Clinical Epidemiology Assignment: Autumn 2019, WSU Medicine
VerifiedAdded on 2022/12/26
|10
|2251
|86
Homework Assignment
AI Summary
This Clinical Epidemiology assignment addresses several key topics within the field. The assignment begins by exploring the impact of Liraglutide, a glucagon-like peptide-1 analogue, on weight change in type II diabetes adults, outlining the PICO elements of the research question. It then investigates the risk factors associated with multi-drug tuberculosis resistance among migrant populations. The assignment continues with a detailed analysis of a search strategy to find literature on the effect of Liraglutide, including database searches and suitable study designs. A specific article is identified and evaluated. Further, the assignment covers the interpretation of a 2x2 contingency table, calculating sensitivity, positive predictive value, and other statistical measures. The assignment then delves into the analysis of treatment effects on weight change, calculating relative risks, relative risk reduction, and the number needed to treat. The document also evaluates the internal validity of a clinical trial and assesses both clinical and statistical significance of the results, including hazard ratios and confidence intervals. Finally, the assignment considers the generalizability of the study's findings, discussing the consistency with other studies, randomization, and the representativeness of the study population.
Clinical Epidemiology Assessment
By
Student’s Name
Course
Tutor
Institution
Date
By
Student’s Name
Course
Tutor
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
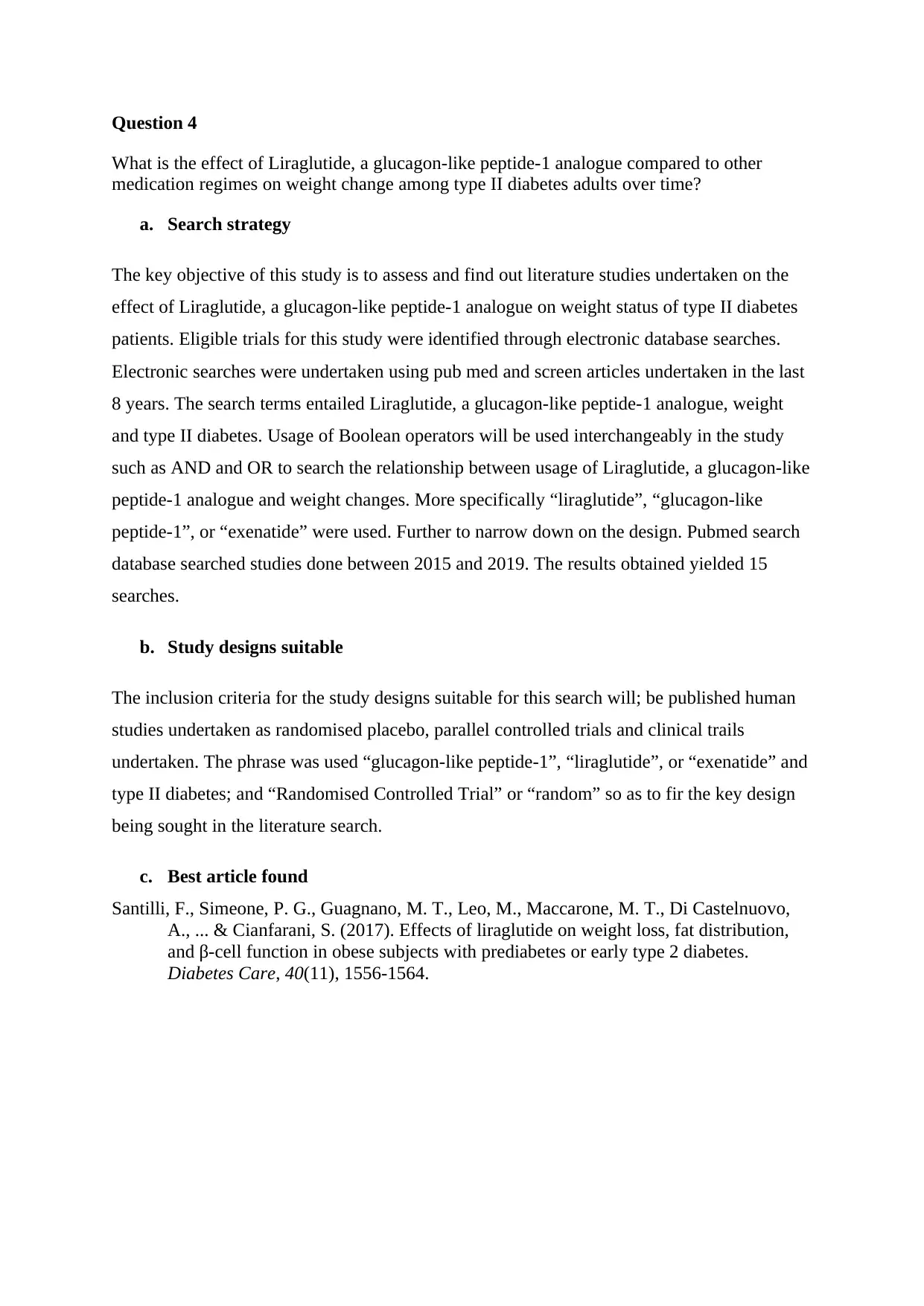
Question 1
a. What is effect of Liraglutide, a glucagon-like peptide-1 analogue compared top other
medication regimes on weight change among type II diabetes adults over time?
