Clinical Practice Guidelines: Development, Uses, and Limitations
VerifiedAdded on 2022/09/26
|19
|4566
|29
Report
AI Summary
This report provides a comprehensive analysis of clinical practice guidelines, emphasizing their role in shaping clinical decision-making and improving the quality of patient care. It defines clinical guidelines, highlighting their function as systematically developed statements that guide practitioners. The report explores the uses of these guidelines, including their role in standardizing evaluation, promoting evidence-based approaches, and improving healthcare effectiveness. It also addresses the limitations, such as the challenge of keeping up with evolving medical knowledge and the need for individualized care. The report further examines the development process, referencing the Institute of Medicine's eight-step process, including transparency, conflict of interest management, stakeholder involvement, systematic reviews, and recommendation articulation. The quality of clinical practice guidelines is assessed based on the strength of evidence and recommendations, with an emphasis on the use of randomized control trials. Finally, the report discusses the challenges of implementing guidelines, including adherence, local circumstances, and cost-effectiveness, emphasizing the importance of organizational readiness and clinician understanding. The provided appendix includes an appraisal of adult urethral catheterization guidelines, assessing scope, stakeholder involvement, and application of the guidelines.

Running head: CLINICAL PRACTICE GUIDELINES 1
Clinical Practice Guidelines
Student’s Name
University
Clinical Practice Guidelines
Student’s Name
University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL PRACTICE GUIDELINES 2
Clinical Practice Guidelines
The rise of evidence based approaches changed the way practitioners approach work and
thus they needed clinical guidelines that shaped the way clinical decisions are made. The role of
these approaches is to improve the quality of care and to make practitioners accountable for the
decisions that they make (Hoffmann, Bennett, & Del Mar, 2017). Clinical guidelines exist as
golden standards of evaluation and practice that professionals. This essay defines clinical
guidelines, their uses, limitation and how they are developed.
Clinical practice guidelines are systematically developed statements used to assist in
making practitioner and patient decisions in clinical circumstances. This implies that the
guidelines define the role of each specific diagnostic and treatment modality when managing
patients. To guide the practitioners well, they offer recommendations that are developed through
rigorous systematic reviews of different medical research materials to suggest the best course of
action that needs to be taken (Kredo, et al., 2016). These guidelines are not fixed protocols that
must be followed but rather exist to assist practitioners in decision making by assisting in
determining the best course of action. Since these guidelines are developed based on evidence-
informed clinical practice guidelines they bridge the gap between policies, best practice, local
contexts and patient choice (Hoffmann, Bennett, & Del Mar, 2017). The benefit that the
implementing organizations derives from these is the decrease of variations, preventing mistakes,
adverse events and even improve the effectiveness of healthcare. In some cases, they form
benchmarks for audit and a way of comparing practices so that quality improvements can be
achieved.
Clinical Practice Guidelines
The rise of evidence based approaches changed the way practitioners approach work and
thus they needed clinical guidelines that shaped the way clinical decisions are made. The role of
these approaches is to improve the quality of care and to make practitioners accountable for the
decisions that they make (Hoffmann, Bennett, & Del Mar, 2017). Clinical guidelines exist as
golden standards of evaluation and practice that professionals. This essay defines clinical
guidelines, their uses, limitation and how they are developed.
Clinical practice guidelines are systematically developed statements used to assist in
making practitioner and patient decisions in clinical circumstances. This implies that the
guidelines define the role of each specific diagnostic and treatment modality when managing
patients. To guide the practitioners well, they offer recommendations that are developed through
rigorous systematic reviews of different medical research materials to suggest the best course of
action that needs to be taken (Kredo, et al., 2016). These guidelines are not fixed protocols that
must be followed but rather exist to assist practitioners in decision making by assisting in
determining the best course of action. Since these guidelines are developed based on evidence-
informed clinical practice guidelines they bridge the gap between policies, best practice, local
contexts and patient choice (Hoffmann, Bennett, & Del Mar, 2017). The benefit that the
implementing organizations derives from these is the decrease of variations, preventing mistakes,
adverse events and even improve the effectiveness of healthcare. In some cases, they form
benchmarks for audit and a way of comparing practices so that quality improvements can be
achieved.
CLINICAL PRACTICE GUIDELINES 3
Despite the fact that the clinical guidelines are important in practice Boudoulas, Leier,
Geleris, & Boudoulas (2015) adds that they are limited by the accumulation of medical
knowledge in the areas of diagnosis and management within the last few years. This has altered
the course of diseases, increased survival and even improved clinical outcomes which makes it
difficult to evaluate the long-term effects of some treatment options. The need for individualized
care makes it difficult to have a uniform approach to different patients. The role of individualized
care is to follow the guidelines but ensure that the care is developed based on the needs of the
patient. Each has to design a care process that reflects patient requirements which makes these
guidelines slightly different from each patient during their application.
According to Kredo, et al. (2016) the Institute of Medicine (IOM) has developed an eight
step process for the development of clinical guidelines. The first step entails the development of
transparency where the gap in the existing guideline is identified. This process is seen through
the preliminary questions of the guidelines that are supposed to be determined. The second step
is the management of conflict of interest where bias is addressed to determine how the new
research will be transparent and how it will add value to the existing knowledge. The third step
entails the development of the group of people, organizations and institutions that will participate
in the process. This entails different scholar groups that have interest in the clinical area of
concern. The fourth step practice is the development of clinical practice guidelines through
systematic review of different studies that have been developed (Murad, 2017). Through
systematic analysis of randomized control trials, gaps are addressed to present new guidelines
that need to be implemented.
The fifth stage is the establishment of foundations for rating the strength of the
recommendations. Since there are existing guidelines, it means that new ones can only be
Despite the fact that the clinical guidelines are important in practice Boudoulas, Leier,
Geleris, & Boudoulas (2015) adds that they are limited by the accumulation of medical
knowledge in the areas of diagnosis and management within the last few years. This has altered
the course of diseases, increased survival and even improved clinical outcomes which makes it
difficult to evaluate the long-term effects of some treatment options. The need for individualized
care makes it difficult to have a uniform approach to different patients. The role of individualized
care is to follow the guidelines but ensure that the care is developed based on the needs of the
patient. Each has to design a care process that reflects patient requirements which makes these
guidelines slightly different from each patient during their application.
