Nursing Assessment and Care Plan: Robert Brown's Head Injury Case
VerifiedAdded on 2023/06/13
|6
|2597
|169
Case Study
AI Summary
This case study presents the situation of Mr. Robert Brown, a 30-year-old male who sustained a head injury after being hit by a car. Upon admission, initial assessments missed critical signs of a developing cerebral hemorrhage, leading to improper wound management and a lack of timely reporting of new symptoms. The analysis highlights the importance of thorough patient assessment, accurate documentation, and effective communication among healthcare professionals. Key issues identified include the patient's altered mental status (GCS score of 13), elevated blood pressure and pulse, and a blood-soaked head dressing, all indicative of a potential intracranial bleed. The case study emphasizes the need for ongoing training in wound management, the establishment of clear communication protocols, and the regular review of patient conditions to prevent complications. Failure to address these issues could lead to irreversible cognitive impairment, coma, or even death. Effective care requires proper wound management, timely reporting of symptoms, and a commitment to patient safety, reinforcing the need for continuous learning and improvement in nursing practice. Desklib provides access to similar case studies and resources to aid students in their learning.
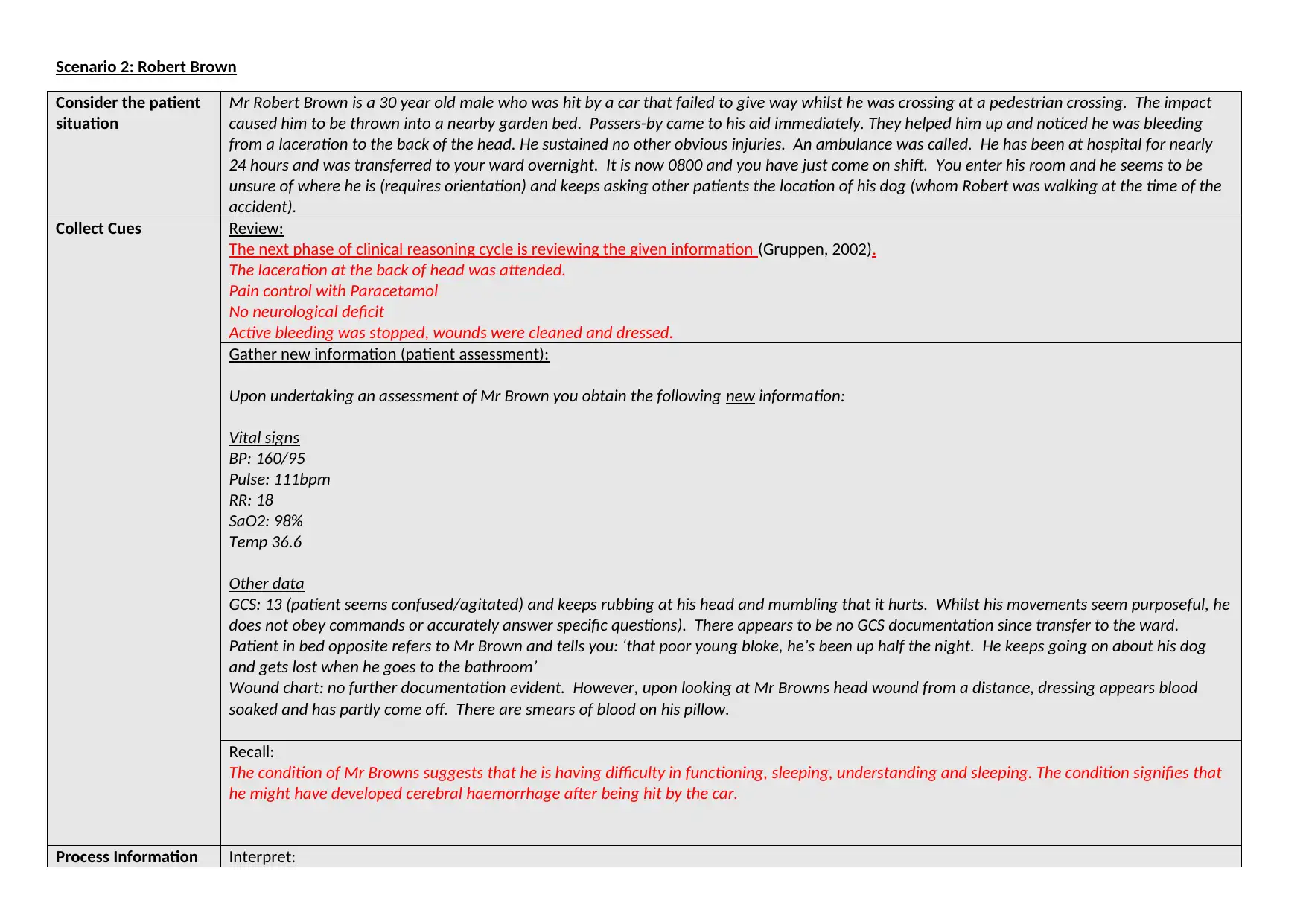
Scenario 2: Robert Brown
Consider the patient
situation
Mr Robert Brown is a 30 year old male who was hit by a car that failed to give way whilst he was crossing at a pedestrian crossing. The impact
caused him to be thrown into a nearby garden bed. Passers-by came to his aid immediately. They helped him up and noticed he was bleeding
from a laceration to the back of the head. He sustained no other obvious injuries. An ambulance was called. He has been at hospital for nearly
24 hours and was transferred to your ward overnight. It is now 0800 and you have just come on shift. You enter his room and he seems to be
unsure of where he is (requires orientation) and keeps asking other patients the location of his dog (whom Robert was walking at the time of the
accident).
