MCC patient-care
(Source: Grembowski, Schaefer, Johnson, Fischer, Moore, et al., 2014).
The Conceptual-model delves into the inherent complexity in delivery of patient care assessing the
needs and requirement of the patients, addressing the challenges faced by MCC patient. The
Conceptual-Model thereby serves as a guideline in patient care and research in the arena
(Grembowski, et al., 2014). Complexity as defined by the model, addresses the gap existing
between the patients’ requirements and the healthcare practices revolving around multiple
considerations affecting MCC patient needs and several contextual factors which influence the
service delivery. Processes of healthcare and outcomes are reframed by the Conceptual-model
hence, including clinical-care experience of patient, quality of care, patient health and wellbeing
and life quality overall. The paradigm for treatment of patient needs are thus disintegrated,
highlighting MCC patient-care need which must be addressed through a dynamic care system.
Thus, the misalignment existing between services delivered and patient needs is discussed in terms
of Complexity to offer insights for researching and developing new solutions meeting the needs of
patient care.
The Conceptual-Model has 3 objectives as: defining complexity concepts in MCC patients;
description of contextual factors which influences complexity; reviewing model’s implications for
research, patient-care and health policy. In the aforementioned Figure, the ecological model,
encourages interconnection of the component elements. “Complexity” is present in the centre and
indicates the gap present between health-service-delivery and patient-needs. The Gap of “Need-
Service” indicates system capacity in interaction to patient need. “Social-support” and “Person”
side on left, determines severity, number, duration of chronic condition, affecting need level,
existence of concordant or discordant conditions (Regidor, 2016). “Need” is also influenced by age,
socio-economic-status, sex, ethnicity, preference, values and race. “Self-management” is essential
too, to provide adequate social-support to MCC patient, absence of which increases need further.
“Comorbidity” often unequally distributed and common in elderly, socially-deprived community or
ethnicity (McLean, Guthrie, Mercer, & Watt, 2015). Unmet-Needs increase also due to “lacking
health-insurance”. “Service-delivery” on right, factors affecting system-capacity are health policy
(local, state, national), evidence base for MCC patient treatment, availability of health-information
technology and e-health-record, implementation of clinical-guideline in primary-care. The health-
care system, health-service workforce and MCC patient training program of service providers are
all based on the contextual factors. “Community” also influences capacity of services provided.
“Partnerships” also increase service access and availability.
The Conceptual-Model suggest,
and life quality overall. The paradigm for treatment of patient needs are thus disintegrated,
highlighting MCC patient-care need which must be addressed through a dynamic care system.
Thus, the misalignment existing between services delivered and patient needs is discussed in terms
of Complexity to offer insights for researching and developing new solutions meeting the needs of
patient care.
The Conceptual-Model has 3 objectives as: defining complexity concepts in MCC patients;
description of contextual factors which influences complexity; reviewing model’s implications for
research, patient-care and health policy. In the aforementioned Figure, the ecological model,
encourages interconnection of the component elements. “Complexity” is present in the centre and
indicates the gap present between health-service-delivery and patient-needs. The Gap of “Need-
Service” indicates system capacity in interaction to patient need. “Social-support” and “Person”
side on left, determines severity, number, duration of chronic condition, affecting need level,
existence of concordant or discordant conditions (Regidor, 2016). “Need” is also influenced by age,
socio-economic-status, sex, ethnicity, preference, values and race. “Self-management” is essential
too, to provide adequate social-support to MCC patient, absence of which increases need further.
“Comorbidity” often unequally distributed and common in elderly, socially-deprived community or
ethnicity (McLean, Guthrie, Mercer, & Watt, 2015). Unmet-Needs increase also due to “lacking
health-insurance”. “Service-delivery” on right, factors affecting system-capacity are health policy
(local, state, national), evidence base for MCC patient treatment, availability of health-information
technology and e-health-record, implementation of clinical-guideline in primary-care. The health-
care system, health-service workforce and MCC patient training program of service providers are
all based on the contextual factors. “Community” also influences capacity of services provided.
“Partnerships” also increase service access and availability.
The Conceptual-Model suggest,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Greater complexity > lower care-quality > worsened health-outcome
Thus, in treating MCC patient and to meet their increased needs, System-services must have an
installed higher capacity.
