Clinical Governance Strategies for Sentinel Event Reduction in HK
VerifiedAdded on 2023/06/15
|18
|4703
|267
Essay
AI Summary
This essay discusses the importance of clinical governance in healthcare, particularly in reducing sentinel events within the Hong Kong healthcare system. Using Ishikawa's Fishbone model, the essay analyzes the causes of inpatient suicides, a significant category of sentinel events reported by the Hospital Authority Hong Kong. Key contributing factors identified include poor communication, inadequate risk analysis, delays in activating suicide prevention strategies, and insufficient follow-up with patients on home leave. The essay then explores clinical governance strategies to address these root causes, such as improving communication skills through training, conducting thorough risk assessments, ensuring timely activation of prevention protocols, and implementing integrated care pathways with multidisciplinary teams for comprehensive patient support. Lewin's Force Field Model is employed to understand the driving and restraining forces affecting the implementation of change, highlighting the need to address restraining forces like poor communication and lack of knowledge while strengthening driving forces such as leadership, evidence-based practice, and risk analysis. The essay concludes by emphasizing the importance of a proactive and multifaceted approach to clinical governance to enhance patient safety and reduce the occurrence of sentinel events. Desklib provides access to similar essays and study resources for students.

Running head: Clinical Governance in Nursing
NURSING STUDY
-Clinical Governance
Name of the Student
Name of the University
Author Note
NURSING STUDY
-Clinical Governance
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Clinical Governance in Nursing
Introduction:
Clinical governance is an ‘umbrella term’ that refers to a system through which
healthcare organization develop the responsibility for continuous quality improvement and
maintain high quality care by fostering an environment that can facilitate excellence and
flourishing clinical care (Scally and Donaldson 2015; rcn.org.uk 2018). Clinical Governance
ensures proper care for everyone seeking healthcare, facilitates the best practice by staff,
maintenance of the best possible standards (Qotba 2018). The importance of clinical
governance is supported by the duty of healthcare organisations in the maintenance of quality
and safety of care. Because of such aspects, clinical governance has been implemented in the
UK by the National Health Service (NHS) and involves 5 key themes: patient focus,
information focus, quality improvement, staff focus, leadership (rcn.org.uk 2018). This can
be considered as a part of Total Quality Management (TQM) which is an approach towards
long term success through customer satisfaction, where the members of the organization
are involved in the improvement of the process, services or products as well as the work
culture (asq.org 2018). Such aspects of TQM have been incorporated into the HA Annual
Plan framework 2017-2018 that included three strategies: a) providing patient centered care
b) developing competency and commitment in workforce c) improve financial
sustainability (Ha.org.hk 2018). Al-Shdaifat (2015) suggested that the most important factor
in the implementation of TQM was to maintain a customer focus as the first priority,
attributed through interviews with nurses. Hong Kong uses the clinical governance model
utilized by the UK because of two reasons a) similarity in the professional training systems
between UK and Hong Kong and b) the developmental stage of the UK model allows scope
for learning through their experiences (Leng 2005)
In this essay, the importance of clinical governance will be discussed briefly, and then
the causes of the selected scenario (scenario 2) will be visualised using the Fishbone model.
Introduction:
Clinical governance is an ‘umbrella term’ that refers to a system through which
healthcare organization develop the responsibility for continuous quality improvement and
maintain high quality care by fostering an environment that can facilitate excellence and
flourishing clinical care (Scally and Donaldson 2015; rcn.org.uk 2018). Clinical Governance
ensures proper care for everyone seeking healthcare, facilitates the best practice by staff,
maintenance of the best possible standards (Qotba 2018). The importance of clinical
governance is supported by the duty of healthcare organisations in the maintenance of quality
and safety of care. Because of such aspects, clinical governance has been implemented in the
UK by the National Health Service (NHS) and involves 5 key themes: patient focus,
information focus, quality improvement, staff focus, leadership (rcn.org.uk 2018). This can
be considered as a part of Total Quality Management (TQM) which is an approach towards
long term success through customer satisfaction, where the members of the organization
are involved in the improvement of the process, services or products as well as the work
culture (asq.org 2018). Such aspects of TQM have been incorporated into the HA Annual
Plan framework 2017-2018 that included three strategies: a) providing patient centered care
b) developing competency and commitment in workforce c) improve financial
sustainability (Ha.org.hk 2018). Al-Shdaifat (2015) suggested that the most important factor
in the implementation of TQM was to maintain a customer focus as the first priority,
attributed through interviews with nurses. Hong Kong uses the clinical governance model
utilized by the UK because of two reasons a) similarity in the professional training systems
between UK and Hong Kong and b) the developmental stage of the UK model allows scope
for learning through their experiences (Leng 2005)
In this essay, the importance of clinical governance will be discussed briefly, and then
the causes of the selected scenario (scenario 2) will be visualised using the Fishbone model.
2Clinical Governance in Nursing
After this, the strategies to address such causes will be discussed to identify appropriate
clinical governance strategies. In the conclusion, the key aspects of the discussion will be
highlighted.
Main Body:
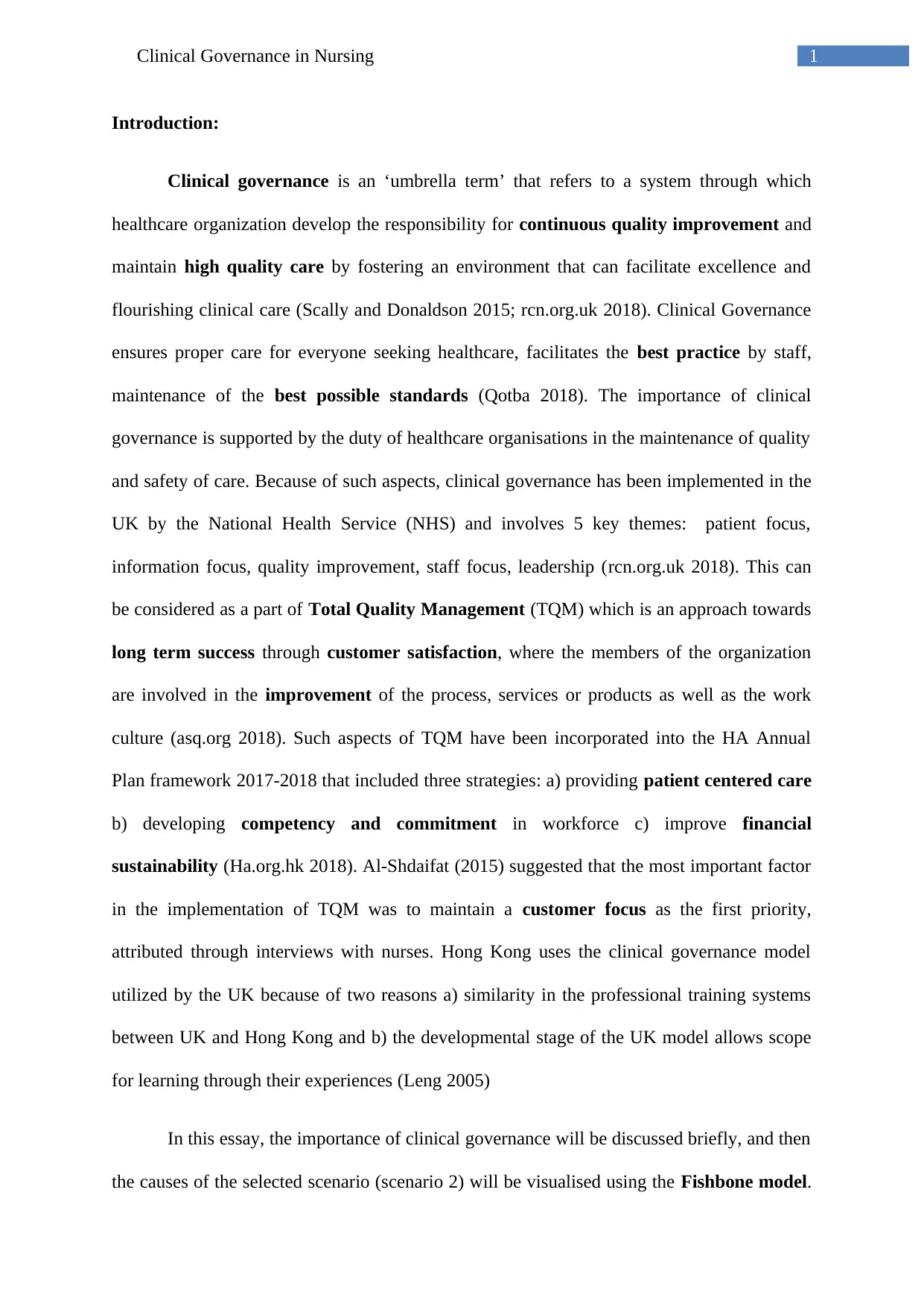
Ishikawa’s Fishbone Analysis is a universal model that can be used in the
identification of cause and effects associated with a given problem and represented in a
structured format. This visual tool allows several contributing factors to be changed
simultaneously and helps to fully comprehend the identification of multiple factors associated
with a situation or problem. It allows scope for team discussions and solving problems, and
facilitates systematic discourse while maintaining focus on the problem. IN the fishbone
model, the problems are categorised into different groups like: people (the involved
personnel in the process); process (any important pasrt6 of the process); equipment (used in
the process); material used and management (evaluation of quality through evaluation of
data) and environment (Vetter et al. 2016).