b. PICO elements in the research question
Population : Type II diabetes adults
Intervention : Liraglutide, a glucagon-like peptide-1 analogue
Comparison : Other type II diabetes
Outcome : weight reduction
Time : Medication period
Question 2
a. What are the risk factors associated to multi drug tuberculosis resistances among the
migrant populations after regular tuberculosis management?
b. PICO elements in the research question
Population : Migrant Populations
Intervention : Risk factors
Comparison : Other type II diabetes
Outcome : multi drug tuberculosis resistances
Time : -
Question 3
I : b
II : a
III : a
IV : a
V : e
VI : a
VII : d
a. What is effect of Liraglutide, a glucagon-like peptide-1 analogue compared top other
medication regimes on weight change among type II diabetes adults over time?
b. PICO elements in the research question
Population : Type II diabetes adults
Intervention : Liraglutide, a glucagon-like peptide-1 analogue
Comparison : Other type II diabetes
Outcome : weight reduction
Time : Medication period
Question 2
a. What are the risk factors associated to multi drug tuberculosis resistances among the
migrant populations after regular tuberculosis management?
b. PICO elements in the research question
Population : Migrant Populations
Intervention : Risk factors
Comparison : Other type II diabetes
Outcome : multi drug tuberculosis resistances
Time : -
Question 3
I : b
II : a
III : a
IV : a
V : e
VI : a
VII : d
Question 4
What is the effect of Liraglutide, a glucagon-like peptide-1 analogue compared to other
medication regimes on weight change among type II diabetes adults over time?
a. Search strategy
The key objective of this study is to assess and find out literature studies undertaken on the
effect of Liraglutide, a glucagon-like peptide-1 analogue on weight status of type II diabetes
patients. Eligible trials for this study were identified through electronic database searches.
Electronic searches were undertaken using pub med and screen articles undertaken in the last
8 years. The search terms entailed Liraglutide, a glucagon-like peptide-1 analogue, weight
and type II diabetes. Usage of Boolean operators will be used interchangeably in the study
such as AND and OR to search the relationship between usage of Liraglutide, a glucagon-like
peptide-1 analogue and weight changes. More specifically “liraglutide”, “glucagon-like
peptide-1”, or “exenatide” were used. Further to narrow down on the design. Pubmed search
database searched studies done between 2015 and 2019. The results obtained yielded 15
searches.
b. Study designs suitable
The inclusion criteria for the study designs suitable for this search will; be published human
studies undertaken as randomised placebo, parallel controlled trials and clinical trails
undertaken. The phrase was used “glucagon-like peptide-1”, “liraglutide”, or “exenatide” and
type II diabetes; and “Randomised Controlled Trial” or “random” so as to fir the key design
being sought in the literature search.
c. Best article found
Santilli, F., Simeone, P. G., Guagnano, M. T., Leo, M., Maccarone, M. T., Di Castelnuovo,
A., ... & Cianfarani, S. (2017). Effects of liraglutide on weight loss, fat distribution,
and β-cell function in obese subjects with prediabetes or early type 2 diabetes.
Diabetes Care, 40(11), 1556-1564.
What is the effect of Liraglutide, a glucagon-like peptide-1 analogue compared to other
medication regimes on weight change among type II diabetes adults over time?
a. Search strategy
The key objective of this study is to assess and find out literature studies undertaken on the
effect of Liraglutide, a glucagon-like peptide-1 analogue on weight status of type II diabetes
patients. Eligible trials for this study were identified through electronic database searches.
Electronic searches were undertaken using pub med and screen articles undertaken in the last
8 years. The search terms entailed Liraglutide, a glucagon-like peptide-1 analogue, weight
and type II diabetes. Usage of Boolean operators will be used interchangeably in the study
such as AND and OR to search the relationship between usage of Liraglutide, a glucagon-like
peptide-1 analogue and weight changes. More specifically “liraglutide”, “glucagon-like
peptide-1”, or “exenatide” were used. Further to narrow down on the design. Pubmed search
database searched studies done between 2015 and 2019. The results obtained yielded 15
searches.
b. Study designs suitable
The inclusion criteria for the study designs suitable for this search will; be published human
studies undertaken as randomised placebo, parallel controlled trials and clinical trails
undertaken. The phrase was used “glucagon-like peptide-1”, “liraglutide”, or “exenatide” and
type II diabetes; and “Randomised Controlled Trial” or “random” so as to fir the key design
being sought in the literature search.
c. Best article found
Santilli, F., Simeone, P. G., Guagnano, M. T., Leo, M., Maccarone, M. T., Di Castelnuovo,
A., ... & Cianfarani, S. (2017). Effects of liraglutide on weight loss, fat distribution,
and β-cell function in obese subjects with prediabetes or early type 2 diabetes.
