Comprehensive Clinical Assessment and Planning Case Study Analysis
VerifiedAdded on 2021/06/17
|20
|5819
|28
Case Study
AI Summary
This case study delves into the multifaceted aspects of clinical assessment and planning, examining various scenarios and interventions within a healthcare context. It begins by outlining factors to consider before and after assessments, emphasizing the importance of patient health status, age, and mental capacity. The study then analyzes the psychological factors influencing patient care, including family, friends, and healthcare networks, followed by a detailed examination of a patient's vital signs, including temperature, pulse, respiration, blood pressure, and oxygen saturation. The neurological observation and assessment section explores the collection of data, including consciousness levels, pupil activity, and sensory responses, to determine potential neurological issues. Further analysis is conducted on the patient's age, vital signs, and the steps involved in managing a colostomy bag. The case study also addresses factors associated with immobility, such as visual impairment and dementia, and explores assessment tools like the Stroke Engine. It provides guidance on preparing a patient for mobility and suggests dietary recommendations for patients with dysphagia, promoting dignity and independence during mealtimes. Additionally, the case study covers screening assessments for pressure injuries, intrinsic and extrinsic factors, and strategies to prevent them. Finally, it outlines the nurse's role in the discharge process, ensuring patients are ready for independent living and have a comprehensive understanding of their health management.

Running head: CLINICAL ASSESSMENT AND PLANNING 1
Clinical Assessment and Planning
Student’s Name
Institutional Affiliation
Clinical Assessment and Planning
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL ASSESSMENT AND PLANNING 2
Case study 1
1 (a) Factors to consider before and after clinical assessment
Before the assessment, the nurse should check at the status of health of an individual. A
critically ill individual requires an immediate assessment. The age factor is critical for evaluation
(Ervin, & Kulbok, 2018). Additionally, the nurse should gauge the mental capacity of the patient.
After the assessment, the physician should look at the differences in response between the young
and old patients. Furthermore, the nurse should ask for the occupation of the patient.
(b) The psychological factors include the: relatives and friends of the patient, nurses, and
healthcare network (Ervin, & Kulbok, 2018). Mr Bott leaves alone since the wife is late and the
son is away. The nurse attending to him should be competent enough to carry out final
assessments. The system of healthcare needs to have an array of treatment options that the
patient can decide the mode of care.
(c)
Temperature
Mr Bott's temperature is 36.5º C whereas the average body temperature is 37º C (Al-Ali,
Diab, Kiani, Kopotic, & Tobler, 2016). His temperature is within the normal range.
Pulse
He has a rate of 120 beats per minute. The standard rate ranges from 60-100 pounds in a
minute (Al-Ali et al., 2016). His records show a pulse rate that is higher than usual.
Respirations
His reading is 24 beats per minute. The normal range is 12-20 beats in a minute (Al-Ali et
al., 2016). Therefore, Mr Bott's respiration rates are higher than the normal.
Blood pressure
Case study 1
1 (a) Factors to consider before and after clinical assessment
Before the assessment, the nurse should check at the status of health of an individual. A
critically ill individual requires an immediate assessment. The age factor is critical for evaluation
(Ervin, & Kulbok, 2018). Additionally, the nurse should gauge the mental capacity of the patient.
After the assessment, the physician should look at the differences in response between the young
and old patients. Furthermore, the nurse should ask for the occupation of the patient.
(b) The psychological factors include the: relatives and friends of the patient, nurses, and
healthcare network (Ervin, & Kulbok, 2018). Mr Bott leaves alone since the wife is late and the
son is away. The nurse attending to him should be competent enough to carry out final
assessments. The system of healthcare needs to have an array of treatment options that the
patient can decide the mode of care.
(c)
Temperature
Mr Bott's temperature is 36.5º C whereas the average body temperature is 37º C (Al-Ali,
Diab, Kiani, Kopotic, & Tobler, 2016). His temperature is within the normal range.
Pulse
He has a rate of 120 beats per minute. The standard rate ranges from 60-100 pounds in a
minute (Al-Ali et al., 2016). His records show a pulse rate that is higher than usual.
Respirations
His reading is 24 beats per minute. The normal range is 12-20 beats in a minute (Al-Ali et
al., 2016). Therefore, Mr Bott's respiration rates are higher than the normal.
Blood pressure
CLINICAL ASSESSMENT AND PLANNING 3
The average blood pressure ranges from 120/80 mmHg to 140/90 mmHg (Al-Ali et al.,
2016). Mr Saheed has elevated blood pressure of 180/90 mmHg.
Oxygen Saturation
The standard rates of oxygen levels range from 70 to 100mmHg (Al-Ali et al., 2016). Mr
Saheed has upper quartile oxygen saturation levels. The readings indicate 94mmHg.
2. Neurological observation and Assessment
I would collect the following data during my inspections:
Firstly is the conscious level of Mr Bott. I would ask him if he knows where he is and
who brought him to the hospital. Furthermore, I would slowly open his eyes to examine the level
of activity of the pupil. I would ask him random questions to gauge his response. Additionally, I
would slowly touch his forehead and note whether he is aware of the primary stimuli that I have
generated or otherwise. I would wave my hands in front of his eyes to gauge whether he can
detect my hands and what I am doing.
In the neurological assessment, I would find out which sensory organs are not functioning
correctly. I would look at the exact location of the neurological problem. A good scenario is
determining the part of the brain that the infection has affected (Powers et al., 2015). After
gauging those areas, I would come up with appropriate diagnostic and treatment strategies. I
would then screen for any signs of abnormal conditions in Mr Bott. I would then document my
findings for future references. Additionally, I would test the state of his mind and look at the
general nervous system. Moreover, I would gauge the strength of the muscles and look at the
reflex action.
