Clinical Reasoning Cycle: Case Study on Coronary Artery Disease
VerifiedAdded on 2022/12/15
|11
|1743
|165
Presentation
AI Summary
This presentation analyzes a case study of Mr. Tomasi Joni, a 56-year-old mechanical engineer with a history of hypertension, AMI, and other health complications. The presentation follows the clinical reasoning cycle to assess Mr. Joni's risk of developing coronary artery disease (CAD). It begins by considering the patient's situation, including his medical history, lifestyle, and current health indicators. The presentation then collects and processes information, identifying key cues such as elevated blood pressure, abnormal cholesterol levels, and other risk factors. The core of the presentation focuses on the pathophysiology of CAD, explaining the mechanisms of the disease and its clinical manifestations. Goals are established to restore balance between oxygen demand and supply and take action by administering medications and initiating lifestyle changes. The presentation concludes by discussing the outcomes of the nursing care plan and the importance of clinical reasoning in understanding and managing CAD. The presentation also includes references to support the discussed concepts.
Clinical reasoning cycle
Name of the Student
Name of the University
The purpose of the presentation is to select a potential health complication
from the case study and discuss it following the clinical reasoning cycle
Name of the Student
Name of the University
The purpose of the presentation is to select a potential health complication
from the case study and discuss it following the clinical reasoning cycle
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
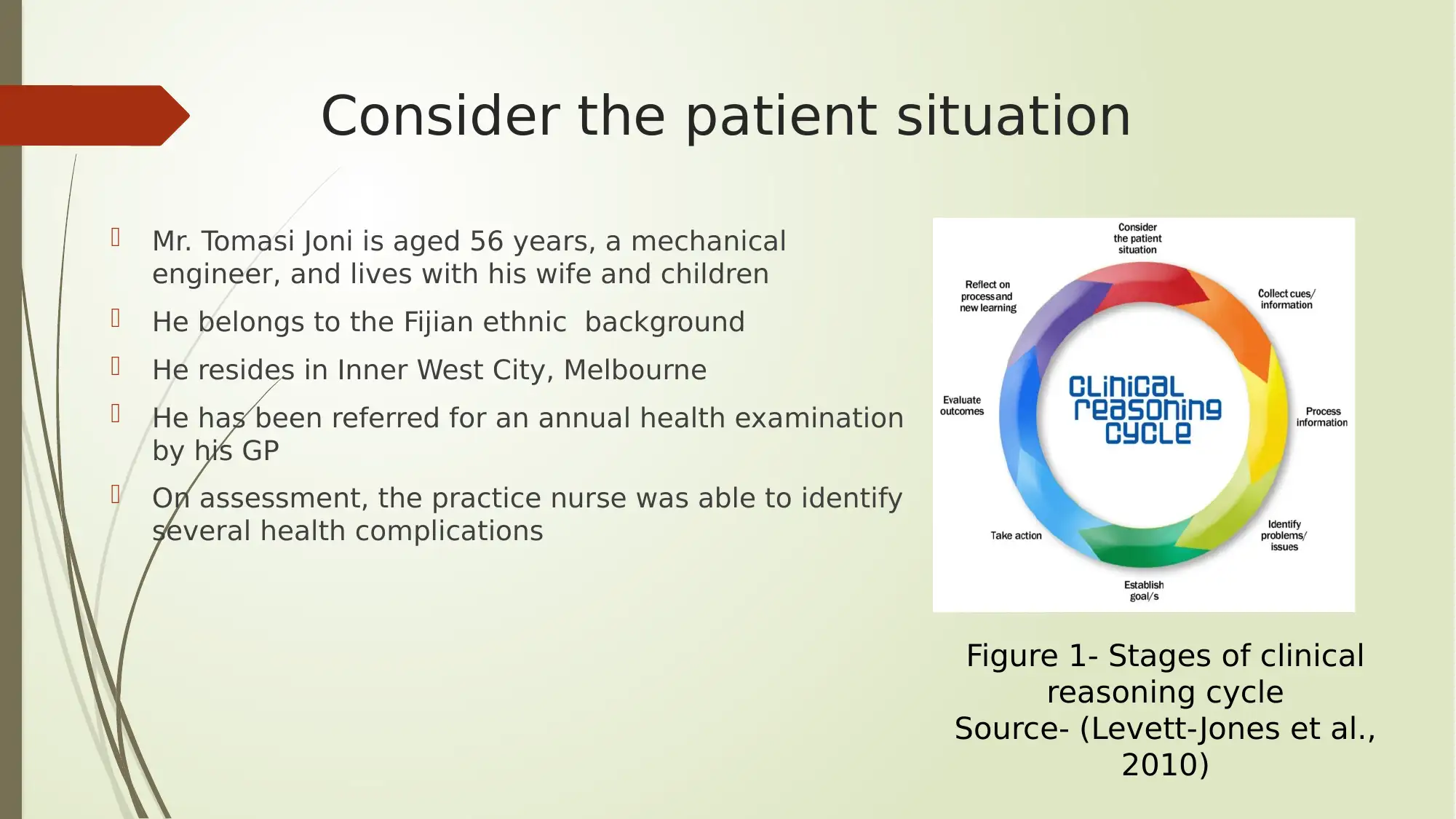
Consider the patient situation
Mr. Tomasi Joni is aged 56 years, a mechanical
engineer, and lives with his wife and children
He belongs to the Fijian ethnic background
He resides in Inner West City, Melbourne
He has been referred for an annual health examination
by his GP
On assessment, the practice nurse was able to identify
several health complications
Figure 1- Stages of clinical
reasoning cycle
Source- (Levett-Jones et al.,
2010)
Mr. Tomasi Joni is aged 56 years, a mechanical
engineer, and lives with his wife and children
He belongs to the Fijian ethnic background
He resides in Inner West City, Melbourne
He has been referred for an annual health examination
by his GP
On assessment, the practice nurse was able to identify
several health complications
Figure 1- Stages of clinical
reasoning cycle
Source- (Levett-Jones et al.,
2010)
Collect cues/information
Currently he works for more than 50 hours each week
He tries to perform physical activity during leisure
He smokes and consumes alcohol and consumes takeaway food
regularly
Medical history- hypertension, AMI in 2016, obstructive sleep apnea
(OSA) and CPAP for sleep
Family history- Hyperlipidemia (father) and breast cancer (mother)
Currently under three medications: metoprolol, aspirin and allopurinol
Currently he works for more than 50 hours each week