Diabetes Care, 40(11), 1556-1564.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
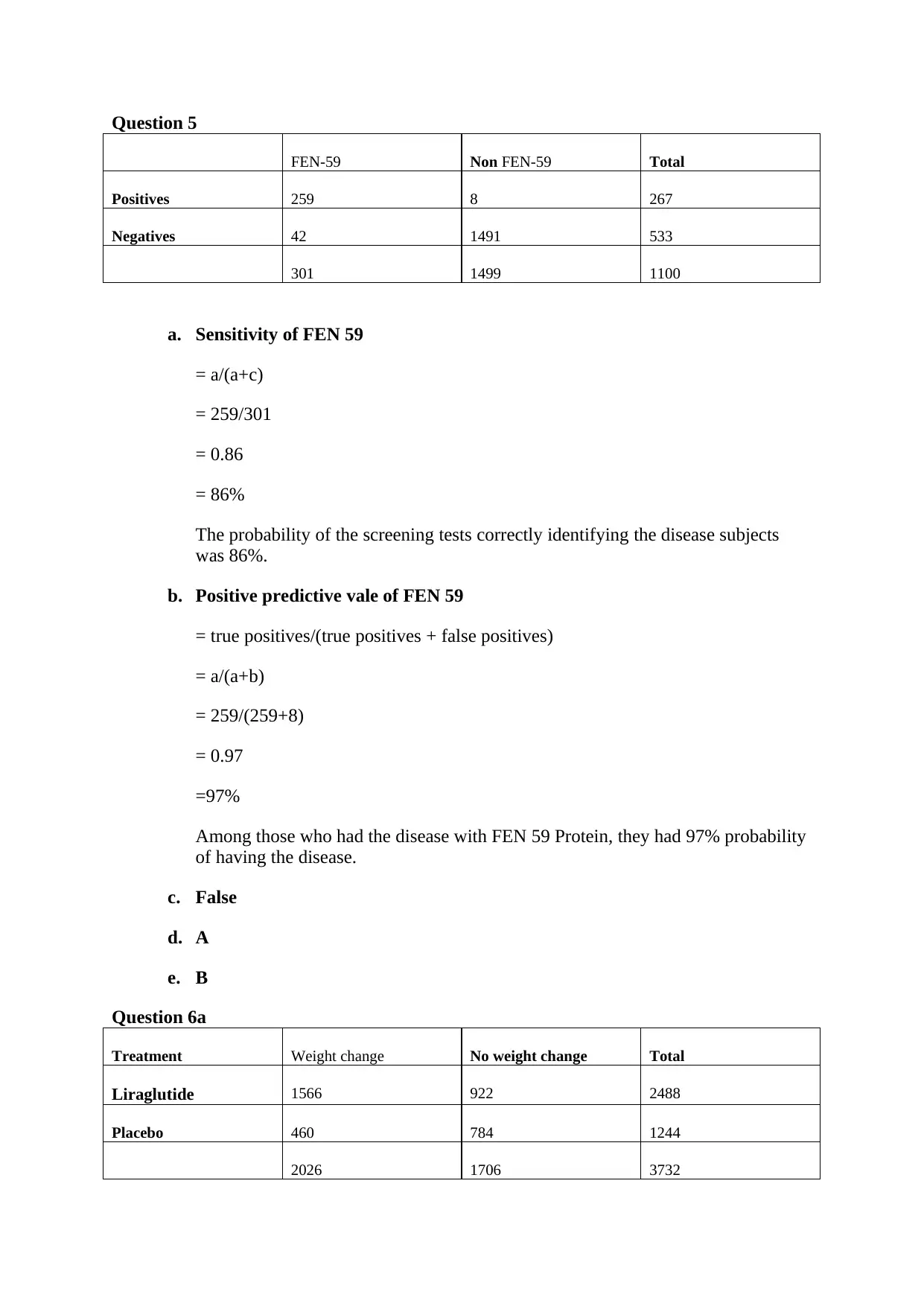
Question 5
FEN-59 Non FEN-59 Total
Positives 259 8 267
Negatives 42 1491 533
301 1499 1100
a. Sensitivity of FEN 59
= a/(a+c)
= 259/301
= 0.86
= 86%
The probability of the screening tests correctly identifying the disease subjects
was 86%.
b. Positive predictive vale of FEN 59
= true positives/(true positives + false positives)
= a/(a+b)
= 259/(259+8)
= 0.97
=97%
Among those who had the disease with FEN 59 Protein, they had 97% probability
of having the disease.