According to Kredo, et al. (2016) the Institute of Medicine (IOM) has developed an eight
step process for the development of clinical guidelines. The first step entails the development of
transparency where the gap in the existing guideline is identified. This process is seen through
the preliminary questions of the guidelines that are supposed to be determined. The second step
is the management of conflict of interest where bias is addressed to determine how the new
research will be transparent and how it will add value to the existing knowledge. The third step
entails the development of the group of people, organizations and institutions that will participate
in the process. This entails different scholar groups that have interest in the clinical area of
concern. The fourth step practice is the development of clinical practice guidelines through
systematic review of different studies that have been developed (Murad, 2017). Through
systematic analysis of randomized control trials, gaps are addressed to present new guidelines
that need to be implemented.
The fifth stage is the establishment of foundations for rating the strength of the
recommendations. Since there are existing guidelines, it means that new ones can only be
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL PRACTICE GUIDELINES 4
accepted if they are seen to have more strength and value than the existing ones. In the sixth
stage the recommendations for the new found recommendations are articulated so that they can
be reviewed to determine whether these recommendations meet the required needs (Murad,
2017). The seventh stage is the external review of the recommendations that have been made by
an independent team that verifies and presents the review on whether the findings can be
accepted or not. If the recommendations are approved by the external team they are updated to
the existing ones in the last stage of development.
The quality of a clinical practice guideline is determined by the quality of evidence and
the strength of the recommendations. The quality of evidence is based on the studies that are
used in collecting the evidence for the recommendation. Murad (2017) suggests that higher
confidence in randomised control trials makes them the best factor for assesing the quality of
trials. Since these studies are based on controls that lead to the finding of the benefits and harms
of the evidence and the methodological limitations of the evidence that has been gathered. In
addition to that, the confidence level of these studies becomes the pillar of developing clinical
guidelines since the quality of studies used determines the quality of evidence. Further, Guyatt,
et al. (2008) suggests that the rise of evidence-based methods has led to the need to make
decisions based on evidence rather than expert opinion. In this case the quality of a clinical
practice guideline is based on the level of evidence used. This is the reason why randomised
control trials are the only source of evidence used in the development of evidence for guidelines.
The introduction of clinical guidelines in hospital settings can be challenging since they
can change the clinical practice or affect patient outcome. This means that there could be
adherence challenges that clinicians need to consider when applying them. This means that
clinicians need to understand the local circumstances and how these guidelines will affect
accepted if they are seen to have more strength and value than the existing ones. In the sixth
stage the recommendations for the new found recommendations are articulated so that they can
be reviewed to determine whether these recommendations meet the required needs (Murad,
2017). The seventh stage is the external review of the recommendations that have been made by
an independent team that verifies and presents the review on whether the findings can be
accepted or not. If the recommendations are approved by the external team they are updated to
the existing ones in the last stage of development.
The quality of a clinical practice guideline is determined by the quality of evidence and
the strength of the recommendations. The quality of evidence is based on the studies that are
used in collecting the evidence for the recommendation. Murad (2017) suggests that higher
confidence in randomised control trials makes them the best factor for assesing the quality of
trials. Since these studies are based on controls that lead to the finding of the benefits and harms
of the evidence and the methodological limitations of the evidence that has been gathered. In
addition to that, the confidence level of these studies becomes the pillar of developing clinical
guidelines since the quality of studies used determines the quality of evidence. Further, Guyatt,
et al. (2008) suggests that the rise of evidence-based methods has led to the need to make
decisions based on evidence rather than expert opinion. In this case the quality of a clinical
practice guideline is based on the level of evidence used. This is the reason why randomised
control trials are the only source of evidence used in the development of evidence for guidelines.
The introduction of clinical guidelines in hospital settings can be challenging since they
can change the clinical practice or affect patient outcome. This means that there could be
adherence challenges that clinicians need to consider when applying them. This means that
clinicians need to understand the local circumstances and how these guidelines will affect
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL PRACTICE GUIDELINES 5
practice (Jones & Reeve, 2018). This implies that there is need to understand the educational
understanding and the capacity to implement such guidelines. Since the guidelines are developed
using evidence, it is important for clinicians to use the same evidence to understand the issues
being raised in the guidelines and how this will affect the organization. When implementing the
guidelines, priority needs to be given to local guidelines and not national ones. This is because
local guidelines reflect the patient needs and the individualized care approaches that focus on the
needs of the patients.
Another consideration is the need to identify organizational readiness to implement the
new guidelines and at the same time the cost effectiveness of implementing these new
guidelines. Graham & Harrison (2018) state that when new guidelines are implemented in an
organization, there is need to the cost of this process and how this will affect the institution.
Since practitioners need to understand the role of each guideline and how they will be
implemented, it means that clinicians need to determine the cost of this new process and how this
will be achieved. By preparing the clinical team within the hospital, it is important to ensure that
they are well equipped to apply the new guidelines in practice.
Clinical guidelines are developed to improve the quality of care and assist practitioners in
decision making within hospital settings. They are developed through evidence based approaches
that involve systematic reviews of clinical trials to present new evidence that addresses the gaps
that exist in evidence. In this case, the role of developing these guidelines is to ensure that issues
within the clinical environment are addressed. When introducing these guidelines in a clinical
environment, clinicians need to understand how they relate to local guidelines of practice.
Therefore, when developed and implemented well, the guidelines can improve the practice,
decisions making and quality of practice to increase outcomes and avoid mistakes.
practice (Jones & Reeve, 2018). This implies that there is need to understand the educational
understanding and the capacity to implement such guidelines. Since the guidelines are developed
using evidence, it is important for clinicians to use the same evidence to understand the issues
being raised in the guidelines and how this will affect the organization. When implementing the
guidelines, priority needs to be given to local guidelines and not national ones. This is because
local guidelines reflect the patient needs and the individualized care approaches that focus on the
needs of the patients.
Another consideration is the need to identify organizational readiness to implement the
new guidelines and at the same time the cost effectiveness of implementing these new
guidelines. Graham & Harrison (2018) state that when new guidelines are implemented in an
organization, there is need to the cost of this process and how this will affect the institution.
