Case Study: Clinical Reasoning Cycle and Patient MR Amari's Condition
VerifiedAdded on 2020/03/01
|10
|2400
|456
Case Study
AI Summary
This case study explores the clinical reasoning process of a nurse caring for a patient, Mrs. Amari, admitted with transient ischemic attack (TIA) symptoms. The nurse follows the clinical reasoning cycle, starting with assessing the patient's situation, including her medical history of hypertension, hypercholesterolemia, and tribal customs of smoking. The case details the collection of cues, including physical assessments such as facial droop, slurred speech, and vital signs. The nurse gathers information, recalls relevant medical knowledge about TIA and stroke, interprets the gathered data, discriminates between potential diagnoses, and infers relationships between the patient's condition and her medical history and vital signs. Diagnostic tests, including the FAST and ROSIER assessments, are employed to evaluate the patient's condition, leading to the conclusion that Mrs. Amari is likely experiencing another TIA or potentially a stroke, prompting the nurse to recommend immediate interventions and diagnostic testing. The case study emphasizes the importance of a methodical approach to patient care and the application of clinical reasoning skills in identifying, diagnosing, and managing neurological conditions like TIA and stroke.

Running head: CLINICAL REASONING
CLINICAL REASONING
Name of the student:
Name of the university:
Author note:
CLINICAL REASONING
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
CLINICAL REASONING
Introduction:
Clinical reasoning cycle is a methodical procedure which is followed by nurses in their
practices as it helps them to collect information about the patients and thereby come to an
understanding about the problem or the situation of the patient. This cycle then helps the nurses
to plan and implement interventions necessary for the patients and then helps in proper
evaluation of the outcomes of the interventions on the patients. The entire situation would then
be reflected by the nurses so that they can learn from any mistakes that they have made or they
can promote their practices for betterment. In the following case study, a patient’s named MR
Amari had been admitted and the nurse would follow a proper clinical reasoning skill to develop
ideas about the interventions that she would take.
Patient’s situations:
The first step of the clinical reasoning cycle is considering the patient situations. The patient who
has been shifted from the emergency department to the medical department is called Mrs. Amari.
She is an indigenous New Zealand citizen belong to the Maori tribe. She is living with her son
and daughter in law and with two grandchildren. However, she is a patient of hypertension as
well as hypercholestemia and these had been the major contributors of the present condition she
is suffering from which is transient ischemic attack. Actually, her tribal customs had made her
take tobacco for almost years which might have had a very bad impact on her health. Although
he had quitted smoking, but the after effects had stayed with her as many researchers suggest that
smoking leads to strokes and heart disorders (Miller et al. 2016). Moreover, she has a positive
family history of heart diseases and therefore she is also within the vulnerable zone of being
affected by heart disorders. Therefore following her family history, it becomes evident that her
CLINICAL REASONING
Introduction:
Clinical reasoning cycle is a methodical procedure which is followed by nurses in their
practices as it helps them to collect information about the patients and thereby come to an
understanding about the problem or the situation of the patient. This cycle then helps the nurses
to plan and implement interventions necessary for the patients and then helps in proper
evaluation of the outcomes of the interventions on the patients. The entire situation would then
be reflected by the nurses so that they can learn from any mistakes that they have made or they
can promote their practices for betterment. In the following case study, a patient’s named MR
Amari had been admitted and the nurse would follow a proper clinical reasoning skill to develop
ideas about the interventions that she would take.
Patient’s situations:
The first step of the clinical reasoning cycle is considering the patient situations. The patient who
has been shifted from the emergency department to the medical department is called Mrs. Amari.
She is an indigenous New Zealand citizen belong to the Maori tribe. She is living with her son
and daughter in law and with two grandchildren. However, she is a patient of hypertension as
well as hypercholestemia and these had been the major contributors of the present condition she
is suffering from which is transient ischemic attack. Actually, her tribal customs had made her
take tobacco for almost years which might have had a very bad impact on her health. Although
he had quitted smoking, but the after effects had stayed with her as many researchers suggest that
smoking leads to strokes and heart disorders (Miller et al. 2016). Moreover, she has a positive
family history of heart diseases and therefore she is also within the vulnerable zone of being
affected by heart disorders. Therefore following her family history, it becomes evident that her
2
CLINICAL REASONING
heredity might have also played an important part in her present condition. After the death of her
husband, she had to move in with her son to Australia as he was not being able to cope up with
the financial crisis and had been staying in Australia and lives heavily as a carer for her
grandchildren.