c. False
d. A
e. B
Question 6a
Treatment Weight change No weight change Total
Liraglutide 1566 922 2488
Placebo 460 784 1244
2026 1706 3732
FEN-59 Non FEN-59 Total
Positives 259 8 267
Negatives 42 1491 533
301 1499 1100
a. Sensitivity of FEN 59
= a/(a+c)
= 259/301
= 0.86
= 86%
The probability of the screening tests correctly identifying the disease subjects
was 86%.
b. Positive predictive vale of FEN 59
= true positives/(true positives + false positives)
= a/(a+b)
= 259/(259+8)
= 0.97
=97%
Among those who had the disease with FEN 59 Protein, they had 97% probability
of having the disease.
c. False
d. A
e. B
Question 6a
Treatment Weight change No weight change Total
Liraglutide 1566 922 2488
Placebo 460 784 1244
2026 1706 3732
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
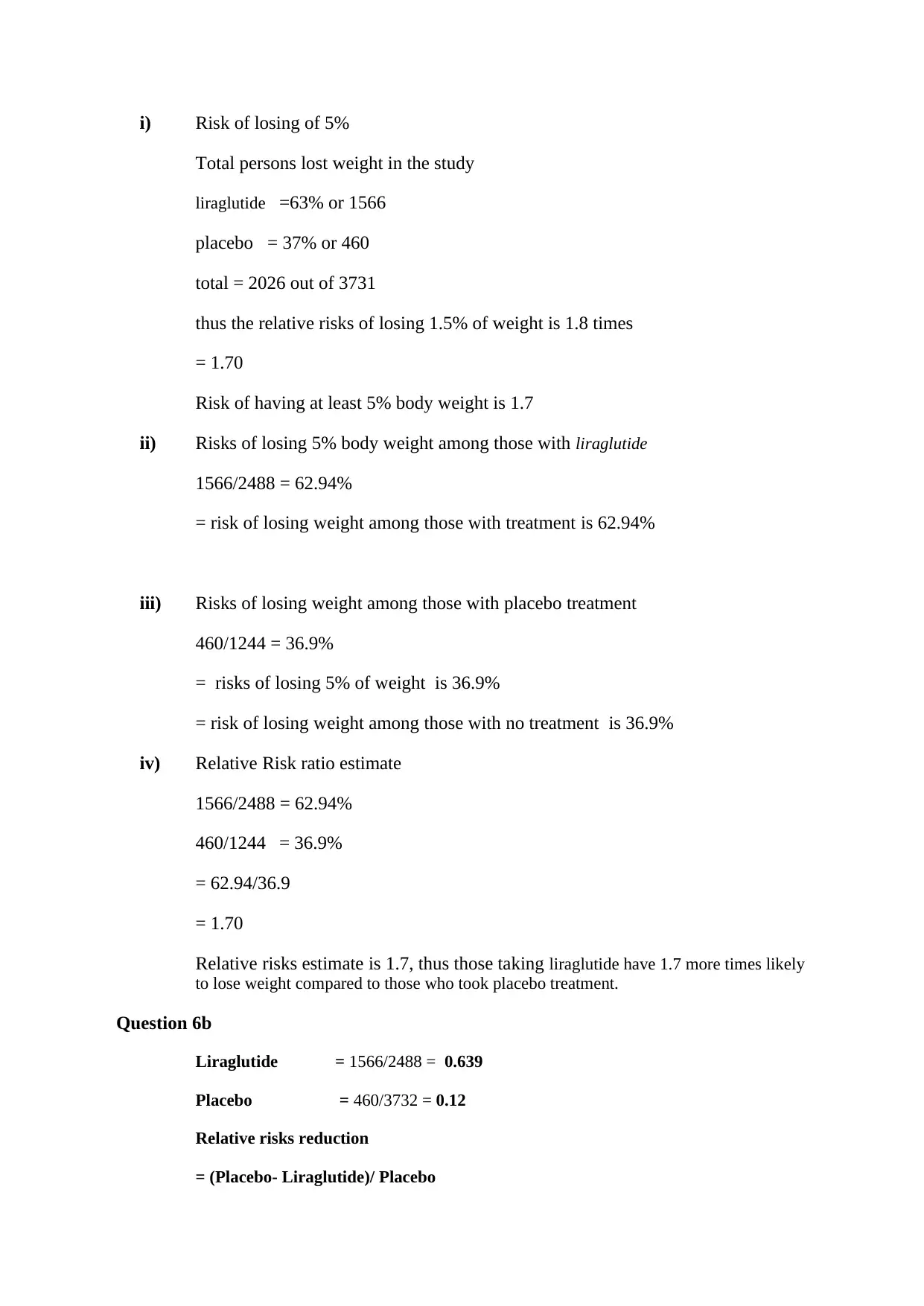
i) Risk of losing of 5%
Total persons lost weight in the study
liraglutide =63% or 1566
placebo = 37% or 460
total = 2026 out of 3731
thus the relative risks of losing 1.5% of weight is 1.8 times
= 1.70
Risk of having at least 5% body weight is 1.7
ii) Risks of losing 5% body weight among those with liraglutide
1566/2488 = 62.94%
= risk of losing weight among those with treatment is 62.94%
iii) Risks of losing weight among those with placebo treatment
460/1244 = 36.9%
= risks of losing 5% of weight is 36.9%
= risk of losing weight among those with no treatment is 36.9%
iv) Relative Risk ratio estimate
1566/2488 = 62.94%
460/1244 = 36.9%
= 62.94/36.9
= 1.70
Relative risks estimate is 1.7, thus those taking liraglutide have 1.7 more times likely
to lose weight compared to those who took placebo treatment.
