Hospital Gastroenteritis Patient Risk and Error Prevention Report
VerifiedAdded on 2023/02/01
|1
|972
|46
Report
AI Summary
This report focuses on a 4-year-old patient, Ruby Bell, hospitalized with gastroenteritis, and the associated risks during her nursing care. It identifies potential clinical errors, including dehydration, food poisoning, and the impact of fever. The report emphasizes the importance of training, communication, and patient education to prevent these errors. Strategies discussed include implementing training programs for nurses, improving communication channels with patients and families, and providing clear explanations of treatment plans and potential risks. The analysis highlights the need for proactive measures to address dehydration, monitor patient conditions, and provide supportive care, particularly in cases where parental support is limited. The report underscores the significance of patient-centered care in managing gastroenteritis and preventing adverse outcomes, offering insights into effective nursing interventions to improve patient safety and recovery.
CLINICAL PRACTICE AND GASTROENTERITIS
Identify chosen patient
Ruby Bell is the chosen patient who is a 4 year old kid and hospitalised with gastroenteritis. Her parents were
taking turns to stay with her in hospital, but many times, they were not been able to give their time due to
responsibilities towards their other children at home.
Description of risk with respect to clinical errors
There are several factors that put the patients like Ruby to risks whilst in hospital receiving nursing care. It
has been demonstrated that gastroenteritis is one of the communicable diseases that can further cause food
poisoning. This has mostly affected people with weak immunity levels and it is mostly takes place due to
viruses such as adenovirus, rotavirus etc. (Humphries and Linscott, 2015) The major implications consists of
diarrhoea, feeling nauseous or runny water, vomiting and also leads to fever and tummy pains. However, these
can be treated but there is possibility of risks and other uncertain challenges that put Ruby's well being at
stake.
The major effect on Ruby is an imbalance in electrolytes due to constant vomiting and diarrhoea. Moreover,
she might get headaches, weakness and body aches which leads to more risks in her recovery. In absence of
her parents, the nurses should have been more approachable to make her understand about infection and its
effects. The patient must be kept separately since the disease spreads easily and also precautionary measures
like hand washing, cleanliness while using wash-rooms should have been encouraged to practise (Cianferoni
and Spergel, 2015). Along with, the major risk is dehydration which must not be entertained and body fluids
must be monitored properly to avoid any formation of risks.
Consequences of clinical errors that may result during their hospitalisation
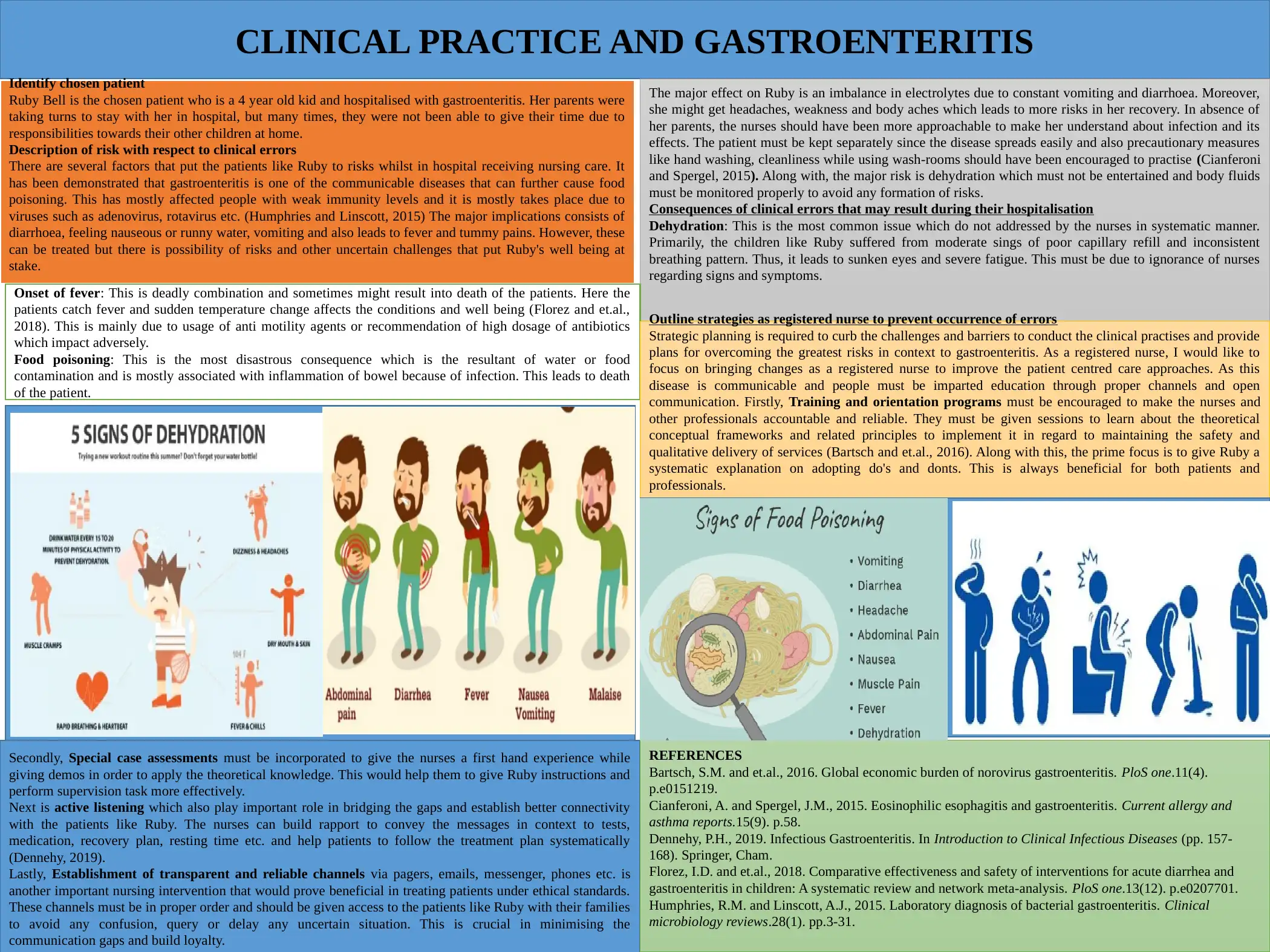
Dehydration: This is the most common issue which do not addressed by the nurses in systematic manner.
Primarily, the children like Ruby suffered from moderate sings of poor capillary refill and inconsistent
breathing pattern. Thus, it leads to sunken eyes and severe fatigue. This must be due to ignorance of nurses
regarding signs and symptoms.
