Health Initiative: Obesity Prevention Program with Clinical Governance
VerifiedAdded on 2023/04/21
|14
|3383
|96
Project
AI Summary
This health project initiative details a comprehensive health promotion program designed for obesity prevention among adults, particularly targeting university students. The program utilizes the Plan-Do-Study-Act (PDSA) cycle for implementation and continuous improvement, emphasizing clinical governance and risk management strategies to ensure program feasibility and effectiveness. The plan includes statistical evidence, target audience selection, program outline with workout sessions and diet plans, implementation using the PDSA cycle, and identification and management of risks through clinical governance. Effective leadership styles are also discussed to ensure the success of the project and improve patient outcomes. Data collection and analysis methods are outlined to evaluate the program's success, focusing on changes in body weight and BMI, as well as feedback from participants. The project aims to create a sustainable and impactful health initiative that promotes healthy living and reduces the prevalence of obesity.

Running head: HEALTH PROMOTION
OBESITY PREVENETION AND HEALTH PROMOTION
Name of the Student:
Name of the University:
Author Note:
OBESITY PREVENETION AND HEALTH PROMOTION
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH PROMOTION
Introduction:
According to Foundation (2019), obesity can be defines as a complex disorder
characterized by the accumulation of excessive fat within the body. Obesity is not restricted to a
cosmetic concern but increases the risk of developing multiple health problems such as Diabetes,
Hypertension and Cardiovascular disorders. As mentioned by the World Health Organization
(2019), from among the English-speaking nations, Australia has the third highest prevalence of
overweight and obese adults. It has also been estimated that obesity in Australia is a serious
concern and is emerging as an epidemic with an increasing frequency. In addition to this,
research studies have predicted that the prevalence of obesity in Australia has almost doubled
since the last decade. Obesity is caused by the interplay of genetic, hormonal and behavioral
influences on the body weight of individuals (Frood et al., 2013). An individual is said to turn
obese only when the intake of calories exceeds the amount of calorie burnt through rigorous
exercise or other activities of daily living. According to Buchmueller and Johar (2015), the major
reasons that lead to obesity include unhealthy diet and eating habits, lack of physical activity and
a sedentary lifestyle.
According to a report published by Grima and Dixon (2013), six million Australians aged
18 and above were reported to be overweight with the Basal Metabolism Index (BMI) being in
between 25.0kg/m2 to 29.9kg/m2. The recorded prevalence accounted for a total of 36% of the
Australian adults (Grima & Dixon, 2013; Lehnert et al., 2013). Further, 3.5 million Australian
men aged 18 and above were reported to be overweight against 2.5 million Australian women
belonging to the similar age group (Tanamas, 2013). Therefore, this paper intends to develop a
health promotion program for the prevention of obesity and promotion of healthy living among
obese adults.
Introduction:
According to Foundation (2019), obesity can be defines as a complex disorder
characterized by the accumulation of excessive fat within the body. Obesity is not restricted to a
cosmetic concern but increases the risk of developing multiple health problems such as Diabetes,
Hypertension and Cardiovascular disorders. As mentioned by the World Health Organization
(2019), from among the English-speaking nations, Australia has the third highest prevalence of
overweight and obese adults. It has also been estimated that obesity in Australia is a serious
concern and is emerging as an epidemic with an increasing frequency. In addition to this,
research studies have predicted that the prevalence of obesity in Australia has almost doubled
since the last decade. Obesity is caused by the interplay of genetic, hormonal and behavioral
influences on the body weight of individuals (Frood et al., 2013). An individual is said to turn
obese only when the intake of calories exceeds the amount of calorie burnt through rigorous
exercise or other activities of daily living. According to Buchmueller and Johar (2015), the major
reasons that lead to obesity include unhealthy diet and eating habits, lack of physical activity and
a sedentary lifestyle.
According to a report published by Grima and Dixon (2013), six million Australians aged
18 and above were reported to be overweight with the Basal Metabolism Index (BMI) being in
between 25.0kg/m2 to 29.9kg/m2. The recorded prevalence accounted for a total of 36% of the
Australian adults (Grima & Dixon, 2013; Lehnert et al., 2013). Further, 3.5 million Australian
men aged 18 and above were reported to be overweight against 2.5 million Australian women
belonging to the similar age group (Tanamas, 2013). Therefore, this paper intends to develop a
health promotion program for the prevention of obesity and promotion of healthy living among
obese adults.