Question 6b
Liraglutide = 1566/2488 = 0.639
Placebo = 460/3732 = 0.12
Relative risks reduction
= (Placebo- Liraglutide)/ Placebo
Total persons lost weight in the study
liraglutide =63% or 1566
placebo = 37% or 460
total = 2026 out of 3731
thus the relative risks of losing 1.5% of weight is 1.8 times
= 1.70
Risk of having at least 5% body weight is 1.7
ii) Risks of losing 5% body weight among those with liraglutide
1566/2488 = 62.94%
= risk of losing weight among those with treatment is 62.94%
iii) Risks of losing weight among those with placebo treatment
460/1244 = 36.9%
= risks of losing 5% of weight is 36.9%
= risk of losing weight among those with no treatment is 36.9%
iv) Relative Risk ratio estimate
1566/2488 = 62.94%
460/1244 = 36.9%
= 62.94/36.9
= 1.70
Relative risks estimate is 1.7, thus those taking liraglutide have 1.7 more times likely
to lose weight compared to those who took placebo treatment.
Question 6b
Liraglutide = 1566/2488 = 0.639
Placebo = 460/3732 = 0.12
Relative risks reduction
= (Placebo- Liraglutide)/ Placebo
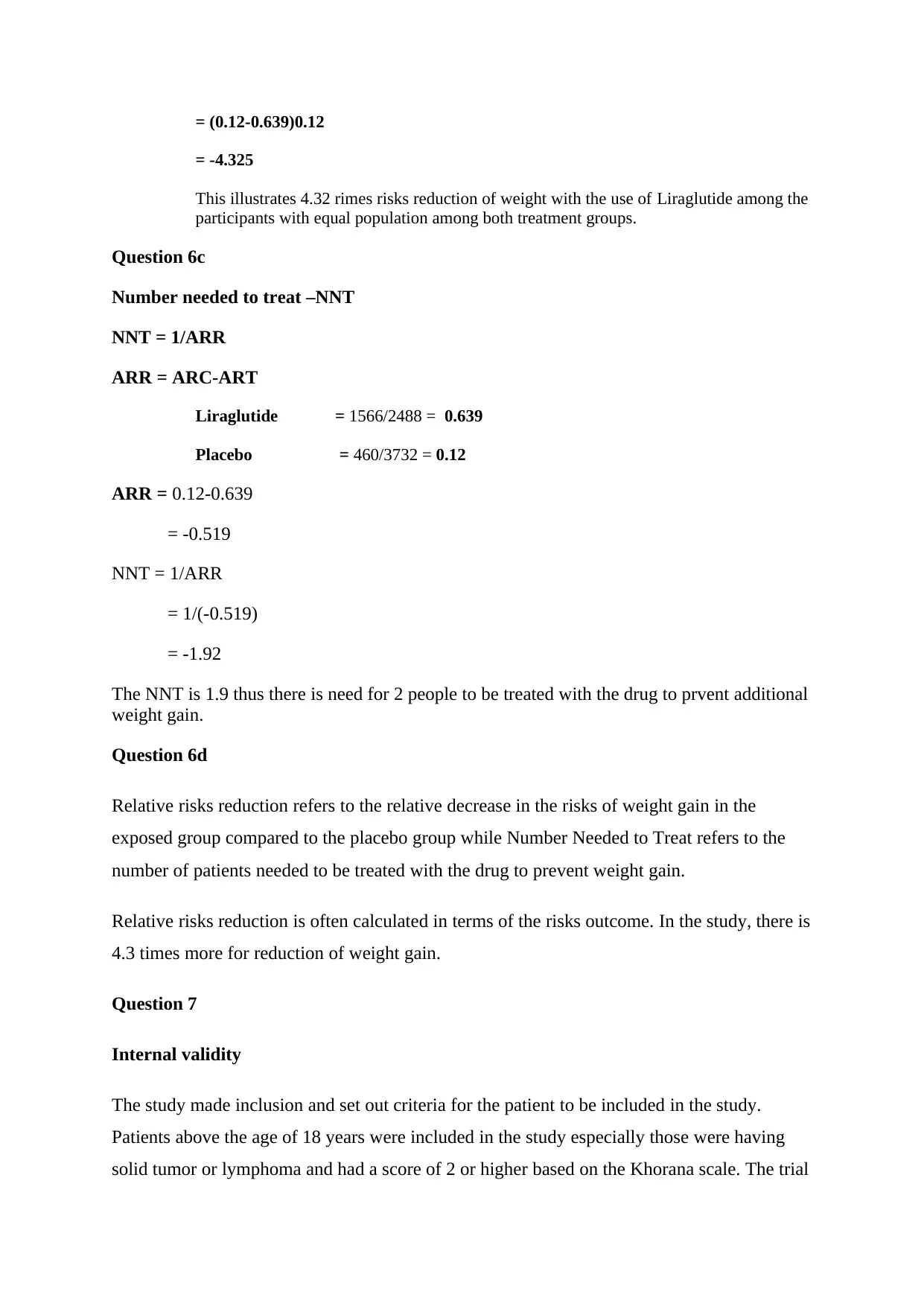
= (0.12-0.639)0.12
= -4.325
This illustrates 4.32 rimes risks reduction of weight with the use of Liraglutide among the
participants with equal population among both treatment groups.