Since practitioners need to understand the role of each guideline and how they will be
implemented, it means that clinicians need to determine the cost of this new process and how this
will be achieved. By preparing the clinical team within the hospital, it is important to ensure that
they are well equipped to apply the new guidelines in practice.
Clinical guidelines are developed to improve the quality of care and assist practitioners in
decision making within hospital settings. They are developed through evidence based approaches
that involve systematic reviews of clinical trials to present new evidence that addresses the gaps
that exist in evidence. In this case, the role of developing these guidelines is to ensure that issues
within the clinical environment are addressed. When introducing these guidelines in a clinical
environment, clinicians need to understand how they relate to local guidelines of practice.
Therefore, when developed and implemented well, the guidelines can improve the practice,
decisions making and quality of practice to increase outcomes and avoid mistakes.

CLINICAL PRACTICE GUIDELINES 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL PRACTICE GUIDELINES 7
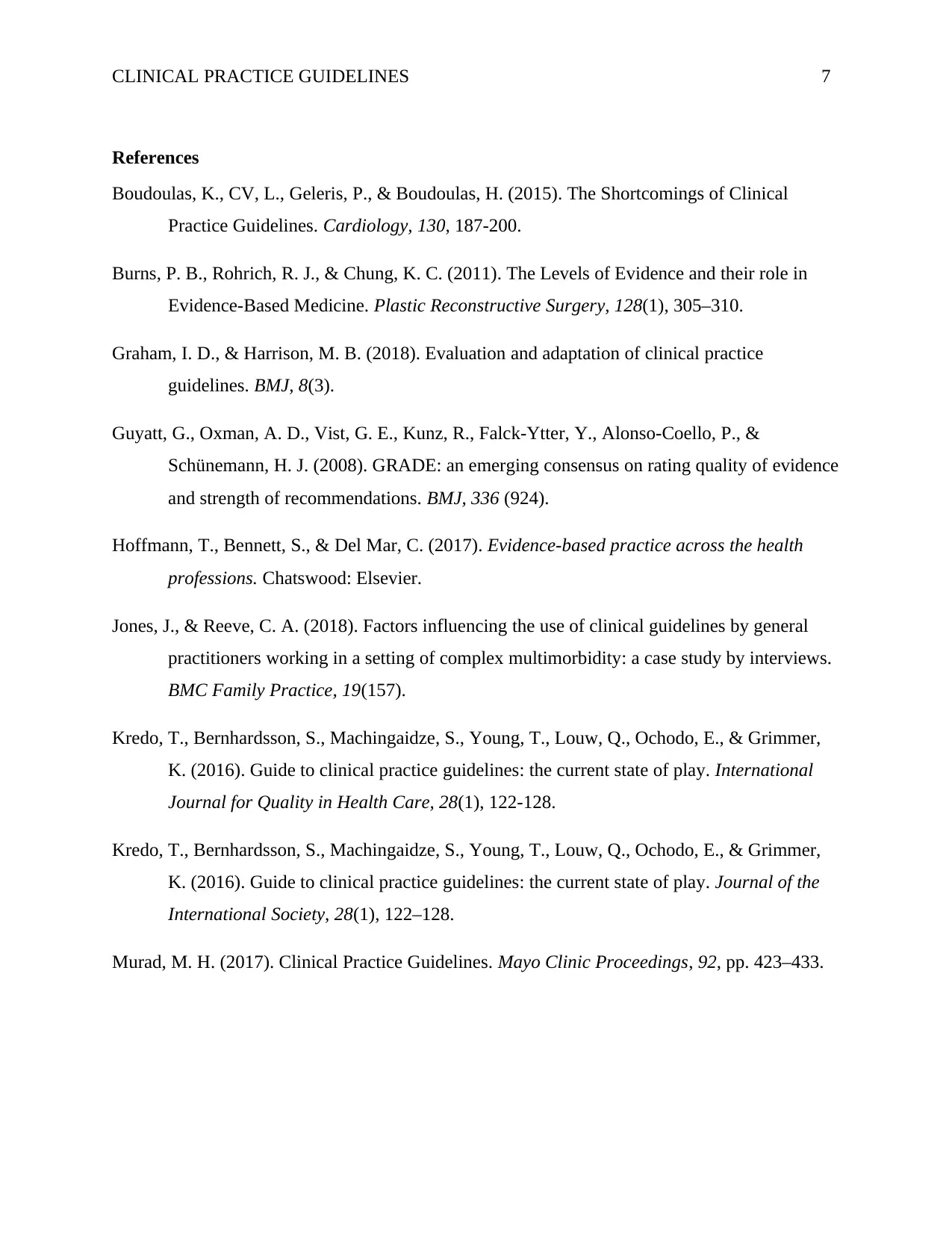
References
Boudoulas, K., CV, L., Geleris, P., & Boudoulas, H. (2015). The Shortcomings of Clinical
Practice Guidelines. Cardiology, 130, 187-200.
Burns, P. B., Rohrich, R. J., & Chung, K. C. (2011). The Levels of Evidence and their role in
Evidence-Based Medicine. Plastic Reconstructive Surgery, 128(1), 305–310.
Graham, I. D., & Harrison, M. B. (2018). Evaluation and adaptation of clinical practice
guidelines. BMJ, 8(3).
Guyatt, G., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., &
Schünemann, H. J. (2008). GRADE: an emerging consensus on rating quality of evidence
and strength of recommendations. BMJ, 336 (924).
Hoffmann, T., Bennett, S., & Del Mar, C. (2017). Evidence-based practice across the health
professions. Chatswood: Elsevier.
Jones, J., & Reeve, C. A. (2018). Factors influencing the use of clinical guidelines by general
practitioners working in a setting of complex multimorbidity: a case study by interviews.
BMC Family Practice, 19(157).
Kredo, T., Bernhardsson, S., Machingaidze, S., Young, T., Louw, Q., Ochodo, E., & Grimmer,
K. (2016). Guide to clinical practice guidelines: the current state of play. International
Journal for Quality in Health Care, 28(1), 122-128.
Kredo, T., Bernhardsson, S., Machingaidze, S., Young, T., Louw, Q., Ochodo, E., & Grimmer,
K. (2016). Guide to clinical practice guidelines: the current state of play. Journal of the
International Society, 28(1), 122–128.
Murad, M. H. (2017). Clinical Practice Guidelines. Mayo Clinic Proceedings, 92, pp. 423–433.
