Clinical Reasoning Cycle: Matthew's Case Study and Reflection
VerifiedAdded on 2022/11/09
|11
|3275
|160
Essay
AI Summary
This essay applies the eight stages of the Levett-Jones' Clinical Reasoning Cycle to analyze a clinical decision made during a Bachelor of Nursing clinical placement, focusing on the case of Matthew, a 72-year-old patient diagnosed with colon cancer and experiencing fluid and electrolyte imbalance post-surgery. The essay details the application of each stage of the clinical reasoning cycle, including considering the patient's situation, collecting and processing information, identifying problems (hypovolemia and dehydration), establishing goals, taking action (fluid challenge and IV rate adjustments), evaluating outcomes, and reflecting on the experience. The reflection highlights the importance of controlling hypotension and preventing excessive blood loss, emphasizing the learning gained from the clinical incident. The essay also discusses applicable Registered Nurse Standards for Practice, providing a comprehensive analysis of the clinical reasoning process in a real-world nursing scenario.

Running Head: CLINICAL REASONING CYCLE 1
Clinical reasoning cycle
Name
University affiliation
Clinical reasoning cycle
Name
University affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL REASONING CYCLE 2
Clinical reasoning cycle
Professional nurses and other healthcare providers are required to employ clinical
reasoning daily when it comes to making critical judgments that impact the lives of their
patients. Researchers such as Oostra, Astle & Meyerhoff (2016) and Levett-Jones et al.
(2010) outlined that clinical reasoning is the process by which expert nurses and other
healthcare providers gather signs and symptoms of their patients. Further, they process their
patient’s provided information, comprehend their patient’s ailments, strategize as well as
implement interferences, assess consequences and reflect on and gain a learning lesson from
the process. Additionally, education provided to nurses aims at preparing them to use clinical
reasoning skills when it comes to clinical decision making which leads to the provision of
excellent health care services (Levett-Jones et al., 2010). For instance, according to a report
provided by the Canadian Association of Schools of Nursing (2014) Baccalaureate nursing
education – an education facility established in Canada –is responsible for the provision of
the groundwork for sound clinical reasoning and acute philosophy, clinical conclusions, as
well as robust principled comportment in nursing. Therefore, clinical reasoning can be used a
tool when it comes to providing essential health care within the healthcare systems (Oostra,
Astle, & Meyerhoff, 2016). This means it allows patients to be taken off in their specific
manner while simultaneously concentrating on their individual needs in regards to an
effective healing process. This essay aims at utilizing the application of the eight steps of the
clinical reasoning cycle using the Levett-Jones’ Clinical Reasoning Cycle to discuss as I
simultaneously provide my reflection on a clinical decision in regards to Matthew’s case. The
paper will also discuss applicable Registered Nurse Standards for Practice.
From Matthew’s situation, it is evident that he has two care priorities since he suffers
from fluid and electrolyte imbalance. As established by Levett-Jones et al. (2010) during her
research clinical reasoning cycle is a practice-based form of thinking which necessitates in-
Clinical reasoning cycle
Professional nurses and other healthcare providers are required to employ clinical
reasoning daily when it comes to making critical judgments that impact the lives of their
patients. Researchers such as Oostra, Astle & Meyerhoff (2016) and Levett-Jones et al.
(2010) outlined that clinical reasoning is the process by which expert nurses and other
healthcare providers gather signs and symptoms of their patients. Further, they process their
patient’s provided information, comprehend their patient’s ailments, strategize as well as
implement interferences, assess consequences and reflect on and gain a learning lesson from
the process. Additionally, education provided to nurses aims at preparing them to use clinical
reasoning skills when it comes to clinical decision making which leads to the provision of
excellent health care services (Levett-Jones et al., 2010). For instance, according to a report
provided by the Canadian Association of Schools of Nursing (2014) Baccalaureate nursing
education – an education facility established in Canada –is responsible for the provision of
the groundwork for sound clinical reasoning and acute philosophy, clinical conclusions, as
well as robust principled comportment in nursing. Therefore, clinical reasoning can be used a
tool when it comes to providing essential health care within the healthcare systems (Oostra,
Astle, & Meyerhoff, 2016). This means it allows patients to be taken off in their specific
manner while simultaneously concentrating on their individual needs in regards to an
effective healing process. This essay aims at utilizing the application of the eight steps of the
clinical reasoning cycle using the Levett-Jones’ Clinical Reasoning Cycle to discuss as I
simultaneously provide my reflection on a clinical decision in regards to Matthew’s case. The
paper will also discuss applicable Registered Nurse Standards for Practice.