3. The age: Mr Bott's is of advanced age, nothing can reverse his age
Blood pressure is high; an exercise is a good option for reducing hypertension
The average blood pressure ranges from 120/80 mmHg to 140/90 mmHg (Al-Ali et al.,
2016). Mr Saheed has elevated blood pressure of 180/90 mmHg.
Oxygen Saturation
The standard rates of oxygen levels range from 70 to 100mmHg (Al-Ali et al., 2016). Mr
Saheed has upper quartile oxygen saturation levels. The readings indicate 94mmHg.
2. Neurological observation and Assessment
I would collect the following data during my inspections:
Firstly is the conscious level of Mr Bott. I would ask him if he knows where he is and
who brought him to the hospital. Furthermore, I would slowly open his eyes to examine the level
of activity of the pupil. I would ask him random questions to gauge his response. Additionally, I
would slowly touch his forehead and note whether he is aware of the primary stimuli that I have
generated or otherwise. I would wave my hands in front of his eyes to gauge whether he can
detect my hands and what I am doing.
In the neurological assessment, I would find out which sensory organs are not functioning
correctly. I would look at the exact location of the neurological problem. A good scenario is
determining the part of the brain that the infection has affected (Powers et al., 2015). After
gauging those areas, I would come up with appropriate diagnostic and treatment strategies. I
would then screen for any signs of abnormal conditions in Mr Bott. I would then document my
findings for future references. Additionally, I would test the state of his mind and look at the
general nervous system. Moreover, I would gauge the strength of the muscles and look at the
reflex action.
3. The age: Mr Bott's is of advanced age, nothing can reverse his age
Blood pressure is high; an exercise is a good option for reducing hypertension
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL ASSESSMENT AND PLANNING 4
The temperature is average and should remain untouched.
Exercise can also normalise the respiration rate
The oxygen rate is reasonable. The rate needs maintenance
The pulse rate is higher than usual. Physical regiments lower the rate to average figures.
4. Steps in emptying and changing the Colostomy bag
The nurse needs to obtain the necessary tools to carry out the emptying process. Firstly,
the nurse opens the bag’s Clamp and cuff out its tail. Secondly, the physician transfers the
components of the Colostomy bag into a clean basin or pit latrine (Ambe et al., 2018). The nurse
should note down the pattern size of the stoma (Ambe et al., 2018). The nurse should trace the
boundaries of the hole and carefully remove a small part to come up with an opening (Ambe et
al., 2018). The next step involves the removal of backing material out of the wafer (Ambe et al.,
2018). Furthermore, the nurse should get rid of the previous bag. The nurse throws away the old
container. The new skin underwent inspection and washed without detergents (Ambe et al.,
2018). The nurse then dries the new bag. The nurse then applies paste at the bottom of the bag
(Ambe et al., 2018). Then add deodorant. Get rid of the remaining items used during the
emptying and replacing exercise.
5. (a) Factors associated with immobility
Visual impairment
Loss of sight prevents an individual from moving from one place to the other. One cause of
sight loss is the stroke. The onset of stroke restricts blood flow to the brain (Balasubramanian,
Melendez-Calderon, Roby-Brami, & Burdet, 2015). Therefore, the CNS cannot receive the
necessary nutrients to perform its functions. Moreover, the brain lacks oxygen to carry out its
The temperature is average and should remain untouched.
Exercise can also normalise the respiration rate
The oxygen rate is reasonable. The rate needs maintenance
The pulse rate is higher than usual. Physical regiments lower the rate to average figures.
4. Steps in emptying and changing the Colostomy bag
The nurse needs to obtain the necessary tools to carry out the emptying process. Firstly,
the nurse opens the bag’s Clamp and cuff out its tail. Secondly, the physician transfers the
components of the Colostomy bag into a clean basin or pit latrine (Ambe et al., 2018). The nurse
should note down the pattern size of the stoma (Ambe et al., 2018). The nurse should trace the
boundaries of the hole and carefully remove a small part to come up with an opening (Ambe et
al., 2018). The next step involves the removal of backing material out of the wafer (Ambe et al.,
2018). Furthermore, the nurse should get rid of the previous bag. The nurse throws away the old
container. The new skin underwent inspection and washed without detergents (Ambe et al.,
2018). The nurse then dries the new bag. The nurse then applies paste at the bottom of the bag
(Ambe et al., 2018). Then add deodorant. Get rid of the remaining items used during the
emptying and replacing exercise.
5. (a) Factors associated with immobility
Visual impairment
Loss of sight prevents an individual from moving from one place to the other. One cause of
sight loss is the stroke. The onset of stroke restricts blood flow to the brain (Balasubramanian,
Melendez-Calderon, Roby-Brami, & Burdet, 2015). Therefore, the CNS cannot receive the
necessary nutrients to perform its functions. Moreover, the brain lacks oxygen to carry out its
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL ASSESSMENT AND PLANNING 5
metabolic activities (Balasubramanian et al., 2015). Therefore, the CNS is unable to coordinate
vision. An individual who cannot see properly cannot move from one place to the other.
Hip fracture
The fracture occurs as a result of accidents. When the hip damages, the legs lose the ability to
stand still and support the body mass, therefore one cannot maintain balance (Balasubramanian
et al., 2015). Such an individual cannot move from one place to the other.
Dementia
The disorder refers to the impairment of an individual’s integration capabilities
(Balasubramanian et al., 2015). Dementia occurs as a result of neuronal abnormalities
(Balasubramanian et al., 2015). Such an individual loses the ability to balance the body and
cannot move freely.
