Nursing Case Study: Clinical Prioritization in Emergency Care
VerifiedAdded on 2023/01/05
|11
|3646
|88
Case Study
AI Summary
This nursing case study presents a detailed assessment of a 79-year-old male admitted to the emergency department with shortness of breath, bilateral extremity swelling, and reduced urinary output. The case study utilizes the HIRAID framework (History, Identify Red flags, Assessment, Interventions, Diagnostics, reassessment and communication) to evaluate subjective and objective data, including vital signs and diagnostic values. The patient's medical history includes hypertension, coronary artery disease, and sleep apnea. Clinical priorities identified are ineffective breathing pattern, ineffective airway clearance, activity intolerance, and inappropriate voiding pattern. The study emphasizes the importance of informed consent, recognizing red flags, and implementing structured assessment frameworks to improve patient outcomes in the emergency department. The case highlights the need for interventions related to respiratory distress, activity intolerance, and potential complications such as anemia and malnutrition, offering insights into effective nursing care and clinical decision-making.
Nursing Case Study
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Nursing assessment framework:
Evidence suggested that structured nursing assessment frame comprises of History, Identify
Red flags, Assessment, Interventions, Diagnostics, reassessment and communication.
(HIRAID) proved beneficial in the comprehensive assessment of patient to identify patient’s
clinical priorities. HIRAID proved beneficial in improving patient safety (Munroe, Curtis,
Murphy, Strachan, and Buckley, 2015). This assessment frame is most suitable in nursing
practice because assessment is central to the nursing practice and clinical decision making.
Safe and effective care depends on effective assessment. Patients in the Emergency
department (ED) are unique in comparison to other clinical areas because patients are usually
associated with multiple complaints, broad-spectrum signs and symptoms and without
previous diagnosis. It is evident that occurrence of preventable adverse effects and errors in
the ED ranges from 37-72 %. Most of these adverse events and errors are related to improper
clinical assessment, wrong diagnosis and medication errors. These errors can be effectively
reduced through implementation of structured assessment framework. Evidence also reported
that structured assessment framework is beneficial in improving clinical documentation,
clinical practice and patient outcome. It is also beneficial in readily identifying patient’s
deterioration. HIRAID is beneficial in identifying gaps in the clinical practice because it
comprises of seven components (Munroe, Curtis, Buckley, Lewis, and Atkins, 2018). It
provides systematic guide for clinical assessment of the patient. Structured assessment
framework is also useful in reducing anxiety of nurses and improving their self-efficacy and
self-efficiency. Different components of the structured assessment framework are useful in
collecting relevant and patient specific information. Collection of information related to
history is useful in gathering patient’s current problem and patient’s health history because it
directs physical assessment and inspire investigations and priorities for patient health services
(Munroe et al., 2016). Identification of red flags are helpful in the recognising historical and
physiological critical signs of emergency which reflect patient’s critical illness and potential
deterioration. Identification of red flags is important because judicious recognition of critical
illness indicators is helpful in escalating care and providing suitable clinical response to
reduce morbidity and mortality. Assessment is beneficial in gathering information through
primary survey, vital signs and targeted assessments. Assessment is necessary because it is
beneficial in identification of signs and symptoms of patient’s condition, formulating
diagnosis and informing treatment (Munroe et al., 2016).
2
Evidence suggested that structured nursing assessment frame comprises of History, Identify
Red flags, Assessment, Interventions, Diagnostics, reassessment and communication.
(HIRAID) proved beneficial in the comprehensive assessment of patient to identify patient’s
clinical priorities. HIRAID proved beneficial in improving patient safety (Munroe, Curtis,
Murphy, Strachan, and Buckley, 2015). This assessment frame is most suitable in nursing
practice because assessment is central to the nursing practice and clinical decision making.
Safe and effective care depends on effective assessment. Patients in the Emergency
department (ED) are unique in comparison to other clinical areas because patients are usually
associated with multiple complaints, broad-spectrum signs and symptoms and without
previous diagnosis. It is evident that occurrence of preventable adverse effects and errors in
the ED ranges from 37-72 %. Most of these adverse events and errors are related to improper
clinical assessment, wrong diagnosis and medication errors. These errors can be effectively
reduced through implementation of structured assessment framework. Evidence also reported
that structured assessment framework is beneficial in improving clinical documentation,
clinical practice and patient outcome. It is also beneficial in readily identifying patient’s
deterioration. HIRAID is beneficial in identifying gaps in the clinical practice because it
comprises of seven components (Munroe, Curtis, Buckley, Lewis, and Atkins, 2018). It
provides systematic guide for clinical assessment of the patient. Structured assessment
framework is also useful in reducing anxiety of nurses and improving their self-efficacy and
self-efficiency. Different components of the structured assessment framework are useful in
collecting relevant and patient specific information. Collection of information related to
history is useful in gathering patient’s current problem and patient’s health history because it
directs physical assessment and inspire investigations and priorities for patient health services
(Munroe et al., 2016). Identification of red flags are helpful in the recognising historical and
physiological critical signs of emergency which reflect patient’s critical illness and potential
deterioration. Identification of red flags is important because judicious recognition of critical
illness indicators is helpful in escalating care and providing suitable clinical response to
reduce morbidity and mortality. Assessment is beneficial in gathering information through
primary survey, vital signs and targeted assessments. Assessment is necessary because it is
beneficial in identification of signs and symptoms of patient’s condition, formulating
diagnosis and informing treatment (Munroe et al., 2016).