He tries to perform physical activity during leisure
He smokes and consumes alcohol and consumes takeaway food
regularly
Medical history- hypertension, AMI in 2016, obstructive sleep apnea
(OSA) and CPAP for sleep
Family history- Hyperlipidemia (father) and breast cancer (mother)
Currently under three medications: metoprolol, aspirin and allopurinol
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Process information
BP 142/96 mm Hg provides indication for hypertension (Bloom, Kemp &
Lubel, 2015)
Heart rate was 96 bpm that was within the normal limit of 60-100 bpm,
thus indicating normal functioning of the heart
Respiratory rate of 22 breaths/min indicated a slight elevation from
normal condition, thus indicating shortness of breath (Anzueto &
Miravitlles, 2017)
SpO2 was 96% on RA and normal
Body temperature of 36.7°C indicated hypothermia or loss of heat at a
rapid rate from the body (Nassal et al., 2017)
BP 142/96 mm Hg provides indication for hypertension (Bloom, Kemp &
Lubel, 2015)
Heart rate was 96 bpm that was within the normal limit of 60-100 bpm,
thus indicating normal functioning of the heart
Respiratory rate of 22 breaths/min indicated a slight elevation from
normal condition, thus indicating shortness of breath (Anzueto &
Miravitlles, 2017)
SpO2 was 96% on RA and normal
Body temperature of 36.7°C indicated hypothermia or loss of heat at a
rapid rate from the body (Nassal et al., 2017)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Process information (2)
Excess abdominal fat, indicating obesity
Waist circumference of 104 cm
