Improving Healthcare: A Clinical Excellence and Safety Report
VerifiedAdded on 2023/06/05
|10
|2359
|311
Report
AI Summary
This report analyzes a personal experience of a patient fall incident using the Fishbone Model and the London Protocol to identify risk factors and improve the safety and quality of care under clinical governance frameworks. The case study involves an elderly Aboriginal patient with dementia who suffered a broken radial bone due to a fall in the emergency department. The analysis reveals failures in previous healthcare encounters, including inadequate risk assessment, lack of patient and family education, and ineffective communication. The report emphasizes the importance of consumer participation, clinical effectiveness, effective workforce, and risk management to prevent future incidents and ensure quality care. It highlights the need for a multidisciplinary approach, thorough assessment of environmental and physiological risks, and implementation of strategies to improve patient balance, gait, and memory.

Running head: PROMOTING CLINICAL EXCELLENCE
Promoting Clinical Excellence
Name of the Student
Name of the University
Author Note
Promoting Clinical Excellence
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PROMOTING CLINICAL EXCELLENCE
Introduction:
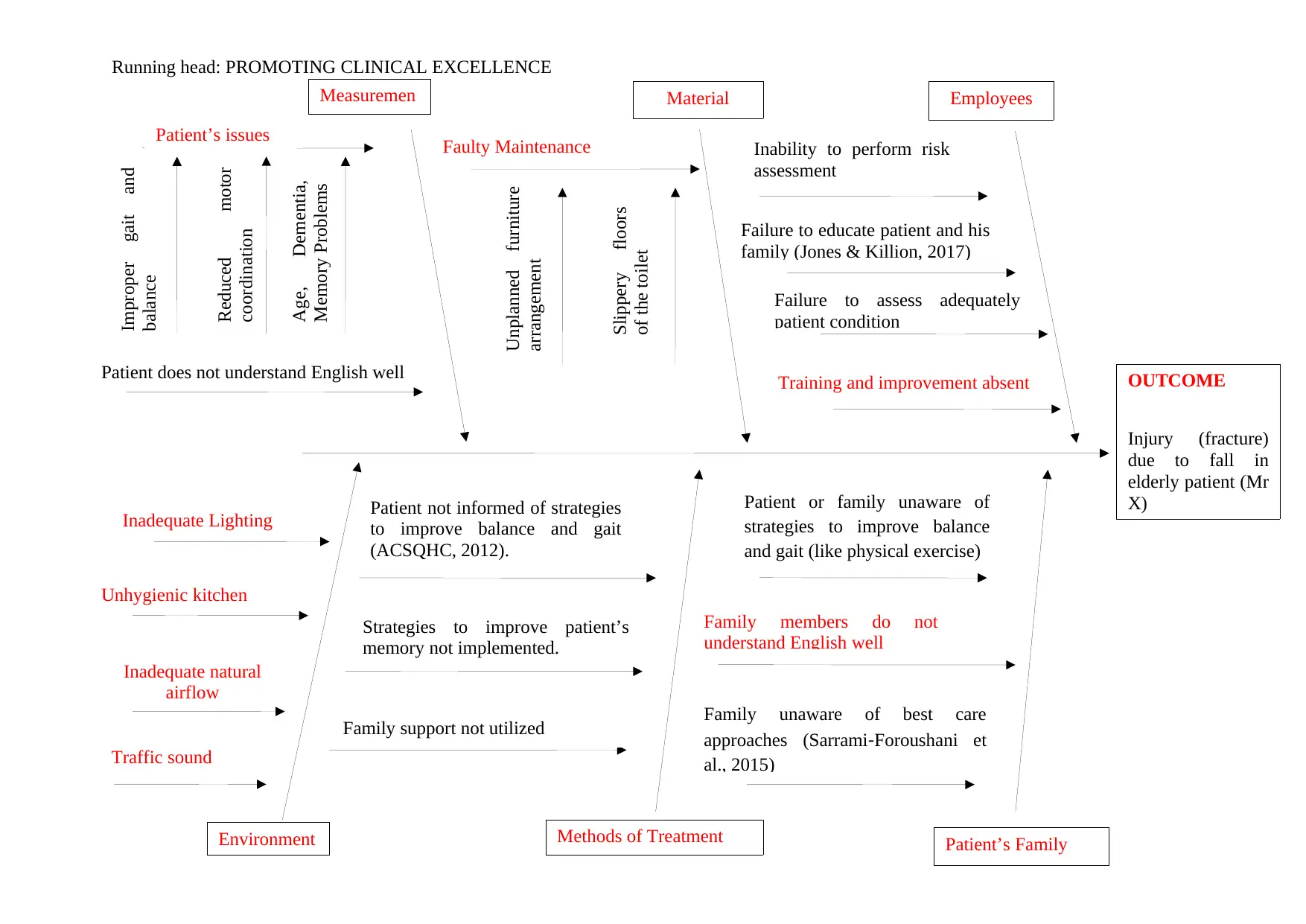
The aim of this study is to analyze a personal experience (Using the Fishbone Model)
of an incident caused due to failure in the delivery of appropriate and safe care for a patient
resulting in an accident (Luo et al., 2018). The case study would be analyzed following the
London Protocol and outline the information related to the experience and event according to
what happened, individuals who were involved, when the incident occurred, severity of the
potential or actual harm, possibility of recurrence and the consequences of the event (Lamba
et al., 2014). The risk factors are then analyzed using the Fishbone model to identify how the
safety and quality of care can be improved under clinical governance frameworks (Currie et
al., 2017).
