CNA344: Practice Portfolio of Evidence: Clinical Encounter Analysis
VerifiedAdded on 2022/08/30
|8
|2769
|17
Practical Assignment
AI Summary
This assignment is a clinical encounter analysis from a student nurse, focusing on a patient with dementia who exhibited aggressive behavior in a residential aged care unit. The analysis follows the clinical reasoning cycle, addressing the patient's situation, available information, gathered assessments, and existing knowledge. The student identifies the problems of aggressive behavior and risk of harm to others, proposing goals and rationalizing nursing actions, including de-escalation techniques and environmental modifications. The student also explores the potential consequences of inaction and evaluates the outcomes of the clinical encounter, referencing evidence-based literature to support their decisions. The assignment demonstrates the student's ability to apply clinical reasoning and critical thinking skills in managing a complex patient situation.
CNA344: Becoming a RN: Practice consolidation
Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
Consider the patient
situation/context
(@150 words)
Provide an overview
of the encounter.
What happened, how
it occurred, what was
it that alerted you to
that fact that you
needed to take action
in the encounter.
As part of the my placement at a residential aged care unit, I was assigned to the care of Mr. Jones (pseudonym), a 70 years old man with history
of dementia. The patient was admitted to the hospital following a fall in the bathroom. He sustained a hair line fracture of the ankles and he was
in intense pain last night. However, during my assessment in the morning, he was found to be much more comfortable. I checked his dressings
and supported him in changing his clothes and taking breakfast. The client was responding well to my questions. To ensure that the patient gets
a comfortable environment, I opened the curtains and tried to introduce patient to another patient on the ward so that he does not feels
gloomy all the day. However, as soon as I did this, the patient became very aggressive. He became out of control and tried to hit me with any
possible object he found near him. He was not listening at all and he tried to open all the saline tube attached to his wrist too.
Review (@150 words)
What key information
was already available
to you and how did
this influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
Gather(@150 words)
What was the new
information you
gathered from
Review:
When I was handed over to Mr. Jones for care, I had reviewed the medical history of patient. The patient had a history of dementia and memory
problems since the past two years. He also had diabetes and hypertension. He was operated three years ago for an intestinal surgery. Following
the fall, blood test and X-ray was done. Mr. Jones was brought to the hospital by her daughter. He wife was staying at home due to vision
problems. Mr. Jones was attached to his wife. However, since the past two months, he started avoiding contact with his wife and daughter too.
He wanted to be alone all the time. However, the information that I failed to notice was that he had a past history of violent behaviour
particularly when he encountered unfamiliar people all of a sudden.
I found the patient to be worried because of his fracture as throughout my conversation with the patient, I found that he was gloomy about his
future. I decided to make a change to his environment. The main intention of introducing him to other patient was to distract him. According to
Mackintosh-Franklin (2018), use of distraction technique is important to calm the patient and manage their anxiety related to pain or other
health problems.
Relevant medications (where relevant): (not included in word count)
The patient was taking two regular medications for diabetes and hypertension. After hospitalization, Mr. Jones was being given analgesics for
the management of pain.
1
Practice Portfolio of Evidence PART B: Clinical Encounter Analysis
Consider the patient
situation/context
(@150 words)
Provide an overview
of the encounter.
What happened, how
it occurred, what was
it that alerted you to
that fact that you
needed to take action
in the encounter.
As part of the my placement at a residential aged care unit, I was assigned to the care of Mr. Jones (pseudonym), a 70 years old man with history
of dementia. The patient was admitted to the hospital following a fall in the bathroom. He sustained a hair line fracture of the ankles and he was
in intense pain last night. However, during my assessment in the morning, he was found to be much more comfortable. I checked his dressings
and supported him in changing his clothes and taking breakfast. The client was responding well to my questions. To ensure that the patient gets
a comfortable environment, I opened the curtains and tried to introduce patient to another patient on the ward so that he does not feels
gloomy all the day. However, as soon as I did this, the patient became very aggressive. He became out of control and tried to hit me with any
possible object he found near him. He was not listening at all and he tried to open all the saline tube attached to his wrist too.
Review (@150 words)
What key information
was already available
to you and how did
this influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
Gather(@150 words)
What was the new
information you
gathered from
Review:
When I was handed over to Mr. Jones for care, I had reviewed the medical history of patient. The patient had a history of dementia and memory
problems since the past two years. He also had diabetes and hypertension. He was operated three years ago for an intestinal surgery. Following
the fall, blood test and X-ray was done. Mr. Jones was brought to the hospital by her daughter. He wife was staying at home due to vision
problems. Mr. Jones was attached to his wife. However, since the past two months, he started avoiding contact with his wife and daughter too.