Elevated level of blood cholesterol 9.2mmol/L (much higher than optimal
2.59-3.34 mmol/L) (Cahill et al., 2019)
Excess abdominal fat, indicating obesity
Waist circumference of 104 cm
Elevated level of blood cholesterol 9.2mmol/L (much higher than optimal
2.59-3.34 mmol/L) (Cahill et al., 2019)
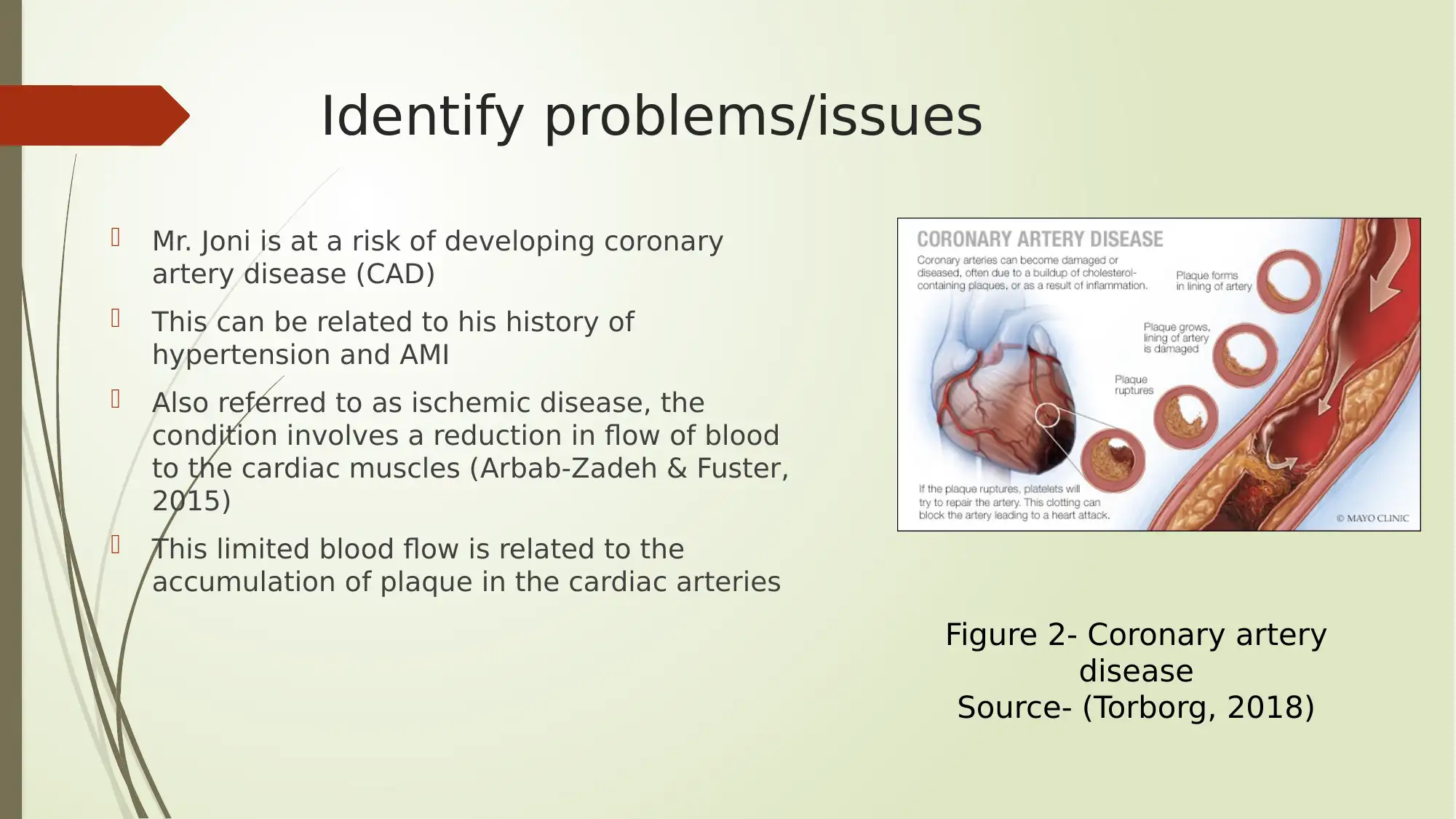
Identify problems/issues
Mr. Joni is at a risk of developing coronary
artery disease (CAD)
This can be related to his history of
hypertension and AMI
Also referred to as ischemic disease, the
condition involves a reduction in flow of blood
to the cardiac muscles (Arbab-Zadeh & Fuster,
2015)
This limited blood flow is related to the
accumulation of plaque in the cardiac arteries
Figure 2- Coronary artery
disease
Source- (Torborg, 2018)
Mr. Joni is at a risk of developing coronary
artery disease (CAD)
This can be related to his history of
hypertension and AMI
Also referred to as ischemic disease, the
condition involves a reduction in flow of blood
to the cardiac muscles (Arbab-Zadeh & Fuster,
2015)
This limited blood flow is related to the
accumulation of plaque in the cardiac arteries
Figure 2- Coronary artery
disease
Source- (Torborg, 2018)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
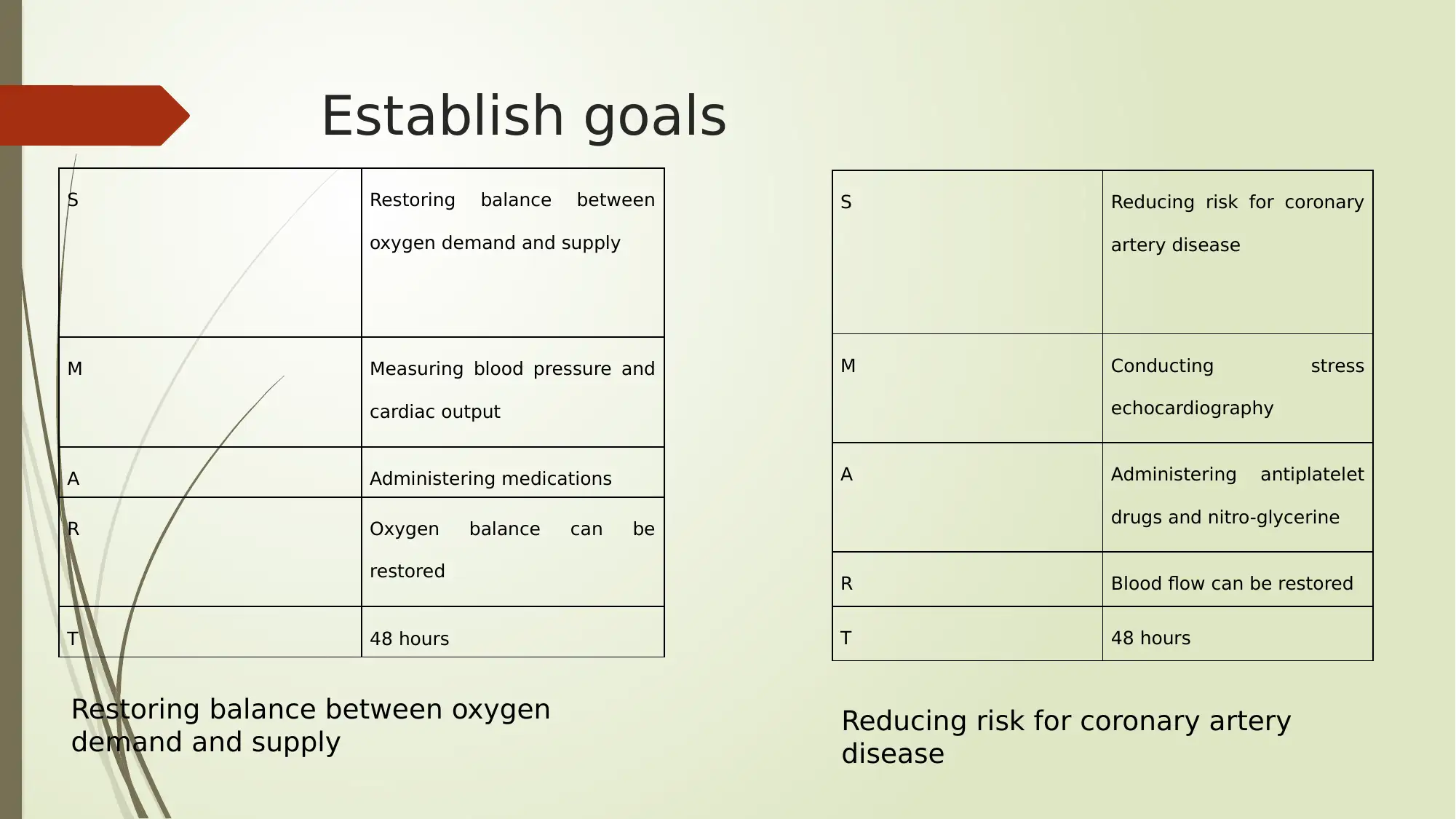
Establish goals
S Restoring balance between
oxygen demand and supply
M Measuring blood pressure and
cardiac output
A Administering medications
R Oxygen balance can be
restored
T 48 hours
S Reducing risk for coronary
artery disease
M Conducting stress