Patient Needs
In contrast to patient with single-disease condition, MCC patients need increased clinic visits,
increased fragmented care, more healthcare cost, increased hospital-stays, and wider variations in
are quality. These patients often seek multiple healthcare provider, a low or higher sided care-
coordination can potently affect the system capacity (Gray, Wodchis, Upshur, Cott, McKinstry, et
al., 2016). With severe health conditions, MCC patients face increased mortality rate, lower quality
of life, high psychological stress and depression. The struggle of clinicians is challenging,
considering short-visits, competing-priorities, and limited organisational support for multi-
morbidity. Iatrogenic effects are caused due to the complexity gap. Patients also need mobile-based
health-care infrastructure, to transform service delivery facilities in chronic situations.
Services delivery
Healthcare services must address the development in modern day technology, imbibing it in routine
practices of daily life. Mobile-healthcare services can help patients by letting them transfer data
electronically of home measurements to clinics, can conduct automated queries through updated
databases to update patients on laboratory reminders over text messages, e-health record and
clinical prescriptions on their basis can fasten treatment procedures.
Nursing-care aspects and collaborative care in relativity to
Conceptual-care Model
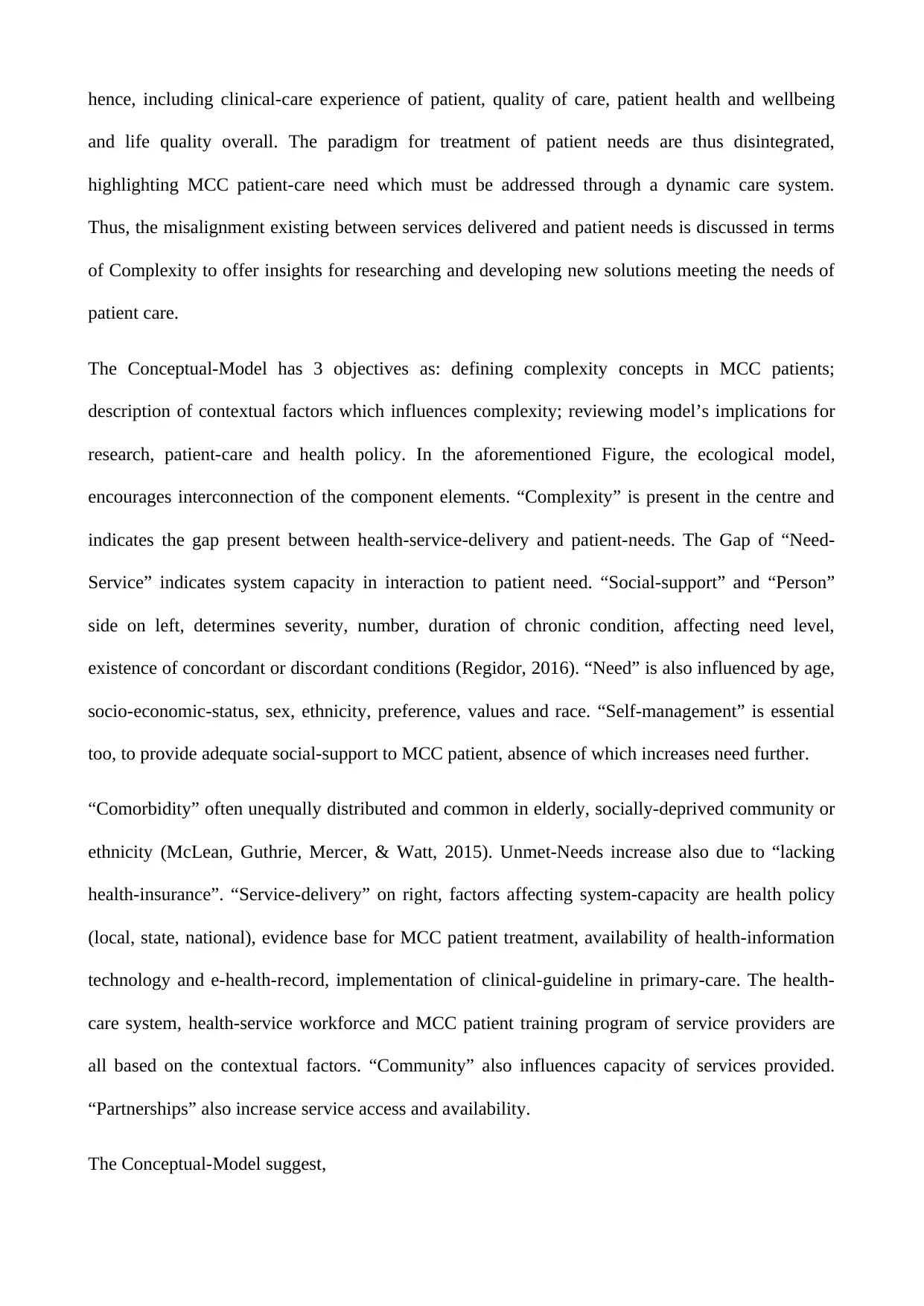
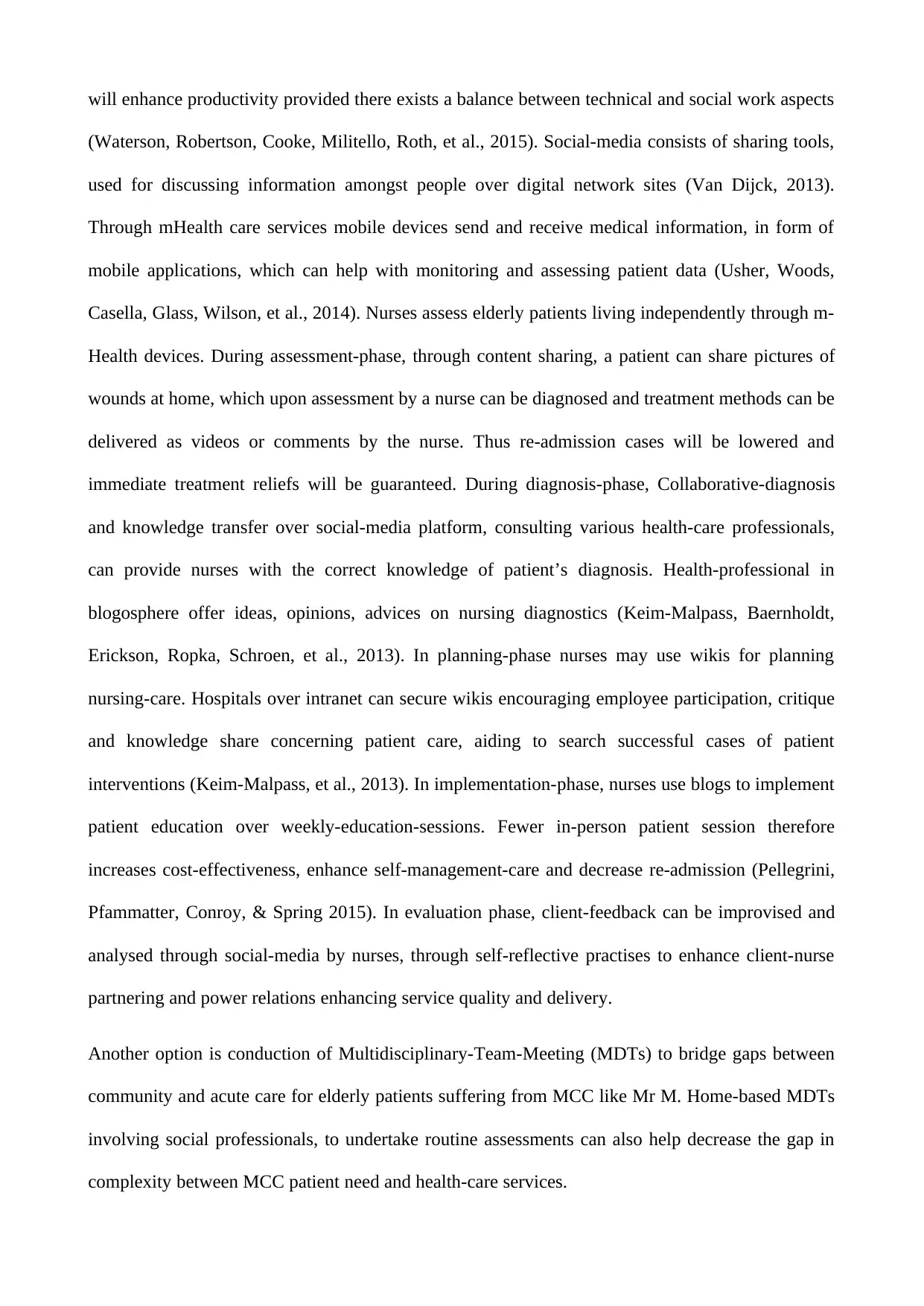
Nursing is a process containing 5 continuous overlapping stages of: assessment, diagnosis,
planning, implementing and evaluation.
