Seclusion Report: Clinical Audit on Seclusion in Mental Health Care
VerifiedAdded on 2020/03/04
|24
|7229
|31
Report
AI Summary
This report, titled "Seclusion," addresses the controversial practice of seclusion in mental health hospitals, focusing on its use to control aggressive behavior in psychiatric patients. The report begins with an introduction outlining the rationale and aims, followed by a background and rationale that discusses the advantages of seclusion over restraints. It presents a clinical audit question and a PICO (Population, Intervention, Comparison, Outcome) framework, along with a detailed search strategy involving various databases, keywords, and inclusion/exclusion criteria. The report then critically analyzes the evidence obtained through the Joanna Briggs Institute's levels of evidence, examining themes such as recovery-oriented care and effective support. It highlights findings from multiple studies, emphasizing the importance of patient-centered care, staff training, and adherence to best practices to ensure patient safety and well-being. The report concludes by discussing the implications of these findings for evidence-based practice and providing recommendations for improving seclusion practices in mental health settings.

Running head: SECLUSION
Seclusion
Name of the Student
Name of the University
Author note
Seclusion
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1SECLUSION
Introduction
The aim of the report paper part A is to develop a clinical audit question regarding the
use of seclusion for the psychiatric patients in mental health hospitals. For this, the background
and rationale will be discussed in the first section of the report. A clinical audit question will be
outlined and the development of the PICO question is discussed in the following sections with
the search strategy. Thereafter, part B will deal with the critical analysis of the evidences that
will be obtained to develop the clinical bottom line and best recommendations for the evidence-
based practice.
Part A
Background and Rationale
Although, seclusion is an emotive and controversial subject in mental health nursing, it is
still practiced in the mental health hospitals widely. There are varied opinions regarding the use
of this practice, however, it is still a legitimate intervention to use seclusion as compared to the
efficacy of restraints to control aggressive behaviour in psychiatric patients (Knox & Holloman
Jr, 2012). The focus of the paper is the use of seclusion to control aggressive behaviour through
safe practice and guidelines in mental health patients as practiced in mental health institutions.
The rationale for choosing this topic is that restraint in psychiatric patients has led to
exacerbation of aggressive behaviour that cause harm to other patients and mental staffs. On the
other hand, seclusion is preferred over restraint in managing and protecting the patients from
aggressive behaviour. Seclusion causes no harm to the patients and is an effective intervention
for the management of the aggressive incidents.
Introduction
The aim of the report paper part A is to develop a clinical audit question regarding the
use of seclusion for the psychiatric patients in mental health hospitals. For this, the background
and rationale will be discussed in the first section of the report. A clinical audit question will be
outlined and the development of the PICO question is discussed in the following sections with
the search strategy. Thereafter, part B will deal with the critical analysis of the evidences that
will be obtained to develop the clinical bottom line and best recommendations for the evidence-
based practice.
Part A
Background and Rationale
Although, seclusion is an emotive and controversial subject in mental health nursing, it is
still practiced in the mental health hospitals widely. There are varied opinions regarding the use
of this practice, however, it is still a legitimate intervention to use seclusion as compared to the
efficacy of restraints to control aggressive behaviour in psychiatric patients (Knox & Holloman
Jr, 2012). The focus of the paper is the use of seclusion to control aggressive behaviour through
safe practice and guidelines in mental health patients as practiced in mental health institutions.
The rationale for choosing this topic is that restraint in psychiatric patients has led to
exacerbation of aggressive behaviour that cause harm to other patients and mental staffs. On the
other hand, seclusion is preferred over restraint in managing and protecting the patients from
aggressive behaviour. Seclusion causes no harm to the patients and is an effective intervention
for the management of the aggressive incidents.
2SECLUSION
According to Perkins et al., (2012), the mental health nurses for inpatients in psychiatric
wards practice restraint when a patient shows aggressive behaviour, acts out or does not follow
the rules. However, current data suggests that restraints is not a therapeutic intervention, rather
jeopardise the mental health status of the psychiatric patients. In a structured questionnaire study
conducted by Vishnivetsky et al., (2013), secluding psychiatric adolescent inpatients was
preferable as compared to physical restraint. About 82% of the total participants preferred
secluding in the room is preferable as it was less frightening and improved their mental status as
compared to restraint. On a contrary, seclusion is used that maximizes the freedom of the
patients and protect them from risk by providing them a safe and secure environment
(Vishnivetsky et al., 2013). However, there are various arguments reading the use of seclusion as
it deprives them of liberty and practice social control as a coercive and negative experience.
There is mixed literature regarding the use of seclusion as a way to control violent behaviour and
have long-term benefits, however, seclusion is a safe option than restraints.
In seclusion, the psychiatric patient is locked in a room, is being isolated from other
patients and medical staffs, with loose items, and is allowed to leave the room. The locked
patient is continuously observed and is a direct response to their aggressive behaviour that it is
because of a psychological behaviour. Thus, the clinical audit will be focusing on the seclusion
practice as a better intervention in controlling aggressive behaviour than restraint in psychiatric
patients. The best practice is to provide seclusion where as compared to restraint and the mental
ward nurses consider it a clear benefit for the person who is being secluded. It is considered a
protective measure where the mental ward nurses utilize seclusion complying with the best
practice and for the benefit of the patient. Although, seclusion is used insufficiently in the current
practice, however while using the nurses follow basic guidelines and standards while utilizing
According to Perkins et al., (2012), the mental health nurses for inpatients in psychiatric
wards practice restraint when a patient shows aggressive behaviour, acts out or does not follow
the rules. However, current data suggests that restraints is not a therapeutic intervention, rather
jeopardise the mental health status of the psychiatric patients. In a structured questionnaire study
conducted by Vishnivetsky et al., (2013), secluding psychiatric adolescent inpatients was
preferable as compared to physical restraint. About 82% of the total participants preferred
secluding in the room is preferable as it was less frightening and improved their mental status as
compared to restraint. On a contrary, seclusion is used that maximizes the freedom of the
patients and protect them from risk by providing them a safe and secure environment
(Vishnivetsky et al., 2013). However, there are various arguments reading the use of seclusion as
it deprives them of liberty and practice social control as a coercive and negative experience.
There is mixed literature regarding the use of seclusion as a way to control violent behaviour and
have long-term benefits, however, seclusion is a safe option than restraints.