References
Boudoulas, K., CV, L., Geleris, P., & Boudoulas, H. (2015). The Shortcomings of Clinical
Practice Guidelines. Cardiology, 130, 187-200.
Burns, P. B., Rohrich, R. J., & Chung, K. C. (2011). The Levels of Evidence and their role in
Evidence-Based Medicine. Plastic Reconstructive Surgery, 128(1), 305–310.
Graham, I. D., & Harrison, M. B. (2018). Evaluation and adaptation of clinical practice
guidelines. BMJ, 8(3).
Guyatt, G., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., &
Schünemann, H. J. (2008). GRADE: an emerging consensus on rating quality of evidence
and strength of recommendations. BMJ, 336 (924).
Hoffmann, T., Bennett, S., & Del Mar, C. (2017). Evidence-based practice across the health
professions. Chatswood: Elsevier.
Jones, J., & Reeve, C. A. (2018). Factors influencing the use of clinical guidelines by general
practitioners working in a setting of complex multimorbidity: a case study by interviews.
BMC Family Practice, 19(157).
Kredo, T., Bernhardsson, S., Machingaidze, S., Young, T., Louw, Q., Ochodo, E., & Grimmer,
K. (2016). Guide to clinical practice guidelines: the current state of play. International
Journal for Quality in Health Care, 28(1), 122-128.
Kredo, T., Bernhardsson, S., Machingaidze, S., Young, T., Louw, Q., Ochodo, E., & Grimmer,
K. (2016). Guide to clinical practice guidelines: the current state of play. Journal of the
International Society, 28(1), 122–128.
Murad, M. H. (2017). Clinical Practice Guidelines. Mayo Clinic Proceedings, 92, pp. 423–433.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL PRACTICE GUIDELINES 8
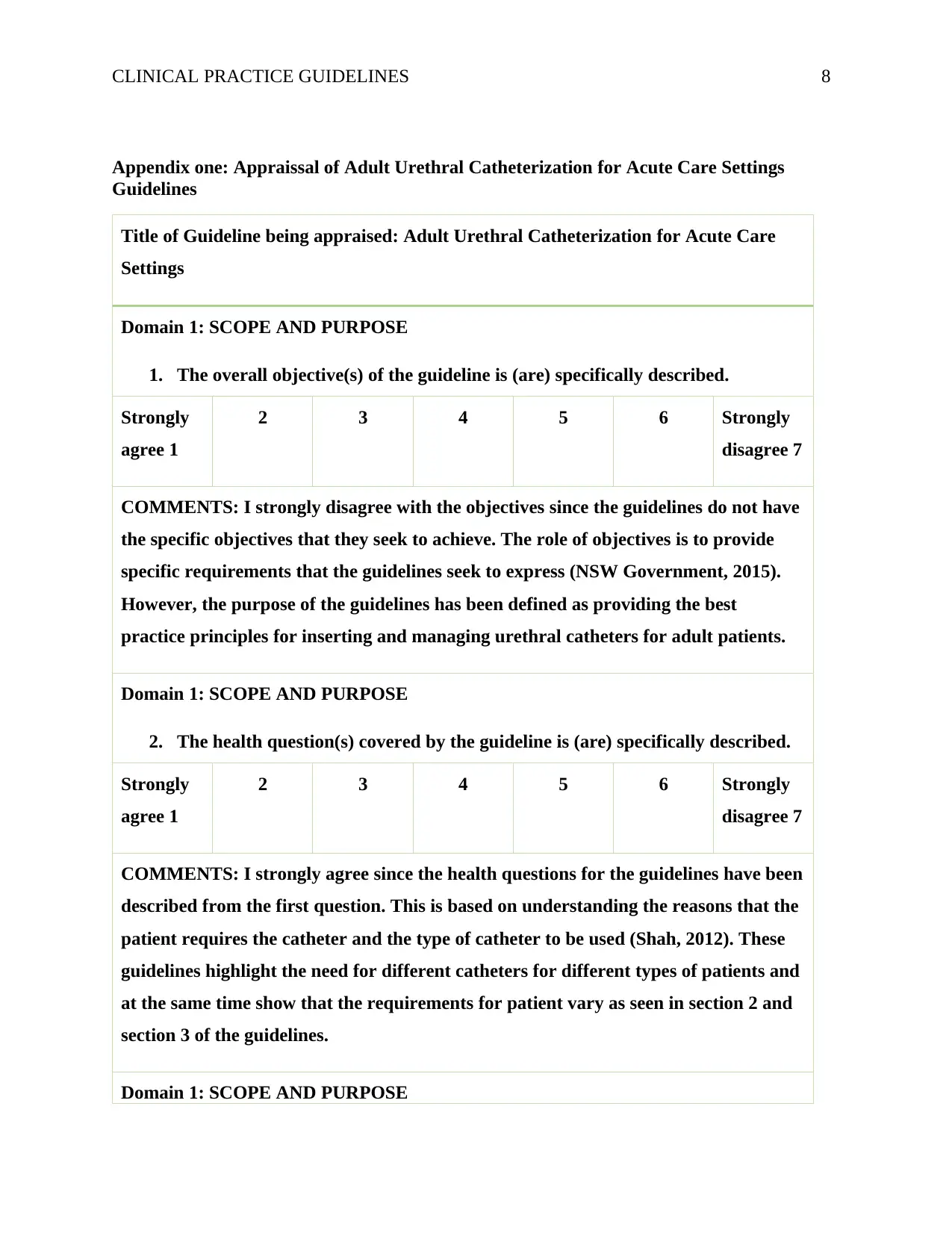
Appendix one: Appraissal of Adult Urethral Catheterization for Acute Care Settings
Guidelines
Title of Guideline being appraised: Adult Urethral Catheterization for Acute Care
Settings
Domain 1: SCOPE AND PURPOSE
1. The overall objective(s) of the guideline is (are) specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly disagree with the objectives since the guidelines do not have
the specific objectives that they seek to achieve. The role of objectives is to provide
specific requirements that the guidelines seek to express (NSW Government, 2015).
However, the purpose of the guidelines has been defined as providing the best
practice principles for inserting and managing urethral catheters for adult patients.