He wanted to be alone all the time. However, the information that I failed to notice was that he had a past history of violent behaviour
particularly when he encountered unfamiliar people all of a sudden.
I found the patient to be worried because of his fracture as throughout my conversation with the patient, I found that he was gloomy about his
future. I decided to make a change to his environment. The main intention of introducing him to other patient was to distract him. According to
Mackintosh-Franklin (2018), use of distraction technique is important to calm the patient and manage their anxiety related to pain or other
health problems.
Relevant medications (where relevant): (not included in word count)
The patient was taking two regular medications for diabetes and hypertension. After hospitalization, Mr. Jones was being given analgesics for
the management of pain.
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
additional
assessment?
Dot points are fine for
this section
Recall(@200 words)
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
Gather:
Apart from the review of past medical history, I also conducted pain assessment and cognitive assessment for Mr. Jones using the PQRST
format. PQRST format helps to analyse five factors such as palliation, quality/quantity, radiation, severity and timing (Gauchan 2019). Based on
this assessment, his pain score was found to be 2. The patient reported getting relief from pain since morning and differences in his pain post
the prescribed pain medication. However, it was also found that raising his legs or putting his foot to the ground increased his pain level or
intensity.
I conducted cognitive assessment of patient to assess cognitive parameters of patient such as orientation to place and time, memory, attention,
thinking, language and executive function. He was found to be oriented to place and time. He had memory recall issues but he was able to
remember things once the event was repeated to him. He had organized thoughts and good level of concentration. However, his executive
functioning seemed affected.
Recall:
Based on the medical history, I conducted cognitive assessment of patient. However, as I failed to pay attention to the history of aggressiveness
issue of Mr. Jones, I avoided doing behavioural assessment. I think I should have looked at the medical history more thoroughly because this
would have helped me to careful assess behavioural changes and interpret the impact of the issue on the patient. On recalling the knowledge
related to nursing assessment of dementia patient, I feel that monitoring of behavioural changes like anxiety and aggression and the factors
triggering it was important. According to Kales, Gitlin and Lyketsos (2015), apart from psychological symptoms, dementia patients have many
other behavioural issues such as aggression, sleep problems, agitation and wandering. In addition to the disease related problem, behavioural
and psychological symptoms occur due to other factors like unmet needs, environmental triggers and interaction with others.
Since this was my first encounter with sudden behaviour change of a patient, I became very nervous. This situation required me to think like a
registered nurse. However, since the situation was an emergency issue, engaging in quick actions to the same became very challenging for me.
The behaviour of patient was very unpredictable and it was challenging for me to decide best intervention to minimize further trauma to the
patient and others (ACSQHC 2017). This situation made me act like a registered nurse as I had to reflect to experiences, knowledge and actions
to take decision regarding safe and quality care for patients (NMBA 2017).
2
assessment?
Dot points are fine for
this section
Recall(@200 words)
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
Gather:
Apart from the review of past medical history, I also conducted pain assessment and cognitive assessment for Mr. Jones using the PQRST
format. PQRST format helps to analyse five factors such as palliation, quality/quantity, radiation, severity and timing (Gauchan 2019). Based on
this assessment, his pain score was found to be 2. The patient reported getting relief from pain since morning and differences in his pain post
the prescribed pain medication. However, it was also found that raising his legs or putting his foot to the ground increased his pain level or
intensity.
I conducted cognitive assessment of patient to assess cognitive parameters of patient such as orientation to place and time, memory, attention,
thinking, language and executive function. He was found to be oriented to place and time. He had memory recall issues but he was able to
remember things once the event was repeated to him. He had organized thoughts and good level of concentration. However, his executive
functioning seemed affected.
Recall:
Based on the medical history, I conducted cognitive assessment of patient. However, as I failed to pay attention to the history of aggressiveness
issue of Mr. Jones, I avoided doing behavioural assessment. I think I should have looked at the medical history more thoroughly because this
would have helped me to careful assess behavioural changes and interpret the impact of the issue on the patient. On recalling the knowledge
related to nursing assessment of dementia patient, I feel that monitoring of behavioural changes like anxiety and aggression and the factors
triggering it was important. According to Kales, Gitlin and Lyketsos (2015), apart from psychological symptoms, dementia patients have many
other behavioural issues such as aggression, sleep problems, agitation and wandering. In addition to the disease related problem, behavioural
and psychological symptoms occur due to other factors like unmet needs, environmental triggers and interaction with others.
Since this was my first encounter with sudden behaviour change of a patient, I became very nervous. This situation required me to think like a
registered nurse. However, since the situation was an emergency issue, engaging in quick actions to the same became very challenging for me.