Thus, in treating MCC patient and to meet their increased needs, System-services must have an
installed higher capacity.
Patient Needs
In contrast to patient with single-disease condition, MCC patients need increased clinic visits,
increased fragmented care, more healthcare cost, increased hospital-stays, and wider variations in
are quality. These patients often seek multiple healthcare provider, a low or higher sided care-
coordination can potently affect the system capacity (Gray, Wodchis, Upshur, Cott, McKinstry, et
al., 2016). With severe health conditions, MCC patients face increased mortality rate, lower quality
of life, high psychological stress and depression. The struggle of clinicians is challenging,
considering short-visits, competing-priorities, and limited organisational support for multi-
morbidity. Iatrogenic effects are caused due to the complexity gap. Patients also need mobile-based
health-care infrastructure, to transform service delivery facilities in chronic situations.
Services delivery
Healthcare services must address the development in modern day technology, imbibing it in routine
practices of daily life. Mobile-healthcare services can help patients by letting them transfer data
electronically of home measurements to clinics, can conduct automated queries through updated
databases to update patients on laboratory reminders over text messages, e-health record and
clinical prescriptions on their basis can fasten treatment procedures.
Nursing-care aspects and collaborative care in relativity to
Conceptual-care Model
Nursing is a process containing 5 continuous overlapping stages of: assessment, diagnosis,
planning, implementing and evaluation.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Figure: Nursing Process
(Source: Berman, Snyder, & Frandsen, 2016).
Multi-morbidity provides challenges for elderly patients like Mr M, the caregivers, families and
healthcare service providers. The situation demands the nursing profession to identify and
understand several cues and issues showcased by patients under critical care conditions in hospital
settings, so as to provide the necessary support to “at-risk” patients through judicious use of
“Clinical-Reasoning” (CR). The changes in nursing education, practice and research is extremely
important for addressing the collaborative functioning of nursing with multidisciplinary teams,
families and patients for enhanced management aimed towards preventing nurse-led “failure-to-
rescue” situations in MCC patients.
To deal with the MCC patient needs and to deliver excellent services to patients, the following
themes needs focus by the nursing profession (Rushton, Green, Jaarsma, Walsh, Strömberg, et al.,
2015):
Addressing treatment burden of patients and how to cope
Most MCC aged patient, find it challenging to schedule and attend multiple appointments
with diverse specialties, refraining from complicated cure regimes, like in case of Mr M,
(Source: Berman, Snyder, & Frandsen, 2016).
Multi-morbidity provides challenges for elderly patients like Mr M, the caregivers, families and
healthcare service providers. The situation demands the nursing profession to identify and
understand several cues and issues showcased by patients under critical care conditions in hospital
settings, so as to provide the necessary support to “at-risk” patients through judicious use of
“Clinical-Reasoning” (CR). The changes in nursing education, practice and research is extremely
important for addressing the collaborative functioning of nursing with multidisciplinary teams,
families and patients for enhanced management aimed towards preventing nurse-led “failure-to-
rescue” situations in MCC patients.
To deal with the MCC patient needs and to deliver excellent services to patients, the following
themes needs focus by the nursing profession (Rushton, Green, Jaarsma, Walsh, Strömberg, et al.,
2015):
Addressing treatment burden of patients and how to cope
Most MCC aged patient, find it challenging to schedule and attend multiple appointments
with diverse specialties, refraining from complicated cure regimes, like in case of Mr M,
suffering from 3 chronic illnesses like cardiovascular disease, kidney disease and type-2
diabetes. The families, children and caregivers all face the burden in supporting multi-
morbidity patients’.
