Chronic Renal Failure: Nursing Assessment, Treatment, and Education
VerifiedAdded on 2021/02/21
|14
|3386
|230
Report
AI Summary
This nursing report provides a comprehensive overview of chronic renal failure (CRF), detailing its renal anatomy and physiology, and exploring its pathophysiology. It differentiates between chronic and acute renal failure, examines renal replacement therapy, and discusses medication side effects with associated nursing considerations. The report analyzes the results of GFR and Hb blood tests, and emphasizes the importance of the teach-back method in patient education. Furthermore, it addresses the management of CRF through patient education regarding fluid intake. The report also highlights key aspects of nursing care, including medication management, patient assessment, and the implementation of educational strategies to improve patient outcomes. The report provides a detailed analysis of the disease, including the causes, symptoms, diagnosis, and treatment options, with a focus on nursing interventions and patient education.
Nursing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
1.1 Renal anatomy and physiology........................................................................................3
1.2 Pathophysiology in relation with chronic renal failure....................................................4
1.3 Difference between chronic and acute renal failure.........................................................5
1.4 Renal replacement therapy...............................................................................................6
2.1 Side effects and nursing consideration in relation with medication. ...............................6
2.2 Results of GFR and Hb blood test....................................................................................7
3.1 Teach-back method..........................................................................................................8
3.2 Managing the chronic renal failure by educating individual regarding fluid intake........8
CONCLUSION................................................................................................................................8
REFERENCES..............................................................................................................................10
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
1.1 Renal anatomy and physiology........................................................................................3
1.2 Pathophysiology in relation with chronic renal failure....................................................4
1.3 Difference between chronic and acute renal failure.........................................................5
1.4 Renal replacement therapy...............................................................................................6
2.1 Side effects and nursing consideration in relation with medication. ...............................6
2.2 Results of GFR and Hb blood test....................................................................................7
3.1 Teach-back method..........................................................................................................8
3.2 Managing the chronic renal failure by educating individual regarding fluid intake........8
CONCLUSION................................................................................................................................8
REFERENCES..............................................................................................................................10
INTRODUCTION
Nursing is an effective technique within the health care sector in order to focus on care
and support. This in turn helps in maintaining and recovering the quality of life and recover the
optimal health of the individual.
This study will highlight, renal anatomy and physiology. It will also take into
consideration pathophysiology in relation with chronic renal failure. This study will also
demonstrate renal replacement therapy. It will also highlight, side effects and nursing
consideration in relation with medication. Furthermore, it will evaluate the results of GFR and
Hb blood test. This study further helps in managing the chronic renal failure by educating
individual regarding fluid intake.
MAIN BODY
PART 1
1.1 Renal anatomy and physiology.
According to Chalmers (2019), Renal anatomy of the kidney is divided into major
structures such as inner renal medulla and outer renal cortex. These structures take shape of 8 to
18 cone shaped renal lobes. Each renal contains renal cortex is surrounded with the portion of
medulla which is referred to as renal pyramid. Kidney is found in vertebrates and is a two bean
shaped organ. The left kidney is at T 12 to L3 vertebrae. Kidney receive blood from the renal
arteries and the blood exits into paired renal veins. Kidney helps in regulating the concentration
and volume of fluid in the body. Kidney helps in detoxifying various harmful substances,
production of erythropoietin and increase in absorption of calcium. Kidney also helps in
secreting renin that helps in balancing blood pressure and electrolyte in the body. This also
results in chronic renal failure which results in permanent partial loss of how the kidney works.
This results in high blood pressure and diabetes (Renal System & Kidney Anatomy, 2014). The
key function of kidney is excretion and filtration of waste products from the body.
Nephrons and Vessels
Nephrons is one of the functional units of kidney that cleanse the blood and effectively
balance the circulation (ANATOMY AND PHYSIOLOGY, 2019). The afferent arterioles form
high pressure capillaries for about 200 μm in diameter known as glomerulus.
Cortex
Nursing is an effective technique within the health care sector in order to focus on care
and support. This in turn helps in maintaining and recovering the quality of life and recover the
optimal health of the individual.
This study will highlight, renal anatomy and physiology. It will also take into
consideration pathophysiology in relation with chronic renal failure. This study will also
demonstrate renal replacement therapy. It will also highlight, side effects and nursing
consideration in relation with medication. Furthermore, it will evaluate the results of GFR and
Hb blood test. This study further helps in managing the chronic renal failure by educating
individual regarding fluid intake.
MAIN BODY
PART 1
1.1 Renal anatomy and physiology.
According to Chalmers (2019), Renal anatomy of the kidney is divided into major
structures such as inner renal medulla and outer renal cortex. These structures take shape of 8 to
18 cone shaped renal lobes. Each renal contains renal cortex is surrounded with the portion of
medulla which is referred to as renal pyramid. Kidney is found in vertebrates and is a two bean
shaped organ. The left kidney is at T 12 to L3 vertebrae. Kidney receive blood from the renal
arteries and the blood exits into paired renal veins. Kidney helps in regulating the concentration
and volume of fluid in the body. Kidney helps in detoxifying various harmful substances,
production of erythropoietin and increase in absorption of calcium. Kidney also helps in
secreting renin that helps in balancing blood pressure and electrolyte in the body. This also
results in chronic renal failure which results in permanent partial loss of how the kidney works.