From Matthew’s situation, it is evident that he has two care priorities since he suffers
from fluid and electrolyte imbalance. As established by Levett-Jones et al. (2010) during her
research clinical reasoning cycle is a practice-based form of thinking which necessitates in-
CLINICAL REASONING CYCLE 3
depth research as well as scientific-based knowledge. Therefore, in the case of Matthew,
professional nurses should have the ability separate the relevant circumstantial knowledge
and abilities as they simultaneously apply them when it comes to providing excellent health
care services. Health care services provided to Matthew should be tailored according to his
distinct ailment, rather than providing a general healthcare treatment that other patients with
related condition in the hospital receive. However, this is a crucial aspect in regards to
clinical reasoning since it requires special skills as well as abilities to identify gaps when it
comes to personal understanding to address the situation (Daly, 2018).
As developed by Levett-Jones et al (2010) and Daly (2018) effective clinical
reasoning process in all healthcare systems should include collection of cues, processing
patient’s facts and data, understanding the patient’s ailment, problem or causes towards
mismanagement of their treatment, scheduling and implementing interventions, evaluating
outcomes as well as learning from the process. According to Cappelletti, Engel & Prentice
(2014), it is common for patients to experience fluid alterations which in most cases it tends
to manifest rapidly leading to fatal consequences especially with the older adults who have
several comorbidities. According to a research conducted by Levett-Jones et al. (2010), the
most integral part of nursing care within the healthcare system for the past few years is
sustaining the subtle fluid as well as the electrolyte equilibrium of post-operative in patients.
In support of Levett-Jones et al. (2010) research Cappelletti, Engel, & Prentice, (2014)
mentioned that fluid imbalances, especially in older patients, often leads to significant
morbidity as well as mortality. Nevertheless, application of effective clinical reasoning when
taking care of these patients enables professional nurses and other healthcare providers to be
aware of as well as manage their patient’s deterioration within the early stages of the
treatment, thus inhibiting any adverse outcomes that may occur to their patients (Keith-Lucas,
2015).
depth research as well as scientific-based knowledge. Therefore, in the case of Matthew,
professional nurses should have the ability separate the relevant circumstantial knowledge
and abilities as they simultaneously apply them when it comes to providing excellent health
care services. Health care services provided to Matthew should be tailored according to his
distinct ailment, rather than providing a general healthcare treatment that other patients with
related condition in the hospital receive. However, this is a crucial aspect in regards to
clinical reasoning since it requires special skills as well as abilities to identify gaps when it
comes to personal understanding to address the situation (Daly, 2018).
As developed by Levett-Jones et al (2010) and Daly (2018) effective clinical
reasoning process in all healthcare systems should include collection of cues, processing
patient’s facts and data, understanding the patient’s ailment, problem or causes towards
mismanagement of their treatment, scheduling and implementing interventions, evaluating
outcomes as well as learning from the process. According to Cappelletti, Engel & Prentice
(2014), it is common for patients to experience fluid alterations which in most cases it tends
to manifest rapidly leading to fatal consequences especially with the older adults who have
several comorbidities. According to a research conducted by Levett-Jones et al. (2010), the
most integral part of nursing care within the healthcare system for the past few years is
sustaining the subtle fluid as well as the electrolyte equilibrium of post-operative in patients.
In support of Levett-Jones et al. (2010) research Cappelletti, Engel, & Prentice, (2014)
mentioned that fluid imbalances, especially in older patients, often leads to significant
morbidity as well as mortality. Nevertheless, application of effective clinical reasoning when
taking care of these patients enables professional nurses and other healthcare providers to be
aware of as well as manage their patient’s deterioration within the early stages of the
treatment, thus inhibiting any adverse outcomes that may occur to their patients (Keith-Lucas,
2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL REASONING CYCLE 4
Matthew’s background.
Recently, Matthew, who is a 72-year-old man was recently diagnosed to be suffering from
colon cancer in a local hospital during my Bachelor of Nursing clinical placement. Matthew
had come to seek medical services at the hospital after noticing rectal bleeding. During his
consultation period with the general practitioner of the hospital, Matthew mentioned that
during the past few days he had started to notice several changes in his bowel habits which
were accompanied by occasional diarrhea. General practitioner’s speculations revealed that
Matthew was anemic while his family history indicated several cases of bowel cancer
(Oxford, 2013). He executed a digital rectal examination on Matthew where he could not
identify any substantial rectal mass thus referring him to a gastroenterologist as he
simultaneously scheduled for a subsequent colonoscopy. However, after the general
practitioner had conducted a colonoscopy, he realized that Matthew was sick from a left-
sided cancer of the colon incorporated with a bowel resection.