echocardiography
A Administering antiplatelet
drugs and nitro-glycerine
R Blood flow can be restored
T 48 hours
Restoring balance between oxygen
demand and supply Reducing risk for coronary artery
disease
S Restoring balance between
oxygen demand and supply
M Measuring blood pressure and
cardiac output
A Administering medications
R Oxygen balance can be
restored
T 48 hours
S Reducing risk for coronary
artery disease
M Conducting stress
echocardiography
A Administering antiplatelet
drugs and nitro-glycerine
R Blood flow can be restored
T 48 hours
Restoring balance between oxygen
demand and supply Reducing risk for coronary artery
disease
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
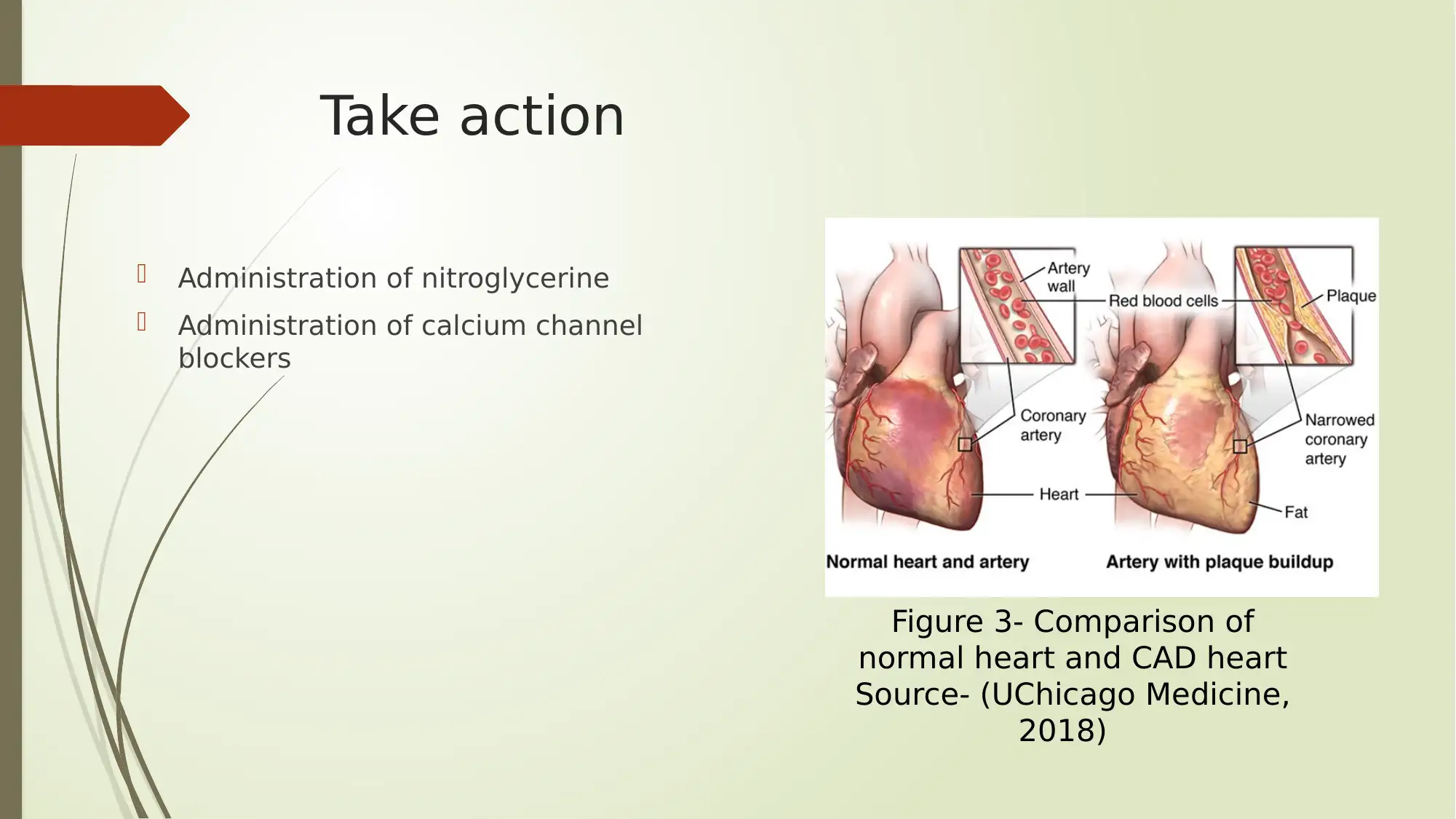
Take action
Administration of nitroglycerine
Administration of calcium channel
blockers
Figure 3- Comparison of
normal heart and CAD heart
Source- (UChicago Medicine,
2018)
Administration of nitroglycerine
Administration of calcium channel
blockers
Figure 3- Comparison of
normal heart and CAD heart
Source- (UChicago Medicine,
2018)
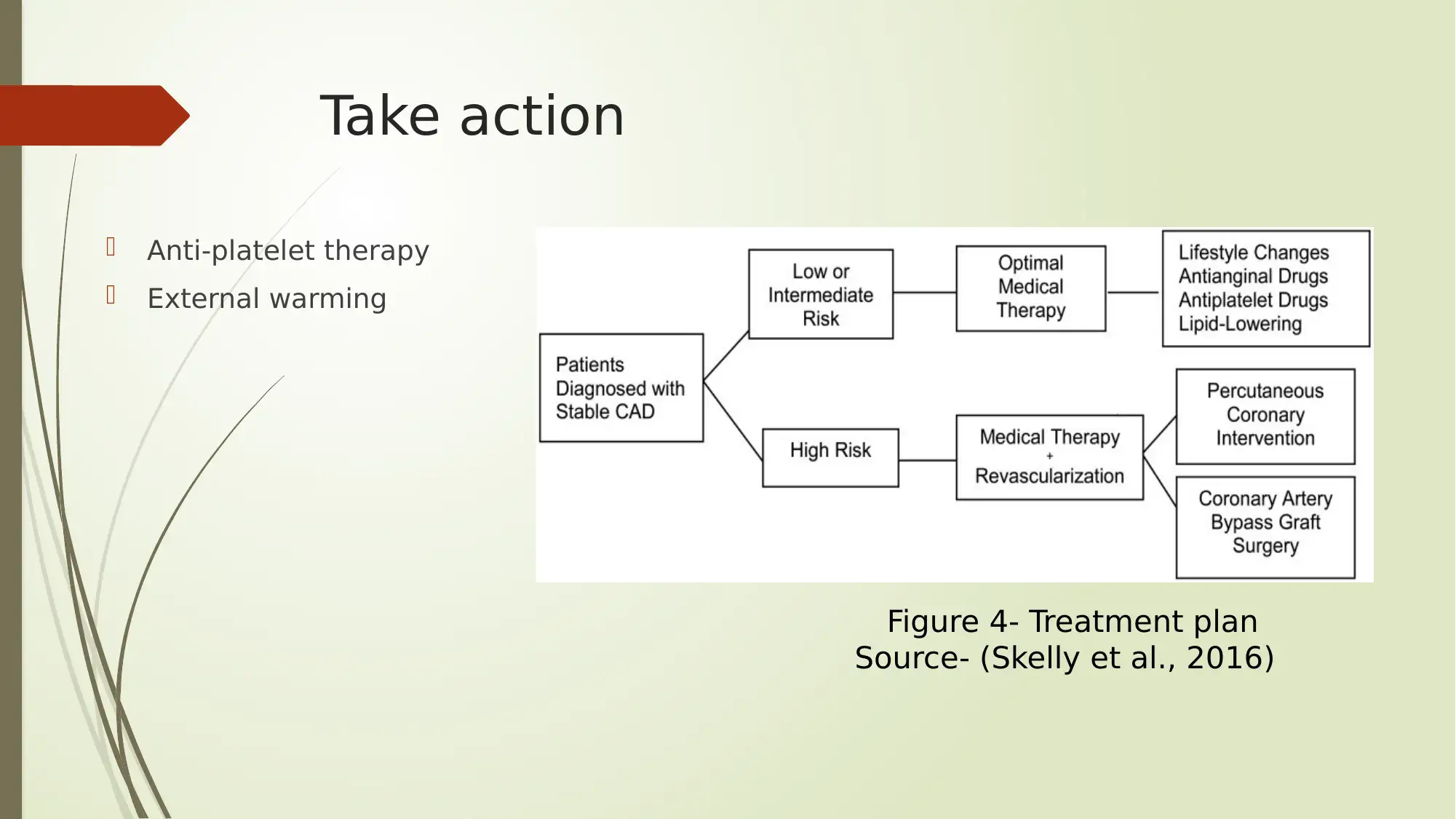
Take action
Anti-platelet therapy
External warming
Figure 4- Treatment plan
Source- (Skelly et al., 2016)
Anti-platelet therapy
External warming
Figure 4- Treatment plan
Source- (Skelly et al., 2016)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Conclusion
Hence, the case study suggested that the patient was at a risk of developing CAD.
The following outcomes will determine success of the nursing care plan discussed