Figure 1: Ishikawa’s Fishbone model; source: (Vetter et al. 2016).
Advantages of the fishbone model are:
After this, the strategies to address such causes will be discussed to identify appropriate
clinical governance strategies. In the conclusion, the key aspects of the discussion will be
highlighted.
Main Body:
Ishikawa’s Fishbone Analysis is a universal model that can be used in the
identification of cause and effects associated with a given problem and represented in a
structured format. This visual tool allows several contributing factors to be changed
simultaneously and helps to fully comprehend the identification of multiple factors associated
with a situation or problem. It allows scope for team discussions and solving problems, and
facilitates systematic discourse while maintaining focus on the problem. IN the fishbone
model, the problems are categorised into different groups like: people (the involved
personnel in the process); process (any important pasrt6 of the process); equipment (used in
the process); material used and management (evaluation of quality through evaluation of
data) and environment (Vetter et al. 2016).
Figure 1: Ishikawa’s Fishbone model; source: (Vetter et al. 2016).
Advantages of the fishbone model are:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Clinical Governance in Nursing
Allows a comprehensive analysis of the causes of a problem without the possibility of
overlooking any root cause
Easy implementation of the model.
Easy to comprehend due to the visual representation of the cause-effect relation.
Enables focussing on the big picture in relation to the influences of the identified
factors on the problem or issue being discussed.
It also allows identification of areas of weakness, and therefore the scope of further
improvement and rectifications.
Disadvantages of this model are:
Complex situations, involving interrelation of several different factors might be
difficult to represent on the fish bone.
Lack of space while drawing the fishbone can leave inadequate scope for the
exploration of cause-effect relation properly.
The model only focuses in analysing the causes of a problem but not on any solutions.
(siteresources.worldbank.org 2018)
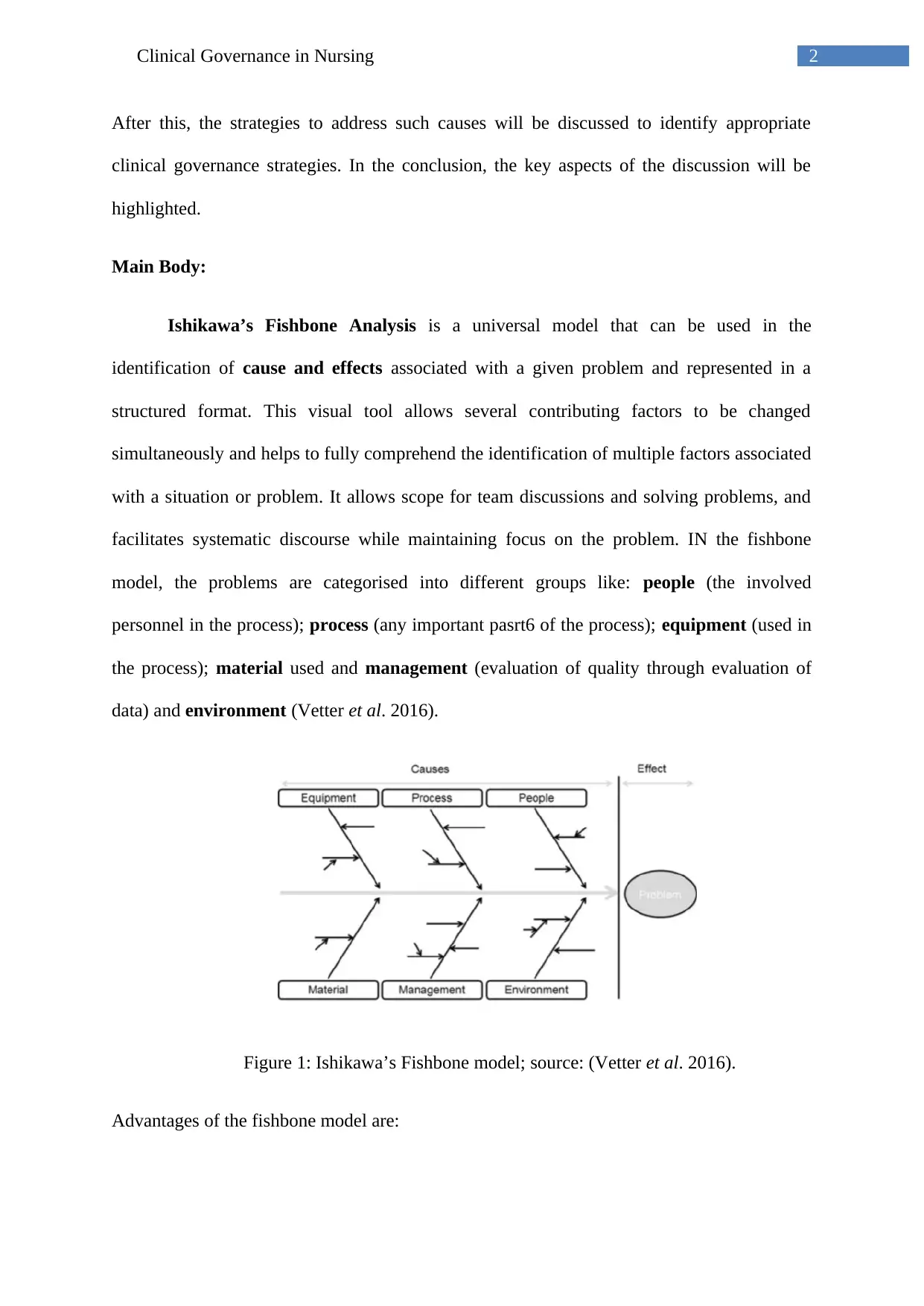
The Annual report on sentinel and serious untoward events- 1 October 2013 to 20
September 2014 published by Hospital Authority Hong Kong on January 2015, showed 19
cases of death of an inpatient due to suicide (that included 10 patients on home leave and 2
patients reported missing. The report showed that most of the Sentinel Events in the hospitals
were contributed by retained instruments or materials during surgery (20 events) and due to
inpatient suicides (19 events). However, the suicide cases accounted for most of the severity
of the consequences compared to other sentinel events (Ha.org.hk 2015).
Allows a comprehensive analysis of the causes of a problem without the possibility of
overlooking any root cause
Easy implementation of the model.
Easy to comprehend due to the visual representation of the cause-effect relation.
Enables focussing on the big picture in relation to the influences of the identified
factors on the problem or issue being discussed.
It also allows identification of areas of weakness, and therefore the scope of further
improvement and rectifications.
Disadvantages of this model are:
Complex situations, involving interrelation of several different factors might be
difficult to represent on the fish bone.
Lack of space while drawing the fishbone can leave inadequate scope for the
exploration of cause-effect relation properly.
The model only focuses in analysing the causes of a problem but not on any solutions.
(siteresources.worldbank.org 2018)
The Annual report on sentinel and serious untoward events- 1 October 2013 to 20
September 2014 published by Hospital Authority Hong Kong on January 2015, showed 19
cases of death of an inpatient due to suicide (that included 10 patients on home leave and 2
patients reported missing. The report showed that most of the Sentinel Events in the hospitals
were contributed by retained instruments or materials during surgery (20 events) and due to
inpatient suicides (19 events). However, the suicide cases accounted for most of the severity
of the consequences compared to other sentinel events (Ha.org.hk 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Clinical Governance in Nursing
Figure 2: Outcomes of Sentinel Events reported between October 2013 to September 2014
represented categorically; source: (Ha.org.hk 2015).
The report highlighted the following factors that attributed to such events:
Communication: The study showed an inadequate communication taking place
between the patient, staff and the patient’s family. Due to this, the patient’s mental health
status was not properly understood, and any plans of the patient to commit suicide went
unnoticed by either staff or the patient’s family.
Environment: Presence of environmental risks in the hospital environment (like in
the patient’s toilet or bathroom) for any point of anchorage for hanging was not thoroughly
assessed. Also, presence of sharp objects that could be used by the patient for self inflicted
injuries by stabbing and bleeding was not properly analysed, due to which such items might
have been used by the patients to commit suicides.
Policies/Procedures/Guidelines: There was a delay in the activation or reactivation
of suicide precautionary strategies for patients with unstable emotional state or identified at
Figure 2: Outcomes of Sentinel Events reported between October 2013 to September 2014
represented categorically; source: (Ha.org.hk 2015).
