Clinical Project: Nursing Management of Diabetic Foot and Ulcers
VerifiedAdded on 2023/06/10
|15
|3210
|79
Report
AI Summary
This report delves into the nursing management of diabetic foot, a critical area of healthcare given the increasing prevalence of diabetes and its associated complications. It begins with an introduction highlighting the global impact of diabetes and the significant risk of diabetic foot ulcers, including potential outcomes like amputation. The report then explores Benner's Novice to Expert theory, outlining the stages of clinical competence and how nurses progress in their ability to care for patients. A clinical project focused on identifying factors contributing to diabetic foot infections and ulcers, prevention strategies, and the importance of patient education is also examined. Key risk factors such as poor footwear, poorly controlled diabetes, and infections are discussed, emphasizing the role of nurses in providing patient education on foot care principles. The report outlines essential diabetic foot care principles gained through nurse education, including daily foot examinations, hygiene practices, and appropriate footwear choices. Furthermore, it addresses the major contributors to diabetic foot ulcers (peripheral vascular disease, infections, and peripheral neuropathy) and the critical roles nurses play in screening, wound dressing, and overall patient care. The report emphasizes the need for early intervention and comprehensive nursing care to improve outcomes for individuals with diabetic foot complications.

Running head: NURSING MANAGEMENT OF DIABETIC FOOT 1
Nursing Management of Diabetic Foot
Name
Institutional affiliation
Nursing Management of Diabetic Foot
Name
Institutional affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING MANAGEMENT OF DIABETIC FOOT 2
Introduction
Reports emanating from the World Health Organisation (WHO) indicate that by 2000,
the number of patients suffering from diabetes had reached 171 million with the figure being
prospected to escalate to 380 million by the year 2025 (WHO, 2016). Existing evidence is
enough demonstration of the sub sequential consequences that have prevailed on the patients
themselves, providers of healthcare and to the community at large. To the patients, for instance,
Diabetes malady leads to excess glucose (a type of sugar) in their blood. As times moves by,
surplus content of glucose in the blood damages the body's organs. Conceivable impediments
include damage to small (microvascular) and large (macrovascular) blood vessels, which can
contribute to stroke, heart attack, and complications with the gums, nerves, feet, kidneys, and
eyes. The solution to this menace can only therefore be attained through close interrelationships
between people and health systems. Previous studies have also gone further into proving that of
all diabetic patients, 15% of them will suffer from diabetic foot ulcer throughout their entire life.
Diabetic patients find this type of ulcer as the most common cause of their hospitalization.
It is worth noting that whenever adequate care is not availed to diabetic foot ulcers,
severe conditions which include gangrene, other infections, amputations and even death may
result (McDermott, 2016). Risk factors associated with the progress of diabetic foot ulcers are
older age, cigarette smoking, infection, poor glycemic control, ischemia of small and large blood
vessels, previous foot ulcerations or amputations, diabetic neuropathy, and peripheral vascular
disease. Previous antiquity of foot disease, foot malformations which create strangely weakened
ability to look after personal care (for example visual impairment), renal failure, oedema, high
forces of pressure are further risk factors concomitant with diabetic foot ulcer. It has been
documented that the rate of amputation of the lower limbs in non-diabetic patients is generally
Introduction
Reports emanating from the World Health Organisation (WHO) indicate that by 2000,
the number of patients suffering from diabetes had reached 171 million with the figure being
prospected to escalate to 380 million by the year 2025 (WHO, 2016). Existing evidence is
enough demonstration of the sub sequential consequences that have prevailed on the patients
themselves, providers of healthcare and to the community at large. To the patients, for instance,
Diabetes malady leads to excess glucose (a type of sugar) in their blood. As times moves by,
surplus content of glucose in the blood damages the body's organs. Conceivable impediments
include damage to small (microvascular) and large (macrovascular) blood vessels, which can
contribute to stroke, heart attack, and complications with the gums, nerves, feet, kidneys, and
eyes. The solution to this menace can only therefore be attained through close interrelationships
between people and health systems. Previous studies have also gone further into proving that of
all diabetic patients, 15% of them will suffer from diabetic foot ulcer throughout their entire life.
Diabetic patients find this type of ulcer as the most common cause of their hospitalization.
It is worth noting that whenever adequate care is not availed to diabetic foot ulcers,
severe conditions which include gangrene, other infections, amputations and even death may
result (McDermott, 2016). Risk factors associated with the progress of diabetic foot ulcers are
older age, cigarette smoking, infection, poor glycemic control, ischemia of small and large blood
vessels, previous foot ulcerations or amputations, diabetic neuropathy, and peripheral vascular
disease. Previous antiquity of foot disease, foot malformations which create strangely weakened
ability to look after personal care (for example visual impairment), renal failure, oedema, high
forces of pressure are further risk factors concomitant with diabetic foot ulcer. It has been
documented that the rate of amputation of the lower limbs in non-diabetic patients is generally
NURSING MANAGEMENT OF DIABETIC FOOT 3
30 times lower that of diabetic patients it has again been proven that diabetes results to one leg
being amputated every thirty seconds worldwide. Generally, two years after the first amputation,
the patient is at a 50% risk to undergo a second amputation. About three years after the
amputation of the lower limb, death occurs to more than 50% of the patients.