Collection of cues:
The second step of the clinical reasoning cycle mainly incorporates the activity of the nurses for
collection of cues as well as information about the patient’s condition, giving a detailed
explanation of the various details which the nurse should incorporate in her time of critical
reasoning so that she can perform the next step properly.
Review:
When the patient was admitted to the hospital it was seen that the patient had a facial droop and
her mouth was diverted to the right side. She had numbness in the right side of her face and also
in the right arm. However she did not show any acute signs of stroke like weakness and were
easily able to swallow and had a steady gait. She was also able to move her extremities and was
able to follow commands. Moreover she did not have a headache and also denied nausea,
vomiting, chest pain, diaphoresis as well as visual complaints. She was alert and oriented.
Therefore, it helped nursing professionals to come to a conclusion that she was not a stroke
patient but rather suffered from TIA (Beltowski 2014). When the nurse of the next shift came,
she was handed a document which stated that all the symptoms of the patient had resolved.
However, she witnessed an entirely different case. She saw that her condition was again
deteriorating as her speech had become slurred again and the right side of the mouth is drooping.
Gather:
CLINICAL REASONING
heredity might have also played an important part in her present condition. After the death of her
husband, she had to move in with her son to Australia as he was not being able to cope up with
the financial crisis and had been staying in Australia and lives heavily as a carer for her
grandchildren.
Collection of cues:
The second step of the clinical reasoning cycle mainly incorporates the activity of the nurses for
collection of cues as well as information about the patient’s condition, giving a detailed
explanation of the various details which the nurse should incorporate in her time of critical
reasoning so that she can perform the next step properly.
Review:
When the patient was admitted to the hospital it was seen that the patient had a facial droop and
her mouth was diverted to the right side. She had numbness in the right side of her face and also
in the right arm. However she did not show any acute signs of stroke like weakness and were
easily able to swallow and had a steady gait. She was also able to move her extremities and was
able to follow commands. Moreover she did not have a headache and also denied nausea,
vomiting, chest pain, diaphoresis as well as visual complaints. She was alert and oriented.
Therefore, it helped nursing professionals to come to a conclusion that she was not a stroke
patient but rather suffered from TIA (Beltowski 2014). When the nurse of the next shift came,
she was handed a document which stated that all the symptoms of the patient had resolved.
However, she witnessed an entirely different case. She saw that her condition was again
deteriorating as her speech had become slurred again and the right side of the mouth is drooping.
Gather:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
CLINICAL REASONING
When the nurse of the next morning shift took her vital signs, they did not good results and the
nurses understood that the patient is not absolutely in the best health. When the vital signs were
taken, it showed that Blood pressure: was 175/98 which was considered to be very high as the
normal blood pressure of the individuals should be 120/80 mmHg. Her Pulse was however 9
which was within the range of 60 to 100 betas and considered normal. Her Respiratory rate: 13
which is also between the normal range of 12 to 18 breaths per minute, Oxygen saturation which
was also normal was 92%. The glucose level was found to be high as the blood glucose level was
6.6 mol much higher than the mean value of 5.5 mmol/L, Glasgow Coma Scale was 11/15.
Recall:
In most cases it is seen that TIA of the patients often exposes the patients to a stroke within 48
hours and therefore the nurse should take this point in her consideration. Usually, in the case of
TIA, blood flow to the brain usually get blocked or reduced usually by blood clots or due to the
formation of plaques in the arterial vessels. This often gives rise to stroke like symptoms (Mellon
et al. 2016). Usually within a short time, when the blood flows again, the symptoms go away.
They do not cause any brain cell damage or permanent disability. As a result of these, the tests
which were conducted did not provide any information of such occurrences in the brain like
formation of clots and others. However, this disorder often provides an early sign or warning of
the occurrences of stroke as researchers suggest that every 1 in 3 TIA patients have stroke.
Therefore the nurse should first take into consideration about the patient’s chance of having a
stroke when the symptoms of facial dropping and slurring of speech occurs again (Catangui et al.