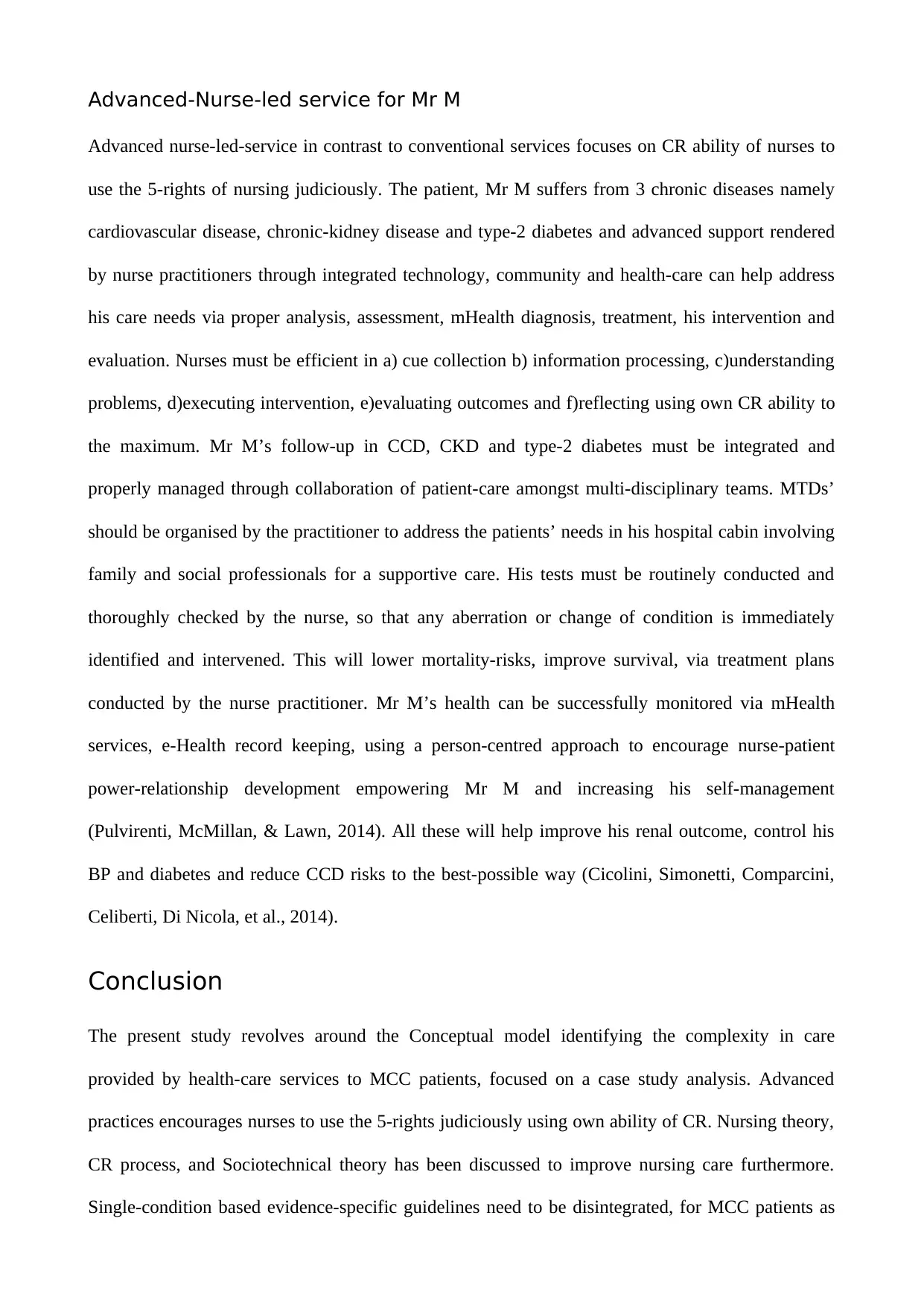
Delivery of Holistic-Care
The care that nurses provide must be based on CR, drawing out a comprehensive assessment
on patient stories for meeting patient needs and for recognising “at-risk” situations instantly
in admitted MCC patients, preventing “failure-to-rescue” (Koharchik, Caputi, Robb, &
Culleiton, 2015). Nurses should hence follow the CR process directly linking them with the
“5-rights”.
Figure: Describing CR
process
(Source: Koharchik, Caputi, Robb, & Culleiton, 2015).