The behaviour of patient was very unpredictable and it was challenging for me to decide best intervention to minimize further trauma to the
patient and others (ACSQHC 2017). This situation made me act like a registered nurse as I had to reflect to experiences, knowledge and actions
to take decision regarding safe and quality care for patients (NMBA 2017).
2
Process
Information(@400
words)
Interpret, relate and
infer from the
information gathered
Interpret, Relate and Infer:
The main issue I faced during the clinical encounter was the display of sudden behavioural change in patient associated with aggression and
harm of others. On review of the cause behind aggressiveness and sudden behavioural change in dementia patient, I have been able to better
understand the reason for such behaviour of patient. The aggressive behaviour of Mr. Jones is a sign that his needs have been not met or he is
not able to communicate the same verbally. Thus, understanding what is causing the problem may help to find solution to the problem.
There is a possibility that unmet physical needs might have led to the problem. Alzheimer’s patient may be in pain or there might be something
3
Information(@400
words)
Interpret, relate and
infer from the
information gathered
Interpret, Relate and Infer:
The main issue I faced during the clinical encounter was the display of sudden behavioural change in patient associated with aggression and
harm of others. On review of the cause behind aggressiveness and sudden behavioural change in dementia patient, I have been able to better
understand the reason for such behaviour of patient. The aggressive behaviour of Mr. Jones is a sign that his needs have been not met or he is
not able to communicate the same verbally. Thus, understanding what is causing the problem may help to find solution to the problem.
There is a possibility that unmet physical needs might have led to the problem. Alzheimer’s patient may be in pain or there might be something
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
to demonstrate an
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
Predict (@100 words)
What could/would
have happened in your
encounter if you were
to have taken NO
action and why?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
wrong with the environment stimulating aggression in the patient. I had opened the curtain and too much brightness might have disturbed the
patient and led to aggression too (Du et al. 2017). Aggression is one of the behavioural symptoms of dementia and managing this is important as
poor management can lead to distress for caregivers as well as progression of the disease. The evidence by Wolf, Goldberg and Freedman (2018)
shows that dementia patient display aggressive behaviour in response to stimulus in the patient’s environment. In case of my clinical encounter,
too exposure too unfamiliar environment might have triggered the behavioural change. Aggressiveness is also reflective of poor coping skills in
patients. Some medications like antipsychotics agents also lead to aggressiveness. However, based on the medication review, it has been found
that the patient was not taking any antipsychotic medication. Hence, impact of medication on behavioural change has been ruled out. The major
problem identified is the issue of aggression as it affects the quality of life of patient.
The second problem identified in case of the encounter is the risk of injury to others due to aggressive behaviour. This action might have
occurred because of changes in environment. For people with dementia, familiarity with the environment is important t to facilitate their sense
of comfort. However, because of my action, a change in both physical and social environment of Mr. Jones occurred. This form of disturbance
might have resulted in such aggressive behaviour by patient (Maria Gramegna and Biamonti, 2017). As Mr. Jones showed assaultive behaviour,
there is a need to quickly manage the issue to avoid harm to others too (Wharton and Ford 2014). According to the ACQHS standard 5.33, it is
important to mitigate situations that may precipitate aggression (ACSQHC 2017).
Predict:
I think my behaviour of changing the patient’s environment was the main cause behind such behaviour change in patient. If I had taken no
action to introduce Mr. Jones to other patient, the situation would have been much better. Mr. Jones would have got a familiar environment
and other patient would not have to suffer because of the issue. Maintaining a safe environment during the delivery of care i s important as
patient with cognitive impairment often experience distress because of unfamiliar and busy environments (ACSQHC 2017).
4
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
Predict (@100 words)
What could/would
have happened in your
encounter if you were
to have taken NO
action and why?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
wrong with the environment stimulating aggression in the patient. I had opened the curtain and too much brightness might have disturbed the
patient and led to aggression too (Du et al. 2017). Aggression is one of the behavioural symptoms of dementia and managing this is important as
poor management can lead to distress for caregivers as well as progression of the disease. The evidence by Wolf, Goldberg and Freedman (2018)
shows that dementia patient display aggressive behaviour in response to stimulus in the patient’s environment. In case of my clinical encounter,
too exposure too unfamiliar environment might have triggered the behavioural change. Aggressiveness is also reflective of poor coping skills in
patients. Some medications like antipsychotics agents also lead to aggressiveness. However, based on the medication review, it has been found
that the patient was not taking any antipsychotic medication. Hence, impact of medication on behavioural change has been ruled out. The major
problem identified is the issue of aggression as it affects the quality of life of patient.