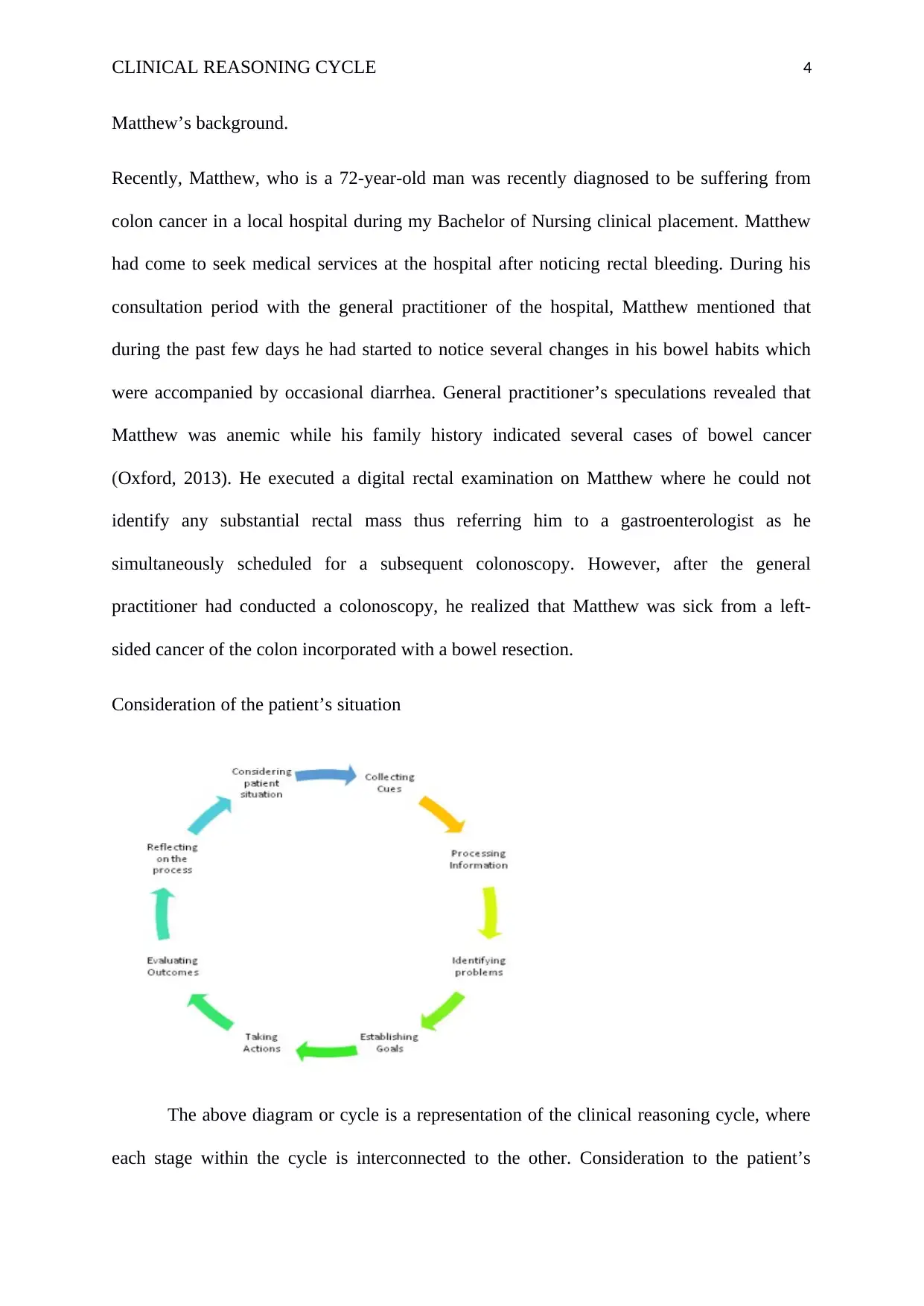
Consideration of the patient’s situation
The above diagram or cycle is a representation of the clinical reasoning cycle, where
each stage within the cycle is interconnected to the other. Consideration to the patient’s
Matthew’s background.
