Flinders University: Clinical Governance and Nursing Practices
VerifiedAdded on 2023/06/03
|11
|2586
|419
Report
AI Summary
This report delves into the multifaceted concept of clinical governance within healthcare, with a specific focus on infection control and its implications for nursing practices. The study begins by defining clinical governance and its role in enhancing accountability and improving service quality within healthcare institutions. It then examines the critical issue of healthcare-associated infections (HAIs), highlighting their financial and social burdens. The report explores the significance of nurses' behaviors and adherence to established policies in preventing HAIs, along with the importance of training, professional development, and incident reporting. A summary table provides an overview of three key research articles: one quantitative study, one qualitative study, and a systematic literature review. These articles investigate the infection prevention behaviors of nurses, control practices in critical care settings, and factors influencing infection control program implementation. The report synthesizes the findings of these studies, emphasizing the role of nurses, the importance of system-wide policies, and the need for effective surveillance and audit mechanisms to minimize the spread of infections. The conclusion underscores the need for continuous education, adherence to policies, and the acquisition of relevant skills to improve patient safety and outcomes.

Running head: CLINICAL GOVERNANCE 1
Clinical Governance
Name
Institution
Clinical Governance
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL GOVERNANCE 2
Clinical Governance
Introduction
Clinical governance is defined as the process through which healthcare institutions
enhance their levels of responsibility and accountability for pertinent organizational activities
such as enhancing the quality of the services offered, promoting high standards and instilling
systems aimed at fostering clinical outcomes that are above board through institutionalization of
operational environments that advocate for flourishing of excellence (Rowley, Clares, Poll,
Thomas, and White, 2017). The processes of controlling and preventing infections in healthcare
settings occupy a central position in clinical governance. According to Jackson, Lowton, and
Griffiths (2014), Europe incurred over €7 Billion as the healthcare costs associated with
infections acquired in hospital settings in 2011. However, Anderson et al. (2014) explain that
despite the policy frameworks put in place to minimize the financial, social and economic
burdens associated with the infections that are acquired by patients seeking services, the
contributions made by caregivers is still minimal. The scholars reveal that while nurses in acute
care settings raise their levels of concern on ensuring that they stir other stakeholders’ intuitions
to be considered as good and knowledgeable professionals, minimal efforts have been adopted to
ensure that the policies and procedures guiding their endeavors are followed. The caregivers
inculcate their own behavioral positions and justifications for all forms of irrational deviations
from the set institutional policies; an aspect that limits the effectiveness of applying the
principles of clinical governance. On the other hand, AL-Rawajfah (2016) reveals that while
healthcare associated infections have been considered as major challenges in critical hospital
sections such as the intensive care units, they can be controlled through acquisition of effective
frameworks aimed at educating caregivers on the most effective practices. In their study, Lo et
Clinical Governance
Introduction
Clinical governance is defined as the process through which healthcare institutions
enhance their levels of responsibility and accountability for pertinent organizational activities
such as enhancing the quality of the services offered, promoting high standards and instilling
systems aimed at fostering clinical outcomes that are above board through institutionalization of
operational environments that advocate for flourishing of excellence (Rowley, Clares, Poll,
Thomas, and White, 2017). The processes of controlling and preventing infections in healthcare
settings occupy a central position in clinical governance. According to Jackson, Lowton, and
Griffiths (2014), Europe incurred over €7 Billion as the healthcare costs associated with
infections acquired in hospital settings in 2011. However, Anderson et al. (2014) explain that
despite the policy frameworks put in place to minimize the financial, social and economic
burdens associated with the infections that are acquired by patients seeking services, the
contributions made by caregivers is still minimal. The scholars reveal that while nurses in acute
care settings raise their levels of concern on ensuring that they stir other stakeholders’ intuitions
to be considered as good and knowledgeable professionals, minimal efforts have been adopted to
ensure that the policies and procedures guiding their endeavors are followed. The caregivers
inculcate their own behavioral positions and justifications for all forms of irrational deviations
from the set institutional policies; an aspect that limits the effectiveness of applying the
principles of clinical governance. On the other hand, AL-Rawajfah (2016) reveals that while
healthcare associated infections have been considered as major challenges in critical hospital
sections such as the intensive care units, they can be controlled through acquisition of effective
frameworks aimed at educating caregivers on the most effective practices. In their study, Lo et
CLINICAL GOVERNANCE 3
al. (2014) demystify that medical institutions can instill the measures of controlling and
preventing infections in hospital settings by adopting efficient collaborative frameworks with
infection control link nurses (ICLNs). In their perspective, the scholars demystify that ICLNs are
better placed to inculcate workplace trainings aimed at acquainting other caregivers with both
technical and psychological skills necessary to alleviate the infections reported in acute care
facilities.