Domain 1: SCOPE AND PURPOSE
2. The health question(s) covered by the guideline is (are) specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly agree since the health questions for the guidelines have been
described from the first question. This is based on understanding the reasons that the
patient requires the catheter and the type of catheter to be used (Shah, 2012). These
guidelines highlight the need for different catheters for different types of patients and
at the same time show that the requirements for patient vary as seen in section 2 and
section 3 of the guidelines.
Domain 1: SCOPE AND PURPOSE
Appendix one: Appraissal of Adult Urethral Catheterization for Acute Care Settings
Guidelines
Title of Guideline being appraised: Adult Urethral Catheterization for Acute Care
Settings
Domain 1: SCOPE AND PURPOSE
1. The overall objective(s) of the guideline is (are) specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly disagree with the objectives since the guidelines do not have
the specific objectives that they seek to achieve. The role of objectives is to provide
specific requirements that the guidelines seek to express (NSW Government, 2015).
However, the purpose of the guidelines has been defined as providing the best
practice principles for inserting and managing urethral catheters for adult patients.
Domain 1: SCOPE AND PURPOSE
2. The health question(s) covered by the guideline is (are) specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly agree since the health questions for the guidelines have been
described from the first question. This is based on understanding the reasons that the
patient requires the catheter and the type of catheter to be used (Shah, 2012). These
guidelines highlight the need for different catheters for different types of patients and
at the same time show that the requirements for patient vary as seen in section 2 and
section 3 of the guidelines.
Domain 1: SCOPE AND PURPOSE
CLINICAL PRACTICE GUIDELINES 9
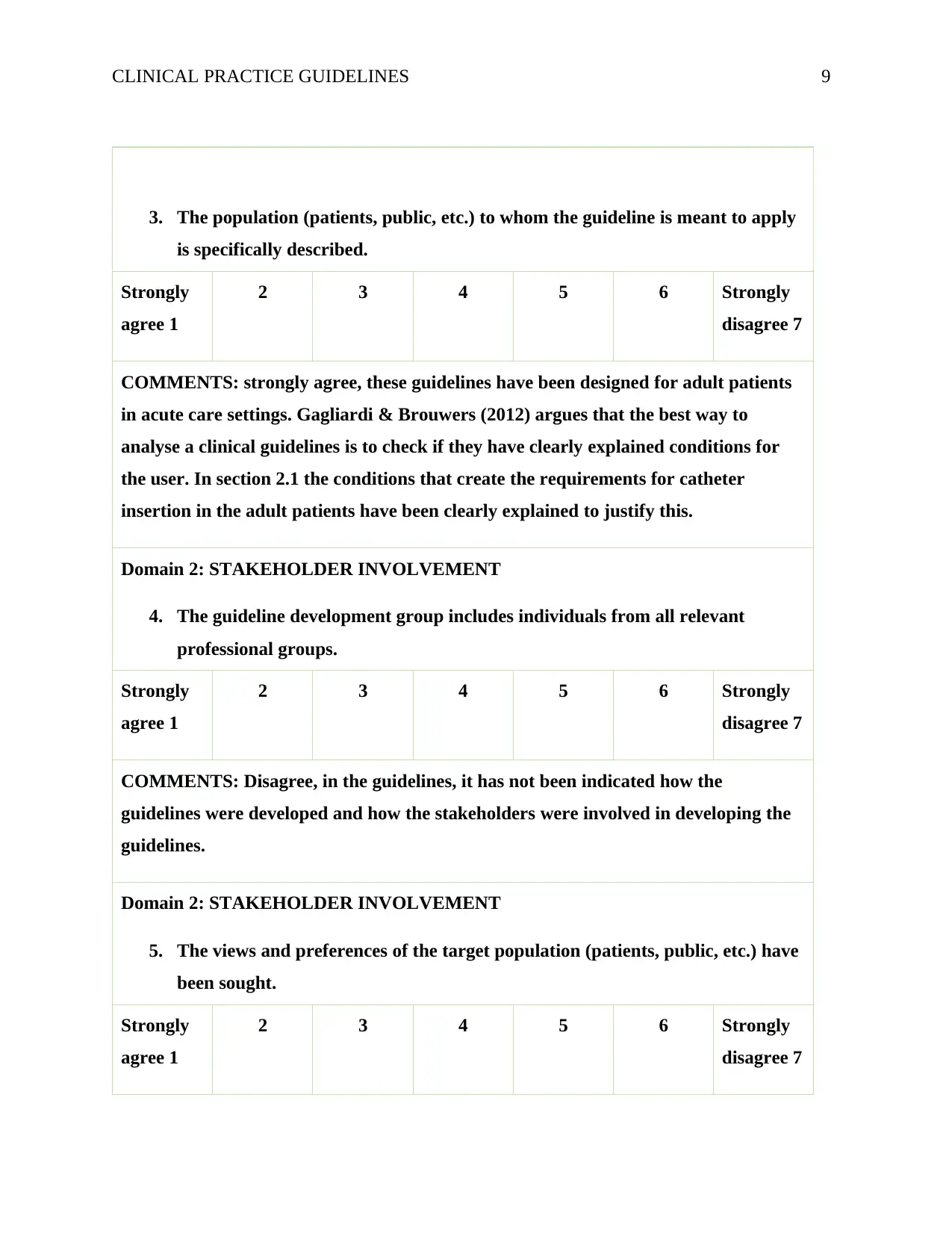
3. The population (patients, public, etc.) to whom the guideline is meant to apply
is specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, these guidelines have been designed for adult patients
in acute care settings. Gagliardi & Brouwers (2012) argues that the best way to
analyse a clinical guidelines is to check if they have clearly explained conditions for
the user. In section 2.1 the conditions that create the requirements for catheter
insertion in the adult patients have been clearly explained to justify this.
Domain 2: STAKEHOLDER INVOLVEMENT
4. The guideline development group includes individuals from all relevant
professional groups.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: Disagree, in the guidelines, it has not been indicated how the
guidelines were developed and how the stakeholders were involved in developing the
guidelines.