Recently, Matthew, who is a 72-year-old man was recently diagnosed to be suffering from
colon cancer in a local hospital during my Bachelor of Nursing clinical placement. Matthew
had come to seek medical services at the hospital after noticing rectal bleeding. During his
consultation period with the general practitioner of the hospital, Matthew mentioned that
during the past few days he had started to notice several changes in his bowel habits which
were accompanied by occasional diarrhea. General practitioner’s speculations revealed that
Matthew was anemic while his family history indicated several cases of bowel cancer
(Oxford, 2013). He executed a digital rectal examination on Matthew where he could not
identify any substantial rectal mass thus referring him to a gastroenterologist as he
simultaneously scheduled for a subsequent colonoscopy. However, after the general
practitioner had conducted a colonoscopy, he realized that Matthew was sick from a left-
sided cancer of the colon incorporated with a bowel resection.
Consideration of the patient’s situation
The above diagram or cycle is a representation of the clinical reasoning cycle, where
each stage within the cycle is interconnected to the other. Consideration to the patient’s
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL REASONING CYCLE 5
situation is the first step where professional nurses and other healthcare providers are
required to describe in detail the condition of their patients including all the facts in regards to
the illness and various situations which might be affecting the healing process of the patient.
In this case, Matthew who is 72 years old has been diagnosed by bowel cancer with a partial
colectomy as well as a formation of a colostomy. Cappelletti, Engel, & Prentice, (2014)
defined partial colectomy as the process of extracting a section of the large or small bowel.
Matthew indicated stability throughout his surgery, and now he has an intra-operative therapy
(IV) and morphine running at 84 mls per hour (Morens, Taubenberger, & Fauci, 2018).
However, during the night he experienced a drop in his BP which led to him having a restless
night. In the morning I gave him an independent drainage catheter (IDC) which would help
hourly monitoring of his health which shows no improvement.
On the other hand, his wound is well dressed and has remained intact. His oxygen
therapy is also placed at six liters every minute, and his tolerance to the mask is great. His
daughter will be able to visit him today since she is the only closest member of the family
where his wife died a couple of years ago.
Collection of information
This is the second stage and the most critical stage in nursing practice. According to
Levett-Jones et al. (2010), professional nurses at this point, are required to review
information that had been provided by the patient. This includes reviewing reports, patient’s
historical background as well as previously undertaken nursing assessments. Additionally,
nurses also gather new information using their knowledge and skills (Kobasa et al. 2014). In
the case of Matthew, the first step is to review his current observations which include an
unstable blood pressure of 90/50, temperatures of 37 degrees, pulse rate of 112, average
hourly urine out of 26mL/hr and a blood glucose level (BLG) of 4 mmol/L. I will also recall
situation is the first step where professional nurses and other healthcare providers are
required to describe in detail the condition of their patients including all the facts in regards to
the illness and various situations which might be affecting the healing process of the patient.
In this case, Matthew who is 72 years old has been diagnosed by bowel cancer with a partial
colectomy as well as a formation of a colostomy. Cappelletti, Engel, & Prentice, (2014)
defined partial colectomy as the process of extracting a section of the large or small bowel.
Matthew indicated stability throughout his surgery, and now he has an intra-operative therapy
(IV) and morphine running at 84 mls per hour (Morens, Taubenberger, & Fauci, 2018).
However, during the night he experienced a drop in his BP which led to him having a restless
night. In the morning I gave him an independent drainage catheter (IDC) which would help
hourly monitoring of his health which shows no improvement.
On the other hand, his wound is well dressed and has remained intact. His oxygen
therapy is also placed at six liters every minute, and his tolerance to the mask is great. His
daughter will be able to visit him today since she is the only closest member of the family
where his wife died a couple of years ago.
Collection of information
This is the second stage and the most critical stage in nursing practice. According to
Levett-Jones et al. (2010), professional nurses at this point, are required to review
information that had been provided by the patient. This includes reviewing reports, patient’s
historical background as well as previously undertaken nursing assessments. Additionally,
nurses also gather new information using their knowledge and skills (Kobasa et al. 2014). In
the case of Matthew, the first step is to review his current observations which include an
unstable blood pressure of 90/50, temperatures of 37 degrees, pulse rate of 112, average
hourly urine out of 26mL/hr and a blood glucose level (BLG) of 4 mmol/L. I will also recall
CLINICAL REASONING CYCLE 6
my knowledge in regards to physiology, cultural aspects, context of care and epidemiology
which will be essential when it comes to relating BP to fluid status of the patient and an
understanding of evidence-based practices. According to a research conducted by Oostra,
Astle, & Meyerhoff, (2016) and Cappelletti, Engel, & Prentice, (2014), this step
does not only involve a strong basis when it comes to the nurse’s knowledge and improved
skills, but requires the capability to synthesise as well as apply the knowledge to clinical
circumstances as well. Cappelletti, Engel, & Prentice, (2014) conclude that this tends to
be a challenge to most students due to its complexity and fluid.