2
Informed consent:
Written informed consent form was taken form Mr. A. Consent form is helpful in providing
information related to assessment procedure and treatment to Mr. A. Informed consent form
is useful in providing information to Mr. A about risks and benefits of the procedures, to take
opinion of Mr. A about the procedures, to give opportunity for Mr. A to ask questions until
his satisfaction, to discuss with family members, to take decision and to inform doctor about
his decisions. Informed consent is important for Mr. A because his older age might not allow
him to take proper decision (Cocanour et al., 2017).
Subjective data:
A 79-year male, named A was admitted to the Emergency department (ED) of the XYZ
medical centre. He complained that his condition was gradually falling; since last 10 days due
to shortness of breath. He also mentioned that he was experiencing relief after rest. He also
stated that he was experiencing bilateral extremity swelling and reduced urinary output over
last 10 days. He was experiencing reduced capability of daily activities of living due to
shortness of breath and swelling in the extremity. Upon enquiry, he disagrees other symptoms
like chest pain, palpitations, orthopnea, cough, fever, or chills. Patient’s past medical history
indicate hypertension, hyperlipidaemia, coronary artery disease, and sleep apnea (on CPAP at
eight). On social front, he agrees that he was a smoker for almost 40 years with
approximately 10 cigarettes per day; however, he quit smoking since last three years.
Moreover, he mentioned that he was chewing tobacco after quitting smoking. He was
habituated to alcohol or illegal drugs. He stated that he never experienced food and
medication allergies. After reviewing symptoms, it was evident that he was experiencing
shortness of breath after exertion, general fatigue and alteration in the weight due to swelling
in the extremities. He was living alone; since, his wife expired five years ago. His son was
staying approximately 200 km away from him. Since, he keeps on visiting Mr. A monthly
once.
Objective data :
Vital signs : Following were the observed vital signs upon his admission.
Body temperature : 36.2̊C (normal range 36.5̊C-37.2̊C)
Blood pressure: 134/75 mmHg (normal BP in adults above 70 years 140/90 mmHg)
Hear rate : 62 beats per minute (bpm) (normal range 60 – 100 bpm)
3
Written informed consent form was taken form Mr. A. Consent form is helpful in providing
information related to assessment procedure and treatment to Mr. A. Informed consent form
is useful in providing information to Mr. A about risks and benefits of the procedures, to take
opinion of Mr. A about the procedures, to give opportunity for Mr. A to ask questions until
his satisfaction, to discuss with family members, to take decision and to inform doctor about
his decisions. Informed consent is important for Mr. A because his older age might not allow
him to take proper decision (Cocanour et al., 2017).
Subjective data:
A 79-year male, named A was admitted to the Emergency department (ED) of the XYZ
medical centre. He complained that his condition was gradually falling; since last 10 days due
to shortness of breath. He also mentioned that he was experiencing relief after rest. He also
stated that he was experiencing bilateral extremity swelling and reduced urinary output over
last 10 days. He was experiencing reduced capability of daily activities of living due to
shortness of breath and swelling in the extremity. Upon enquiry, he disagrees other symptoms
like chest pain, palpitations, orthopnea, cough, fever, or chills. Patient’s past medical history
indicate hypertension, hyperlipidaemia, coronary artery disease, and sleep apnea (on CPAP at
eight). On social front, he agrees that he was a smoker for almost 40 years with
approximately 10 cigarettes per day; however, he quit smoking since last three years.
Moreover, he mentioned that he was chewing tobacco after quitting smoking. He was
habituated to alcohol or illegal drugs. He stated that he never experienced food and
medication allergies. After reviewing symptoms, it was evident that he was experiencing
shortness of breath after exertion, general fatigue and alteration in the weight due to swelling
in the extremities. He was living alone; since, his wife expired five years ago. His son was
staying approximately 200 km away from him. Since, he keeps on visiting Mr. A monthly
once.
Objective data :
Vital signs : Following were the observed vital signs upon his admission.
Body temperature : 36.2̊C (normal range 36.5̊C-37.2̊C)
Blood pressure: 134/75 mmHg (normal BP in adults above 70 years 140/90 mmHg)
Hear rate : 62 beats per minute (bpm) (normal range 60 – 100 bpm)
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Respiratory rate : 34 breaths per minute (bpm) (normal range 10 – 30 breathe per minute)
PaO2 : 86 % on room air (normal range above 94 %).
Measured body temperature in Mr. A was slightly lower than the normal body temperature.
