Clinical Governance and Practice Development: Chronic Back Pain Report
VerifiedAdded on 2023/01/06
|8
|1773
|95
Report
AI Summary
This report addresses the clinical problem of chronic back pain, a significant challenge in primary care, characterized by remissions and exacerbations that impact daily activities. The report highlights the clinical problem in nursing practice, emphasizing patient care through health screening and promotion of recovery. It formulates a clinical question using the PICOT format to structure the relevance of the topic for professional knowledge. The report discusses the transition from acute to chronic pain, its prevalence, and adverse psychological and physical outcomes. It emphasizes the importance of proper pain management and the role of nurses in a multidisciplinary team. The report also raises a clinical question about the effectiveness of exercise and physical activities in treating chronic back pain, comparing it with Acupressure, and concludes with the importance of further research.
Clinical Governance and Practice
Development
Development
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Table of Contents
Introduction......................................................................................................................................1
Potential clinical problem................................................................................................................1
Clinical Question.............................................................................................................................2
Conclusion.......................................................................................................................................3
REFERENCES................................................................................................................................4
Introduction......................................................................................................................................1
Potential clinical problem................................................................................................................1
Clinical Question.............................................................................................................................2
Conclusion.......................................................................................................................................3
REFERENCES................................................................................................................................4

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Introduction
Management of chronic back pain is one of the major challenges faced by primary care
physicians, in terms of accessing common treatment modalities of such patients. This problem
can be characterised by remissions, exacerbations and attacks that causes disability of individuals
in carrying out their routine work, especially when recurrence rate is high weeks (Alzahrani and
et. al., 2019). The present report is going to highlight clinical problem associated with chronic
back pain in nursing practice. It also emphasises on modalities of patient care in terms of
supporting and preventing them from such trauma, by health screening and different promotion
activities of recovery. For further investigation on the chosen topic, a question will be framed by
using PICOT format to structure relevance of it, for professional knowledge.
Potential clinical problem
At some stage of live, most of the people experience virtually bouts of low back pain, which
is classified as acute or chronic. Acute pain also known as postoperative pain, generally recover
easily after some rest, where healing takes place within 2 to 3 (Tarescavage, Scheman and Ben-
Porath, 2018). While chronic pain persists after a surgery or an injury whose sources are hard to
determine, but can be subdivided into non-malignant and cancer-related pain like low-back pain,
arthritis and peripheral neuropath. In other words, chronic pain defined as lower back pain which
remains lasts over 3 months and is usually severe for people who does not respond easily to
initial treatments, therefore, requires a thorough medical workup for determining exact source of
same. For a number of reasons, acute pain develops into the chronic pain, therefore, before
providing any treatment, it is essential for providers to determine the same through a medical
evaluation (Kim, Wu and Jang, 2020). The highest prevalence rate of related symptoms of this
pain refer to be most frequent medical complaints among people of age–group of 45 to 65 years.
Inadequately, managing such pain may lead to adverse psychological and physical patient
outcomes for patients individually. Continuous, reoccurrence and unrelieved pain results in
activating the pituitary-adrenal axis, which may suppress body’s immune system, postsurgical
infection as well as poor wound healing. Moreover, Sympathetic Nervous System (SNS)
activation negatively impact on various organs and functions of an individual, which includes
cardiovascular, renal systems, gastrointestinal, predisposing and more (Petzke and et. al., 2020).
1
Management of chronic back pain is one of the major challenges faced by primary care
physicians, in terms of accessing common treatment modalities of such patients. This problem
can be characterised by remissions, exacerbations and attacks that causes disability of individuals
in carrying out their routine work, especially when recurrence rate is high weeks (Alzahrani and
et. al., 2019). The present report is going to highlight clinical problem associated with chronic
back pain in nursing practice. It also emphasises on modalities of patient care in terms of
supporting and preventing them from such trauma, by health screening and different promotion
activities of recovery. For further investigation on the chosen topic, a question will be framed by
using PICOT format to structure relevance of it, for professional knowledge.