The report highlighted the following factors that attributed to such events:
Communication: The study showed an inadequate communication taking place
between the patient, staff and the patient’s family. Due to this, the patient’s mental health
status was not properly understood, and any plans of the patient to commit suicide went
unnoticed by either staff or the patient’s family.
Environment: Presence of environmental risks in the hospital environment (like in
the patient’s toilet or bathroom) for any point of anchorage for hanging was not thoroughly
assessed. Also, presence of sharp objects that could be used by the patient for self inflicted
injuries by stabbing and bleeding was not properly analysed, due to which such items might
have been used by the patients to commit suicides.
Policies/Procedures/Guidelines: There was a delay in the activation or reactivation
of suicide precautionary strategies for patients with unstable emotional state or identified at
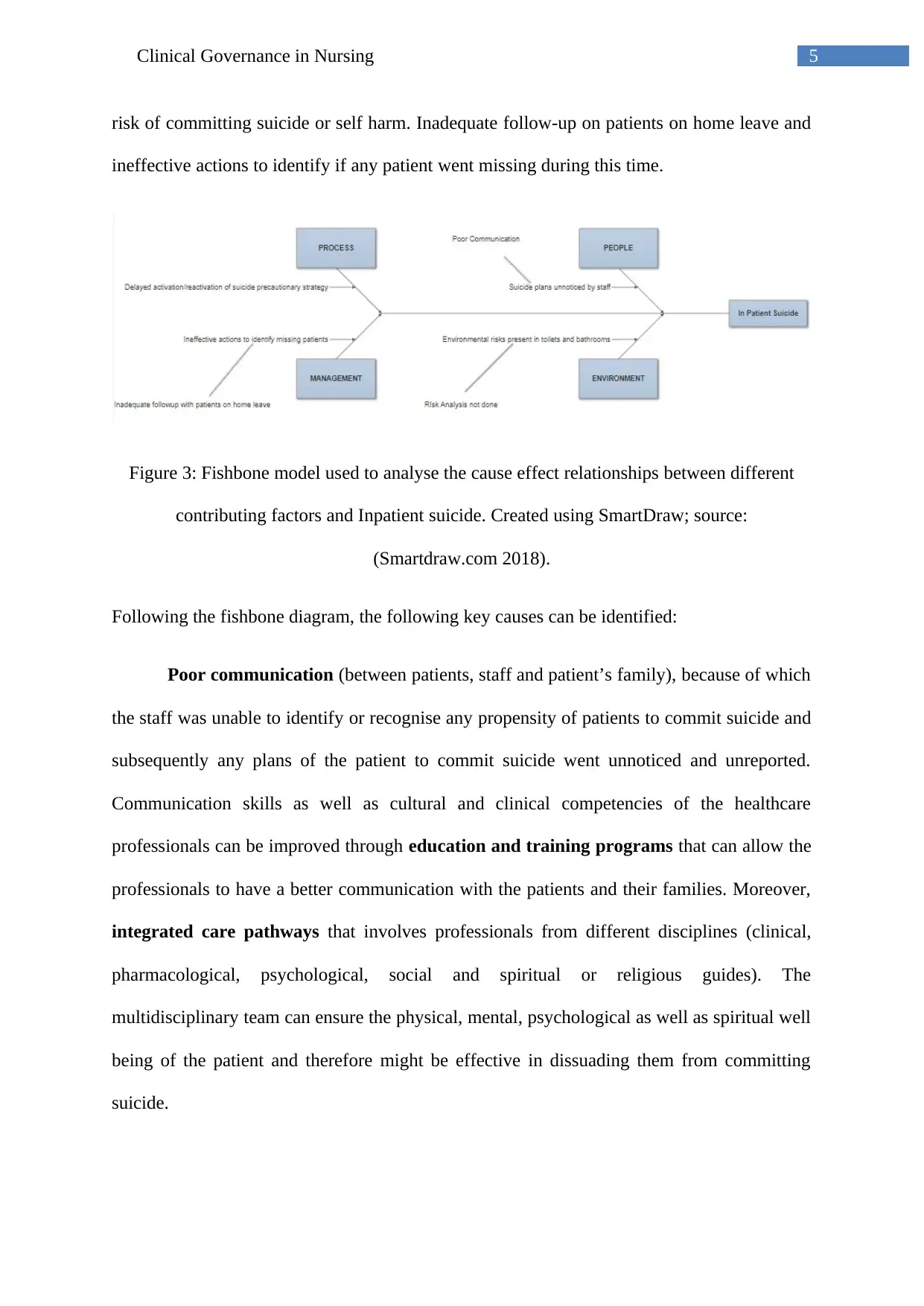
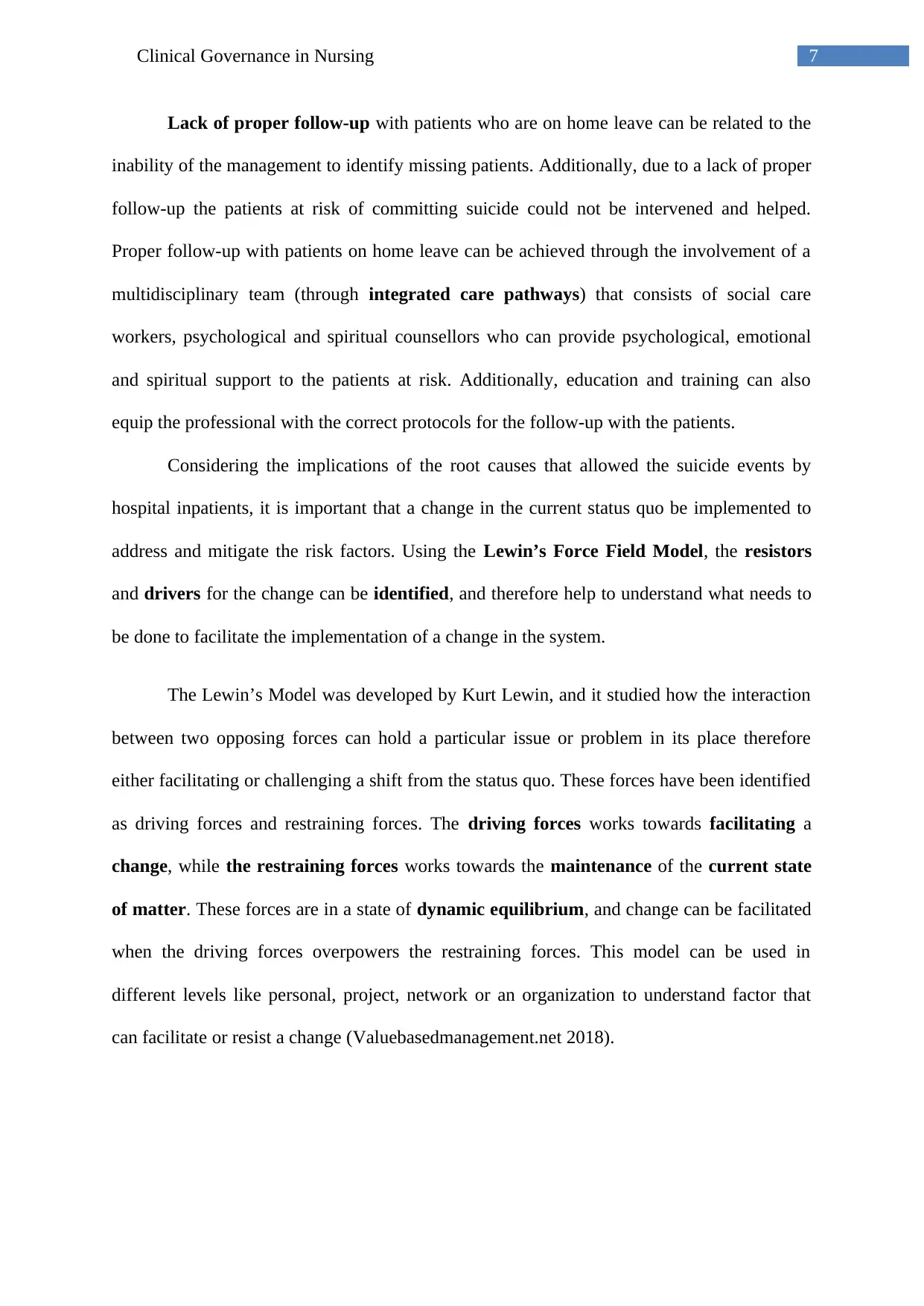
5Clinical Governance in Nursing
risk of committing suicide or self harm. Inadequate follow-up on patients on home leave and
ineffective actions to identify if any patient went missing during this time.
