BHS203A: Clinical Diagnosis Case Study - Ms. Diana F's Diagnosis
VerifiedAdded on 2022/11/07
|15
|3058
|93
Case Study
AI Summary
This case study presents the clinical diagnosis of Ms. Diana F, a 27-year-old female, exhibiting worsening lower abdominal pain, with a two-year history of occasional abdominal pain accompanied by diarrhea, sometimes with blood, and weight loss. The patient's history includes childhood asthma and a tonsillectomy. The assessment includes detailed questioning about the patient's symptoms, past medical and family history, social habits (smoking and alcohol consumption), allergies, and a review of systems. Vital signs revealed a fever, tachycardia, and normal blood pressure and respiratory rate. Physical examination revealed a tender abdomen with hyperactive bowel sounds. The patient's blood tests showed elevated white blood cell count, ESR, and CRP, indicating inflammation. Differential diagnoses considered included ulcerative colitis, Crohn's disease, colorectal cancer, and infectious colitis. Based on the patient's presentation, history, and investigations, the diagnosis of Crohn's disease was made. The document includes a referral letter to a nutritionist, detailing the patient's condition, treatment, and lab results. The case study highlights the importance of considering multiple factors in clinical diagnosis.

Running head: CLININICAL DIAGNOSIS 1
Clinical Diagnosis
Students Name
Institutional Affiliation
Clinical Diagnosis
Students Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
CLINICAL DIAGNOSIS
Introduction
The patient is Ms Diana F, a 27-year-old female, presented for treatment of lower abdominal
pain that is worsening.
History of presenting symptom and illness
Patient reports that the pain started four days ago and has been increasing in intensity
prompting seek for treatment. The pain is located in the lower abdomen and is cramp-like and
does not radiate to any parts of the abdomen. The patient states the pain to be accompanied by
sweating and diarrhoea. The patient reports her pain to be at 7. The patient says that since two
years ago, she has been having abdominal pain occasional times with diarrhoea that sometimes
contains blood. Some of the questions I would ask include; what pattern does the pain take over
24 hours? Does the pain have an effect on daily activities? Can you explain a single pain
episode? How often are your bowel movements? Have you experienced any changes in bowel
movements? How often do you experience bloody diarrhea and how much is it?
Past medical history
The patient has a history of childhood asthma which was effectively controlled. She had
tonsillectomy done at the age of 15 years and reports no complications afterwards. The patient
has no history of any previous GIT problems such as appendicitis, ulcers or gall bladder disease.
No previous abdominal surgeries or any injuries to the abdomen.
Family history
CLINICAL DIAGNOSIS
Introduction
The patient is Ms Diana F, a 27-year-old female, presented for treatment of lower abdominal
pain that is worsening.
History of presenting symptom and illness
Patient reports that the pain started four days ago and has been increasing in intensity
prompting seek for treatment. The pain is located in the lower abdomen and is cramp-like and
does not radiate to any parts of the abdomen. The patient states the pain to be accompanied by
sweating and diarrhoea. The patient reports her pain to be at 7. The patient says that since two
years ago, she has been having abdominal pain occasional times with diarrhoea that sometimes
contains blood. Some of the questions I would ask include; what pattern does the pain take over
24 hours? Does the pain have an effect on daily activities? Can you explain a single pain
episode? How often are your bowel movements? Have you experienced any changes in bowel
movements? How often do you experience bloody diarrhea and how much is it?
Past medical history
The patient has a history of childhood asthma which was effectively controlled. She had
tonsillectomy done at the age of 15 years and reports no complications afterwards. The patient
has no history of any previous GIT problems such as appendicitis, ulcers or gall bladder disease.
No previous abdominal surgeries or any injuries to the abdomen.
Family history
3
Mother has a history of suffering from chronic asthma and eczema. There is no history of
GIT problems in the family neither there is chronic abdominal pains or diarrhea. No history of
cigarette smoking or alcohol use.
Social history
She smokes cigarette at least 10 per day and takes alcohol during weekends
approximately 3-5 drinks. Cigarette smoking triggers the relapse if inflammatory conditions such
as asthma and crohns disease.
Medical allergies
Patient reports having an allergy to NSAIDS and no known food allergy. Asthma is
related to development of crohns disease. The patient might be allergic to pollen, cold or fur and
the GIT symptoms may exacerbate during exposure to this allergens.
Systems Review to ensure that there are not any other conditions or complications.
GIT system.
I will ask on the feeding patterns of the patient and ask the time the last meal was
ingested. The rationale is because normally after meals, there is an increase in bowel sounds.
Approximately 5 hours after a meal, the bowel sounds are heard rapidly on the right lower
quadrant during emptying into the large intestine. I will ask about the duration of the diarrhea.