Processing the gathered information.
The third step within the cycle of clinical reasoning is encompassed on interpreting
the already collected data cues of your patient as you simultaneously conducted a careful
analysis. However, Forsberg et al. (2014) mentioned that this stage requires professional
nurses and other healthcare providers to apply their knowledge about fluid balance. During
my placement at the hospital this step of comparing normal versus abnormal, helped me gain
a complete understanding of Matthew’s signs and symptoms. For instance, during the
analysis of his data and other physiological parameters I had a better understanding of his
temperatures (37 degrees) and pulse rate (112 beats per minute). Which in my opinion
compared to other parameters, these measurements were normal for Matthew at the time.
From the information I acquired, it now easy to narrow down the most important information.
However, previous research, such as Holder (2018) indicates that nurses, especially on
trainee placements, tend to be reluctant when it comes searching for cues, thus waits until
they identify a problem. Expert nurses, on the other hand show proactivity when it comes to
gathering an extensive range of signs and symptoms to detect as well as inhibit possible
patient’s impediments and deteriorations (Holder, 2018).
my knowledge in regards to physiology, cultural aspects, context of care and epidemiology
which will be essential when it comes to relating BP to fluid status of the patient and an
understanding of evidence-based practices. According to a research conducted by Oostra,
Astle, & Meyerhoff, (2016) and Cappelletti, Engel, & Prentice, (2014), this step
does not only involve a strong basis when it comes to the nurse’s knowledge and improved
skills, but requires the capability to synthesise as well as apply the knowledge to clinical
circumstances as well. Cappelletti, Engel, & Prentice, (2014) conclude that this tends to
be a challenge to most students due to its complexity and fluid.
Processing the gathered information.
The third step within the cycle of clinical reasoning is encompassed on interpreting
the already collected data cues of your patient as you simultaneously conducted a careful
analysis. However, Forsberg et al. (2014) mentioned that this stage requires professional
nurses and other healthcare providers to apply their knowledge about fluid balance. During
my placement at the hospital this step of comparing normal versus abnormal, helped me gain
a complete understanding of Matthew’s signs and symptoms. For instance, during the
analysis of his data and other physiological parameters I had a better understanding of his
temperatures (37 degrees) and pulse rate (112 beats per minute). Which in my opinion
compared to other parameters, these measurements were normal for Matthew at the time.
From the information I acquired, it now easy to narrow down the most important information.
However, previous research, such as Holder (2018) indicates that nurses, especially on
trainee placements, tend to be reluctant when it comes searching for cues, thus waits until
they identify a problem. Expert nurses, on the other hand show proactivity when it comes to
gathering an extensive range of signs and symptoms to detect as well as inhibit possible
patient’s impediments and deteriorations (Holder, 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL REASONING CYCLE 7
Identifying problems
This stage requires synthesizing all of the facts of data collected and interpretations
made to make a decisive nursing diagnosis of Matthew’s major problem. According to
Gummesson Sundén & Fex (2018) appropriately identifying the main problem of the patient,
enables proper diagnosis and correct prescriptions. In the case of Matthew, his diagnosis was
Hypovolaemia and dehydration. This deterioration was caused by two Pico preps that he was
given on the night of his surgery. Fors & Gunning (2014) developed that Pico preps tend to
cause adverse effects of osmotic diarrhea. Patients suffering from osmotic diarrhea may end
up losing many liters of fluids from the circulating volume through the wall of the intestine as
the bowel is evacuated. Additionally, blood lost during Matthew’s surgery as well as through
the drainage from the bellovacs led to further depletion of intravascular volume.
Establishing goals
In every healthcare system, professional nurses and healthcare providers should
describe goals and achievements they aspire to accomplish within a given time frame.
Previous research also indicates that it is easier to achieve excellent healthcare services when
goals are set (Mamelund, 2016). Therefore, it is important Matthew to have better
management of his condition. The goal is for him to be normotensive with urine output at
least 35-40mls per hour within the next 2-4 hours.