Benner Novice Theory
Dr. Patricia Benner, a nursing theorist formulated a model of the stages to be adopted
towards clinical competence (Benner, 2001) as documented in her book, "From Novice to
Expert: Excellence and Power in Clinical Nursing Practice." This is what later adopted the name
Benner Novice Theory. The first stage is referred to as Novice. Usually the student here is at
his/her first year of education. Such students have very limited potential of predicting the
possible outcomes of patients in particular situations. Such a student is able to recognize
complex signs and symptoms which could include variations in mental status only after exposure
to patients with similar signs. At the second stage, the student graduates to an advanced beginner.
It is here that they have already gained relevant and adequate experience to enable them
distinguish meaningful and recurrent compositions of a patient’s situation. However, although
they have already grasped substantial amounts of knowledge and knowledge, they are still in
deficit of adequate in-depth experience (Utley, 2010).
At the third stage, they are to acquire relevant competency (Siviter, 2013). Though the
student is now sailing towards nursing excellence, the main hindering block at this stage is lack
of flexibility and speed that is required of a proficient nurse. They have however mastered
relevant skills on the art of advanced organisation and planning. They however need to make
recognition of nature and patterns of clinical situations at a quicker pace so as to distinguish
themselves from advanced beginners. The student now becomes proficient at the fourth stage.
30 times lower that of diabetic patients it has again been proven that diabetes results to one leg
being amputated every thirty seconds worldwide. Generally, two years after the first amputation,
the patient is at a 50% risk to undergo a second amputation. About three years after the
amputation of the lower limb, death occurs to more than 50% of the patients.
Benner Novice Theory
Dr. Patricia Benner, a nursing theorist formulated a model of the stages to be adopted
towards clinical competence (Benner, 2001) as documented in her book, "From Novice to
Expert: Excellence and Power in Clinical Nursing Practice." This is what later adopted the name
Benner Novice Theory. The first stage is referred to as Novice. Usually the student here is at
his/her first year of education. Such students have very limited potential of predicting the
possible outcomes of patients in particular situations. Such a student is able to recognize
complex signs and symptoms which could include variations in mental status only after exposure
to patients with similar signs. At the second stage, the student graduates to an advanced beginner.
It is here that they have already gained relevant and adequate experience to enable them
distinguish meaningful and recurrent compositions of a patient’s situation. However, although
they have already grasped substantial amounts of knowledge and knowledge, they are still in
deficit of adequate in-depth experience (Utley, 2010).
At the third stage, they are to acquire relevant competency (Siviter, 2013). Though the
student is now sailing towards nursing excellence, the main hindering block at this stage is lack
of flexibility and speed that is required of a proficient nurse. They have however mastered
relevant skills on the art of advanced organisation and planning. They however need to make
recognition of nature and patterns of clinical situations at a quicker pace so as to distinguish
themselves from advanced beginners. The student now becomes proficient at the fourth stage.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING MANAGEMENT OF DIABETIC FOOT 4
Here, they are able to integrate situations wholly rather than partly (Fitzpatrick & Wallace,
2006). Proficient nurses have the capability to make modifications to plans as a way of
responding to different situations while at the same time they have the ability to tell the events
that are to occur by basing on past experiences.
The fifth and final stage is where the students become an expert in the field. Here, the
nurse is able to attain his/her goals by recognizing the demand s and resources to apply in
particular situations. Such a nurse knows exactly what is supposed to be done and therefore no
longer relies on rules for guidance whenever taking actions for any situation (Masters, 2014).
Basing on their deep experience and knowledge, they have already grasped the go about of any
kind of situation that may prevail. They have again learnt to focus on situations that are of great
relevance while at the same time dedicating less focus on irrelevant situations. Whenever they
are in deficit of experience, most probably due to the occurrence of a new event, or when events
occur contrary to expectations, expert nurses embrace the use of analytical tools in order to get
the way forward in terms of the directions to adopt in such a situation (DeLaune, Ladner,
McTier, Tollefson , & Lawrence, 2016).
Clinical project for Nursing Management of Diabetic Foot
The chief aim of this project was to identify the various factors that cause foot infections
in a diabetic patient. Also studied are the various factors that are the chief drivers towards
development of diabetic foot ulcers. Various methods of preventing the same were identified and
patient education identified as the most effective way of caring for diabetic foot. Appropriate
resources were reviewed to come up with relevant information for to boost success if the project.
In connection to this, the articles that were reviewed were, Wells, C. (2015, September).
Orchestrating Healing: a Grounded Theory of Registered Nurses Caring for Patients with
Here, they are able to integrate situations wholly rather than partly (Fitzpatrick & Wallace,
2006). Proficient nurses have the capability to make modifications to plans as a way of
responding to different situations while at the same time they have the ability to tell the events
that are to occur by basing on past experiences.
The fifth and final stage is where the students become an expert in the field. Here, the
nurse is able to attain his/her goals by recognizing the demand s and resources to apply in
particular situations. Such a nurse knows exactly what is supposed to be done and therefore no
longer relies on rules for guidance whenever taking actions for any situation (Masters, 2014).
Basing on their deep experience and knowledge, they have already grasped the go about of any
kind of situation that may prevail. They have again learnt to focus on situations that are of great
relevance while at the same time dedicating less focus on irrelevant situations. Whenever they
are in deficit of experience, most probably due to the occurrence of a new event, or when events
occur contrary to expectations, expert nurses embrace the use of analytical tools in order to get
the way forward in terms of the directions to adopt in such a situation (DeLaune, Ladner,
McTier, Tollefson , & Lawrence, 2016).