According to Ocampo et al. (2017), clinical performance and evaluation by the use of
nursing care plans plays a significant role in auditing the efficacy, validity and reliability of
healthcare procedures such as identification of outcomes, diagnosis and implementation of the
treatment procedures put in place. On the other hand, Louh et al. (2017) explain that professional
development and management is a pillar of clinical governance aimed at advancing the
healthcare workforce through impartation of the necessary skills and knowledge. Similarly,
incident reporting is considered by Zingg et al. (2017) as an essential component of minimizing
clinical risks based on its effectiveness in identifying the areas of weakness and advancing
platforms on which learning will take place. Lastly, feedback in healthcare settings strengthens
consumer value through inclusion of avenues aimed at evaluating the quality of services offered
based on the clients’ viewpoints. According to Storr et al. (2017), proper implementation of
clinical governance in medical settings is associated with an increase in the quality of services
offered, overall outcomes in patient care, optimal performance and revenue generation.
Summary Table
Author/s (year)
Country
Aims
or
Purpose
Sample/ setting
or
Key stake-holders
Design/
methods
or
Main findings
or
Primary
Strengths and
limitations of the
paper
al. (2014) demystify that medical institutions can instill the measures of controlling and
preventing infections in hospital settings by adopting efficient collaborative frameworks with
infection control link nurses (ICLNs). In their perspective, the scholars demystify that ICLNs are
better placed to inculcate workplace trainings aimed at acquainting other caregivers with both
technical and psychological skills necessary to alleviate the infections reported in acute care
facilities.
According to Ocampo et al. (2017), clinical performance and evaluation by the use of
nursing care plans plays a significant role in auditing the efficacy, validity and reliability of
healthcare procedures such as identification of outcomes, diagnosis and implementation of the
treatment procedures put in place. On the other hand, Louh et al. (2017) explain that professional
development and management is a pillar of clinical governance aimed at advancing the
healthcare workforce through impartation of the necessary skills and knowledge. Similarly,
incident reporting is considered by Zingg et al. (2017) as an essential component of minimizing
clinical risks based on its effectiveness in identifying the areas of weakness and advancing
platforms on which learning will take place. Lastly, feedback in healthcare settings strengthens
consumer value through inclusion of avenues aimed at evaluating the quality of services offered