An acute diarrhea originates from an infection like fecal oral transmission and lasts to a
maximum of two weeks. Chronic diarrhea lasts more than four weeks and it is normally
associated with crohns disease or ulcerative colitis (Aganzo, Luiza, Herrero, &Vazquez, 2018). I
will ask on the amount of diarrhea, the frequency and viscosity. Watery frequent stools that
Mother has a history of suffering from chronic asthma and eczema. There is no history of
GIT problems in the family neither there is chronic abdominal pains or diarrhea. No history of
cigarette smoking or alcohol use.
Social history
She smokes cigarette at least 10 per day and takes alcohol during weekends
approximately 3-5 drinks. Cigarette smoking triggers the relapse if inflammatory conditions such
as asthma and crohns disease.
Medical allergies
Patient reports having an allergy to NSAIDS and no known food allergy. Asthma is
related to development of crohns disease. The patient might be allergic to pollen, cold or fur and
the GIT symptoms may exacerbate during exposure to this allergens.
Systems Review to ensure that there are not any other conditions or complications.
GIT system.
I will ask on the feeding patterns of the patient and ask the time the last meal was
ingested. The rationale is because normally after meals, there is an increase in bowel sounds.
Approximately 5 hours after a meal, the bowel sounds are heard rapidly on the right lower
quadrant during emptying into the large intestine. I will ask about the duration of the diarrhea.
An acute diarrhea originates from an infection like fecal oral transmission and lasts to a
maximum of two weeks. Chronic diarrhea lasts more than four weeks and it is normally
associated with crohns disease or ulcerative colitis (Aganzo, Luiza, Herrero, &Vazquez, 2018). I
will ask on the amount of diarrhea, the frequency and viscosity. Watery frequent stools that
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
occur in large amounts originate from the small intestine. Mucoid, pus or blood-stained stools
originate from inflammatory cases of colon and rectum.
Respiratory system
I will assess for any symptoms of asthma exacerbation or occurrence of pneumonia as a
complication. Chest pain experienced in pneumonia can be referred to the abdomen and mislead
the diagnosis.
Integumentary system
The patient has a history of eczema in the family. I will ask the patient on the age of onset
of eczema on the mother and assess for any symptoms. I will perform immune tests since eczema
is an autoimmune disease.
Genitourinary system
I will ask on the frequency, of urination and any changes of the past days. Urinary
infection can lead to conditions such as appendicitis or diverticulum that can present as lower
abdominal pain (Ciccone et al., 2015). I will ask on the last menstrual period and perform a
pregnancy test since case of ruptured ectopic can present with lower abdominal pain.
Musculoskeletal system
I will ask on evidence of joint swelling. Patient with Crohn’s disease present with
inflammation of joints. Performing range of motion on joints and palpating them can reveal areas
of swelling (Mahmood, Shabbir, Chistol, I., & Khan, 2019).
occur in large amounts originate from the small intestine. Mucoid, pus or blood-stained stools
originate from inflammatory cases of colon and rectum.
Respiratory system
I will assess for any symptoms of asthma exacerbation or occurrence of pneumonia as a
complication. Chest pain experienced in pneumonia can be referred to the abdomen and mislead
the diagnosis.
Integumentary system
The patient has a history of eczema in the family. I will ask the patient on the age of onset
of eczema on the mother and assess for any symptoms. I will perform immune tests since eczema
is an autoimmune disease.
Genitourinary system
I will ask on the frequency, of urination and any changes of the past days. Urinary
infection can lead to conditions such as appendicitis or diverticulum that can present as lower
abdominal pain (Ciccone et al., 2015). I will ask on the last menstrual period and perform a
pregnancy test since case of ruptured ectopic can present with lower abdominal pain.
Musculoskeletal system
I will ask on evidence of joint swelling. Patient with Crohn’s disease present with
inflammation of joints. Performing range of motion on joints and palpating them can reveal areas
of swelling (Mahmood, Shabbir, Chistol, I., & Khan, 2019).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
General appearance
The patient appears weak, and tired. She has an unsteady gait, and it’s evident from her
facial expression that she is in pain. The patient is uncomfortable, has her arms wrapped around
her lower abdomen. The general appearance contributes to my coming up with the diagnosis of
Crohns disease.
Vital observations
Temperature 38.5⁰C
Heart rate- 105 beats/min
BP- 120/80 mmHg
RR- 16b/min.
Normal ranges of temperature are 36.5-37.5⁰C. A temperature above 38⁰C depicts that
the patient has a fever. Regarding Ms Diana, with a temperature of 38.5⁰C, it is evident that she
is suffering from an infection. A heart rate that is over 100 beats/min is considered tachycardia. It
can be caused due to pain, infection, smoking, excessive use of alcohol or cardiac disease
(Carroll et al., 2017). It's also the first sign when the patient is going to shock. The respiratory
rate and blood pressure are within normal ranges of an adult. The vital signs recording imply that
the patient is in pain and has an infection or an inflammatory disease (Birimberg-Schwartz et al.,
2016). I will consider taking the SpO2 to identify the tissue perfusion.