2HEALTH PROMOTION
Outline of the plan:
Statistical evidence suggests that the prevalence of obesity in Victoria is equivalent to
63.3% (Tanamas, 2013). Also, the prevalence has been reported to be higher in adults aged 18
years and above. Therefore, the target audience for the health promotion program would be
individuals aged between 18 to 25 years (Buchmueller & Johar, 2015). Individuals belonging to
the targeted age group are mostly students. Therefore, the health promotion program would be
conducted at the University of Victoria. The promotion program would take place inside the
university campus and would extend for 6 weeks. Prior to the commencement of the program,
approval would be obtained from the concerned university authorities. After obtaining the
approval, the details about the promotion program would be published in the official website of
the university and circulated on social media so as to draw the attention of the students.
Interested students would be requested to mail their personal details to the registration desk. The
registration for the first batch would be closed after obtaining 10 responses and the students
would then be contacted personally through email to attend the program. The program would
typically comprise of assisting the students with weight loss through work out sessions, diet
plans (Dietz et al., 2015). For students who are morbidly obese, the program would offer
information about bariatric surgery and other medical assistance that could help in losing weight
(Williams et al., 2015). In addition to this, the program would also disseminate awareness among
the students about the health related risk factors that are triggered by obesity. After the
completion of the program, the participants would be required to fill out a survey feedback form.
The responses would be analyzed to determine the success of the program. Also, on the day of
commencement, the body weight and the BMI of the participants would be documented and the
participants would be asked to document their desired ‘ideal weight’. On the day of completion
Outline of the plan:
Statistical evidence suggests that the prevalence of obesity in Victoria is equivalent to
63.3% (Tanamas, 2013). Also, the prevalence has been reported to be higher in adults aged 18
years and above. Therefore, the target audience for the health promotion program would be
individuals aged between 18 to 25 years (Buchmueller & Johar, 2015). Individuals belonging to
the targeted age group are mostly students. Therefore, the health promotion program would be
conducted at the University of Victoria. The promotion program would take place inside the
university campus and would extend for 6 weeks. Prior to the commencement of the program,
approval would be obtained from the concerned university authorities. After obtaining the
approval, the details about the promotion program would be published in the official website of
the university and circulated on social media so as to draw the attention of the students.
Interested students would be requested to mail their personal details to the registration desk. The
registration for the first batch would be closed after obtaining 10 responses and the students
would then be contacted personally through email to attend the program. The program would
typically comprise of assisting the students with weight loss through work out sessions, diet
plans (Dietz et al., 2015). For students who are morbidly obese, the program would offer
information about bariatric surgery and other medical assistance that could help in losing weight
(Williams et al., 2015). In addition to this, the program would also disseminate awareness among
the students about the health related risk factors that are triggered by obesity. After the
completion of the program, the participants would be required to fill out a survey feedback form.
The responses would be analyzed to determine the success of the program. Also, on the day of
commencement, the body weight and the BMI of the participants would be documented and the
participants would be asked to document their desired ‘ideal weight’. On the day of completion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH PROMOTION
of the program, the body weight and BMI would again be calculated and compared to the ‘ideal
weight’ mentioned by the participant on the first day to analyze the effectiveness of the program.
Implementation using the PDSA cycle:
According to Donnelly and Kirk (2015), the PDSA cycle or the Plan-Do-Act cycle is an
integral improvement model that helps in rendering continuous quality improvement during the
process of implementing a health promotion program. On setting the aim and objectives of the
program and after finalizing the membership committee, it is important to develop improvement
strategies so as to ensure that whether or not the planned change could bring out a positive effect.
The next step comprises of testing the outcome of the implemented strategies. The PDSA cycle
therefore covers the process of planning a change, implementing the change, observing the
results and then reflecting upon the process (Leis & Shojania, 2017).
In this section the implementation of the obesity program would be mentioned in detail in
compliance with the PDSA framework.
Step 1: Plan:
This stage would comprise of planning the health promotion program and selecting the
appropriate data collection plan for collecting the data. In this context, it should be noted that the
planning stage would extend over two phases. The first phase would comprise of finalizing the
target population and the venue where the health promotion program was to be conducted. The
second stage would comprise of developing an outline of the program and planning the activities
that would be covered in the program. In addition to this, the body weight and the BMI would be
considered as the parameters for data collection. Three teams would be created with 7 members
in total. The first team would comprise of two student volunteers who would be responsible for
of the program, the body weight and BMI would again be calculated and compared to the ‘ideal
weight’ mentioned by the participant on the first day to analyze the effectiveness of the program.