Taking action
Efficient nurses have the responsibility to take desirable actions when it comes to the
wellness of their patients. Oostra, Astle, & Meyerhoff, (2016) defined nursing action as
the subsequent behavior from a particular decision. This stage incorporates practical skills,
communication skills as well as intellectual activities. Victor-Chmil (2014) provides that
nurses have the task decide on what plan should be the priority and what procedures and
Identifying problems
This stage requires synthesizing all of the facts of data collected and interpretations
made to make a decisive nursing diagnosis of Matthew’s major problem. According to
Gummesson Sundén & Fex (2018) appropriately identifying the main problem of the patient,
enables proper diagnosis and correct prescriptions. In the case of Matthew, his diagnosis was
Hypovolaemia and dehydration. This deterioration was caused by two Pico preps that he was
given on the night of his surgery. Fors & Gunning (2014) developed that Pico preps tend to
cause adverse effects of osmotic diarrhea. Patients suffering from osmotic diarrhea may end
up losing many liters of fluids from the circulating volume through the wall of the intestine as
the bowel is evacuated. Additionally, blood lost during Matthew’s surgery as well as through
the drainage from the bellovacs led to further depletion of intravascular volume.
Establishing goals
In every healthcare system, professional nurses and healthcare providers should
describe goals and achievements they aspire to accomplish within a given time frame.
Previous research also indicates that it is easier to achieve excellent healthcare services when
goals are set (Mamelund, 2016). Therefore, it is important Matthew to have better
management of his condition. The goal is for him to be normotensive with urine output at
least 35-40mls per hour within the next 2-4 hours.
Taking action
Efficient nurses have the responsibility to take desirable actions when it comes to the
wellness of their patients. Oostra, Astle, & Meyerhoff, (2016) defined nursing action as
the subsequent behavior from a particular decision. This stage incorporates practical skills,
communication skills as well as intellectual activities. Victor-Chmil (2014) provides that
nurses have the task decide on what plan should be the priority and what procedures and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL REASONING CYCLE 8
policies to be involved during the treatment process. Considering Matthew’s cases the most
important action is to notify the doctor if his condition, Check that the IV cannula is not
kinked or blocked as well as administering a fluid challenge and increase his IV fluid rate.
Evaluation
Matthew was given a fluid challenge as he simultaneously had his IV rate to an average of
125 mL/hr (Hollingsworth, Ferguson, & Anderson, 2016). Therefore, this stage involves
monitoring Matthew’s signs and symptoms which will determine whether the interventions
were effective or not. Evaluation of his health also includes if condition is improving.
Regardless of his cognitive remaining the same, his urine output improved to 30mL/hr and
improving blood pressure. However, he remained pale due to his poor oral intake.
Reflection
Lastly, a reflection of the healing process involves reflecting what you have gained. In my
context, next time to prevent Matthew’s deterioration I would consider controlling
hypotension. According to recent research conducted by Forsberg (2014), patients suffering
from hypotension tend to experience a decrease in glomerular filtration rate which in most
cases leads to urine output decrease. Additionally, I should have advised the doctors on how
to dress him properly to prevent excessive blood loss during surgery. I have also learned that
hypovolemic stage is common especially when patients undergo surgery. Therefore, it is vital
for professional nurses to provide constant monitoring to their patients since any deterioration
that is likely to occur would be critical (Liaw et al., 2018).
Conclusion
The paper has shown that clinical reasoning can be used a tool when it comes to providing
essential health care within the healthcare systems. Also, it has shown that it allows patients
to be taken off in their specific manner while simultaneously concentrating on their
policies to be involved during the treatment process. Considering Matthew’s cases the most
important action is to notify the doctor if his condition, Check that the IV cannula is not
kinked or blocked as well as administering a fluid challenge and increase his IV fluid rate.
Evaluation
Matthew was given a fluid challenge as he simultaneously had his IV rate to an average of
125 mL/hr (Hollingsworth, Ferguson, & Anderson, 2016). Therefore, this stage involves
monitoring Matthew’s signs and symptoms which will determine whether the interventions
were effective or not. Evaluation of his health also includes if condition is improving.
Regardless of his cognitive remaining the same, his urine output improved to 30mL/hr and
improving blood pressure. However, he remained pale due to his poor oral intake.
