Report: Clinical Judgement and Reasoning in Cardiovascular Disease
VerifiedAdded on 2022/11/14
|9
|2474
|144
Report
AI Summary
This report presents a clinical judgement and reasoning analysis of a 62-year-old female patient presenting with symptoms of cardiovascular disease. The report correlates the patient's history, including pre-existing conditions like depression, diabetes, and alcohol addiction, with the observed symptoms such as chest pain, shortness of breath, and fatigue. The assessment utilizes the PQRST pain assessment strategy to clarify the origin and nature of the pain, linking it to potential cardiac infection based on the patient's responses. The pathophysiology of cardiovascular disease is discussed, highlighting the impact of blood vessel or heart system interference. Recommendations for patient management include blood pressure control, dietary adjustments (DASH diet, reduced salt intake), cholesterol management, weight reduction, physical activity, and addressing depression and diabetes. Specific medications, such as aspirin and hormone replacement therapy, are also suggested. The report emphasizes the importance of a holistic approach to managing cardiovascular disease and provides a comprehensive overview of the patient's condition and potential interventions.

Running head: CLINICAL JUDGEMENT AND REASONING 1
Clinical Judgement and Reasoning
Student’s Name
Institutional Affiliation
Clinical Judgement and Reasoning
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL JUDGMENT AND REASONING 2
Clinical Judgement and Reasoning
Correlation between the Patient's History, Assessment, and Pathophysiology of the Disease
This report involves an elderly patient (woman aged 62 years) who arrived at X hospital
at 0800 hours presenting symptoms that relate to cardiac vascular disease. The patient had a
medical history of using inhaler whenever she experienced a breath shortage. However, she later
realized the inhaler was of no significant help as the condition was adversely deteriorating.
Furthermore, the patient had been diagnosed with depression and diabetes one year ago. Also,
the patient is addicted to excessive alcohol consumption. The patient lacks dietary knowledge for
she seems to come from an illiterate background. Some of the evident signs and symptoms that
revealed the presence of cardiovascular disease include chest pain, shortness of breath,
palpitations, dizziness, fatigue, nausea pain around the left shoulder and arms. Even though the
patient was undergoing chest pain, it was not proven beyond a reasonable doubt that the pain
originated from cardiovascular disease. However, I went a further step to carry out pain
assessment using PQRST pain assessment strategy as a tool for clarifying the cause of the pain.
Under the PQRST technology, the initial “P” stands for position/provoking factors (Friedman, &
Alexander, 2013). At this point, I asked the patient a set of queries. These questions include
what makes the pain better? What makes the pain worse? Does the pain change with
repositioning? What was the patient doing when the pain started? Where is the pain and Whether
or not the patient can point the pain? The fact that repositioning has no impact on the pain
implied that the pain originated from cardiac infection. Following the pathophysiology of
cardiovascular disease, it is clear that the disease arises from interference of either the blood
vessels or the heart system. These are internal organs whose activity cannot be impacted by
repositioning. Hence, we don't expect repositioning to have an effect on chest pain that originates
Clinical Judgement and Reasoning
Correlation between the Patient's History, Assessment, and Pathophysiology of the Disease
This report involves an elderly patient (woman aged 62 years) who arrived at X hospital
at 0800 hours presenting symptoms that relate to cardiac vascular disease. The patient had a
medical history of using inhaler whenever she experienced a breath shortage. However, she later
realized the inhaler was of no significant help as the condition was adversely deteriorating.
Furthermore, the patient had been diagnosed with depression and diabetes one year ago. Also,
the patient is addicted to excessive alcohol consumption. The patient lacks dietary knowledge for
she seems to come from an illiterate background. Some of the evident signs and symptoms that
revealed the presence of cardiovascular disease include chest pain, shortness of breath,
palpitations, dizziness, fatigue, nausea pain around the left shoulder and arms. Even though the
patient was undergoing chest pain, it was not proven beyond a reasonable doubt that the pain
originated from cardiovascular disease. However, I went a further step to carry out pain
assessment using PQRST pain assessment strategy as a tool for clarifying the cause of the pain.