However, it can not be considered as hypothermic temperature. Systolic blood pressure in
Mr. A can be considered close to normal blood pressure; however diastolic blood pressure
should be considered as low blood pressure because it much less than the normal diastolic
pressure of his age group. Though, his heart was determined in the normal range, it should be
considered in the lower range because it is almost near to lower threshold of heart rate (Mok,
Wang, and Liaw, 2015). Respiratory rate and percentage oxygen saturation in Mr. A were
deviating from the normal range.
Mr. A exhibited alertness to time, place and self and it was evident that he was awake. He
was neurologically intact; however, he stated that he was experiencing equivalent bilateral
weakness on both upper and lower extremities.
Following were his diagnostic values:
WBC – 7.2 X 10-3/mL (4.0 to 10.5 X 10-3/mL)
Hemoglobin – 9.5 g/dL (14.0 to 18.0 g/dL)
Hematocrit – 28.8 % (42.0 – 25.0 %)
Platelets – 192 X 10-3/ mL (140 – 415 X 10-3/ mL)
Creatinine – 1.65 mg/dL (0.7 – 1.4 mg/dL)
Albumin – 3.0 g/dL (3.5 – 5.0 g/dL)
BNP – 330 pg/mL (normal range less than 100 pg/mL)
White blood cell (WBC) and platelet count in Mr. A were in the normal range which indicate
there was no inflammation. Hemoglobin and haematocrit levels were in the lower range
which indicate signs of anemia for Mr. A. Increased levels of creatinine was observed in Mr.
A which might be due to reduced clearance of creatinine by the kidneys. Reduced levels of
blood albumin was observed in Mr. A. Reduced levels of blood albumin usually occur due
inflammation or malnutrition. Since, blood count indicate, there was no inflammation in Mr.
A, reduced blood albumin levels might be due to malnutrition. Increased B-type natriuretic
4
PaO2 : 86 % on room air (normal range above 94 %).
Measured body temperature in Mr. A was slightly lower than the normal body temperature.
However, it can not be considered as hypothermic temperature. Systolic blood pressure in
Mr. A can be considered close to normal blood pressure; however diastolic blood pressure
should be considered as low blood pressure because it much less than the normal diastolic
pressure of his age group. Though, his heart was determined in the normal range, it should be
considered in the lower range because it is almost near to lower threshold of heart rate (Mok,
Wang, and Liaw, 2015). Respiratory rate and percentage oxygen saturation in Mr. A were
deviating from the normal range.
Mr. A exhibited alertness to time, place and self and it was evident that he was awake. He
was neurologically intact; however, he stated that he was experiencing equivalent bilateral
weakness on both upper and lower extremities.
Following were his diagnostic values:
WBC – 7.2 X 10-3/mL (4.0 to 10.5 X 10-3/mL)
Hemoglobin – 9.5 g/dL (14.0 to 18.0 g/dL)
Hematocrit – 28.8 % (42.0 – 25.0 %)
Platelets – 192 X 10-3/ mL (140 – 415 X 10-3/ mL)
Creatinine – 1.65 mg/dL (0.7 – 1.4 mg/dL)
Albumin – 3.0 g/dL (3.5 – 5.0 g/dL)
BNP – 330 pg/mL (normal range less than 100 pg/mL)
White blood cell (WBC) and platelet count in Mr. A were in the normal range which indicate
there was no inflammation. Hemoglobin and haematocrit levels were in the lower range
which indicate signs of anemia for Mr. A. Increased levels of creatinine was observed in Mr.
A which might be due to reduced clearance of creatinine by the kidneys. Reduced levels of
blood albumin was observed in Mr. A. Reduced levels of blood albumin usually occur due
inflammation or malnutrition. Since, blood count indicate, there was no inflammation in Mr.
A, reduced blood albumin levels might be due to malnutrition. Increased B-type natriuretic
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
peptide (BNP) indicate mild hypertension in Mr. A (Wood, Chaboyer, and Carr, 2019; Odell,
2015).
His heart rate was exhibiting normal sinus rhythm and heart sounds S1, S2. Lungs are clear in
the upper lobes with equal expansion. His capillary refill was within the normal range and
negative demonstration of use of accessory muscles or clubbing. His skin was observed as
intact and pink. Bowl sounds were recorded in all the quadrants with negative impression of
pain. Mr. A was passing less amount of urine with clear yellow urine without much difficulty.
He emptied his bowel in morning for the last time and it was without diarrhoea or melena.
Clinical prioritise:
Collection of the information about medical history, subjective and objective data and
analysis of the data indicate; he is associated with respiratory distress. Hence, clinical
prioritise identified in Mr. A are ineffective breathing pattern, ineffective airway clearance,
activity intolerance and inappropriate voiding pattern. Ineffective breathing pattern mainly
occurs in Mr. A due to alteration in the breathing rate. Normal breathing rate should be
between 10 – 30 bpm. However, observed breathing rate in Mr. is 34 bpm. Ineffective
breathing pattern is important clinical priority in Mr. A because it essential to maintain
normal breathing pattern in him; since, altered breathing pattern affects multiple
physiological processes in him. Altered breathing pattern might lead to altered ABG (arterial
blood gas) in Mr. A. Altered ABG lead to reduced supply of oxygen to different cells and
tissues which adversely affect multiple physiological processes. Prioritising ineffective
breathing in Mr. A is also essential because he might be associated with lung infection and
lung inflammation; since, ineffective breathing is the prominent symptoms of lung
dysfunction. Moreover, he was associated with the smoking for the longer duration of his life.