2015). For this the nurse should at first provide her with medication to remove any plaques or
fatty deposits from the vessel or to prevent blood clots in the arteries that supply blood to the
brain and immediately perform diagnostic tests to confirm whether she is having another attack
CLINICAL REASONING
When the nurse of the next morning shift took her vital signs, they did not good results and the
nurses understood that the patient is not absolutely in the best health. When the vital signs were
taken, it showed that Blood pressure: was 175/98 which was considered to be very high as the
normal blood pressure of the individuals should be 120/80 mmHg. Her Pulse was however 9
which was within the range of 60 to 100 betas and considered normal. Her Respiratory rate: 13
which is also between the normal range of 12 to 18 breaths per minute, Oxygen saturation which
was also normal was 92%. The glucose level was found to be high as the blood glucose level was
6.6 mol much higher than the mean value of 5.5 mmol/L, Glasgow Coma Scale was 11/15.
Recall:
In most cases it is seen that TIA of the patients often exposes the patients to a stroke within 48
hours and therefore the nurse should take this point in her consideration. Usually, in the case of
TIA, blood flow to the brain usually get blocked or reduced usually by blood clots or due to the
formation of plaques in the arterial vessels. This often gives rise to stroke like symptoms (Mellon
et al. 2016). Usually within a short time, when the blood flows again, the symptoms go away.
They do not cause any brain cell damage or permanent disability. As a result of these, the tests
which were conducted did not provide any information of such occurrences in the brain like
formation of clots and others. However, this disorder often provides an early sign or warning of
the occurrences of stroke as researchers suggest that every 1 in 3 TIA patients have stroke.
Therefore the nurse should first take into consideration about the patient’s chance of having a
stroke when the symptoms of facial dropping and slurring of speech occurs again (Catangui et al.
2015). For this the nurse should at first provide her with medication to remove any plaques or
fatty deposits from the vessel or to prevent blood clots in the arteries that supply blood to the
brain and immediately perform diagnostic tests to confirm whether she is having another attack
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
CLINICAL REASONING
of TIA or is having a stroke. The neurological assessment that would mainly be conducted by the
nurse is the FAST assessment which mainly checks the face, arm, speech and time test. The
score of the test would help her o understand the seriousness of the issue. She can also conduct
the Rosier scale test to check the occurrence of stroke possibility (Howard 2016). She should
perform magnetic resonance imaging called MIR scan, computerized topography scan to test for
TIA. For the diagnosis of stroke, she should perform tests like carotid ultrasound, cerebral
angiogram, echocardiogram. The results of the tests have to be verified in order to check whether
she is having another TIA or stroke.
The next step of the clinical reasoning cycle is processing of the information that the nurse
usually collects by handling the case effectively.
Interpret:
The next step of the clinical reasoning cycle is processing of the information that the nurse