Onset of fever: This is deadly combination and sometimes might result into death of the patients. Here the
patients catch fever and sudden temperature change affects the conditions and well being (Florez and et.al.,
2018). This is mainly due to usage of anti motility agents or recommendation of high dosage of antibiotics
which impact adversely.
Food poisoning: This is the most disastrous consequence which is the resultant of water or food
contamination and is mostly associated with inflammation of bowel because of infection. This leads to death
of the patient.
Outline strategies as registered nurse to prevent occurrence of errors
Strategic planning is required to curb the challenges and barriers to conduct the clinical practises and provide
plans for overcoming the greatest risks in context to gastroenteritis. As a registered nurse, I would like to
focus on bringing changes as a registered nurse to improve the patient centred care approaches. As this
disease is communicable and people must be imparted education through proper channels and open
communication. Firstly, Training and orientation programs must be encouraged to make the nurses and
other professionals accountable and reliable. They must be given sessions to learn about the theoretical
conceptual frameworks and related principles to implement it in regard to maintaining the safety and
qualitative delivery of services (Bartsch and et.al., 2016). Along with this, the prime focus is to give Ruby a
systematic explanation on adopting do's and donts. This is always beneficial for both patients and
professionals.
Secondly, Special case assessments must be incorporated to give the nurses a first hand experience while
giving demos in order to apply the theoretical knowledge. This would help them to give Ruby instructions and
perform supervision task more effectively.
Next is active listening which also play important role in bridging the gaps and establish better connectivity
with the patients like Ruby. The nurses can build rapport to convey the messages in context to tests,
medication, recovery plan, resting time etc. and help patients to follow the treatment plan systematically
(Dennehy, 2019).
Lastly, Establishment of transparent and reliable channels via pagers, emails, messenger, phones etc. is
another important nursing intervention that would prove beneficial in treating patients under ethical standards.
These channels must be in proper order and should be given access to the patients like Ruby with their families
to avoid any confusion, query or delay any uncertain situation. This is crucial in minimising the
communication gaps and build loyalty.
REFERENCES
Bartsch, S.M. and et.al., 2016. Global economic burden of norovirus gastroenteritis. PloS one.11(4).
p.e0151219.
Cianferoni, A. and Spergel, J.M., 2015. Eosinophilic esophagitis and gastroenteritis. Current allergy and
asthma reports.15(9). p.58.
Dennehy, P.H., 2019. Infectious Gastroenteritis. In Introduction to Clinical Infectious Diseases (pp. 157-
168). Springer, Cham.
Florez, I.D. and et.al., 2018. Comparative effectiveness and safety of interventions for acute diarrhea and
gastroenteritis in children: A systematic review and network meta-analysis. PloS one.13(12). p.e0207701.
Humphries, R.M. and Linscott, A.J., 2015. Laboratory diagnosis of bacterial gastroenteritis. Clinical
microbiology reviews.28(1). pp.3-31.