This results in high blood pressure and diabetes (Renal System & Kidney Anatomy, 2014). The
key function of kidney is excretion and filtration of waste products from the body.
Nephrons and Vessels
Nephrons is one of the functional units of kidney that cleanse the blood and effectively
balance the circulation (ANATOMY AND PHYSIOLOGY, 2019). The afferent arterioles form
high pressure capillaries for about 200 μm in diameter known as glomerulus.
Cortex
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
It is the outer portion of the kidney which is between renal medulla and renal capsule. It
contains majority of length of nephrons and also filters fluid from the body.
Ureter
It is a tube that effectively carries urine from kidney to the urinary bladder. Two types of
ureter are there in kidney (Beachey, (2017)). One attached to each kidney. Lower half is in pelvic
area and the upper half is in abdomen.
Urinary bladder
It is a muscular sac in pelvis area near pubic bone. Urine is formed in kidney and is
travelled down through two tubes known as ureters to bladder.
1.2 Pathophysiology in relation with chronic renal failure.
Chronic kidney disease is referred to as progressive deterioration of the renal function in
the body. There are various symptoms which develop slowly in advanced level which in turn
results in nausea, vomiting, muscle twitches, water retention, under nutrition, cramps, pruritus,
dysgeusia, etc. This happens because renal tissue loses function and results in various
deformities. Pruritus is a troublesome complication is an unpleasant sensation that provokes the
urge to scratch (Pathophysiology of chronic renal failure, 2003). Melanie Johnson was feeling
tired, general pruritus and nausea. She was suffering from severe headaches and palpitations
from over 5 years. Chronic kidney disease results in diminishing the renal reserve and
inefficiency which in turn results in renal failure i.e., end stage renal disease (Mårtensson &
Bellomo, (2017)). Glomerular filtration rate (GFR) is effectively used to check how well is the
kidney working. There is a decline in Glomerular filtration rate (GFR). This in turn results in
filtration of macromolecules and protein (Nishi, Bergamaschi & Campos, (2015)). It helps in
estimating the circulation of blood through the glomeruli every minute. Glomeruli helps in
filtering the waste from the blood. This in turn results in chronic kidney failure. At the age of
55-59 years old the normal range of Glomerular filtration rate (GFR) is 174 and the range is
between 48-149. The GFR of the Melanie Johnson is said to be 10ml/min/1.73m2 which states
that she is in critical situation of chronic disease failure and kidney dysfunction. Melanie
Johnson has been suffering from severe headaches and palpitations. She has been consuming
Ibuprofen and naproxen for headaches over 12 years without considering any medical consultation. End
stage renal disease results in loss of kidney capability because of progressive chronic kidney failure
contains majority of length of nephrons and also filters fluid from the body.
Ureter
It is a tube that effectively carries urine from kidney to the urinary bladder. Two types of
ureter are there in kidney (Beachey, (2017)). One attached to each kidney. Lower half is in pelvic
area and the upper half is in abdomen.
Urinary bladder
It is a muscular sac in pelvis area near pubic bone. Urine is formed in kidney and is
travelled down through two tubes known as ureters to bladder.
1.2 Pathophysiology in relation with chronic renal failure.
Chronic kidney disease is referred to as progressive deterioration of the renal function in
the body. There are various symptoms which develop slowly in advanced level which in turn
results in nausea, vomiting, muscle twitches, water retention, under nutrition, cramps, pruritus,
dysgeusia, etc. This happens because renal tissue loses function and results in various
deformities. Pruritus is a troublesome complication is an unpleasant sensation that provokes the
urge to scratch (Pathophysiology of chronic renal failure, 2003). Melanie Johnson was feeling
tired, general pruritus and nausea. She was suffering from severe headaches and palpitations
from over 5 years. Chronic kidney disease results in diminishing the renal reserve and
inefficiency which in turn results in renal failure i.e., end stage renal disease (Mårtensson &
Bellomo, (2017)). Glomerular filtration rate (GFR) is effectively used to check how well is the
kidney working. There is a decline in Glomerular filtration rate (GFR). This in turn results in
filtration of macromolecules and protein (Nishi, Bergamaschi & Campos, (2015)). It helps in
estimating the circulation of blood through the glomeruli every minute. Glomeruli helps in
filtering the waste from the blood. This in turn results in chronic kidney failure. At the age of
55-59 years old the normal range of Glomerular filtration rate (GFR) is 174 and the range is
between 48-149. The GFR of the Melanie Johnson is said to be 10ml/min/1.73m2 which states
that she is in critical situation of chronic disease failure and kidney dysfunction. Melanie
Johnson has been suffering from severe headaches and palpitations. She has been consuming
Ibuprofen and naproxen for headaches over 12 years without considering any medical consultation. End
stage renal disease results in loss of kidney capability because of progressive chronic kidney failure
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Oxburgh, (2018)). This in turn requires regular dialysis for the survival. Kidney helps in regulating the
blood pressure. Renal failure results in kidney unable to filter the waste products out of the blood
effectively. Use of Ibuprofen and naproxen results in impaired blood flow to the kidney. In case of
Melanie Johnson she has been using Ibuprofen and naproxen for 12 years which in turn resulted in
chronic kidney disease. Ibuprofen blocks the prostaglandins, dilate blood vessels, block natural blood
chemicals which in turn decreases the blood flow to the kidney. Consumption of such medication resulted
in nausea, tiredness, general pruritus, headache and palpitations. Melanie Johnson has to undergo through
renal replacement therapy (Haemodialysis). Haemodialysis is an artificial kidney which helps in
removing waste, chemicals and additional fluids. Regular dialysis helps in more beneficial health
outcomes and better functioning of the body (Khan & et.al. (2017)).