usually collects by handling the case effectively. The first step is the interpretation steps where
the nurses need to assess the result of the steps that she had conducted. In this case, the nurses
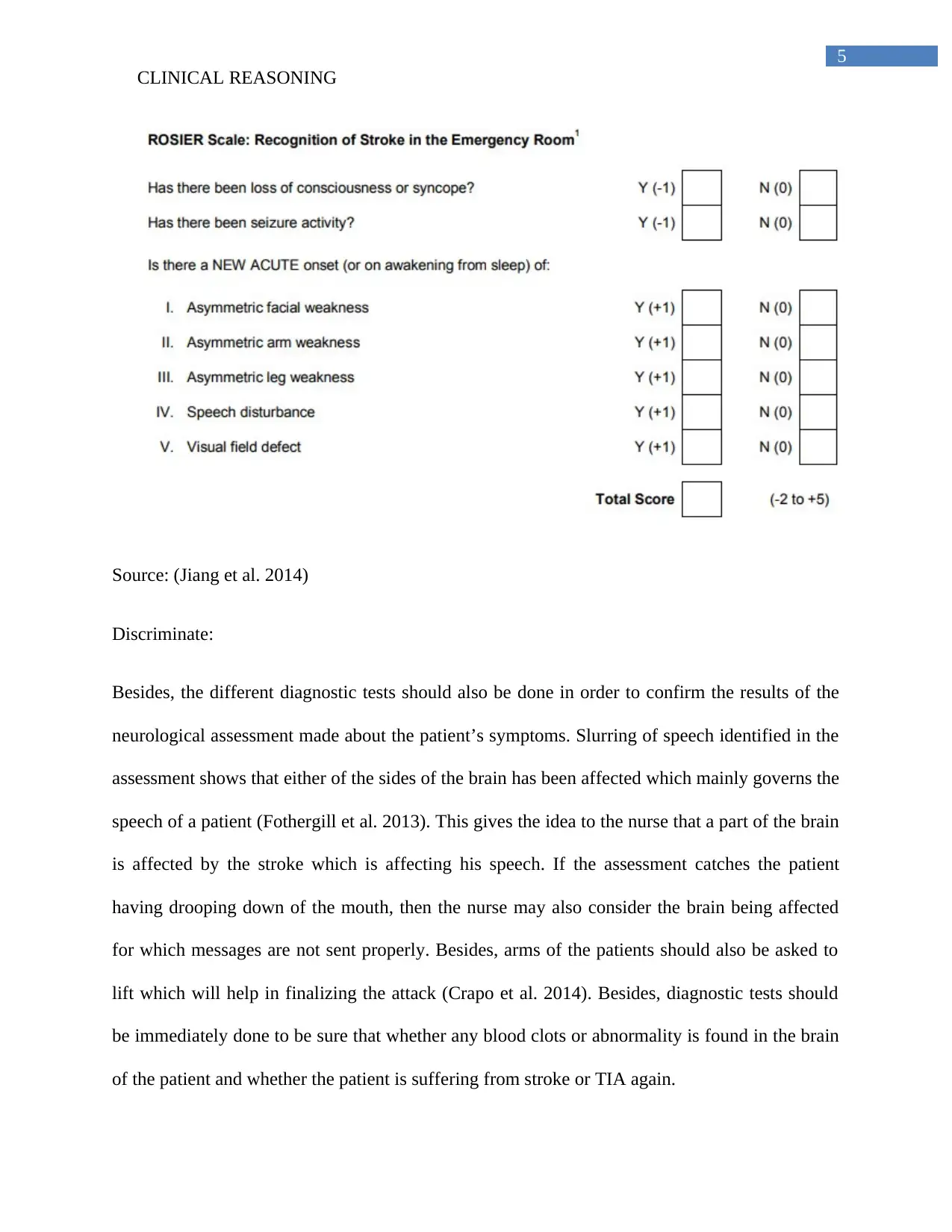
need to conduct the FAST tool assessment as well as the ROSIER assessment. In the FAST
assessment, the nurse should check whether the Face has drooped, whether the patient can lift
both the arms, has their speech slurred and if all the three things are present there is an
emergency and suggests that the Time is critical for the patients (Wang et al. 2013). Moreover
form the rosier scale assessment; if the marks are greater than or equal to +1, then the nurse may
become sure of the attack of stroke (Jiang et al. 2014).
CLINICAL REASONING
of TIA or is having a stroke. The neurological assessment that would mainly be conducted by the
nurse is the FAST assessment which mainly checks the face, arm, speech and time test. The
score of the test would help her o understand the seriousness of the issue. She can also conduct
the Rosier scale test to check the occurrence of stroke possibility (Howard 2016). She should
perform magnetic resonance imaging called MIR scan, computerized topography scan to test for
TIA. For the diagnosis of stroke, she should perform tests like carotid ultrasound, cerebral
angiogram, echocardiogram. The results of the tests have to be verified in order to check whether
she is having another TIA or stroke.
The next step of the clinical reasoning cycle is processing of the information that the nurse
usually collects by handling the case effectively.
Interpret:
The next step of the clinical reasoning cycle is processing of the information that the nurse
usually collects by handling the case effectively. The first step is the interpretation steps where
the nurses need to assess the result of the steps that she had conducted. In this case, the nurses
need to conduct the FAST tool assessment as well as the ROSIER assessment. In the FAST
assessment, the nurse should check whether the Face has drooped, whether the patient can lift
both the arms, has their speech slurred and if all the three things are present there is an
emergency and suggests that the Time is critical for the patients (Wang et al. 2013). Moreover
form the rosier scale assessment; if the marks are greater than or equal to +1, then the nurse may
become sure of the attack of stroke (Jiang et al. 2014).
5
CLINICAL REASONING
Source: (Jiang et al. 2014)
Discriminate:
Besides, the different diagnostic tests should also be done in order to confirm the results of the
neurological assessment made about the patient’s symptoms. Slurring of speech identified in the
assessment shows that either of the sides of the brain has been affected which mainly governs the
speech of a patient (Fothergill et al. 2013). This gives the idea to the nurse that a part of the brain
is affected by the stroke which is affecting his speech. If the assessment catches the patient
having drooping down of the mouth, then the nurse may also consider the brain being affected
for which messages are not sent properly. Besides, arms of the patients should also be asked to
lift which will help in finalizing the attack (Crapo et al. 2014). Besides, diagnostic tests should
be immediately done to be sure that whether any blood clots or abnormality is found in the brain
of the patient and whether the patient is suffering from stroke or TIA again.