Domain 2: STAKEHOLDER INVOLVEMENT
5. The views and preferences of the target population (patients, public, etc.) have
been sought.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
3. The population (patients, public, etc.) to whom the guideline is meant to apply
is specifically described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, these guidelines have been designed for adult patients
in acute care settings. Gagliardi & Brouwers (2012) argues that the best way to
analyse a clinical guidelines is to check if they have clearly explained conditions for
the user. In section 2.1 the conditions that create the requirements for catheter
insertion in the adult patients have been clearly explained to justify this.
Domain 2: STAKEHOLDER INVOLVEMENT
4. The guideline development group includes individuals from all relevant
professional groups.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: Disagree, in the guidelines, it has not been indicated how the
guidelines were developed and how the stakeholders were involved in developing the
guidelines.
Domain 2: STAKEHOLDER INVOLVEMENT
5. The views and preferences of the target population (patients, public, etc.) have
been sought.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL PRACTICE GUIDELINES 10
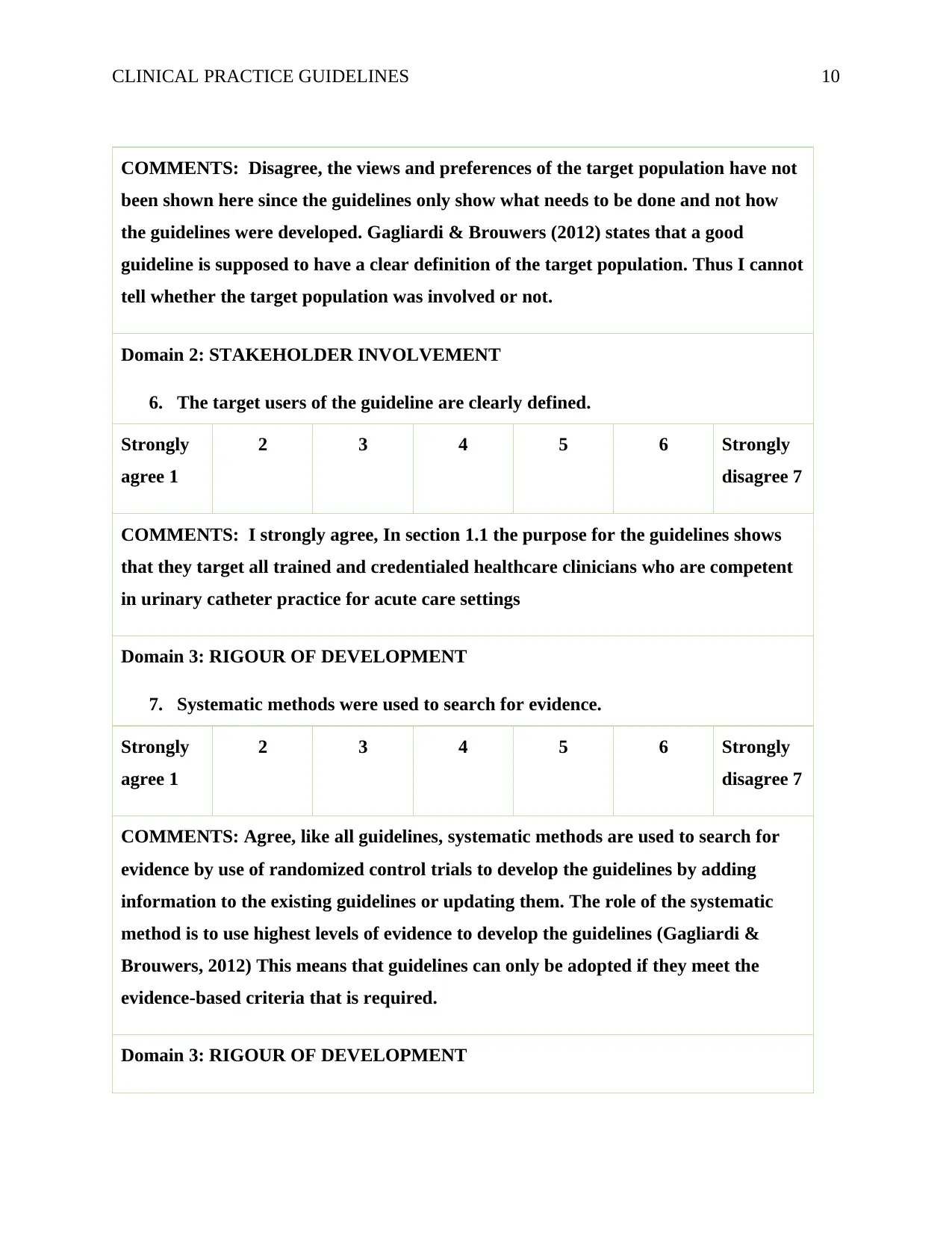
COMMENTS: Disagree, the views and preferences of the target population have not
been shown here since the guidelines only show what needs to be done and not how
the guidelines were developed. Gagliardi & Brouwers (2012) states that a good
guideline is supposed to have a clear definition of the target population. Thus I cannot
tell whether the target population was involved or not.
Domain 2: STAKEHOLDER INVOLVEMENT
6. The target users of the guideline are clearly defined.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly agree, In section 1.1 the purpose for the guidelines shows
that they target all trained and credentialed healthcare clinicians who are competent
in urinary catheter practice for acute care settings
Domain 3: RIGOUR OF DEVELOPMENT
7. Systematic methods were used to search for evidence.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: Agree, like all guidelines, systematic methods are used to search for
evidence by use of randomized control trials to develop the guidelines by adding
information to the existing guidelines or updating them. The role of the systematic
method is to use highest levels of evidence to develop the guidelines (Gagliardi &
Brouwers, 2012) This means that guidelines can only be adopted if they meet the
evidence-based criteria that is required.
Domain 3: RIGOUR OF DEVELOPMENT
COMMENTS: Disagree, the views and preferences of the target population have not
been shown here since the guidelines only show what needs to be done and not how
the guidelines were developed. Gagliardi & Brouwers (2012) states that a good
guideline is supposed to have a clear definition of the target population. Thus I cannot
tell whether the target population was involved or not.