Question 6c
Number needed to treat –NNT
NNT = 1/ARR
ARR = ARC-ART
Liraglutide = 1566/2488 = 0.639
Placebo = 460/3732 = 0.12
ARR = 0.12-0.639
= -0.519
NNT = 1/ARR
= 1/(-0.519)
= -1.92
The NNT is 1.9 thus there is need for 2 people to be treated with the drug to prvent additional
weight gain.
Question 6d
Relative risks reduction refers to the relative decrease in the risks of weight gain in the
exposed group compared to the placebo group while Number Needed to Treat refers to the
number of patients needed to be treated with the drug to prevent weight gain.
Relative risks reduction is often calculated in terms of the risks outcome. In the study, there is
4.3 times more for reduction of weight gain.
Question 7
Internal validity
The study made inclusion and set out criteria for the patient to be included in the study.
Patients above the age of 18 years were included in the study especially those were having
solid tumor or lymphoma and had a score of 2 or higher based on the Khorana scale. The trial
= -4.325
This illustrates 4.32 rimes risks reduction of weight with the use of Liraglutide among the
participants with equal population among both treatment groups.
Question 6c
Number needed to treat –NNT
NNT = 1/ARR
ARR = ARC-ART
Liraglutide = 1566/2488 = 0.639
Placebo = 460/3732 = 0.12
ARR = 0.12-0.639
= -0.519
NNT = 1/ARR
= 1/(-0.519)
= -1.92
The NNT is 1.9 thus there is need for 2 people to be treated with the drug to prvent additional
weight gain.
Question 6d
Relative risks reduction refers to the relative decrease in the risks of weight gain in the
exposed group compared to the placebo group while Number Needed to Treat refers to the
number of patients needed to be treated with the drug to prevent weight gain.
Relative risks reduction is often calculated in terms of the risks outcome. In the study, there is
4.3 times more for reduction of weight gain.
Question 7
Internal validity
The study made inclusion and set out criteria for the patient to be included in the study.
Patients above the age of 18 years were included in the study especially those were having
solid tumor or lymphoma and had a score of 2 or higher based on the Khorana scale. The trial
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
design employed was a multicenter randomized double-blind, placebo-controlled study in
phase 3 b trial. The patients were enrolled and underwent venous duplex compression
ultrasonography of both legs in order to eliminate any chance of existing deep vein
thrombosis. The study undertook the random assignment of the subjects in an equal ratio of
1:1 in order of receiving the treatment drug and those of the placebo treatment limited
confounding factors related to the selection of treatment biases. There was randomization and
stratification base on the tumor site location. Further, there was an adjustment of the trials
visits undertaken in all the treatment sites.
In order to assess measurement accurately and ensures that internal errors were minimized,
primary efficacy endpoint was undertaken in the study so as to have objective confirmation of
whether there was confirmed symptomatic or asymptomatic occurrence of proximal deep
vein thrombosis on the lower limb, symptomatic occurrence the upper limb, occurrence of
pulmonary embolism and death occurrence of venous thromboembolism. Further, secondary
efficacy methods encompassed primary endpoint assessments. These included symptomatic
venous thromboembolism and other clinically relevant endpoint activities. This was critical to
ensure that occurrence of the disease of interest was carefully assessed with a clear protocol.
Further endpoint assessment measures were undertaken using the endpoint committee who
were double-blind and not aware of the study details.
Further, the trial was over sighted by a steering committee that had enough input on the
endpoint selection and adjustment of analysis. The oversight committee was essential in
assessing and oversight in how the study was conducted and data reporting so as to get
accurate data from the study. Further to ensure there was no biased in the reporting of the
results, all the authors and input in the overall interpretation of the results of the study, thus
improving the general internal validity of the findings obtained.
Question 8 Clinical and statistical significance
The statistical significance of the results based on primary efficacy endpoint composite
demonstrated that 6% in the rivaroxaban group and in 8.8% in the placebo group (hazard
ratio, 0.66; 95% confidence interval [CI], 0.40 to 1.09; P = 0.10 signifying statistical
significance, after adjusting for confiding factors such as the death, the occurring hazard ratio
the hazard ratio was 0.64 [95% CI, 0.39 to 1.07].