Gastrointestinal examination
General appearance
The patient appears weak, and tired. She has an unsteady gait, and it’s evident from her
facial expression that she is in pain. The patient is uncomfortable, has her arms wrapped around
her lower abdomen. The general appearance contributes to my coming up with the diagnosis of
Crohns disease.
Vital observations
Temperature 38.5⁰C
Heart rate- 105 beats/min
BP- 120/80 mmHg
RR- 16b/min.
Normal ranges of temperature are 36.5-37.5⁰C. A temperature above 38⁰C depicts that
the patient has a fever. Regarding Ms Diana, with a temperature of 38.5⁰C, it is evident that she
is suffering from an infection. A heart rate that is over 100 beats/min is considered tachycardia. It
can be caused due to pain, infection, smoking, excessive use of alcohol or cardiac disease
(Carroll et al., 2017). It's also the first sign when the patient is going to shock. The respiratory
rate and blood pressure are within normal ranges of an adult. The vital signs recording imply that
the patient is in pain and has an infection or an inflammatory disease (Birimberg-Schwartz et al.,
2016). I will consider taking the SpO2 to identify the tissue perfusion.
Gastrointestinal examination
6
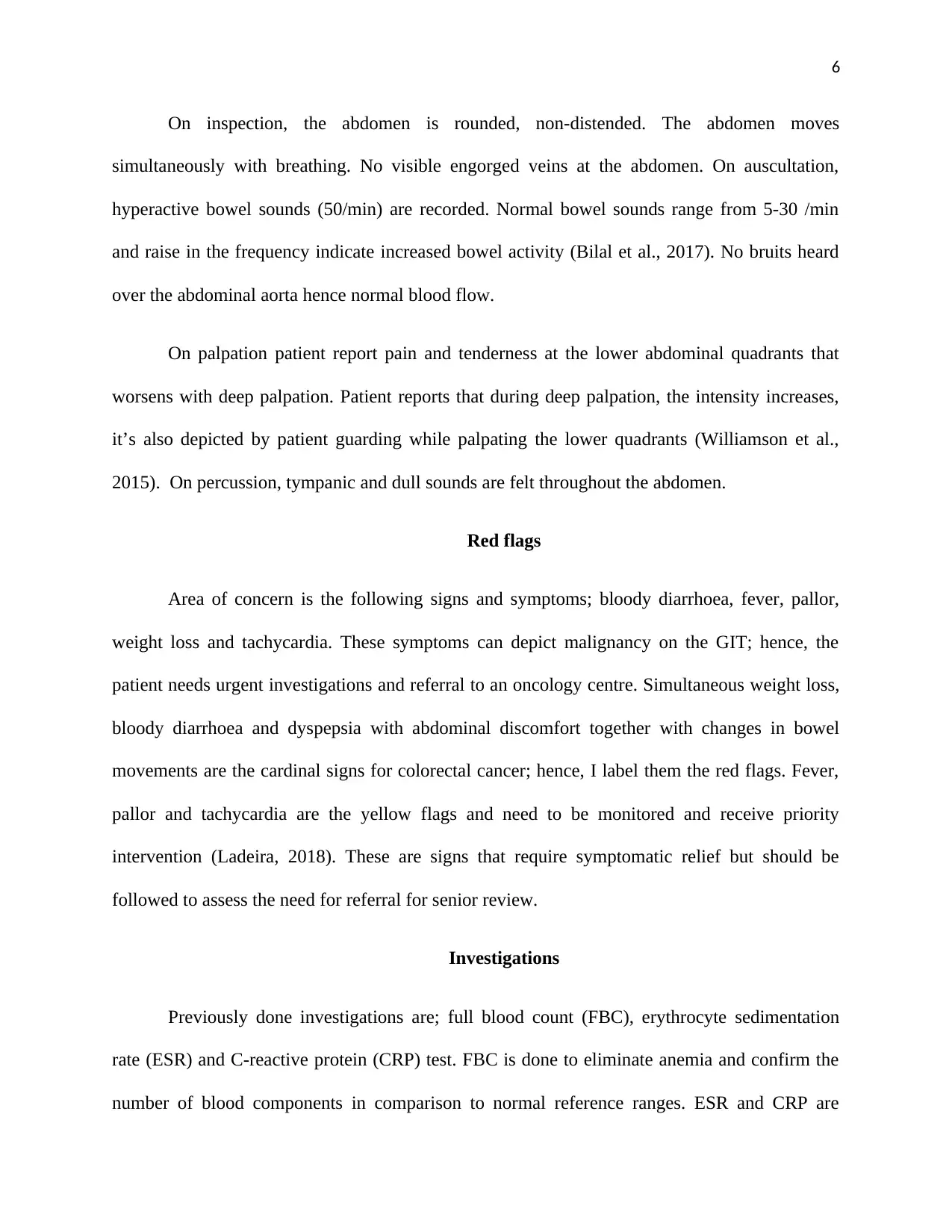
On inspection, the abdomen is rounded, non-distended. The abdomen moves
simultaneously with breathing. No visible engorged veins at the abdomen. On auscultation,
hyperactive bowel sounds (50/min) are recorded. Normal bowel sounds range from 5-30 /min
and raise in the frequency indicate increased bowel activity (Bilal et al., 2017). No bruits heard
over the abdominal aorta hence normal blood flow.