Domain 2: STAKEHOLDER INVOLVEMENT
6. The target users of the guideline are clearly defined.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: I strongly agree, In section 1.1 the purpose for the guidelines shows
that they target all trained and credentialed healthcare clinicians who are competent
in urinary catheter practice for acute care settings
Domain 3: RIGOUR OF DEVELOPMENT
7. Systematic methods were used to search for evidence.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: Agree, like all guidelines, systematic methods are used to search for
evidence by use of randomized control trials to develop the guidelines by adding
information to the existing guidelines or updating them. The role of the systematic
method is to use highest levels of evidence to develop the guidelines (Gagliardi &
Brouwers, 2012) This means that guidelines can only be adopted if they meet the
evidence-based criteria that is required.
Domain 3: RIGOUR OF DEVELOPMENT
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL PRACTICE GUIDELINES 11
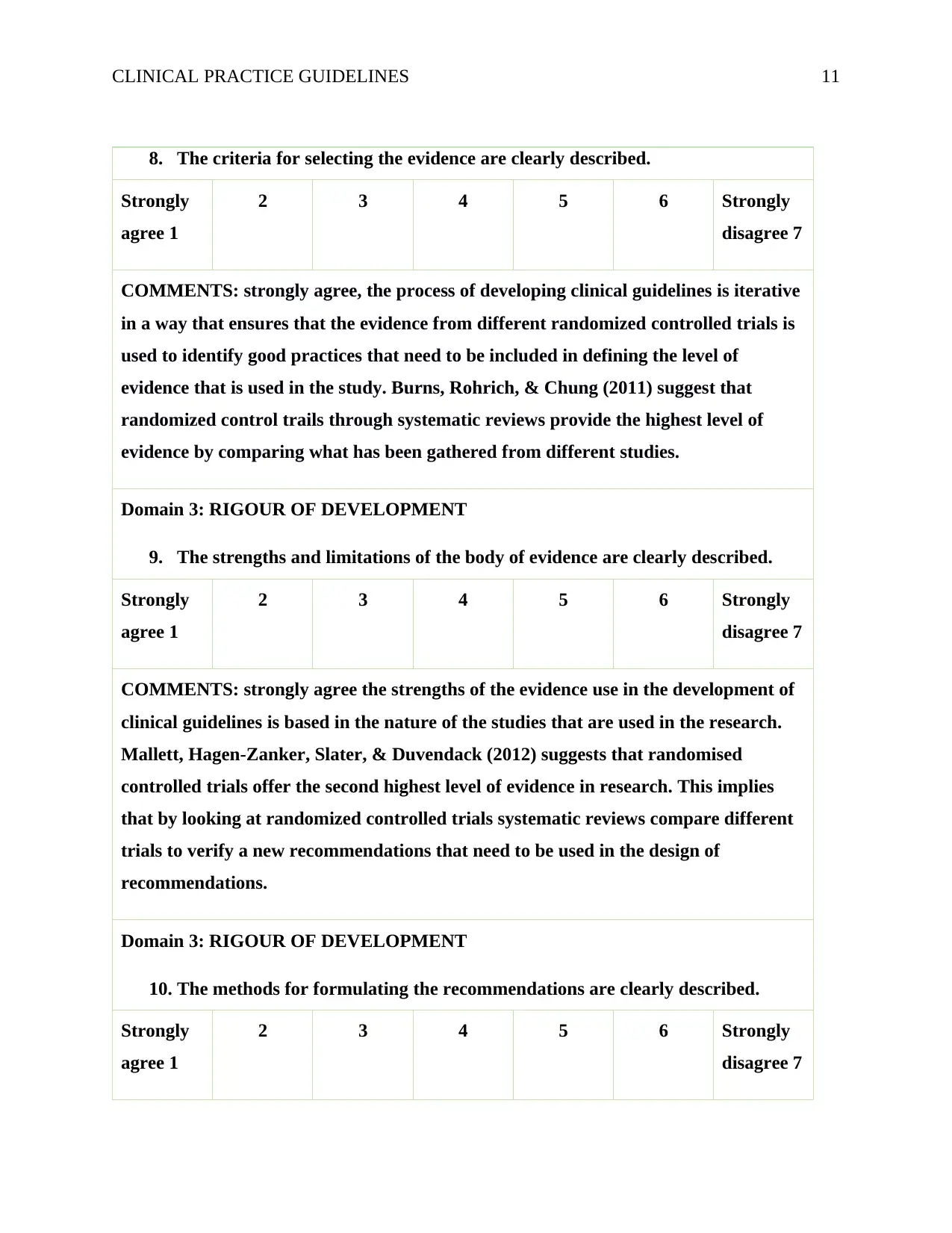
8. The criteria for selecting the evidence are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the process of developing clinical guidelines is iterative
in a way that ensures that the evidence from different randomized controlled trials is
used to identify good practices that need to be included in defining the level of
evidence that is used in the study. Burns, Rohrich, & Chung (2011) suggest that
randomized control trails through systematic reviews provide the highest level of
evidence by comparing what has been gathered from different studies.
Domain 3: RIGOUR OF DEVELOPMENT
9. The strengths and limitations of the body of evidence are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree the strengths of the evidence use in the development of
clinical guidelines is based in the nature of the studies that are used in the research.
Mallett, Hagen-Zanker, Slater, & Duvendack (2012) suggests that randomised
controlled trials offer the second highest level of evidence in research. This implies
that by looking at randomized controlled trials systematic reviews compare different
trials to verify a new recommendations that need to be used in the design of
recommendations.
Domain 3: RIGOUR OF DEVELOPMENT
10. The methods for formulating the recommendations are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
8. The criteria for selecting the evidence are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the process of developing clinical guidelines is iterative
in a way that ensures that the evidence from different randomized controlled trials is
used to identify good practices that need to be included in defining the level of
evidence that is used in the study. Burns, Rohrich, & Chung (2011) suggest that
randomized control trails through systematic reviews provide the highest level of
evidence by comparing what has been gathered from different studies.
Domain 3: RIGOUR OF DEVELOPMENT
9. The strengths and limitations of the body of evidence are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree the strengths of the evidence use in the development of
clinical guidelines is based in the nature of the studies that are used in the research.
Mallett, Hagen-Zanker, Slater, & Duvendack (2012) suggests that randomised
controlled trials offer the second highest level of evidence in research. This implies
that by looking at randomized controlled trials systematic reviews compare different
trials to verify a new recommendations that need to be used in the design of
recommendations.