Collect Cues Review:
The next phase of clinical reasoning cycle is reviewing the given information (Gruppen, 2002).
The laceration at the back of head was attended.
Pain control with Paracetamol
No neurological deficit
Active bleeding was stopped, wounds were cleaned and dressed.
Gather new information (patient assessment):
Upon undertaking an assessment of Mr Brown you obtain the following new information:
Vital signs
BP: 160/95
Pulse: 111bpm
RR: 18
SaO2: 98%
Temp 36.6
Other data
GCS: 13 (patient seems confused/agitated) and keeps rubbing at his head and mumbling that it hurts. Whilst his movements seem purposeful, he
does not obey commands or accurately answer specific questions). There appears to be no GCS documentation since transfer to the ward.
Patient in bed opposite refers to Mr Brown and tells you: ‘that poor young bloke, he’s been up half the night. He keeps going on about his dog
and gets lost when he goes to the bathroom’
Wound chart: no further documentation evident. However, upon looking at Mr Browns head wound from a distance, dressing appears blood
soaked and has partly come off. There are smears of blood on his pillow.
Recall:
The condition of Mr Browns suggests that he is having difficulty in functioning, sleeping, understanding and sleeping. The condition signifies that
he might have developed cerebral haemorrhage after being hit by the car.
Process Information Interpret:
Consider the patient
situation
Mr Robert Brown is a 30 year old male who was hit by a car that failed to give way whilst he was crossing at a pedestrian crossing. The impact
caused him to be thrown into a nearby garden bed. Passers-by came to his aid immediately. They helped him up and noticed he was bleeding
from a laceration to the back of the head. He sustained no other obvious injuries. An ambulance was called. He has been at hospital for nearly
24 hours and was transferred to your ward overnight. It is now 0800 and you have just come on shift. You enter his room and he seems to be
unsure of where he is (requires orientation) and keeps asking other patients the location of his dog (whom Robert was walking at the time of the
accident).
Collect Cues Review:
The next phase of clinical reasoning cycle is reviewing the given information (Gruppen, 2002).
The laceration at the back of head was attended.
Pain control with Paracetamol
No neurological deficit
Active bleeding was stopped, wounds were cleaned and dressed.
Gather new information (patient assessment):
Upon undertaking an assessment of Mr Brown you obtain the following new information:
Vital signs
BP: 160/95
Pulse: 111bpm
RR: 18
SaO2: 98%
Temp 36.6
Other data
GCS: 13 (patient seems confused/agitated) and keeps rubbing at his head and mumbling that it hurts. Whilst his movements seem purposeful, he
does not obey commands or accurately answer specific questions). There appears to be no GCS documentation since transfer to the ward.
Patient in bed opposite refers to Mr Brown and tells you: ‘that poor young bloke, he’s been up half the night. He keeps going on about his dog
and gets lost when he goes to the bathroom’
Wound chart: no further documentation evident. However, upon looking at Mr Browns head wound from a distance, dressing appears blood
soaked and has partly come off. There are smears of blood on his pillow.
Recall:
The condition of Mr Browns suggests that he is having difficulty in functioning, sleeping, understanding and sleeping. The condition signifies that
he might have developed cerebral haemorrhage after being hit by the car.
