Report: Clinical Assessment of TIA Leading to Stroke in Healthcare
VerifiedAdded on 2020/03/07
|12
|2789
|75
Report
AI Summary
This report presents a clinical assessment of a patient, Mrs. Amari, who experienced a transient ischemic attack (TIA), highlighting the critical steps in diagnosis, management, and prevention of stroke. The report details the patient's history, including hypertension, hypercholesterolemia, and smoking. The primary assessment involved vital signs and neurological evaluations, leading to a TIA diagnosis. Investigations, including ABCD2 scoring and imaging, were conducted to assess stroke risk. The report emphasizes the importance of lifestyle modifications and medical interventions, such as antihypertensive medications, statins, and smoking cessation, to manage risk factors. It discusses the prognosis of TIA and preventive measures to reduce the risk of future stroke occurrences, underscoring the need for early recognition and intervention. The report concludes by referencing key studies and guidelines related to TIA and stroke management.

Running head: CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Clinical assessment of TIA leading to stroke
Name of the Student
Name of the University
Author Note
Clinical assessment of TIA leading to stroke
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Executive Summary:
Stroke happens to be one of the common causes of disability and can lead to death if not
treated on time. Recognising Transient ischemic attack (TIA) in the early stage can prevent
subsequent stroke. The specific treatment for preventing stroke is based on the underlying
cause of TIA with cerebrovascular localization followed by other clinical problems.
Modifying the risk factors associated with stroke can be done by therapeutic approaches.
Therefore by understanding the clinical symptoms of TIA can help in early detection of
stroke and likewise preventive measures can be implemented. The proper maintenance of the
risk factors such as controlling blood pressure with controlled cholesterol level, inhibiting
smoking tendency and controlled diabetes can reduce the prevalence of stroke followed by
recurrent TIA. In this report the management of TIA in primary care through proper
assessment, diagnosis followed by preventive measures to reduce the occurrence of stroke
has been discussed with respect to a patient diagnosed with TIA.
Executive Summary:
Stroke happens to be one of the common causes of disability and can lead to death if not
treated on time. Recognising Transient ischemic attack (TIA) in the early stage can prevent
subsequent stroke. The specific treatment for preventing stroke is based on the underlying
cause of TIA with cerebrovascular localization followed by other clinical problems.
Modifying the risk factors associated with stroke can be done by therapeutic approaches.
Therefore by understanding the clinical symptoms of TIA can help in early detection of
stroke and likewise preventive measures can be implemented. The proper maintenance of the
risk factors such as controlling blood pressure with controlled cholesterol level, inhibiting
smoking tendency and controlled diabetes can reduce the prevalence of stroke followed by
recurrent TIA. In this report the management of TIA in primary care through proper
assessment, diagnosis followed by preventive measures to reduce the occurrence of stroke
has been discussed with respect to a patient diagnosed with TIA.
2CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Table of Contents
1. Patient situation:.....................................................................................................................3
1.1. Previous history:..............................................................................................................3
2. Primary assessment:...............................................................................................................3
2.1. Information gathered:......................................................................................................3
2.2. Current situation:.............................................................................................................4
2.3. Epidemiology with aetiology:.........................................................................................4
2.4. Undertaking the diagnosis:..............................................................................................5
2.5. TIA symptoms:................................................................................................................5
3. Investigations:........................................................................................................................6
3.1. Management of the situation:..........................................................................................7
3.2. Prognosis:........................................................................................................................8
3.3. Preventing future occurrence:.........................................................................................8
4. References:.............................................................................................................................9
Table of Contents
1. Patient situation:.....................................................................................................................3
1.1. Previous history:..............................................................................................................3
2. Primary assessment:...............................................................................................................3
2.1. Information gathered:......................................................................................................3
2.2. Current situation:.............................................................................................................4
2.3. Epidemiology with aetiology:.........................................................................................4
2.4. Undertaking the diagnosis:..............................................................................................5
2.5. TIA symptoms:................................................................................................................5
3. Investigations:........................................................................................................................6
3.1. Management of the situation:..........................................................................................7
3.2. Prognosis:........................................................................................................................8
3.3. Preventing future occurrence:.........................................................................................8
4. References:.............................................................................................................................9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
1. Patient situation:
A 59 year old widow named Mrs. Amari was brought to the emergency department by
her son, Niko. He noticed a sudden slurring in her mother’s speech with drooped face on one
side. She reported her son about the numbness of right side of her face including her right
arm. Niko brought her to the hospital after having a fear of stroke.