based on the clients’ viewpoints. According to Storr et al. (2017), proper implementation of
clinical governance in medical settings is associated with an increase in the quality of services
offered, overall outcomes in patient care, optimal performance and revenue generation.
Summary Table
Author/s (year)
Country
Aims
or
Purpose
Sample/ setting
or
Key stake-holders
Design/
methods
or
Main findings
or
Primary
Strengths and
limitations of the
paper
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL GOVERNANCE 4
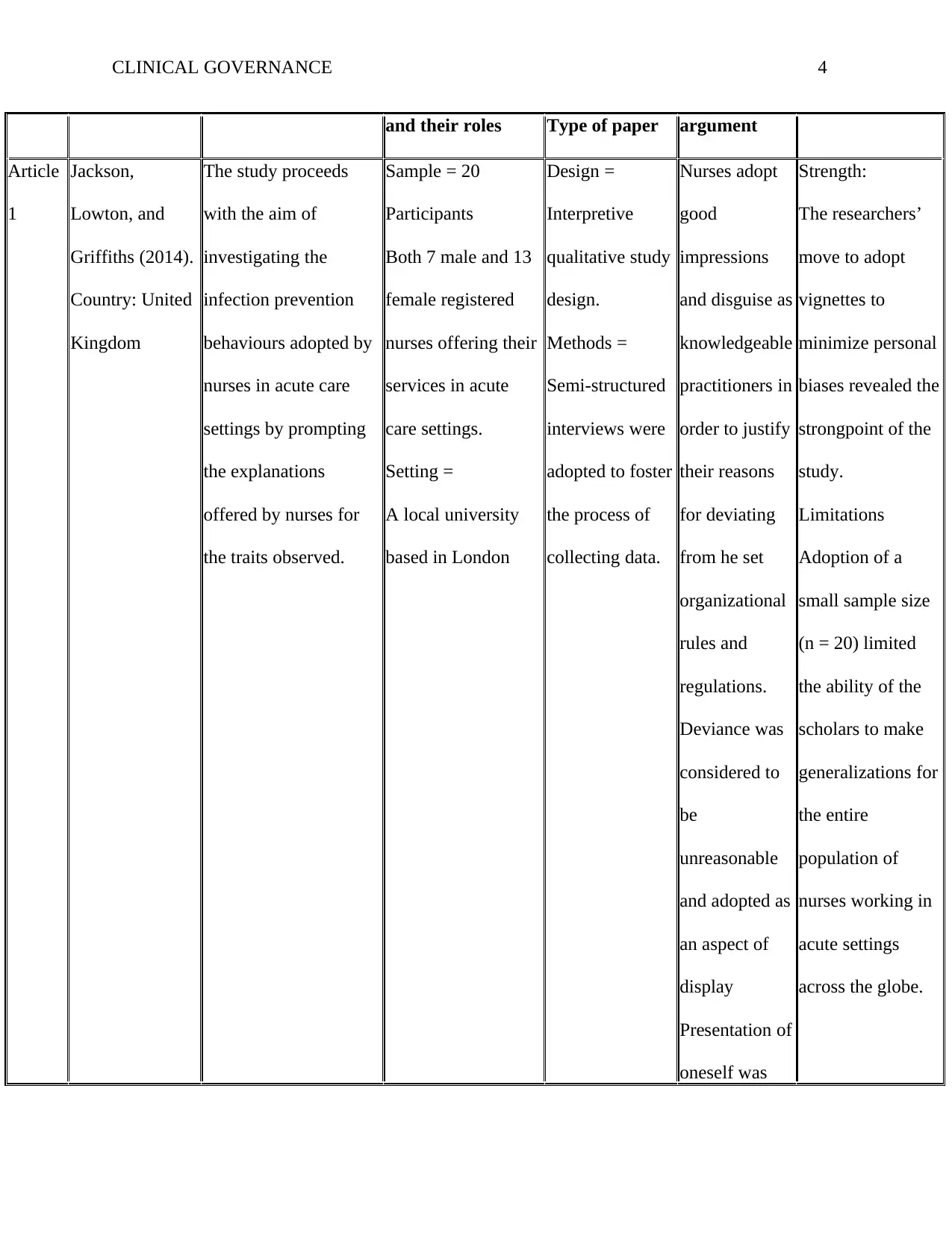
and their roles Type of paper argument
Article
1
Jackson,
Lowton, and
Griffiths (2014).
Country: United
Kingdom
The study proceeds
with the aim of
investigating the
infection prevention
behaviours adopted by
nurses in acute care
settings by prompting
the explanations
offered by nurses for
the traits observed.
Sample = 20
Participants
Both 7 male and 13
female registered
nurses offering their
services in acute
care settings.
Setting =
A local university
based in London
Design =
Interpretive
qualitative study
design.
Methods =
Semi-structured
interviews were
adopted to foster
the process of
collecting data.
Nurses adopt
good
impressions
and disguise as
knowledgeable
practitioners in
order to justify
their reasons
for deviating
from he set
organizational
rules and
regulations.
Deviance was
considered to
be
unreasonable
and adopted as
an aspect of
display
Presentation of
oneself was
Strength:
The researchers’
move to adopt
vignettes to
minimize personal
biases revealed the
strongpoint of the
study.
Limitations
Adoption of a
small sample size
(n = 20) limited
the ability of the
scholars to make
generalizations for
the entire
population of
nurses working in
acute settings
across the globe.
and their roles Type of paper argument
Article
1
Jackson,
Lowton, and
Griffiths (2014).
Country: United
Kingdom
The study proceeds
with the aim of
investigating the
infection prevention
behaviours adopted by
nurses in acute care
settings by prompting
the explanations
offered by nurses for
the traits observed.
Sample = 20
Participants
Both 7 male and 13
female registered
nurses offering their
services in acute
care settings.
Setting =
A local university
based in London
Design =
Interpretive
qualitative study
design.
Methods =
Semi-structured
interviews were
adopted to foster
the process of
collecting data.
Nurses adopt
good
impressions
and disguise as
knowledgeable
practitioners in
order to justify
their reasons
for deviating
from he set
organizational
rules and
regulations.
Deviance was
considered to
be
unreasonable
and adopted as
an aspect of
display
Presentation of
oneself was
Strength:
The researchers’
move to adopt
vignettes to
minimize personal
biases revealed the
strongpoint of the
study.