Smoking is one of the most important risk factors for the development of lung diseases like
asthma and chronic obstructive lung disease (COPD) (Wang, Tan, Xiao, and Deng, 2017).
Prioritising ineffective breathing in Mr. A is also important because reduced intake of oxygen
might lead to increased ventilation during performing activities. In case of Mr. also it has
been observed that his breathing rate was normal during rest and increased during exercise
and performing activities. It is also evident that Mr. A was not able to perform his activities
of daily living. It might affect his routine activities and produce psychological stress in him.
Effective breathing requires coordination between diaphragm, abdominal muscles, and
muscles of rib cage. However, ineffective breathing might increase load on diaphragm and
5
2015).
His heart rate was exhibiting normal sinus rhythm and heart sounds S1, S2. Lungs are clear in
the upper lobes with equal expansion. His capillary refill was within the normal range and
negative demonstration of use of accessory muscles or clubbing. His skin was observed as
intact and pink. Bowl sounds were recorded in all the quadrants with negative impression of
pain. Mr. A was passing less amount of urine with clear yellow urine without much difficulty.
He emptied his bowel in morning for the last time and it was without diarrhoea or melena.
Clinical prioritise:
Collection of the information about medical history, subjective and objective data and
analysis of the data indicate; he is associated with respiratory distress. Hence, clinical
prioritise identified in Mr. A are ineffective breathing pattern, ineffective airway clearance,
activity intolerance and inappropriate voiding pattern. Ineffective breathing pattern mainly
occurs in Mr. A due to alteration in the breathing rate. Normal breathing rate should be
between 10 – 30 bpm. However, observed breathing rate in Mr. is 34 bpm. Ineffective
breathing pattern is important clinical priority in Mr. A because it essential to maintain
normal breathing pattern in him; since, altered breathing pattern affects multiple
physiological processes in him. Altered breathing pattern might lead to altered ABG (arterial
blood gas) in Mr. A. Altered ABG lead to reduced supply of oxygen to different cells and
tissues which adversely affect multiple physiological processes. Prioritising ineffective
breathing in Mr. A is also essential because he might be associated with lung infection and
lung inflammation; since, ineffective breathing is the prominent symptoms of lung
dysfunction. Moreover, he was associated with the smoking for the longer duration of his life.
Smoking is one of the most important risk factors for the development of lung diseases like
asthma and chronic obstructive lung disease (COPD) (Wang, Tan, Xiao, and Deng, 2017).
Prioritising ineffective breathing in Mr. A is also important because reduced intake of oxygen
might lead to increased ventilation during performing activities. In case of Mr. also it has
been observed that his breathing rate was normal during rest and increased during exercise
and performing activities. It is also evident that Mr. A was not able to perform his activities
of daily living. It might affect his routine activities and produce psychological stress in him.
Effective breathing requires coordination between diaphragm, abdominal muscles, and
muscles of rib cage. However, ineffective breathing might increase load on diaphragm and
5
muscles of abdomen and rib cages (Baroi, McNamara, McKenzie, Gandevia, and Brodie,
2018). Hence, it would consume more energy producing weakness and lethargy in him.
Moreover, he was also exhibiting anaemia. Ineffective breathing pattern also might occur due
to psychological factors like stress, anxiety and fear. Hence, prioritising and assessing
ineffective breathing pattern in Mr. A is essential to rule out other possibilities of ineffective
breathing. It is essential to prioritise the ineffective breathing pattern in Mr. A because it
would be helpful in the improving pulmonary ventilation and oxygenation, promoting ease
and comfort of breathing, improving capabilities to participate in daily activities, reducing
skin and tissue breakdown, improving acid-balance and minimising feeling of social isolation
and hopelessness (Yang et al., 2017).
Ineffective airway clearance is another clinical priority which need to be considered in case
of Mr. A. Ineffective airway clearance lead to airway obstruction which might lead to
increased breathing rate, altered breathing pattern and use of accessory muscles like
abdominal and rib cage muscles. All these conditions are evident in Mr. A. Ineffective airway
clearance usually occur due to deposition of secretions in the airways. Deposition of
secretions in the airways might increase susceptibility to infection. Moreover, evidence
suggested that patients with respiratory distress are prone to infection as compared to the
normal people. Infection in patients with respiratory distress might lead to sepsis; hence,
there can be multiple organ dysfunction. Moreover, older age of Mr. A also prone to produce
multiple organ dysfunction at faster rate. Infection and ineffective airway clearance might
lead to the ineffective breathing pattern which might lead to inability of Mr. A to maintain
normal ventilation to sustain normal life. Evidence, also suggested that constant nursing care
is necessary to monitor infection susceptibility and to clear the respiratory tract (Yang et al.,
2017).
Activity intolerance is another clinical priority which need to be addressed in case of Mr.A.