Reflection
Lastly, a reflection of the healing process involves reflecting what you have gained. In my
context, next time to prevent Matthew’s deterioration I would consider controlling
hypotension. According to recent research conducted by Forsberg (2014), patients suffering
from hypotension tend to experience a decrease in glomerular filtration rate which in most
cases leads to urine output decrease. Additionally, I should have advised the doctors on how
to dress him properly to prevent excessive blood loss during surgery. I have also learned that
hypovolemic stage is common especially when patients undergo surgery. Therefore, it is vital
for professional nurses to provide constant monitoring to their patients since any deterioration
that is likely to occur would be critical (Liaw et al., 2018).
Conclusion
The paper has shown that clinical reasoning can be used a tool when it comes to providing
essential health care within the healthcare systems. Also, it has shown that it allows patients
to be taken off in their specific manner while simultaneously concentrating on their
CLINICAL REASONING CYCLE 9
individual needs in regards to an effective healing process. Subsequently, it becomes to
utilize the application of the eight steps of the clinical reasoning cycle using the Levett-Jones’
Clinical Reasoning Cycle. Also, the discussion of my reflection on a clinical decision in
regards to Matthew’s case. The paper has given deep insights on the applicable Registered
Nurse Standards for Practice.
References
Canadian Association of Schools of Nursing. (2014). National nursing education framework.
Ottawa: CASN.
Cappelletti, A., Engel, J., & Prentice, D. (2014). Systematic review of clinical judgment
and reasoning in nursing. Journal of Nursing Education, 53 (8), 453-458.
Daly, P. (2018). A concise guide to clinical reasoning. Journal of evaluation in clinical
practice, 24(5), 966-972.
Forsberg, E. (2014). Virtual patients for assessment of clinical reasoning. Inst för klinisk
vetenskap, intervention och teknik/Dept of Clinical Science, Intervention and
Technology.
Fors, U., & Gunning, WT. (2014). The impact of different scoring rubrics for grading
virtual patient-based exams. Journal of Educational Computing Research, 50 (1).
individual needs in regards to an effective healing process. Subsequently, it becomes to
utilize the application of the eight steps of the clinical reasoning cycle using the Levett-Jones’
Clinical Reasoning Cycle. Also, the discussion of my reflection on a clinical decision in
regards to Matthew’s case. The paper has given deep insights on the applicable Registered
Nurse Standards for Practice.
References
Canadian Association of Schools of Nursing. (2014). National nursing education framework.
Ottawa: CASN.
Cappelletti, A., Engel, J., & Prentice, D. (2014). Systematic review of clinical judgment
and reasoning in nursing. Journal of Nursing Education, 53 (8), 453-458.
Daly, P. (2018). A concise guide to clinical reasoning. Journal of evaluation in clinical
practice, 24(5), 966-972.
Forsberg, E. (2014). Virtual patients for assessment of clinical reasoning. Inst för klinisk
vetenskap, intervention och teknik/Dept of Clinical Science, Intervention and
Technology.
Fors, U., & Gunning, WT. (2014). The impact of different scoring rubrics for grading
virtual patient-based exams. Journal of Educational Computing Research, 50 (1).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CLINICAL REASONING CYCLE 10
Forsberg, E., Ziegert, K., Hult, H., & Fors, U. (2014). Assessing progression of clinical
reasoning through Virtual Patients: an explorative study.
Gummesson, C., Sundén, A., & Fex, A. (2018). Clinical reasoning as a conceptual
framework for interprofessional learning: a literature review and a case
study. Physical Therapy Reviews, 23(1), 29-34.
Holder, A. G. (2018). Clinical Reasoning: A State of the Science Report. International
journal of nursing education scholarship, 15(1).
Hollingsworth, T. D., Ferguson, N. M., & Anderson, R. M. (2016). Will travel restrictions
control the international clinical cycles?. Nature medicine, 12(5), 497.
Keith-Lucas, B. (2015). Some influences are affecting the development of sanitary legislation
in England. The Economic History Review, 6(3), 290-296.
Kobasa, D., Takada, A., Shinya, K., Hatta, M., Halfmann, P., Theriault, S., ... & Usui, T.
(2014). Enhanced virulence clinical cycles with the haemagglutinin of the
1918 pandemic virus. Nature, 431(7009), 703.
Mamelund, S. E. (2016). Geography may explain adult mortality from the clinical trials and
tests . Epidemics, 3(1), 46-60.
Morens, D. M., Taubenberger, J. K., & Fauci, A. S. (2018). The predominant role of bacterial
pneumonia as a cause of death in pandemic influenza: implications for pandemic
influenza preparedness. The Journal of infectious diseases, 198(7), 962-970.