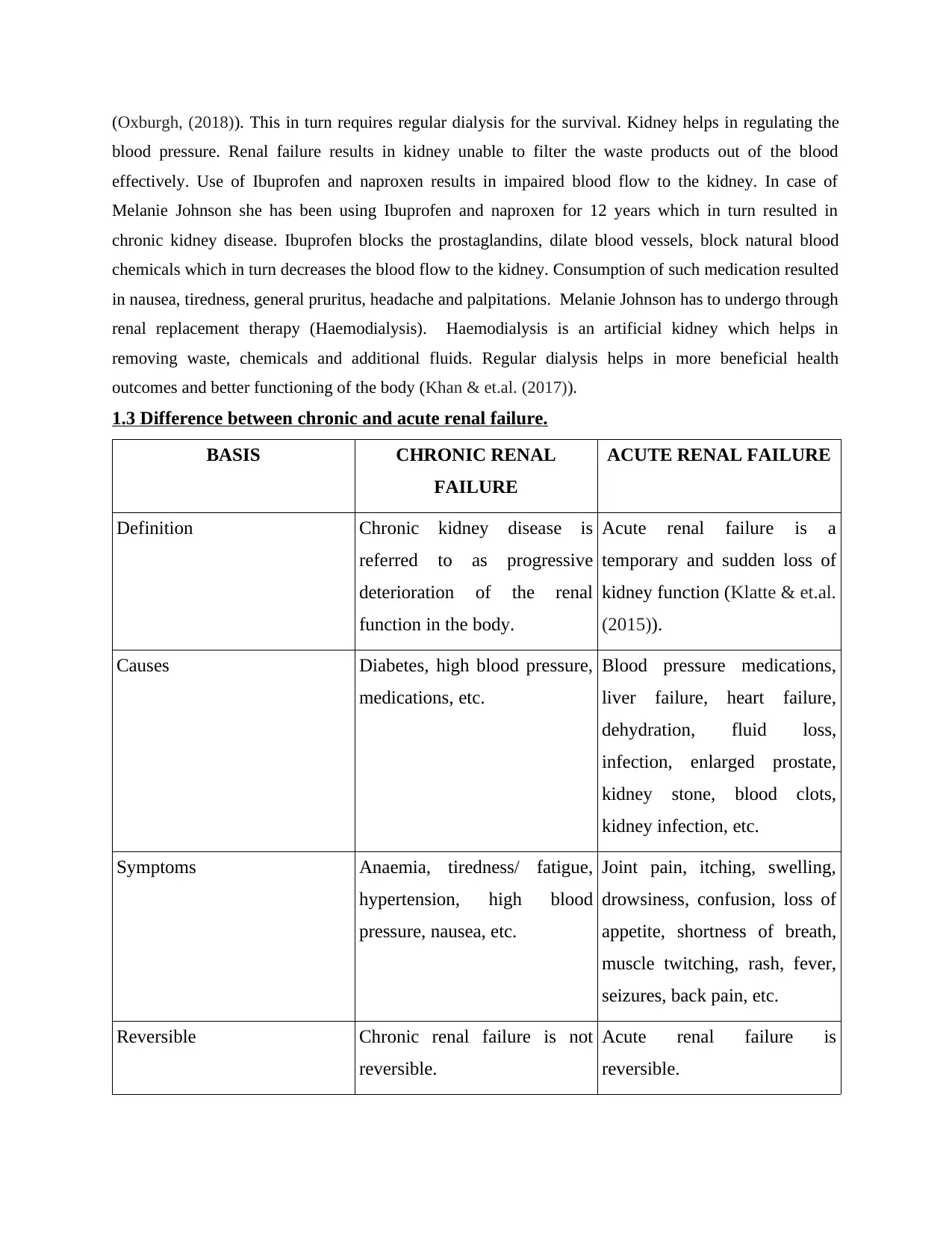
1.3 Difference between chronic and acute renal failure.
BASIS CHRONIC RENAL
FAILURE
ACUTE RENAL FAILURE
Definition Chronic kidney disease is
referred to as progressive
deterioration of the renal
function in the body.
Acute renal failure is a
temporary and sudden loss of
kidney function (Klatte & et.al.
(2015)).
Causes Diabetes, high blood pressure,
medications, etc.
Blood pressure medications,
liver failure, heart failure,
dehydration, fluid loss,
infection, enlarged prostate,
kidney stone, blood clots,
kidney infection, etc.
Symptoms Anaemia, tiredness/ fatigue,
hypertension, high blood
pressure, nausea, etc.
Joint pain, itching, swelling,
drowsiness, confusion, loss of
appetite, shortness of breath,
muscle twitching, rash, fever,
seizures, back pain, etc.