Activity intolerance might occur in him due to generalised weakness, imbalance in demand
and supply of oxygen due to shortness of breath. It is necessary to address this clinical
priority in Mr. A because he needs to perform his normal activities on regular basis to
maintain his health and well-being. It is also useful to maintain his personal hygiene. It is
necessary to address activity intolerance in him because it would be helpful in improving his
nutritional status also. Adequate amount of nutrients and energy are required for maintaining
normal activities in him. However, from the data it is evident that he is associated with
deficient in nutrients. His blood albumin level is below normal level. Activity intolerance is
6
2018). Hence, it would consume more energy producing weakness and lethargy in him.
Moreover, he was also exhibiting anaemia. Ineffective breathing pattern also might occur due
to psychological factors like stress, anxiety and fear. Hence, prioritising and assessing
ineffective breathing pattern in Mr. A is essential to rule out other possibilities of ineffective
breathing. It is essential to prioritise the ineffective breathing pattern in Mr. A because it
would be helpful in the improving pulmonary ventilation and oxygenation, promoting ease
and comfort of breathing, improving capabilities to participate in daily activities, reducing
skin and tissue breakdown, improving acid-balance and minimising feeling of social isolation
and hopelessness (Yang et al., 2017).
Ineffective airway clearance is another clinical priority which need to be considered in case
of Mr. A. Ineffective airway clearance lead to airway obstruction which might lead to
increased breathing rate, altered breathing pattern and use of accessory muscles like
abdominal and rib cage muscles. All these conditions are evident in Mr. A. Ineffective airway
clearance usually occur due to deposition of secretions in the airways. Deposition of
secretions in the airways might increase susceptibility to infection. Moreover, evidence
suggested that patients with respiratory distress are prone to infection as compared to the
normal people. Infection in patients with respiratory distress might lead to sepsis; hence,
there can be multiple organ dysfunction. Moreover, older age of Mr. A also prone to produce
multiple organ dysfunction at faster rate. Infection and ineffective airway clearance might
lead to the ineffective breathing pattern which might lead to inability of Mr. A to maintain
normal ventilation to sustain normal life. Evidence, also suggested that constant nursing care
is necessary to monitor infection susceptibility and to clear the respiratory tract (Yang et al.,
2017).
Activity intolerance is another clinical priority which need to be addressed in case of Mr.A.
Activity intolerance might occur in him due to generalised weakness, imbalance in demand
and supply of oxygen due to shortness of breath. It is necessary to address this clinical
priority in Mr. A because he needs to perform his normal activities on regular basis to
maintain his health and well-being. It is also useful to maintain his personal hygiene. It is
necessary to address activity intolerance in him because it would be helpful in improving his
nutritional status also. Adequate amount of nutrients and energy are required for maintaining
normal activities in him. However, from the data it is evident that he is associated with
deficient in nutrients. His blood albumin level is below normal level. Activity intolerance is
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
also associated with cardiopulmonary functions. Moreover, it is evident that his breathing rate
is increasing with activity or exertion. Evidence also suggested that heart failure is also
responsible for activity intolerance. Hence, it is necessary to address activity intolerance to
perform activities without much effect on cardiopulmonary functions of Mr. A (Ladwig,
Ackley, and Makic, 2016). Anaemia is also one of the major contributing factors for
weakness and activity intolerance. Hence, it is necessary to prioritise activity intolerance in
Mr. A to address causative factors for activity intolerance in him. In addition to the
generalised weakness, activity intolerance can also occur secondary to acute or chronic
illness. Mr. A is associated with both cardiovascular and pulmonary disorders which are
mainly responsible for the activity intolerance. Aging is also one of the major contributory
factors for the activity intolerance due to reduction in strength and function of muscles.
Hence, age of Mr. A can also be contributory factor for activity intolerance in Mr. A. Activity
intolerance for the longer duration of time can lead to the development of psychological
stress and depression. Moreover, it can also lead to social isolation of Mr. A. Hence, all these
factors can exaggerate his physical and mental health (Ladwig, Ackley, and Makic, 2016).
Mr. A’s inappropriate voiding pattern is another clinical priority which need to be addressed.
Inappropriate voiding pattern in Mr. A might be due to heart failure which produce reduced
urinary output, increased blood BNP and creatinine levels. Prioritising inappropriate voiding
pattern in Mr. A is important because it might occur due to infection and obstruction in the
bladder. Hence, it is necessary to identify exact cause of voiding problem in Mr. A. Age is
also one of the important factors for the inappropriate voiding pattern in Mr. A. Voiding
problem is associated with multiple dysfunctions like frequency and urgency, urge
incontinence, voiding difficulty and urinary retention. All these dysfunctions can lead to
multiple abnormalities due to retention of toxic and unwanted substances in the body.