Process Information Interpret:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
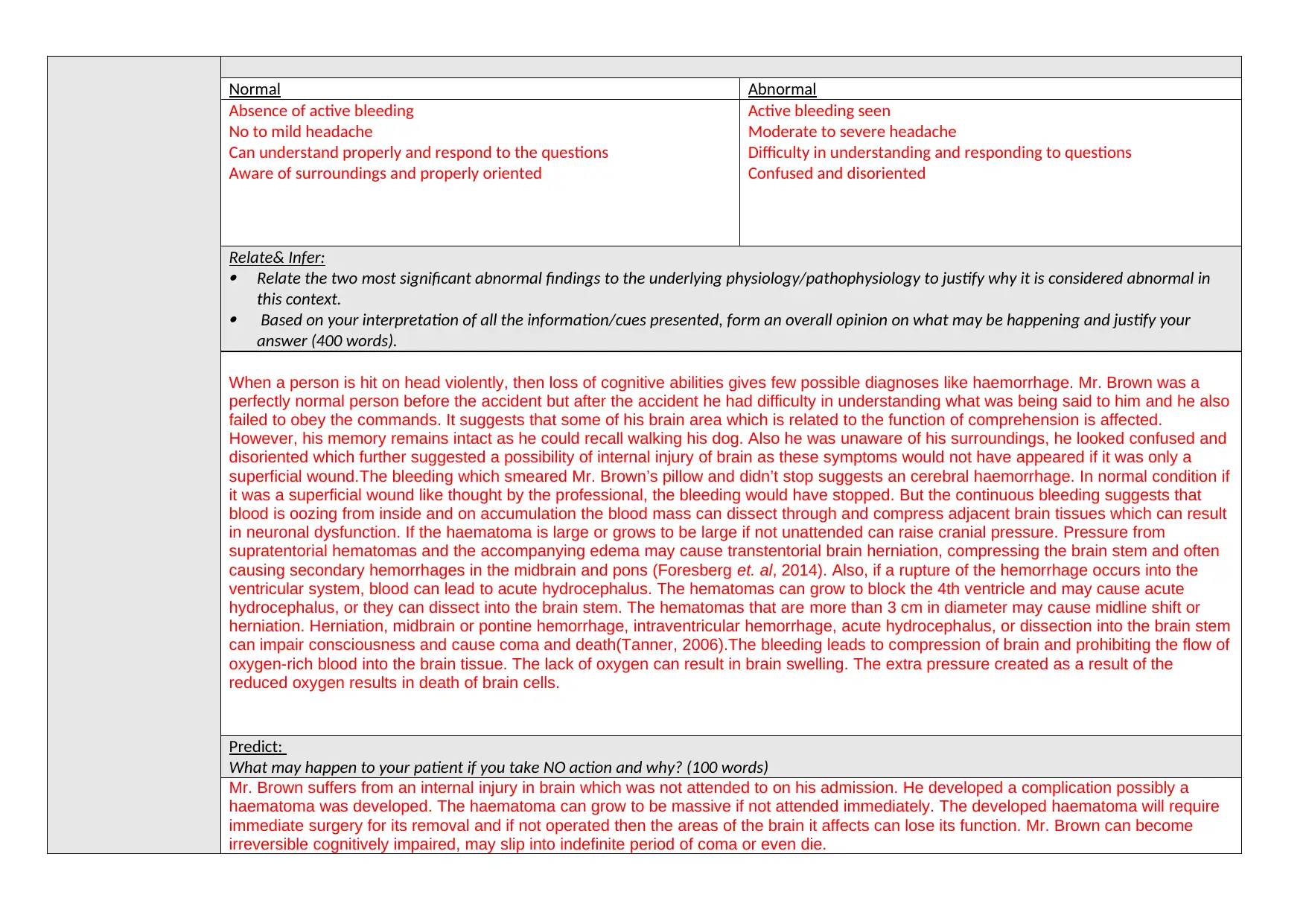
Normal Abnormal
Absence of active bleeding
No to mild headache
Can understand properly and respond to the questions
Aware of surroundings and properly oriented
Active bleeding seen
Moderate to severe headache
Difficulty in understanding and responding to questions
Confused and disoriented
Relate& Infer:
Relate the two most significant abnormal findings to the underlying physiology/pathophysiology to justify why it is considered abnormal in
this context.
Based on your interpretation of all the information/cues presented, form an overall opinion on what may be happening and justify your
answer (400 words).
When a person is hit on head violently, then loss of cognitive abilities gives few possible diagnoses like haemorrhage. Mr. Brown was a
perfectly normal person before the accident but after the accident he had difficulty in understanding what was being said to him and he also
failed to obey the commands. It suggests that some of his brain area which is related to the function of comprehension is affected.