On palpation patient report pain and tenderness at the lower abdominal quadrants that
worsens with deep palpation. Patient reports that during deep palpation, the intensity increases,
it’s also depicted by patient guarding while palpating the lower quadrants (Williamson et al.,
2015). On percussion, tympanic and dull sounds are felt throughout the abdomen.
Red flags
Area of concern is the following signs and symptoms; bloody diarrhoea, fever, pallor,
weight loss and tachycardia. These symptoms can depict malignancy on the GIT; hence, the
patient needs urgent investigations and referral to an oncology centre. Simultaneous weight loss,
bloody diarrhoea and dyspepsia with abdominal discomfort together with changes in bowel
movements are the cardinal signs for colorectal cancer; hence, I label them the red flags. Fever,
pallor and tachycardia are the yellow flags and need to be monitored and receive priority
intervention (Ladeira, 2018). These are signs that require symptomatic relief but should be
followed to assess the need for referral for senior review.
Investigations
Previously done investigations are; full blood count (FBC), erythrocyte sedimentation
rate (ESR) and C-reactive protein (CRP) test. FBC is done to eliminate anemia and confirm the
number of blood components in comparison to normal reference ranges. ESR and CRP are
On inspection, the abdomen is rounded, non-distended. The abdomen moves
simultaneously with breathing. No visible engorged veins at the abdomen. On auscultation,
hyperactive bowel sounds (50/min) are recorded. Normal bowel sounds range from 5-30 /min
and raise in the frequency indicate increased bowel activity (Bilal et al., 2017). No bruits heard
over the abdominal aorta hence normal blood flow.
On palpation patient report pain and tenderness at the lower abdominal quadrants that
worsens with deep palpation. Patient reports that during deep palpation, the intensity increases,
it’s also depicted by patient guarding while palpating the lower quadrants (Williamson et al.,
2015). On percussion, tympanic and dull sounds are felt throughout the abdomen.
Red flags
Area of concern is the following signs and symptoms; bloody diarrhoea, fever, pallor,
weight loss and tachycardia. These symptoms can depict malignancy on the GIT; hence, the
patient needs urgent investigations and referral to an oncology centre. Simultaneous weight loss,
bloody diarrhoea and dyspepsia with abdominal discomfort together with changes in bowel
movements are the cardinal signs for colorectal cancer; hence, I label them the red flags. Fever,
pallor and tachycardia are the yellow flags and need to be monitored and receive priority
intervention (Ladeira, 2018). These are signs that require symptomatic relief but should be
followed to assess the need for referral for senior review.
Investigations
Previously done investigations are; full blood count (FBC), erythrocyte sedimentation
rate (ESR) and C-reactive protein (CRP) test. FBC is done to eliminate anemia and confirm the
number of blood components in comparison to normal reference ranges. ESR and CRP are
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
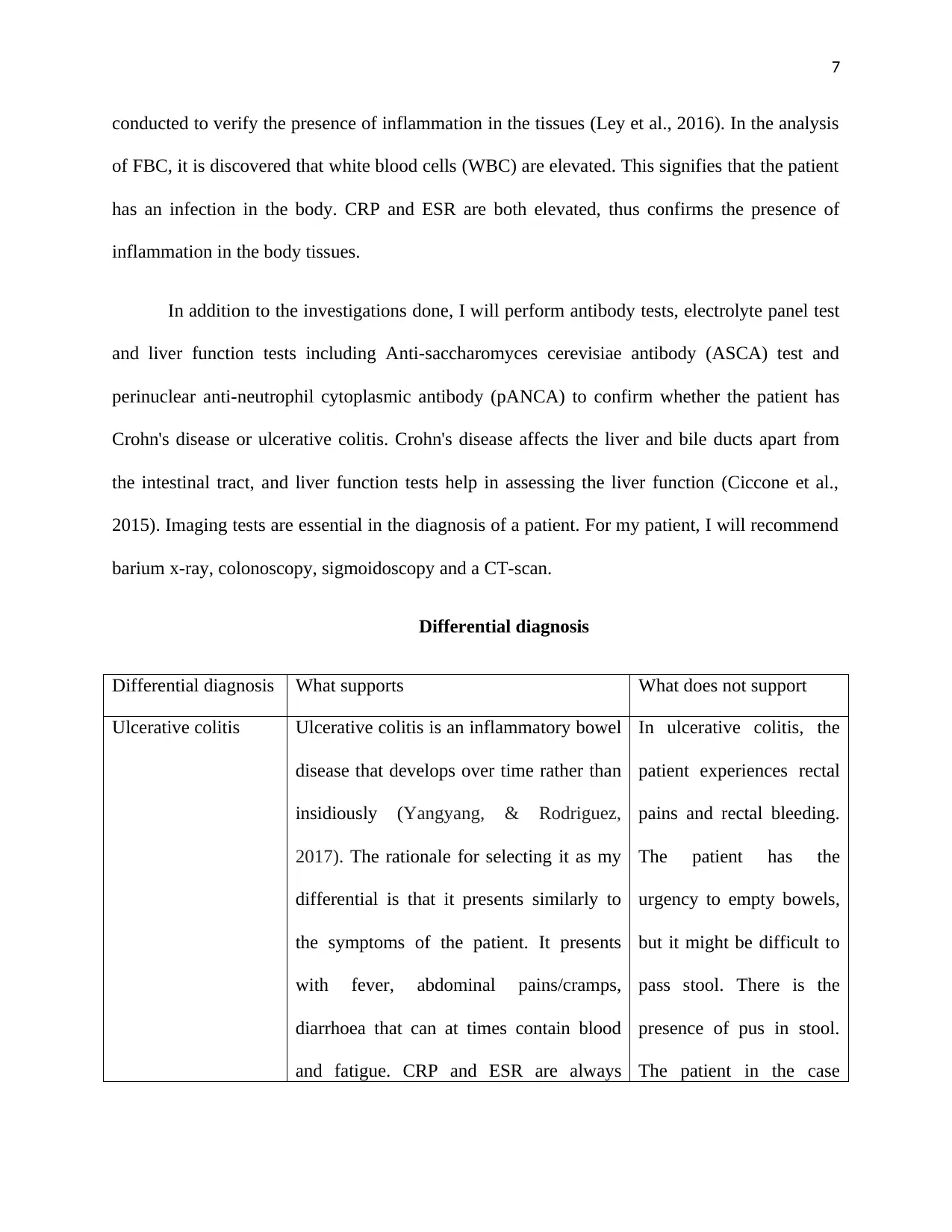