Implications:
Application of the structured assessment framework would be helpful in improving clinical
practice through enhancement in the patient assessment. It would also be helpful in reducing
chances of wrong collection of data and wrong interpretation of the collected data. It is
necessary to integrate the structured assessment framework in the nursing and clinical
education programme to improve capability of nurses for systematic assessment approach to
deliver safe patient care. Further evaluation of the structured assessment programme is
necessary to get more insight into the assessment and improve clinical performance. It can be
7
is increasing with activity or exertion. Evidence also suggested that heart failure is also
responsible for activity intolerance. Hence, it is necessary to address activity intolerance to
perform activities without much effect on cardiopulmonary functions of Mr. A (Ladwig,
Ackley, and Makic, 2016). Anaemia is also one of the major contributing factors for
weakness and activity intolerance. Hence, it is necessary to prioritise activity intolerance in
Mr. A to address causative factors for activity intolerance in him. In addition to the
generalised weakness, activity intolerance can also occur secondary to acute or chronic
illness. Mr. A is associated with both cardiovascular and pulmonary disorders which are
mainly responsible for the activity intolerance. Aging is also one of the major contributory
factors for the activity intolerance due to reduction in strength and function of muscles.
Hence, age of Mr. A can also be contributory factor for activity intolerance in Mr. A. Activity
intolerance for the longer duration of time can lead to the development of psychological
stress and depression. Moreover, it can also lead to social isolation of Mr. A. Hence, all these
factors can exaggerate his physical and mental health (Ladwig, Ackley, and Makic, 2016).
Mr. A’s inappropriate voiding pattern is another clinical priority which need to be addressed.
Inappropriate voiding pattern in Mr. A might be due to heart failure which produce reduced
urinary output, increased blood BNP and creatinine levels. Prioritising inappropriate voiding
pattern in Mr. A is important because it might occur due to infection and obstruction in the
bladder. Hence, it is necessary to identify exact cause of voiding problem in Mr. A. Age is
also one of the important factors for the inappropriate voiding pattern in Mr. A. Voiding
problem is associated with multiple dysfunctions like frequency and urgency, urge
incontinence, voiding difficulty and urinary retention. All these dysfunctions can lead to
multiple abnormalities due to retention of toxic and unwanted substances in the body.
Implications:
Application of the structured assessment framework would be helpful in improving clinical
practice through enhancement in the patient assessment. It would also be helpful in reducing
chances of wrong collection of data and wrong interpretation of the collected data. It is
necessary to integrate the structured assessment framework in the nursing and clinical
education programme to improve capability of nurses for systematic assessment approach to
deliver safe patient care. Further evaluation of the structured assessment programme is
necessary to get more insight into the assessment and improve clinical performance. It can be
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

used as the intrinsic and instrumental tool in achieving the nursing goals. It is useful in the
assessment of the patient through holistic approach comprising of physical, psychological and
sociological approach (Munroe et al., 2016). Clinical priority setting is a useful skill in the
nursing practice and effective implementation of it can be achieved through proper education
and training. Hence, nurse should be experienced to make decisions on clinical priority. It is
necessary for the nurse to organise the problems on the priority basis and to establish the
preferential order. Nurse should have expertise in integrating different aspects like patient
condition, resources availability, models of care, ward organisation, nurse-patient relationship
and cognitive strategy for effectively identifying clinical prioritise (Coster, Watkins , and
Norman, 2018).
8
assessment of the patient through holistic approach comprising of physical, psychological and
sociological approach (Munroe et al., 2016). Clinical priority setting is a useful skill in the
nursing practice and effective implementation of it can be achieved through proper education
and training. Hence, nurse should be experienced to make decisions on clinical priority. It is
necessary for the nurse to organise the problems on the priority basis and to establish the
preferential order. Nurse should have expertise in integrating different aspects like patient
condition, resources availability, models of care, ward organisation, nurse-patient relationship
and cognitive strategy for effectively identifying clinical prioritise (Coster, Watkins , and
Norman, 2018).
8
References:
Baroi, S., McNamara, R.J., McKenzie, D.K., Gandevia, S., and Brodie, M.A. (2018).
Advances in Remote Respiratory Assessments for People with Chronic Obstructive
Pulmonary Disease: A Systematic Review. Telemedicine journal and e-health, 24(6),
415-424.
Cocanour, C.S. (2017). Informed consent-It's more than a signature on a piece of paper.
American Journal of Surgery, 214(6), 993-997.
Coster, S., Watkins, M., and Norman, I.J. (2018). What is the impact of professional nursing
on patients' outcomes globally? An overview of research evidence. International
Journal of Nursing Studies, 78, 76-83.
Ladwig, G. B., Ackley, B. J., and Makic, M. B. F. (2016). Mosby's Guide to Nursing
Diagnosis - E-Book. Elsevier Health Sciences. New York. United States.
Mok, W.Q., Wang, W., and Liaw, S.Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International Journal of Nursing
Practice, 2, 91-8.
Munroe, B., Curtis, K., Murphy, M., Strachan, L., and Buckley, T. (2015). HIRAID: An
evidence-informed emergency nursing assessment framework. Australasian
Emergency Nursing Journal, 18(2), 83-97.
Munroe, B., Curtis, K., Buckley, T., Lewis, M., and Atkins, L. (2018). Optimising
implementation of a patient-assessment framework for emergency nurses: A mixed-
method study. Journal of Clinical Nursing, 27(1-2), e269-e286.