Domain 3: RIGOUR OF DEVELOPMENT
10. The methods for formulating the recommendations are clearly described.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
CLINICAL PRACTICE GUIDELINES 12
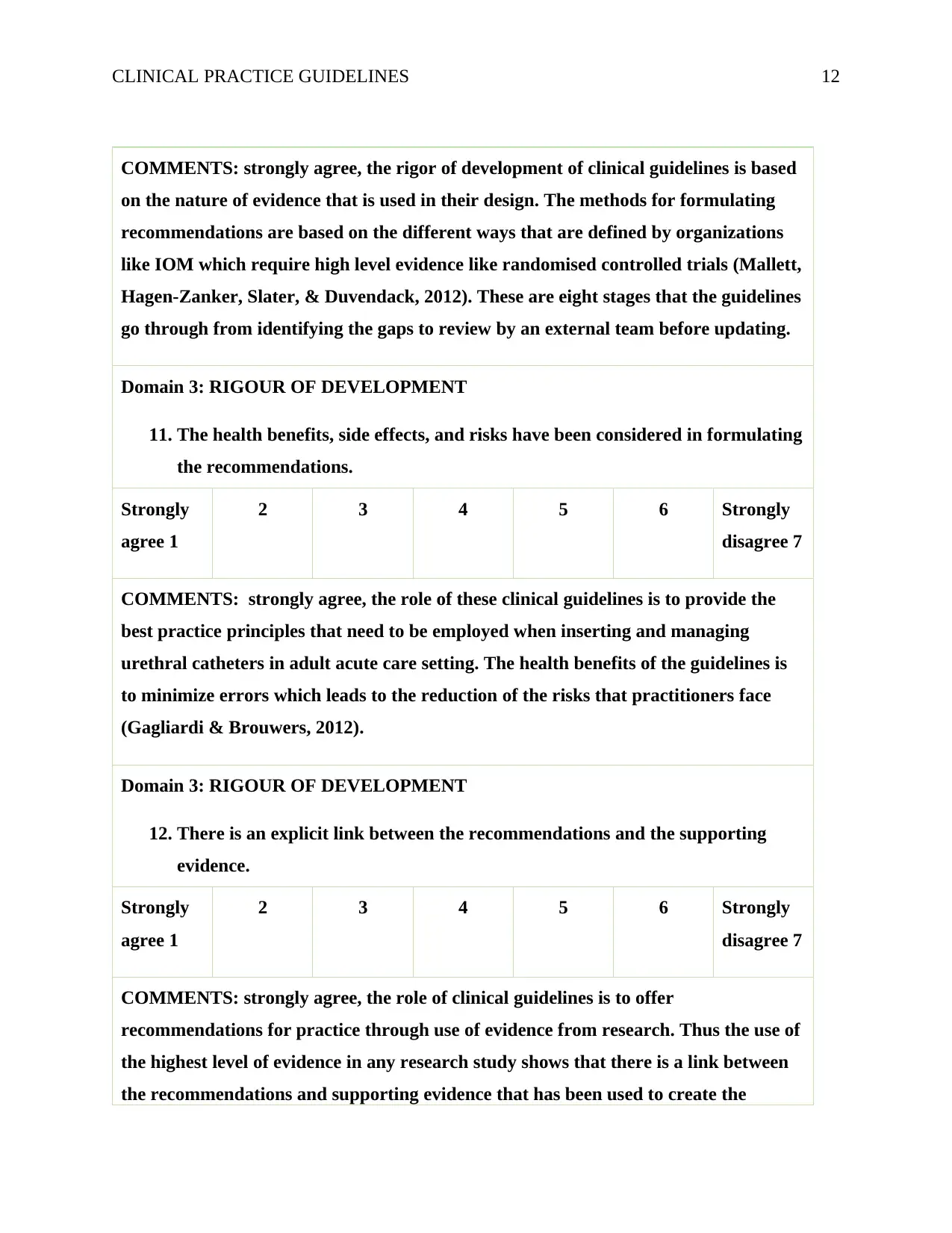
COMMENTS: strongly agree, the rigor of development of clinical guidelines is based
on the nature of evidence that is used in their design. The methods for formulating
recommendations are based on the different ways that are defined by organizations
like IOM which require high level evidence like randomised controlled trials (Mallett,
Hagen-Zanker, Slater, & Duvendack, 2012). These are eight stages that the guidelines
go through from identifying the gaps to review by an external team before updating.
Domain 3: RIGOUR OF DEVELOPMENT
11. The health benefits, side effects, and risks have been considered in formulating
the recommendations.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the role of these clinical guidelines is to provide the
best practice principles that need to be employed when inserting and managing
urethral catheters in adult acute care setting. The health benefits of the guidelines is
to minimize errors which leads to the reduction of the risks that practitioners face
(Gagliardi & Brouwers, 2012).
Domain 3: RIGOUR OF DEVELOPMENT
12. There is an explicit link between the recommendations and the supporting
evidence.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the role of clinical guidelines is to offer
recommendations for practice through use of evidence from research. Thus the use of
the highest level of evidence in any research study shows that there is a link between
the recommendations and supporting evidence that has been used to create the
COMMENTS: strongly agree, the rigor of development of clinical guidelines is based
on the nature of evidence that is used in their design. The methods for formulating
recommendations are based on the different ways that are defined by organizations
like IOM which require high level evidence like randomised controlled trials (Mallett,
Hagen-Zanker, Slater, & Duvendack, 2012). These are eight stages that the guidelines
go through from identifying the gaps to review by an external team before updating.
Domain 3: RIGOUR OF DEVELOPMENT
11. The health benefits, side effects, and risks have been considered in formulating
the recommendations.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the role of these clinical guidelines is to provide the
best practice principles that need to be employed when inserting and managing
urethral catheters in adult acute care setting. The health benefits of the guidelines is
to minimize errors which leads to the reduction of the risks that practitioners face
(Gagliardi & Brouwers, 2012).
Domain 3: RIGOUR OF DEVELOPMENT
12. There is an explicit link between the recommendations and the supporting
evidence.
Strongly
agree 1
2 3 4 5 6 Strongly
disagree 7
COMMENTS: strongly agree, the role of clinical guidelines is to offer
recommendations for practice through use of evidence from research. Thus the use of
the highest level of evidence in any research study shows that there is a link between
the recommendations and supporting evidence that has been used to create the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