(b) Assessment tools
The Stroke Engine
The engine is used to assess the progress of stroke patients in rehabilitation centres. The
tool development aligns with the new technology, and it is easy to use (Balasubramanian et al.,
2015). Furthermore, it has an elaborate description of how to use it (Balasubramanian et al.,
2015). The specification includes the review of the machine, a table of summary, and the
properties of the Engine (Balasubramanian et al., 2015).
(c) Factors to consider before assisting Mr Bott to move around
Before, the nurse can help Mr Bott in movement; they should wash their hands first.
Proper hygiene is essential in handling patients to avoid contaminations which would result in a
new disease (Balasubramanian et al., 2015). The nurse should learn all the precautions in the
patient’s room. Additionally, the nurse should take care not to break any rules. The nurse should
metabolic activities (Balasubramanian et al., 2015). Therefore, the CNS is unable to coordinate
vision. An individual who cannot see properly cannot move from one place to the other.
Hip fracture
The fracture occurs as a result of accidents. When the hip damages, the legs lose the ability to
stand still and support the body mass, therefore one cannot maintain balance (Balasubramanian
et al., 2015). Such an individual cannot move from one place to the other.
Dementia
The disorder refers to the impairment of an individual’s integration capabilities
(Balasubramanian et al., 2015). Dementia occurs as a result of neuronal abnormalities
(Balasubramanian et al., 2015). Such an individual loses the ability to balance the body and
cannot move freely.
(b) Assessment tools
The Stroke Engine
The engine is used to assess the progress of stroke patients in rehabilitation centres. The
tool development aligns with the new technology, and it is easy to use (Balasubramanian et al.,
2015). Furthermore, it has an elaborate description of how to use it (Balasubramanian et al.,
2015). The specification includes the review of the machine, a table of summary, and the
properties of the Engine (Balasubramanian et al., 2015).
(c) Factors to consider before assisting Mr Bott to move around
Before, the nurse can help Mr Bott in movement; they should wash their hands first.
Proper hygiene is essential in handling patients to avoid contaminations which would result in a
new disease (Balasubramanian et al., 2015). The nurse should learn all the precautions in the
patient’s room. Additionally, the nurse should take care not to break any rules. The nurse should
CLINICAL ASSESSMENT AND PLANNING 6
then conduct an introductory session between Mr Bott and themselves. A lively introduction
forms the basis of therapeutic interaction. Moreover, the presentation is in line with the
principles of person-centred care.
The nurse should respect the demands of the patient. They should move patients to the
directions that Mr Bott requests and at his preferred speed. The nurse should adequately arrange
the room before mobilisation (Balasubramanian et al., 2015). The physician should ensure that
the place is spacious. Moreover, the nurse should remove any destructing objects from the way.
The nurse should offer energy foods to the patient before mobilising him.
6 (a) Food suggestions for patients with Dysphagia
Mr Bott should take a lot of liquids. But since people with conditions such as his may
find difficulties in swallowing, the nurse can suggest for liquids with a thicker profile. Thin
profiled liquids such as water and fruit juice may pose a challenge during swallowing (Beck,
Kjaersgaard, Hansen, & Poulsen, 2017). Dysphagia patients cannot readily consume food rich in
calories (Beck et al., 2017). The nutritionists should perform calorie fortification with proteins to
ease swallowing by Mr Bott. The patients should consume more of soft foods (Beck et al., 2017).
Any hard foods such as meat should undergo pondering to improve the chances of the patient to
swallow them.
(b) Promoting dignity and independence of Mr Bott during lunch time
The nurse should provide Mr Bott with food that the patient chooses. The meal should be
full of nutrients and trigger the appetite of Mr Bott. In case the patient finds difficulty in feeding
themselves, the nurse should provide the necessary assistance (Alagiakrishnan, Fisher, & Kurian,
2015). The nurse should only offer thick liquids since the thin ones give dysphagia patients a
problem during swallowing(Alagiakrishnan, Fisher, & Kurian, 2015). The physician should
then conduct an introductory session between Mr Bott and themselves. A lively introduction
forms the basis of therapeutic interaction. Moreover, the presentation is in line with the
principles of person-centred care.
The nurse should respect the demands of the patient. They should move patients to the
directions that Mr Bott requests and at his preferred speed. The nurse should adequately arrange
the room before mobilisation (Balasubramanian et al., 2015). The physician should ensure that
the place is spacious. Moreover, the nurse should remove any destructing objects from the way.
The nurse should offer energy foods to the patient before mobilising him.
6 (a) Food suggestions for patients with Dysphagia
Mr Bott should take a lot of liquids. But since people with conditions such as his may
find difficulties in swallowing, the nurse can suggest for liquids with a thicker profile. Thin
profiled liquids such as water and fruit juice may pose a challenge during swallowing (Beck,
Kjaersgaard, Hansen, & Poulsen, 2017). Dysphagia patients cannot readily consume food rich in
calories (Beck et al., 2017). The nutritionists should perform calorie fortification with proteins to
ease swallowing by Mr Bott. The patients should consume more of soft foods (Beck et al., 2017).
Any hard foods such as meat should undergo pondering to improve the chances of the patient to
swallow them.
(b) Promoting dignity and independence of Mr Bott during lunch time
The nurse should provide Mr Bott with food that the patient chooses. The meal should be
full of nutrients and trigger the appetite of Mr Bott. In case the patient finds difficulty in feeding
themselves, the nurse should provide the necessary assistance (Alagiakrishnan, Fisher, & Kurian,
2015). The nurse should only offer thick liquids since the thin ones give dysphagia patients a
problem during swallowing(Alagiakrishnan, Fisher, & Kurian, 2015). The physician should
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL ASSESSMENT AND PLANNING 7
provide food that follows a particular order. The nutritionist should ensure that the patient feeds
on fortified and well-pounded foods (Alagiakrishnan, Fisher, & Kurian, 2015). A dysphagic
patient should follow a strict timetable during feeding.