conducted to verify the presence of inflammation in the tissues (Ley et al., 2016). In the analysis
of FBC, it is discovered that white blood cells (WBC) are elevated. This signifies that the patient
has an infection in the body. CRP and ESR are both elevated, thus confirms the presence of
inflammation in the body tissues.
In addition to the investigations done, I will perform antibody tests, electrolyte panel test
and liver function tests including Anti-saccharomyces cerevisiae antibody (ASCA) test and
perinuclear anti-neutrophil cytoplasmic antibody (pANCA) to confirm whether the patient has
Crohn's disease or ulcerative colitis. Crohn's disease affects the liver and bile ducts apart from
the intestinal tract, and liver function tests help in assessing the liver function (Ciccone et al.,
2015). Imaging tests are essential in the diagnosis of a patient. For my patient, I will recommend
barium x-ray, colonoscopy, sigmoidoscopy and a CT-scan.
Differential diagnosis
Differential diagnosis What supports What does not support
Ulcerative colitis Ulcerative colitis is an inflammatory bowel
disease that develops over time rather than
insidiously (Yangyang, & Rodriguez,
2017). The rationale for selecting it as my
differential is that it presents similarly to
the symptoms of the patient. It presents
with fever, abdominal pains/cramps,
diarrhoea that can at times contain blood
and fatigue. CRP and ESR are always
In ulcerative colitis, the
patient experiences rectal
pains and rectal bleeding.
The patient has the
urgency to empty bowels,
but it might be difficult to
pass stool. There is the
presence of pus in stool.
The patient in the case
conducted to verify the presence of inflammation in the tissues (Ley et al., 2016). In the analysis
of FBC, it is discovered that white blood cells (WBC) are elevated. This signifies that the patient
has an infection in the body. CRP and ESR are both elevated, thus confirms the presence of
inflammation in the body tissues.
In addition to the investigations done, I will perform antibody tests, electrolyte panel test
and liver function tests including Anti-saccharomyces cerevisiae antibody (ASCA) test and
perinuclear anti-neutrophil cytoplasmic antibody (pANCA) to confirm whether the patient has
Crohn's disease or ulcerative colitis. Crohn's disease affects the liver and bile ducts apart from
the intestinal tract, and liver function tests help in assessing the liver function (Ciccone et al.,
2015). Imaging tests are essential in the diagnosis of a patient. For my patient, I will recommend
barium x-ray, colonoscopy, sigmoidoscopy and a CT-scan.
Differential diagnosis
Differential diagnosis What supports What does not support
Ulcerative colitis Ulcerative colitis is an inflammatory bowel
disease that develops over time rather than
insidiously (Yangyang, & Rodriguez,
2017). The rationale for selecting it as my
differential is that it presents similarly to
the symptoms of the patient. It presents
with fever, abdominal pains/cramps,
diarrhoea that can at times contain blood
and fatigue. CRP and ESR are always
In ulcerative colitis, the
patient experiences rectal
pains and rectal bleeding.