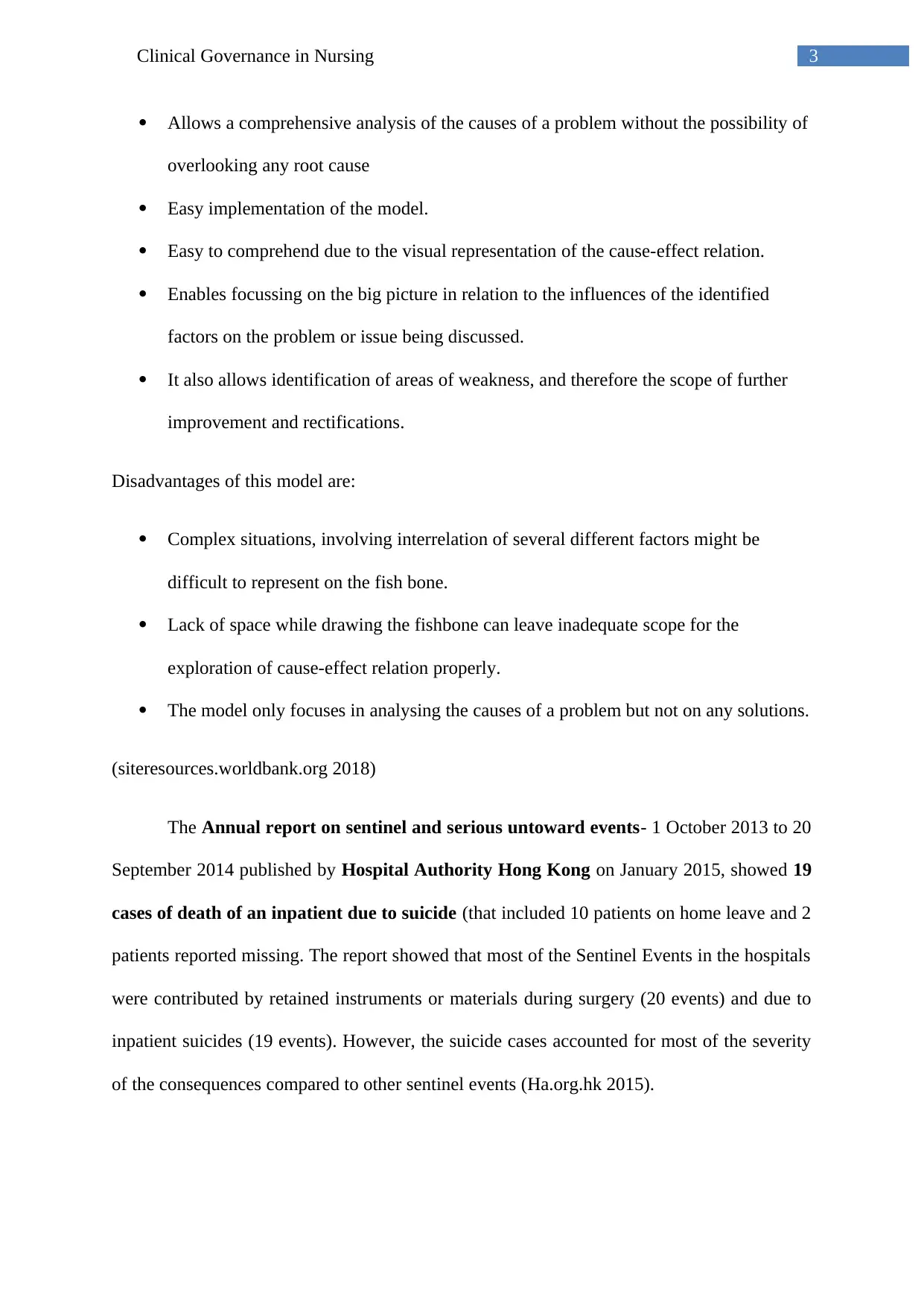
Figure 3: Fishbone model used to analyse the cause effect relationships between different
contributing factors and Inpatient suicide. Created using SmartDraw; source:
(Smartdraw.com 2018).
Following the fishbone diagram, the following key causes can be identified:
Poor communication (between patients, staff and patient’s family), because of which
the staff was unable to identify or recognise any propensity of patients to commit suicide and
subsequently any plans of the patient to commit suicide went unnoticed and unreported.
Communication skills as well as cultural and clinical competencies of the healthcare
professionals can be improved through education and training programs that can allow the
professionals to have a better communication with the patients and their families. Moreover,
integrated care pathways that involves professionals from different disciplines (clinical,
pharmacological, psychological, social and spiritual or religious guides). The
multidisciplinary team can ensure the physical, mental, psychological as well as spiritual well
being of the patient and therefore might be effective in dissuading them from committing
suicide.
risk of committing suicide or self harm. Inadequate follow-up on patients on home leave and
ineffective actions to identify if any patient went missing during this time.
Figure 3: Fishbone model used to analyse the cause effect relationships between different
contributing factors and Inpatient suicide. Created using SmartDraw; source:
(Smartdraw.com 2018).
Following the fishbone diagram, the following key causes can be identified:
Poor communication (between patients, staff and patient’s family), because of which
the staff was unable to identify or recognise any propensity of patients to commit suicide and
subsequently any plans of the patient to commit suicide went unnoticed and unreported.
Communication skills as well as cultural and clinical competencies of the healthcare
professionals can be improved through education and training programs that can allow the
professionals to have a better communication with the patients and their families. Moreover,
integrated care pathways that involves professionals from different disciplines (clinical,
pharmacological, psychological, social and spiritual or religious guides). The
multidisciplinary team can ensure the physical, mental, psychological as well as spiritual well
being of the patient and therefore might be effective in dissuading them from committing
suicide.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Clinical Governance in Nursing
Proper Risk Analysis was not done, which allowed the presence of hazardous or risky
environment to persist in the toilets or bathrooms like potential anchorages for hanging inside
toilets and bathrooms or any sharp objects used to inflict self harm. The patients consequently
were able to use the curtain rails, door beam, and metal rods in toilets and or bathrooms as a
point of anchorage and waist belts, cloth strips from bed linen, plastic chains or nylon ropes
for hanging. Few patients also committed suicide by stabbing and bleeding, showing that they
had access to sharp objects that can inflict serious and fatal injuries. This highlights the
necessity of conducting a risk management to identify and eliminate any factors that can
increase the risk of self harm done by the patient.
Delay in the activation or inactivation of suicide prevention strategies for patients
identified at risk for committing suicide was another significant factor that allowed such
events to occur. This can be caused due to a lack of understanding of mental health issues
which can increase risks of suicides, and the inability of staff to identify such patients at risk
of committing suicide, for example identification of patients who might show emotional
instability. This highlights the necessity of an improvement in the understanding of different
mental health issues that can push a patient towards suicide, and therefore help in the early
identification of patients showing signs of mental instability, and suicidal tendencies.
Education and training provided to healthcare professionals can equip them with such
important knowledge, and allow timely activation or reactivation of precautionary and
preventative strategies for the patients. Development of research based practice and clinical
competency can also allow the application of effective strategies to prevent suicide. Research
based practices can lead to an improved clinical competency, and therefore foster proper
clinical decisions to be made, based on evidence and best practice guidelines, that can
benefit the patient.
Proper Risk Analysis was not done, which allowed the presence of hazardous or risky
environment to persist in the toilets or bathrooms like potential anchorages for hanging inside
toilets and bathrooms or any sharp objects used to inflict self harm. The patients consequently
were able to use the curtain rails, door beam, and metal rods in toilets and or bathrooms as a
point of anchorage and waist belts, cloth strips from bed linen, plastic chains or nylon ropes
for hanging. Few patients also committed suicide by stabbing and bleeding, showing that they
had access to sharp objects that can inflict serious and fatal injuries. This highlights the
necessity of conducting a risk management to identify and eliminate any factors that can
increase the risk of self harm done by the patient.
Delay in the activation or inactivation of suicide prevention strategies for patients
identified at risk for committing suicide was another significant factor that allowed such
events to occur. This can be caused due to a lack of understanding of mental health issues
which can increase risks of suicides, and the inability of staff to identify such patients at risk
of committing suicide, for example identification of patients who might show emotional
instability. This highlights the necessity of an improvement in the understanding of different
mental health issues that can push a patient towards suicide, and therefore help in the early
identification of patients showing signs of mental instability, and suicidal tendencies.
Education and training provided to healthcare professionals can equip them with such
important knowledge, and allow timely activation or reactivation of precautionary and
preventative strategies for the patients. Development of research based practice and clinical
competency can also allow the application of effective strategies to prevent suicide. Research
based practices can lead to an improved clinical competency, and therefore foster proper
clinical decisions to be made, based on evidence and best practice guidelines, that can
benefit the patient.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Clinical Governance in Nursing
Lack of proper follow-up with patients who are on home leave can be related to the
inability of the management to identify missing patients. Additionally, due to a lack of proper
follow-up the patients at risk of committing suicide could not be intervened and helped.