However, his memory remains intact as he could recall walking his dog. Also he was unaware of his surroundings, he looked confused and
disoriented which further suggested a possibility of internal injury of brain as these symptoms would not have appeared if it was only a
superficial wound.The bleeding which smeared Mr. Brown’s pillow and didn’t stop suggests an cerebral haemorrhage. In normal condition if
it was a superficial wound like thought by the professional, the bleeding would have stopped. But the continuous bleeding suggests that
blood is oozing from inside and on accumulation the blood mass can dissect through and compress adjacent brain tissues which can result
in neuronal dysfunction. If the haematoma is large or grows to be large if not unattended can raise cranial pressure. Pressure from
supratentorial hematomas and the accompanying edema may cause transtentorial brain herniation, compressing the brain stem and often
causing secondary hemorrhages in the midbrain and pons (Foresberg et. al, 2014). Also, if a rupture of the hemorrhage occurs into the
ventricular system, blood can lead to acute hydrocephalus. The hematomas can grow to block the 4th ventricle and may cause acute
hydrocephalus, or they can dissect into the brain stem. The hematomas that are more than 3 cm in diameter may cause midline shift or
herniation. Herniation, midbrain or pontine hemorrhage, intraventricular hemorrhage, acute hydrocephalus, or dissection into the brain stem
can impair consciousness and cause coma and death(Tanner, 2006).The bleeding leads to compression of brain and prohibiting the flow of
oxygen-rich blood into the brain tissue. The lack of oxygen can result in brain swelling. The extra pressure created as a result of the
reduced oxygen results in death of brain cells.
Predict:
What may happen to your patient if you take NO action and why? (100 words)
Mr. Brown suffers from an internal injury in brain which was not attended to on his admission. He developed a complication possibly a
haematoma was developed. The haematoma can grow to be massive if not attended immediately. The developed haematoma will require
immediate surgery for its removal and if not operated then the areas of the brain it affects can lose its function. Mr. Brown can become
irreversible cognitively impaired, may slip into indefinite period of coma or even die.
Absence of active bleeding
No to mild headache
Can understand properly and respond to the questions
Aware of surroundings and properly oriented
Active bleeding seen
Moderate to severe headache
Difficulty in understanding and responding to questions
Confused and disoriented
Relate& Infer:
Relate the two most significant abnormal findings to the underlying physiology/pathophysiology to justify why it is considered abnormal in
this context.
Based on your interpretation of all the information/cues presented, form an overall opinion on what may be happening and justify your
answer (400 words).
When a person is hit on head violently, then loss of cognitive abilities gives few possible diagnoses like haemorrhage. Mr. Brown was a
perfectly normal person before the accident but after the accident he had difficulty in understanding what was being said to him and he also
failed to obey the commands. It suggests that some of his brain area which is related to the function of comprehension is affected.
However, his memory remains intact as he could recall walking his dog. Also he was unaware of his surroundings, he looked confused and
disoriented which further suggested a possibility of internal injury of brain as these symptoms would not have appeared if it was only a
superficial wound.The bleeding which smeared Mr. Brown’s pillow and didn’t stop suggests an cerebral haemorrhage. In normal condition if
it was a superficial wound like thought by the professional, the bleeding would have stopped. But the continuous bleeding suggests that
blood is oozing from inside and on accumulation the blood mass can dissect through and compress adjacent brain tissues which can result
in neuronal dysfunction. If the haematoma is large or grows to be large if not unattended can raise cranial pressure. Pressure from
supratentorial hematomas and the accompanying edema may cause transtentorial brain herniation, compressing the brain stem and often
causing secondary hemorrhages in the midbrain and pons (Foresberg et. al, 2014). Also, if a rupture of the hemorrhage occurs into the
ventricular system, blood can lead to acute hydrocephalus. The hematomas can grow to block the 4th ventricle and may cause acute
hydrocephalus, or they can dissect into the brain stem. The hematomas that are more than 3 cm in diameter may cause midline shift or
herniation. Herniation, midbrain or pontine hemorrhage, intraventricular hemorrhage, acute hydrocephalus, or dissection into the brain stem
can impair consciousness and cause coma and death(Tanner, 2006).The bleeding leads to compression of brain and prohibiting the flow of
oxygen-rich blood into the brain tissue. The lack of oxygen can result in brain swelling. The extra pressure created as a result of the
reduced oxygen results in death of brain cells.
Predict:
What may happen to your patient if you take NO action and why? (100 words)
Mr. Brown suffers from an internal injury in brain which was not attended to on his admission. He developed a complication possibly a
haematoma was developed. The haematoma can grow to be massive if not attended immediately. The developed haematoma will require
immediate surgery for its removal and if not operated then the areas of the brain it affects can lose its function. Mr. Brown can become
irreversible cognitively impaired, may slip into indefinite period of coma or even die.