Clinical project for Nursing Management of Diabetic Foot
The chief aim of this project was to identify the various factors that cause foot infections
in a diabetic patient. Also studied are the various factors that are the chief drivers towards
development of diabetic foot ulcers. Various methods of preventing the same were identified and
patient education identified as the most effective way of caring for diabetic foot. Appropriate
resources were reviewed to come up with relevant information for to boost success if the project.
In connection to this, the articles that were reviewed were, Wells, C. (2015, September).
Orchestrating Healing: a Grounded Theory of Registered Nurses Caring for Patients with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING MANAGEMENT OF DIABETIC FOOT 5
Diabetic Foot Ulcers, McDermott, A. (2016). Diabetes and amputation. Healthline amongst other
books.
For any person suffering from diabetes, the levels of blood sugars or blood glucose is
definitely too high (Ruhl, 2017). With passage of time, such high levels cause damage to blood
vessels or to the nerves. Diabetes instigated nerve damage causes one to completely loose feeling
in their feet and as a result such individuals may not feel a sore, blister or even a cut (Holt,
2009). Such foot injuries are the key causal factors of infections and ulcers. It is of great
significance for individuals and more precisely diabetes patients to seek medical intervention
upon noticing such sores as serious cases would even result to amputation of the limbs. Damage
caused on blood vessels also mean that there is no proper circulation of oxygen and blood and
hence healing of the foot may prove hard. Treatment efforts are also rendered fruitless as poor
blood circulation sees to it that antibiotics ingested do not get to the infection site. Once a person
has developed such diabetic foot problems, it is of great significance that they receive intensive
nursing care to propel healing of their condition in relation to quality nursing care.
There are several keys compelling factors towards diabetic foot problems, the key
amongst them being the type of footwear that an individual use (Nather, 2008). Shoes that are
poorly fitting are the leading factors towards the same. Presence of blisters, corns, sore spots,
consistent pain, calluses and/or red spots in the legs, with the pre-mentioned being directly
attributable to poor footwear, new shoes that are properly fitting must be obtained with
immediate effect. Poorly controlled diabetes or that which could be long-standing greatly
increases the risks of such individuals of suffering from peripheral neuropathy. A wide range of
infections are also known to trigger diabetic foot problems (Edmonds, Foster, & Sanders, 2008).
Serious bacterial infections could emanate from Athlete’s foot which is just a fungal infection.
Diabetic Foot Ulcers, McDermott, A. (2016). Diabetes and amputation. Healthline amongst other
books.
For any person suffering from diabetes, the levels of blood sugars or blood glucose is
definitely too high (Ruhl, 2017). With passage of time, such high levels cause damage to blood
vessels or to the nerves. Diabetes instigated nerve damage causes one to completely loose feeling
in their feet and as a result such individuals may not feel a sore, blister or even a cut (Holt,
2009). Such foot injuries are the key causal factors of infections and ulcers. It is of great
significance for individuals and more precisely diabetes patients to seek medical intervention
upon noticing such sores as serious cases would even result to amputation of the limbs. Damage
caused on blood vessels also mean that there is no proper circulation of oxygen and blood and
hence healing of the foot may prove hard. Treatment efforts are also rendered fruitless as poor
blood circulation sees to it that antibiotics ingested do not get to the infection site. Once a person
has developed such diabetic foot problems, it is of great significance that they receive intensive
nursing care to propel healing of their condition in relation to quality nursing care.
There are several keys compelling factors towards diabetic foot problems, the key
amongst them being the type of footwear that an individual use (Nather, 2008). Shoes that are
poorly fitting are the leading factors towards the same. Presence of blisters, corns, sore spots,
consistent pain, calluses and/or red spots in the legs, with the pre-mentioned being directly
attributable to poor footwear, new shoes that are properly fitting must be obtained with
immediate effect. Poorly controlled diabetes or that which could be long-standing greatly
increases the risks of such individuals of suffering from peripheral neuropathy. A wide range of
infections are also known to trigger diabetic foot problems (Edmonds, Foster, & Sanders, 2008).
Serious bacterial infections could emanate from Athlete’s foot which is just a fungal infection.
NURSING MANAGEMENT OF DIABETIC FOOT 6
Toenail fungus should be treated with immediate effect and is to be avoided by involving a foot
specialist in handling ingrown toenails. It is also worth noting that any form of tobacco that is
smokes results to damage of blood vessels located in the legs.