Case Study:
The incident took place when I was working as a trainee in the emergency
department, when an elderly male patient (Ethnicity: Aboriginal), aged 80 years old (Mr X)
presented with a case of accidental injury due to a fall and resulted in a broken radial bone on
the right hand. The patient was suffering from Dementia, and is mobility and gait was
affected due to his condition. Mr X was given a rolling walker to aid his balance and gait,
however, he forgot to take the walker with him while going to the toilet, slipped and fell. He
broke his right radial bone while trying to break his fall and it hit the basin. Mr X was in a lot
of pain when he arrived and was promptly given sedatives. After talking to the family of Mr
X (his wife and daughter), it was found that the walker was given to him a month ago, after
he fell while getting out of the bed and hurt his head and that a risk assessment of the
patient’s house was not performed to identify and address the fall hazards. Further assessment
of the patient revealed that his motor reflexes are poor leading to improper hand to eye
coordination, which increased his risks of falling. The incident occurred in the morning that
Introduction:
The aim of this study is to analyze a personal experience (Using the Fishbone Model)
of an incident caused due to failure in the delivery of appropriate and safe care for a patient
resulting in an accident (Luo et al., 2018). The case study would be analyzed following the
London Protocol and outline the information related to the experience and event according to
what happened, individuals who were involved, when the incident occurred, severity of the
potential or actual harm, possibility of recurrence and the consequences of the event (Lamba
et al., 2014). The risk factors are then analyzed using the Fishbone model to identify how the
safety and quality of care can be improved under clinical governance frameworks (Currie et
al., 2017).
Case Study:
The incident took place when I was working as a trainee in the emergency
department, when an elderly male patient (Ethnicity: Aboriginal), aged 80 years old (Mr X)
presented with a case of accidental injury due to a fall and resulted in a broken radial bone on
the right hand. The patient was suffering from Dementia, and is mobility and gait was
affected due to his condition. Mr X was given a rolling walker to aid his balance and gait,
however, he forgot to take the walker with him while going to the toilet, slipped and fell. He
broke his right radial bone while trying to break his fall and it hit the basin. Mr X was in a lot
of pain when he arrived and was promptly given sedatives. After talking to the family of Mr
X (his wife and daughter), it was found that the walker was given to him a month ago, after
he fell while getting out of the bed and hurt his head and that a risk assessment of the
patient’s house was not performed to identify and address the fall hazards. Further assessment
of the patient revealed that his motor reflexes are poor leading to improper hand to eye
coordination, which increased his risks of falling. The incident occurred in the morning that
2PROMOTING CLINICAL EXCELLENCE
day, when the patient was conducting his activities of daily living. The fall occurred because
the patient was unable to balance himself and the floor of the toilet was slippery. With the
type of fall the patient took, it could be understood that under the given conditions, the fall
could have had serious and even fatal consequences. Moreover, due to his condition and the
patient is still at high risks of falling with the possibility of even more serious outcomes. This
shows a failure of the healthcare organization in the providence of safe and quality care for
the patient in the previous health encounter (Taylor et al., 2017).