Proper follow-up with patients on home leave can be achieved through the involvement of a
multidisciplinary team (through integrated care pathways) that consists of social care
workers, psychological and spiritual counsellors who can provide psychological, emotional
and spiritual support to the patients at risk. Additionally, education and training can also
equip the professional with the correct protocols for the follow-up with the patients.
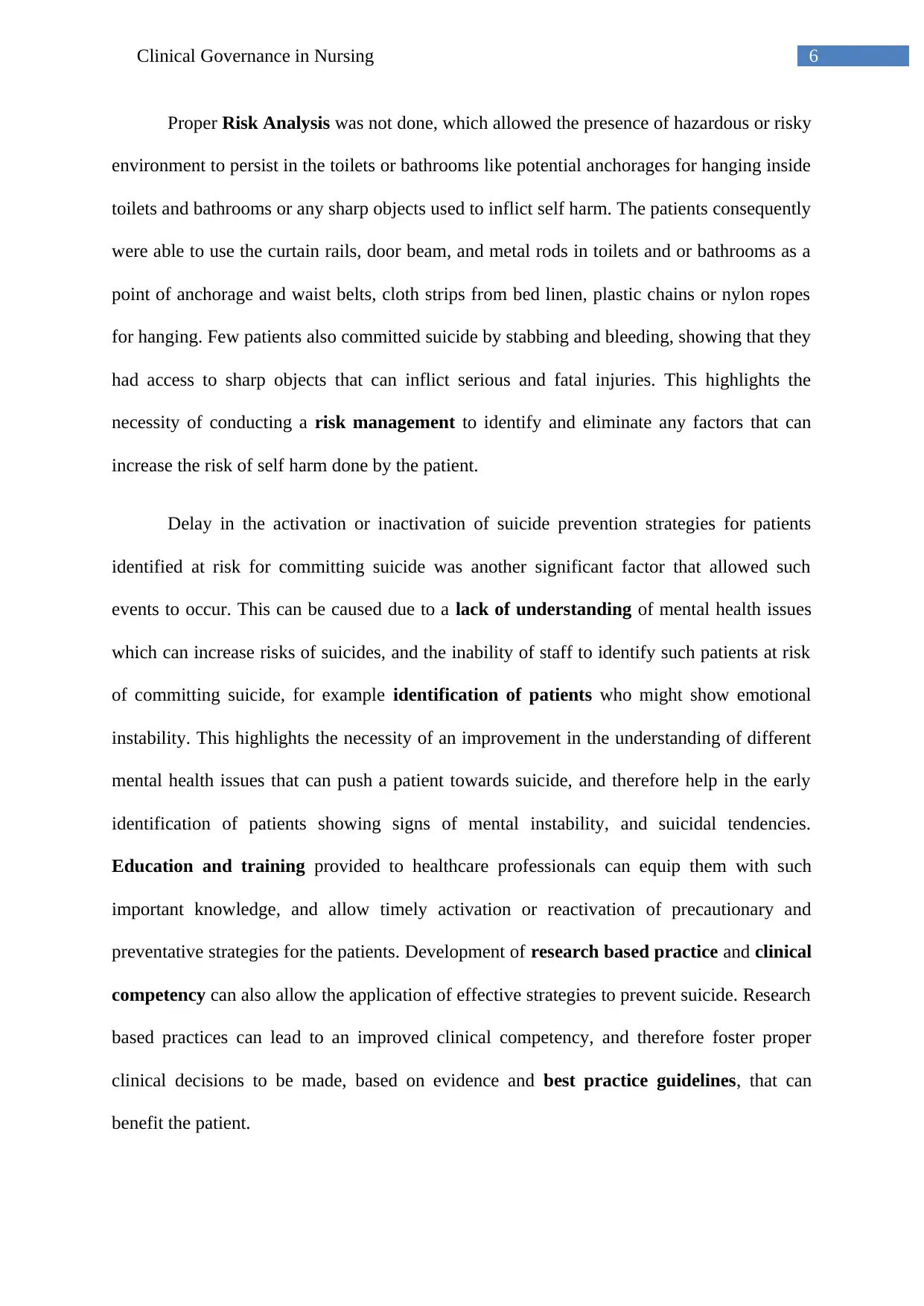
Considering the implications of the root causes that allowed the suicide events by
hospital inpatients, it is important that a change in the current status quo be implemented to
address and mitigate the risk factors. Using the Lewin’s Force Field Model, the resistors
and drivers for the change can be identified, and therefore help to understand what needs to
be done to facilitate the implementation of a change in the system.
The Lewin’s Model was developed by Kurt Lewin, and it studied how the interaction
between two opposing forces can hold a particular issue or problem in its place therefore
either facilitating or challenging a shift from the status quo. These forces have been identified
as driving forces and restraining forces. The driving forces works towards facilitating a
change, while the restraining forces works towards the maintenance of the current state
of matter. These forces are in a state of dynamic equilibrium, and change can be facilitated
when the driving forces overpowers the restraining forces. This model can be used in
different levels like personal, project, network or an organization to understand factor that
can facilitate or resist a change (Valuebasedmanagement.net 2018).
Lack of proper follow-up with patients who are on home leave can be related to the
inability of the management to identify missing patients. Additionally, due to a lack of proper
follow-up the patients at risk of committing suicide could not be intervened and helped.
Proper follow-up with patients on home leave can be achieved through the involvement of a
multidisciplinary team (through integrated care pathways) that consists of social care
workers, psychological and spiritual counsellors who can provide psychological, emotional
and spiritual support to the patients at risk. Additionally, education and training can also
equip the professional with the correct protocols for the follow-up with the patients.
Considering the implications of the root causes that allowed the suicide events by
hospital inpatients, it is important that a change in the current status quo be implemented to
address and mitigate the risk factors. Using the Lewin’s Force Field Model, the resistors
and drivers for the change can be identified, and therefore help to understand what needs to
be done to facilitate the implementation of a change in the system.
The Lewin’s Model was developed by Kurt Lewin, and it studied how the interaction
between two opposing forces can hold a particular issue or problem in its place therefore
either facilitating or challenging a shift from the status quo. These forces have been identified
as driving forces and restraining forces. The driving forces works towards facilitating a
change, while the restraining forces works towards the maintenance of the current state
of matter. These forces are in a state of dynamic equilibrium, and change can be facilitated
when the driving forces overpowers the restraining forces. This model can be used in
different levels like personal, project, network or an organization to understand factor that
can facilitate or resist a change (Valuebasedmanagement.net 2018).