Thus nurses, must be efficient in a) cue collection b)information processing, c)understand the
problem, d)plan and execute intervention, e)evaluate the outcomes and f)reflect from the process.
Often novice nurses in contrast to experience nurses, fail to implement the correct intervention due
to untimely problem identification and this leads to critical state of patients like Mr M, whose
condition may deteriorate further leading to death and “failure-to-rescue”. Thus drifting apart from
contemporary nursing practice, nurses should provide “person-centred care” to MCC patients, using
their ability in collecting right cues, for taking right action, for right patient at right time and for
diabetes. The families, children and caregivers all face the burden in supporting multi-
morbidity patients’.
Delivery of Holistic-Care
The care that nurses provide must be based on CR, drawing out a comprehensive assessment
on patient stories for meeting patient needs and for recognising “at-risk” situations instantly
in admitted MCC patients, preventing “failure-to-rescue” (Koharchik, Caputi, Robb, &
Culleiton, 2015). Nurses should hence follow the CR process directly linking them with the
“5-rights”.
Figure: Describing CR
process
(Source: Koharchik, Caputi, Robb, & Culleiton, 2015).
Thus nurses, must be efficient in a) cue collection b)information processing, c)understand the
problem, d)plan and execute intervention, e)evaluate the outcomes and f)reflect from the process.
Often novice nurses in contrast to experience nurses, fail to implement the correct intervention due
to untimely problem identification and this leads to critical state of patients like Mr M, whose
condition may deteriorate further leading to death and “failure-to-rescue”. Thus drifting apart from
contemporary nursing practice, nurses should provide “person-centred care” to MCC patients, using
their ability in collecting right cues, for taking right action, for right patient at right time and for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

right reasons. Due to lacing continuity between health-care services, clinical pathways are often not
linked up when patients shift from primary care to secondary and back, depending on nurse’s roles
to ensure collaboration of patient-care amongst multi-disciplinary teams for multi-morbidity
patients.
Evidence-base development
Lacking evidence-base in form of researches conducted in this field, is a challenge addressing the
management of MCC patients’ facing long-term multiple chronic conditions. Integrated care models
must be researched upon and implemented for integrating the landscape of social care and health in
future.
Stimulated Learning
Nursing education needs to be targeted at the root for efficient support to MCC patients like Mr M.
Nurses should be thorough not only in generalist skills, in specific chronic diseases to address
comorbidity, but non-clinical skills in nurses are also essential. They should communicate
professionally with patients, multiple professionals, and families to deliver coordinated care.
Furthermore, technology-based nursing education relying on mobile health and fluency in
technology can leverage nursing services to care for patients with complex priorities. Nurses must
also be trained in genomics for dealing with rare diseases.
Re-design of Health Service
The present design of health-care services increases the frustration of MCC patients, with an
increase in MCC patients every year but no changes in existing healthcare processes fit for
addressing those patients’ need. Single-disease focuses must be disintegrated being unfit for serving
the multiple-disease challenge. Increased technology usage via robotics, wearable device, and social
media must be focused upon for serving MCC paints even at home to provide enhanced access to
health-care services instead of forcing them to visit multiple specialists by hospital visits. Mobile
Health services can play a role here. The socio-technical theory, 1960 suggests Australian Nurses
linked up when patients shift from primary care to secondary and back, depending on nurse’s roles
to ensure collaboration of patient-care amongst multi-disciplinary teams for multi-morbidity
patients.
Evidence-base development
Lacking evidence-base in form of researches conducted in this field, is a challenge addressing the
management of MCC patients’ facing long-term multiple chronic conditions. Integrated care models
must be researched upon and implemented for integrating the landscape of social care and health in
future.
Stimulated Learning
Nursing education needs to be targeted at the root for efficient support to MCC patients like Mr M.
Nurses should be thorough not only in generalist skills, in specific chronic diseases to address
comorbidity, but non-clinical skills in nurses are also essential. They should communicate
professionally with patients, multiple professionals, and families to deliver coordinated care.
Furthermore, technology-based nursing education relying on mobile health and fluency in
technology can leverage nursing services to care for patients with complex priorities. Nurses must
also be trained in genomics for dealing with rare diseases.