day, when the patient was conducting his activities of daily living. The fall occurred because
the patient was unable to balance himself and the floor of the toilet was slippery. With the
type of fall the patient took, it could be understood that under the given conditions, the fall
could have had serious and even fatal consequences. Moreover, due to his condition and the
patient is still at high risks of falling with the possibility of even more serious outcomes. This
shows a failure of the healthcare organization in the providence of safe and quality care for
the patient in the previous health encounter (Taylor et al., 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Running head: PROMOTING CLINICAL EXCELLENCE
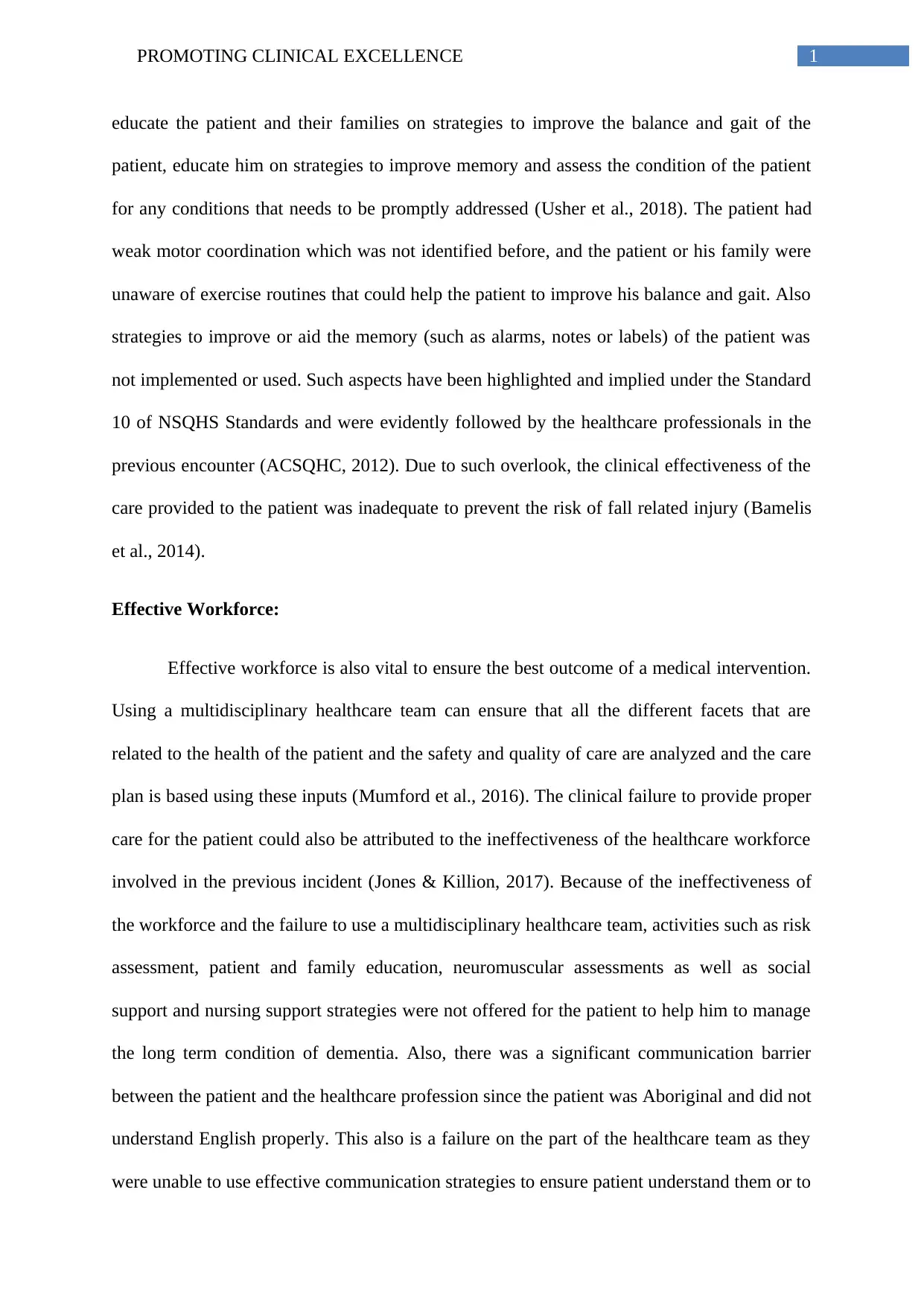
OUTCOME
Injury (fracture)
due to fall in
elderly patient (Mr
X)
EmployeesMaterialMeasuremen
t
Inadequate Lighting
Patient’s FamilyMethods of TreatmentEnvironment
Improper gait and
balance
Patient does not understand English well
Patient not informed of strategies
to improve balance and gait
(ACSQHC, 2012).