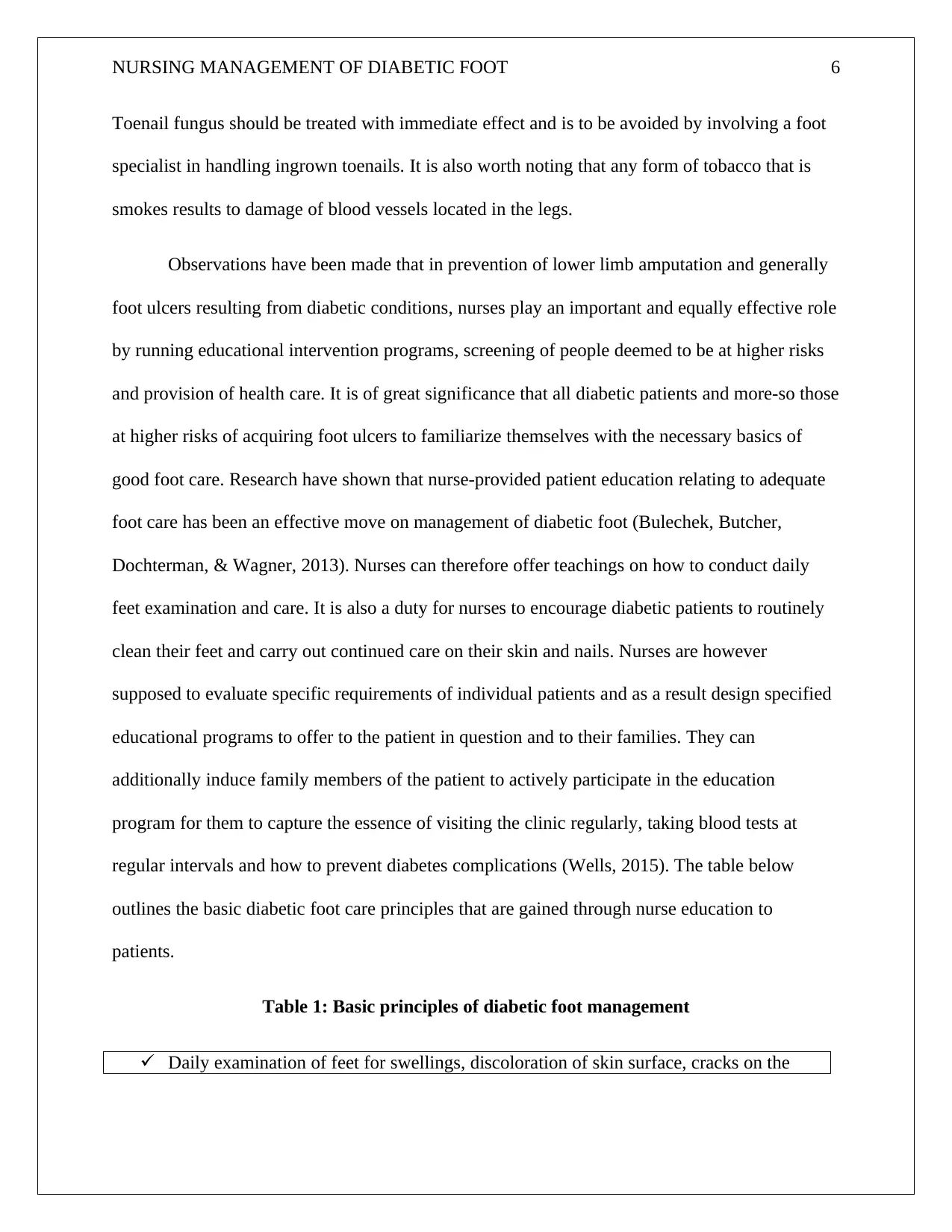
Observations have been made that in prevention of lower limb amputation and generally
foot ulcers resulting from diabetic conditions, nurses play an important and equally effective role
by running educational intervention programs, screening of people deemed to be at higher risks
and provision of health care. It is of great significance that all diabetic patients and more-so those
at higher risks of acquiring foot ulcers to familiarize themselves with the necessary basics of
good foot care. Research have shown that nurse-provided patient education relating to adequate
foot care has been an effective move on management of diabetic foot (Bulechek, Butcher,
Dochterman, & Wagner, 2013). Nurses can therefore offer teachings on how to conduct daily
feet examination and care. It is also a duty for nurses to encourage diabetic patients to routinely
clean their feet and carry out continued care on their skin and nails. Nurses are however
supposed to evaluate specific requirements of individual patients and as a result design specified
educational programs to offer to the patient in question and to their families. They can
additionally induce family members of the patient to actively participate in the education
program for them to capture the essence of visiting the clinic regularly, taking blood tests at
regular intervals and how to prevent diabetes complications (Wells, 2015). The table below
outlines the basic diabetic foot care principles that are gained through nurse education to
patients.
Table 1: Basic principles of diabetic foot management
Daily examination of feet for swellings, discoloration of skin surface, cracks on the
Toenail fungus should be treated with immediate effect and is to be avoided by involving a foot
specialist in handling ingrown toenails. It is also worth noting that any form of tobacco that is
smokes results to damage of blood vessels located in the legs.
Observations have been made that in prevention of lower limb amputation and generally
foot ulcers resulting from diabetic conditions, nurses play an important and equally effective role
by running educational intervention programs, screening of people deemed to be at higher risks
and provision of health care. It is of great significance that all diabetic patients and more-so those
at higher risks of acquiring foot ulcers to familiarize themselves with the necessary basics of
good foot care. Research have shown that nurse-provided patient education relating to adequate
foot care has been an effective move on management of diabetic foot (Bulechek, Butcher,
Dochterman, & Wagner, 2013). Nurses can therefore offer teachings on how to conduct daily
feet examination and care. It is also a duty for nurses to encourage diabetic patients to routinely
clean their feet and carry out continued care on their skin and nails. Nurses are however
supposed to evaluate specific requirements of individual patients and as a result design specified
educational programs to offer to the patient in question and to their families. They can
additionally induce family members of the patient to actively participate in the education
program for them to capture the essence of visiting the clinic regularly, taking blood tests at
regular intervals and how to prevent diabetes complications (Wells, 2015). The table below
outlines the basic diabetic foot care principles that are gained through nurse education to
patients.