Potential clinical problem
At some stage of live, most of the people experience virtually bouts of low back pain, which
is classified as acute or chronic. Acute pain also known as postoperative pain, generally recover
easily after some rest, where healing takes place within 2 to 3 (Tarescavage, Scheman and Ben-
Porath, 2018). While chronic pain persists after a surgery or an injury whose sources are hard to
determine, but can be subdivided into non-malignant and cancer-related pain like low-back pain,
arthritis and peripheral neuropath. In other words, chronic pain defined as lower back pain which
remains lasts over 3 months and is usually severe for people who does not respond easily to
initial treatments, therefore, requires a thorough medical workup for determining exact source of
same. For a number of reasons, acute pain develops into the chronic pain, therefore, before
providing any treatment, it is essential for providers to determine the same through a medical
evaluation (Kim, Wu and Jang, 2020). The highest prevalence rate of related symptoms of this
pain refer to be most frequent medical complaints among people of age–group of 45 to 65 years.
Inadequately, managing such pain may lead to adverse psychological and physical patient
outcomes for patients individually. Continuous, reoccurrence and unrelieved pain results in
activating the pituitary-adrenal axis, which may suppress body’s immune system, postsurgical
infection as well as poor wound healing. Moreover, Sympathetic Nervous System (SNS)
activation negatively impact on various organs and functions of an individual, which includes
cardiovascular, renal systems, gastrointestinal, predisposing and more (Petzke and et. al., 2020).
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Therefore, of particular importance within nursing care, it has analysed that unrelieved pain
might reduce patient mobility, in terms of increasing complications like deep vein thrombosis,
pneumonia and pulmonary embolus (Malfliet and et. al. (2019). Along with this, post-surgical
complications of inadequate pain management also adversely affect the welfare of patients and
performance of healthcare organisations, due to extend in lengths of stay and readmissions, that
both results in increasing the cost of care.
The human back usually composed of a complex structure of bones, muscles, ligaments,
disks and tendons, that work together for supporting the body and enable to move around.
Therefore, if problem occurs in functioning of any of these components leads to cause back pain
either acute of chronic, where in some cases, cause of occurrence remains unclear (Almeida and
et. al., 2018). In this regard, poorly managing the chronic pain may put clinicians higher at risk
for legal action. Standards for pain management, outlined by Department of Health and Health
Administration Regulation 2005), require that chronic situations need to be promptly addressed
and managed by clinicians at priority. Having standards of care aid to increases risk related to
legal actions, if not done properly against clinicians and healthcare institutions (Volpato and et.
al., 2020). Nurses, being a part of multi-disciplinary team are responsible for managing pain of
patients during hospitalization, so, they are also liable for legal action. For this purpose, physical
activities and few exercises are generally recommended by physicians to patients with chronic
back pain. Through engagement of patients in fitness activities and exercise, physicians can
easily support patients to heal their pains and overcome from the same (Yarznbowicz and et. al.
(2018).
Clinical Question
Analysing the symptoms and factors that turns acute low back pain into chronic, arise a
question that whether engagement in physical activities help people to get over from chronic
pain. Because in most of the cases when SNS activates in body then it would difficult for people
to respond easily or do their normal routine work (Hasenbring, Fehrmann and Ebenbichler,
2020). Further, it also makes difficult for an individual to carry out physical movement and other
activities. So, not all exercises prove beneficial, where any mild discomfort may lead to increase
pain in muscles and other components of human nervous system. It is not essential that all
physical exercises result in relief of muscle pain. So this situation, give rise to a question that
what are the major clinical practices that should be implement for the individuals of 18 years and
2
might reduce patient mobility, in terms of increasing complications like deep vein thrombosis,
pneumonia and pulmonary embolus (Malfliet and et. al. (2019). Along with this, post-surgical
complications of inadequate pain management also adversely affect the welfare of patients and
performance of healthcare organisations, due to extend in lengths of stay and readmissions, that
both results in increasing the cost of care.
The human back usually composed of a complex structure of bones, muscles, ligaments,
disks and tendons, that work together for supporting the body and enable to move around.