Age, Dementia,
Memory Problems
Reduced motor
coordination
Patient’s issues Faulty Maintenance
Slippery floors
of the toilet
Unplanned furniture
arrangement
Unhygienic kitchen
Strategies to improve patient’s
memory not implemented.
Family support not utilized
Inadequate natural
airflow
Inability to perform risk
assessment
Failure to educate patient and his
family (Jones & Killion, 2017)
Failure to assess adequately
patient condition
Patient or family unaware of
strategies to improve balance
and gait (like physical exercise)
Family unaware of best care
approaches (Sarrami‐Foroushani et
al., 2015)
Family members do not
understand English well
Traffic sound
Training and improvement absent
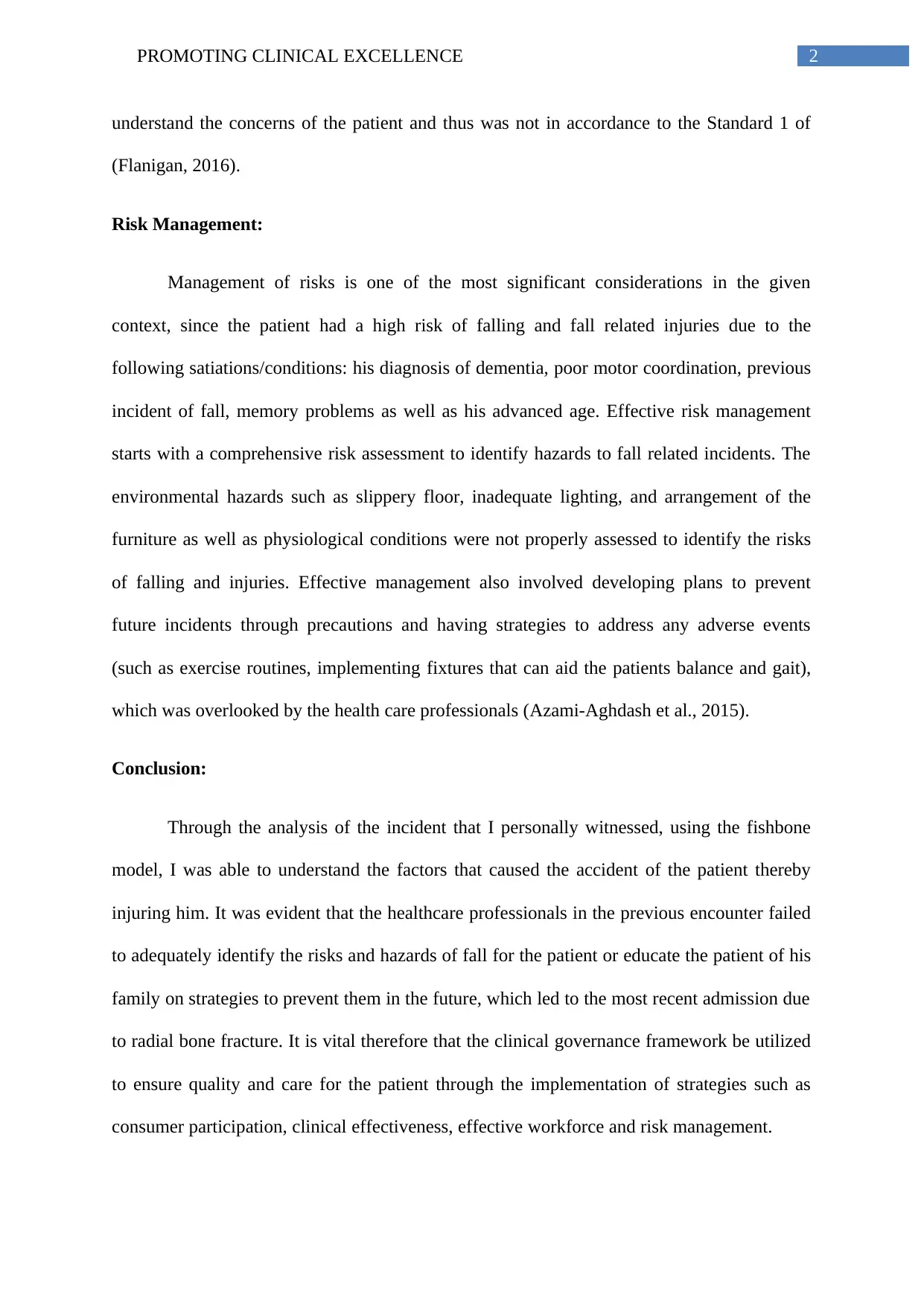
OUTCOME
Injury (fracture)
due to fall in
elderly patient (Mr
X)
EmployeesMaterialMeasuremen
t
Inadequate Lighting
Patient’s FamilyMethods of TreatmentEnvironment
Improper gait and
balance
Patient does not understand English well
Patient not informed of strategies
to improve balance and gait
(ACSQHC, 2012).