Table 1: Basic principles of diabetic foot management
Daily examination of feet for swellings, discoloration of skin surface, cracks on the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING MANAGEMENT OF DIABETIC FOOT 7
skin, numbness and pain.
Implementation of self-help techniques such as use of mirrors to aid in examination of
feet.
Maintaining proper foot hygiene by washing feet and then drying them properly more
so between the fingers on a daily basis.
Regulating the temperature of water to ensure its appropriate before dipping foot in for
washing.
To always wear socks before wearing shoes and to avoid walking bear footed.
To make choices of shoes that are fitting. Afternoon is the most appropriate time for
making purchases of shoes.
Fingernails are to be cut directly and regularly.
Foot lesions e.g. corn should not be manipulated at all costs.
Creams rich in moisture should be applied on dry surfaces to keep them moist but
exempting between the fingers.
Whenever they note any reduction in visual acuity, they should seek professional help.
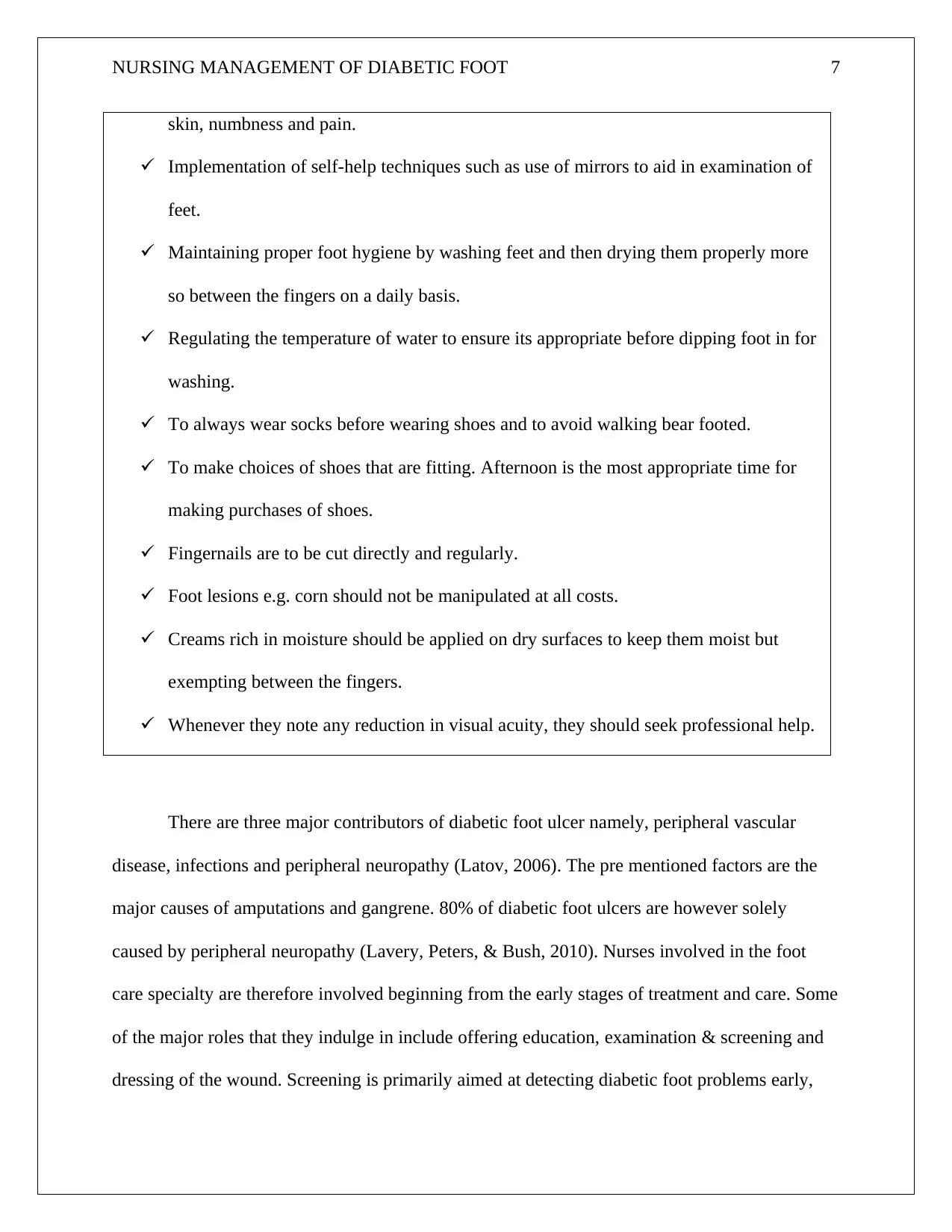
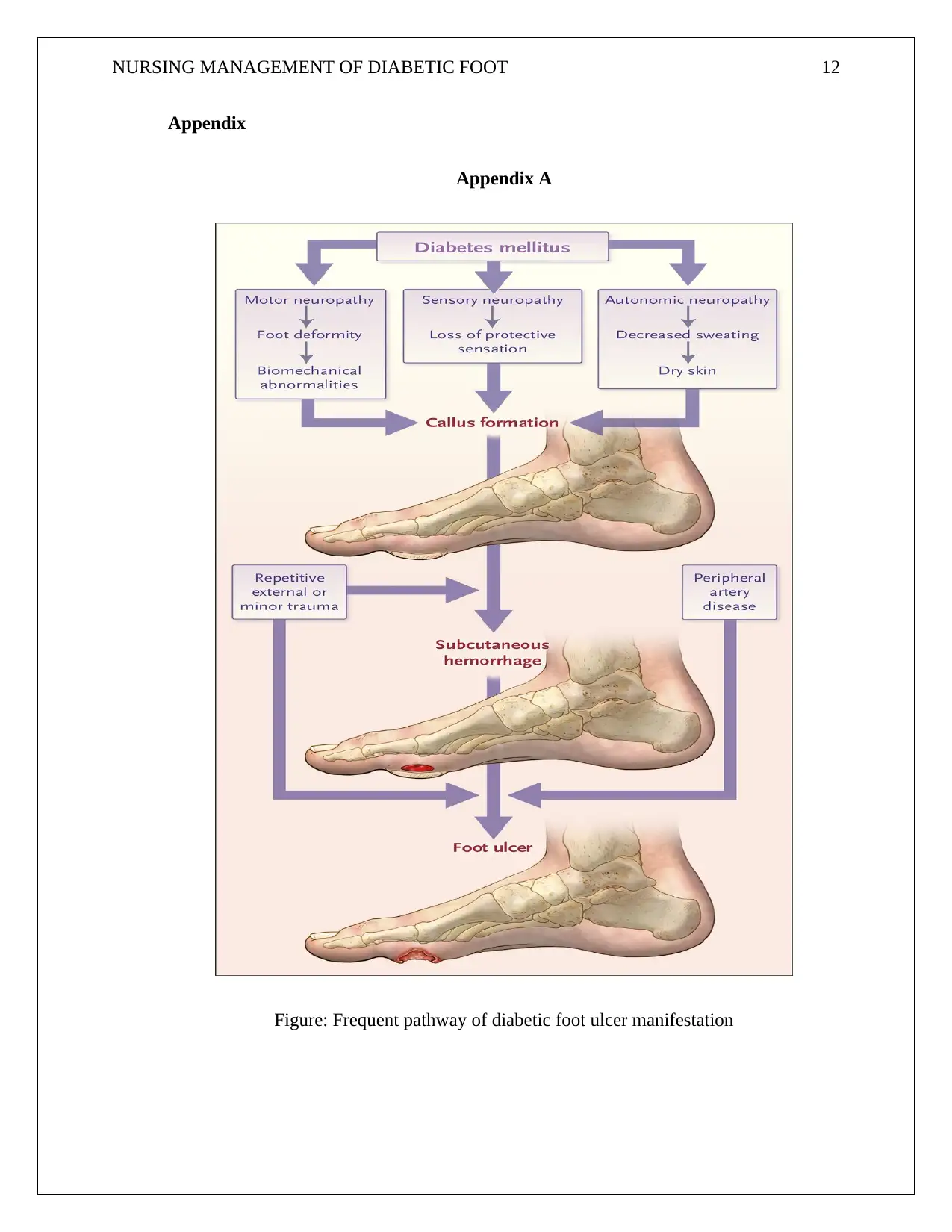
There are three major contributors of diabetic foot ulcer namely, peripheral vascular
disease, infections and peripheral neuropathy (Latov, 2006). The pre mentioned factors are the
major causes of amputations and gangrene. 80% of diabetic foot ulcers are however solely
caused by peripheral neuropathy (Lavery, Peters, & Bush, 2010). Nurses involved in the foot
care specialty are therefore involved beginning from the early stages of treatment and care. Some
of the major roles that they indulge in include offering education, examination & screening and
dressing of the wound. Screening is primarily aimed at detecting diabetic foot problems early,