Re-design of Health Service
The present design of health-care services increases the frustration of MCC patients, with an
increase in MCC patients every year but no changes in existing healthcare processes fit for
addressing those patients’ need. Single-disease focuses must be disintegrated being unfit for serving
the multiple-disease challenge. Increased technology usage via robotics, wearable device, and social
media must be focused upon for serving MCC paints even at home to provide enhanced access to
health-care services instead of forcing them to visit multiple specialists by hospital visits. Mobile
Health services can play a role here. The socio-technical theory, 1960 suggests Australian Nurses
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
will enhance productivity provided there exists a balance between technical and social work aspects
(Waterson, Robertson, Cooke, Militello, Roth, et al., 2015). Social-media consists of sharing tools,
used for discussing information amongst people over digital network sites (Van Dijck, 2013).
Through mHealth care services mobile devices send and receive medical information, in form of
mobile applications, which can help with monitoring and assessing patient data (Usher, Woods,
Casella, Glass, Wilson, et al., 2014). Nurses assess elderly patients living independently through m-
Health devices. During assessment-phase, through content sharing, a patient can share pictures of
wounds at home, which upon assessment by a nurse can be diagnosed and treatment methods can be
delivered as videos or comments by the nurse. Thus re-admission cases will be lowered and
immediate treatment reliefs will be guaranteed. During diagnosis-phase, Collaborative-diagnosis
and knowledge transfer over social-media platform, consulting various health-care professionals,
can provide nurses with the correct knowledge of patient’s diagnosis. Health-professional in
blogosphere offer ideas, opinions, advices on nursing diagnostics (Keim-Malpass, Baernholdt,
Erickson, Ropka, Schroen, et al., 2013). In planning-phase nurses may use wikis for planning
nursing-care. Hospitals over intranet can secure wikis encouraging employee participation, critique
and knowledge share concerning patient care, aiding to search successful cases of patient
interventions (Keim-Malpass, et al., 2013). In implementation-phase, nurses use blogs to implement
patient education over weekly-education-sessions. Fewer in-person patient session therefore
increases cost-effectiveness, enhance self-management-care and decrease re-admission (Pellegrini,
Pfammatter, Conroy, & Spring 2015). In evaluation phase, client-feedback can be improvised and
analysed through social-media by nurses, through self-reflective practises to enhance client-nurse
partnering and power relations enhancing service quality and delivery.
Another option is conduction of Multidisciplinary-Team-Meeting (MDTs) to bridge gaps between
community and acute care for elderly patients suffering from MCC like Mr M. Home-based MDTs
involving social professionals, to undertake routine assessments can also help decrease the gap in
complexity between MCC patient need and health-care services.
(Waterson, Robertson, Cooke, Militello, Roth, et al., 2015). Social-media consists of sharing tools,
used for discussing information amongst people over digital network sites (Van Dijck, 2013).
Through mHealth care services mobile devices send and receive medical information, in form of
mobile applications, which can help with monitoring and assessing patient data (Usher, Woods,
Casella, Glass, Wilson, et al., 2014). Nurses assess elderly patients living independently through m-
Health devices. During assessment-phase, through content sharing, a patient can share pictures of
wounds at home, which upon assessment by a nurse can be diagnosed and treatment methods can be
delivered as videos or comments by the nurse. Thus re-admission cases will be lowered and
immediate treatment reliefs will be guaranteed. During diagnosis-phase, Collaborative-diagnosis
and knowledge transfer over social-media platform, consulting various health-care professionals,
can provide nurses with the correct knowledge of patient’s diagnosis. Health-professional in
blogosphere offer ideas, opinions, advices on nursing diagnostics (Keim-Malpass, Baernholdt,
Erickson, Ropka, Schroen, et al., 2013). In planning-phase nurses may use wikis for planning
nursing-care. Hospitals over intranet can secure wikis encouraging employee participation, critique
and knowledge share concerning patient care, aiding to search successful cases of patient
interventions (Keim-Malpass, et al., 2013). In implementation-phase, nurses use blogs to implement
patient education over weekly-education-sessions. Fewer in-person patient session therefore
increases cost-effectiveness, enhance self-management-care and decrease re-admission (Pellegrini,
Pfammatter, Conroy, & Spring 2015). In evaluation phase, client-feedback can be improvised and
analysed through social-media by nurses, through self-reflective practises to enhance client-nurse
partnering and power relations enhancing service quality and delivery.