In seclusion, the psychiatric patient is locked in a room, is being isolated from other
patients and medical staffs, with loose items, and is allowed to leave the room. The locked
patient is continuously observed and is a direct response to their aggressive behaviour that it is
because of a psychological behaviour. Thus, the clinical audit will be focusing on the seclusion
practice as a better intervention in controlling aggressive behaviour than restraint in psychiatric
patients. The best practice is to provide seclusion where as compared to restraint and the mental
ward nurses consider it a clear benefit for the person who is being secluded. It is considered a
protective measure where the mental ward nurses utilize seclusion complying with the best
practice and for the benefit of the patient. Although, seclusion is used insufficiently in the current
practice, however while using the nurses follow basic guidelines and standards while utilizing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3SECLUSION
seclusion (Osborne & Webster, 2009). They follow safe delivery of seclusion in a secure
environment that ensures patient safety prioritizing staff education and support so that there is
patient-centred care and strong leadership, monitoring, commitment, oversight and transparency
while using seclusion in psychiatric wards (Kuosmanen et al., 2015). The current practice also
suggests that mental health staffs should abide by the principles of seclusion like use of positive
behavioural support and decreased use of physical restraint. Mental health nurses also take into
account the policy considerations that manage risk. According to Kontio et al., (2012), the nurses
choose seclusion as the last option; however, they use it when they are not left with any other
option. They do not continue it for longer and use it as a way to safeguard the patient and staffs
from violent behaviour.
The care staffs keep the secluded person in sight, sound inside the secluded room, and
observe them directly through CCTV or direct observation. The nurse ensures that the patient is
safe inside the room and pay attention to the consciousness level of the secluded patient. They
also stay alert and concerned about the particular needs of the patient and provide immediate
care for the secluded patient. However, in the real world scenario, mental health nurses does not
comply with the guidelines of seclusion and are attempting to include the best practice in the
seclusion (Jacobsen, 2012). For this, the nurses need to be properly trained and be competent
with the recovery principles after seclusion and informed care.
Clinical audit topic
Do nurses in mental health wards comply with best practice when utilising seclusion?
seclusion (Osborne & Webster, 2009). They follow safe delivery of seclusion in a secure
environment that ensures patient safety prioritizing staff education and support so that there is
patient-centred care and strong leadership, monitoring, commitment, oversight and transparency
while using seclusion in psychiatric wards (Kuosmanen et al., 2015). The current practice also
suggests that mental health staffs should abide by the principles of seclusion like use of positive
behavioural support and decreased use of physical restraint. Mental health nurses also take into
account the policy considerations that manage risk. According to Kontio et al., (2012), the nurses
choose seclusion as the last option; however, they use it when they are not left with any other
option. They do not continue it for longer and use it as a way to safeguard the patient and staffs
from violent behaviour.
The care staffs keep the secluded person in sight, sound inside the secluded room, and
observe them directly through CCTV or direct observation. The nurse ensures that the patient is
safe inside the room and pay attention to the consciousness level of the secluded patient. They
also stay alert and concerned about the particular needs of the patient and provide immediate
care for the secluded patient. However, in the real world scenario, mental health nurses does not
comply with the guidelines of seclusion and are attempting to include the best practice in the
seclusion (Jacobsen, 2012). For this, the nurses need to be properly trained and be competent
with the recovery principles after seclusion and informed care.
Clinical audit topic
Do nurses in mental health wards comply with best practice when utilising seclusion?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4SECLUSION
Application of PICO
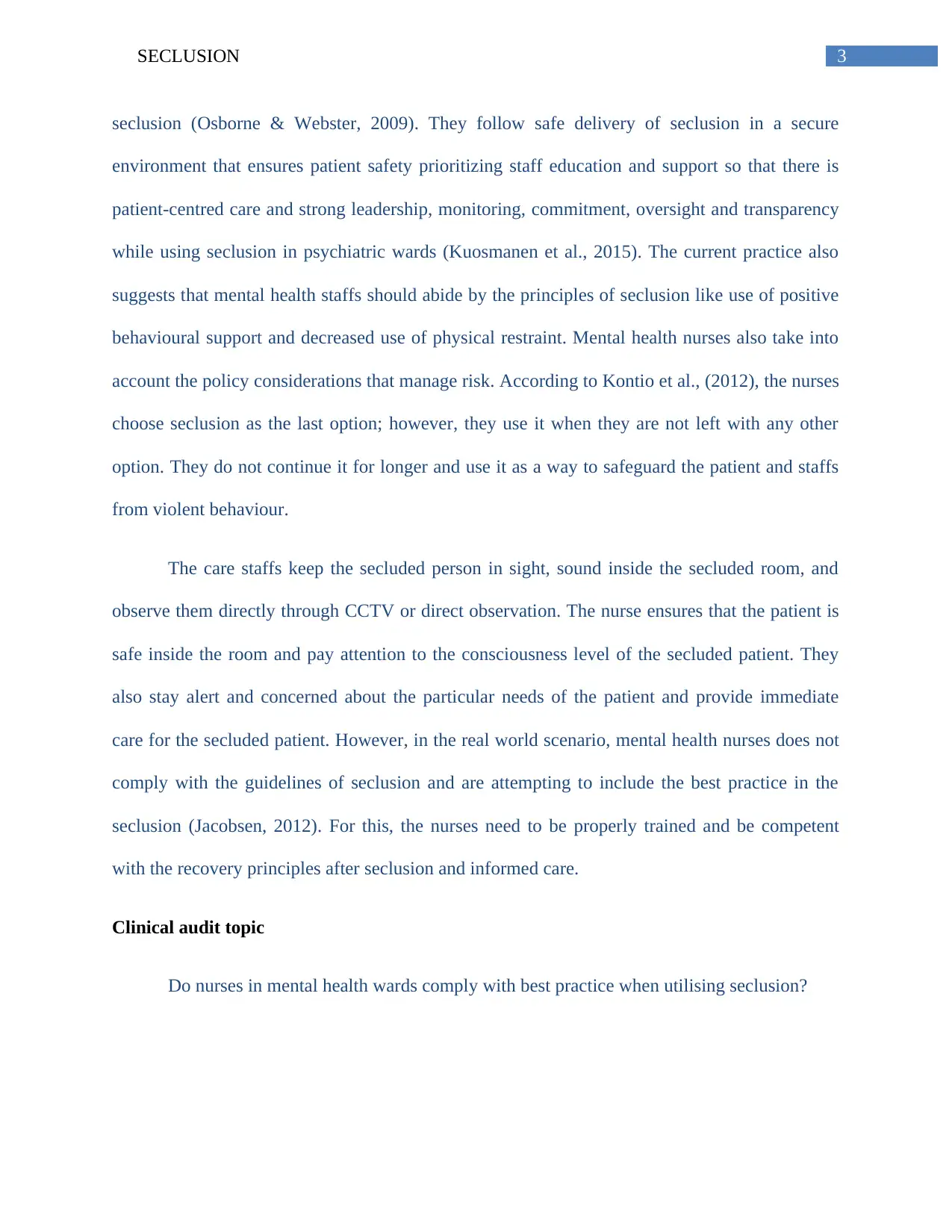
The audit topic is broken into a PICO format that explains that Population, Intervention
as a treatment option, procedure or a diagnostic test as compared to another intervention and the
outcome of the applied intervention (Methley et al., 2014). This format is helpful in defining the
clinical audit topic and enables us to carry out a useful search by using keywords and Boolean
operators (Robinson, Saldanha & Mckoy, 2011).