1.1. Previous history:
Her mother had a history of hypertension with hypercholesterolemia with 25 years of
tobacco usage which she had stopped ten years ago. She showed a positive history of family
line with heart disease. She does not follow a regular exercise regimen with occasional walk
in neighbourhood.
2. Primary assessment:
The nursing staff in the emergency department assessed her and found a slight
diversion of mouth in the right side with speech slightly slurred. Further assessment showed
no such weakness with steady gait and could swallow without any difficulty. She followed
all the commands and looked oriented. The pupal examination showed round, equal and
normally reacting to light (4mm to 2mm). No such nystagmus was noted. She did not
complain of any kind of headache followed by nausea, vomiting, chest pain, diaphoresis or
visual complaints.
2.1. Information gathered:
On examining her vital signs her temperature was 36.7ºC with an increased blood
pressure of 148/97mmHg, pulse recorded 81, respiratory rate was 14 and the oxygen
saturation was 94%. Numbering through Glasgow Coma Scale showed 15 with 6.6mmol/L
blood glucose level. Based on the history and examination result she was diagnosed by a
1. Patient situation:
A 59 year old widow named Mrs. Amari was brought to the emergency department by
her son, Niko. He noticed a sudden slurring in her mother’s speech with drooped face on one
side. She reported her son about the numbness of right side of her face including her right
arm. Niko brought her to the hospital after having a fear of stroke.
1.1. Previous history:
Her mother had a history of hypertension with hypercholesterolemia with 25 years of
tobacco usage which she had stopped ten years ago. She showed a positive history of family
line with heart disease. She does not follow a regular exercise regimen with occasional walk
in neighbourhood.
2. Primary assessment:
The nursing staff in the emergency department assessed her and found a slight
diversion of mouth in the right side with speech slightly slurred. Further assessment showed
no such weakness with steady gait and could swallow without any difficulty. She followed
all the commands and looked oriented. The pupal examination showed round, equal and
normally reacting to light (4mm to 2mm). No such nystagmus was noted. She did not
complain of any kind of headache followed by nausea, vomiting, chest pain, diaphoresis or
visual complaints.
2.1. Information gathered:
On examining her vital signs her temperature was 36.7ºC with an increased blood
pressure of 148/97mmHg, pulse recorded 81, respiratory rate was 14 and the oxygen
saturation was 94%. Numbering through Glasgow Coma Scale showed 15 with 6.6mmol/L
blood glucose level. Based on the history and examination result she was diagnosed by a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
transient ischemic attack (TIA) also termed as mini attack. A scan of the head computed
tomography (CT) showed no such change in intracranial structure with MRI (Magnetic
Resonance Imagery) reports normal. The neurologist referred her to the stroke unit for further
observation followed by treatment.
2.2. Current situation:
The visit to Mrs. Amari in the next day showed some changes in the clinical features.
Her speech sounded slurry with drooped mouth in the right side. Examining her vital signs
should an elevated change in blood pressure to 175/105mmHg with decrease in the SpO2 by
92%. The examination history showed consistency with the TIA. The change in the vital
signs with increased ABCD scores (The Airway, Breathing, Circulation, Disability)
constituted a risk of stroke in the upcoming 48 hours (Daniels et al. 2012). Hence, in this
clinical report based on the case study of Mrs. Amari the methods relating the assessment,
diagnosis and management of TIA followed by stoke signs will be evaluated with required
interventions.