8Clinical Governance in Nursing
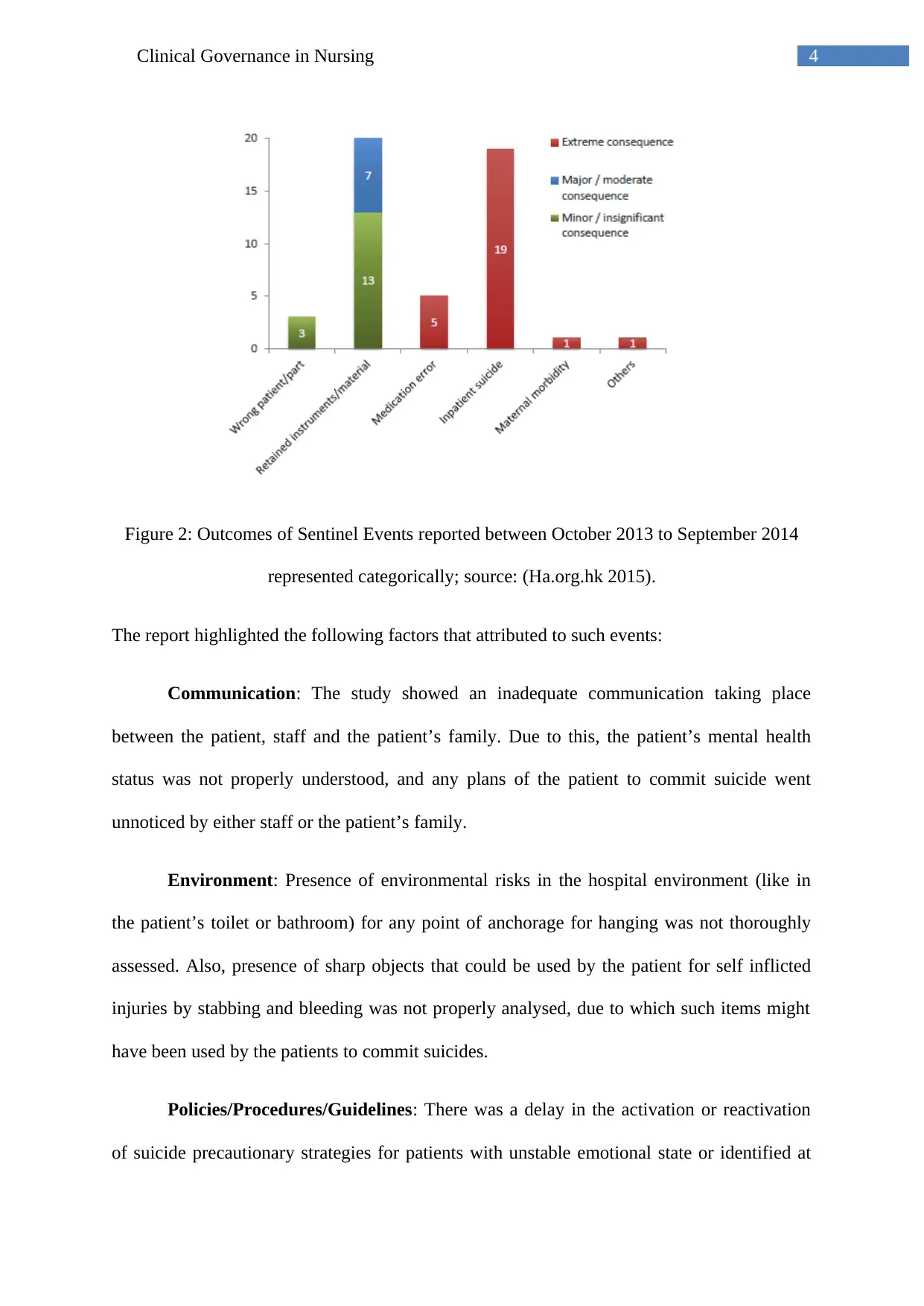
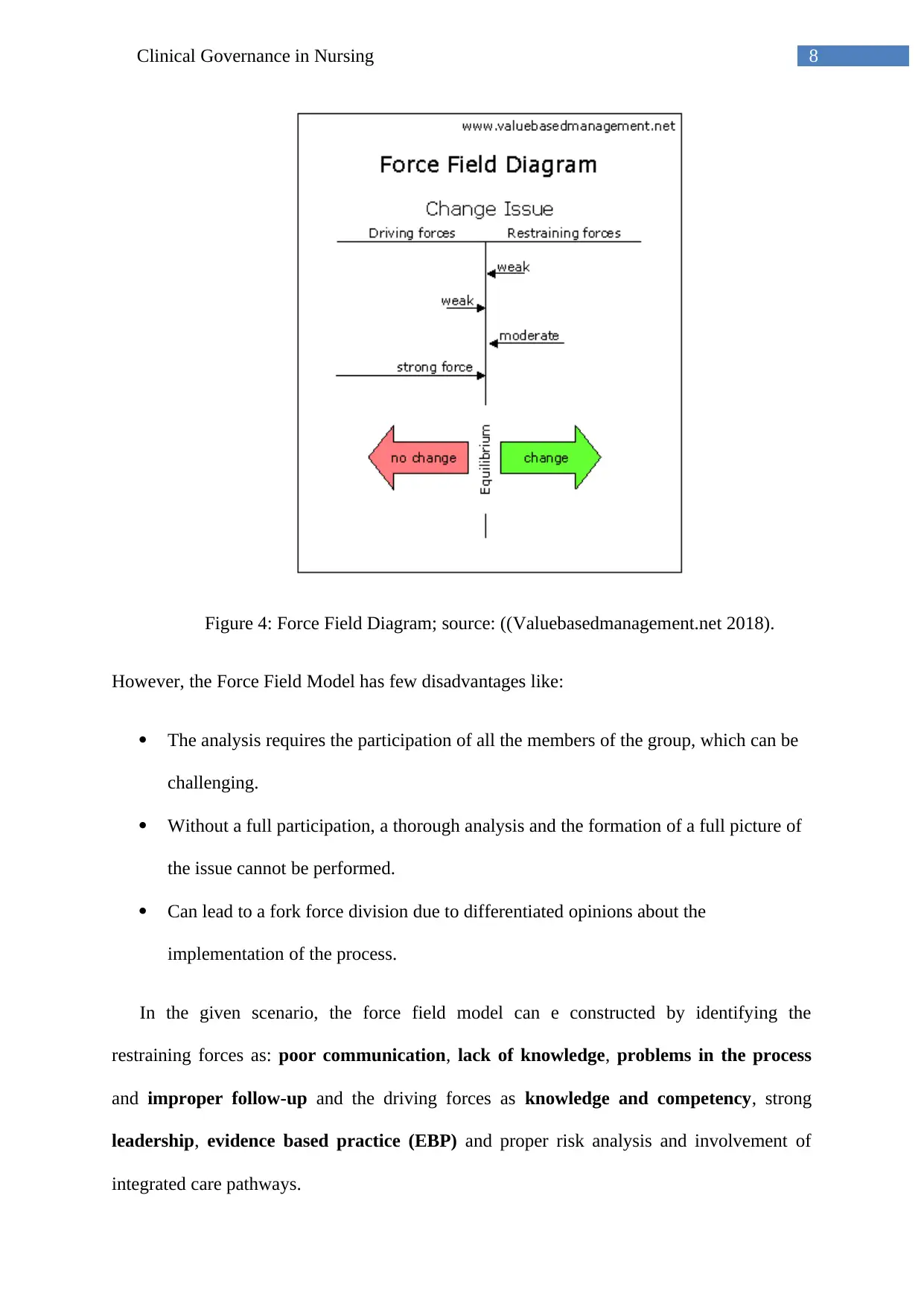
Figure 4: Force Field Diagram; source: ((Valuebasedmanagement.net 2018).
However, the Force Field Model has few disadvantages like:
The analysis requires the participation of all the members of the group, which can be
challenging.
Without a full participation, a thorough analysis and the formation of a full picture of
the issue cannot be performed.
Can lead to a fork force division due to differentiated opinions about the
implementation of the process.
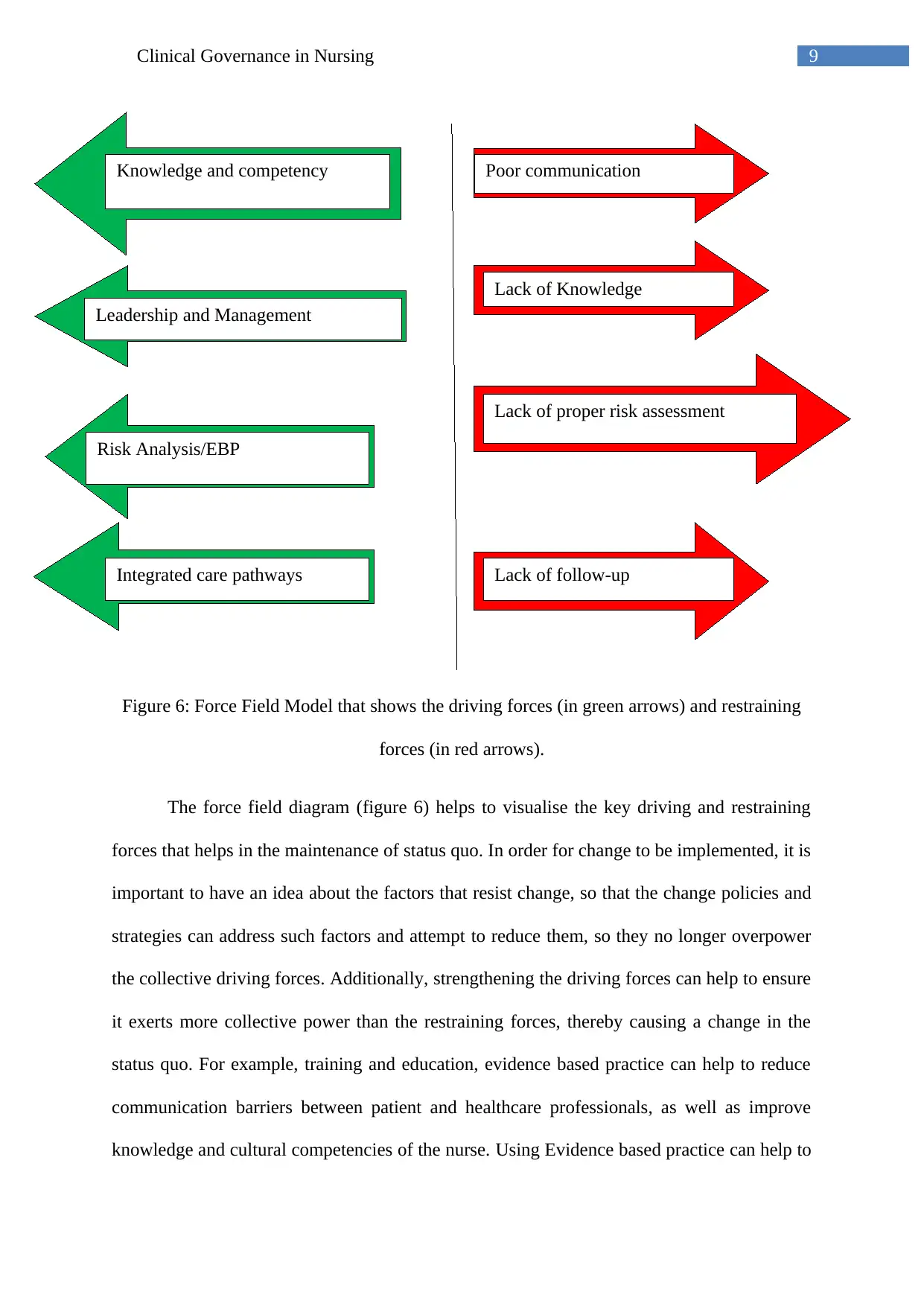
In the given scenario, the force field model can e constructed by identifying the
restraining forces as: poor communication, lack of knowledge, problems in the process
and improper follow-up and the driving forces as knowledge and competency, strong
leadership, evidence based practice (EBP) and proper risk analysis and involvement of
integrated care pathways.