Table 1 (Application of PICO)
Population Psychiatric patients who show aggressive
behaviour due to psychological disorders are not
managed or controlled in a proper way by the
nursing staffs. Incorrect management can harm the
other patients and staffs in the wards and have
serious consequences to the patient’s well-being.
Intervention Seclusion is an intervention that can be used for
controlling aggressive behaviour in inpatients in a
psychiatric ward.
Comparison The multidisciplinary team (MDT) should also
utilize the same guidelines or approach while using
seclusion. According to New South Wales (NSW)
for Clinical Innovation, although seclusion need to
be reduced in the psychiatric units, there should be
proper care plan, staff training and education and
well handover meetings to ensure safety of the
Application of PICO
The audit topic is broken into a PICO format that explains that Population, Intervention
as a treatment option, procedure or a diagnostic test as compared to another intervention and the
outcome of the applied intervention (Methley et al., 2014). This format is helpful in defining the
clinical audit topic and enables us to carry out a useful search by using keywords and Boolean
operators (Robinson, Saldanha & Mckoy, 2011).
Table 1 (Application of PICO)
Population Psychiatric patients who show aggressive
behaviour due to psychological disorders are not
managed or controlled in a proper way by the
nursing staffs. Incorrect management can harm the
other patients and staffs in the wards and have
serious consequences to the patient’s well-being.
Intervention Seclusion is an intervention that can be used for
controlling aggressive behaviour in inpatients in a
psychiatric ward.
Comparison The multidisciplinary team (MDT) should also
utilize the same guidelines or approach while using
seclusion. According to New South Wales (NSW)
for Clinical Innovation, although seclusion need to
be reduced in the psychiatric units, there should be
proper care plan, staff training and education and
well handover meetings to ensure safety of the
5SECLUSION
patient and staffs (Callaghan & Ryan, 2014).
Outcome It is reasonable to suggest that although seclusion
has no proper therapeutic benefits, it is used by the
nurses, at the same time should assure that
everyone is safe, and causes no harm.
Search strategy and findings
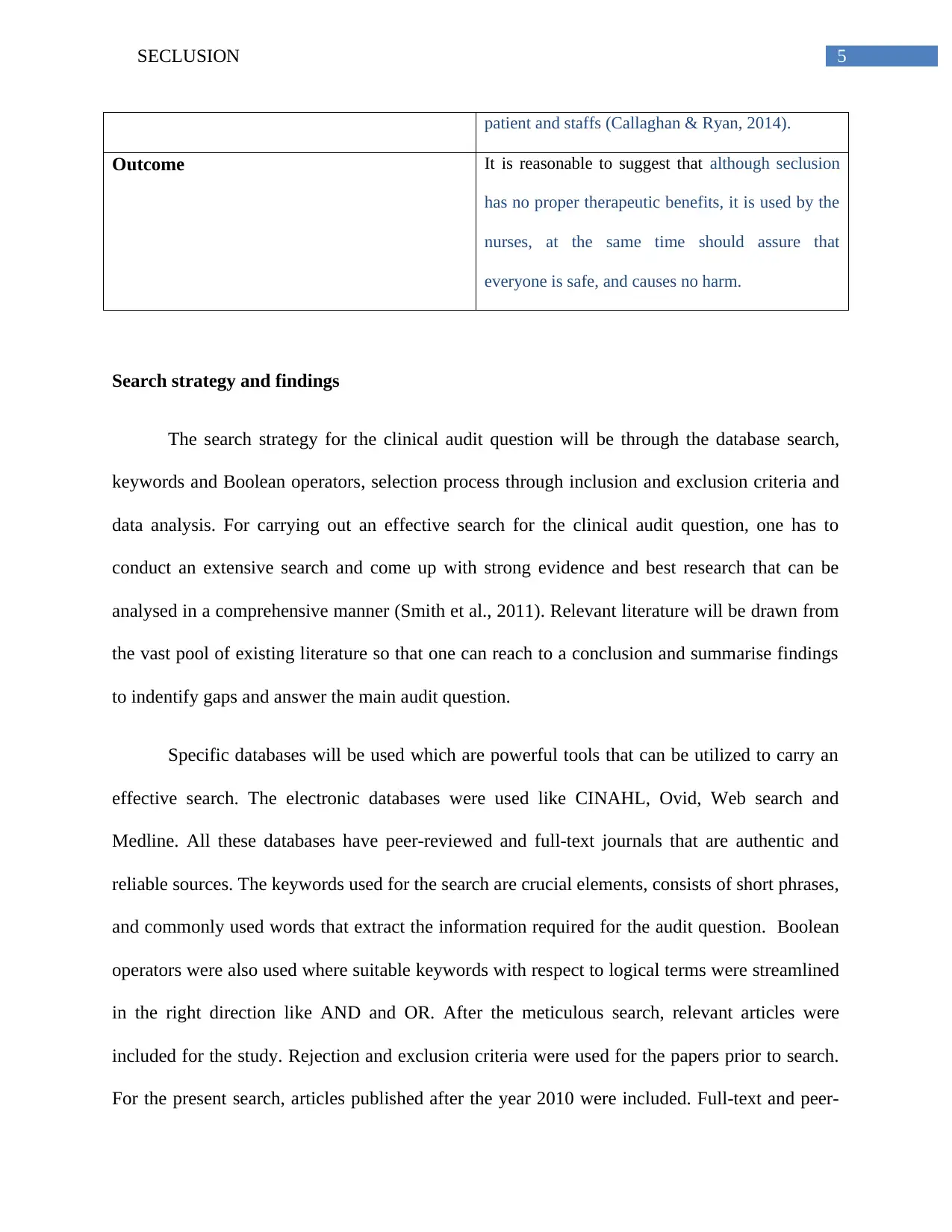
The search strategy for the clinical audit question will be through the database search,
keywords and Boolean operators, selection process through inclusion and exclusion criteria and
data analysis. For carrying out an effective search for the clinical audit question, one has to
conduct an extensive search and come up with strong evidence and best research that can be
analysed in a comprehensive manner (Smith et al., 2011). Relevant literature will be drawn from
the vast pool of existing literature so that one can reach to a conclusion and summarise findings
to indentify gaps and answer the main audit question.