skin, numbness and pain.
Implementation of self-help techniques such as use of mirrors to aid in examination of
feet.
Maintaining proper foot hygiene by washing feet and then drying them properly more
so between the fingers on a daily basis.
Regulating the temperature of water to ensure its appropriate before dipping foot in for
washing.
To always wear socks before wearing shoes and to avoid walking bear footed.
To make choices of shoes that are fitting. Afternoon is the most appropriate time for
making purchases of shoes.
Fingernails are to be cut directly and regularly.
Foot lesions e.g. corn should not be manipulated at all costs.
Creams rich in moisture should be applied on dry surfaces to keep them moist but
exempting between the fingers.
Whenever they note any reduction in visual acuity, they should seek professional help.
There are three major contributors of diabetic foot ulcer namely, peripheral vascular
disease, infections and peripheral neuropathy (Latov, 2006). The pre mentioned factors are the
major causes of amputations and gangrene. 80% of diabetic foot ulcers are however solely
caused by peripheral neuropathy (Lavery, Peters, & Bush, 2010). Nurses involved in the foot
care specialty are therefore involved beginning from the early stages of treatment and care. Some
of the major roles that they indulge in include offering education, examination & screening and
dressing of the wound. Screening is primarily aimed at detecting diabetic foot problems early,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING MANAGEMENT OF DIABETIC FOOT 8
identifying those at risk of suffering from foot ulcers and therefore reduce the overall number of
patients. The table below outlines the steps involved in dressing of a diabetic foot ulcer (Shai &
Maibach, 2004).