Another option is conduction of Multidisciplinary-Team-Meeting (MDTs) to bridge gaps between
community and acute care for elderly patients suffering from MCC like Mr M. Home-based MDTs
involving social professionals, to undertake routine assessments can also help decrease the gap in
complexity between MCC patient need and health-care services.
Advanced-Nurse-led service for Mr M
Advanced nurse-led-service in contrast to conventional services focuses on CR ability of nurses to
use the 5-rights of nursing judiciously. The patient, Mr M suffers from 3 chronic diseases namely
cardiovascular disease, chronic-kidney disease and type-2 diabetes and advanced support rendered
by nurse practitioners through integrated technology, community and health-care can help address
his care needs via proper analysis, assessment, mHealth diagnosis, treatment, his intervention and
evaluation. Nurses must be efficient in a) cue collection b) information processing, c)understanding
problems, d)executing intervention, e)evaluating outcomes and f)reflecting using own CR ability to
the maximum. Mr M’s follow-up in CCD, CKD and type-2 diabetes must be integrated and
properly managed through collaboration of patient-care amongst multi-disciplinary teams. MTDs’
should be organised by the practitioner to address the patients’ needs in his hospital cabin involving
family and social professionals for a supportive care. His tests must be routinely conducted and
thoroughly checked by the nurse, so that any aberration or change of condition is immediately
identified and intervened. This will lower mortality-risks, improve survival, via treatment plans
conducted by the nurse practitioner. Mr M’s health can be successfully monitored via mHealth
services, e-Health record keeping, using a person-centred approach to encourage nurse-patient
power-relationship development empowering Mr M and increasing his self-management
(Pulvirenti, McMillan, & Lawn, 2014). All these will help improve his renal outcome, control his
BP and diabetes and reduce CCD risks to the best-possible way (Cicolini, Simonetti, Comparcini,
Celiberti, Di Nicola, et al., 2014).
Conclusion
The present study revolves around the Conceptual model identifying the complexity in care
provided by health-care services to MCC patients, focused on a case study analysis. Advanced
practices encourages nurses to use the 5-rights judiciously using own ability of CR. Nursing theory,
CR process, and Sociotechnical theory has been discussed to improve nursing care furthermore.
Single-condition based evidence-specific guidelines need to be disintegrated, for MCC patients as
Advanced nurse-led-service in contrast to conventional services focuses on CR ability of nurses to
use the 5-rights of nursing judiciously. The patient, Mr M suffers from 3 chronic diseases namely
cardiovascular disease, chronic-kidney disease and type-2 diabetes and advanced support rendered
by nurse practitioners through integrated technology, community and health-care can help address
his care needs via proper analysis, assessment, mHealth diagnosis, treatment, his intervention and
evaluation. Nurses must be efficient in a) cue collection b) information processing, c)understanding
problems, d)executing intervention, e)evaluating outcomes and f)reflecting using own CR ability to
the maximum. Mr M’s follow-up in CCD, CKD and type-2 diabetes must be integrated and
properly managed through collaboration of patient-care amongst multi-disciplinary teams. MTDs’
should be organised by the practitioner to address the patients’ needs in his hospital cabin involving
family and social professionals for a supportive care. His tests must be routinely conducted and
thoroughly checked by the nurse, so that any aberration or change of condition is immediately
identified and intervened. This will lower mortality-risks, improve survival, via treatment plans
conducted by the nurse practitioner. Mr M’s health can be successfully monitored via mHealth
services, e-Health record keeping, using a person-centred approach to encourage nurse-patient
power-relationship development empowering Mr M and increasing his self-management
(Pulvirenti, McMillan, & Lawn, 2014). All these will help improve his renal outcome, control his
BP and diabetes and reduce CCD risks to the best-possible way (Cicolini, Simonetti, Comparcini,
Celiberti, Di Nicola, et al., 2014).
Conclusion
The present study revolves around the Conceptual model identifying the complexity in care
provided by health-care services to MCC patients, focused on a case study analysis. Advanced
practices encourages nurses to use the 5-rights judiciously using own ability of CR. Nursing theory,
CR process, and Sociotechnical theory has been discussed to improve nursing care furthermore.
Single-condition based evidence-specific guidelines need to be disintegrated, for MCC patients as
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