2.3. Epidemiology with aetiology:
Transient ischemic attack (TIA) is a common clinical disorder with incidental rate of
0.5 out of 1000 people. It usually affects the communication, motor functioning and
sensibility. TIA is often followed by strokes which go unrecognised in patients (Hickey
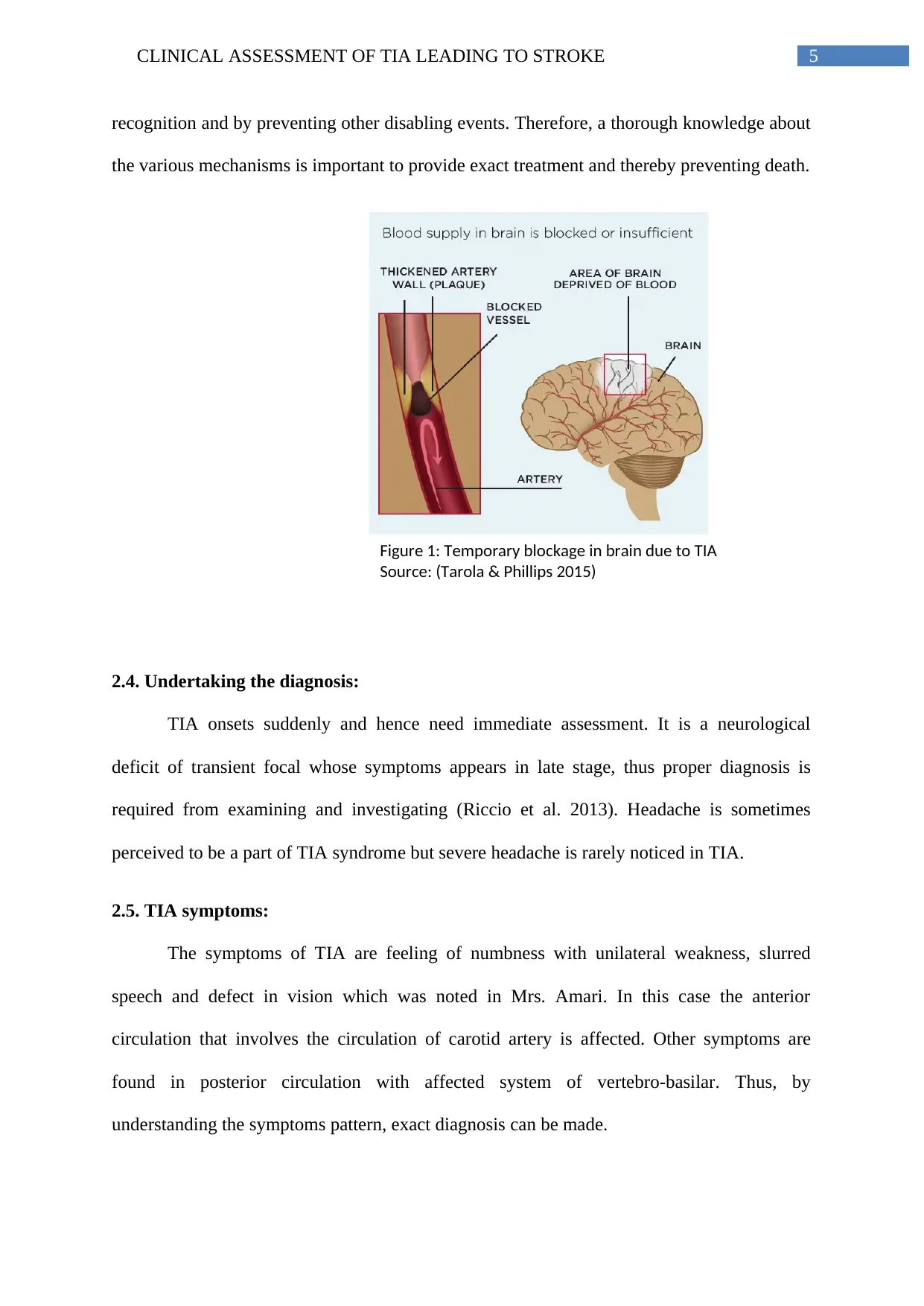
2012). This symptom occurs when the blood vessel inside the brain is clogged (Figure 1).
This clinical presentation occurs due to death of the brain cells (Rosenberg 2012). TIA differs
from stroke in duration of the symptom, in which TIA does not persist more than one hour.
Obstructed blood flow termed ischemia causes permanent damage in brain causing (CVA)
cerebrovascular accident (Sanderson et al. 2013). In TIA brain shows temporary damage.