The second problem identified in case of the encounter is the risk of injury to others due to aggressive behaviour. This action might have
occurred because of changes in environment. For people with dementia, familiarity with the environment is important t to facilitate their sense
of comfort. However, because of my action, a change in both physical and social environment of Mr. Jones occurred. This form of disturbance
might have resulted in such aggressive behaviour by patient (Maria Gramegna and Biamonti, 2017). As Mr. Jones showed assaultive behaviour,
there is a need to quickly manage the issue to avoid harm to others too (Wharton and Ford 2014). According to the ACQHS standard 5.33, it is
important to mitigate situations that may precipitate aggression (ACSQHC 2017).
Predict:
I think my behaviour of changing the patient’s environment was the main cause behind such behaviour change in patient. If I had taken no
action to introduce Mr. Jones to other patient, the situation would have been much better. Mr. Jones would have got a familiar environment
and other patient would not have to suffer because of the issue. Maintaining a safe environment during the delivery of care i s important as
patient with cognitive impairment often experience distress because of unfamiliar and busy environments (ACSQHC 2017).
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
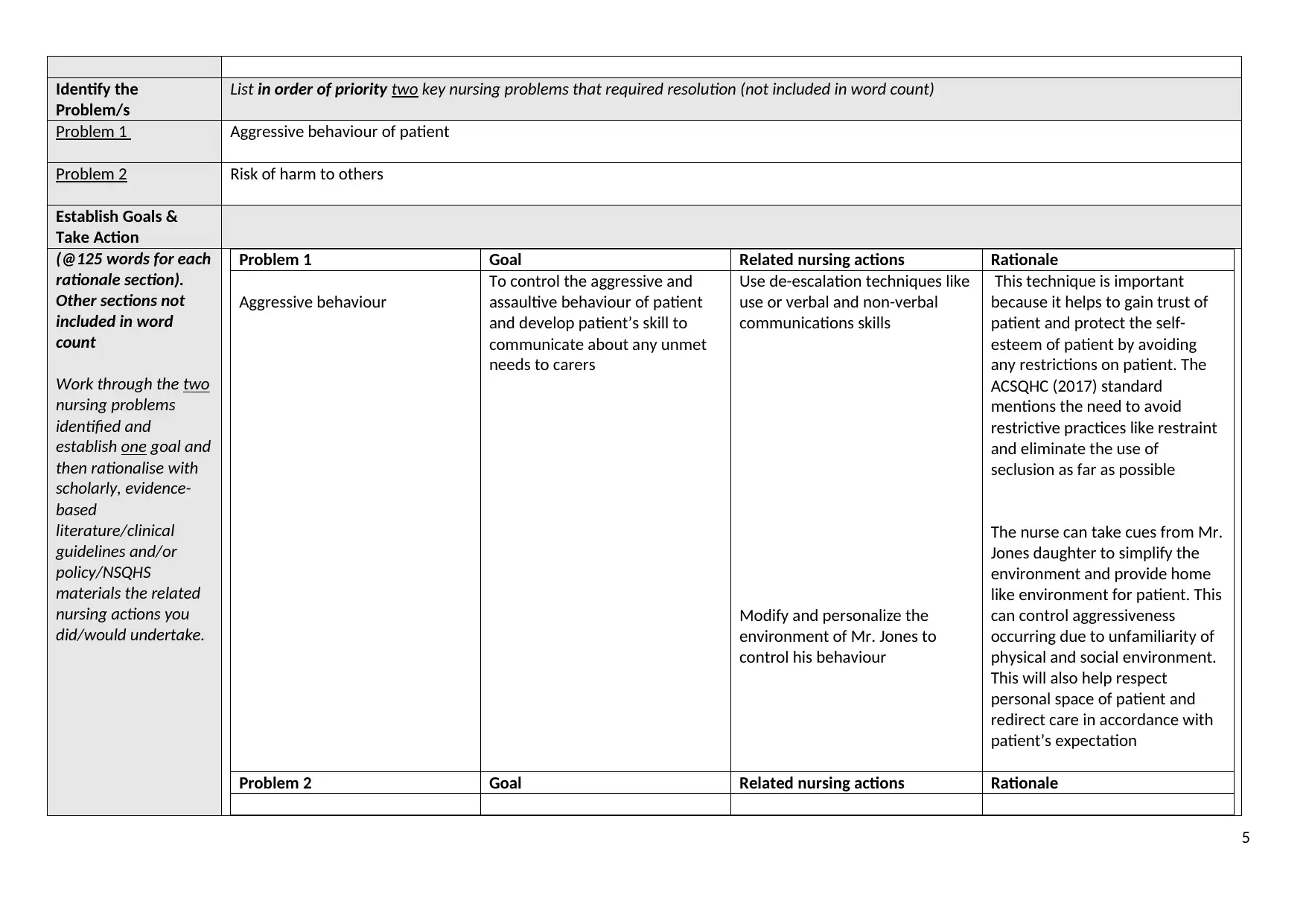
Identify the
Problem/s
List in order of priority two key nursing problems that required resolution (not included in word count)
Problem 1 Aggressive behaviour of patient
Problem 2 Risk of harm to others
Establish Goals &
Take Action
(@125 words for each
rationale section).