Age, Dementia,
Memory Problems
Reduced motor
coordination
Patient’s issues Faulty Maintenance
Slippery floors
of the toilet
Unplanned furniture
arrangement
Unhygienic kitchen
Strategies to improve patient’s
memory not implemented.
Family support not utilized
Inadequate natural
airflow
Inability to perform risk
assessment
Failure to educate patient and his
family (Jones & Killion, 2017)
Failure to assess adequately
patient condition
Patient or family unaware of
strategies to improve balance
and gait (like physical exercise)
Family unaware of best care
approaches (Sarrami‐Foroushani et
al., 2015)
Family members do not
understand English well
Traffic sound
Training and improvement absent
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Running head: PROMOTING CLINICAL EXCELLENCE
Using the clinical Governance Framework to improve the quality and safety of care for
the patient:
Consumer Participation:
The importance of the participation of the consumer (or patients and their families) in
the planning and implementation of a safe and quality care has been implemented by the
Australian Comission on Safety and Quality in Healthcare (Standard 2) and the principle of
patient centered care followed by healthcare organizations in Australia (Australian
Commission on Safety and Quality in Health Care, 2012). This framework supports the
importance of the views, opinions and preferences of the patient and their families in the care
delivery strategy and develops a care. Involving patients and their families in the care
planning and also helps to improve communication and better sharing of information. In the
given scenario, the nurses and healthcare professionals from the previous health incident did
not assess the preferences of the patient or their family and also failed to inform the family of
the best practices to care for the patient or did not share important information such as
strategies to improve gait and balance and support memory. This also shows a failure to
develop a therapeutic relation with the patient. This significantly increased the risks of a
recurrence of fall related injury leading up to the recent admission that I witnessed. Thus it
was necessary to involve the patient and his family to ensure the health and wellbeing of the
patient (Sarrami‐Foroushani et al., 2015).
Clinical Effectiveness:
A lack of clinical effectiveness was caused because of the failure of the previous
healthcare professionals who was involved in the previous health encounter to perform a
thorough assessment of the patient’s home for any fall related hazards to identify any risks
and mitigate them accordingly. The healthcare professionals also overlooked the necessity to
Using the clinical Governance Framework to improve the quality and safety of care for
the patient:
Consumer Participation:
The importance of the participation of the consumer (or patients and their families) in
the planning and implementation of a safe and quality care has been implemented by the
Australian Comission on Safety and Quality in Healthcare (Standard 2) and the principle of
patient centered care followed by healthcare organizations in Australia (Australian
Commission on Safety and Quality in Health Care, 2012). This framework supports the
importance of the views, opinions and preferences of the patient and their families in the care
delivery strategy and develops a care. Involving patients and their families in the care
planning and also helps to improve communication and better sharing of information. In the
given scenario, the nurses and healthcare professionals from the previous health incident did
not assess the preferences of the patient or their family and also failed to inform the family of
the best practices to care for the patient or did not share important information such as
strategies to improve gait and balance and support memory. This also shows a failure to
develop a therapeutic relation with the patient. This significantly increased the risks of a
recurrence of fall related injury leading up to the recent admission that I witnessed. Thus it
was necessary to involve the patient and his family to ensure the health and wellbeing of the
patient (Sarrami‐Foroushani et al., 2015).
Clinical Effectiveness:
A lack of clinical effectiveness was caused because of the failure of the previous
healthcare professionals who was involved in the previous health encounter to perform a
thorough assessment of the patient’s home for any fall related hazards to identify any risks
and mitigate them accordingly. The healthcare professionals also overlooked the necessity to
1PROMOTING CLINICAL EXCELLENCE
educate the patient and their families on strategies to improve the balance and gait of the
patient, educate him on strategies to improve memory and assess the condition of the patient
for any conditions that needs to be promptly addressed (Usher et al., 2018). The patient had
weak motor coordination which was not identified before, and the patient or his family were
unaware of exercise routines that could help the patient to improve his balance and gait. Also
strategies to improve or aid the memory (such as alarms, notes or labels) of the patient was
not implemented or used. Such aspects have been highlighted and implied under the Standard
10 of NSQHS Standards and were evidently followed by the healthcare professionals in the
previous encounter (ACSQHC, 2012). Due to such overlook, the clinical effectiveness of the
care provided to the patient was inadequate to prevent the risk of fall related injury (Bamelis
et al., 2014).