Oxford, J. S. (2013). The so-called Great Spanish Influenza Pandemic of 1918 may have
originated in France in 1916. Philosophical Transactions of the Royal Society
of London. Series B: Biological Sciences, 356(1416), 1857-1859.
Forsberg, E., Ziegert, K., Hult, H., & Fors, U. (2014). Assessing progression of clinical
reasoning through Virtual Patients: an explorative study.
Gummesson, C., Sundén, A., & Fex, A. (2018). Clinical reasoning as a conceptual
framework for interprofessional learning: a literature review and a case
study. Physical Therapy Reviews, 23(1), 29-34.
Holder, A. G. (2018). Clinical Reasoning: A State of the Science Report. International
journal of nursing education scholarship, 15(1).
Hollingsworth, T. D., Ferguson, N. M., & Anderson, R. M. (2016). Will travel restrictions
control the international clinical cycles?. Nature medicine, 12(5), 497.
Keith-Lucas, B. (2015). Some influences are affecting the development of sanitary legislation
in England. The Economic History Review, 6(3), 290-296.
Kobasa, D., Takada, A., Shinya, K., Hatta, M., Halfmann, P., Theriault, S., ... & Usui, T.
(2014). Enhanced virulence clinical cycles with the haemagglutinin of the
1918 pandemic virus. Nature, 431(7009), 703.
Mamelund, S. E. (2016). Geography may explain adult mortality from the clinical trials and
tests . Epidemics, 3(1), 46-60.
Morens, D. M., Taubenberger, J. K., & Fauci, A. S. (2018). The predominant role of bacterial
pneumonia as a cause of death in pandemic influenza: implications for pandemic
influenza preparedness. The Journal of infectious diseases, 198(7), 962-970.
Oxford, J. S. (2013). The so-called Great Spanish Influenza Pandemic of 1918 may have
originated in France in 1916. Philosophical Transactions of the Royal Society
of London. Series B: Biological Sciences, 356(1416), 1857-1859.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CLINICAL REASONING CYCLE 11
Selten, J. P., Brown, A. S., Moons, K. G., Slaets, J. P., Susser, E. S., & Kahn, R. S. (2016).
Critical thinking versus clinical reasoning versus clinical
judgment. Schizophrenia Research, 38(2-3), 85-91.
Liaw, S. Y., Rashasegaran, A., Wong, L. F., Deneen, C. C., Cooper, S., Levett-Jones, T., ...
&Ignacio, J. (2018). Development and psychometric testing of a Clinical
Reasoning Evaluation Simulation Tool (CREST) for assessing nursing students'
abilities to recognize and respond to clinical deterioration. Nurse education today, 62,
74-79.
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J.,
&
Hickey, N. (2010). The „five rights‟ of clinical reasoning: an educational model to
enhance nursing students‟ ability to identify and manage clinically „at risk‟ patients.
Nurse Education Today. 30(6), 515-520.
Oostra, K. L., Astle, B., & Meyerhoff, H. (2016). Clinical Reasoning on an Assignment:
Perceptions of Third Year Baccalaureate Nursing Students.
Victor-Chmil, J. (2014). Critical thinking versus clinical reasoning versus clinical judgment:
Differential diagnosis. Nurse Educator, 38(1), 34-36.
Selten, J. P., Brown, A. S., Moons, K. G., Slaets, J. P., Susser, E. S., & Kahn, R. S. (2016).
Critical thinking versus clinical reasoning versus clinical
judgment. Schizophrenia Research, 38(2-3), 85-91.
Liaw, S. Y., Rashasegaran, A., Wong, L. F., Deneen, C. C., Cooper, S., Levett-Jones, T., ...
&Ignacio, J. (2018). Development and psychometric testing of a Clinical
Reasoning Evaluation Simulation Tool (CREST) for assessing nursing students'
abilities to recognize and respond to clinical deterioration. Nurse education today, 62,
74-79.
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J.,
&
Hickey, N. (2010). The „five rights‟ of clinical reasoning: an educational model to
enhance nursing students‟ ability to identify and manage clinically „at risk‟ patients.
Nurse Education Today. 30(6), 515-520.
Oostra, K. L., Astle, B., & Meyerhoff, H. (2016). Clinical Reasoning on an Assignment:
Perceptions of Third Year Baccalaureate Nursing Students.
Victor-Chmil, J. (2014). Critical thinking versus clinical reasoning versus clinical judgment:
Differential diagnosis. Nurse Educator, 38(1), 34-36.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