Under the PQRST technology, the initial “P” stands for position/provoking factors (Friedman, &
Alexander, 2013). At this point, I asked the patient a set of queries. These questions include
what makes the pain better? What makes the pain worse? Does the pain change with
repositioning? What was the patient doing when the pain started? Where is the pain and Whether
or not the patient can point the pain? The fact that repositioning has no impact on the pain
implied that the pain originated from cardiac infection. Following the pathophysiology of
cardiovascular disease, it is clear that the disease arises from interference of either the blood
vessels or the heart system. These are internal organs whose activity cannot be impacted by
repositioning. Hence, we don't expect repositioning to have an effect on chest pain that originates
CLINICAL JUDGMENT AND REASONING 3
from such an infection. Furthermore, the association of the pain with other symptoms such as
dizziness, nausea, back pain, fatigue, and shortness of breath revealed a significant life-
threatening cardiac infection (Sara et al., 2015).
The “Q” stands for quality whereby I asked the patient to describe the pain as sharp, dull,
stabbing, or crushing (Munroe, Curtis, Considine, & Buckley, 2013). In this case, the pain was
reported in the middle and upper sub-sternal region. This implied that the pain originated from
cardiac infection. On a similar note, "R" stands for radiation. At this point, I asked the patient to
tell if the pain radiates to other locations. With the patient at hand, it was clear that radiating pain
was extending to other sites such as arms and shoulders. Radiating pain is a significant symptom
in patients whose chest pain is caused by cardiac infection.
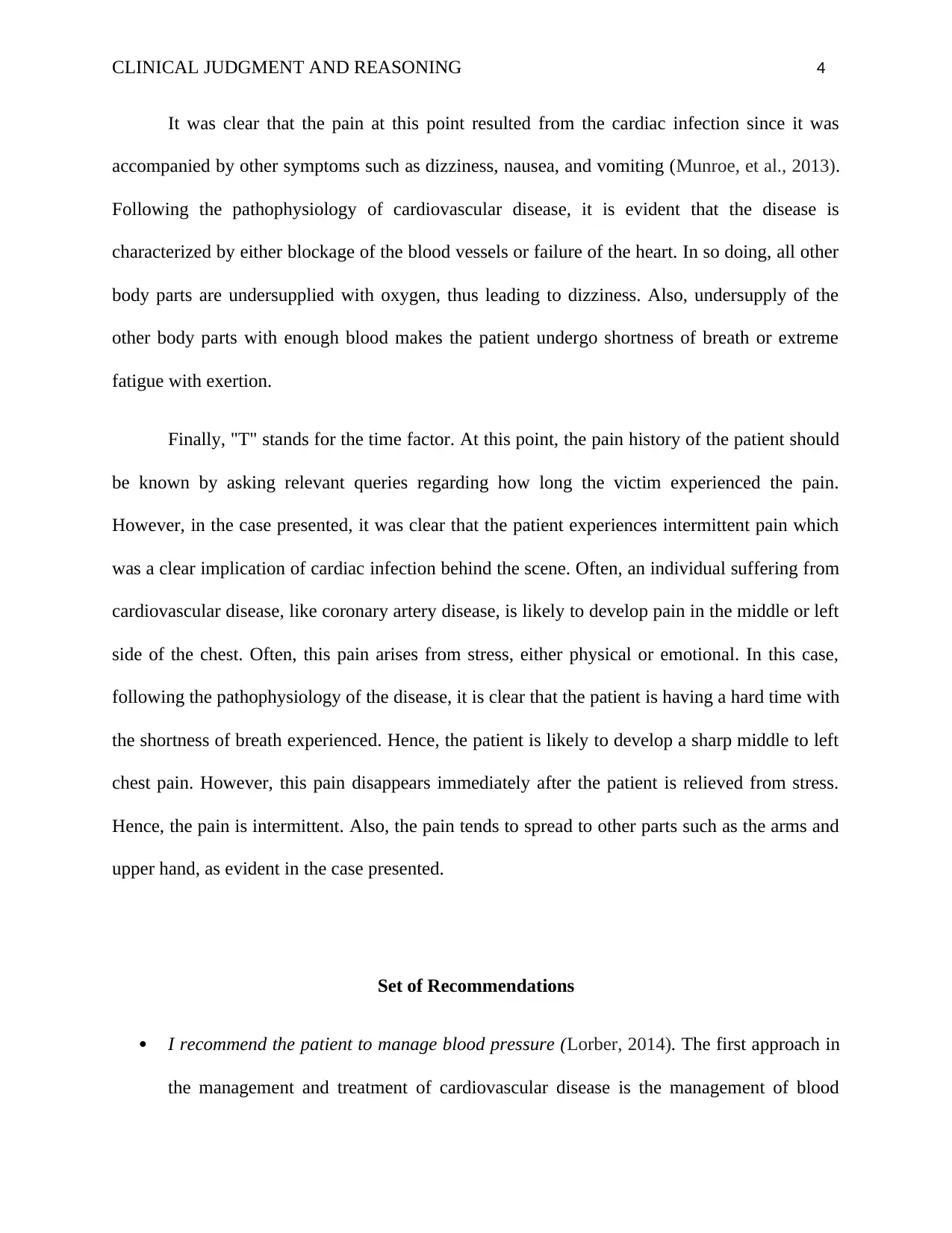
"S" stands for severity/symptoms. At this point, it is essential to rate the pain out of ten
and provide other accompanying symptoms. I used faces pain assessment scale to rate the
intensity of the pain. The figure below indicates the display of faces pain scale.
Retrieved from: (Garra et al., 2010)
from such an infection. Furthermore, the association of the pain with other symptoms such as
dizziness, nausea, back pain, fatigue, and shortness of breath revealed a significant life-
threatening cardiac infection (Sara et al., 2015).
The “Q” stands for quality whereby I asked the patient to describe the pain as sharp, dull,
stabbing, or crushing (Munroe, Curtis, Considine, & Buckley, 2013). In this case, the pain was