The patient has the
urgency to empty bowels,
but it might be difficult to
pass stool. There is the
presence of pus in stool.
The patient in the case
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
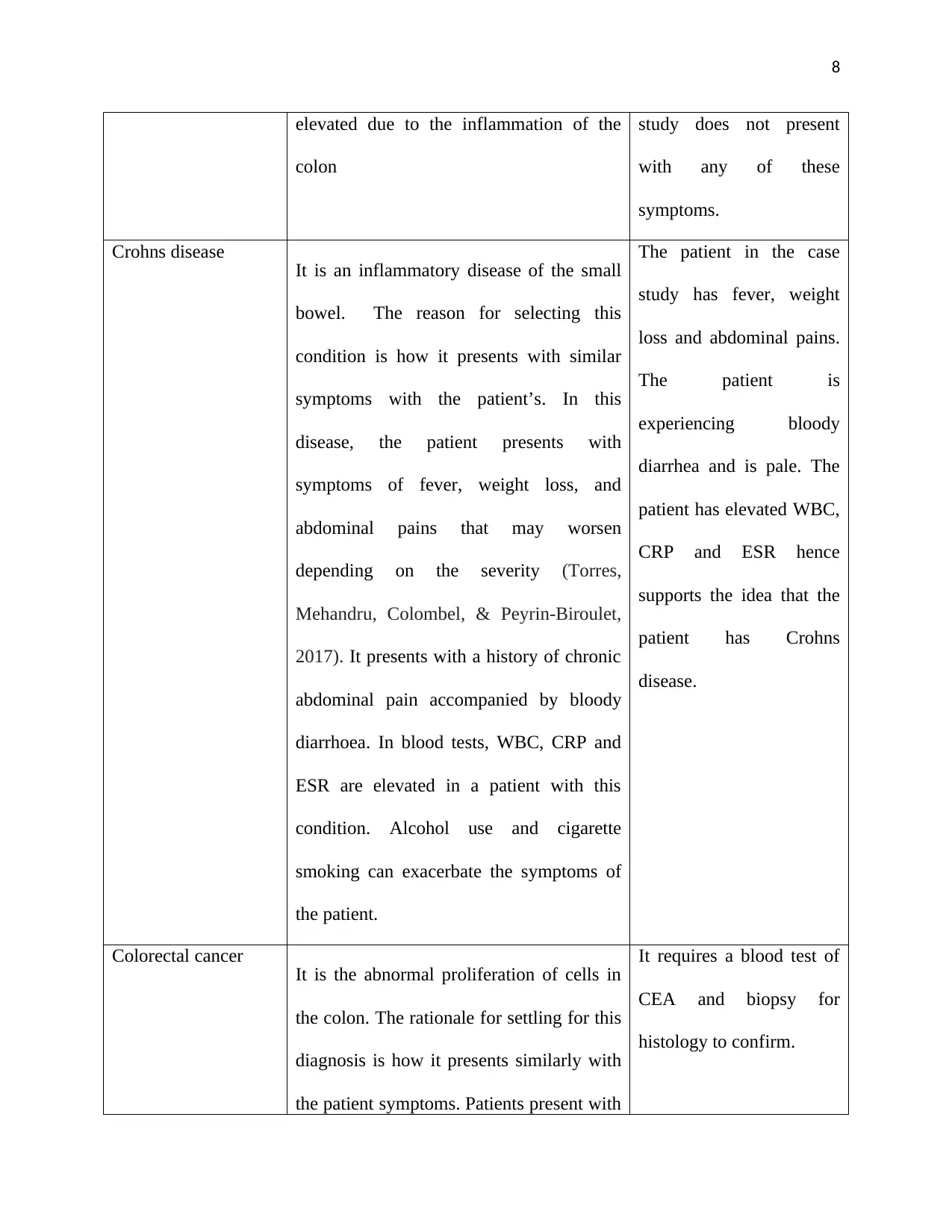
elevated due to the inflammation of the
colon
study does not present
with any of these
symptoms.
Crohns disease It is an inflammatory disease of the small
bowel. The reason for selecting this
condition is how it presents with similar
symptoms with the patient’s. In this
disease, the patient presents with
symptoms of fever, weight loss, and
abdominal pains that may worsen
depending on the severity (Torres,
Mehandru, Colombel, & Peyrin-Biroulet,
2017). It presents with a history of chronic
abdominal pain accompanied by bloody
diarrhoea. In blood tests, WBC, CRP and
ESR are elevated in a patient with this
condition. Alcohol use and cigarette
smoking can exacerbate the symptoms of
the patient.
The patient in the case
study has fever, weight
loss and abdominal pains.
The patient is
experiencing bloody
diarrhea and is pale. The
patient has elevated WBC,
CRP and ESR hence
supports the idea that the
patient has Crohns
disease.