Specific databases will be used which are powerful tools that can be utilized to carry an
effective search. The electronic databases were used like CINAHL, Ovid, Web search and
Medline. All these databases have peer-reviewed and full-text journals that are authentic and
reliable sources. The keywords used for the search are crucial elements, consists of short phrases,
and commonly used words that extract the information required for the audit question. Boolean
operators were also used where suitable keywords with respect to logical terms were streamlined
in the right direction like AND and OR. After the meticulous search, relevant articles were
included for the study. Rejection and exclusion criteria were used for the papers prior to search.
For the present search, articles published after the year 2010 were included. Full-text and peer-
patient and staffs (Callaghan & Ryan, 2014).
Outcome It is reasonable to suggest that although seclusion
has no proper therapeutic benefits, it is used by the
nurses, at the same time should assure that
everyone is safe, and causes no harm.
Search strategy and findings
The search strategy for the clinical audit question will be through the database search,
keywords and Boolean operators, selection process through inclusion and exclusion criteria and
data analysis. For carrying out an effective search for the clinical audit question, one has to
conduct an extensive search and come up with strong evidence and best research that can be
analysed in a comprehensive manner (Smith et al., 2011). Relevant literature will be drawn from
the vast pool of existing literature so that one can reach to a conclusion and summarise findings
to indentify gaps and answer the main audit question.
Specific databases will be used which are powerful tools that can be utilized to carry an
effective search. The electronic databases were used like CINAHL, Ovid, Web search and
Medline. All these databases have peer-reviewed and full-text journals that are authentic and
reliable sources. The keywords used for the search are crucial elements, consists of short phrases,
and commonly used words that extract the information required for the audit question. Boolean
operators were also used where suitable keywords with respect to logical terms were streamlined
in the right direction like AND and OR. After the meticulous search, relevant articles were
included for the study. Rejection and exclusion criteria were used for the papers prior to search.
For the present search, articles published after the year 2010 were included. Full-text and peer-
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6SECLUSION
reviewed articles were included and 20 articles were screened for studies. The selected articles
were in English language form different countries and use of seclusion for aggression
management in psychiatric patients.
Clinical Practice Guidelines from the (National Health and Medical Research Council)
NHMRC suggest that under the Australian National Seclusion and Restraint Project, mental
health facilities should follow the key principles while utilizing the seclusion. There should be
protection of fundamental human rights, right to highest care, protection of the secluded person
against degrading treatment, right to medical examination, compliance with regulations and
legislation and most importantly, benefit of the secluded person (Runciman et al., 2012).
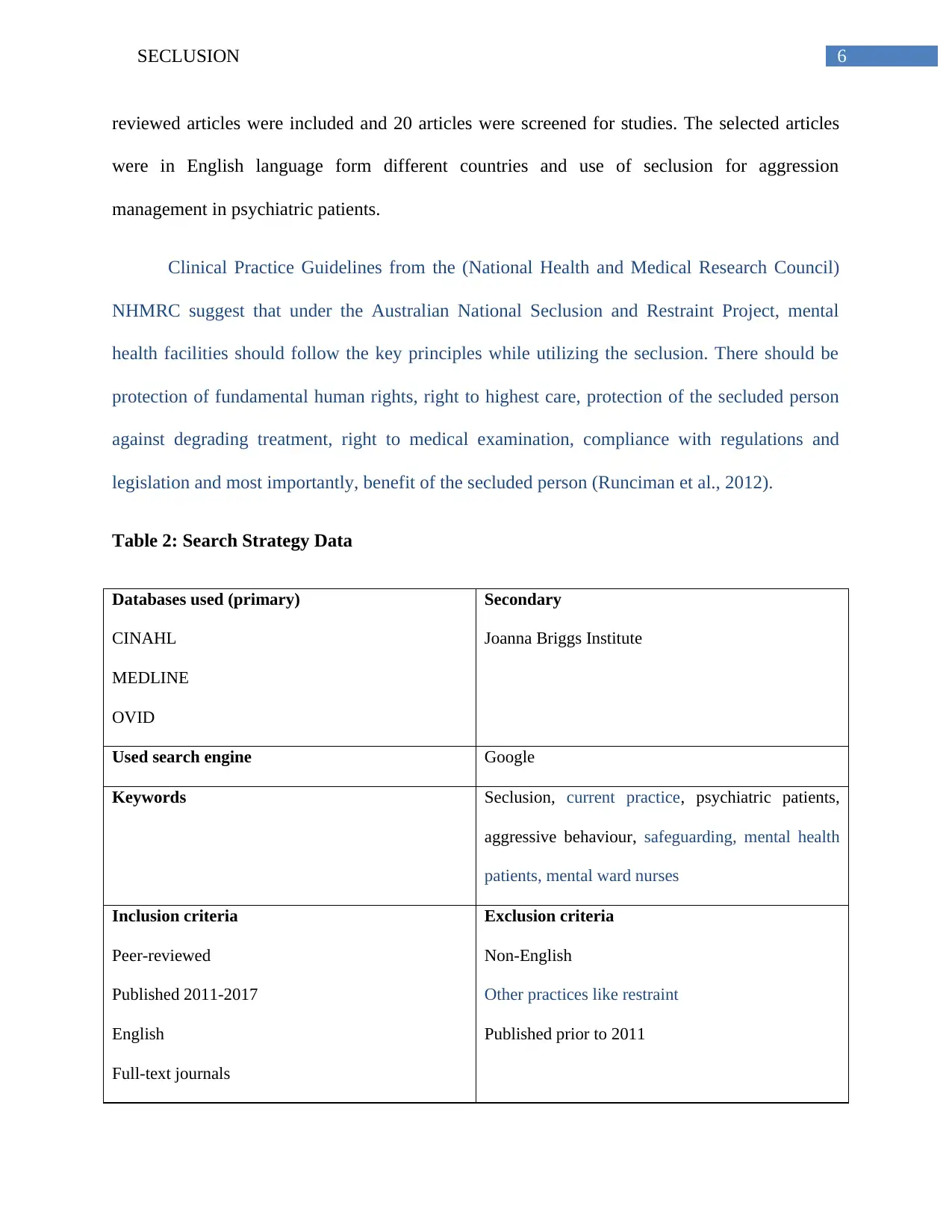
Table 2: Search Strategy Data
Databases used (primary)
CINAHL
MEDLINE
OVID
Secondary
Joanna Briggs Institute
Used search engine Google
Keywords Seclusion, current practice, psychiatric patients,
aggressive behaviour, safeguarding, mental health
patients, mental ward nurses
Inclusion criteria
Peer-reviewed
Published 2011-2017
English
Full-text journals
Exclusion criteria
Non-English
Other practices like restraint
Published prior to 2011
reviewed articles were included and 20 articles were screened for studies. The selected articles
were in English language form different countries and use of seclusion for aggression
management in psychiatric patients.