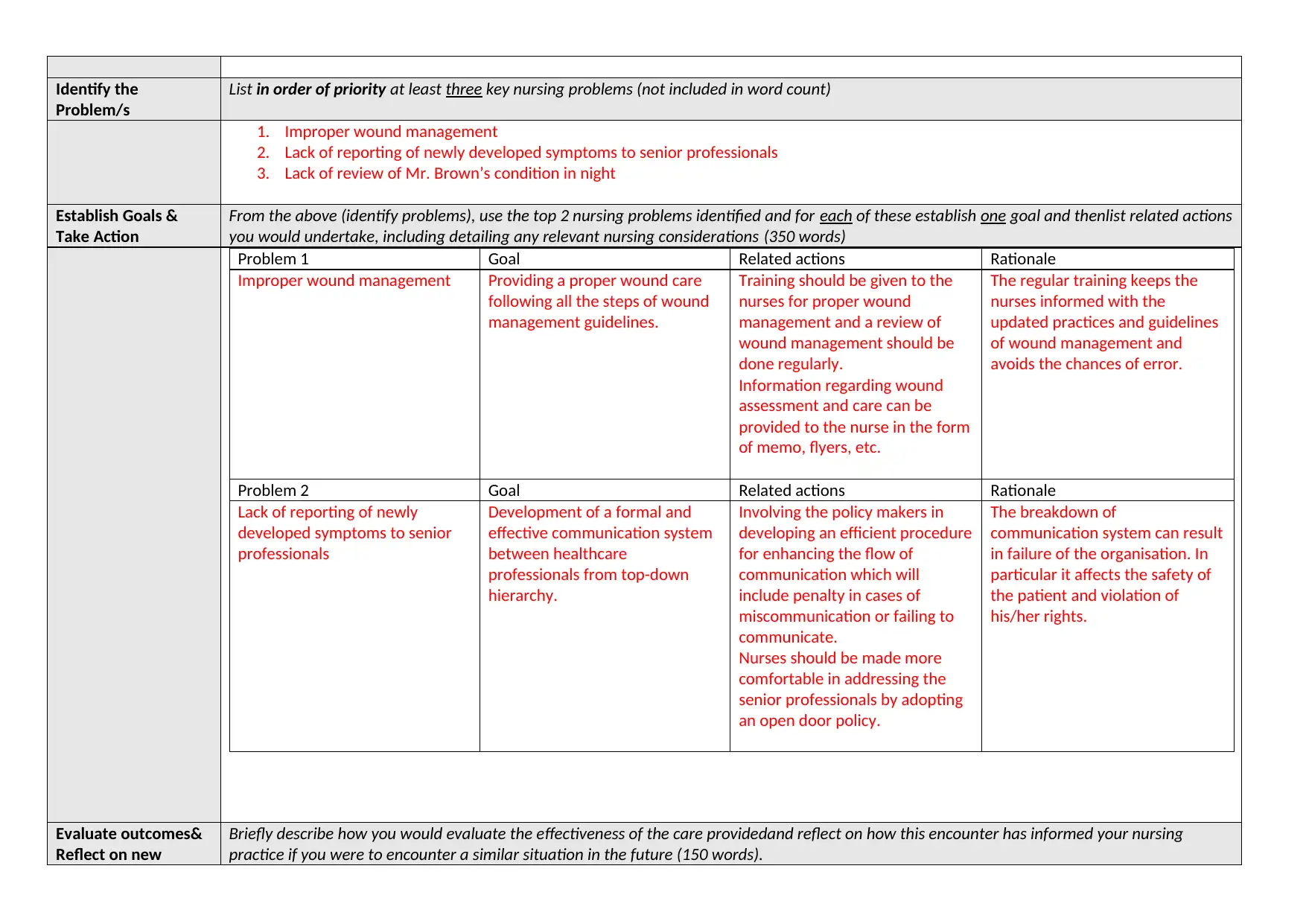
Identify the
Problem/s
List in order of priority at least three key nursing problems (not included in word count)
1. Improper wound management
2. Lack of reporting of newly developed symptoms to senior professionals
3. Lack of review of Mr. Brown’s condition in night
Establish Goals &
Take Action
From the above (identify problems), use the top 2 nursing problems identified and for each of these establish one goal and thenlist related actions
you would undertake, including detailing any relevant nursing considerations (350 words)
Problem 1 Goal Related actions Rationale
Improper wound management Providing a proper wound care
following all the steps of wound
management guidelines.
Training should be given to the
nurses for proper wound
management and a review of
wound management should be
done regularly.
Information regarding wound
assessment and care can be
provided to the nurse in the form
of memo, flyers, etc.
The regular training keeps the
nurses informed with the
updated practices and guidelines
of wound management and
avoids the chances of error.
Problem 2 Goal Related actions Rationale
Lack of reporting of newly
developed symptoms to senior
professionals
Development of a formal and
effective communication system
between healthcare
professionals from top-down
hierarchy.