Limitations
Adoption of a
small sample size
(n = 20) limited
the ability of the
scholars to make
generalizations for
the entire
population of
nurses working in
acute settings
across the globe.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL GOVERNANCE 5
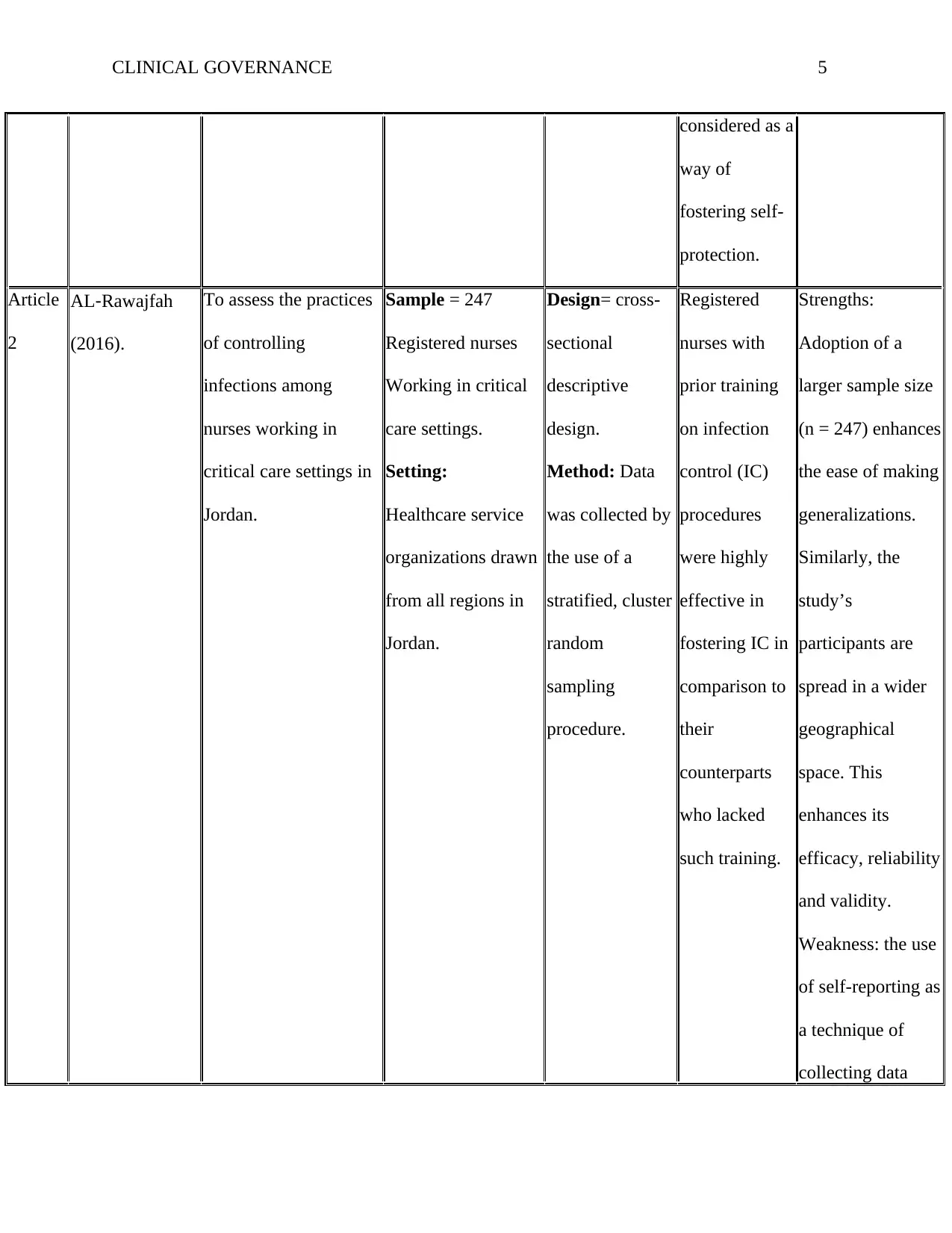
considered as a
way of
fostering self-
protection.
Article
2
AL‐Rawajfah
(2016).
To assess the practices
of controlling
infections among
nurses working in
critical care settings in
Jordan.
Sample = 247
Registered nurses
Working in critical
care settings.
Setting:
Healthcare service
organizations drawn
from all regions in
Jordan.
Design= cross-
sectional
descriptive
design.
Method: Data
was collected by
the use of a
stratified, cluster
random
sampling
procedure.
Registered
nurses with
prior training
on infection
control (IC)
procedures
were highly
effective in
fostering IC in
comparison to
their
counterparts
who lacked
such training.
Strengths:
Adoption of a
larger sample size
(n = 247) enhances
the ease of making
generalizations.
Similarly, the
study’s
participants are
spread in a wider
geographical
space. This
enhances its
efficacy, reliability
and validity.
Weakness: the use
of self-reporting as
a technique of
collecting data
considered as a
way of
fostering self-
protection.
Article
2
AL‐Rawajfah
(2016).
To assess the practices
of controlling
infections among
nurses working in
critical care settings in
Jordan.
Sample = 247
Registered nurses
Working in critical
care settings.
Setting:
Healthcare service
organizations drawn
from all regions in
Jordan.
Design= cross-
sectional
descriptive
design.
Method: Data
was collected by
the use of a
stratified, cluster
random
sampling
procedure.
Registered
nurses with
prior training
on infection
control (IC)
procedures
were highly
effective in
fostering IC in
comparison to
their
counterparts
who lacked
such training.