Among the randomized patients, assessment during the intervention period showed that 2.6%
phase 3 b trial. The patients were enrolled and underwent venous duplex compression
ultrasonography of both legs in order to eliminate any chance of existing deep vein
thrombosis. The study undertook the random assignment of the subjects in an equal ratio of
1:1 in order of receiving the treatment drug and those of the placebo treatment limited
confounding factors related to the selection of treatment biases. There was randomization and
stratification base on the tumor site location. Further, there was an adjustment of the trials
visits undertaken in all the treatment sites.
In order to assess measurement accurately and ensures that internal errors were minimized,
primary efficacy endpoint was undertaken in the study so as to have objective confirmation of
whether there was confirmed symptomatic or asymptomatic occurrence of proximal deep
vein thrombosis on the lower limb, symptomatic occurrence the upper limb, occurrence of
pulmonary embolism and death occurrence of venous thromboembolism. Further, secondary
efficacy methods encompassed primary endpoint assessments. These included symptomatic
venous thromboembolism and other clinically relevant endpoint activities. This was critical to
ensure that occurrence of the disease of interest was carefully assessed with a clear protocol.
Further endpoint assessment measures were undertaken using the endpoint committee who
were double-blind and not aware of the study details.
Further, the trial was over sighted by a steering committee that had enough input on the
endpoint selection and adjustment of analysis. The oversight committee was essential in
assessing and oversight in how the study was conducted and data reporting so as to get
accurate data from the study. Further to ensure there was no biased in the reporting of the
results, all the authors and input in the overall interpretation of the results of the study, thus
improving the general internal validity of the findings obtained.
Question 8 Clinical and statistical significance
The statistical significance of the results based on primary efficacy endpoint composite
demonstrated that 6% in the rivaroxaban group and in 8.8% in the placebo group (hazard
ratio, 0.66; 95% confidence interval [CI], 0.40 to 1.09; P = 0.10 signifying statistical
significance, after adjusting for confiding factors such as the death, the occurring hazard ratio
the hazard ratio was 0.64 [95% CI, 0.39 to 1.07].
Among the randomized patients, assessment during the intervention period showed that 2.6%
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of the patients in the rivaroxaban group and 27 of 421 (6.4%) in the placebo group (hazard
ratio, 0.40; 95% CI, 0.20 to 0.80). there was no heterogeneity of effect was observed among
the rivaroxaban treatment was detected for any pre-specified subgroup with P>0.10.
The primary endpoint revealed that the occurrence of arterial thrombo embolisms occurred
among 1% of the rivaroxaban group and in 1.7% in the placebo group. The pre-specified
analysis showed that lower incidences of thromboembolic events lower in the rivaroxaban
group than in the placebo group (6.9% vs. 10.7%; hazard ratio, 0.62; 95% CI, 0.39 to 0.99).
In the secondary endpoint assessments, endpoint deaths in the study period showed that 20%
deaths occurred among the rivaroxaban group and 100 deaths (23.8%) in the placebo group
(hazard ratio, 0.83; 95% CI, 0.62 to 1.11). further in a prespecified composite of the primary
endpoint on death and any other cause occurred among them in 23.1% of the patients in the
rivaroxaban group and in 29.5% of those in the placebo group (hazard ratio, 0.75; 95% CI,
0.57 to 0.97).
Further on endpoint safety, showed that major bleeding was observed among 2% receiving
rivaroxaban and in 1.0% receiving placebo (hazard ratio, 1.96; 95% CI, 0.59 to 6.49. further
clinical relevancy no major bleeding was observed among 2.7% of the patients in the
treatment group compared to 2% in the placebo group at hazard ratio at 1.34; 95% CI, 0.54 to
3.32.
Comparing the rivaroxaban with placebo for primary thromboprophylaxis among the
ambulated patients having cancer having high risks occurrence of venous thromboembolism
and were initiating a new systemic cancer therapy. The study adopted an intention to treat
approach; the primary endpoint occurred in lower levels among patient randomly assigned to
treatment with rivaroxaban, the results were not significantly relevant. However, despite this
pre-specified assessment showed that there was change by 4% favoring the use of
rivaroxaban against the placebo treatment on endpoint venous thromboembolism and venous
thromboembolism-related death. Further, all-cause mortality was lower in the treatment
group is 3.8% lower than the placebo group and endpoint composite event of venous
thromboembolism was lower by 6.4%. The rivaroxaban treatment was clinically significant
and relevant among the venous thromboembolism patients.
ratio, 0.40; 95% CI, 0.20 to 0.80). there was no heterogeneity of effect was observed among
the rivaroxaban treatment was detected for any pre-specified subgroup with P>0.10.