Involving the policy makers in
developing an efficient procedure
for enhancing the flow of
communication which will
include penalty in cases of
miscommunication or failing to
communicate.
Nurses should be made more
comfortable in addressing the
senior professionals by adopting
an open door policy.
The breakdown of
communication system can result
in failure of the organisation. In
particular it affects the safety of
the patient and violation of
his/her rights.
Evaluate outcomes&
Reflect on new
Briefly describe how you would evaluate the effectiveness of the care providedand reflect on how this encounter has informed your nursing
practice if you were to encounter a similar situation in the future (150 words).
Problem/s
List in order of priority at least three key nursing problems (not included in word count)
1. Improper wound management
2. Lack of reporting of newly developed symptoms to senior professionals
3. Lack of review of Mr. Brown’s condition in night
Establish Goals &
Take Action
From the above (identify problems), use the top 2 nursing problems identified and for each of these establish one goal and thenlist related actions
you would undertake, including detailing any relevant nursing considerations (350 words)
Problem 1 Goal Related actions Rationale
Improper wound management Providing a proper wound care
following all the steps of wound
management guidelines.
Training should be given to the
nurses for proper wound
management and a review of
wound management should be
done regularly.
Information regarding wound
assessment and care can be
provided to the nurse in the form
of memo, flyers, etc.
The regular training keeps the
nurses informed with the
updated practices and guidelines
of wound management and
avoids the chances of error.
Problem 2 Goal Related actions Rationale
Lack of reporting of newly
developed symptoms to senior
professionals
Development of a formal and
effective communication system
between healthcare
professionals from top-down
hierarchy.
Involving the policy makers in
developing an efficient procedure
for enhancing the flow of
communication which will
include penalty in cases of
miscommunication or failing to
communicate.
Nurses should be made more
comfortable in addressing the
senior professionals by adopting
an open door policy.
The breakdown of
communication system can result
in failure of the organisation. In
particular it affects the safety of
the patient and violation of
his/her rights.
Evaluate outcomes&
Reflect on new
Briefly describe how you would evaluate the effectiveness of the care providedand reflect on how this encounter has informed your nursing
practice if you were to encounter a similar situation in the future (150 words).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
learning
The care provided to Mr. Brown was of substandard nature risking his life and not adhering to the guidelines of patient safety. If the service
provision was effective in Brown’s case his case may have been saved from developing complications.
However, I learnt from Mr. Brown’s case that no wound should be taken lightly and a proper wound assessment and management should be
undertaken. I also believe that it is important to review patients regularly as the patient may develop certain symptoms or develop
complications later. It becomes important to communicate and document accurately regarding the condition of the patient so that the doctors
can his condition accurately and formulate therapeutic interventions. In future, if I will ever encounter such situation I will ensure that I have
assessed the wound properly and will regularly check on the patient or ask the other nurse on shift to check on patient’s condition
timely(Meissner, 2011).
References
Abel, W., & Freeze, M. 2006.Evaluation of concept mapping in an associate degree nursing program.Journal of Nursing Education, 45 (9), pp. 356-364.
Allen, G., Rubenfeld, M. G., &Scheffer, B., 2004. Reliability of assessment of critical thinking.Journal of Professional Nursing, 20 (1), pp. 15-22.
Banning, M. (2008). The think aloud approach as an educational tool to develop and assess clinical reasoning in undergraduate students. Nurse Education Today , 28, 8-14.
Burns, H., O'Donnell, J., &Artman, J., 2010. High-fidelity simulation in teaching problem solving to 1st year nursing students: A novel use of the nursing process. Clinical
Simulation in Nursing, 6, 87-95.
Chabeli, M. (2007). Facilitating critical thinking within the nursing proces framework: A literature review. Health SA Gesondheid, 12 (4), 69-89.
Di Vito-Thomas, P. (2005). Nursing student stories on learning how to think like a nurse. Nurse Educator, 3, 133-136.
Duchscher, J. (2003). Critical thinking: Perceptions of newly graduated female baccalaureate nurses. Journal of Nursing Education, 42 (1), 14-27.
Ellermann, C., Kataoka-Yahiro, M., & Wong, L. (2006). Logic models used to enhance critical thinking. Journal of Nursing Education, 45 (6), 220-227.
Facione, N., &Facione, P. (1996). Externalizing the critical thinking in knowledge development and clinical judgment.Nursing Outlook, 44, 129-136.
Facione, P. (1990). Critical thinking: A statement of expert consensus for purposes of educational assessment and instruction. Research findings and recommendations.
Ferguson, L., Yonge, O., & Myrick, F. (2004). Students’ involvement in faculty research: Ethical and methodological issues. International Journal of Qualitative Methods, 3
(4), 1-14.