Strengths:
Adoption of a
larger sample size
(n = 247) enhances
the ease of making
generalizations.
Similarly, the
study’s
participants are
spread in a wider
geographical
space. This
enhances its
efficacy, reliability
and validity.
Weakness: the use
of self-reporting as
a technique of
collecting data
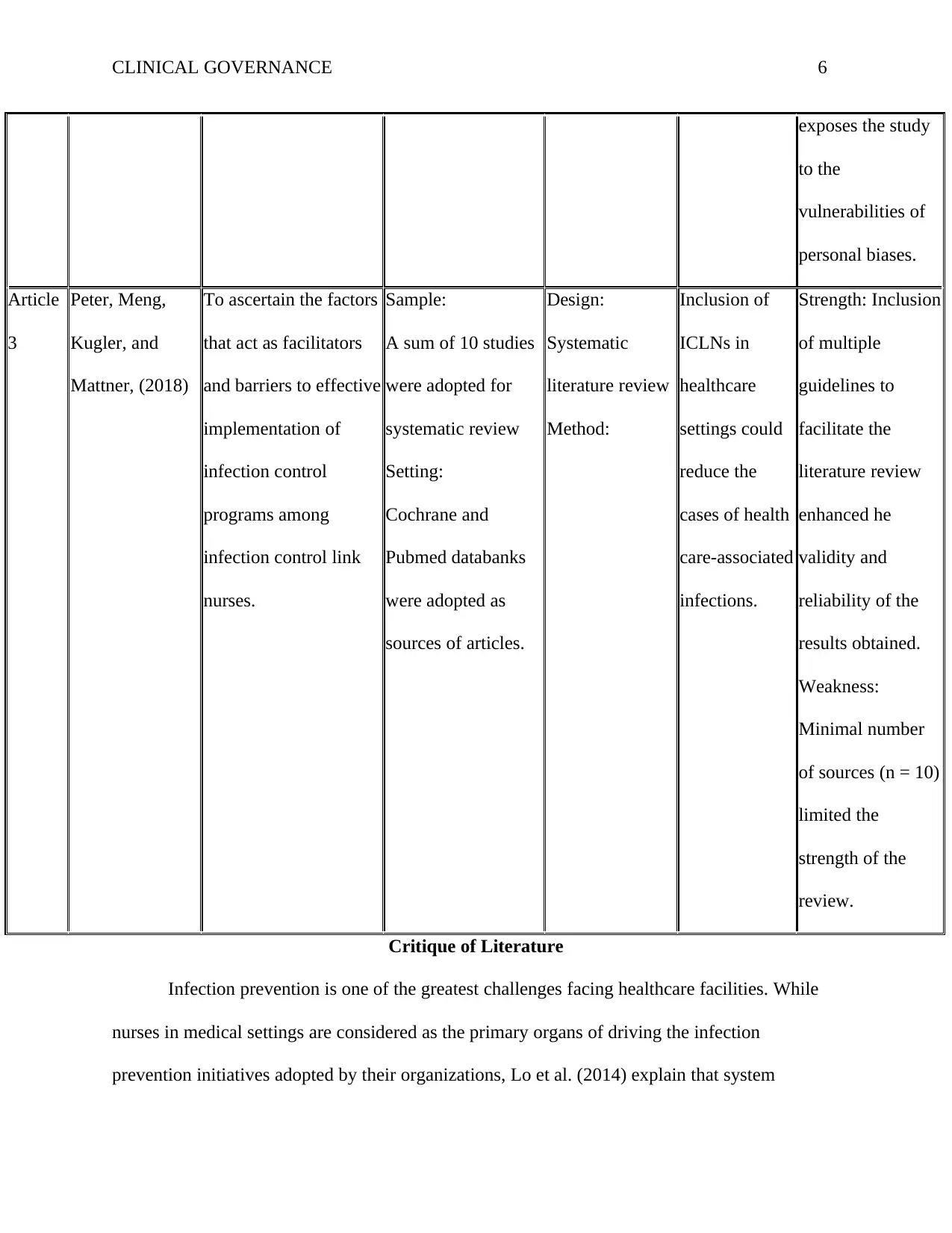
CLINICAL GOVERNANCE 6
exposes the study
to the
vulnerabilities of
personal biases.
Article
3
Peter, Meng,
Kugler, and
Mattner, (2018)
To ascertain the factors
that act as facilitators
and barriers to effective
implementation of
infection control
programs among
infection control link
nurses.
Sample:
A sum of 10 studies
were adopted for
systematic review
Setting:
Cochrane and
Pubmed databanks
were adopted as
sources of articles.
Design:
Systematic
literature review
Method:
Inclusion of
ICLNs in
healthcare
settings could
reduce the
cases of health
care-associated
infections.