Other sections not
included in word
count
Work through the two
nursing problems
identified and
establish one goal and
then rationalise with
scholarly, evidence-
based
literature/clinical
guidelines and/or
policy/NSQHS
materials the related
nursing actions you
did/would undertake.
Problem 1 Goal Related nursing actions Rationale
Aggressive behaviour
To control the aggressive and
assaultive behaviour of patient
and develop patient’s skill to
communicate about any unmet
needs to carers
Use de-escalation techniques like
use or verbal and non-verbal
communications skills
Modify and personalize the
environment of Mr. Jones to
control his behaviour
This technique is important
because it helps to gain trust of
patient and protect the self-
esteem of patient by avoiding
any restrictions on patient. The
ACSQHC (2017) standard
mentions the need to avoid
restrictive practices like restraint
and eliminate the use of
seclusion as far as possible
The nurse can take cues from Mr.
Jones daughter to simplify the
environment and provide home
like environment for patient. This
can control aggressiveness
occurring due to unfamiliarity of
physical and social environment.
This will also help respect
personal space of patient and
redirect care in accordance with
patient’s expectation
Problem 2 Goal Related nursing actions Rationale
5
Problem/s
List in order of priority two key nursing problems that required resolution (not included in word count)
Problem 1 Aggressive behaviour of patient
Problem 2 Risk of harm to others
Establish Goals &
Take Action
(@125 words for each
rationale section).
Other sections not
included in word
count
Work through the two
nursing problems
identified and
establish one goal and
then rationalise with
scholarly, evidence-
based
literature/clinical
guidelines and/or
policy/NSQHS
materials the related
nursing actions you
did/would undertake.
Problem 1 Goal Related nursing actions Rationale
Aggressive behaviour
To control the aggressive and
assaultive behaviour of patient
and develop patient’s skill to
communicate about any unmet
needs to carers
Use de-escalation techniques like
use or verbal and non-verbal
communications skills
Modify and personalize the
environment of Mr. Jones to
control his behaviour
This technique is important
because it helps to gain trust of
patient and protect the self-
esteem of patient by avoiding
any restrictions on patient. The
ACSQHC (2017) standard
mentions the need to avoid
restrictive practices like restraint
and eliminate the use of