The care provided to Mr. Brown was of substandard nature risking his life and not adhering to the guidelines of patient safety. If the service
provision was effective in Brown’s case his case may have been saved from developing complications.
However, I learnt from Mr. Brown’s case that no wound should be taken lightly and a proper wound assessment and management should be
undertaken. I also believe that it is important to review patients regularly as the patient may develop certain symptoms or develop
complications later. It becomes important to communicate and document accurately regarding the condition of the patient so that the doctors
can his condition accurately and formulate therapeutic interventions. In future, if I will ever encounter such situation I will ensure that I have
assessed the wound properly and will regularly check on the patient or ask the other nurse on shift to check on patient’s condition
timely(Meissner, 2011).
References
Abel, W., & Freeze, M. 2006.Evaluation of concept mapping in an associate degree nursing program.Journal of Nursing Education, 45 (9), pp. 356-364.
Allen, G., Rubenfeld, M. G., &Scheffer, B., 2004. Reliability of assessment of critical thinking.Journal of Professional Nursing, 20 (1), pp. 15-22.
Banning, M. (2008). The think aloud approach as an educational tool to develop and assess clinical reasoning in undergraduate students. Nurse Education Today , 28, 8-14.
Burns, H., O'Donnell, J., &Artman, J., 2010. High-fidelity simulation in teaching problem solving to 1st year nursing students: A novel use of the nursing process. Clinical
Simulation in Nursing, 6, 87-95.
Chabeli, M. (2007). Facilitating critical thinking within the nursing proces framework: A literature review. Health SA Gesondheid, 12 (4), 69-89.
Di Vito-Thomas, P. (2005). Nursing student stories on learning how to think like a nurse. Nurse Educator, 3, 133-136.
Duchscher, J. (2003). Critical thinking: Perceptions of newly graduated female baccalaureate nurses. Journal of Nursing Education, 42 (1), 14-27.
Ellermann, C., Kataoka-Yahiro, M., & Wong, L. (2006). Logic models used to enhance critical thinking. Journal of Nursing Education, 45 (6), 220-227.
Facione, N., &Facione, P. (1996). Externalizing the critical thinking in knowledge development and clinical judgment.Nursing Outlook, 44, 129-136.
Facione, P. (1990). Critical thinking: A statement of expert consensus for purposes of educational assessment and instruction. Research findings and recommendations.
Ferguson, L., Yonge, O., & Myrick, F. (2004). Students’ involvement in faculty research: Ethical and methodological issues. International Journal of Qualitative Methods, 3
(4), 1-14.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Forsberg, E., Ziegert, K., Hult, H., &Fors, U. (2014). Clinical reasoning in nursing, a thinkaloud study using virtual patients - A base for an innovative assessment. Nurse
Education Today, 34, 538-542.
Glynn, D. (2012). Clinical judgment development using structured classroom reflective practice: A qualitative study. Journal of Nursing Education, 51 (3), 134-139.
Goudreau, J., Boyer, L., & Letourneau, D. (2014). Clinical nursing reasoning in nursing practice: A cognitive learning model based on a think aloud methodology . Quality
Advancement in Nursing Education, 1(1), 1-18.
Gruppen, 2002. Clinical Reasoning. Dordrecht: Springer International Handbook of Research in Medical Education.
Kuiper, R., &Pesut, D. (2004).Promoting cognitive and metacognitive reflective reasoning skills in nursing practice: Self-regulated learning theory. Issues and Innovations in
Lee, M., &Brysiewicz, P. (2009). Enhancing problem solving and nursing diagnosis in year III Bachelor of Nursing students.Nurse Education Today, 29, 389-397.
Levett-Jones, T., Hoffmann, K., Dempsey, J., Yeun-Sim Jeong, S., Nobel, D., Norton, C., Hickey, N. (2010). The 'five rights' of clinical reasoning: An educational model to
Marchigiano, G., Eduljee, N., & Harvey, K. (2011). Developing critical thinking skills from clinical assignments: A pilot study on nursing students' self-reported
perceptions.Journal of Nursing Management, 19, 143-152.
Meissner, 2011.Exploring indigenous health using the clinical reasoning cycle: a student paper.Contemporary Nurse, 37(1), pp.82-9.
Newark: American Philosophical Association.
Newton, S., & Moore, G. (2013).Critical thinking skills of basic baccalaureate and accelerated second-degree nursing students.Nursing Education Perspectives, 34 (3), 154-
158.
Nursing Education, 45 (4), 381-391.