Identify chosen patient
Ruby Bell is the chosen patient who is a 4 year old kid and hospitalised with gastroenteritis. Her parents were
taking turns to stay with her in hospital, but many times, they were not been able to give their time due to
responsibilities towards their other children at home.
Description of risk with respect to clinical errors
There are several factors that put the patients like Ruby to risks whilst in hospital receiving nursing care. It
has been demonstrated that gastroenteritis is one of the communicable diseases that can further cause food
poisoning. This has mostly affected people with weak immunity levels and it is mostly takes place due to
viruses such as adenovirus, rotavirus etc. (Humphries and Linscott, 2015) The major implications consists of
diarrhoea, feeling nauseous or runny water, vomiting and also leads to fever and tummy pains. However, these
can be treated but there is possibility of risks and other uncertain challenges that put Ruby's well being at
stake.
The major effect on Ruby is an imbalance in electrolytes due to constant vomiting and diarrhoea. Moreover,
she might get headaches, weakness and body aches which leads to more risks in her recovery. In absence of
her parents, the nurses should have been more approachable to make her understand about infection and its
effects. The patient must be kept separately since the disease spreads easily and also precautionary measures
like hand washing, cleanliness while using wash-rooms should have been encouraged to practise (Cianferoni
and Spergel, 2015). Along with, the major risk is dehydration which must not be entertained and body fluids
must be monitored properly to avoid any formation of risks.
Consequences of clinical errors that may result during their hospitalisation
Dehydration: This is the most common issue which do not addressed by the nurses in systematic manner.
Primarily, the children like Ruby suffered from moderate sings of poor capillary refill and inconsistent
breathing pattern. Thus, it leads to sunken eyes and severe fatigue. This must be due to ignorance of nurses
regarding signs and symptoms.
Onset of fever: This is deadly combination and sometimes might result into death of the patients. Here the
patients catch fever and sudden temperature change affects the conditions and well being (Florez and et.al.,
2018). This is mainly due to usage of anti motility agents or recommendation of high dosage of antibiotics
which impact adversely.
Food poisoning: This is the most disastrous consequence which is the resultant of water or food
contamination and is mostly associated with inflammation of bowel because of infection. This leads to death
of the patient.
Outline strategies as registered nurse to prevent occurrence of errors
Strategic planning is required to curb the challenges and barriers to conduct the clinical practises and provide
plans for overcoming the greatest risks in context to gastroenteritis. As a registered nurse, I would like to
focus on bringing changes as a registered nurse to improve the patient centred care approaches. As this
disease is communicable and people must be imparted education through proper channels and open
communication. Firstly, Training and orientation programs must be encouraged to make the nurses and
other professionals accountable and reliable. They must be given sessions to learn about the theoretical
conceptual frameworks and related principles to implement it in regard to maintaining the safety and
qualitative delivery of services (Bartsch and et.al., 2016). Along with this, the prime focus is to give Ruby a
systematic explanation on adopting do's and donts. This is always beneficial for both patients and
professionals.
Secondly, Special case assessments must be incorporated to give the nurses a first hand experience while
giving demos in order to apply the theoretical knowledge. This would help them to give Ruby instructions and
perform supervision task more effectively.
Next is active listening which also play important role in bridging the gaps and establish better connectivity
with the patients like Ruby. The nurses can build rapport to convey the messages in context to tests,
medication, recovery plan, resting time etc. and help patients to follow the treatment plan systematically
(Dennehy, 2019).
Lastly, Establishment of transparent and reliable channels via pagers, emails, messenger, phones etc. is
another important nursing intervention that would prove beneficial in treating patients under ethical standards.
These channels must be in proper order and should be given access to the patients like Ruby with their families
to avoid any confusion, query or delay any uncertain situation. This is crucial in minimising the
communication gaps and build loyalty.
REFERENCES
Bartsch, S.M. and et.al., 2016. Global economic burden of norovirus gastroenteritis. PloS one.11(4).
p.e0151219.
Cianferoni, A. and Spergel, J.M., 2015. Eosinophilic esophagitis and gastroenteritis. Current allergy and
asthma reports.15(9). p.58.
Dennehy, P.H., 2019. Infectious Gastroenteritis. In Introduction to Clinical Infectious Diseases (pp. 157-
168). Springer, Cham.
Florez, I.D. and et.al., 2018. Comparative effectiveness and safety of interventions for acute diarrhea and
gastroenteritis in children: A systematic review and network meta-analysis. PloS one.13(12). p.e0207701.
Humphries, R.M. and Linscott, A.J., 2015. Laboratory diagnosis of bacterial gastroenteritis. Clinical
microbiology reviews.28(1). pp.3-31.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