seclusion as far as possible
The nurse can take cues from Mr.
Jones daughter to simplify the
environment and provide home
like environment for patient. This
can control aggressiveness
occurring due to unfamiliarity of
physical and social environment.
This will also help respect
personal space of patient and
redirect care in accordance with
patient’s expectation
Problem 2 Goal Related nursing actions Rationale
5
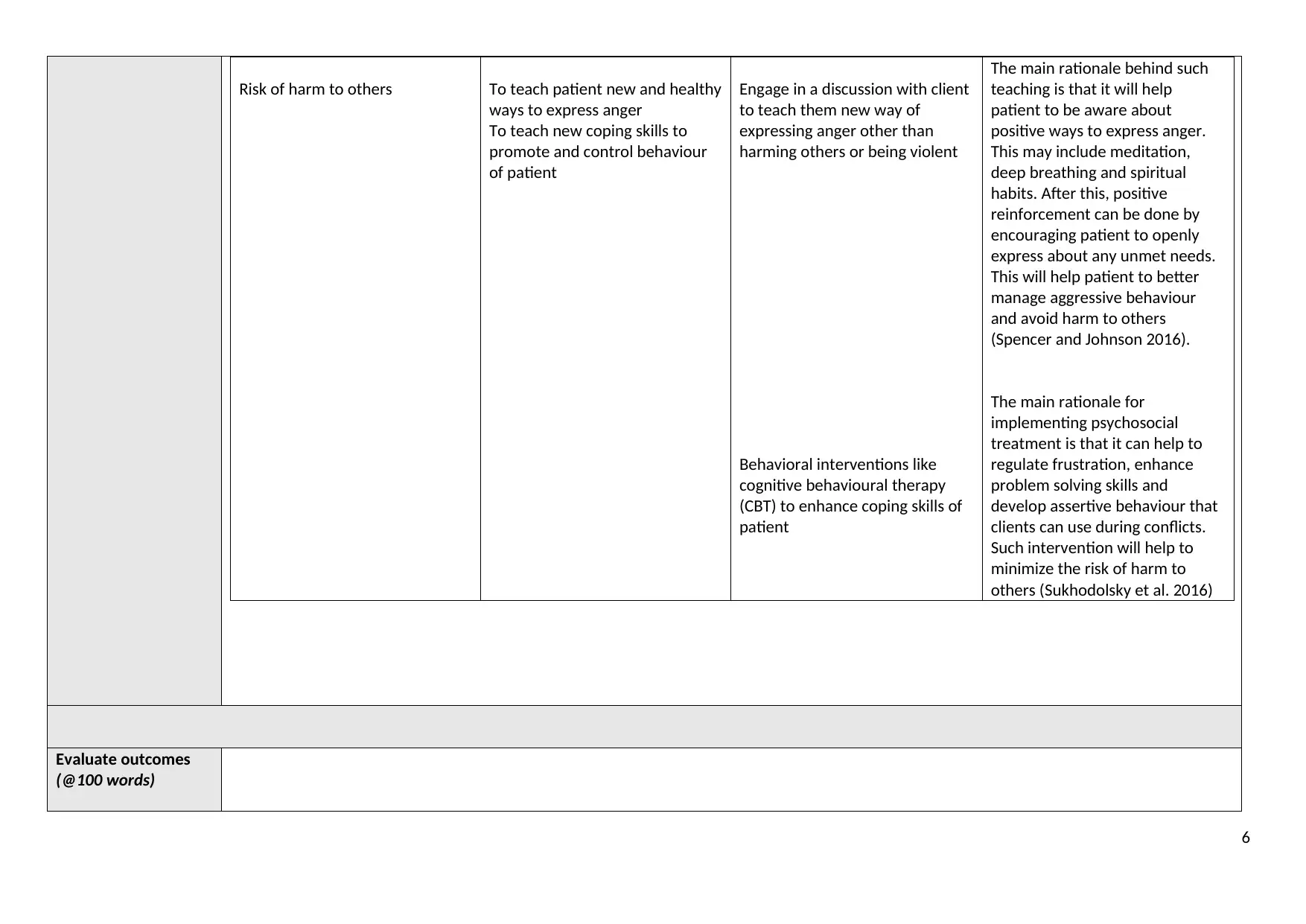
Risk of harm to others To teach patient new and healthy
ways to express anger
To teach new coping skills to
promote and control behaviour
of patient
Engage in a discussion with client
to teach them new way of
expressing anger other than
harming others or being violent
Behavioral interventions like
cognitive behavioural therapy
(CBT) to enhance coping skills of
patient
The main rationale behind such
teaching is that it will help
patient to be aware about
positive ways to express anger.
This may include meditation,
deep breathing and spiritual
habits. After this, positive
reinforcement can be done by
encouraging patient to openly
express about any unmet needs.
This will help patient to better
manage aggressive behaviour
and avoid harm to others
(Spencer and Johnson 2016).
The main rationale for
implementing psychosocial
treatment is that it can help to
regulate frustration, enhance
problem solving skills and
develop assertive behaviour that
clients can use during conflicts.
Such intervention will help to
minimize the risk of harm to
others (Sukhodolsky et al. 2016)
Evaluate outcomes
(@100 words)
6
ways to express anger
To teach new coping skills to
promote and control behaviour
of patient
Engage in a discussion with client
to teach them new way of
expressing anger other than
harming others or being violent
Behavioral interventions like
cognitive behavioural therapy
(CBT) to enhance coping skills of
patient
The main rationale behind such
teaching is that it will help
patient to be aware about
positive ways to express anger.
This may include meditation,
deep breathing and spiritual
habits. After this, positive
reinforcement can be done by
encouraging patient to openly
express about any unmet needs.
This will help patient to better
manage aggressive behaviour
and avoid harm to others
(Spencer and Johnson 2016).
The main rationale for
implementing psychosocial
treatment is that it can help to
regulate frustration, enhance
problem solving skills and
develop assertive behaviour that
clients can use during conflicts.