Table 2: Dressing of a diabetic foot ulcer.
i. Prepare a whirlpool bath and dip the foot in it.
ii. By use of a catheter and syringe, wash away the dead tissue that is in the ulcer.
iii. Apply wetness to a dry cotton wool and use it to remove dead tissue from the ulcer.
iv. Apply enzymes on the ulcer to help in dissolution of dead tissue found on the wound.
v. On the ulcer, apply special maggots that will eat away only the dead skin and
simultaneously produce substances that are of a chemical nature to aid in healing of the
culture.
vi. Dress the wound using a clean and treated bandage.
vii. The dressing should be changed at least twice per day.
From the above studies, it prevailed that change process was necessary in order to effect
appropriate care. The most significant change that ought to be implemented with immediate
effect was to offer additional education by means introducing short courses to nurses directly
involved in nursing care of patients with diabetic foot ulcers. Additionally, nurses should embark
on home to home visits for diabetic patients to educate them on the basic management practices
for diabetic foot. Home to home visits will prove more effective as the nurses involved will reach
out to majority of patients including those who previously never attended clinics.
identifying those at risk of suffering from foot ulcers and therefore reduce the overall number of
patients. The table below outlines the steps involved in dressing of a diabetic foot ulcer (Shai &
Maibach, 2004).
Table 2: Dressing of a diabetic foot ulcer.
i. Prepare a whirlpool bath and dip the foot in it.
ii. By use of a catheter and syringe, wash away the dead tissue that is in the ulcer.
iii. Apply wetness to a dry cotton wool and use it to remove dead tissue from the ulcer.
iv. Apply enzymes on the ulcer to help in dissolution of dead tissue found on the wound.
v. On the ulcer, apply special maggots that will eat away only the dead skin and
simultaneously produce substances that are of a chemical nature to aid in healing of the
culture.
vi. Dress the wound using a clean and treated bandage.
vii. The dressing should be changed at least twice per day.
From the above studies, it prevailed that change process was necessary in order to effect
appropriate care. The most significant change that ought to be implemented with immediate
effect was to offer additional education by means introducing short courses to nurses directly
involved in nursing care of patients with diabetic foot ulcers. Additionally, nurses should embark
on home to home visits for diabetic patients to educate them on the basic management practices
for diabetic foot. Home to home visits will prove more effective as the nurses involved will reach
out to majority of patients including those who previously never attended clinics.
NURSING MANAGEMENT OF DIABETIC FOOT 9
Conclusion
Diabetic foot which is the main trigger of hospitalization of diabetic patients has been identified
as a major concern in the health care systems. Individuals suffering from this disease frequently
develop diabetic neuropathy owing to numerous neurovascular and metabolic factors. Peripheral
neuropathy leads to loss of feeling or pain in the feet, legs, arms, and toes, and because of low
blood flow and distal nerve impairment. Sores and blisters appear on numb sections of the legs
and feet such as metatarso-phalangeal intersections, heel part and as a consequence injury or
pressure goes unobserved and finally become gateway of entry for infection and bacteria. In
addition to playing their role in public education, health care, management of health systems,
improvement of life quality and caring for patients, nurses who are members of the team
involved with diabetes care ought to fully attend specialized training. This will help them embark
on implementation of the latest instructions concerning diabetic foot care in a bid to enhance
effectiveness of their services in promotion of the health of diabetic patients. This therefore calls
for short term training courses to educate nurses on how enforce algorithms and clinical
guidelines for diabetic care in hospitals and clinics.
Conclusion
Diabetic foot which is the main trigger of hospitalization of diabetic patients has been identified
as a major concern in the health care systems. Individuals suffering from this disease frequently
develop diabetic neuropathy owing to numerous neurovascular and metabolic factors. Peripheral
neuropathy leads to loss of feeling or pain in the feet, legs, arms, and toes, and because of low
blood flow and distal nerve impairment. Sores and blisters appear on numb sections of the legs
and feet such as metatarso-phalangeal intersections, heel part and as a consequence injury or
pressure goes unobserved and finally become gateway of entry for infection and bacteria. In
addition to playing their role in public education, health care, management of health systems,
improvement of life quality and caring for patients, nurses who are members of the team
involved with diabetes care ought to fully attend specialized training. This will help them embark
on implementation of the latest instructions concerning diabetic foot care in a bid to enhance
effectiveness of their services in promotion of the health of diabetic patients. This therefore calls
for short term training courses to educate nurses on how enforce algorithms and clinical
guidelines for diabetic care in hospitals and clinics.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING MANAGEMENT OF DIABETIC FOOT 10
Bibliography
Benner, P. E. (2001). From Novice to Expert: Excellence and Power in Clinical Nursing
Practice. Prentice Hall.
Bulechek, G. M., Butcher, H. K., Dochterman, J. M., & Wagner, C. (2013). Nursing
Interventions Classification (NIC)6: Nursing Interventions Classification (NIC) (Revised
ed.). Elsevier Health Sciences.
DeLaune, S. C., Ladner, P. K., McTier, L., Tollefson, J., & Lawrence, J. (2016). Fundamentals
of Nursing: Australia & NZ (Revised ed.). Cengage AU.