CVA with ruptured artery with bleeding within brain is called haemorrhage. TIA and stroke
are distinguished depending on the cause. Hence, the patients with TIA can be cured by early
transient ischemic attack (TIA) also termed as mini attack. A scan of the head computed
tomography (CT) showed no such change in intracranial structure with MRI (Magnetic
Resonance Imagery) reports normal. The neurologist referred her to the stroke unit for further
observation followed by treatment.
2.2. Current situation:
The visit to Mrs. Amari in the next day showed some changes in the clinical features.
Her speech sounded slurry with drooped mouth in the right side. Examining her vital signs
should an elevated change in blood pressure to 175/105mmHg with decrease in the SpO2 by
92%. The examination history showed consistency with the TIA. The change in the vital
signs with increased ABCD scores (The Airway, Breathing, Circulation, Disability)
constituted a risk of stroke in the upcoming 48 hours (Daniels et al. 2012). Hence, in this
clinical report based on the case study of Mrs. Amari the methods relating the assessment,
diagnosis and management of TIA followed by stoke signs will be evaluated with required
interventions.
2.3. Epidemiology with aetiology:
Transient ischemic attack (TIA) is a common clinical disorder with incidental rate of
0.5 out of 1000 people. It usually affects the communication, motor functioning and
sensibility. TIA is often followed by strokes which go unrecognised in patients (Hickey
2012). This symptom occurs when the blood vessel inside the brain is clogged (Figure 1).
This clinical presentation occurs due to death of the brain cells (Rosenberg 2012). TIA differs
from stroke in duration of the symptom, in which TIA does not persist more than one hour.
Obstructed blood flow termed ischemia causes permanent damage in brain causing (CVA)
cerebrovascular accident (Sanderson et al. 2013). In TIA brain shows temporary damage.
CVA with ruptured artery with bleeding within brain is called haemorrhage. TIA and stroke
are distinguished depending on the cause. Hence, the patients with TIA can be cured by early
5CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Figure 1: Temporary blockage in brain due to TIA
Source: (Tarola & Phillips 2015)
recognition and by preventing other disabling events. Therefore, a thorough knowledge about
the various mechanisms is important to provide exact treatment and thereby preventing death.
2.4. Undertaking the diagnosis:
TIA onsets suddenly and hence need immediate assessment. It is a neurological
deficit of transient focal whose symptoms appears in late stage, thus proper diagnosis is
required from examining and investigating (Riccio et al. 2013). Headache is sometimes
perceived to be a part of TIA syndrome but severe headache is rarely noticed in TIA.
2.5. TIA symptoms:
The symptoms of TIA are feeling of numbness with unilateral weakness, slurred
speech and defect in vision which was noted in Mrs. Amari. In this case the anterior
circulation that involves the circulation of carotid artery is affected. Other symptoms are
found in posterior circulation with affected system of vertebro-basilar. Thus, by
understanding the symptoms pattern, exact diagnosis can be made.
Figure 1: Temporary blockage in brain due to TIA
Source: (Tarola & Phillips 2015)
recognition and by preventing other disabling events. Therefore, a thorough knowledge about
the various mechanisms is important to provide exact treatment and thereby preventing death.
2.4. Undertaking the diagnosis:
TIA onsets suddenly and hence need immediate assessment. It is a neurological
deficit of transient focal whose symptoms appears in late stage, thus proper diagnosis is
required from examining and investigating (Riccio et al. 2013). Headache is sometimes
perceived to be a part of TIA syndrome but severe headache is rarely noticed in TIA.