Implementation using the PDSA cycle:
According to Donnelly and Kirk (2015), the PDSA cycle or the Plan-Do-Act cycle is an
integral improvement model that helps in rendering continuous quality improvement during the
process of implementing a health promotion program. On setting the aim and objectives of the
program and after finalizing the membership committee, it is important to develop improvement
strategies so as to ensure that whether or not the planned change could bring out a positive effect.
The next step comprises of testing the outcome of the implemented strategies. The PDSA cycle
therefore covers the process of planning a change, implementing the change, observing the
results and then reflecting upon the process (Leis & Shojania, 2017).
In this section the implementation of the obesity program would be mentioned in detail in
compliance with the PDSA framework.
Step 1: Plan:
This stage would comprise of planning the health promotion program and selecting the
appropriate data collection plan for collecting the data. In this context, it should be noted that the
planning stage would extend over two phases. The first phase would comprise of finalizing the
target population and the venue where the health promotion program was to be conducted. The
second stage would comprise of developing an outline of the program and planning the activities
that would be covered in the program. In addition to this, the body weight and the BMI would be
considered as the parameters for data collection. Three teams would be created with 7 members
in total. The first team would comprise of two student volunteers who would be responsible for
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTH PROMOTION
the registration process. The second team would comprise of a community nurse, a fitness expert
and a dietician who would be responsible for conducting the wellness sessions. The third team
would comprise of the researcher and a volunteer who would be responsible for data collection,
documentation and data analysis.
The data collection procedure is to be conducted in two phases the first included the
documentation of the body weight and BMI of the patient on the day of commencement of the
program. The second would include the collection of the collection of the survey feedback form
from the participants after the collection of the program. On the day of the commencement of the
program, the participants would need to mention their ‘desired’ ideal weight and on the final day,
the body weight and BMI would be compared with the initial figure to calculate the success
ratio. Also, the survey feedback collected would be analyzed using statistical analysis to
determine the success rate of the program.
Step 2: DO:
This step covers the implementation of the planned health promotion program. The
PDSA framework suggests that the program must first be tested on a small sample. This accounts
for the rationale why it was decided that the program would not include more than 10
participants. On the first day of the program, the community nurse would document the body
weight and calculate the BMI of the participants. Then each participant would be asked to
mention their desired ‘ideal weight’ which would be documented. Through the weeks that follow
the participants would be trained on fitness exercises by the fitness expert and would also be
offered customized diet plans by the nutritionist. In addition to this, the community nurse would
conduct sessions where the negative effect of obesity on physical health would be discussed. The
the registration process. The second team would comprise of a community nurse, a fitness expert
and a dietician who would be responsible for conducting the wellness sessions. The third team
would comprise of the researcher and a volunteer who would be responsible for data collection,
documentation and data analysis.
The data collection procedure is to be conducted in two phases the first included the
documentation of the body weight and BMI of the patient on the day of commencement of the
program. The second would include the collection of the collection of the survey feedback form
from the participants after the collection of the program. On the day of the commencement of the
program, the participants would need to mention their ‘desired’ ideal weight and on the final day,
the body weight and BMI would be compared with the initial figure to calculate the success
ratio. Also, the survey feedback collected would be analyzed using statistical analysis to
determine the success rate of the program.
Step 2: DO:
This step covers the implementation of the planned health promotion program. The
PDSA framework suggests that the program must first be tested on a small sample. This accounts
for the rationale why it was decided that the program would not include more than 10
participants. On the first day of the program, the community nurse would document the body
weight and calculate the BMI of the participants. Then each participant would be asked to
mention their desired ‘ideal weight’ which would be documented. Through the weeks that follow
the participants would be trained on fitness exercises by the fitness expert and would also be
offered customized diet plans by the nutritionist. In addition to this, the community nurse would
conduct sessions where the negative effect of obesity on physical health would be discussed. The
5HEALTH PROMOTION
fitness expert would also conduct motivation sessions so as to ensure that the participants
continue with the program and do not quit the program mid-way. Also, the participants would be
assisted with the help of web-based applications that would help them keep a track of their diet
and physical activity throughout the day. On the final day of the program, the body weight of the
participants would be measured again and their BMI would be calculated.
Step 3: Study
This step includes the data analyses to evaluate the result and findings. This step would
take place on completion of the program at the end of the sixth week. This step would
exclusively involve analysis of the documented body weight and BMI calculation to evaluate the
difference in body weight of the participants. In addition to this, this stage would also involve the
data collection of the survey response forms. It can be expected that the wellness program would
help in fostering weight loss up to 5 kg among the 10 participants.