Effective Workforce:
Effective workforce is also vital to ensure the best outcome of a medical intervention.
Using a multidisciplinary healthcare team can ensure that all the different facets that are
related to the health of the patient and the safety and quality of care are analyzed and the care
plan is based using these inputs (Mumford et al., 2016). The clinical failure to provide proper
care for the patient could also be attributed to the ineffectiveness of the healthcare workforce
involved in the previous incident (Jones & Killion, 2017). Because of the ineffectiveness of
the workforce and the failure to use a multidisciplinary healthcare team, activities such as risk
assessment, patient and family education, neuromuscular assessments as well as social
support and nursing support strategies were not offered for the patient to help him to manage
the long term condition of dementia. Also, there was a significant communication barrier
between the patient and the healthcare profession since the patient was Aboriginal and did not
understand English properly. This also is a failure on the part of the healthcare team as they
were unable to use effective communication strategies to ensure patient understand them or to
educate the patient and their families on strategies to improve the balance and gait of the
patient, educate him on strategies to improve memory and assess the condition of the patient
for any conditions that needs to be promptly addressed (Usher et al., 2018). The patient had
weak motor coordination which was not identified before, and the patient or his family were
unaware of exercise routines that could help the patient to improve his balance and gait. Also
strategies to improve or aid the memory (such as alarms, notes or labels) of the patient was
not implemented or used. Such aspects have been highlighted and implied under the Standard
10 of NSQHS Standards and were evidently followed by the healthcare professionals in the
previous encounter (ACSQHC, 2012). Due to such overlook, the clinical effectiveness of the
care provided to the patient was inadequate to prevent the risk of fall related injury (Bamelis
et al., 2014).
Effective Workforce:
Effective workforce is also vital to ensure the best outcome of a medical intervention.
Using a multidisciplinary healthcare team can ensure that all the different facets that are
related to the health of the patient and the safety and quality of care are analyzed and the care
plan is based using these inputs (Mumford et al., 2016). The clinical failure to provide proper
care for the patient could also be attributed to the ineffectiveness of the healthcare workforce
involved in the previous incident (Jones & Killion, 2017). Because of the ineffectiveness of
the workforce and the failure to use a multidisciplinary healthcare team, activities such as risk
assessment, patient and family education, neuromuscular assessments as well as social
support and nursing support strategies were not offered for the patient to help him to manage
the long term condition of dementia. Also, there was a significant communication barrier
between the patient and the healthcare profession since the patient was Aboriginal and did not
understand English properly. This also is a failure on the part of the healthcare team as they
were unable to use effective communication strategies to ensure patient understand them or to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2PROMOTING CLINICAL EXCELLENCE
understand the concerns of the patient and thus was not in accordance to the Standard 1 of
(Flanigan, 2016).
Risk Management:
Management of risks is one of the most significant considerations in the given
context, since the patient had a high risk of falling and fall related injuries due to the
following satiations/conditions: his diagnosis of dementia, poor motor coordination, previous
incident of fall, memory problems as well as his advanced age. Effective risk management
starts with a comprehensive risk assessment to identify hazards to fall related incidents. The
environmental hazards such as slippery floor, inadequate lighting, and arrangement of the
furniture as well as physiological conditions were not properly assessed to identify the risks
of falling and injuries. Effective management also involved developing plans to prevent
future incidents through precautions and having strategies to address any adverse events
(such as exercise routines, implementing fixtures that can aid the patients balance and gait),
which was overlooked by the health care professionals (Azami-Aghdash et al., 2015).
Conclusion:
Through the analysis of the incident that I personally witnessed, using the fishbone
model, I was able to understand the factors that caused the accident of the patient thereby
injuring him. It was evident that the healthcare professionals in the previous encounter failed
to adequately identify the risks and hazards of fall for the patient or educate the patient of his
family on strategies to prevent them in the future, which led to the most recent admission due
to radial bone fracture. It is vital therefore that the clinical governance framework be utilized
to ensure quality and care for the patient through the implementation of strategies such as
consumer participation, clinical effectiveness, effective workforce and risk management.
understand the concerns of the patient and thus was not in accordance to the Standard 1 of
(Flanigan, 2016).