7 (a) Screening assessment for prevention and management of pressure injuries
The first step is to screen the damage and identify the causes and possible consequences
of the wound. Secondly, the nurse should consult both the patients and the family members on
reasonable treatment procedures (Qaseem, Mir, Starkey, & Denberg, 2015). Additionally, the
physician should come up with an appropriate healthcare plan. The treatment plan should focus
on the patient and also lack side effects (Qaseem et al., 2015). Moreover, the health facility
should only allow experts to do management. The nurse should consider the views of the patient
before the onset of the care. The health organisation should provide nurses with the necessary
equipment to manage the injuries.
(b) Intrinsic and extrinsic factors that cause pressure injuries
The difficulty in movement-patients who cannot change locations can easily be affected
by the pain ulcers (de Carvalho et al., 2016). The patient who eats unbalanced diet is at risk of
getting pressure ulcers than those who eat a balanced diet (de Carvalho et al., 2016). Moreover,
patients who have a problem with the flow of blood can develop pressure diseases (de Carvalho
et al., 2016). The disruption of the flow of blood leads to arterial complications.
(c) Strategy to prevent pressure injuries in Mr Bott
The nurses should aid Mr Bott in the movement from one place to the other to prevent
him from falling (Tanwar, Kundu, & Vashisht, 2016). Furthermore, the physician should ensure
that Bott consumes a balanced diet (Tanwar, Kundu, & Vashisht, 2016). The doctors should
provide food that follows a particular order. The nutritionist should ensure that the patient feeds
on fortified and well-pounded foods (Alagiakrishnan, Fisher, & Kurian, 2015). A dysphagic
patient should follow a strict timetable during feeding.
7 (a) Screening assessment for prevention and management of pressure injuries
The first step is to screen the damage and identify the causes and possible consequences
of the wound. Secondly, the nurse should consult both the patients and the family members on
reasonable treatment procedures (Qaseem, Mir, Starkey, & Denberg, 2015). Additionally, the
physician should come up with an appropriate healthcare plan. The treatment plan should focus
on the patient and also lack side effects (Qaseem et al., 2015). Moreover, the health facility
should only allow experts to do management. The nurse should consider the views of the patient
before the onset of the care. The health organisation should provide nurses with the necessary
equipment to manage the injuries.
(b) Intrinsic and extrinsic factors that cause pressure injuries
The difficulty in movement-patients who cannot change locations can easily be affected
by the pain ulcers (de Carvalho et al., 2016). The patient who eats unbalanced diet is at risk of
getting pressure ulcers than those who eat a balanced diet (de Carvalho et al., 2016). Moreover,
patients who have a problem with the flow of blood can develop pressure diseases (de Carvalho
et al., 2016). The disruption of the flow of blood leads to arterial complications.
(c) Strategy to prevent pressure injuries in Mr Bott
The nurses should aid Mr Bott in the movement from one place to the other to prevent
him from falling (Tanwar, Kundu, & Vashisht, 2016). Furthermore, the physician should ensure
that Bott consumes a balanced diet (Tanwar, Kundu, & Vashisht, 2016). The doctors should
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL ASSESSMENT AND PLANNING 8
check to regulate the blood flow. If the movement of blood is abnormal, it needs urgent
rectification (Tanwar, Kundu, & Vashisht, 2016).
(d) The treatment and management of pressure should assume a collaborative approach. The
patient’s view on the best treatment option should take centre stage (Boyko, Longaker, & Yang,
2018). As I nurse, I need to consult with my fellow professionals to come up with the best ways
of managing the condition. Nurses who are unsure of the treatment options should opt for
evidence-based research using the available e-sources (Boyko, Longaker, & Yang, 2018). The
parent health organisation also has a pivot role to play. The health facility should avail the
necessary resources for the treatment and management of pressure injuries (Boyko, Longaker, &
Yang, 2018). Additionally, the parent hospital should hire the services of a translator when
necessary.