reported in the middle and upper sub-sternal region. This implied that the pain originated from
cardiac infection. On a similar note, "R" stands for radiation. At this point, I asked the patient to
tell if the pain radiates to other locations. With the patient at hand, it was clear that radiating pain
was extending to other sites such as arms and shoulders. Radiating pain is a significant symptom
in patients whose chest pain is caused by cardiac infection.
"S" stands for severity/symptoms. At this point, it is essential to rate the pain out of ten
and provide other accompanying symptoms. I used faces pain assessment scale to rate the
intensity of the pain. The figure below indicates the display of faces pain scale.
Retrieved from: (Garra et al., 2010)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL JUDGMENT AND REASONING 4
It was clear that the pain at this point resulted from the cardiac infection since it was
accompanied by other symptoms such as dizziness, nausea, and vomiting (Munroe, et al., 2013).
Following the pathophysiology of cardiovascular disease, it is evident that the disease is
characterized by either blockage of the blood vessels or failure of the heart. In so doing, all other
body parts are undersupplied with oxygen, thus leading to dizziness. Also, undersupply of the
other body parts with enough blood makes the patient undergo shortness of breath or extreme
fatigue with exertion.
Finally, "T" stands for the time factor. At this point, the pain history of the patient should
be known by asking relevant queries regarding how long the victim experienced the pain.
However, in the case presented, it was clear that the patient experiences intermittent pain which
was a clear implication of cardiac infection behind the scene. Often, an individual suffering from
cardiovascular disease, like coronary artery disease, is likely to develop pain in the middle or left
side of the chest. Often, this pain arises from stress, either physical or emotional. In this case,
following the pathophysiology of the disease, it is clear that the patient is having a hard time with
the shortness of breath experienced. Hence, the patient is likely to develop a sharp middle to left
chest pain. However, this pain disappears immediately after the patient is relieved from stress.
Hence, the pain is intermittent. Also, the pain tends to spread to other parts such as the arms and
upper hand, as evident in the case presented.