Figure 4: Force Field Diagram; source: ((Valuebasedmanagement.net 2018).
However, the Force Field Model has few disadvantages like:
The analysis requires the participation of all the members of the group, which can be
challenging.
Without a full participation, a thorough analysis and the formation of a full picture of
the issue cannot be performed.
Can lead to a fork force division due to differentiated opinions about the
implementation of the process.
In the given scenario, the force field model can e constructed by identifying the
restraining forces as: poor communication, lack of knowledge, problems in the process
and improper follow-up and the driving forces as knowledge and competency, strong
leadership, evidence based practice (EBP) and proper risk analysis and involvement of
integrated care pathways.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Clinical Governance in Nursing
Figure 6: Force Field Model that shows the driving forces (in green arrows) and restraining
forces (in red arrows).
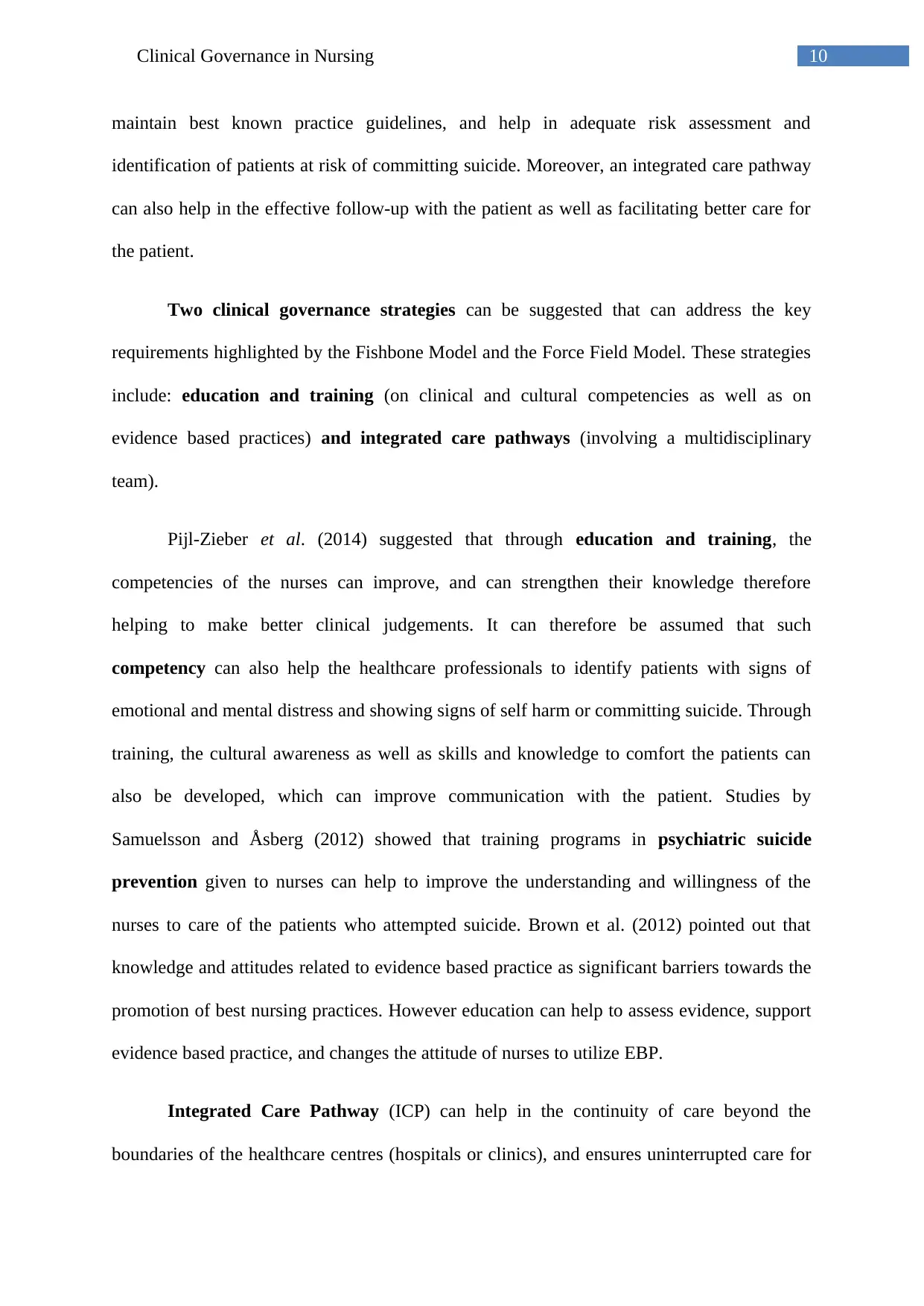
The force field diagram (figure 6) helps to visualise the key driving and restraining
forces that helps in the maintenance of status quo. In order for change to be implemented, it is
important to have an idea about the factors that resist change, so that the change policies and
strategies can address such factors and attempt to reduce them, so they no longer overpower
the collective driving forces. Additionally, strengthening the driving forces can help to ensure
it exerts more collective power than the restraining forces, thereby causing a change in the
status quo. For example, training and education, evidence based practice can help to reduce
communication barriers between patient and healthcare professionals, as well as improve
knowledge and cultural competencies of the nurse. Using Evidence based practice can help to
Poor communication
Lack of Knowledge
Lack of proper risk assessment
Lack of follow-up
Knowledge and competency
Leadership and Management
Risk Analysis/EBP
Integrated care pathways
Figure 6: Force Field Model that shows the driving forces (in green arrows) and restraining
forces (in red arrows).
The force field diagram (figure 6) helps to visualise the key driving and restraining
forces that helps in the maintenance of status quo. In order for change to be implemented, it is
important to have an idea about the factors that resist change, so that the change policies and
strategies can address such factors and attempt to reduce them, so they no longer overpower
the collective driving forces. Additionally, strengthening the driving forces can help to ensure
it exerts more collective power than the restraining forces, thereby causing a change in the
status quo. For example, training and education, evidence based practice can help to reduce
communication barriers between patient and healthcare professionals, as well as improve
knowledge and cultural competencies of the nurse. Using Evidence based practice can help to
Poor communication
Lack of Knowledge
Lack of proper risk assessment
Lack of follow-up
Knowledge and competency
Leadership and Management
Risk Analysis/EBP
Integrated care pathways
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10Clinical Governance in Nursing
maintain best known practice guidelines, and help in adequate risk assessment and
identification of patients at risk of committing suicide. Moreover, an integrated care pathway
can also help in the effective follow-up with the patient as well as facilitating better care for
the patient.
Two clinical governance strategies can be suggested that can address the key
requirements highlighted by the Fishbone Model and the Force Field Model. These strategies
include: education and training (on clinical and cultural competencies as well as on
evidence based practices) and integrated care pathways (involving a multidisciplinary
team).