Step 4: Act
The analysis would be done with the help of statistical analysis using the SPSS software.
This step would require another 1 week for completion and the findings would help in
concluding the success rate of the health promotion program. It should be noted in this context,
that the data analysis step would be carried out by the researcher and the research volunteer
exclusively in this step to determine the effectiveness of the promotion program.
fitness expert would also conduct motivation sessions so as to ensure that the participants
continue with the program and do not quit the program mid-way. Also, the participants would be
assisted with the help of web-based applications that would help them keep a track of their diet
and physical activity throughout the day. On the final day of the program, the body weight of the
participants would be measured again and their BMI would be calculated.
Step 3: Study
This step includes the data analyses to evaluate the result and findings. This step would
take place on completion of the program at the end of the sixth week. This step would
exclusively involve analysis of the documented body weight and BMI calculation to evaluate the
difference in body weight of the participants. In addition to this, this stage would also involve the
data collection of the survey response forms. It can be expected that the wellness program would
help in fostering weight loss up to 5 kg among the 10 participants.
Step 4: Act
The analysis would be done with the help of statistical analysis using the SPSS software.
This step would require another 1 week for completion and the findings would help in
concluding the success rate of the health promotion program. It should be noted in this context,
that the data analysis step would be carried out by the researcher and the research volunteer
exclusively in this step to determine the effectiveness of the promotion program.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTH PROMOTION
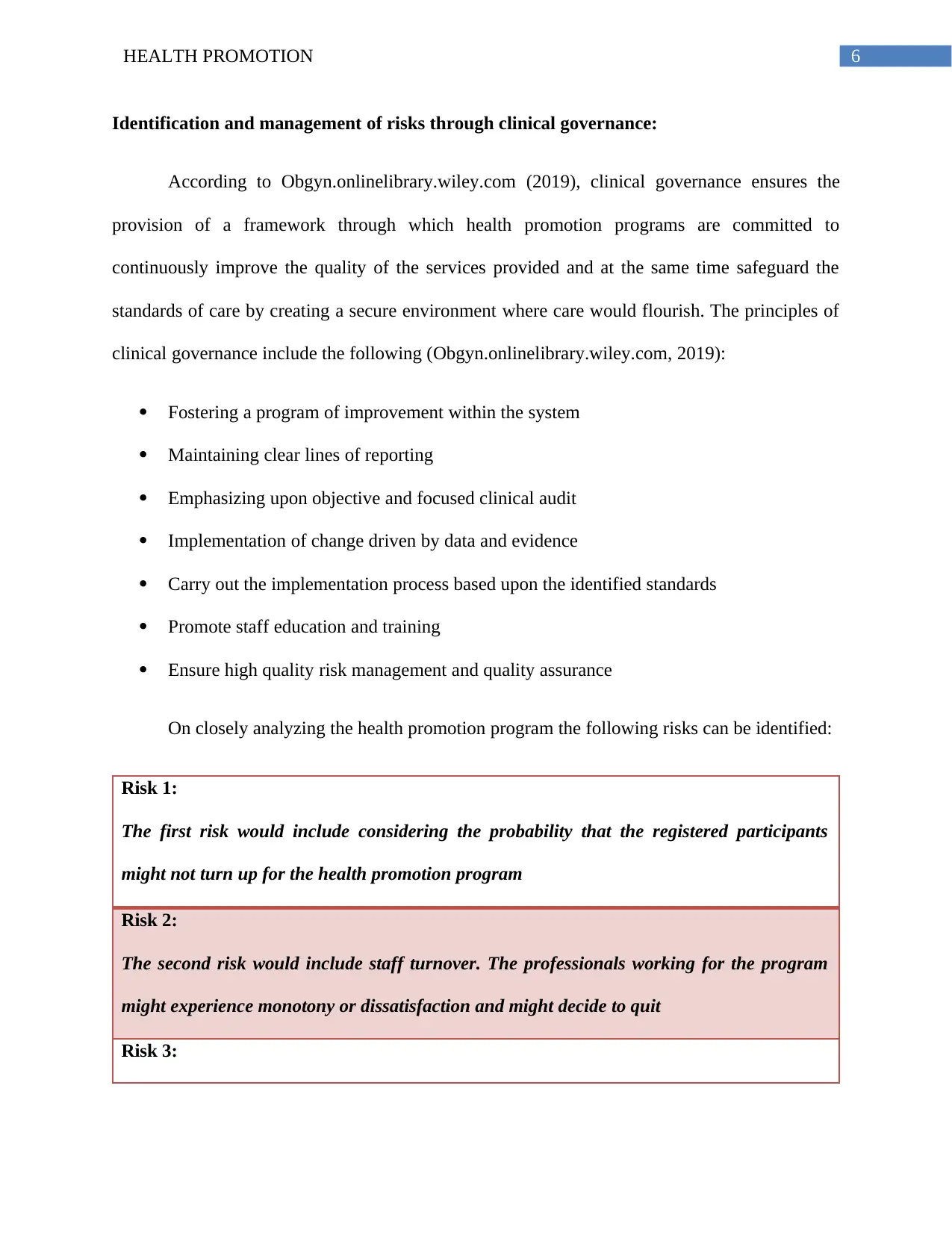
Identification and management of risks through clinical governance:
According to Obgyn.onlinelibrary.wiley.com (2019), clinical governance ensures the
provision of a framework through which health promotion programs are committed to
continuously improve the quality of the services provided and at the same time safeguard the
standards of care by creating a secure environment where care would flourish. The principles of
clinical governance include the following (Obgyn.onlinelibrary.wiley.com, 2019):
Fostering a program of improvement within the system
Maintaining clear lines of reporting
Emphasizing upon objective and focused clinical audit