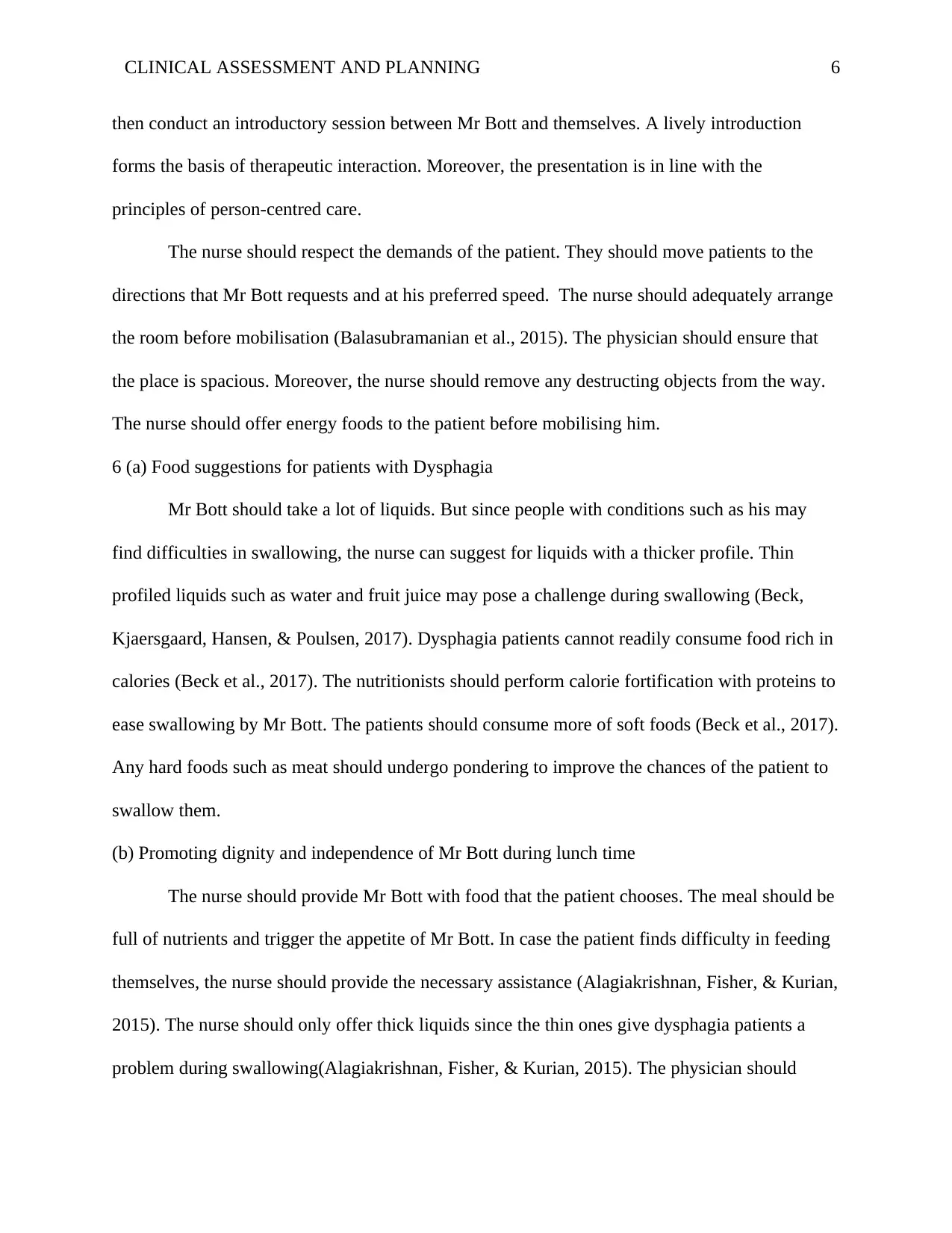
(e) Progress note on Pressure Injury (Cereda, Klersy, Serioli, Crespi, & D'andrea, 2015)
Problem Strategy/Solution
Poor diet Improving diet to accommodate all food components
Disruption in the flow of
blood
Implementation of corrective measures to restore the normal
blood flow
Difficulty in walking Provision of walking aids
Helping Mr Bott in moving from one place to the other.
Proper lighting of the hospital corridors.
8 (a) Role of nurse in the discharge process
The nurse should discharge the patients when their conditions have improved. Mr Bott
should free himself when he can walk freely. Additionally, the patient should contribute to the
check to regulate the blood flow. If the movement of blood is abnormal, it needs urgent
rectification (Tanwar, Kundu, & Vashisht, 2016).
(d) The treatment and management of pressure should assume a collaborative approach. The
patient’s view on the best treatment option should take centre stage (Boyko, Longaker, & Yang,
2018). As I nurse, I need to consult with my fellow professionals to come up with the best ways
of managing the condition. Nurses who are unsure of the treatment options should opt for
evidence-based research using the available e-sources (Boyko, Longaker, & Yang, 2018). The
parent health organisation also has a pivot role to play. The health facility should avail the
necessary resources for the treatment and management of pressure injuries (Boyko, Longaker, &
Yang, 2018). Additionally, the parent hospital should hire the services of a translator when
necessary.
(e) Progress note on Pressure Injury (Cereda, Klersy, Serioli, Crespi, & D'andrea, 2015)
Problem Strategy/Solution
Poor diet Improving diet to accommodate all food components
Disruption in the flow of
blood
Implementation of corrective measures to restore the normal
blood flow
Difficulty in walking Provision of walking aids
Helping Mr Bott in moving from one place to the other.
Proper lighting of the hospital corridors.
8 (a) Role of nurse in the discharge process
The nurse should discharge the patients when their conditions have improved. Mr Bott
should free himself when he can walk freely. Additionally, the patient should contribute to the
CLINICAL ASSESSMENT AND PLANNING 9
option of their discharge (Morton, Fontaine, Hudak, & Gallo, 2017). A patient who says that they
are still unwell should stay longer in the hospital. However, a patient who is on their path to
recovery should attain a discharge. Before the release, the hospital administration should have a
say (Morton et al., 2017). Moreover, the family members should ascertain whether the patient is
fit enough for discharge. The community should support Mr Bott by aiding him in walking
before he can entirely walk on his own.
(b) Risks of overstaying in the hospital
Overstay in hospital leads to muscle problems. An individual's body gains a prolonged
stay hence weakens thereby finding difficulties in doing daily chores (Abetz, Adams, Newnham,
Smit, & Mitra, 2017). Secondly, the patient can develop sores at some body parts which are
experiencing pressure when an individual lies down (Abetz et al., 2017). Moreover, the patient
gets depressed due to loneliness and inability to carry out their chores (Abetz et al., 2017).
9. Factors to consider before the beginning of the shift
• Whether the resources needed are ready
Before I start to attend to Mr Bott, I should ensure that all treatment items are in place. The
necessary equipment is necessary to carry out substantial medical attention (Abetz et al., 2017).
Availability of treatment manuals
The treatment guidelines should be ready. In case of the unclear mode of treatment, the manuals
should guide the nurse. The physician should explain the various treatment options to the patient
and let them chose one (Abetz et al., 2017).