previously:
Reduction in blood pressure
Reduction in respiratory rate
No reports of angina episode
Initiation of lifestyle changes
The clinical reasoning helped in gaining an understanding of risk factors for CAD
It helped in understanding pathophysiology of the health abnormalities manifested by
Mr. Joni. However, the nursing care plan could have been done differently, by placing
due focus on other treatment strategies such as, antiplatelet drugs, angioplasty, and
coronary artery bypass grafting.
Hence, the case study suggested that the patient was at a risk of developing CAD.
The following outcomes will determine success of the nursing care plan discussed
previously:
Reduction in blood pressure
Reduction in respiratory rate
No reports of angina episode
Initiation of lifestyle changes
The clinical reasoning helped in gaining an understanding of risk factors for CAD
It helped in understanding pathophysiology of the health abnormalities manifested by
Mr. Joni. However, the nursing care plan could have been done differently, by placing
due focus on other treatment strategies such as, antiplatelet drugs, angioplasty, and
coronary artery bypass grafting.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Anzueto, A., & Miravitlles, M. (2017). Pathophysiology of dyspnea in COPD. Postgraduate medicine, 129(3), 366-374.
Arbab-Zadeh, A., & Fuster, V. (2015). The myth of the “vulnerable plaque”: transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. Journal of the American College of Cardiology, 65(8), 846-855.