Set of Recommendations
I recommend the patient to manage blood pressure (Lorber, 2014). The first approach in
the management and treatment of cardiovascular disease is the management of blood
It was clear that the pain at this point resulted from the cardiac infection since it was
accompanied by other symptoms such as dizziness, nausea, and vomiting (Munroe, et al., 2013).
Following the pathophysiology of cardiovascular disease, it is evident that the disease is
characterized by either blockage of the blood vessels or failure of the heart. In so doing, all other
body parts are undersupplied with oxygen, thus leading to dizziness. Also, undersupply of the
other body parts with enough blood makes the patient undergo shortness of breath or extreme
fatigue with exertion.
Finally, "T" stands for the time factor. At this point, the pain history of the patient should
be known by asking relevant queries regarding how long the victim experienced the pain.
However, in the case presented, it was clear that the patient experiences intermittent pain which
was a clear implication of cardiac infection behind the scene. Often, an individual suffering from
cardiovascular disease, like coronary artery disease, is likely to develop pain in the middle or left
side of the chest. Often, this pain arises from stress, either physical or emotional. In this case,
following the pathophysiology of the disease, it is clear that the patient is having a hard time with
the shortness of breath experienced. Hence, the patient is likely to develop a sharp middle to left
chest pain. However, this pain disappears immediately after the patient is relieved from stress.
Hence, the pain is intermittent. Also, the pain tends to spread to other parts such as the arms and
upper hand, as evident in the case presented.
Set of Recommendations
I recommend the patient to manage blood pressure (Lorber, 2014). The first approach in
the management and treatment of cardiovascular disease is the management of blood
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL JUDGMENT AND REASONING 5
pressure. At this point, it is imperative neither for the patient to understand and know
personal blood pressure numbers and ensure that they are neither bellow nor above the
normal range. The blood pressure numbers include the systolic (the pressure of the blood
when the heart is beating to pump blood) and diastolic pressures (the pressure the heart is
at rest between the beats) (Agca et al., 2017). It is thus crucial to regularly check one's
blood pressure and engage in operations that will regulate the blood pressure in normal
ranges. For instance, one may formulate a healthy eating plan, engage in physical
activity, and take appropriate medication for the management of high blood pressure.
I recommend the patent to reduce salt intake (Kahn, Robbins, Kim, & Fuster, 2013):
Reduction of sodium consumption has proven to play a vital role in reducing blood
pressure among patients. More significantly, the impact of sodium intake reduction on
blood pressure is greater in patients with hypertension than those with normal blood
ranges.
I recommend the patient to execute Dietary Approach to Stop Hypertension (DASH diet).
The DASH diet is a meal ration comprising of fruits, vegetables, low-fat dairy foods,
whole grains, nuts, chicken, lean meat, fish and low saturated fats. Research reveals that
consumption of such meals leads to a reduction of blood pressure among hypertension
patients.
I recommend the patient to reduce alcohol consumption. Research reveals a significant
correlation between alcohol consumption and hypertension. Thus, it recommended that
individuals should not consume more than two standard drinks in a day.
I recommend the patient to manage cholesterol. It is imperative for the patient to know
and understand individual body cholesterol content. Several tools can be utilized in
pressure. At this point, it is imperative neither for the patient to understand and know
personal blood pressure numbers and ensure that they are neither bellow nor above the
normal range. The blood pressure numbers include the systolic (the pressure of the blood
when the heart is beating to pump blood) and diastolic pressures (the pressure the heart is
at rest between the beats) (Agca et al., 2017). It is thus crucial to regularly check one's
blood pressure and engage in operations that will regulate the blood pressure in normal
ranges. For instance, one may formulate a healthy eating plan, engage in physical
activity, and take appropriate medication for the management of high blood pressure.
I recommend the patent to reduce salt intake (Kahn, Robbins, Kim, & Fuster, 2013):
Reduction of sodium consumption has proven to play a vital role in reducing blood
pressure among patients. More significantly, the impact of sodium intake reduction on
blood pressure is greater in patients with hypertension than those with normal blood
ranges.