Implementation of change driven by data and evidence
Carry out the implementation process based upon the identified standards
Promote staff education and training
Ensure high quality risk management and quality assurance
On closely analyzing the health promotion program the following risks can be identified:
Risk 1:
The first risk would include considering the probability that the registered participants
might not turn up for the health promotion program
Risk 2:
The second risk would include staff turnover. The professionals working for the program
might experience monotony or dissatisfaction and might decide to quit
Risk 3:
Identification and management of risks through clinical governance:
According to Obgyn.onlinelibrary.wiley.com (2019), clinical governance ensures the
provision of a framework through which health promotion programs are committed to
continuously improve the quality of the services provided and at the same time safeguard the
standards of care by creating a secure environment where care would flourish. The principles of
clinical governance include the following (Obgyn.onlinelibrary.wiley.com, 2019):
Fostering a program of improvement within the system
Maintaining clear lines of reporting
Emphasizing upon objective and focused clinical audit
Implementation of change driven by data and evidence
Carry out the implementation process based upon the identified standards
Promote staff education and training
Ensure high quality risk management and quality assurance
On closely analyzing the health promotion program the following risks can be identified:
Risk 1:
The first risk would include considering the probability that the registered participants
might not turn up for the health promotion program
Risk 2:
The second risk would include staff turnover. The professionals working for the program
might experience monotony or dissatisfaction and might decide to quit
Risk 3:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH PROMOTION
The third risk would comprise of considering the possibility that the planned budget for the
program might not be sufficient to address the smart objectives of the program
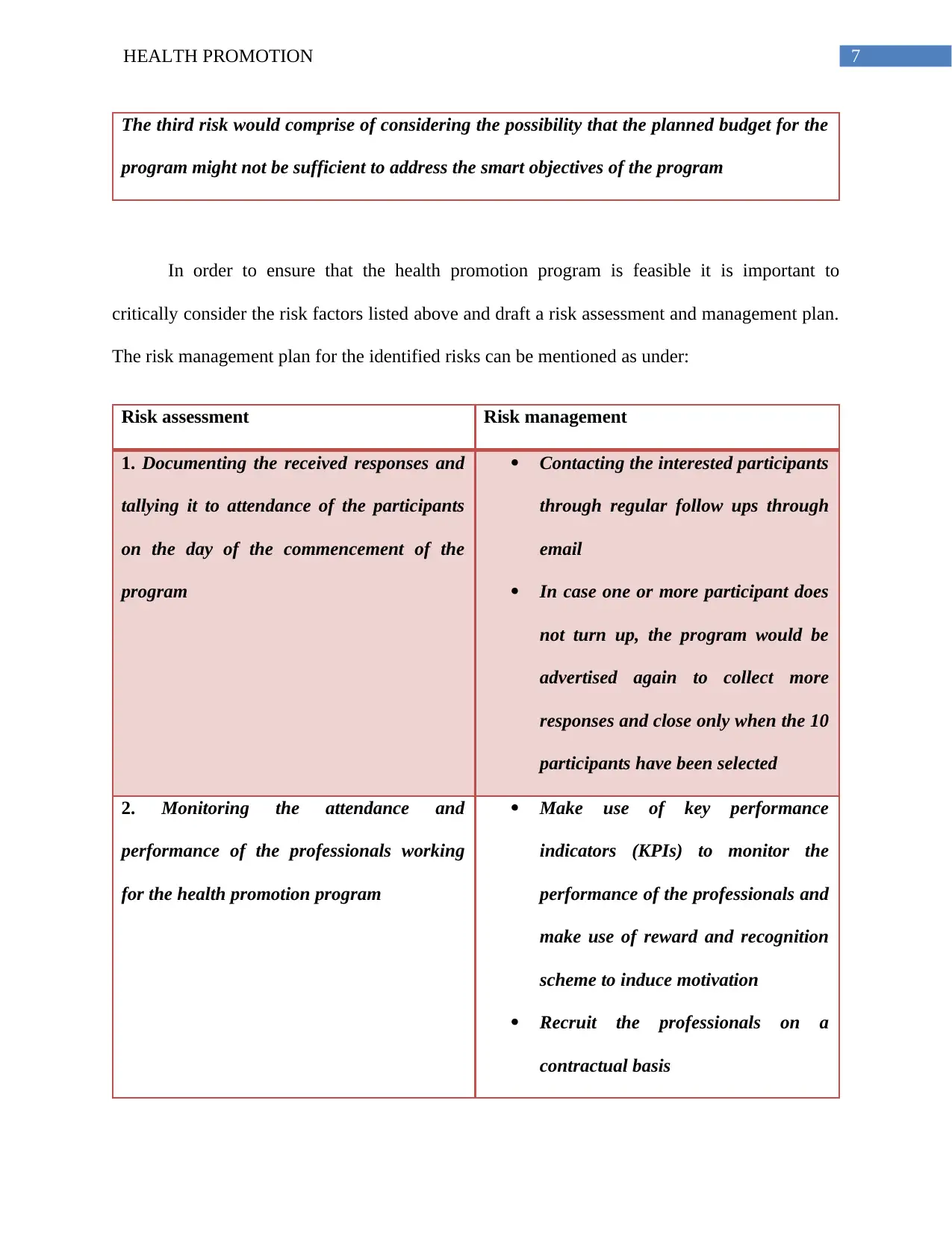
In order to ensure that the health promotion program is feasible it is important to
critically consider the risk factors listed above and draft a risk assessment and management plan.
The risk management plan for the identified risks can be mentioned as under:
Risk assessment Risk management
1. Documenting the received responses and
tallying it to attendance of the participants
on the day of the commencement of the
program
Contacting the interested participants