Munroe, B., Curtis, K., Murphy, M., Strachan, L., Considine, J.,… and Buckley, T. (2016). A
structured framework improves clinical patient assessment and nontechnical skills of
early career emergency nurses: a pre-post study using full immersion simulation.
Journal of Clinical Nursing, 25(15-16), 2262-74.
Munroe, B., Buckley, T., Curtis, K., Murphy, M., Strachan, L.,… and Fethney, J. (2016). The
impact of HIRAID on emergency nurses' self-efficacy, anxiety and perceived control:
A simulated study. International Emergency Nursing, 25, 53-8.
Odell, M. (2015). Detection and management of the deteriorating ward patient: an evaluation
of nursing practice. Journal of Clinical Nursing, 24(1-2), 173-82.
Pauls, R.N., Hanson, E., and Crisp, C.C. (2015). Voiding diaries: adherence in the clinical
setting. International Urogynecology Journal, 26(1), 91-7.
Wang, T., Tan, J.Y., Xiao, LD., and Deng, R. (2017). Effectiveness of disease-specific self-
management education on health outcomes in patients with chronic obstructive
pulmonary disease: An updated systematic review and meta-analysis. Patient
Education and Counseling, 100(8), 1432-1446.
Wood, C., Chaboyer, W., and Carr, P. (2019). How do nurses use early warning scoring
systems to detect and act on patient deterioration to ensure patient safety? A scoping
review. International Journal of Nursing Studies, 94, 166-178.
9
Baroi, S., McNamara, R.J., McKenzie, D.K., Gandevia, S., and Brodie, M.A. (2018).
Advances in Remote Respiratory Assessments for People with Chronic Obstructive
Pulmonary Disease: A Systematic Review. Telemedicine journal and e-health, 24(6),
415-424.
Cocanour, C.S. (2017). Informed consent-It's more than a signature on a piece of paper.
American Journal of Surgery, 214(6), 993-997.
Coster, S., Watkins, M., and Norman, I.J. (2018). What is the impact of professional nursing
on patients' outcomes globally? An overview of research evidence. International
Journal of Nursing Studies, 78, 76-83.
Ladwig, G. B., Ackley, B. J., and Makic, M. B. F. (2016). Mosby's Guide to Nursing
Diagnosis - E-Book. Elsevier Health Sciences. New York. United States.
Mok, W.Q., Wang, W., and Liaw, S.Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International Journal of Nursing
Practice, 2, 91-8.
Munroe, B., Curtis, K., Murphy, M., Strachan, L., and Buckley, T. (2015). HIRAID: An
evidence-informed emergency nursing assessment framework. Australasian
Emergency Nursing Journal, 18(2), 83-97.
Munroe, B., Curtis, K., Buckley, T., Lewis, M., and Atkins, L. (2018). Optimising
implementation of a patient-assessment framework for emergency nurses: A mixed-
method study. Journal of Clinical Nursing, 27(1-2), e269-e286.
Munroe, B., Curtis, K., Murphy, M., Strachan, L., Considine, J.,… and Buckley, T. (2016). A
structured framework improves clinical patient assessment and nontechnical skills of
early career emergency nurses: a pre-post study using full immersion simulation.
Journal of Clinical Nursing, 25(15-16), 2262-74.
Munroe, B., Buckley, T., Curtis, K., Murphy, M., Strachan, L.,… and Fethney, J. (2016). The
impact of HIRAID on emergency nurses' self-efficacy, anxiety and perceived control:
A simulated study. International Emergency Nursing, 25, 53-8.
Odell, M. (2015). Detection and management of the deteriorating ward patient: an evaluation
of nursing practice. Journal of Clinical Nursing, 24(1-2), 173-82.
Pauls, R.N., Hanson, E., and Crisp, C.C. (2015). Voiding diaries: adherence in the clinical
setting. International Urogynecology Journal, 26(1), 91-7.
Wang, T., Tan, J.Y., Xiao, LD., and Deng, R. (2017). Effectiveness of disease-specific self-
management education on health outcomes in patients with chronic obstructive
pulmonary disease: An updated systematic review and meta-analysis. Patient
Education and Counseling, 100(8), 1432-1446.
Wood, C., Chaboyer, W., and Carr, P. (2019). How do nurses use early warning scoring
systems to detect and act on patient deterioration to ensure patient safety? A scoping
review. International Journal of Nursing Studies, 94, 166-178.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Yang, I., Brown, J., George J, Jenkins, S., McDonald, C.F., McDonald, V.M., … Dabschec,
E. (2017). COPD-X Australian and New Zealand guidelines for the diagnosis and
management of chronic obstructive pulmonary disease: 2017 update. Medical Journal
of Australia, 207, 436-442.