Evidence-based care is necessary
option of their discharge (Morton, Fontaine, Hudak, & Gallo, 2017). A patient who says that they
are still unwell should stay longer in the hospital. However, a patient who is on their path to
recovery should attain a discharge. Before the release, the hospital administration should have a
say (Morton et al., 2017). Moreover, the family members should ascertain whether the patient is
fit enough for discharge. The community should support Mr Bott by aiding him in walking
before he can entirely walk on his own.
(b) Risks of overstaying in the hospital
Overstay in hospital leads to muscle problems. An individual's body gains a prolonged
stay hence weakens thereby finding difficulties in doing daily chores (Abetz, Adams, Newnham,
Smit, & Mitra, 2017). Secondly, the patient can develop sores at some body parts which are
experiencing pressure when an individual lies down (Abetz et al., 2017). Moreover, the patient
gets depressed due to loneliness and inability to carry out their chores (Abetz et al., 2017).
9. Factors to consider before the beginning of the shift
• Whether the resources needed are ready
Before I start to attend to Mr Bott, I should ensure that all treatment items are in place. The
necessary equipment is necessary to carry out substantial medical attention (Abetz et al., 2017).
Availability of treatment manuals
The treatment guidelines should be ready. In case of the unclear mode of treatment, the manuals
should guide the nurse. The physician should explain the various treatment options to the patient
and let them chose one (Abetz et al., 2017).
Evidence-based care is necessary
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL ASSESSMENT AND PLANNING 10
The treatment tailored towards Mr Bott should relate to current research findings. The
methodology should have supporting literature from globally accepted scientists (Abetz et al.,
2017).
Availability of other colleagues
I should ensure that at least two colleagues are available for consultations. If the nurse forgets a
critical treatment step, the workmates become handy (Abetz et al., 2017).
Availability of Mr Bott's family members
His wife is late, and the son is far from him. The family members should be close to assist him in
making decisions (Abetz et al., 2017).
Mr Bott's opinion
The stand of a patient is essential during treatment. I would allow him to choose the
treatment option that suits his preferences. By so doing, I am ensuring person-centred care
(Abetz et al., 2017).
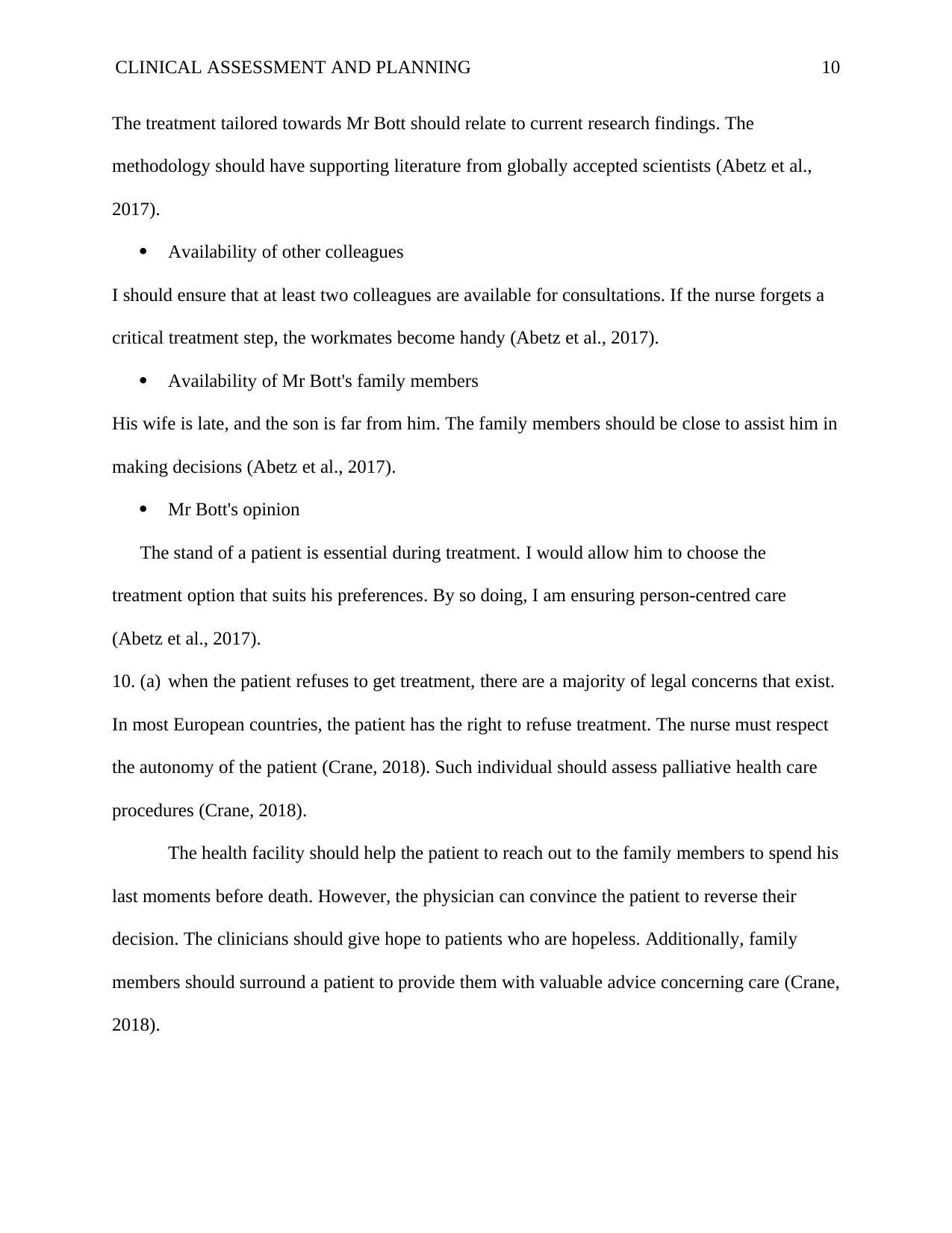
10. (a) when the patient refuses to get treatment, there are a majority of legal concerns that exist.