through regular follow ups through
email
In case one or more participant does
not turn up, the program would be
advertised again to collect more
responses and close only when the 10
participants have been selected
2. Monitoring the attendance and
performance of the professionals working
for the health promotion program
Make use of key performance
indicators (KPIs) to monitor the
performance of the professionals and
make use of reward and recognition
scheme to induce motivation
Recruit the professionals on a
contractual basis
The third risk would comprise of considering the possibility that the planned budget for the
program might not be sufficient to address the smart objectives of the program
In order to ensure that the health promotion program is feasible it is important to
critically consider the risk factors listed above and draft a risk assessment and management plan.
The risk management plan for the identified risks can be mentioned as under:
Risk assessment Risk management
1. Documenting the received responses and
tallying it to attendance of the participants
on the day of the commencement of the
program
Contacting the interested participants
through regular follow ups through
In case one or more participant does
not turn up, the program would be
advertised again to collect more
responses and close only when the 10
participants have been selected
2. Monitoring the attendance and
performance of the professionals working
for the health promotion program
Make use of key performance
indicators (KPIs) to monitor the
performance of the professionals and
make use of reward and recognition
scheme to induce motivation
Recruit the professionals on a
contractual basis
8HEALTH PROMOTION
3. Planning and evaluation of the program
budget at every stage
Effectively planning the budget while
considering overhead surcharges
Maintaining account audit of the
planned program budget so as to
ensure stable expenditure
Discussion on the leadership style followed:
Studies suggest that the type of leadership style adapted to direct a program largely
determines its success rate (Dumdum et al., 2013; McCleskey, 2014). It is extremely important to
make use of an effective leadership style that is aligned to the set objectives of the program. An
effective leadership style helps in maintaining a smooth flow of communication that makes the
flow of work easier and at the same time also helps in preventing unwanted conflicts that could
hamper the progress of the team. The team leader is essentially responsible for monitoring the
performance output of the team members and at the same time induces motivation among the
team members to acquire maximum performance output.