Risk Management:
Management of risks is one of the most significant considerations in the given
context, since the patient had a high risk of falling and fall related injuries due to the
following satiations/conditions: his diagnosis of dementia, poor motor coordination, previous
incident of fall, memory problems as well as his advanced age. Effective risk management
starts with a comprehensive risk assessment to identify hazards to fall related incidents. The
environmental hazards such as slippery floor, inadequate lighting, and arrangement of the
furniture as well as physiological conditions were not properly assessed to identify the risks
of falling and injuries. Effective management also involved developing plans to prevent
future incidents through precautions and having strategies to address any adverse events
(such as exercise routines, implementing fixtures that can aid the patients balance and gait),
which was overlooked by the health care professionals (Azami-Aghdash et al., 2015).
Conclusion:
Through the analysis of the incident that I personally witnessed, using the fishbone
model, I was able to understand the factors that caused the accident of the patient thereby
injuring him. It was evident that the healthcare professionals in the previous encounter failed
to adequately identify the risks and hazards of fall for the patient or educate the patient of his
family on strategies to prevent them in the future, which led to the most recent admission due
to radial bone fracture. It is vital therefore that the clinical governance framework be utilized
to ensure quality and care for the patient through the implementation of strategies such as
consumer participation, clinical effectiveness, effective workforce and risk management.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
3PROMOTING CLINICAL EXCELLENCE
References:
Australian Commission on Safety and Quality in Health Care. (2012). National safety and
quality health service standards. Australian Commission on Safety and Quality in
Health Care.Retrieved from:
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-
Standards-Sept-2012.pdf
Azami-Aghdash, S., Tabrizi, J. S., Sadeghi-Bazargani, H., Hajebrahimi, S., & Naghavi-
Behzad, M. (2015). Developing performance indicators for clinical governance in
dimensions of risk management and clinical effectiveness. International Journal for
Quality in Health Care, 27(2), 110-116. DOI: https://doi.org/10.1093/intqhc/mzu102
Bamelis, L. L., Evers, S. M., Spinhoven, P., & Arntz, A. (2014). Results of a multicenter
randomized controlled trial of the clinical effectiveness of schema therapy for
personality disorders. American Journal of Psychiatry, 171(3), 305-322. DOI:
https://doi.org/10.1176/appi.ajp.2013.12040518
Currie, J., Mateer, J., Weston, D., Anderson, E., & Harding, J. (2017). Implementation of a
clinical governance framework to 17 combat service support brigade, Australian
army. International Journal of Health Governance, 22(1), 15-24. DOI:
https://doi.org/10.1108/IJHG-04-2016-0024
Flanigan, K. (2016). NSQHS standard-patient identification. ACORN: The Journal of
Perioperative Nursing in Australia, 29(1), 23. Retieved from:
https://search.informit.com.au/documentSummary;dn=883877754554045;res=IELHE
A
References:
Australian Commission on Safety and Quality in Health Care. (2012). National safety and
quality health service standards. Australian Commission on Safety and Quality in
Health Care.Retrieved from:
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-
Standards-Sept-2012.pdf
Azami-Aghdash, S., Tabrizi, J. S., Sadeghi-Bazargani, H., Hajebrahimi, S., & Naghavi-
Behzad, M. (2015). Developing performance indicators for clinical governance in
dimensions of risk management and clinical effectiveness. International Journal for
Quality in Health Care, 27(2), 110-116. DOI: https://doi.org/10.1093/intqhc/mzu102
Bamelis, L. L., Evers, S. M., Spinhoven, P., & Arntz, A. (2014). Results of a multicenter
randomized controlled trial of the clinical effectiveness of schema therapy for
personality disorders. American Journal of Psychiatry, 171(3), 305-322. DOI:
https://doi.org/10.1176/appi.ajp.2013.12040518
Currie, J., Mateer, J., Weston, D., Anderson, E., & Harding, J. (2017). Implementation of a
clinical governance framework to 17 combat service support brigade, Australian
army. International Journal of Health Governance, 22(1), 15-24. DOI:
https://doi.org/10.1108/IJHG-04-2016-0024
Flanigan, K. (2016). NSQHS standard-patient identification. ACORN: The Journal of
Perioperative Nursing in Australia, 29(1), 23. Retieved from:
https://search.informit.com.au/documentSummary;dn=883877754554045;res=IELHE
A
4PROMOTING CLINICAL EXCELLENCE
Jones, A., & Killion, S. (2017). title Clinical governance for Primary Health Networks.