Clinical Practice Guidelines from the (National Health and Medical Research Council)
NHMRC suggest that under the Australian National Seclusion and Restraint Project, mental
health facilities should follow the key principles while utilizing the seclusion. There should be
protection of fundamental human rights, right to highest care, protection of the secluded person
against degrading treatment, right to medical examination, compliance with regulations and
legislation and most importantly, benefit of the secluded person (Runciman et al., 2012).
Table 2: Search Strategy Data
Databases used (primary)
CINAHL
MEDLINE
OVID
Secondary
Joanna Briggs Institute
Used search engine Google
Keywords Seclusion, current practice, psychiatric patients,
aggressive behaviour, safeguarding, mental health
patients, mental ward nurses
Inclusion criteria
Peer-reviewed
Published 2011-2017
English
Full-text journals
Exclusion criteria
Non-English
Other practices like restraint
Published prior to 2011
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7SECLUSION
Journals hand searched NIL
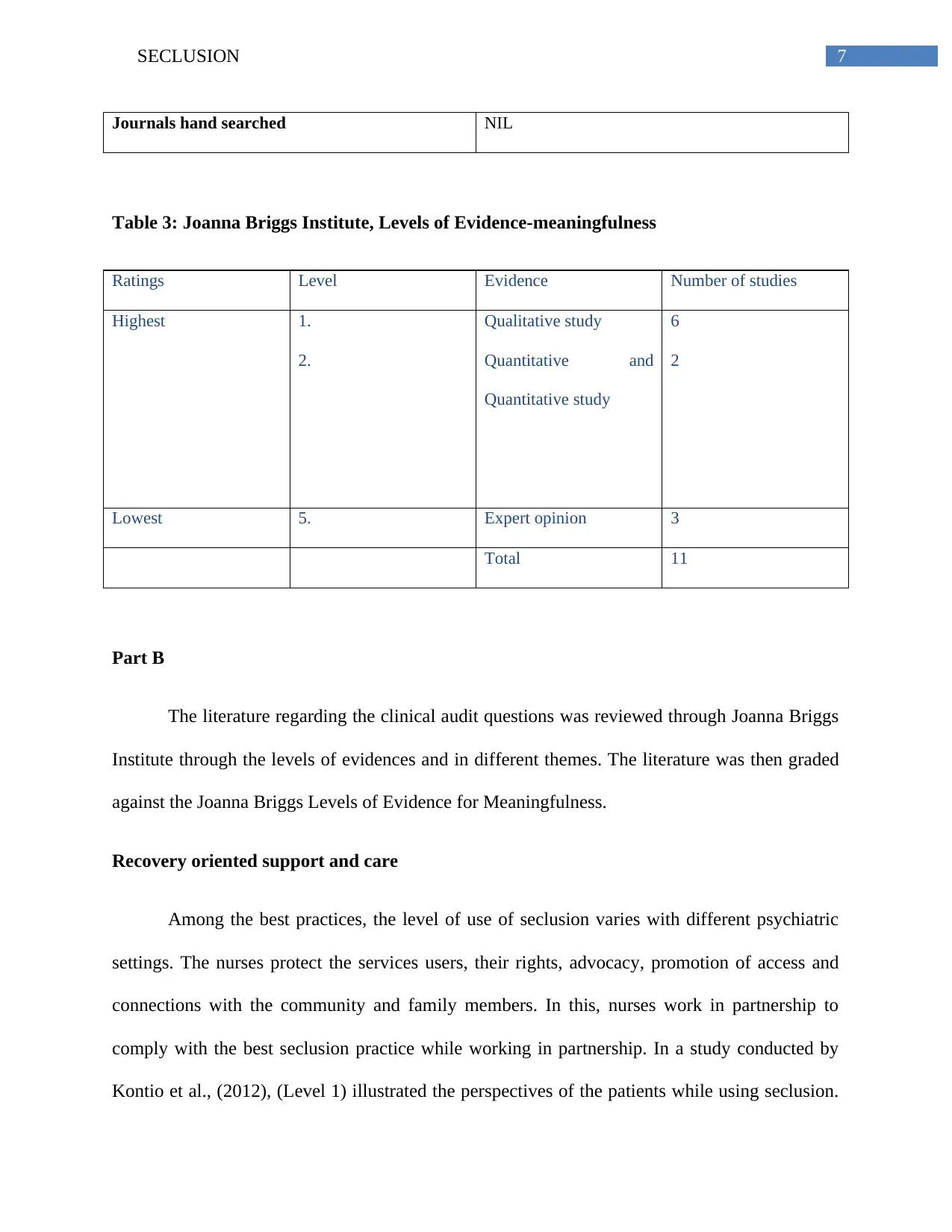
Table 3: Joanna Briggs Institute, Levels of Evidence-meaningfulness
Ratings Level Evidence Number of studies
Highest 1.
2.
Qualitative study
Quantitative and
Quantitative study
6
2
Lowest 5. Expert opinion 3
Total 11
Part B
The literature regarding the clinical audit questions was reviewed through Joanna Briggs
Institute through the levels of evidences and in different themes. The literature was then graded
against the Joanna Briggs Levels of Evidence for Meaningfulness.
Recovery oriented support and care
Among the best practices, the level of use of seclusion varies with different psychiatric
settings. The nurses protect the services users, their rights, advocacy, promotion of access and
connections with the community and family members. In this, nurses work in partnership to
comply with the best seclusion practice while working in partnership. In a study conducted by
Kontio et al., (2012), (Level 1) illustrated the perspectives of the patients while using seclusion.
Journals hand searched NIL
Table 3: Joanna Briggs Institute, Levels of Evidence-meaningfulness
Ratings Level Evidence Number of studies
Highest 1.
2.
Qualitative study
Quantitative and
Quantitative study
6
2
Lowest 5. Expert opinion 3
Total 11
Part B
The literature regarding the clinical audit questions was reviewed through Joanna Briggs
Institute through the levels of evidences and in different themes. The literature was then graded
against the Joanna Briggs Levels of Evidence for Meaningfulness.