Reversible Chronic renal failure is not
reversible.
Acute renal failure is
reversible.
blood pressure. Renal failure results in kidney unable to filter the waste products out of the blood
effectively. Use of Ibuprofen and naproxen results in impaired blood flow to the kidney. In case of
Melanie Johnson she has been using Ibuprofen and naproxen for 12 years which in turn resulted in
chronic kidney disease. Ibuprofen blocks the prostaglandins, dilate blood vessels, block natural blood
chemicals which in turn decreases the blood flow to the kidney. Consumption of such medication resulted
in nausea, tiredness, general pruritus, headache and palpitations. Melanie Johnson has to undergo through
renal replacement therapy (Haemodialysis). Haemodialysis is an artificial kidney which helps in
removing waste, chemicals and additional fluids. Regular dialysis helps in more beneficial health
outcomes and better functioning of the body (Khan & et.al. (2017)).
1.3 Difference between chronic and acute renal failure.
BASIS CHRONIC RENAL
FAILURE
ACUTE RENAL FAILURE
Definition Chronic kidney disease is
referred to as progressive
deterioration of the renal
function in the body.
Acute renal failure is a
temporary and sudden loss of
kidney function (Klatte & et.al.
(2015)).
Causes Diabetes, high blood pressure,
medications, etc.
Blood pressure medications,
liver failure, heart failure,
dehydration, fluid loss,
infection, enlarged prostate,
kidney stone, blood clots,
kidney infection, etc.
Symptoms Anaemia, tiredness/ fatigue,
hypertension, high blood
pressure, nausea, etc.
Joint pain, itching, swelling,
drowsiness, confusion, loss of
appetite, shortness of breath,
muscle twitching, rash, fever,
seizures, back pain, etc.
Reversible Chronic renal failure is not
reversible.
Acute renal failure is
reversible.
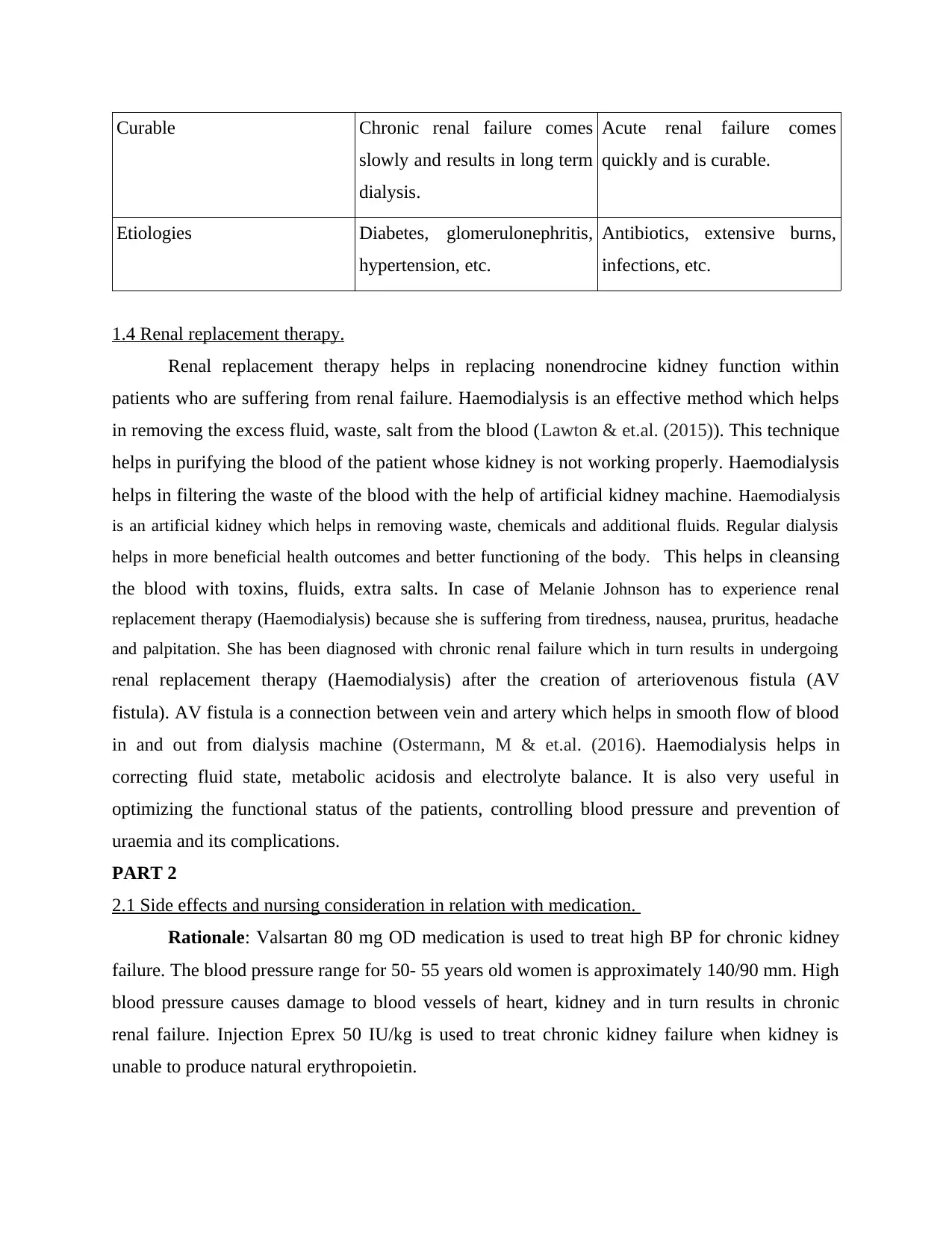
Curable Chronic renal failure comes
slowly and results in long term
dialysis.