Strength: Inclusion
of multiple
guidelines to
facilitate the
literature review
enhanced he
validity and
reliability of the
results obtained.
Weakness:
Minimal number
of sources (n = 10)
limited the
strength of the
review.
Critique of Literature
Infection prevention is one of the greatest challenges facing healthcare facilities. While
nurses in medical settings are considered as the primary organs of driving the infection
prevention initiatives adopted by their organizations, Lo et al. (2014) explain that system
exposes the study
to the
vulnerabilities of
personal biases.
Article
3
Peter, Meng,
Kugler, and
Mattner, (2018)
To ascertain the factors
that act as facilitators
and barriers to effective
implementation of
infection control
programs among
infection control link
nurses.
Sample:
A sum of 10 studies
were adopted for
systematic review
Setting:
Cochrane and
Pubmed databanks
were adopted as
sources of articles.
Design:
Systematic
literature review
Method:
Inclusion of
ICLNs in
healthcare
settings could
reduce the
cases of health
care-associated
infections.
Strength: Inclusion
of multiple
guidelines to
facilitate the
literature review
enhanced he
validity and
reliability of the
results obtained.
Weakness:
Minimal number
of sources (n = 10)
limited the
strength of the
review.
Critique of Literature
Infection prevention is one of the greatest challenges facing healthcare facilities. While
nurses in medical settings are considered as the primary organs of driving the infection
prevention initiatives adopted by their organizations, Lo et al. (2014) explain that system
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL GOVERNANCE 7
administrators and stakeholders at large need to share this burden by ensuring that the programs
put in place are streamlined through: acquisition and proper management of institution based
information in order to gauge the efficacy of the structure for reporting outbreaks; ensuring that
the existing policy procedures are effectively updated; prevention of antimicrobial resistances
through advancement of individualized remedies; and inculcating proper training initiatives
targeting all stakeholders. In essence, the three scholarly materials put a lot of emphasis on
nurses working in different healthcare settings as the major agents of preventing infections. For
instance, the research conducted by Jackson et al. (2014) proceeds with the aim of investigating
the infection prevention behaviors adopted by nurses in acute care settings by prompting the
explanations offered by nurses for the traits observed. On the other hand, the cross-sectional
descriptive study conducted by AL- Rawajfah (2018) investigates the practices of controlling
infections among nurses working in critical care settings in Jordan. Lastly, Peter et al. (2018)
ascertain the factors that act as facilitators and barriers to effective implementation of infection
control programs among infection control link nurses. While the three studies are highly
effective in vetting the roles of nurses in fostering infection prevention, they do not look into the
efficacy of other contributing factors such as the efficiency of the entire healthcare system in
forming the desired policies, audits and regulatory frameworks to correct this menace.
Nurses play a significant role in fostering and initiating the infection control programs
adopted in their institutions. However, effective adoption of instruments aimed at strengthening
the surveillance and audit functions in healthcare settings could be of critical essence in
minimizing the rates of spread of infections in clinical settings. As revealed by Jackson et al.
(2018), the system has seen an increase in the number of hospital based infections due to the
suboptimal initiatives put in place by nurses. As a mater of fact, the scholars report that nurses
administrators and stakeholders at large need to share this burden by ensuring that the programs
put in place are streamlined through: acquisition and proper management of institution based
information in order to gauge the efficacy of the structure for reporting outbreaks; ensuring that
the existing policy procedures are effectively updated; prevention of antimicrobial resistances
through advancement of individualized remedies; and inculcating proper training initiatives
targeting all stakeholders. In essence, the three scholarly materials put a lot of emphasis on
nurses working in different healthcare settings as the major agents of preventing infections. For
instance, the research conducted by Jackson et al. (2014) proceeds with the aim of investigating
the infection prevention behaviors adopted by nurses in acute care settings by prompting the
explanations offered by nurses for the traits observed. On the other hand, the cross-sectional
descriptive study conducted by AL- Rawajfah (2018) investigates the practices of controlling
infections among nurses working in critical care settings in Jordan. Lastly, Peter et al. (2018)
ascertain the factors that act as facilitators and barriers to effective implementation of infection
control programs among infection control link nurses. While the three studies are highly
effective in vetting the roles of nurses in fostering infection prevention, they do not look into the
efficacy of other contributing factors such as the efficiency of the entire healthcare system in
forming the desired policies, audits and regulatory frameworks to correct this menace.
Nurses play a significant role in fostering and initiating the infection control programs
adopted in their institutions. However, effective adoption of instruments aimed at strengthening
the surveillance and audit functions in healthcare settings could be of critical essence in
minimizing the rates of spread of infections in clinical settings. As revealed by Jackson et al.