In this case, the leadership style that would be adapted by the project leader would
include the transactional style of leadership. It is important to note here that the project leader or
the coordinator would be the researcher who would plan the outline of the program. In this
context, it should be mentioned that the transactional leadership is based upon making use of
rewards and punishments to ensure compliance by the followers or the team of professionals who
would be responsible for managing the program (McCleskey, 2014). As has already been
mentioned, the program would comprise a total of three teams with 7 professionals working for
3. Planning and evaluation of the program
budget at every stage
Effectively planning the budget while
considering overhead surcharges
Maintaining account audit of the
planned program budget so as to
ensure stable expenditure
Discussion on the leadership style followed:
Studies suggest that the type of leadership style adapted to direct a program largely
determines its success rate (Dumdum et al., 2013; McCleskey, 2014). It is extremely important to
make use of an effective leadership style that is aligned to the set objectives of the program. An
effective leadership style helps in maintaining a smooth flow of communication that makes the
flow of work easier and at the same time also helps in preventing unwanted conflicts that could
hamper the progress of the team. The team leader is essentially responsible for monitoring the
performance output of the team members and at the same time induces motivation among the
team members to acquire maximum performance output.
In this case, the leadership style that would be adapted by the project leader would
include the transactional style of leadership. It is important to note here that the project leader or
the coordinator would be the researcher who would plan the outline of the program. In this
context, it should be mentioned that the transactional leadership is based upon making use of
rewards and punishments to ensure compliance by the followers or the team of professionals who
would be responsible for managing the program (McCleskey, 2014). As has already been
mentioned, the program would comprise a total of three teams with 7 professionals working for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTH PROMOTION
the program. The performance of the professionals would be stringently monitored by the project
coordinator with the use of key performance indicator tools. Professionals actively complying
with the objectives and delivering excellent performance would be rewarded in the form of
incentives after the completion of the program. On the other hand, professionals not complying
with the instructions, taking unplanned leaves or performing poorly would be penalized in the
form of deduction in their total reimbursement. The rationale for the choice of transactional
leadership to conduct the project can be explained as the short tenure of the program with
minimal participants. Studies mention that the use of transactional form of leadership can
effectively help in managing short term projects that are goal specific. In addition to this, the
transactional form of leadership also helps in inducing motivation among employees that
facilitates retention.
Conclusion:
Therefore, to conclude, it can be mentioned that the health promotion program would
focus on obesity prevention among young Australian adults. On the basis of the research studies
and statistical report, it was found that the prevalence of obesity was higher in young adults who
belonged to the age group of 18 to 25 years of age. Individuals belonging to the mentioned age
group were mostly students and that accounted for the reason why the health promotion program
was conducted in a university campus. Further, the program was conducted within the campus of
Victoria University because the prevalence percentage of obesity was reported to be higher in
Victoria. The implementation of the health promotion program was largely based upon the
PDSA framework of the Plan, Do, Study and Act guideline. Advertisement about the health
promotion program would be circulated on social media and the official university site.
Individuals showing interest would be contacted personally through email for registration. A
the program. The performance of the professionals would be stringently monitored by the project
coordinator with the use of key performance indicator tools. Professionals actively complying
with the objectives and delivering excellent performance would be rewarded in the form of
incentives after the completion of the program. On the other hand, professionals not complying
with the instructions, taking unplanned leaves or performing poorly would be penalized in the
form of deduction in their total reimbursement. The rationale for the choice of transactional
leadership to conduct the project can be explained as the short tenure of the program with
minimal participants. Studies mention that the use of transactional form of leadership can
effectively help in managing short term projects that are goal specific. In addition to this, the
transactional form of leadership also helps in inducing motivation among employees that
facilitates retention.
Conclusion:
Therefore, to conclude, it can be mentioned that the health promotion program would
focus on obesity prevention among young Australian adults. On the basis of the research studies
and statistical report, it was found that the prevalence of obesity was higher in young adults who
belonged to the age group of 18 to 25 years of age. Individuals belonging to the mentioned age
group were mostly students and that accounted for the reason why the health promotion program
was conducted in a university campus. Further, the program was conducted within the campus of
Victoria University because the prevalence percentage of obesity was reported to be higher in
Victoria. The implementation of the health promotion program was largely based upon the
PDSA framework of the Plan, Do, Study and Act guideline. Advertisement about the health
promotion program would be circulated on social media and the official university site.