Paans, W., Sermeus, W., Nieweg, R., & Van Der Schans, C. (2010). Determinants of the accuracy of nursing diagnoses: Influence of ready knowledge, knowledge sources,
dispostion toward critical thinking, and reasoning skills. Journal of Professional Nursing, 26 (4), 232-241.
Parsons, S., & Teel, V. (2012). Double testing: A student perspective. Nursing Education Perspectives, 34 (2), 127-128.
Tanner, C. (1998). State of the science: Clinical judgment and evidence-based nursing practice: Conclusions and controversies. Communicating Nursing Research, 31, pp.
14-26.
Tanner, C. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), pp. 204-211.
Thompson, C., &Stapley, S. (2011). Do educational interventions improve nurses' clinical decision making and judgement? A systematic review. International Journal of
Nursing Studies, 48, pp. 881-893.
Thorne, S. (2008). Interpretive description. Walnut Creek, CA: Left Coast Press.
Van Horn, R. (2000). The reflective process in nursing clinicals using journaling and dialogue. Andrews University, pp. 1-179.
Education Today, 34, 538-542.
Glynn, D. (2012). Clinical judgment development using structured classroom reflective practice: A qualitative study. Journal of Nursing Education, 51 (3), 134-139.
Goudreau, J., Boyer, L., & Letourneau, D. (2014). Clinical nursing reasoning in nursing practice: A cognitive learning model based on a think aloud methodology . Quality
Advancement in Nursing Education, 1(1), 1-18.
Gruppen, 2002. Clinical Reasoning. Dordrecht: Springer International Handbook of Research in Medical Education.
Kuiper, R., &Pesut, D. (2004).Promoting cognitive and metacognitive reflective reasoning skills in nursing practice: Self-regulated learning theory. Issues and Innovations in
Lee, M., &Brysiewicz, P. (2009). Enhancing problem solving and nursing diagnosis in year III Bachelor of Nursing students.Nurse Education Today, 29, 389-397.
Levett-Jones, T., Hoffmann, K., Dempsey, J., Yeun-Sim Jeong, S., Nobel, D., Norton, C., Hickey, N. (2010). The 'five rights' of clinical reasoning: An educational model to
Marchigiano, G., Eduljee, N., & Harvey, K. (2011). Developing critical thinking skills from clinical assignments: A pilot study on nursing students' self-reported
perceptions.Journal of Nursing Management, 19, 143-152.
Meissner, 2011.Exploring indigenous health using the clinical reasoning cycle: a student paper.Contemporary Nurse, 37(1), pp.82-9.
Newark: American Philosophical Association.
Newton, S., & Moore, G. (2013).Critical thinking skills of basic baccalaureate and accelerated second-degree nursing students.Nursing Education Perspectives, 34 (3), 154-
158.
Nursing Education, 45 (4), 381-391.
Paans, W., Sermeus, W., Nieweg, R., & Van Der Schans, C. (2010). Determinants of the accuracy of nursing diagnoses: Influence of ready knowledge, knowledge sources,
dispostion toward critical thinking, and reasoning skills. Journal of Professional Nursing, 26 (4), 232-241.
Parsons, S., & Teel, V. (2012). Double testing: A student perspective. Nursing Education Perspectives, 34 (2), 127-128.
Tanner, C. (1998). State of the science: Clinical judgment and evidence-based nursing practice: Conclusions and controversies. Communicating Nursing Research, 31, pp.
14-26.
Tanner, C. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), pp. 204-211.
Thompson, C., &Stapley, S. (2011). Do educational interventions improve nurses' clinical decision making and judgement? A systematic review. International Journal of
Nursing Studies, 48, pp. 881-893.
Thorne, S. (2008). Interpretive description. Walnut Creek, CA: Left Coast Press.
Van Horn, R. (2000). The reflective process in nursing clinicals using journaling and dialogue. Andrews University, pp. 1-179.
Wangensteen, S., Johansson, I., Bjorkstrom, M., & Nordstrom, G. (2010). Critical thinking dispositions among newly gradated nurses.Journal of Advanced Nursing, 66 (10),
2170-2181.
Wilkinson, J. (2012). Nursing process and critical thinking. Upper Saddle River, NJ: Pearson.
Wotton, K., Davis, J., Button, D., & Kelton, M. ,2010. Third-year undergraduate nursing students' perceptions of high-fidelity simulation. Journal of Nursing Education, 49
(11), pp. 632-639.
2170-2181.
Wilkinson, J. (2012). Nursing process and critical thinking. Upper Saddle River, NJ: Pearson.
Wotton, K., Davis, J., Button, D., & Kelton, M. ,2010. Third-year undergraduate nursing students' perceptions of high-fidelity simulation. Journal of Nursing Education, 49
(11), pp. 632-639.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