10
E. (2017). COPD-X Australian and New Zealand guidelines for the diagnosis and
management of chronic obstructive pulmonary disease: 2017 update. Medical Journal
of Australia, 207, 436-442.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
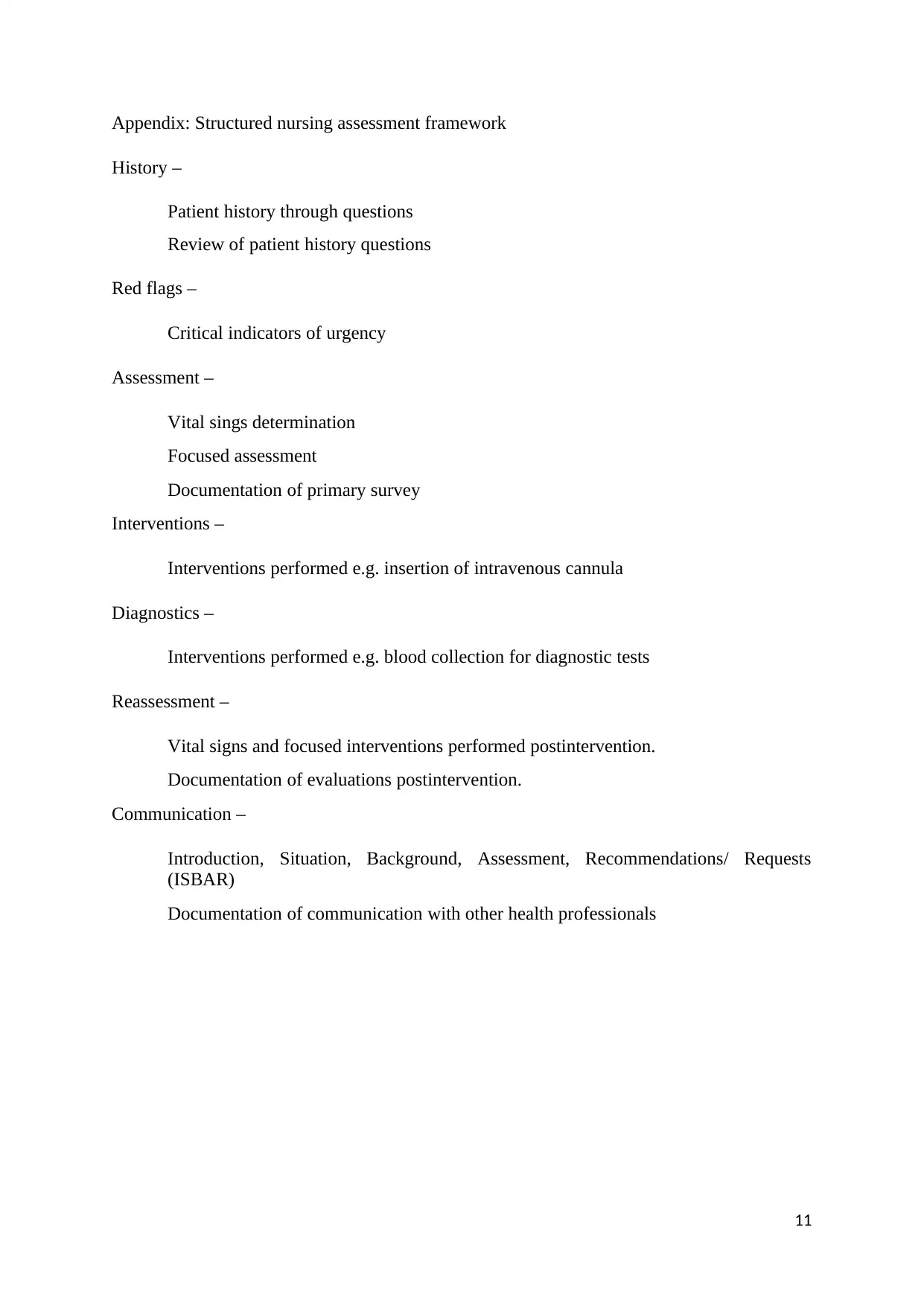
Appendix: Structured nursing assessment framework
History –
Patient history through questions
Review of patient history questions
Red flags –
Critical indicators of urgency
Assessment –
Vital sings determination
Focused assessment
Documentation of primary survey
Interventions –
Interventions performed e.g. insertion of intravenous cannula
Diagnostics –
Interventions performed e.g. blood collection for diagnostic tests
Reassessment –
Vital signs and focused interventions performed postintervention.
Documentation of evaluations postintervention.
Communication –
Introduction, Situation, Background, Assessment, Recommendations/ Requests
(ISBAR)
Documentation of communication with other health professionals
11
History –
Patient history through questions
Review of patient history questions
Red flags –
Critical indicators of urgency
Assessment –
Vital sings determination
Focused assessment
Documentation of primary survey
Interventions –
Interventions performed e.g. insertion of intravenous cannula
Diagnostics –
Interventions performed e.g. blood collection for diagnostic tests
Reassessment –
Vital signs and focused interventions performed postintervention.
Documentation of evaluations postintervention.
Communication –
Introduction, Situation, Background, Assessment, Recommendations/ Requests
(ISBAR)
Documentation of communication with other health professionals
11
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