(2018), the system has seen an increase in the number of hospital based infections due to the
suboptimal initiatives put in place by nurses. As a mater of fact, the scholars report that nurses
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL GOVERNANCE 8
resort to revealing behaviours that reveal higher levels of deviance from the set frameworks of
clinical governance. While such traits could be as a result of the influences of the environments
in which these practitioners offer their services, Ocampo et al. (2017) explain that training and
education could play a role in inculcating the desired attributes. For instance, Peter et al. (2018)
demystify the effectiveness of while the acceptation of ICLNs in clinical settings is still minimal,
these professionals have the potential of minimizing the infections acquired in healthcare settings
through advancement of psychological and technical skills.
Findings
The articles by Jackson et al (2014), AL-Rawajfah (2016) and Peter et al. (2018) provide
an array of insights on the most effective ways of preventing acquisition and spread of infections
in healthcare settings. Based on the literature presented by these scholars, healthcare related
infections are real, a continuing challenge and are associated with massive cost implications both
on the side of the users and that of the system. In their view, Jackson et al. (2018) reveal that
unnecessary infections are reported by nurses to be highly attributed to the behavioral positions
of their peers as opposed to one’s own; an aspect that calls for inclusion of corrective
mechanisms that adopt multifaceted remedies which may not have been included in the existing
institutional policies, guidelines and regulatory frameworks. On the other hand, AL- Rawajfah
(2016) reveals that the flaws leading to the prevalence of hospital acquired infections can be
minimized through implementation of educational initiatives aimed at enlightening practitioners
on the most effective ways of reducing errors in acute care settings. In particular, the researcher
reveals that medical institutions could induce the infection control programs by implementing
organization based training programs. Despite the efficiency of these training initiatives, Peter et
al. (2018) consider technical and psychological skills to be effective in instilling infection
resort to revealing behaviours that reveal higher levels of deviance from the set frameworks of
clinical governance. While such traits could be as a result of the influences of the environments
in which these practitioners offer their services, Ocampo et al. (2017) explain that training and
education could play a role in inculcating the desired attributes. For instance, Peter et al. (2018)
demystify the effectiveness of while the acceptation of ICLNs in clinical settings is still minimal,
these professionals have the potential of minimizing the infections acquired in healthcare settings
through advancement of psychological and technical skills.
Findings
The articles by Jackson et al (2014), AL-Rawajfah (2016) and Peter et al. (2018) provide
an array of insights on the most effective ways of preventing acquisition and spread of infections
in healthcare settings. Based on the literature presented by these scholars, healthcare related
infections are real, a continuing challenge and are associated with massive cost implications both
on the side of the users and that of the system. In their view, Jackson et al. (2018) reveal that
unnecessary infections are reported by nurses to be highly attributed to the behavioral positions
of their peers as opposed to one’s own; an aspect that calls for inclusion of corrective
mechanisms that adopt multifaceted remedies which may not have been included in the existing
institutional policies, guidelines and regulatory frameworks. On the other hand, AL- Rawajfah
(2016) reveals that the flaws leading to the prevalence of hospital acquired infections can be
minimized through implementation of educational initiatives aimed at enlightening practitioners
on the most effective ways of reducing errors in acute care settings. In particular, the researcher
reveals that medical institutions could induce the infection control programs by implementing
organization based training programs. Despite the efficiency of these training initiatives, Peter et
al. (2018) consider technical and psychological skills to be effective in instilling infection
CLINICAL GOVERNANCE 9
controls. However, they recommend that medical centers need to recruit ICLNs in order to
minimize these errors. The findings in these three studies are of great relevance to healthcare
professionals working as nurses. These caregivers need to emphasize on the importance of
acquiring knowledge, adhering to the set institutional policies, rules and regulations as effective
mechanisms of minimizing the infections acquired in hospital settings.
controls. However, they recommend that medical centers need to recruit ICLNs in order to
minimize these errors. The findings in these three studies are of great relevance to healthcare
professionals working as nurses. These caregivers need to emphasize on the importance of
acquiring knowledge, adhering to the set institutional policies, rules and regulations as effective
mechanisms of minimizing the infections acquired in hospital settings.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL GOVERNANCE 10
References
AL‐Rawajfah, O. M. (2016). Infection control practices among intensive care unit registered
nurses: a Jordanian national study. Nursing in critical care, 21(2), e20-e27.
Anderson, D. J., Podgorny, K., Berrios-Torres, S. I., Bratzler, D. W., Dellinger, E. P., Greene, L.,
... & Kaye, K. S. (2014). Strategies to prevent surgical site infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(S2), S66-S88.
Jackson, C., Lowton, K., & Griffiths, P. (2014). Infection prevention as “a show”: A qualitative
study of nurses’ infection prevention behaviours. International journal of nursing studies,
51(3), 400-408.
Lo, E., Nicolle, L. E., Coffin, S. E., Gould, C., Maragakis, L. L., Meddings, J., ... & Yokoe, D. S.