I recommend the patient to execute Dietary Approach to Stop Hypertension (DASH diet).
The DASH diet is a meal ration comprising of fruits, vegetables, low-fat dairy foods,
whole grains, nuts, chicken, lean meat, fish and low saturated fats. Research reveals that
consumption of such meals leads to a reduction of blood pressure among hypertension
patients.
I recommend the patient to reduce alcohol consumption. Research reveals a significant
correlation between alcohol consumption and hypertension. Thus, it recommended that
individuals should not consume more than two standard drinks in a day.
I recommend the patient to manage cholesterol. It is imperative for the patient to know
and understand individual body cholesterol content. Several tools can be utilized in
CLINICAL JUDGMENT AND REASONING 6
identifying if an individual's cholesterol is too high or low. However, it is also significant
to consider one's family history and cultural background when deciding if cholesterol is
too high. But most importantly, cholesterol level above 6.0 calls for reduction actions.
Often, a slow and periodic buildup of cholesterol in the inner lining of the heart's arteries
is the major cause of coronary disease. Bad cholesterol can build up in the arteries
leading to the narrowing of the blood pathway hence interfering with the flow of blood.
Also, narrow arteries can be clogged, thus stopping the flow of blood. As a result, the
failure of blood to arrive in the heart may result in a heart attack or stroke (in the case of
the brain). Such cardiac diseases have great implications for the wellbeing of an
individual. Blood cholesterol can be managed by maintaining an individual's weight.
Also, an individual may engage in physical activity and healthy eating style.
Furthermore, some medications may be recommended for the purpose of keeping
cholesterol in check.
I recommend the patient to reduce weight and engage in physical activity: When it
comes to the quest of controlling cardiovascular disease, it is imperative to engage in not
only physical activity but also weight reduction. Regular physical activity plays a
significant role in minimizing body fat, cholesterol, and lowering blood pressure.
Furthermore, it recommended rehabilitation for patients who have encountered a stroke.
I recommend the patient to manage depression: As viewed under the pathophysiology of
cardiovascular disease, it’s true that depression and stress are predisposing factors (Hare,
Toukhsati, Johansson & Jaarsma, 2013). In fact, the associated pain comes as a result of
depression and stress. Therefore, it is significant for the patient to control personal
identifying if an individual's cholesterol is too high or low. However, it is also significant
to consider one's family history and cultural background when deciding if cholesterol is
too high. But most importantly, cholesterol level above 6.0 calls for reduction actions.
Often, a slow and periodic buildup of cholesterol in the inner lining of the heart's arteries
is the major cause of coronary disease. Bad cholesterol can build up in the arteries
leading to the narrowing of the blood pathway hence interfering with the flow of blood.
Also, narrow arteries can be clogged, thus stopping the flow of blood. As a result, the
failure of blood to arrive in the heart may result in a heart attack or stroke (in the case of
the brain). Such cardiac diseases have great implications for the wellbeing of an
individual. Blood cholesterol can be managed by maintaining an individual's weight.
Also, an individual may engage in physical activity and healthy eating style.
Furthermore, some medications may be recommended for the purpose of keeping
cholesterol in check.
I recommend the patient to reduce weight and engage in physical activity: When it
comes to the quest of controlling cardiovascular disease, it is imperative to engage in not
only physical activity but also weight reduction. Regular physical activity plays a
significant role in minimizing body fat, cholesterol, and lowering blood pressure.
Furthermore, it recommended rehabilitation for patients who have encountered a stroke.
I recommend the patient to manage depression: As viewed under the pathophysiology of
cardiovascular disease, it’s true that depression and stress are predisposing factors (Hare,
Toukhsati, Johansson & Jaarsma, 2013). In fact, the associated pain comes as a result of
depression and stress. Therefore, it is significant for the patient to control personal
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL JUDGMENT AND REASONING 7
depression either through medications, physical activity, or music therapy, depending on
the effectiveness and availability of the program.