Acute renal failure comes
quickly and is curable.
Etiologies Diabetes, glomerulonephritis,
hypertension, etc.
Antibiotics, extensive burns,
infections, etc.
1.4 Renal replacement therapy.
Renal replacement therapy helps in replacing nonendrocine kidney function within
patients who are suffering from renal failure. Haemodialysis is an effective method which helps
in removing the excess fluid, waste, salt from the blood (Lawton & et.al. (2015)). This technique
helps in purifying the blood of the patient whose kidney is not working properly. Haemodialysis
helps in filtering the waste of the blood with the help of artificial kidney machine. Haemodialysis
is an artificial kidney which helps in removing waste, chemicals and additional fluids. Regular dialysis
helps in more beneficial health outcomes and better functioning of the body. This helps in cleansing
the blood with toxins, fluids, extra salts. In case of Melanie Johnson has to experience renal
replacement therapy (Haemodialysis) because she is suffering from tiredness, nausea, pruritus, headache
and palpitation. She has been diagnosed with chronic renal failure which in turn results in undergoing
renal replacement therapy (Haemodialysis) after the creation of arteriovenous fistula (AV
fistula). AV fistula is a connection between vein and artery which helps in smooth flow of blood
in and out from dialysis machine (Ostermann, M & et.al. (2016). Haemodialysis helps in
correcting fluid state, metabolic acidosis and electrolyte balance. It is also very useful in
optimizing the functional status of the patients, controlling blood pressure and prevention of
uraemia and its complications.
PART 2
2.1 Side effects and nursing consideration in relation with medication.
Rationale: Valsartan 80 mg OD medication is used to treat high BP for chronic kidney
failure. The blood pressure range for 50- 55 years old women is approximately 140/90 mm. High
blood pressure causes damage to blood vessels of heart, kidney and in turn results in chronic
renal failure. Injection Eprex 50 IU/kg is used to treat chronic kidney failure when kidney is
unable to produce natural erythropoietin.
slowly and results in long term
dialysis.
Acute renal failure comes
quickly and is curable.
Etiologies Diabetes, glomerulonephritis,
hypertension, etc.
Antibiotics, extensive burns,
infections, etc.
1.4 Renal replacement therapy.
Renal replacement therapy helps in replacing nonendrocine kidney function within
patients who are suffering from renal failure. Haemodialysis is an effective method which helps
in removing the excess fluid, waste, salt from the blood (Lawton & et.al. (2015)). This technique
helps in purifying the blood of the patient whose kidney is not working properly. Haemodialysis
helps in filtering the waste of the blood with the help of artificial kidney machine. Haemodialysis
is an artificial kidney which helps in removing waste, chemicals and additional fluids. Regular dialysis
helps in more beneficial health outcomes and better functioning of the body. This helps in cleansing
the blood with toxins, fluids, extra salts. In case of Melanie Johnson has to experience renal
replacement therapy (Haemodialysis) because she is suffering from tiredness, nausea, pruritus, headache
and palpitation. She has been diagnosed with chronic renal failure which in turn results in undergoing
renal replacement therapy (Haemodialysis) after the creation of arteriovenous fistula (AV
fistula). AV fistula is a connection between vein and artery which helps in smooth flow of blood
in and out from dialysis machine (Ostermann, M & et.al. (2016). Haemodialysis helps in
correcting fluid state, metabolic acidosis and electrolyte balance. It is also very useful in
optimizing the functional status of the patients, controlling blood pressure and prevention of
uraemia and its complications.
PART 2
2.1 Side effects and nursing consideration in relation with medication.
Rationale: Valsartan 80 mg OD medication is used to treat high BP for chronic kidney
failure. The blood pressure range for 50- 55 years old women is approximately 140/90 mm. High
blood pressure causes damage to blood vessels of heart, kidney and in turn results in chronic
renal failure. Injection Eprex 50 IU/kg is used to treat chronic kidney failure when kidney is
unable to produce natural erythropoietin.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
In case of Melanie Johnson she has blood pressure of 190/110 mm Hg. Eprex may result in
various side effects which includes edema, clotting of vascular assess, joint pain and rash (Ahmed,
(2018)). Valsartan 80 mg OD medication have various side effects which includes increase in headaches,
nausea, hypertension, and heart failure (Andersen & et.al. (2016)). Consumption of Valsartan 80 mg OD
is not recommendable for pregnant woman and child rens younger than 6 years.
Nursing consideration while using Valsartan 80 mg OD medication:
Valsartan 80 mg OD may interact with blood pressure drugs which in turn increases the risk of
high blood potassium, kidney problems and low blood pressure (Currie & et.al. (2017)).
Consumption of potassium supplements with Valsartan 80 mg OD results in increase in the
amount of potassium in Melanie Johnson.