Such intervention will help to
minimize the risk of harm to
others (Sukhodolsky et al. 2016)
Evaluate outcomes
(@100 words)
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
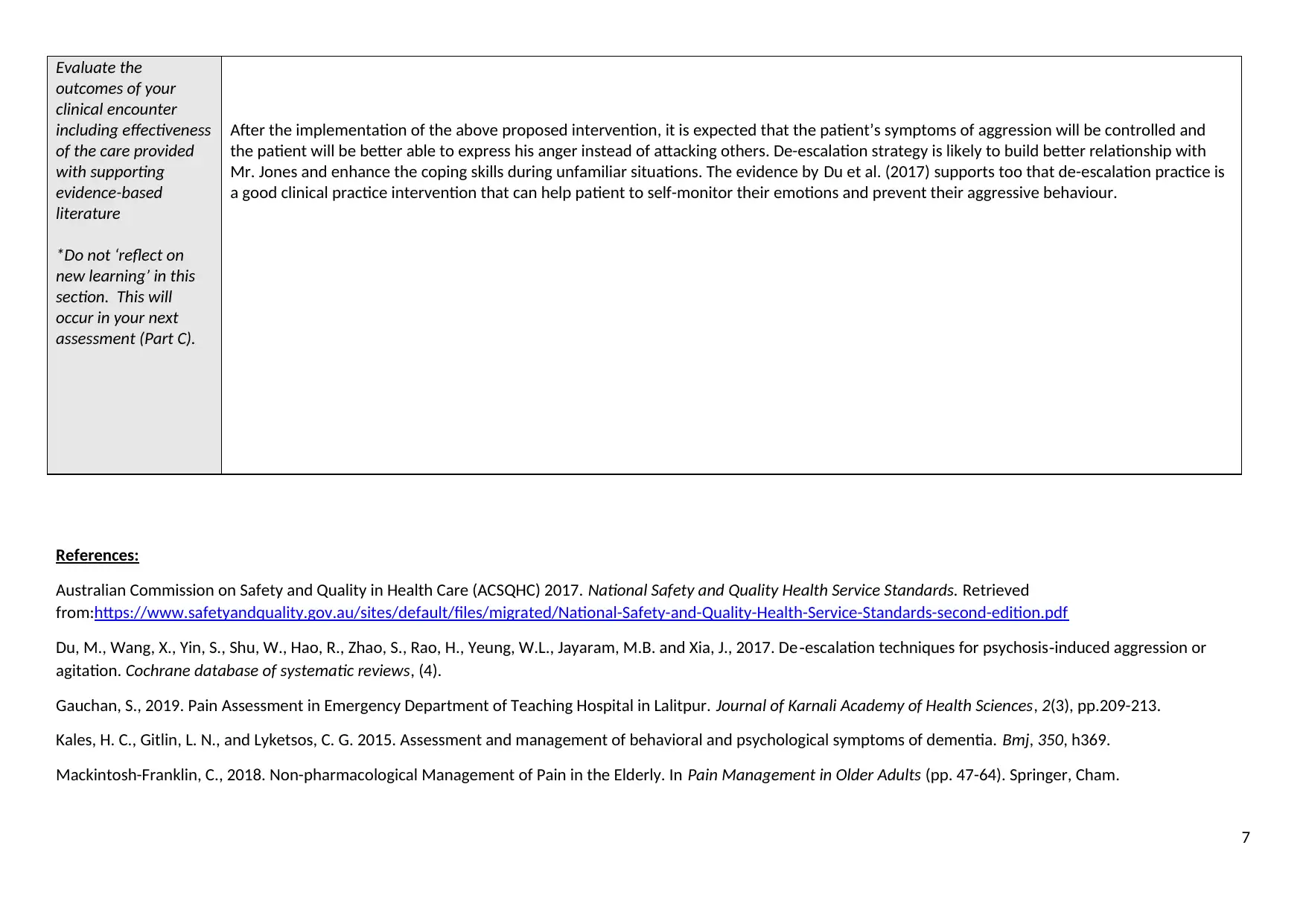
Evaluate the
outcomes of your
clinical encounter
including effectiveness
of the care provided
with supporting
evidence-based
literature
*Do not ‘reflect on
new learning’ in this
section. This will
occur in your next
assessment (Part C).
After the implementation of the above proposed intervention, it is expected that the patient’s symptoms of aggression will be controlled and
the patient will be better able to express his anger instead of attacking others. De-escalation strategy is likely to build better relationship with
Mr. Jones and enhance the coping skills during unfamiliar situations. The evidence by Du et al. (2017) supports too that de-escalation practice is
a good clinical practice intervention that can help patient to self-monitor their emotions and prevent their aggressive behaviour.
References:
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2017. National Safety and Quality Health Service Standards. Retrieved
from:https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf
Du, M., Wang, X., Yin, S., Shu, W., Hao, R., Zhao, S., Rao, H., Yeung, W.L., Jayaram, M.B. and Xia, J., 2017. De‐escalation techniques for psychosis‐induced aggression or
agitation. Cochrane database of systematic reviews, (4).