Colorectal cancer It is the abnormal proliferation of cells in
the colon. The rationale for settling for this
diagnosis is how it presents similarly with
the patient symptoms. Patients present with
It requires a blood test of
CEA and biopsy for
histology to confirm.
elevated due to the inflammation of the
colon
study does not present
with any of these
symptoms.
Crohns disease It is an inflammatory disease of the small
bowel. The reason for selecting this
condition is how it presents with similar
symptoms with the patient’s. In this
disease, the patient presents with
symptoms of fever, weight loss, and
abdominal pains that may worsen
depending on the severity (Torres,
Mehandru, Colombel, & Peyrin-Biroulet,
2017). It presents with a history of chronic
abdominal pain accompanied by bloody
diarrhoea. In blood tests, WBC, CRP and
ESR are elevated in a patient with this
condition. Alcohol use and cigarette
smoking can exacerbate the symptoms of
the patient.
The patient in the case
study has fever, weight
loss and abdominal pains.
The patient is
experiencing bloody
diarrhea and is pale. The
patient has elevated WBC,
CRP and ESR hence
supports the idea that the
patient has Crohns
disease.
Colorectal cancer It is the abnormal proliferation of cells in
the colon. The rationale for settling for this
diagnosis is how it presents similarly with
the patient symptoms. Patients present with
It requires a blood test of
CEA and biopsy for
histology to confirm.
9
unexplained weight loss, abdominal pains
or cramping and tenderness (Walter et al.,
2016). Smoking and alcohol use are among
the risk factors on the development of the
condition.
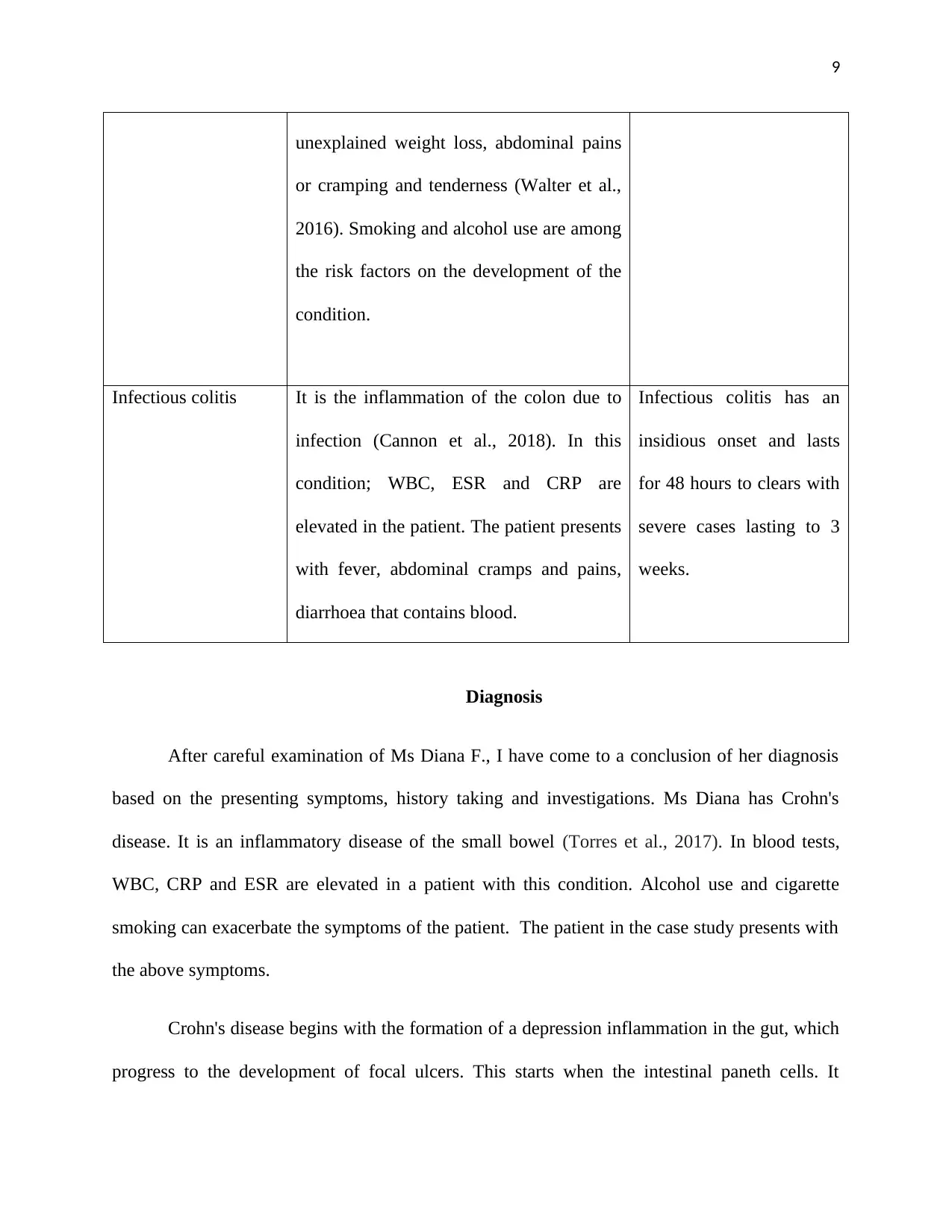
Infectious colitis It is the inflammation of the colon due to
infection (Cannon et al., 2018). In this
condition; WBC, ESR and CRP are
elevated in the patient. The patient presents
with fever, abdominal cramps and pains,
diarrhoea that contains blood.