Bloom, S., Kemp, W., & Lubel, J. (2015). Portal hypertension: pathophysiology, diagnosis and management. Internal medicine journal, 45(1), 16-26.
Cahill, L. E., Sacks, F. M., Rimm, E. B., & Jensen, M. K. (2019). Cholesterol Efflux Capacity, HDL Cholesterol, and Risk of Coronary Heart Disease: a Nested Case-Control Study in Men. Journal of lipid research, jlr-P093823.
Campbell, G., Alderson, P., Smith, A. F., & Warttig, S. (2015). Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews, (4).
Chow, C. K., Redfern, J., Hillis, G. S., Thakkar, J., Santo, K., Hackett, M. L., ... & Bompoint, S. (2015). Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. Jama, 314(12), 1255-1263.
Cui, H., López, M., & Rahmouni, K. (2017). The cellular and molecular bases of leptin and ghrelin resistance in obesity. Nature Reviews Endocrinology, 13(6), 338.
Cury, R. C., Abbara, S., Achenbach, S., Agatston, A., Berman, D. S., Budoff, M. J., ... & Rybicki, F. J. (2016). CAD-RADSTM coronary artery disease–reporting and data system. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT),
the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. Journal of cardiovascular computed tomography, 10(4), 269-281.
Daw, J., Margolis, R., & Wright, L. (2017). Emerging adulthood, emergent health lifestyles: Sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. Journal of health and social behavior, 58(2), 181-197.
Fletcher, G. F., Landolfo, C., Niebauer, J., Ozemek, C., Arena, R., & Lavie, C. J. (2018). Promoting physical activity and exercise: JACC health promotion series. Journal of the American College of Cardiology, 72(14), 1622-1639
Jäger, B., Piackova, E., Haller, P. M., Andric, T., Kahl, B., Christ, G., ... & Huber, K. (2019). Increased platelet reactivity in dyslipidemic patients with coronary artery disease on dual anti-platelet therapy. Archives of medical science: AMS, 15(1), 65.
Kristofik, N. J., Qin, L., Calabro, N. E., Dimitrievska, S., Li, G., Tellides, G., ... & Kyriakides, T. R. (2017). Improving in vivo outcomes of decellularized vascular grafts via incorporation of a novel extracellular matrix. Biomaterials, 141, 63-73.
Levett-Jones, T., Hoffman, K., Dempsey, J., Jeong, S. Y. S., Noble, D., Norton, C. A., ... & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’patients. Nurse education
today, 30(6), 515-520.
Maruhashi, T., Kajikawa, M., Nakashima, A., Iwamoto, Y., Iwamoto, A., Oda, N., ... & Watanabe, N. (2016). Nitroglycerine-induced vasodilation in coronary and brachial arteries in patients with suspected coronary artery disease. International journal of cardiology, 219,
312-316.
Nassal, M. M., Wan, X., Dale, Z., Deschênes, I., Wilson, L. D., & Piktel, J. S. (2017). Integrative Cardiovascular Physiology and Pathophysiology: Mild hypothermia preserves myocardial conduction during ischemia by maintaining gap junction intracellular communication
and Na+ channel function. American Journal of Physiology-Heart and Circulatory Physiology, 312(5), H886.
Skelly, A. C., Hashimoto, R., Buckley, D. I., Brodt, E. D., Noelck, N., Totten, A. M., ... & McDonagh, M. (2016). Noninvasive testing for coronary artery disease.
Tocci, G., Battistoni, A., Passerini, J., Musumeci, M. B., Francia, P., Ferrucci, A., & Volpe, M. (2015). Calcium channel blockers and hypertension. Journal of cardiovascular pharmacology and therapeutics, 20(2), 121-130.
Torborg, L. (2018). Mayo Clinic Q and A: Coronary artery disease — prevention and early warning signs. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-coronary-artery-disease-prevention-and-early-warning-signs/
UChicago Medicine. (2018).Coronary Artery Disease and Chest Pain. https://www.uchicagomedicine.org/conditions-services/heart-vascular/coronary-artery-disease
Wallerstein, N., Minkler, M., Carter-Edwards, L., Avila, M., & Sanchez, V. (2015). Improving health through community engagement, community organization, and community building. Health behavior. Theory, research and practice. 5th ed. Hoboken, NJ:
Jossey-Bass, 277-300.
Warm, J. S., Matthews, G., & Finomore Jr, V. S. (2018). Vigilance, workload, and stress. In Performance under stress (pp. 131-158). CRC Press.
Anzueto, A., & Miravitlles, M. (2017). Pathophysiology of dyspnea in COPD. Postgraduate medicine, 129(3), 366-374.