Recovery oriented support and care
Among the best practices, the level of use of seclusion varies with different psychiatric
settings. The nurses protect the services users, their rights, advocacy, promotion of access and
connections with the community and family members. In this, nurses work in partnership to
comply with the best seclusion practice while working in partnership. In a study conducted by
Kontio et al., (2012), (Level 1) illustrated the perspectives of the patients while using seclusion.
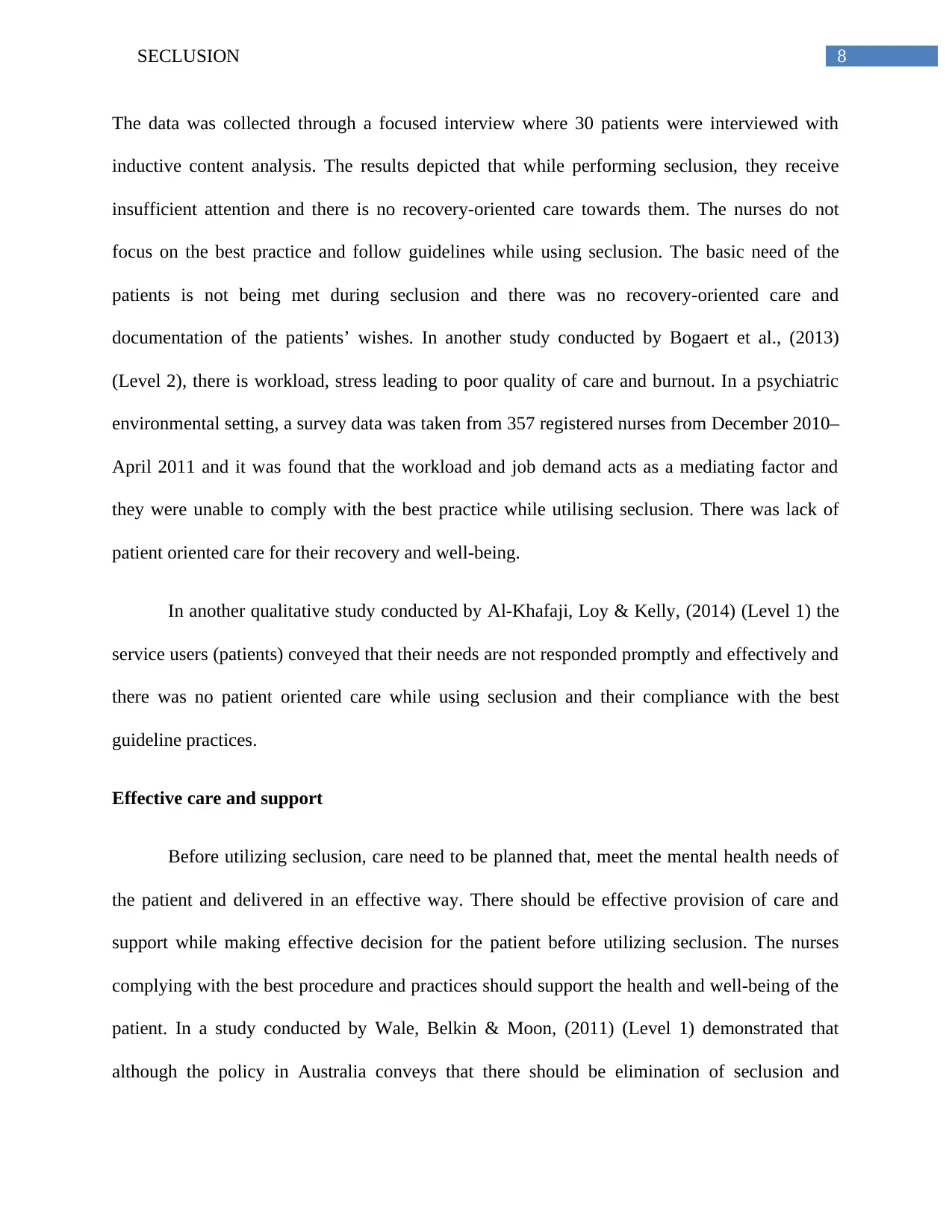
8SECLUSION
The data was collected through a focused interview where 30 patients were interviewed with
inductive content analysis. The results depicted that while performing seclusion, they receive
insufficient attention and there is no recovery-oriented care towards them. The nurses do not
focus on the best practice and follow guidelines while using seclusion. The basic need of the
patients is not being met during seclusion and there was no recovery-oriented care and
documentation of the patients’ wishes. In another study conducted by Bogaert et al., (2013)
(Level 2), there is workload, stress leading to poor quality of care and burnout. In a psychiatric
environmental setting, a survey data was taken from 357 registered nurses from December 2010–
April 2011 and it was found that the workload and job demand acts as a mediating factor and
they were unable to comply with the best practice while utilising seclusion. There was lack of
patient oriented care for their recovery and well-being.
In another qualitative study conducted by Al-Khafaji, Loy & Kelly, (2014) (Level 1) the
service users (patients) conveyed that their needs are not responded promptly and effectively and
there was no patient oriented care while using seclusion and their compliance with the best
guideline practices.
Effective care and support
Before utilizing seclusion, care need to be planned that, meet the mental health needs of
the patient and delivered in an effective way. There should be effective provision of care and
support while making effective decision for the patient before utilizing seclusion. The nurses
complying with the best procedure and practices should support the health and well-being of the
patient. In a study conducted by Wale, Belkin & Moon, (2011) (Level 1) demonstrated that
although the policy in Australia conveys that there should be elimination of seclusion and
The data was collected through a focused interview where 30 patients were interviewed with
inductive content analysis. The results depicted that while performing seclusion, they receive
insufficient attention and there is no recovery-oriented care towards them. The nurses do not
focus on the best practice and follow guidelines while using seclusion. The basic need of the
patients is not being met during seclusion and there was no recovery-oriented care and
documentation of the patients’ wishes. In another study conducted by Bogaert et al., (2013)
(Level 2), there is workload, stress leading to poor quality of care and burnout. In a psychiatric
environmental setting, a survey data was taken from 357 registered nurses from December 2010–
April 2011 and it was found that the workload and job demand acts as a mediating factor and
they were unable to comply with the best practice while utilising seclusion. There was lack of
patient oriented care for their recovery and well-being.