2.5. TIA symptoms:
The symptoms of TIA are feeling of numbness with unilateral weakness, slurred
speech and defect in vision which was noted in Mrs. Amari. In this case the anterior
circulation that involves the circulation of carotid artery is affected. Other symptoms are
found in posterior circulation with affected system of vertebro-basilar. Thus, by
understanding the symptoms pattern, exact diagnosis can be made.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
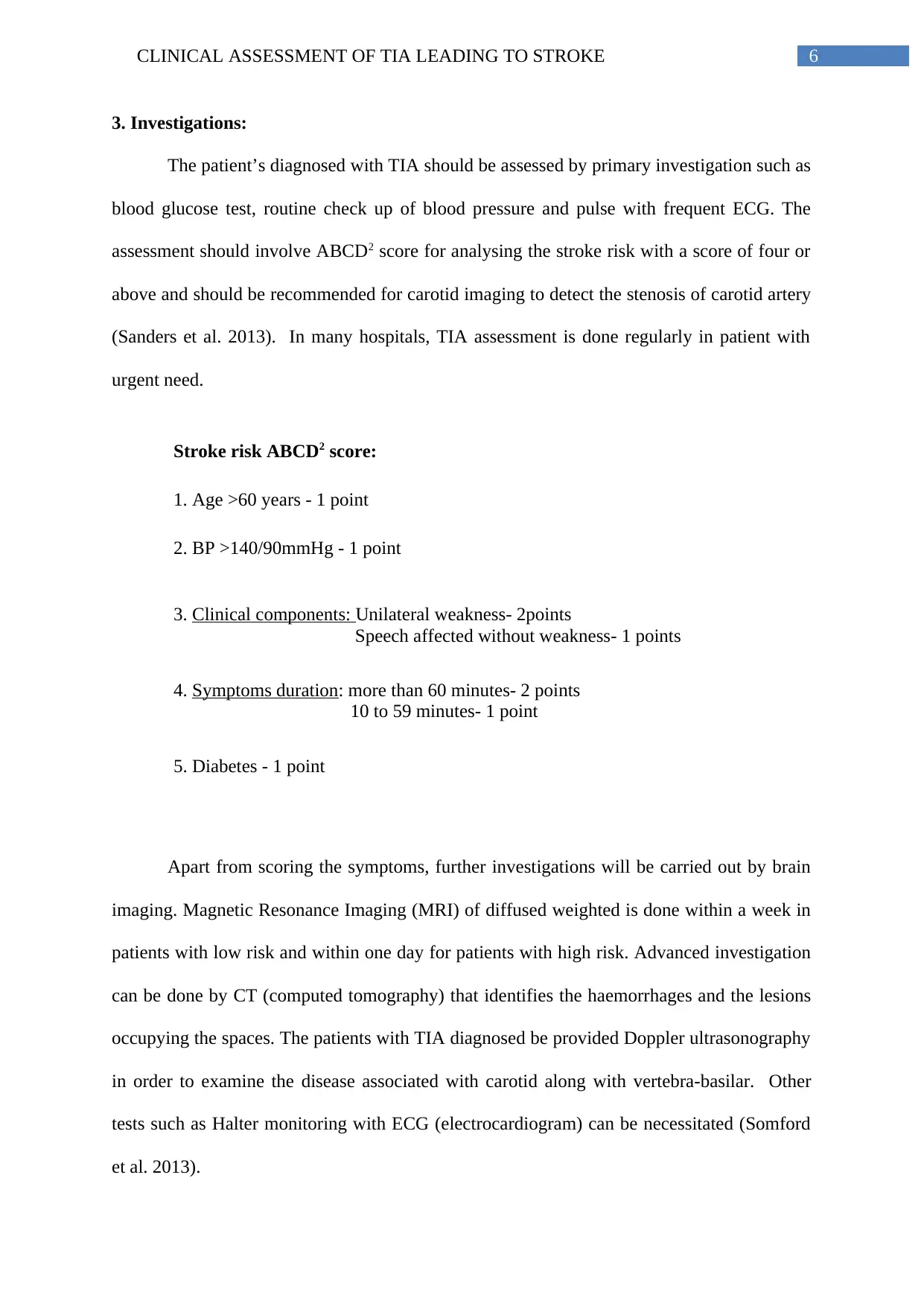
3. Investigations:
The patient’s diagnosed with TIA should be assessed by primary investigation such as
blood glucose test, routine check up of blood pressure and pulse with frequent ECG. The
assessment should involve ABCD2 score for analysing the stroke risk with a score of four or
above and should be recommended for carotid imaging to detect the stenosis of carotid artery
(Sanders et al. 2013). In many hospitals, TIA assessment is done regularly in patient with
urgent need.