Intake of nonsteroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen and naproxen with
Valsartan 80 mg OD results in low kidney function.
Intake of Valsartan 80 mg OD may also result in severe allergic re action which includes hives,
breathing problem and swelling of throat (DeVore & et.al. (2018)).
Nursing consideration while using Injection Eprex 50 IU/kg medication:
Patients who are allergic with epoetin alfa should not use such ingredients with the medication.
No guidelines should be set to give specific medicine. Nurses should evaluate whether it will suit
the patient or not.
It may also result in uncontrolled high blood pressure (Srinivasan & et.al. (2016)).
Nurse should give proper dose to the patient and in case of any allergy and reaction same should
be communicated to healthcare professionals.
Nurses should follow 5 rights of medication.
2.2 Results of GFR and Hb blood test.
The Glomerular filtration rate (GFR) of the Melanie Johnson is 10ml/min/1.73m2 which
states that she is in critical situation of chronic disease failure and kidney dysfunction. The Glomerular
filtration rate (GFR) helps in checking how well the kidney functions and estimates how blood passes
through the glomeruli every minute. There is a decline in the rate of Glomerular filtration rate (GFR)
which turn results in filtration of macromolecules and protein. The normal GFR rate is said to be more
than 90. The Glomerular filtration rate (GFR) is 10ml/min/1.73m2 which states that she is at end stage
renal disease.
The Haemoglobin of the Melanie Johnson is 95g/L. The normal haemoglobin count for women is
12-15 gm/l. Low level of haemoglobin in the body indicates low level of oxygen. High level of
haemoglobin in the body indicates various health problems such as anaemia.
various side effects which includes edema, clotting of vascular assess, joint pain and rash (Ahmed,
(2018)). Valsartan 80 mg OD medication have various side effects which includes increase in headaches,
nausea, hypertension, and heart failure (Andersen & et.al. (2016)). Consumption of Valsartan 80 mg OD
is not recommendable for pregnant woman and child rens younger than 6 years.
Nursing consideration while using Valsartan 80 mg OD medication:
Valsartan 80 mg OD may interact with blood pressure drugs which in turn increases the risk of
high blood potassium, kidney problems and low blood pressure (Currie & et.al. (2017)).
Consumption of potassium supplements with Valsartan 80 mg OD results in increase in the
amount of potassium in Melanie Johnson.
Intake of nonsteroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen and naproxen with
Valsartan 80 mg OD results in low kidney function.
Intake of Valsartan 80 mg OD may also result in severe allergic re action which includes hives,
breathing problem and swelling of throat (DeVore & et.al. (2018)).
Nursing consideration while using Injection Eprex 50 IU/kg medication:
Patients who are allergic with epoetin alfa should not use such ingredients with the medication.
No guidelines should be set to give specific medicine. Nurses should evaluate whether it will suit
the patient or not.
It may also result in uncontrolled high blood pressure (Srinivasan & et.al. (2016)).
Nurse should give proper dose to the patient and in case of any allergy and reaction same should
be communicated to healthcare professionals.
Nurses should follow 5 rights of medication.
2.2 Results of GFR and Hb blood test.
The Glomerular filtration rate (GFR) of the Melanie Johnson is 10ml/min/1.73m2 which
states that she is in critical situation of chronic disease failure and kidney dysfunction. The Glomerular
filtration rate (GFR) helps in checking how well the kidney functions and estimates how blood passes
through the glomeruli every minute. There is a decline in the rate of Glomerular filtration rate (GFR)
which turn results in filtration of macromolecules and protein. The normal GFR rate is said to be more
than 90. The Glomerular filtration rate (GFR) is 10ml/min/1.73m2 which states that she is at end stage
renal disease.
The Haemoglobin of the Melanie Johnson is 95g/L. The normal haemoglobin count for women is
12-15 gm/l. Low level of haemoglobin in the body indicates low level of oxygen. High level of
haemoglobin in the body indicates various health problems such as anaemia.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PART 3
3.1 Teach-back method.
Teach-back method is an effective communication confirmation strategy or technique
which is used by health care providers to confirm whether a care take or a patient has understood
the concept. The patient is asked to communicate the same information to the health care
provider with an intention to improve health literacy (Miller, Lattanzio & Cohen, (2016)). This
helps in reducing the communication gap between healthcare professional and patients in order
to attain better results and care outcomes. Teach-back method is very useful in improving
communication and effective health learning for quality health care results.
3.2 Managing the chronic renal failure by educating individual regarding fluid intake.
Melanie Johnson must prepare a chart diet which contains less sodium and salt. It is very crucial
for her to take right kind of protein in a stipulated amount for better results. She should not consume
processed food like canned meat, frozen meals, sauces, cheese, fast food and salted snacks. Consumption
of unprocessed food which are low at sodium like fresh chicken, fish, vegetables and fruits. Do not use
contents which are high in potassium and sodium. Avoid medicines which contains sodium carbonate or
sodium bicarbonate. Switching of duet plan to high protein and cutting down products such as milk,
cheese, yogurt, etc. Self care behaviour helps in improving health of the individual with chronic disease.