In another qualitative study conducted by Al-Khafaji, Loy & Kelly, (2014) (Level 1) the
service users (patients) conveyed that their needs are not responded promptly and effectively and
there was no patient oriented care while using seclusion and their compliance with the best
guideline practices.
Effective care and support
Before utilizing seclusion, care need to be planned that, meet the mental health needs of
the patient and delivered in an effective way. There should be effective provision of care and
support while making effective decision for the patient before utilizing seclusion. The nurses
complying with the best procedure and practices should support the health and well-being of the
patient. In a study conducted by Wale, Belkin & Moon, (2011) (Level 1) demonstrated that
although the policy in Australia conveys that there should be elimination of seclusion and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
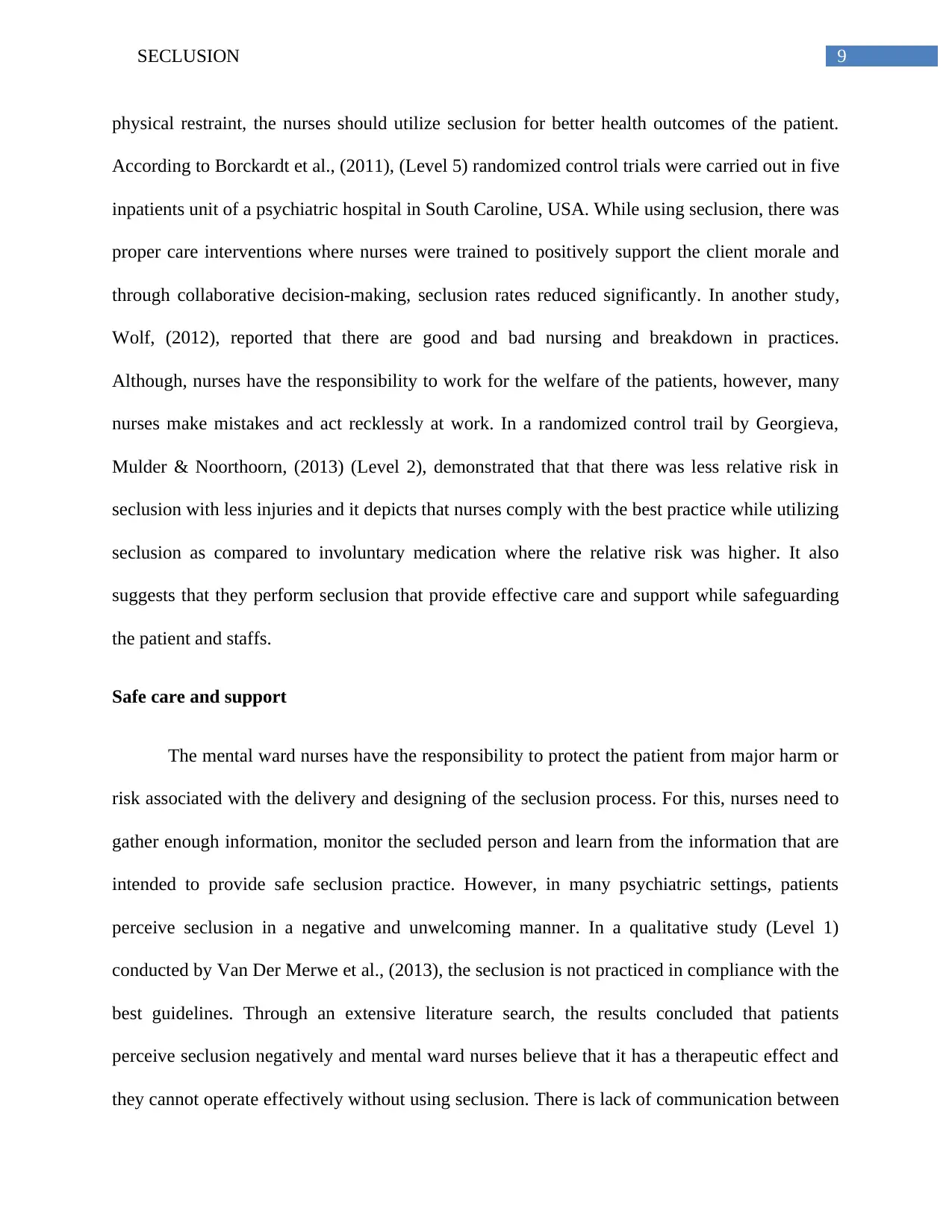
9SECLUSION
physical restraint, the nurses should utilize seclusion for better health outcomes of the patient.
According to Borckardt et al., (2011), (Level 5) randomized control trials were carried out in five
inpatients unit of a psychiatric hospital in South Caroline, USA. While using seclusion, there was
proper care interventions where nurses were trained to positively support the client morale and
through collaborative decision-making, seclusion rates reduced significantly. In another study,
Wolf, (2012), reported that there are good and bad nursing and breakdown in practices.
Although, nurses have the responsibility to work for the welfare of the patients, however, many
nurses make mistakes and act recklessly at work. In a randomized control trail by Georgieva,
Mulder & Noorthoorn, (2013) (Level 2), demonstrated that that there was less relative risk in
seclusion with less injuries and it depicts that nurses comply with the best practice while utilizing
seclusion as compared to involuntary medication where the relative risk was higher. It also
suggests that they perform seclusion that provide effective care and support while safeguarding
the patient and staffs.
Safe care and support
The mental ward nurses have the responsibility to protect the patient from major harm or
risk associated with the delivery and designing of the seclusion process. For this, nurses need to
gather enough information, monitor the secluded person and learn from the information that are
intended to provide safe seclusion practice. However, in many psychiatric settings, patients
perceive seclusion in a negative and unwelcoming manner. In a qualitative study (Level 1)
conducted by Van Der Merwe et al., (2013), the seclusion is not practiced in compliance with the
best guidelines. Through an extensive literature search, the results concluded that patients
perceive seclusion negatively and mental ward nurses believe that it has a therapeutic effect and
they cannot operate effectively without using seclusion. There is lack of communication between
physical restraint, the nurses should utilize seclusion for better health outcomes of the patient.
According to Borckardt et al., (2011), (Level 5) randomized control trials were carried out in five
inpatients unit of a psychiatric hospital in South Caroline, USA. While using seclusion, there was
proper care interventions where nurses were trained to positively support the client morale and
through collaborative decision-making, seclusion rates reduced significantly. In another study,
Wolf, (2012), reported that there are good and bad nursing and breakdown in practices.