Stroke risk ABCD2 score:
1. Age >60 years - 1 point
2. BP >140/90mmHg - 1 point
3. Clinical components: Unilateral weakness- 2points
Speech affected without weakness- 1 points
4. Symptoms duration: more than 60 minutes- 2 points
10 to 59 minutes- 1 point
5. Diabetes - 1 point
Apart from scoring the symptoms, further investigations will be carried out by brain
imaging. Magnetic Resonance Imaging (MRI) of diffused weighted is done within a week in
patients with low risk and within one day for patients with high risk. Advanced investigation
can be done by CT (computed tomography) that identifies the haemorrhages and the lesions
occupying the spaces. The patients with TIA diagnosed be provided Doppler ultrasonography
in order to examine the disease associated with carotid along with vertebra-basilar. Other
tests such as Halter monitoring with ECG (electrocardiogram) can be necessitated (Somford
et al. 2013).
3. Investigations:
The patient’s diagnosed with TIA should be assessed by primary investigation such as
blood glucose test, routine check up of blood pressure and pulse with frequent ECG. The
assessment should involve ABCD2 score for analysing the stroke risk with a score of four or
above and should be recommended for carotid imaging to detect the stenosis of carotid artery
(Sanders et al. 2013). In many hospitals, TIA assessment is done regularly in patient with
urgent need.
Stroke risk ABCD2 score:
1. Age >60 years - 1 point
2. BP >140/90mmHg - 1 point
3. Clinical components: Unilateral weakness- 2points
Speech affected without weakness- 1 points
4. Symptoms duration: more than 60 minutes- 2 points
10 to 59 minutes- 1 point
5. Diabetes - 1 point
Apart from scoring the symptoms, further investigations will be carried out by brain
imaging. Magnetic Resonance Imaging (MRI) of diffused weighted is done within a week in
patients with low risk and within one day for patients with high risk. Advanced investigation
can be done by CT (computed tomography) that identifies the haemorrhages and the lesions
occupying the spaces. The patients with TIA diagnosed be provided Doppler ultrasonography
in order to examine the disease associated with carotid along with vertebra-basilar. Other
tests such as Halter monitoring with ECG (electrocardiogram) can be necessitated (Somford
et al. 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
3.1. Management of the situation:
The TIA management with diagnosis is same in both cases of TIA and stroke.
Although, stratified risks in TIA allows the treatment specialist to decide where and when to
make the referral. Therefore, it is important to evaluate the management of the aggressive risk
components. The advice regarding the lifestyle should point out as much as possible risk
factors. The specific interventions in reducing the rate of stroke have been discussed below
(Ihle‐Hansen et al. 2014)
Hypertension treatment: Treating hypertension by reducing the BP with
antihypertensive can prevent the recurrent stroke along with other vascular problems after
TIA. Combined use of diuretics with ACE inhibitors are found to reduce the BP by
approximately 10/5mmHg (Bunker 2014). Hypertension was recorded in the history of Mrs.
Amari which can be controlled by this treatment.
Hypercholesterolaemia: The drugs related to lowering of cholesterol have been found
to be effective in primary as well as secondary prevention (Rabar et al. 2014). Diets should be
modified with statin use if the total count is more than 3.5mmol/L. Mrs. Amari showed
hypercholesterolemia which can be controlled by this intervention.
Smoking: Smoking is one of the leading causes for 50% stroke rise. Thus, patients
with TIA and strokes should be recommended to quit smoking (Peters, Huxley & Woodward
2013). Mrs. Amati had a smoking history of 25 years but had quit few years back.
Anticoagulants: About 15% of TIA and ischemic strokes are intervened by
anticoagulants based warfarin (Easton et al. 2012). Dabigatran is a new anticoagulant which
has newly emerged but due its cost and irreversible nature, it is detrimental to life.
3.1. Management of the situation:
The TIA management with diagnosis is same in both cases of TIA and stroke.
Although, stratified risks in TIA allows the treatment specialist to decide where and when to
make the referral. Therefore, it is important to evaluate the management of the aggressive risk
components. The advice regarding the lifestyle should point out as much as possible risk
factors. The specific interventions in reducing the rate of stroke have been discussed below
(Ihle‐Hansen et al. 2014)
Hypertension treatment: Treating hypertension by reducing the BP with
antihypertensive can prevent the recurrent stroke along with other vascular problems after
TIA. Combined use of diuretics with ACE inhibitors are found to reduce the BP by
approximately 10/5mmHg (Bunker 2014). Hypertension was recorded in the history of Mrs.