The primary endpoint revealed that the occurrence of arterial thrombo embolisms occurred
among 1% of the rivaroxaban group and in 1.7% in the placebo group. The pre-specified
analysis showed that lower incidences of thromboembolic events lower in the rivaroxaban
group than in the placebo group (6.9% vs. 10.7%; hazard ratio, 0.62; 95% CI, 0.39 to 0.99).
In the secondary endpoint assessments, endpoint deaths in the study period showed that 20%
deaths occurred among the rivaroxaban group and 100 deaths (23.8%) in the placebo group
(hazard ratio, 0.83; 95% CI, 0.62 to 1.11). further in a prespecified composite of the primary
endpoint on death and any other cause occurred among them in 23.1% of the patients in the
rivaroxaban group and in 29.5% of those in the placebo group (hazard ratio, 0.75; 95% CI,
0.57 to 0.97).
Further on endpoint safety, showed that major bleeding was observed among 2% receiving
rivaroxaban and in 1.0% receiving placebo (hazard ratio, 1.96; 95% CI, 0.59 to 6.49. further
clinical relevancy no major bleeding was observed among 2.7% of the patients in the
treatment group compared to 2% in the placebo group at hazard ratio at 1.34; 95% CI, 0.54 to
3.32.
Comparing the rivaroxaban with placebo for primary thromboprophylaxis among the
ambulated patients having cancer having high risks occurrence of venous thromboembolism
and were initiating a new systemic cancer therapy. The study adopted an intention to treat
approach; the primary endpoint occurred in lower levels among patient randomly assigned to
treatment with rivaroxaban, the results were not significantly relevant. However, despite this
pre-specified assessment showed that there was change by 4% favoring the use of
rivaroxaban against the placebo treatment on endpoint venous thromboembolism and venous
thromboembolism-related death. Further, all-cause mortality was lower in the treatment
group is 3.8% lower than the placebo group and endpoint composite event of venous
thromboembolism was lower by 6.4%. The rivaroxaban treatment was clinically significant
and relevant among the venous thromboembolism patients.
Question 9
Generazability of the findings
The findings of this study have demonstrated consistency with other similar studies
undertaken on the treatment drug obtained from larger trials than this study. Further, the
intervention approach used in this study is in tandem with the larger trails cited in the study
which utilized the same intervention period and primary analysis.
Further, there was an effective randomization of the participants used in the study. The
subjects used were representative of the entire population and selection process. Random
assigning was performed among the patient who had no previous history of thrombosis and
received treatment and placebo at an equal ratio of 1:1 limiting any biases. Further computer
randomization was stratified based on the tumor site occurrence, thus limiting any occurrence
of treatment by chance.
Further, the study participants who discontinued on the treatment regime were followed to
assess and guarantee efficacy which demonstrated that 395 of these encountered primary
endpoint events. Evaluation of baseline and outcomes of the patients was under went and
there were no major differences obtained indicating the effect was not influenced by other
causes not accounted in the study design.
The study further, used similar design analysis used and obtained from other studies, which
showed some level of consistency. The population selected to participate in this study fitted
the actual criteria being focussed of the study. The study chooses specifically patients who
met the criteria based on occurrence and presence of solid tumor or lymphoma and has a
minimum score of 2 at baseline using Khorana score. The Khorana is a risks assessment tool
which has been validated to assess risks of venous thromboembolism. Further, the design
study of the study of entrenching randomization and double-blind designs make it efficient to
be generalized to other settings. Thus with all these aspects, the study qualifies for
generalization to other larger settings.
Generazability of the findings
The findings of this study have demonstrated consistency with other similar studies
undertaken on the treatment drug obtained from larger trials than this study. Further, the
intervention approach used in this study is in tandem with the larger trails cited in the study
which utilized the same intervention period and primary analysis.
Further, there was an effective randomization of the participants used in the study. The
subjects used were representative of the entire population and selection process. Random
assigning was performed among the patient who had no previous history of thrombosis and
received treatment and placebo at an equal ratio of 1:1 limiting any biases. Further computer
randomization was stratified based on the tumor site occurrence, thus limiting any occurrence
of treatment by chance.
Further, the study participants who discontinued on the treatment regime were followed to
assess and guarantee efficacy which demonstrated that 395 of these encountered primary
endpoint events. Evaluation of baseline and outcomes of the patients was under went and
there were no major differences obtained indicating the effect was not influenced by other
causes not accounted in the study design.
The study further, used similar design analysis used and obtained from other studies, which
showed some level of consistency. The population selected to participate in this study fitted
the actual criteria being focussed of the study. The study chooses specifically patients who
met the criteria based on occurrence and presence of solid tumor or lymphoma and has a
minimum score of 2 at baseline using Khorana score. The Khorana is a risks assessment tool
which has been validated to assess risks of venous thromboembolism. Further, the design
study of the study of entrenching randomization and double-blind designs make it efficient to
be generalized to other settings. Thus with all these aspects, the study qualifies for
generalization to other larger settings.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