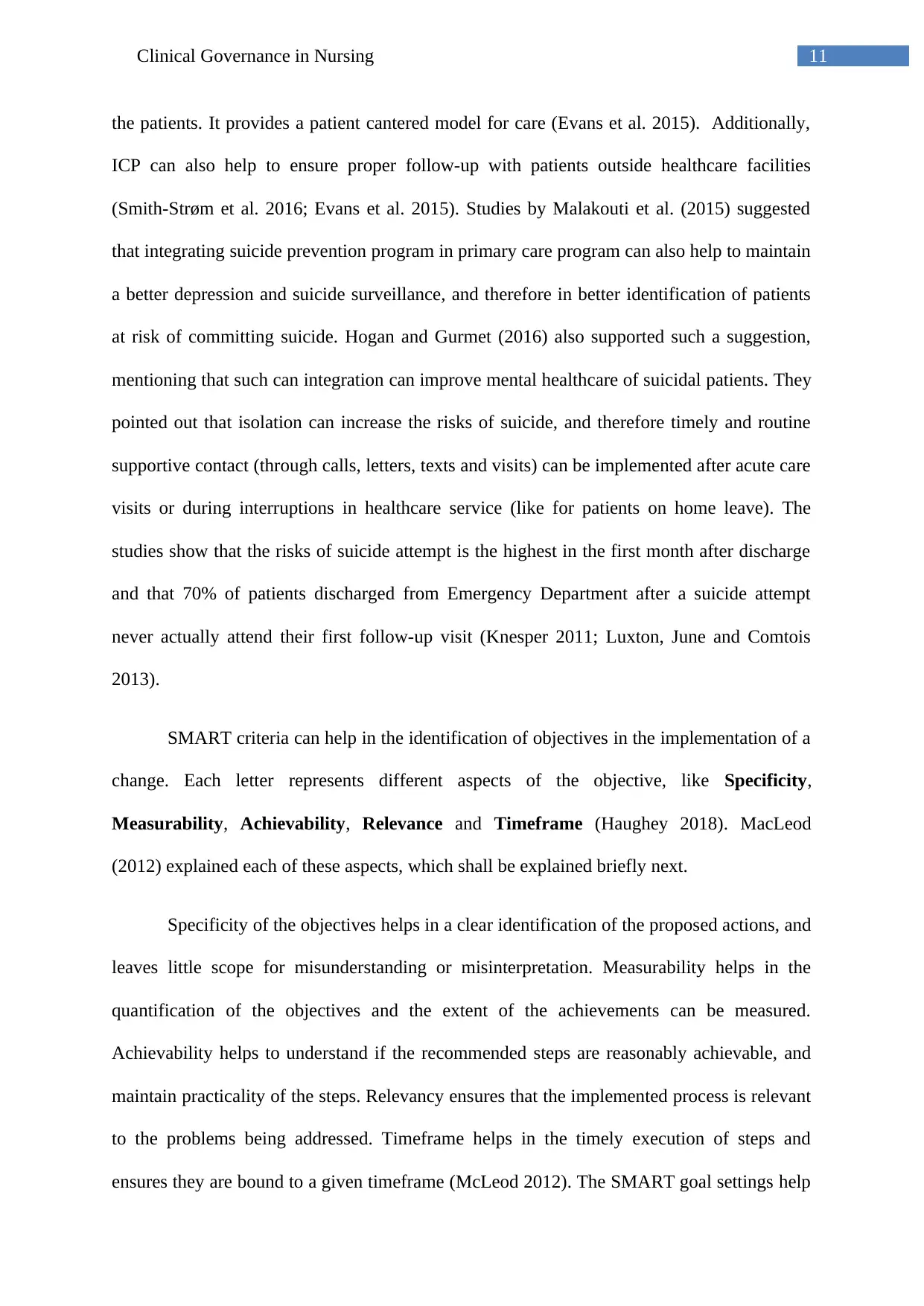
Pijl-Zieber et al. (2014) suggested that through education and training, the
competencies of the nurses can improve, and can strengthen their knowledge therefore
helping to make better clinical judgements. It can therefore be assumed that such
competency can also help the healthcare professionals to identify patients with signs of
emotional and mental distress and showing signs of self harm or committing suicide. Through
training, the cultural awareness as well as skills and knowledge to comfort the patients can
also be developed, which can improve communication with the patient. Studies by
Samuelsson and Åsberg (2012) showed that training programs in psychiatric suicide
prevention given to nurses can help to improve the understanding and willingness of the
nurses to care of the patients who attempted suicide. Brown et al. (2012) pointed out that
knowledge and attitudes related to evidence based practice as significant barriers towards the
promotion of best nursing practices. However education can help to assess evidence, support
evidence based practice, and changes the attitude of nurses to utilize EBP.
Integrated Care Pathway (ICP) can help in the continuity of care beyond the
boundaries of the healthcare centres (hospitals or clinics), and ensures uninterrupted care for
maintain best known practice guidelines, and help in adequate risk assessment and
identification of patients at risk of committing suicide. Moreover, an integrated care pathway
can also help in the effective follow-up with the patient as well as facilitating better care for
the patient.
Two clinical governance strategies can be suggested that can address the key
requirements highlighted by the Fishbone Model and the Force Field Model. These strategies
include: education and training (on clinical and cultural competencies as well as on
evidence based practices) and integrated care pathways (involving a multidisciplinary
team).
Pijl-Zieber et al. (2014) suggested that through education and training, the
competencies of the nurses can improve, and can strengthen their knowledge therefore
helping to make better clinical judgements. It can therefore be assumed that such
competency can also help the healthcare professionals to identify patients with signs of
emotional and mental distress and showing signs of self harm or committing suicide. Through
training, the cultural awareness as well as skills and knowledge to comfort the patients can
also be developed, which can improve communication with the patient. Studies by
Samuelsson and Åsberg (2012) showed that training programs in psychiatric suicide
prevention given to nurses can help to improve the understanding and willingness of the
nurses to care of the patients who attempted suicide. Brown et al. (2012) pointed out that
knowledge and attitudes related to evidence based practice as significant barriers towards the
promotion of best nursing practices. However education can help to assess evidence, support
evidence based practice, and changes the attitude of nurses to utilize EBP.
Integrated Care Pathway (ICP) can help in the continuity of care beyond the
boundaries of the healthcare centres (hospitals or clinics), and ensures uninterrupted care for
11Clinical Governance in Nursing
the patients. It provides a patient cantered model for care (Evans et al. 2015). Additionally,
ICP can also help to ensure proper follow-up with patients outside healthcare facilities
(Smith-Strøm et al. 2016; Evans et al. 2015). Studies by Malakouti et al. (2015) suggested
that integrating suicide prevention program in primary care program can also help to maintain
a better depression and suicide surveillance, and therefore in better identification of patients
at risk of committing suicide. Hogan and Gurmet (2016) also supported such a suggestion,
mentioning that such can integration can improve mental healthcare of suicidal patients. They
pointed out that isolation can increase the risks of suicide, and therefore timely and routine
supportive contact (through calls, letters, texts and visits) can be implemented after acute care
visits or during interruptions in healthcare service (like for patients on home leave). The
studies show that the risks of suicide attempt is the highest in the first month after discharge
and that 70% of patients discharged from Emergency Department after a suicide attempt
never actually attend their first follow-up visit (Knesper 2011; Luxton, June and Comtois
2013).
SMART criteria can help in the identification of objectives in the implementation of a
change. Each letter represents different aspects of the objective, like Specificity,
Measurability, Achievability, Relevance and Timeframe (Haughey 2018). MacLeod
(2012) explained each of these aspects, which shall be explained briefly next.
Specificity of the objectives helps in a clear identification of the proposed actions, and
leaves little scope for misunderstanding or misinterpretation. Measurability helps in the
quantification of the objectives and the extent of the achievements can be measured.
Achievability helps to understand if the recommended steps are reasonably achievable, and
maintain practicality of the steps. Relevancy ensures that the implemented process is relevant
to the problems being addressed. Timeframe helps in the timely execution of steps and
ensures they are bound to a given timeframe (McLeod 2012). The SMART goal settings help
the patients. It provides a patient cantered model for care (Evans et al. 2015). Additionally,
ICP can also help to ensure proper follow-up with patients outside healthcare facilities
(Smith-Strøm et al. 2016; Evans et al. 2015). Studies by Malakouti et al. (2015) suggested
that integrating suicide prevention program in primary care program can also help to maintain
a better depression and suicide surveillance, and therefore in better identification of patients
at risk of committing suicide. Hogan and Gurmet (2016) also supported such a suggestion,
mentioning that such can integration can improve mental healthcare of suicidal patients. They
pointed out that isolation can increase the risks of suicide, and therefore timely and routine
supportive contact (through calls, letters, texts and visits) can be implemented after acute care
visits or during interruptions in healthcare service (like for patients on home leave). The
studies show that the risks of suicide attempt is the highest in the first month after discharge
and that 70% of patients discharged from Emergency Department after a suicide attempt
never actually attend their first follow-up visit (Knesper 2011; Luxton, June and Comtois
2013).
SMART criteria can help in the identification of objectives in the implementation of a
change. Each letter represents different aspects of the objective, like Specificity,
Measurability, Achievability, Relevance and Timeframe (Haughey 2018). MacLeod
(2012) explained each of these aspects, which shall be explained briefly next.
Specificity of the objectives helps in a clear identification of the proposed actions, and
leaves little scope for misunderstanding or misinterpretation. Measurability helps in the
quantification of the objectives and the extent of the achievements can be measured.
Achievability helps to understand if the recommended steps are reasonably achievable, and
maintain practicality of the steps. Relevancy ensures that the implemented process is relevant
to the problems being addressed. Timeframe helps in the timely execution of steps and
ensures they are bound to a given timeframe (McLeod 2012). The SMART goal settings help
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