CLINICAL REASONING
Source: (Jiang et al. 2014)
Discriminate:
Besides, the different diagnostic tests should also be done in order to confirm the results of the
neurological assessment made about the patient’s symptoms. Slurring of speech identified in the
assessment shows that either of the sides of the brain has been affected which mainly governs the
speech of a patient (Fothergill et al. 2013). This gives the idea to the nurse that a part of the brain
is affected by the stroke which is affecting his speech. If the assessment catches the patient
having drooping down of the mouth, then the nurse may also consider the brain being affected
for which messages are not sent properly. Besides, arms of the patients should also be asked to
lift which will help in finalizing the attack (Crapo et al. 2014). Besides, diagnostic tests should
be immediately done to be sure that whether any blood clots or abnormality is found in the brain
of the patient and whether the patient is suffering from stroke or TIA again.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
CLINICAL REASONING
The change of the GCS scale from 15 to 11 showed that the patients should be immediately
taken to the emergency wards for treatment as her condition was found to be deteriorating. Nerve
damage was the main reason that were resulting in the slurring of voice and face droop. Oxygen
saturation decrease was giving clues that her vital organs are having less oxygen which could
have caused her in loss of consciousness and adults.
Infer and relate:
The next part would be to infer and relate the patients assessment results with the main
rationale hat has resulted in the occurrence of the symptoms. The vital signs show that the patient
has high blood pressure than normal. The patient is already seen to suffer from hypertension.
When the pressure of blood is high, it can lead to stroke by the damaging as well as the
weakening of the brains’ blood vessels (Miller et al., 2016). This causes them to be narrow or
even leads to rupture and leak. High blood pressure can also lead to form blood clots in the
arteries which lead to brain that blocks the blood flow and causes stroke. She is also a patient of
hypercholestemia for which cholesterol which is a fatty substance in the blood can increase in
number and high cholesterol in the arteries block the normal flow of blood to brain causing
stroke (Jatuzis 2015). All these might have occurred in the patient and therefore the patient is
suffering from symptoms of stroke or TIA.
Conclusion:
Therefore the nurse who has to handle a patient showing symptoms of stroke or TIA has
first have to conduct a vital sign analysis and neurological assessments of the patient. These tests
would be finalized by the performing of important diagnostic tests like MIR, CT scan and others.
Then the nurse should try to relate the patient history with the biological rational of the
CLINICAL REASONING
The change of the GCS scale from 15 to 11 showed that the patients should be immediately
taken to the emergency wards for treatment as her condition was found to be deteriorating. Nerve
damage was the main reason that were resulting in the slurring of voice and face droop. Oxygen
saturation decrease was giving clues that her vital organs are having less oxygen which could
have caused her in loss of consciousness and adults.
Infer and relate:
The next part would be to infer and relate the patients assessment results with the main
rationale hat has resulted in the occurrence of the symptoms. The vital signs show that the patient
has high blood pressure than normal. The patient is already seen to suffer from hypertension.
When the pressure of blood is high, it can lead to stroke by the damaging as well as the
weakening of the brains’ blood vessels (Miller et al., 2016). This causes them to be narrow or
even leads to rupture and leak. High blood pressure can also lead to form blood clots in the
arteries which lead to brain that blocks the blood flow and causes stroke. She is also a patient of
hypercholestemia for which cholesterol which is a fatty substance in the blood can increase in
number and high cholesterol in the arteries block the normal flow of blood to brain causing
stroke (Jatuzis 2015). All these might have occurred in the patient and therefore the patient is
suffering from symptoms of stroke or TIA.
Conclusion:
Therefore the nurse who has to handle a patient showing symptoms of stroke or TIA has
first have to conduct a vital sign analysis and neurological assessments of the patient. These tests
would be finalized by the performing of important diagnostic tests like MIR, CT scan and others.
Then the nurse should try to relate the patient history with the biological rational of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
CLINICAL REASONING
occurrence of the attacks. These would help her to develop interventions based on the
management of the causing factors.
References:
Bełtowski, J. 2014. Priority paper evaluation: Reverse epidemiology in ischemic stroke: High
cholesterol as a predictor of improved survival in stroke patients. Clinical Lipidology, 9(2), 135-
139.