(2014). Strategies to prevent catheter-associated urinary tract infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(5), 464-479.
Louh, I. K., Greendyke, W. G., Hermann, E. A., Davidson, K. W., Falzon, L., Vawdrey, D. K., ...
& Ting, H. H. (2017). Clostridium difficile infection in acute care hospitals: systematic
review and best practices for prevention. infection control & hospital epidemiology,
38(4), 476-482.
Ocampo, W., Geransar, R., Clayden, N., Jones, J., de Grood, J., Joffe, M., ... & Conly, J. (2017).
Environmental scan of infection prevention and control practices for containment of
hospital-acquired infectious disease outbreaks in acute care hospital settings across
Canada. American journal of infection control, 45(10), 1116-1126.
Peter, D., Meng, M., Kugler, C., & Mattner, F. (2018). Strategies to promote infection
prevention and control in acute care hospitals with the help of infection control link
References
AL‐Rawajfah, O. M. (2016). Infection control practices among intensive care unit registered
nurses: a Jordanian national study. Nursing in critical care, 21(2), e20-e27.
Anderson, D. J., Podgorny, K., Berrios-Torres, S. I., Bratzler, D. W., Dellinger, E. P., Greene, L.,
... & Kaye, K. S. (2014). Strategies to prevent surgical site infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(S2), S66-S88.
Jackson, C., Lowton, K., & Griffiths, P. (2014). Infection prevention as “a show”: A qualitative
study of nurses’ infection prevention behaviours. International journal of nursing studies,
51(3), 400-408.
Lo, E., Nicolle, L. E., Coffin, S. E., Gould, C., Maragakis, L. L., Meddings, J., ... & Yokoe, D. S.
(2014). Strategies to prevent catheter-associated urinary tract infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(5), 464-479.
Louh, I. K., Greendyke, W. G., Hermann, E. A., Davidson, K. W., Falzon, L., Vawdrey, D. K., ...
& Ting, H. H. (2017). Clostridium difficile infection in acute care hospitals: systematic
review and best practices for prevention. infection control & hospital epidemiology,
38(4), 476-482.
Ocampo, W., Geransar, R., Clayden, N., Jones, J., de Grood, J., Joffe, M., ... & Conly, J. (2017).
Environmental scan of infection prevention and control practices for containment of
hospital-acquired infectious disease outbreaks in acute care hospital settings across
Canada. American journal of infection control, 45(10), 1116-1126.
Peter, D., Meng, M., Kugler, C., & Mattner, F. (2018). Strategies to promote infection
prevention and control in acute care hospitals with the help of infection control link
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL GOVERNANCE 11
nurses: A systematic literature review. American journal of infection control, 46(2), 207-
216.
Rowley, S., Clares, S., Poll, K., Thomas, S., & White, K. (2017). a Standard Approach to
Reducing Haematology/bmt “never events” and Other Clinical Incidents in a Bmt
Setting: A Clinical Governance Framework: no005. Bone Marrow Transplantation, 52,
S519.
Storr, J., Twyman, A., Zingg, W., Damani, N., Kilpatrick, C., Reilly, J., ... & Allegranzi, B.
(2017). Core components for effective infection prevention and control programmes: new
WHO evidence-based recommendations. Antimicrobial Resistance & Infection Control,
6(1), 6.
Zingg, W., Hopkins, S., Gayet-Ageron, A., Holmes, A., Sharland, M., Suetens, C., ... & Cairns,
S. (2017). Health-care-associated infections in neonates, children, and adolescents: an
analysis of paediatric data from the European Centre for Disease Prevention and Control
point-prevalence survey. The Lancet Infectious Diseases, 17(4), 381-389.
nurses: A systematic literature review. American journal of infection control, 46(2), 207-
216.
Rowley, S., Clares, S., Poll, K., Thomas, S., & White, K. (2017). a Standard Approach to
Reducing Haematology/bmt “never events” and Other Clinical Incidents in a Bmt
Setting: A Clinical Governance Framework: no005. Bone Marrow Transplantation, 52,
S519.
Storr, J., Twyman, A., Zingg, W., Damani, N., Kilpatrick, C., Reilly, J., ... & Allegranzi, B.
(2017). Core components for effective infection prevention and control programmes: new
WHO evidence-based recommendations. Antimicrobial Resistance & Infection Control,
6(1), 6.
Zingg, W., Hopkins, S., Gayet-Ageron, A., Holmes, A., Sharland, M., Suetens, C., ... & Cairns,
S. (2017). Health-care-associated infections in neonates, children, and adolescents: an
analysis of paediatric data from the European Centre for Disease Prevention and Control
point-prevalence survey. The Lancet Infectious Diseases, 17(4), 381-389.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