Although, nurses have the responsibility to work for the welfare of the patients, however, many
nurses make mistakes and act recklessly at work. In a randomized control trail by Georgieva,
Mulder & Noorthoorn, (2013) (Level 2), demonstrated that that there was less relative risk in
seclusion with less injuries and it depicts that nurses comply with the best practice while utilizing
seclusion as compared to involuntary medication where the relative risk was higher. It also
suggests that they perform seclusion that provide effective care and support while safeguarding
the patient and staffs.
Safe care and support
The mental ward nurses have the responsibility to protect the patient from major harm or
risk associated with the delivery and designing of the seclusion process. For this, nurses need to
gather enough information, monitor the secluded person and learn from the information that are
intended to provide safe seclusion practice. However, in many psychiatric settings, patients
perceive seclusion in a negative and unwelcoming manner. In a qualitative study (Level 1)
conducted by Van Der Merwe et al., (2013), the seclusion is not practiced in compliance with the
best guidelines. Through an extensive literature search, the results concluded that patients
perceive seclusion negatively and mental ward nurses believe that it has a therapeutic effect and
they cannot operate effectively without using seclusion. There is lack of communication between
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10SECLUSION
the patient and staff before and after the seclusion application that affect the care process and
support. Staffs did not guide the seclusion process in an effective manner and failed to adopt a
safe mechanism for utilizing it. It is evident that patients’ experiences during seclusion are
negative and mental ward nurses believe that the units cannot function without operating it.
There is increased risk for the staffs and so seclusion is employed to ensure safety and protect the
patient from aggressive behaviour.
Leadership and management
The mental health services should have effective arrangements that are intended to
deliver best care while utilizing seclusion. There should also be systematic monitoring of the
seclusion process and provide opportunities for safety, quality care and reliability of the mental
health services. For this, there is requirement of effective leadership by the managers that are
intended to promote quality care and safety of the patient and ward staffs while utilizing
seclusion. In a quantitative study conducted by Smith et al., (2015), (Level 1) in Pennsylvania
state hospital system from 2001 to 2010 showed that there was decrease in the seclusion and
mechanical restraint rates. The managers and nurse leaders advocated effective leadership
qualities and transparency with better policy changes and enhanced workforce response and
development that led to the decline in seclusion and restraint rates.
In a study conducted by Azeem et al., (2011) (Level 1), stated that after the
implementation of the six core strategies in trauma informed care, the seclusion and restraint
rates decreased in hospitalized youths. In this qualitative study, leadership and advocacy of the
nurse managers helped to reduce the restraint and seclusion among the hospitalized youth based
on trauma informed care.
the patient and staff before and after the seclusion application that affect the care process and
support. Staffs did not guide the seclusion process in an effective manner and failed to adopt a
safe mechanism for utilizing it. It is evident that patients’ experiences during seclusion are
negative and mental ward nurses believe that the units cannot function without operating it.
There is increased risk for the staffs and so seclusion is employed to ensure safety and protect the
patient from aggressive behaviour.
Leadership and management
The mental health services should have effective arrangements that are intended to
deliver best care while utilizing seclusion. There should also be systematic monitoring of the
seclusion process and provide opportunities for safety, quality care and reliability of the mental
health services. For this, there is requirement of effective leadership by the managers that are
intended to promote quality care and safety of the patient and ward staffs while utilizing
seclusion. In a quantitative study conducted by Smith et al., (2015), (Level 1) in Pennsylvania
state hospital system from 2001 to 2010 showed that there was decrease in the seclusion and
mechanical restraint rates. The managers and nurse leaders advocated effective leadership
qualities and transparency with better policy changes and enhanced workforce response and
development that led to the decline in seclusion and restraint rates.
In a study conducted by Azeem et al., (2011) (Level 1), stated that after the
implementation of the six core strategies in trauma informed care, the seclusion and restraint
rates decreased in hospitalized youths. In this qualitative study, leadership and advocacy of the
nurse managers helped to reduce the restraint and seclusion among the hospitalized youth based
on trauma informed care.
11SECLUSION
Workforce
The mental health services should advocate caring plan, organize and manage the mental
health workforce that achieve the best care, recovery oriented and provide ample support to the
secluded person. The nurses should be recruited through arduous training on seclusion
application with required competencies for safe delivery and protection of the patient. The
mental health workforce should possess competencies that are intended to deliver the best quality
of care and safeguard the patient during seclusion. While utilizing seclusion, the mental health
ward staffs should deliver high quality service that provide recovery oriented and safe services
for the patients and the other staffs.
According to Masters, (2015) (Level 5), the seclusion and restraint are dangerous
coercive measures that have a negative psychological effect on the secluded person and is likely
to create an unprepared or insensitive environment. Nurse Managers should advocate leadership
that evaluate the data on seclusion and restraint that are carried out in inpatient mental health
settings. Staff training is also important where the mental health workforce should be trained to
use seclusion in a recovery oriented and safe manner. There should be collaborative training of
the staffs so that they negotiate with the patients to resolve the disagreements. This increases the
patient autonomy and strengthening their trust in staff resulting effective decision-making.
Clinical bottom line
In qualitative and quantitative studies, recommend that the patients received seclusion in
an ineffective manner where their needs were not addressed and no recovery-oriented
care. Due to workload and demanding nature of job of the mental ward nurses, they fail
to comply with the best practice while utilizing seclusion. As a result, there was lack of
Workforce
The mental health services should advocate caring plan, organize and manage the mental
health workforce that achieve the best care, recovery oriented and provide ample support to the
secluded person. The nurses should be recruited through arduous training on seclusion
application with required competencies for safe delivery and protection of the patient. The
mental health workforce should possess competencies that are intended to deliver the best quality
of care and safeguard the patient during seclusion. While utilizing seclusion, the mental health
ward staffs should deliver high quality service that provide recovery oriented and safe services
for the patients and the other staffs.
According to Masters, (2015) (Level 5), the seclusion and restraint are dangerous
coercive measures that have a negative psychological effect on the secluded person and is likely
to create an unprepared or insensitive environment. Nurse Managers should advocate leadership
that evaluate the data on seclusion and restraint that are carried out in inpatient mental health
settings. Staff training is also important where the mental health workforce should be trained to
use seclusion in a recovery oriented and safe manner. There should be collaborative training of
the staffs so that they negotiate with the patients to resolve the disagreements. This increases the
patient autonomy and strengthening their trust in staff resulting effective decision-making.
Clinical bottom line
In qualitative and quantitative studies, recommend that the patients received seclusion in
an ineffective manner where their needs were not addressed and no recovery-oriented
care. Due to workload and demanding nature of job of the mental ward nurses, they fail
to comply with the best practice while utilizing seclusion. As a result, there was lack of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