Individuals showing interest would be contacted personally through email for registration. A
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HEALTH PROMOTION
total of 10 participants would be considered for the program. The program would be majorly
headed by the community nurse, fitness expert and the nutritionist. The participants would be
assisted with customized diet plan, awareness about obesity and its implication on health and
training on physical exercises that could help in losing weight. On completion of the program,
the participants would be asked to fill out a survey feedback form, which would be analyzed to
determine the success of the campaign.
total of 10 participants would be considered for the program. The program would be majorly
headed by the community nurse, fitness expert and the nutritionist. The participants would be
assisted with customized diet plan, awareness about obesity and its implication on health and
training on physical exercises that could help in losing weight. On completion of the program,
the participants would be asked to fill out a survey feedback form, which would be analyzed to
determine the success of the campaign.
11HEALTH PROMOTION
References:
Buchmueller, T. C., & Johar, M. (2015). Obesity and health expenditures: evidence from
Australia. Economics & Human Biology, 17, 42-58. DOI:
https://doi.org/10.1016/j.ehb.2015.01.001
Dietz, W. H., Baur, L. A., Hall, K., Puhl, R. M., Taveras, E. M., Uauy, R., & Kopelman, P.
(2015). Management of obesity: improvement of health-care training and systems for
prevention and care. The Lancet, 385(9986), 2521-2533. DOI:
https://doi.org/10.1016/S0140-6736(14)61748-7
Donnelly, P., & Kirk, P. (2015). Use the PDSA model for effective change
management. Education for Primary Care, 26(4), 279-281. DOI:
https://doi.org/10.1080/14739879.2015.11494356
Dumdum, U. R., Lowe, K. B., & Avolio, B. J. (2013). A meta-analysis of transformational and
transactional leadership correlates of effectiveness and satisfaction: An update and
extension. In Transformational and Charismatic Leadership: The Road Ahead 10th
Anniversary Edition (pp. 39-70). Emerald Group Publishing Limited. Retrieved from:
https://www.emeraldinsight.com/doi/abs/10.1108/S1479-357120130000005008
Foundation, T. (2019). Overweight and obesity statistics. [online] The Heart Foundation.
Available at: https://www.heartfoundation.org.au/about-us/what-we-do/heart-disease-in-
australia/overweight-and-obesity-statistics [Accessed 29 Mar. 2019].
Frood, S., Johnston, L. M., Matteson, C. L., & Finegood, D. T. (2013). Obesity, complexity, and
the role of the health system. Current obesity reports, 2(4), 320-326. DOI:
https://doi.org/10.1007/s13679-013-0072-9
References:
Buchmueller, T. C., & Johar, M. (2015). Obesity and health expenditures: evidence from
Australia. Economics & Human Biology, 17, 42-58. DOI:
https://doi.org/10.1016/j.ehb.2015.01.001
Dietz, W. H., Baur, L. A., Hall, K., Puhl, R. M., Taveras, E. M., Uauy, R., & Kopelman, P.
(2015). Management of obesity: improvement of health-care training and systems for
prevention and care. The Lancet, 385(9986), 2521-2533. DOI:
https://doi.org/10.1016/S0140-6736(14)61748-7
Donnelly, P., & Kirk, P. (2015). Use the PDSA model for effective change
management. Education for Primary Care, 26(4), 279-281. DOI:
https://doi.org/10.1080/14739879.2015.11494356
Dumdum, U. R., Lowe, K. B., & Avolio, B. J. (2013). A meta-analysis of transformational and
transactional leadership correlates of effectiveness and satisfaction: An update and
extension. In Transformational and Charismatic Leadership: The Road Ahead 10th
Anniversary Edition (pp. 39-70). Emerald Group Publishing Limited. Retrieved from:
https://www.emeraldinsight.com/doi/abs/10.1108/S1479-357120130000005008
Foundation, T. (2019). Overweight and obesity statistics. [online] The Heart Foundation.
Available at: https://www.heartfoundation.org.au/about-us/what-we-do/heart-disease-in-
australia/overweight-and-obesity-statistics [Accessed 29 Mar. 2019].
Frood, S., Johnston, L. M., Matteson, C. L., & Finegood, D. T. (2013). Obesity, complexity, and
the role of the health system. Current obesity reports, 2(4), 320-326. DOI:
https://doi.org/10.1007/s13679-013-0072-9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