In most European countries, the patient has the right to refuse treatment. The nurse must respect
the autonomy of the patient (Crane, 2018). Such individual should assess palliative health care
procedures (Crane, 2018).
The health facility should help the patient to reach out to the family members to spend his
last moments before death. However, the physician can convince the patient to reverse their
decision. The clinicians should give hope to patients who are hopeless. Additionally, family
members should surround a patient to provide them with valuable advice concerning care (Crane,
2018).
The treatment tailored towards Mr Bott should relate to current research findings. The
methodology should have supporting literature from globally accepted scientists (Abetz et al.,
2017).
Availability of other colleagues
I should ensure that at least two colleagues are available for consultations. If the nurse forgets a
critical treatment step, the workmates become handy (Abetz et al., 2017).
Availability of Mr Bott's family members
His wife is late, and the son is far from him. The family members should be close to assist him in
making decisions (Abetz et al., 2017).
Mr Bott's opinion
The stand of a patient is essential during treatment. I would allow him to choose the
treatment option that suits his preferences. By so doing, I am ensuring person-centred care
(Abetz et al., 2017).
10. (a) when the patient refuses to get treatment, there are a majority of legal concerns that exist.
In most European countries, the patient has the right to refuse treatment. The nurse must respect
the autonomy of the patient (Crane, 2018). Such individual should assess palliative health care
procedures (Crane, 2018).
The health facility should help the patient to reach out to the family members to spend his
last moments before death. However, the physician can convince the patient to reverse their
decision. The clinicians should give hope to patients who are hopeless. Additionally, family
members should surround a patient to provide them with valuable advice concerning care (Crane,
2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL ASSESSMENT AND PLANNING 11
The patient should appoint both the enduring guardian and the attorney in case they lose the
ability to reason.
The enduring guardian has the responsibility to decide the fate of that patient well in
good time (Crane, 2018). The attorney can use their constitutional power to aid in end-of-life
decision-making process (Crane, 2018). A patient who is bedridden and is not responding to
treatment is free to terminate treatment. An individual who opts for that should do it. The nurses
and the health fraternity should morally support the family members of the patient (Crane, 2018).
Additionally, nurses are not allowed to take part in the suicidal death of patients.
(b)
The new standards require all nursing students from the university to gain registration
from the body (Cashin et al., 2015). The nurse must practice by ethical and professional conducts
(Cashin et al., 2015). The new rules enable nurses to offer high-quality care.
PART B
1. (a) The standards dictate that a patient who is critically ill should receive argent and quality
care (Cashin et al., 2015). Every patient has the right to care, regardless of the time they visit
the health facility.
(b) The nurse should ask for the appropriate recording sheet from the health facility (Cashin
et al., 2015). Additionally, the nurse should consult widely to ensure that she records the
right information.
(c) Additional parameters on pressure ulcers (Cashin et al., 2015)
Assessment Nursing
problem
Goals Intervention Evaluation
Decreased
mobility
Unbalanced
diet
Within a month
Provision of a
balanced diet
The health facility is
to place Mr Bott in
a balanced diet for a
month
Mr Bott should
improve his
movement
capacity after a
The patient should appoint both the enduring guardian and the attorney in case they lose the
ability to reason.
The enduring guardian has the responsibility to decide the fate of that patient well in
good time (Crane, 2018). The attorney can use their constitutional power to aid in end-of-life
decision-making process (Crane, 2018). A patient who is bedridden and is not responding to
treatment is free to terminate treatment. An individual who opts for that should do it. The nurses
and the health fraternity should morally support the family members of the patient (Crane, 2018).
Additionally, nurses are not allowed to take part in the suicidal death of patients.
(b)
The new standards require all nursing students from the university to gain registration
from the body (Cashin et al., 2015). The nurse must practice by ethical and professional conducts
(Cashin et al., 2015). The new rules enable nurses to offer high-quality care.
PART B
1. (a) The standards dictate that a patient who is critically ill should receive argent and quality
care (Cashin et al., 2015). Every patient has the right to care, regardless of the time they visit
the health facility.
(b) The nurse should ask for the appropriate recording sheet from the health facility (Cashin
et al., 2015). Additionally, the nurse should consult widely to ensure that she records the
right information.