Arbab-Zadeh, A., & Fuster, V. (2015). The myth of the “vulnerable plaque”: transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. Journal of the American College of Cardiology, 65(8), 846-855.
Bloom, S., Kemp, W., & Lubel, J. (2015). Portal hypertension: pathophysiology, diagnosis and management. Internal medicine journal, 45(1), 16-26.
Cahill, L. E., Sacks, F. M., Rimm, E. B., & Jensen, M. K. (2019). Cholesterol Efflux Capacity, HDL Cholesterol, and Risk of Coronary Heart Disease: a Nested Case-Control Study in Men. Journal of lipid research, jlr-P093823.
Campbell, G., Alderson, P., Smith, A. F., & Warttig, S. (2015). Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews, (4).
Chow, C. K., Redfern, J., Hillis, G. S., Thakkar, J., Santo, K., Hackett, M. L., ... & Bompoint, S. (2015). Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. Jama, 314(12), 1255-1263.
Cui, H., López, M., & Rahmouni, K. (2017). The cellular and molecular bases of leptin and ghrelin resistance in obesity. Nature Reviews Endocrinology, 13(6), 338.
Cury, R. C., Abbara, S., Achenbach, S., Agatston, A., Berman, D. S., Budoff, M. J., ... & Rybicki, F. J. (2016). CAD-RADSTM coronary artery disease–reporting and data system. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT),
the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. Journal of cardiovascular computed tomography, 10(4), 269-281.
Daw, J., Margolis, R., & Wright, L. (2017). Emerging adulthood, emergent health lifestyles: Sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. Journal of health and social behavior, 58(2), 181-197.
Fletcher, G. F., Landolfo, C., Niebauer, J., Ozemek, C., Arena, R., & Lavie, C. J. (2018). Promoting physical activity and exercise: JACC health promotion series. Journal of the American College of Cardiology, 72(14), 1622-1639
Jäger, B., Piackova, E., Haller, P. M., Andric, T., Kahl, B., Christ, G., ... & Huber, K. (2019). Increased platelet reactivity in dyslipidemic patients with coronary artery disease on dual anti-platelet therapy. Archives of medical science: AMS, 15(1), 65.
Kristofik, N. J., Qin, L., Calabro, N. E., Dimitrievska, S., Li, G., Tellides, G., ... & Kyriakides, T. R. (2017). Improving in vivo outcomes of decellularized vascular grafts via incorporation of a novel extracellular matrix. Biomaterials, 141, 63-73.
Levett-Jones, T., Hoffman, K., Dempsey, J., Jeong, S. Y. S., Noble, D., Norton, C. A., ... & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’patients. Nurse education
today, 30(6), 515-520.
Maruhashi, T., Kajikawa, M., Nakashima, A., Iwamoto, Y., Iwamoto, A., Oda, N., ... & Watanabe, N. (2016). Nitroglycerine-induced vasodilation in coronary and brachial arteries in patients with suspected coronary artery disease. International journal of cardiology, 219,
312-316.
Nassal, M. M., Wan, X., Dale, Z., Deschênes, I., Wilson, L. D., & Piktel, J. S. (2017). Integrative Cardiovascular Physiology and Pathophysiology: Mild hypothermia preserves myocardial conduction during ischemia by maintaining gap junction intracellular communication
and Na+ channel function. American Journal of Physiology-Heart and Circulatory Physiology, 312(5), H886.
Skelly, A. C., Hashimoto, R., Buckley, D. I., Brodt, E. D., Noelck, N., Totten, A. M., ... & McDonagh, M. (2016). Noninvasive testing for coronary artery disease.
Tocci, G., Battistoni, A., Passerini, J., Musumeci, M. B., Francia, P., Ferrucci, A., & Volpe, M. (2015). Calcium channel blockers and hypertension. Journal of cardiovascular pharmacology and therapeutics, 20(2), 121-130.
Torborg, L. (2018). Mayo Clinic Q and A: Coronary artery disease — prevention and early warning signs. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-coronary-artery-disease-prevention-and-early-warning-signs/
UChicago Medicine. (2018).Coronary Artery Disease and Chest Pain. https://www.uchicagomedicine.org/conditions-services/heart-vascular/coronary-artery-disease
Wallerstein, N., Minkler, M., Carter-Edwards, L., Avila, M., & Sanchez, V. (2015). Improving health through community engagement, community organization, and community building. Health behavior. Theory, research and practice. 5th ed. Hoboken, NJ:
Jossey-Bass, 277-300.
Warm, J. S., Matthews, G., & Finomore Jr, V. S. (2018). Vigilance, workload, and stress. In Performance under stress (pp. 131-158). CRC Press.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