I recommend the patient to manage diabetes. Diabetes, especially type two, leads to
depression and anxiety among the patient (American Diabetes Association, 2016). As a
result, patients with diabetes are most likely to develop cardiovascular disease. Therefore,
it is important for patients to know and understand how to manage their diabetic
conditions (American Diabetes Association, 2018). Most importantly, diabetes calls for
lifestyle changes like reduced sugar intake, physical activity, water intake, etc. (Low,
Hess, Hiatt, & Goldfine, 2016). Therefore, it is imperative for patients to understand how
to manage their diabetic conditions.
I recommend specific medications for the patient: Medications may include aspirin which
is found to have reduced the risk of heart attacks and stroke, especially in women
(Anderson et al., 2016). Also, hormone replacement therapy which is taken from the time
of menopause, has been found to minimize the chances of heart disease.
depression either through medications, physical activity, or music therapy, depending on
the effectiveness and availability of the program.
I recommend the patient to manage diabetes. Diabetes, especially type two, leads to
depression and anxiety among the patient (American Diabetes Association, 2016). As a
result, patients with diabetes are most likely to develop cardiovascular disease. Therefore,
it is important for patients to know and understand how to manage their diabetic
conditions (American Diabetes Association, 2018). Most importantly, diabetes calls for
lifestyle changes like reduced sugar intake, physical activity, water intake, etc. (Low,
Hess, Hiatt, & Goldfine, 2016). Therefore, it is imperative for patients to understand how
to manage their diabetic conditions.
I recommend specific medications for the patient: Medications may include aspirin which
is found to have reduced the risk of heart attacks and stroke, especially in women
(Anderson et al., 2016). Also, hormone replacement therapy which is taken from the time
of menopause, has been found to minimize the chances of heart disease.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL JUDGMENT AND REASONING 8
References
Agca, R., Heslinga, S. C., Rollefstad, S., Heslinga, M., McInnes, I. B., Peters, M. J. L., ... &
Primdahl, J. (2017). EULAR recommendations for cardiovascular disease risk
management in patients with rheumatoid arthritis and other forms of inflammatory joint
disorders: 2015/2016 update. Annals of the rheumatic diseases, 76(1), 17-28.
American Diabetes Association. (2016). 8. Cardiovascular disease and risk
management. Diabetes care, 39(Supplement 1), S60-S71.
American Diabetes Association. (2018). 9. Cardiovascular disease and risk management:
standards of medical care in diabetes—2018. Diabetes care, 41(Supplement 1), S86-
S104.
Anderson, T. J., Gregoire, J., Pearson, G. J., Barry, A. R., Couture, P., Dawes, M., ... & Hegele,
R. A. (2016). 2016 Canadian Cardiovascular Society guidelines for the management of
dyslipidemia for the prevention of cardiovascular disease in the adult. Canadian Journal
of Cardiology, 32(11), 1263-1282.
Friedman, K. G., & Alexander, M. E. (2013). Chest pain and syncope in children: a practical
approach to the diagnosis of cardiac disease. The Journal of pediatrics, 163(3), 896-901.
Garra, G., Singer, A. J., Taira, B. R., Chohan, J., Cardoz, H., Chisena, E., & Thode Jr, H. C.
(2010). Validation of the Wong‐Baker FACES pain rating scale in pediatric emergency
department patients. Academic Emergency Medicine, 17(1), 50-54.
Hare, D. L., Toukhsati, S. R., Johansson, P., & Jaarsma, T. (2013). Depression and
cardiovascular disease: a clinical review. European heart journal, 35(21), 1365-1372.
References
Agca, R., Heslinga, S. C., Rollefstad, S., Heslinga, M., McInnes, I. B., Peters, M. J. L., ... &
Primdahl, J. (2017). EULAR recommendations for cardiovascular disease risk
management in patients with rheumatoid arthritis and other forms of inflammatory joint
disorders: 2015/2016 update. Annals of the rheumatic diseases, 76(1), 17-28.
American Diabetes Association. (2016). 8. Cardiovascular disease and risk
management. Diabetes care, 39(Supplement 1), S60-S71.