Health literacy is very crucial for Melanie Johnson to treat chronic renal failure. Nonsteroidal anti-
inflammatory drugs (NSAIDs) results in reduced kidney blood flow. Teach-back method will help
patients in understanding the fluid and diet restrictions for kidney failure (Centrella-Nigro &
Alexander, (2017)). This will also help in monitoring the blood pressure, pulse rate and urine
output for better care results and health outcomes. Melanie Johnson should avoid drinking
carbonated drinks which may result in negative health outcomes. Diet must be rich in beans, seeds, low
fat dairy products, fruits, veggies, nuts, etc. Consumption of right amount of protein and fluid helps in
managing the chronic renal failure. Taking medication on time helps in improving the health outcomes of
the Melanie Johnson (Peter & et.al. (2015)). She should have fluid control in the body. She should intake
fluid as prescribed by doctor which is dependent on dialysis setting and urine output. She should also
keep in mind the amount of fluid used at the time of cooking.
CONCLUSION
From the above conducted study it has been summarized that, renal failure is occurred
when the kidney looses the ability to filter the waste from the blood. It can be classified into
3.1 Teach-back method.
Teach-back method is an effective communication confirmation strategy or technique
which is used by health care providers to confirm whether a care take or a patient has understood
the concept. The patient is asked to communicate the same information to the health care
provider with an intention to improve health literacy (Miller, Lattanzio & Cohen, (2016)). This
helps in reducing the communication gap between healthcare professional and patients in order
to attain better results and care outcomes. Teach-back method is very useful in improving
communication and effective health learning for quality health care results.
3.2 Managing the chronic renal failure by educating individual regarding fluid intake.
Melanie Johnson must prepare a chart diet which contains less sodium and salt. It is very crucial
for her to take right kind of protein in a stipulated amount for better results. She should not consume
processed food like canned meat, frozen meals, sauces, cheese, fast food and salted snacks. Consumption
of unprocessed food which are low at sodium like fresh chicken, fish, vegetables and fruits. Do not use
contents which are high in potassium and sodium. Avoid medicines which contains sodium carbonate or
sodium bicarbonate. Switching of duet plan to high protein and cutting down products such as milk,
cheese, yogurt, etc. Self care behaviour helps in improving health of the individual with chronic disease.
Health literacy is very crucial for Melanie Johnson to treat chronic renal failure. Nonsteroidal anti-
inflammatory drugs (NSAIDs) results in reduced kidney blood flow. Teach-back method will help
patients in understanding the fluid and diet restrictions for kidney failure (Centrella-Nigro &
Alexander, (2017)). This will also help in monitoring the blood pressure, pulse rate and urine
output for better care results and health outcomes. Melanie Johnson should avoid drinking
carbonated drinks which may result in negative health outcomes. Diet must be rich in beans, seeds, low
fat dairy products, fruits, veggies, nuts, etc. Consumption of right amount of protein and fluid helps in
managing the chronic renal failure. Taking medication on time helps in improving the health outcomes of
the Melanie Johnson (Peter & et.al. (2015)). She should have fluid control in the body. She should intake
fluid as prescribed by doctor which is dependent on dialysis setting and urine output. She should also
keep in mind the amount of fluid used at the time of cooking.
CONCLUSION
From the above conducted study it has been summarized that, renal failure is occurred
when the kidney looses the ability to filter the waste from the blood. It can be classified into
acute and chronic renal failure. This study concludes, pathophysiology in relation with chronic
renal failure and the renal replacement therapy. Furthermore, it demonstrates side effects and
nursing consideration in relation with medication and managing chronic renal failure by
educating individual.
renal failure and the renal replacement therapy. Furthermore, it demonstrates side effects and
nursing consideration in relation with medication and managing chronic renal failure by
educating individual.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals
Ahmed, A. (2018). A Qualitative Assessment of the Saskatchewan Medication Assessment
Program in Patients with Renal Failure or Renal Replacement (Doctoral dissertation,
University of Saskatchewan).
Andersen, M. B & et.al. (2016). LCZ 696 (Valsartan/Sacubitril)–A Possible New Treatment for
Hypertension and Heart Failure. Basic & clinical pharmacology & toxicology. 118(1). 14-
22.
Beachey, W. (2017). Respiratory Care Anatomy and Physiology-E-Book: Foundations for
Clinical Practice. Elsevier Health Sciences.
Centrella-Nigro, A. M., & Alexander, C. (2017). Using the teach-back method in patient
education to improve patient satisfaction. The Journal of Continuing Education in
Nursing.48(1). 47-52.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Currie, G & et.al. (2017). Effect of valsartan on kidney outcomes in people with impaired
glucose tolerance. Diabetes, Obesity and Metabolism. 19(6). 791-799.
DeVore, A. D & et.al. (2018). Patient and Practice Characteristics Associated with
Sacubitril/Valsartan Use in the United States. Journal of Cardiac Failure.24(8). S98-S99.
Khan, Z & et.al. (2017). Three-dimensional morphometric analysis of the renal
vasculature. American Journal of Physiology-Renal Physiology.314(5). F715-F725.
Klatte, T & et.al. (2015). A literature review of renal surgical anatomy and surgical strategies for
partial nephrectomy. European urology, 68(6), 980-992.