Therefore, if problem occurs in functioning of any of these components leads to cause back pain
either acute of chronic, where in some cases, cause of occurrence remains unclear (Almeida and
et. al., 2018). In this regard, poorly managing the chronic pain may put clinicians higher at risk
for legal action. Standards for pain management, outlined by Department of Health and Health
Administration Regulation 2005), require that chronic situations need to be promptly addressed
and managed by clinicians at priority. Having standards of care aid to increases risk related to
legal actions, if not done properly against clinicians and healthcare institutions (Volpato and et.
al., 2020). Nurses, being a part of multi-disciplinary team are responsible for managing pain of
patients during hospitalization, so, they are also liable for legal action. For this purpose, physical
activities and few exercises are generally recommended by physicians to patients with chronic
back pain. Through engagement of patients in fitness activities and exercise, physicians can
easily support patients to heal their pains and overcome from the same (Yarznbowicz and et. al.
(2018).
Clinical Question
Analysing the symptoms and factors that turns acute low back pain into chronic, arise a
question that whether engagement in physical activities help people to get over from chronic
pain. Because in most of the cases when SNS activates in body then it would difficult for people
to respond easily or do their normal routine work (Hasenbring, Fehrmann and Ebenbichler,
2020). Further, it also makes difficult for an individual to carry out physical movement and other
activities. So, not all exercises prove beneficial, where any mild discomfort may lead to increase
pain in muscles and other components of human nervous system. It is not essential that all
physical exercises result in relief of muscle pain. So this situation, give rise to a question that
what are the major clinical practices that should be implement for the individuals of 18 years and
2
above so they can deal with the chronic pain (Bussières and et. al., 2018). Therefore, a clinical
question is arisen below on which further investigation will be carried out, to reach desired
outcomes.
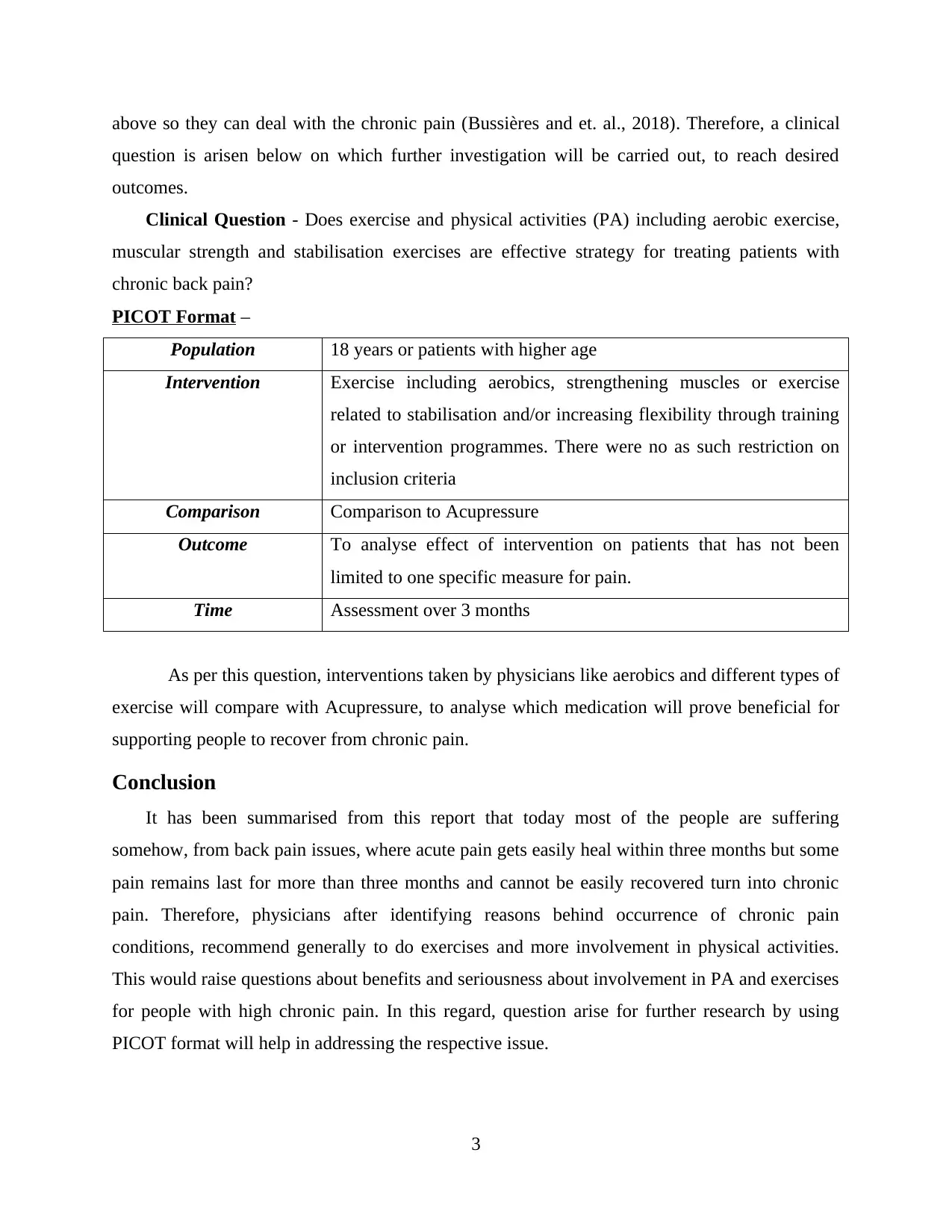
Clinical Question - Does exercise and physical activities (PA) including aerobic exercise,
muscular strength and stabilisation exercises are effective strategy for treating patients with
chronic back pain?