CLINICAL REASONING
occurrence of the attacks. These would help her to develop interventions based on the
management of the causing factors.
References:
Bełtowski, J. 2014. Priority paper evaluation: Reverse epidemiology in ischemic stroke: High
cholesterol as a predictor of improved survival in stroke patients. Clinical Lipidology, 9(2), 135-
139.
8
CLINICAL REASONING
Catangui, E.J., 2015. Thrombolysis for patients with acute ischaemic stroke. Nursing
Standard, 30(8), pp.40-44.
Howard, R.S., 2016. The management of ischaemic stroke. Anaesthesia & Intensive Care
Medicine, 17(12), pp.591-595.
Jatuzis, D., 2015. Ongoing Discussions on Reliability of Diagnosis of Transient Ischemic
Attack. Neuroepidemiology, 45(2), pp.111-112.
Mellon, L., Doyle, F., Williams, D., Brewer, L., Hall, P., and Hickey, A. 2016. Patient behaviour
at the time of stroke onset: a cross-sectional survey of patient response to stroke
symptoms. Emerg Med J, emermed-2015.
Miller, A. P., Navar, A. M., Roubin, G. S., & Oparil, S. (2016). Cardiovascular care for older
adults: hypertension and stroke in the older adult. Journal of geriatric cardiology: JGC, 13(5),
373.
Wang, Y., Wang, Y., Zhao, X., Liu, L., Wang, D., Wang, C., Wang, C., Li, H., Meng, X., Cui, L.
and Jia, J., 2013. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. New
England Journal of Medicine, 369(1), pp.11-19.
Jiang, H.L., Chan, C.P.Y., Leung, Y.K., Li, Y.M., Graham, C.A. and Rainer, T.H., 2014.
Evaluation of the Recognition of Stroke in the Emergency Room (ROSIER) scale in Chinese
patients in Hong Kong. PloS one, 9(10), p.e109762.
CLINICAL REASONING
Catangui, E.J., 2015. Thrombolysis for patients with acute ischaemic stroke. Nursing
Standard, 30(8), pp.40-44.
Howard, R.S., 2016. The management of ischaemic stroke. Anaesthesia & Intensive Care
Medicine, 17(12), pp.591-595.
Jatuzis, D., 2015. Ongoing Discussions on Reliability of Diagnosis of Transient Ischemic
Attack. Neuroepidemiology, 45(2), pp.111-112.
Mellon, L., Doyle, F., Williams, D., Brewer, L., Hall, P., and Hickey, A. 2016. Patient behaviour
at the time of stroke onset: a cross-sectional survey of patient response to stroke
symptoms. Emerg Med J, emermed-2015.
Miller, A. P., Navar, A. M., Roubin, G. S., & Oparil, S. (2016). Cardiovascular care for older
adults: hypertension and stroke in the older adult. Journal of geriatric cardiology: JGC, 13(5),
373.
Wang, Y., Wang, Y., Zhao, X., Liu, L., Wang, D., Wang, C., Wang, C., Li, H., Meng, X., Cui, L.
and Jia, J., 2013. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. New
England Journal of Medicine, 369(1), pp.11-19.
Jiang, H.L., Chan, C.P.Y., Leung, Y.K., Li, Y.M., Graham, C.A. and Rainer, T.H., 2014.
Evaluation of the Recognition of Stroke in the Emergency Room (ROSIER) scale in Chinese
patients in Hong Kong. PloS one, 9(10), p.e109762.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
CLINICAL REASONING
Fothergill, R.T., Williams, J., Edwards, M.J., Russell, I.T. and Gompertz, P., 2013. Does use of
the recognition of stroke in the emergency room stroke assessment tool enhance stroke
recognition by ambulance clinicians?. Stroke, 44(11), pp.3007-3012.
Crapo, S.A., Wooten, J.M. and Brice, J.H., 2014. Stroke and transient ischemic
attack. Prehospital Care of Neurologic Emergencies, p.63.
CLINICAL REASONING
Fothergill, R.T., Williams, J., Edwards, M.J., Russell, I.T. and Gompertz, P., 2013. Does use of
the recognition of stroke in the emergency room stroke assessment tool enhance stroke
recognition by ambulance clinicians?. Stroke, 44(11), pp.3007-3012.
Crapo, S.A., Wooten, J.M. and Brice, J.H., 2014. Stroke and transient ischemic
attack. Prehospital Care of Neurologic Emergencies, p.63.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