Edmonds, M. E., Foster, A. M., & Sanders, L. (2008). A Practical Manual of Diabetic Foot Care
(2 ed.). John Wiley & Sons.
Fitzpatrick, J. J., & Wallace, M. (2006). Encyclopedia of Nursing Research. Springer Publishing
Company.
Holt, P. (2009). Diabetes in Hospital: A Practical Approach for Healthcare Professionals. John
Wiley & Sons.
Latov, N. (2006). Peripheral Neuropathy: When the Numbness, Weakness and Pain Won't Stop.
Demos Medical Publishing.
Lavery, L. A., Peters, E. J., & Bush, R. (2010). High Risk Diabetic Foot: Treatment and
Prevention (Illustrated ed.). CRC Press.
Masters, K. (2014). Nursing Theories: a Framework for Professional Practice. Jones & Bartlett
Publishers.
Bibliography
Benner, P. E. (2001). From Novice to Expert: Excellence and Power in Clinical Nursing
Practice. Prentice Hall.
Bulechek, G. M., Butcher, H. K., Dochterman, J. M., & Wagner, C. (2013). Nursing
Interventions Classification (NIC)6: Nursing Interventions Classification (NIC) (Revised
ed.). Elsevier Health Sciences.
DeLaune, S. C., Ladner, P. K., McTier, L., Tollefson, J., & Lawrence, J. (2016). Fundamentals
of Nursing: Australia & NZ (Revised ed.). Cengage AU.
Edmonds, M. E., Foster, A. M., & Sanders, L. (2008). A Practical Manual of Diabetic Foot Care
(2 ed.). John Wiley & Sons.
Fitzpatrick, J. J., & Wallace, M. (2006). Encyclopedia of Nursing Research. Springer Publishing
Company.
Holt, P. (2009). Diabetes in Hospital: A Practical Approach for Healthcare Professionals. John
Wiley & Sons.
Latov, N. (2006). Peripheral Neuropathy: When the Numbness, Weakness and Pain Won't Stop.
Demos Medical Publishing.
Lavery, L. A., Peters, E. J., & Bush, R. (2010). High Risk Diabetic Foot: Treatment and
Prevention (Illustrated ed.). CRC Press.
Masters, K. (2014). Nursing Theories: a Framework for Professional Practice. Jones & Bartlett
Publishers.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING MANAGEMENT OF DIABETIC FOOT 11
McDermott, A. (2016). Diabetes and amputation. healthline. Retrieved 06 07, 2018, from
https://www.healthline.com/health/diabetes/diabetes-amputation
Nather, A. (2008). Diabetic Foot Problems. World Scientific.
Ruhl, J. (2017). Blood Sugar 101: What They Don't Tell You About Diabetes (Vol. 1). Pronoun.
Shai, A., & Maibach, H. I. (2004). Wound Healing and Ulcers of the Skin: Diagnosis and
Therapy - The Practical Approach. Springer Science & Business Media.
Siviter, B. (2013). The Student Nurse Handbook3: The Student Nurse Handbook. Elsevier Health
Sciences.
Utley, R. (2010). Theory and Research for Academic Nurse Educators: Application to Practice.
Jones & Bartlett Learning.
Wells, C. (2015, September). Orchestrating Healing: a Grounded Theory of Registered Nurses
Caring for Patients with Diabetic Foot Ulcers. ResearchGate. Retrieved 06 07, 2018,
from
https://www.researchgate.net/publication/281971866_Orchestrating_Healing_a_Grounde
d_Theory_of_Registered_Nurses_Caring_for_Patients_with_Diabetic_Foot_Ulcers
WHO. (2016, 04 07). Diabetes: Global Report on Diabetes. Retrieved from World Health
Organisation: http://www.who.int/diabetes/global-report/en/
McDermott, A. (2016). Diabetes and amputation. healthline. Retrieved 06 07, 2018, from
https://www.healthline.com/health/diabetes/diabetes-amputation
Nather, A. (2008). Diabetic Foot Problems. World Scientific.
Ruhl, J. (2017). Blood Sugar 101: What They Don't Tell You About Diabetes (Vol. 1). Pronoun.
Shai, A., & Maibach, H. I. (2004). Wound Healing and Ulcers of the Skin: Diagnosis and
Therapy - The Practical Approach. Springer Science & Business Media.
Siviter, B. (2013). The Student Nurse Handbook3: The Student Nurse Handbook. Elsevier Health
Sciences.
Utley, R. (2010). Theory and Research for Academic Nurse Educators: Application to Practice.
Jones & Bartlett Learning.
Wells, C. (2015, September). Orchestrating Healing: a Grounded Theory of Registered Nurses
Caring for Patients with Diabetic Foot Ulcers. ResearchGate. Retrieved 06 07, 2018,
from
https://www.researchgate.net/publication/281971866_Orchestrating_Healing_a_Grounde
d_Theory_of_Registered_Nurses_Caring_for_Patients_with_Diabetic_Foot_Ulcers
WHO. (2016, 04 07). Diabetes: Global Report on Diabetes. Retrieved from World Health
Organisation: http://www.who.int/diabetes/global-report/en/
NURSING MANAGEMENT OF DIABETIC FOOT 12
Appendix
Appendix A
Figure: Frequent pathway of diabetic foot ulcer manifestation
Appendix
Appendix A
Figure: Frequent pathway of diabetic foot ulcer manifestation
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