Retrieved from:
https://ahha.asn.au/system/files/docs/publications/210417_issues_brief_no_22-
_clinical_governance_for_phns.pdf
Lamba, A. R., Linn, K., & Fletcher, K. E. (2014). Identifying patient safety problems during
team rounds: an ethnographic study. BMJ Qual Saf, bmjqs-2013. DOI:
http://dx.doi.org/10.1136/bmjqs-2013-002324
Luo, T., Wu, C., & Duan, L. (2018). Fishbone diagram and risk matrix analysis method and
its application in safety assessment of natural gas spherical tank. Journal of Cleaner
Production, 174, 296-304. DOI: https://doi.org/10.1016/j.jclepro.2017.10.334
Mumford, K., Young, A. C., & Nawaz, S. (2016). Federal public health workforce
development: an evidence-based approach for defining competencies. Journal of
public health management and practice: JPHMP, 22(3), 290. DOI:
10.1097/PHH.0000000000000205
Sarrami‐Foroushani, P., Travaglia, J., Debono, D., Clay‐Williams, R., & Braithwaite, J.
(2015). Scoping meta‐review: introducing a new methodology. Clinical and
translational science, 8(1), 77-81. DOI: https://doi.org/10.1111/cts.12188
Taylor, M. E., Lord, S. R., Brodaty, H., Kurrle, S. E., Hamilton, S., Ramsay, E., ... & Close,
J. C. (2017). A home-based, carer-enhanced exercise program improves balance and
falls efficacy in community-dwelling older people with dementia. International
psychogeriatrics, 29(1), 81-91. DOI: https://doi.org/10.1017/S1041610216001629
Usher, K., Woods, C., Conway, J., Lea, J., Parker, V., Barrett, F., ... & Jackson, D. (2018).
Patient safety content and delivery in pre-registration nursing curricula: A national
Jones, A., & Killion, S. (2017). title Clinical governance for Primary Health Networks.
Retrieved from:
https://ahha.asn.au/system/files/docs/publications/210417_issues_brief_no_22-
_clinical_governance_for_phns.pdf
Lamba, A. R., Linn, K., & Fletcher, K. E. (2014). Identifying patient safety problems during
team rounds: an ethnographic study. BMJ Qual Saf, bmjqs-2013. DOI:
http://dx.doi.org/10.1136/bmjqs-2013-002324
Luo, T., Wu, C., & Duan, L. (2018). Fishbone diagram and risk matrix analysis method and
its application in safety assessment of natural gas spherical tank. Journal of Cleaner
Production, 174, 296-304. DOI: https://doi.org/10.1016/j.jclepro.2017.10.334
Mumford, K., Young, A. C., & Nawaz, S. (2016). Federal public health workforce
development: an evidence-based approach for defining competencies. Journal of
public health management and practice: JPHMP, 22(3), 290. DOI:
10.1097/PHH.0000000000000205
Sarrami‐Foroushani, P., Travaglia, J., Debono, D., Clay‐Williams, R., & Braithwaite, J.
(2015). Scoping meta‐review: introducing a new methodology. Clinical and
translational science, 8(1), 77-81. DOI: https://doi.org/10.1111/cts.12188
Taylor, M. E., Lord, S. R., Brodaty, H., Kurrle, S. E., Hamilton, S., Ramsay, E., ... & Close,
J. C. (2017). A home-based, carer-enhanced exercise program improves balance and
falls efficacy in community-dwelling older people with dementia. International
psychogeriatrics, 29(1), 81-91. DOI: https://doi.org/10.1017/S1041610216001629
Usher, K., Woods, C., Conway, J., Lea, J., Parker, V., Barrett, F., ... & Jackson, D. (2018).
Patient safety content and delivery in pre-registration nursing curricula: A national
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

5PROMOTING CLINICAL EXCELLENCE
cross-sectional survey study. Nurse education today, 66, 82-89. DOI:
https://doi.org/10.1016/j.nedt.2018.04.013
cross-sectional survey study. Nurse education today, 66, 82-89. DOI:
https://doi.org/10.1016/j.nedt.2018.04.013
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