(c) Additional parameters on pressure ulcers (Cashin et al., 2015)
Assessment Nursing
problem
Goals Intervention Evaluation
Decreased
mobility
Unbalanced
diet
Within a month
Provision of a
balanced diet
The health facility is
to place Mr Bott in
a balanced diet for a
month
Mr Bott should
improve his
movement
capacity after a
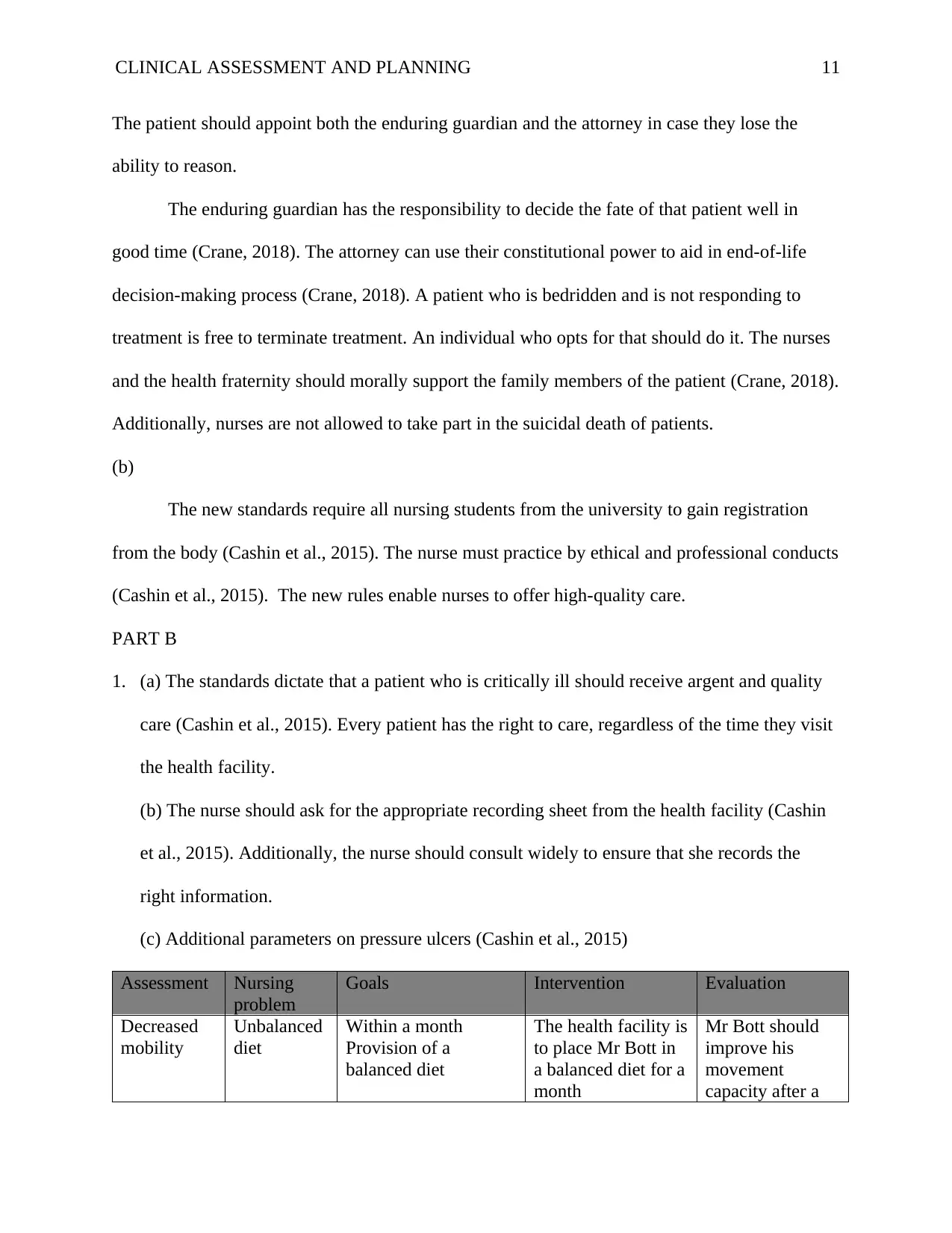
CLINICAL ASSESSMENT AND PLANNING 12
month
Poor blood
flow
Radioactivity
scanning of vessels to
rectify any defections
in the blood channels
Takes one week of
surveillance and the
other week for
defect correction
The blood flow
should return to
normal after the
third week
Broken hip
bones
Scan and rectify the
fracture
Takes six months to
a year to scan and
mend a broken bone
Mr Bott should
be walking
unaided after six
months
Case study 2
1. Stages of Ella’s growth and development
Ella is in the age of going to school which begins from age 5 to 11 years old (Smith,
Cowie, & Blades, 2015). In this stage, children migrate from mid-childhood into the onset of
puberty (Smith, Cowie, & Blades, 2015). Children at this point are inquisitive and ready to learn.
Additionally, they explore a lot and are highly active. They learn new things and are very
experimental in their excursions (Smith, Cowie, & Blades, 2015). Cerebral palsy inhibits the
growth and development of these children due to their fresh tissues. The cells are dividing
actively hence can quickly acquire a new disease (Smith, Cowie, & Blades, 2015). The stage of
development should receive a close monitor to control.
2. (a) Health Issues associated with Cerebral palsy
Malnutrition
Gastrointestinal infections
Bladder abnormalities
Food drooling
Adolescence
Sleeping abnormalities (Samdani et al., 2016)
(b) Accuracy
month
Poor blood
flow
Radioactivity
scanning of vessels to
rectify any defections
in the blood channels
Takes one week of
surveillance and the
other week for
defect correction
The blood flow
should return to
normal after the
third week
Broken hip
bones
Scan and rectify the
fracture
Takes six months to
a year to scan and
mend a broken bone
Mr Bott should
be walking
unaided after six
months
Case study 2
1. Stages of Ella’s growth and development
Ella is in the age of going to school which begins from age 5 to 11 years old (Smith,
Cowie, & Blades, 2015). In this stage, children migrate from mid-childhood into the onset of
puberty (Smith, Cowie, & Blades, 2015). Children at this point are inquisitive and ready to learn.
Additionally, they explore a lot and are highly active. They learn new things and are very
experimental in their excursions (Smith, Cowie, & Blades, 2015). Cerebral palsy inhibits the
growth and development of these children due to their fresh tissues. The cells are dividing
actively hence can quickly acquire a new disease (Smith, Cowie, & Blades, 2015). The stage of
development should receive a close monitor to control.
2. (a) Health Issues associated with Cerebral palsy
Malnutrition
Gastrointestinal infections
Bladder abnormalities
Food drooling
Adolescence
Sleeping abnormalities (Samdani et al., 2016)
(b) Accuracy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