Infectious colitis has an
insidious onset and lasts
for 48 hours to clears with
severe cases lasting to 3
weeks.
Diagnosis
After careful examination of Ms Diana F., I have come to a conclusion of her diagnosis
based on the presenting symptoms, history taking and investigations. Ms Diana has Crohn's
disease. It is an inflammatory disease of the small bowel (Torres et al., 2017). In blood tests,
WBC, CRP and ESR are elevated in a patient with this condition. Alcohol use and cigarette
smoking can exacerbate the symptoms of the patient. The patient in the case study presents with
the above symptoms.
Crohn's disease begins with the formation of a depression inflammation in the gut, which
progress to the development of focal ulcers. This starts when the intestinal paneth cells. It
unexplained weight loss, abdominal pains
or cramping and tenderness (Walter et al.,
2016). Smoking and alcohol use are among
the risk factors on the development of the
condition.
Infectious colitis It is the inflammation of the colon due to
infection (Cannon et al., 2018). In this
condition; WBC, ESR and CRP are
elevated in the patient. The patient presents
with fever, abdominal cramps and pains,
diarrhoea that contains blood.
Infectious colitis has an
insidious onset and lasts
for 48 hours to clears with
severe cases lasting to 3
weeks.
Diagnosis
After careful examination of Ms Diana F., I have come to a conclusion of her diagnosis
based on the presenting symptoms, history taking and investigations. Ms Diana has Crohn's
disease. It is an inflammatory disease of the small bowel (Torres et al., 2017). In blood tests,
WBC, CRP and ESR are elevated in a patient with this condition. Alcohol use and cigarette
smoking can exacerbate the symptoms of the patient. The patient in the case study presents with
the above symptoms.
Crohn's disease begins with the formation of a depression inflammation in the gut, which
progress to the development of focal ulcers. This starts when the intestinal paneth cells. It
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
progresses in three different patterns, primary inflammatory then stenotic pattern then lastly
fistulizing pattern (Speca, & Dubuquoy, 2017). It is an autoimmune condition caused by
abnormal immune response towards invading pathogens. According to WHO, about 3-15 people
are diagnosed with Crohn's disease per 100,000 people per year.
progresses in three different patterns, primary inflammatory then stenotic pattern then lastly
fistulizing pattern (Speca, & Dubuquoy, 2017). It is an autoimmune condition caused by
abnormal immune response towards invading pathogens. According to WHO, about 3-15 people
are diagnosed with Crohn's disease per 100,000 people per year.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
Referral letter
Ms. White
Nutritionist
Australia
General Practitioner,
New Wales Specialist Clinic,
Australia
Dear Dr. Walter
Re: Diana F, 27 years old, Australia
Thank you for agreeing to review Diana F, a 27 years old patient with a probable diagnosis of
crohns disease.
Current treatment
IV metronidazole 500mg TDs
Oral prednisolone 10mg
Paracetamol 1g PRN
Results of lab results done
Blood tests revealed elevated ESR, CRP and WBCs.
Referral letter
Ms. White
Nutritionist
Australia
General Practitioner,
New Wales Specialist Clinic,
Australia
Dear Dr. Walter
Re: Diana F, 27 years old, Australia
Thank you for agreeing to review Diana F, a 27 years old patient with a probable diagnosis of
crohns disease.
Current treatment
IV metronidazole 500mg TDs
Oral prednisolone 10mg
Paracetamol 1g PRN
Results of lab results done
Blood tests revealed elevated ESR, CRP and WBCs.
12
The patient has symptoms of lower abdominal pain for the past four days that is worsening,
Pallor and Muscle wasting. The patient has been having abdominal discomfort and pain for the
past two years, accompanied by bloody diarrhea. The symptoms are inclusive with gradual
weight loss.
The patient has been referred for an abdominal CT- scan, Barium x-ray and colonoscopy. The
patient has also been referred for senior review and further management.
Yours sincerely,
Ms. White.
The patient has symptoms of lower abdominal pain for the past four days that is worsening,
Pallor and Muscle wasting. The patient has been having abdominal discomfort and pain for the
past two years, accompanied by bloody diarrhea. The symptoms are inclusive with gradual
weight loss.
The patient has been referred for an abdominal CT- scan, Barium x-ray and colonoscopy. The
patient has also been referred for senior review and further management.
Yours sincerely,
Ms. White.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