Lawton, P. D & et.al. (2015). Survival of Indigenous Australians receiving renal replacement
therapy: closing the gap?. Medical Journal of Australia.202(4). 200-204.
Mårtensson, J., & Bellomo, R. (2017). Acute Kidney Injury. Inflammation: From Molecular and
Cellular Mechanisms to the Clinic, 1301-1312.
Books and Journals
Ahmed, A. (2018). A Qualitative Assessment of the Saskatchewan Medication Assessment
Program in Patients with Renal Failure or Renal Replacement (Doctoral dissertation,
University of Saskatchewan).
Andersen, M. B & et.al. (2016). LCZ 696 (Valsartan/Sacubitril)–A Possible New Treatment for
Hypertension and Heart Failure. Basic & clinical pharmacology & toxicology. 118(1). 14-
22.
Beachey, W. (2017). Respiratory Care Anatomy and Physiology-E-Book: Foundations for
Clinical Practice. Elsevier Health Sciences.
Centrella-Nigro, A. M., & Alexander, C. (2017). Using the teach-back method in patient
education to improve patient satisfaction. The Journal of Continuing Education in
Nursing.48(1). 47-52.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Currie, G & et.al. (2017). Effect of valsartan on kidney outcomes in people with impaired
glucose tolerance. Diabetes, Obesity and Metabolism. 19(6). 791-799.
DeVore, A. D & et.al. (2018). Patient and Practice Characteristics Associated with
Sacubitril/Valsartan Use in the United States. Journal of Cardiac Failure.24(8). S98-S99.
Khan, Z & et.al. (2017). Three-dimensional morphometric analysis of the renal
vasculature. American Journal of Physiology-Renal Physiology.314(5). F715-F725.
Klatte, T & et.al. (2015). A literature review of renal surgical anatomy and surgical strategies for
partial nephrectomy. European urology, 68(6), 980-992.
Lawton, P. D & et.al. (2015). Survival of Indigenous Australians receiving renal replacement
therapy: closing the gap?. Medical Journal of Australia.202(4). 200-204.
Mårtensson, J., & Bellomo, R. (2017). Acute Kidney Injury. Inflammation: From Molecular and
Cellular Mechanisms to the Clinic, 1301-1312.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Miller, S., Lattanzio, M., & Cohen, S. (2016). “Teach-back” from a patient's
perspective. Nursing2018.46(2). 63-64.
Nishi, E. E., Bergamaschi, C. T., & Campos, R. R. (2015). The crosstalk between the kidney and
the central nervous system: the role of renal nerves in blood pressure
regulation. Experimental physiology.100(5). 479-484.
Ostermann, M & et.al. (2016). Patient selection and timing of continuous renal replacement
therapy. Blood purification. 42(3). 224-237.
Oxburgh, L. (2018). Kidney nephron determination. Annual review of cell and developmental
biology. 34. 427-450.
Peter, D & et.al. (2015). Reducing readmissions using teach-back: enhancing patient and family
education. JONA: The Journal of Nursing Administration. 45(1). 35-42.
Srinivasan, R & et.al. (2016). Assessment of erythropoietin for treatment of anemia in chronic
kidney failure-ESRD patients. Biomedicine & Pharmacotherapy. 82. 44-48.
Online
ANATOMY AND PHYSIOLOGY. 2019. [ONLINE]. Available
through:<https://opentextbc.ca/anatomyandphysiology/chapter/25-4-microscopic-anatomy-
of-the-kidney/>
Pathophysiology of chronic renal failure. 2003. [ONLINE]. Available
through:<https://bjaed.org/article/S1472-2615(17)30020-1/pdf>
Renal System & Kidney Anatomy. 2014. [ONLINE]. Available
through:<http://www.healthcommunities.com/chronic-renal-failure/renal-system-and-
kidney-anatomy.shtml>
perspective. Nursing2018.46(2). 63-64.
Nishi, E. E., Bergamaschi, C. T., & Campos, R. R. (2015). The crosstalk between the kidney and
the central nervous system: the role of renal nerves in blood pressure
regulation. Experimental physiology.100(5). 479-484.
Ostermann, M & et.al. (2016). Patient selection and timing of continuous renal replacement
therapy. Blood purification. 42(3). 224-237.
Oxburgh, L. (2018). Kidney nephron determination. Annual review of cell and developmental
biology. 34. 427-450.
Peter, D & et.al. (2015). Reducing readmissions using teach-back: enhancing patient and family
education. JONA: The Journal of Nursing Administration. 45(1). 35-42.
Srinivasan, R & et.al. (2016). Assessment of erythropoietin for treatment of anemia in chronic
kidney failure-ESRD patients. Biomedicine & Pharmacotherapy. 82. 44-48.
Online
ANATOMY AND PHYSIOLOGY. 2019. [ONLINE]. Available
through:<https://opentextbc.ca/anatomyandphysiology/chapter/25-4-microscopic-anatomy-
of-the-kidney/>
Pathophysiology of chronic renal failure. 2003. [ONLINE]. Available
through:<https://bjaed.org/article/S1472-2615(17)30020-1/pdf>
Renal System & Kidney Anatomy. 2014. [ONLINE]. Available
through:<http://www.healthcommunities.com/chronic-renal-failure/renal-system-and-
kidney-anatomy.shtml>

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