American Diabetes Association. (2018). 9. Cardiovascular disease and risk management:
standards of medical care in diabetes—2018. Diabetes care, 41(Supplement 1), S86-
S104.
Anderson, T. J., Gregoire, J., Pearson, G. J., Barry, A. R., Couture, P., Dawes, M., ... & Hegele,
R. A. (2016). 2016 Canadian Cardiovascular Society guidelines for the management of
dyslipidemia for the prevention of cardiovascular disease in the adult. Canadian Journal
of Cardiology, 32(11), 1263-1282.
Friedman, K. G., & Alexander, M. E. (2013). Chest pain and syncope in children: a practical
approach to the diagnosis of cardiac disease. The Journal of pediatrics, 163(3), 896-901.
Garra, G., Singer, A. J., Taira, B. R., Chohan, J., Cardoz, H., Chisena, E., & Thode Jr, H. C.
(2010). Validation of the Wong‐Baker FACES pain rating scale in pediatric emergency
department patients. Academic Emergency Medicine, 17(1), 50-54.
Hare, D. L., Toukhsati, S. R., Johansson, P., & Jaarsma, T. (2013). Depression and
cardiovascular disease: a clinical review. European heart journal, 35(21), 1365-1372.
CLINICAL JUDGMENT AND REASONING 9
Kahn, M. R., Robbins, M. J., Kim, M. C., & Fuster, V. (2013). Management of cardiovascular
disease in patients with kidney disease. Nature Reviews Cardiology, 10(5), 261.
Lorber, D. (2014). Importance of cardiovascular disease risk management in patients with type 2
diabetes mellitus. Diabetes, metabolic syndrome, and obesity: targets and therapy, 7,
169.
Low, Wang, C. C., Hess, C. N., Hiatt, W. R., & Goldfine, A. B. (2016). Clinical update:
cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and
heart failure in type 2 diabetes mellitus–mechanisms, management, and clinical
considerations. Circulation, 133(24), 2459-2502.
Munroe, B., Curtis, K., Considine, J., & Buckley, T. (2013). The impact structured patient
assessment frameworks have on patient care: an integrative review. Journal of Clinical
Nursing, 22(21-22), 2991-3005.
Sara, J. D., Widmer, R. J., Matsuzawa, Y., Lennon, R. J., Lerman, L. O., & Lerman, A. (2015).
Prevalence of coronary microvascular dysfunction among patients with chest pain and
nonobstructive coronary artery disease. JACC: Cardiovascular Interventions, 8(11),
1445-1453.
Young, K. D. (2017). Assessment of acute pain in children. Clinical Pediatric Emergency
Medicine, 18(4), 235-241.
Kahn, M. R., Robbins, M. J., Kim, M. C., & Fuster, V. (2013). Management of cardiovascular
disease in patients with kidney disease. Nature Reviews Cardiology, 10(5), 261.
Lorber, D. (2014). Importance of cardiovascular disease risk management in patients with type 2
diabetes mellitus. Diabetes, metabolic syndrome, and obesity: targets and therapy, 7,
169.
Low, Wang, C. C., Hess, C. N., Hiatt, W. R., & Goldfine, A. B. (2016). Clinical update:
cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and
heart failure in type 2 diabetes mellitus–mechanisms, management, and clinical
considerations. Circulation, 133(24), 2459-2502.
Munroe, B., Curtis, K., Considine, J., & Buckley, T. (2013). The impact structured patient
assessment frameworks have on patient care: an integrative review. Journal of Clinical
Nursing, 22(21-22), 2991-3005.
Sara, J. D., Widmer, R. J., Matsuzawa, Y., Lennon, R. J., Lerman, L. O., & Lerman, A. (2015).
Prevalence of coronary microvascular dysfunction among patients with chest pain and
nonobstructive coronary artery disease. JACC: Cardiovascular Interventions, 8(11),
1445-1453.
Young, K. D. (2017). Assessment of acute pain in children. Clinical Pediatric Emergency
Medicine, 18(4), 235-241.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