PICOT Format –
Population 18 years or patients with higher age
Intervention Exercise including aerobics, strengthening muscles or exercise
related to stabilisation and/or increasing flexibility through training
or intervention programmes. There were no as such restriction on
inclusion criteria
Comparison Comparison to Acupressure
Outcome To analyse effect of intervention on patients that has not been
limited to one specific measure for pain.
Time Assessment over 3 months
As per this question, interventions taken by physicians like aerobics and different types of
exercise will compare with Acupressure, to analyse which medication will prove beneficial for
supporting people to recover from chronic pain.
Conclusion
It has been summarised from this report that today most of the people are suffering
somehow, from back pain issues, where acute pain gets easily heal within three months but some
pain remains last for more than three months and cannot be easily recovered turn into chronic
pain. Therefore, physicians after identifying reasons behind occurrence of chronic pain
conditions, recommend generally to do exercises and more involvement in physical activities.
This would raise questions about benefits and seriousness about involvement in PA and exercises
for people with high chronic pain. In this regard, question arise for further research by using
PICOT format will help in addressing the respective issue.
3
question is arisen below on which further investigation will be carried out, to reach desired
outcomes.
Clinical Question - Does exercise and physical activities (PA) including aerobic exercise,
muscular strength and stabilisation exercises are effective strategy for treating patients with
chronic back pain?
PICOT Format –
Population 18 years or patients with higher age
Intervention Exercise including aerobics, strengthening muscles or exercise
related to stabilisation and/or increasing flexibility through training
or intervention programmes. There were no as such restriction on
inclusion criteria
Comparison Comparison to Acupressure
Outcome To analyse effect of intervention on patients that has not been
limited to one specific measure for pain.
Time Assessment over 3 months
As per this question, interventions taken by physicians like aerobics and different types of
exercise will compare with Acupressure, to analyse which medication will prove beneficial for
supporting people to recover from chronic pain.
Conclusion
It has been summarised from this report that today most of the people are suffering
somehow, from back pain issues, where acute pain gets easily heal within three months but some
pain remains last for more than three months and cannot be easily recovered turn into chronic
pain. Therefore, physicians after identifying reasons behind occurrence of chronic pain
conditions, recommend generally to do exercises and more involvement in physical activities.
This would raise questions about benefits and seriousness about involvement in PA and exercises
for people with high chronic pain. In this regard, question arise for further research by using
PICOT format will help in addressing the respective issue.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals
Almeida, M., & et. al. (2018). Primary care management of non‐specific low back pain: key
messages from recent clinical guidelines. Medical Journal of Australia. 208(6). 272-275.
Alzahrani, H., & et. al. (2019). Physical activity and chronic back conditions: a population-based
pooled study of 60,134 adults. Journal of sport and health science. 8(4). 386-393.
Bussières, A. E., & et. al. (2018). Spinal manipulative therapy and other conservative treatments
for low back pain: a guideline from the Canadian chiropractic guideline
initiative. Journal of manipulative and physiological therapeutics. 41(4). 265-293.
Hasenbring, M. I., Fehrmann, E., & Ebenbichler, G. (2020). Embodied Pain: There is a Need to
Reflect Interactions Between Cognitions, Behavior, and Neuromuscular Activity in
Chronic Pain. The Clinical Journal of Pain. 36(3). 178-180.