Gauchan, S., 2019. Pain Assessment in Emergency Department of Teaching Hospital in Lalitpur. Journal of Karnali Academy of Health Sciences, 2(3), pp.209-213.
Kales, H. C., Gitlin, L. N., and Lyketsos, C. G. 2015. Assessment and management of behavioral and psychological symptoms of dementia. Bmj, 350, h369.
Mackintosh-Franklin, C., 2018. Non-pharmacological Management of Pain in the Elderly. In Pain Management in Older Adults (pp. 47-64). Springer, Cham.
7
outcomes of your
clinical encounter
including effectiveness
of the care provided
with supporting
evidence-based
literature
*Do not ‘reflect on
new learning’ in this
section. This will
occur in your next
assessment (Part C).
After the implementation of the above proposed intervention, it is expected that the patient’s symptoms of aggression will be controlled and
the patient will be better able to express his anger instead of attacking others. De-escalation strategy is likely to build better relationship with
Mr. Jones and enhance the coping skills during unfamiliar situations. The evidence by Du et al. (2017) supports too that de-escalation practice is
a good clinical practice intervention that can help patient to self-monitor their emotions and prevent their aggressive behaviour.
References:
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2017. National Safety and Quality Health Service Standards. Retrieved
from:https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf
Du, M., Wang, X., Yin, S., Shu, W., Hao, R., Zhao, S., Rao, H., Yeung, W.L., Jayaram, M.B. and Xia, J., 2017. De‐escalation techniques for psychosis‐induced aggression or
agitation. Cochrane database of systematic reviews, (4).
Gauchan, S., 2019. Pain Assessment in Emergency Department of Teaching Hospital in Lalitpur. Journal of Karnali Academy of Health Sciences, 2(3), pp.209-213.
Kales, H. C., Gitlin, L. N., and Lyketsos, C. G. 2015. Assessment and management of behavioral and psychological symptoms of dementia. Bmj, 350, h369.
Mackintosh-Franklin, C., 2018. Non-pharmacological Management of Pain in the Elderly. In Pain Management in Older Adults (pp. 47-64). Springer, Cham.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Maria Gramegna, S. and Biamonti, A., 2017. Environment as non pharmacological intervention in the care of Alzheimer’s disease. The Design Journal, 20(sup1), pp.S2284-
S2292.
Nursing and Midwifery Board of Australia (NMBA) 2017. Registered nurse standards for practice. Retrieved from: https://www.nursingmidwiferyboard.gov.au/Codes-
Guidelines-Statements/Professional-standards/registered-nurse-standards-for-practice.aspx
Spencer, S. and Johnson, P., 2016. Deescalation techniques for managing aggression. Cochrane Database of Systematic Reviews, (1), pp.Art-No.
Sukhodolsky, D. G., Smith, S. D., McCauley, S. A., Ibrahim, K., and Piasecka, J. B. 2016. Behavioral Interventions for Anger, Irritability, and Aggression in Children and
Adolescents. Journal of child and adolescent psychopharmacology, 26(1), 58–64. doi:10.1089/cap.2015.0120
Wharton, T. C., and Ford, B. K. 2014. What is known about dementia care recipient violence and aggression against caregivers?. Journal of gerontological social work, 57(5),
460–477.
Wolf, M.U., Goldberg, Y. and Freedman, M., 2018. Aggression and agitation in dementia. Continuum: lifelong learning in neurology, 24(3), pp.783-803.
8
S2292.
Nursing and Midwifery Board of Australia (NMBA) 2017. Registered nurse standards for practice. Retrieved from: https://www.nursingmidwiferyboard.gov.au/Codes-
Guidelines-Statements/Professional-standards/registered-nurse-standards-for-practice.aspx
Spencer, S. and Johnson, P., 2016. Deescalation techniques for managing aggression. Cochrane Database of Systematic Reviews, (1), pp.Art-No.
Sukhodolsky, D. G., Smith, S. D., McCauley, S. A., Ibrahim, K., and Piasecka, J. B. 2016. Behavioral Interventions for Anger, Irritability, and Aggression in Children and
Adolescents. Journal of child and adolescent psychopharmacology, 26(1), 58–64. doi:10.1089/cap.2015.0120
Wharton, T. C., and Ford, B. K. 2014. What is known about dementia care recipient violence and aggression against caregivers?. Journal of gerontological social work, 57(5),
460–477.
Wolf, M.U., Goldberg, Y. and Freedman, M., 2018. Aggression and agitation in dementia. Continuum: lifelong learning in neurology, 24(3), pp.783-803.
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