Kim, H. S., Wu, P. H., & Jang, I. T. (2020). Lumbar degenerative disease part 1: Anatomy and
pathophysiology of intervertebral discogenic pain and radiofrequency ablation of
basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A
prospective case series and review of literature. International Journal of Molecular
Sciences. 21(4). 1483.
Malfliet, A. & et. al. (2019). Best evidence rehabilitation for chronic pain part 3: Low back
pain. Journal of clinical medicine. 8(7). 1063.
Petzke, F., & et. al. (2020). Opioids for chronic low back pain: An updated systematic review
and meta‐analysis of efficacy, tolerability and safety in randomized placebo‐controlled
studies of at least 4 weeks of double‐blind duration. European Journal of Pain. 24(3).
497-517.
Tarescavage, A. M., Scheman, J., & Ben-Porath, Y. S. (2018). Prospective comparison of the
Minnesota Multiphasic Personality Inventory-2 (MMPI-2) and MMPI-2-Restructured
Form (MMPI-2-RF) in predicting treatment outcomes among patients with chronic low
back pain. Journal of clinical psychology in medical settings. 25(1). 66-79.
Volpato, M. P., & et. al. (2020). Single Cupping Thearpy Session Improves Pain, Sleep, and
Disability in Patients with Nonspecific Chronic Low Back Pain. Journal of acupuncture
and meridian studies. 13(2). 48-52.
Yarznbowicz, R., & et. al. (2018). Pain pattern classification and directional preference are
associated with clinical outcomes for patients with low back pain. Journal of Manual &
Manipulative Therapy. 26(1). 18-24.
4
Books and Journals
Almeida, M., & et. al. (2018). Primary care management of non‐specific low back pain: key
messages from recent clinical guidelines. Medical Journal of Australia. 208(6). 272-275.
Alzahrani, H., & et. al. (2019). Physical activity and chronic back conditions: a population-based
pooled study of 60,134 adults. Journal of sport and health science. 8(4). 386-393.
Bussières, A. E., & et. al. (2018). Spinal manipulative therapy and other conservative treatments
for low back pain: a guideline from the Canadian chiropractic guideline
initiative. Journal of manipulative and physiological therapeutics. 41(4). 265-293.
Hasenbring, M. I., Fehrmann, E., & Ebenbichler, G. (2020). Embodied Pain: There is a Need to
Reflect Interactions Between Cognitions, Behavior, and Neuromuscular Activity in
Chronic Pain. The Clinical Journal of Pain. 36(3). 178-180.
Kim, H. S., Wu, P. H., & Jang, I. T. (2020). Lumbar degenerative disease part 1: Anatomy and
pathophysiology of intervertebral discogenic pain and radiofrequency ablation of
basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A
prospective case series and review of literature. International Journal of Molecular
Sciences. 21(4). 1483.
Malfliet, A. & et. al. (2019). Best evidence rehabilitation for chronic pain part 3: Low back
pain. Journal of clinical medicine. 8(7). 1063.
Petzke, F., & et. al. (2020). Opioids for chronic low back pain: An updated systematic review
and meta‐analysis of efficacy, tolerability and safety in randomized placebo‐controlled
studies of at least 4 weeks of double‐blind duration. European Journal of Pain. 24(3).
497-517.
Tarescavage, A. M., Scheman, J., & Ben-Porath, Y. S. (2018). Prospective comparison of the
Minnesota Multiphasic Personality Inventory-2 (MMPI-2) and MMPI-2-Restructured
Form (MMPI-2-RF) in predicting treatment outcomes among patients with chronic low
back pain. Journal of clinical psychology in medical settings. 25(1). 66-79.
Volpato, M. P., & et. al. (2020). Single Cupping Thearpy Session Improves Pain, Sleep, and
Disability in Patients with Nonspecific Chronic Low Back Pain. Journal of acupuncture
and meridian studies. 13(2). 48-52.
Yarznbowicz, R., & et. al. (2018). Pain pattern classification and directional preference are
associated with clinical outcomes for patients with low back pain. Journal of Manual &
Manipulative Therapy. 26(1). 18-24.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

5
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