Amari which can be controlled by this treatment.
Hypercholesterolaemia: The drugs related to lowering of cholesterol have been found
to be effective in primary as well as secondary prevention (Rabar et al. 2014). Diets should be
modified with statin use if the total count is more than 3.5mmol/L. Mrs. Amari showed
hypercholesterolemia which can be controlled by this intervention.
Smoking: Smoking is one of the leading causes for 50% stroke rise. Thus, patients
with TIA and strokes should be recommended to quit smoking (Peters, Huxley & Woodward
2013). Mrs. Amati had a smoking history of 25 years but had quit few years back.
Anticoagulants: About 15% of TIA and ischemic strokes are intervened by
anticoagulants based warfarin (Easton et al. 2012). Dabigatran is a new anticoagulant which
has newly emerged but due its cost and irreversible nature, it is detrimental to life.
8CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Diabetes: The diabetic patients with TIA or stroke need strict control of glucose level
in order to reduce the vascular related complications (Schnell, Erbach & Hummel 2012).
Antiplatelets such as aspirin are used in patients with past record of TIA or any kind
of stroke to reduce the vascular risks by 13% (Geeganage et al. 2012). But aspirin should not
be administered without doing brain imaging.
3.2. Prognosis:
The prognosis is linked with timely diagnosis of TIA followed by stroke referring to
an immediate treatment with secondary prevention. The TIA prognosis is concerned with
stroke risk followed by vascular events. Statistical studies have shown that 70% patients
couldn’t recognise TIA which delayed in getting medical help (Spurgeon et al. 2012).
Therefore, the people should be educated for estimating the risk with proper planning
programme and regular check up by specialist.
3.3. Preventing future occurrence:
Recurrent occurrence can be controlled by adjusting the diet with modified lifestyle
such as smoking, physiological stress with hypertension and elevated cholesterol level with
medical interventions. Modification in these risk factors can lower the risk of future stroke
recurrence in patients diagnosed with TIA
Diabetes: The diabetic patients with TIA or stroke need strict control of glucose level
in order to reduce the vascular related complications (Schnell, Erbach & Hummel 2012).
Antiplatelets such as aspirin are used in patients with past record of TIA or any kind
of stroke to reduce the vascular risks by 13% (Geeganage et al. 2012). But aspirin should not
be administered without doing brain imaging.
3.2. Prognosis:
The prognosis is linked with timely diagnosis of TIA followed by stroke referring to
an immediate treatment with secondary prevention. The TIA prognosis is concerned with
stroke risk followed by vascular events. Statistical studies have shown that 70% patients
couldn’t recognise TIA which delayed in getting medical help (Spurgeon et al. 2012).
Therefore, the people should be educated for estimating the risk with proper planning
programme and regular check up by specialist.
3.3. Preventing future occurrence:
Recurrent occurrence can be controlled by adjusting the diet with modified lifestyle
such as smoking, physiological stress with hypertension and elevated cholesterol level with
medical interventions. Modification in these risk factors can lower the risk of future stroke
recurrence in patients diagnosed with TIA
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
4. References:
Bunker, J 2014, ‘Hypertension: diagnosis, assessment and management’, Nursing
Standard, vol. 28, no. 42, pp.50-59.
Daniels, EC, Powe, BD, Metoyer, MT, McCray, MG, Baltrus, P & Rust, GS 2012,
‘Increasing knowledge of cardiovascular risk factors among African Americans by use of
community health workers: the ABCD community intervention pilot project’, Journal of the
National Medical Association, vol. 104, p.179.
Easton, JD, Lopes, RD, Bahit, MC, Wojdyla, DM, Granger, CB, Wallentin, L, Alings, M,
Goto, S, Lewis, BS, Rosenqvist, M & Hanna, M 2012, ‘Apixaban compared with warfarin in
patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup
analysis of the ARISTOTLE trial’, The Lancet Neurology, vol. 11, no. 6, pp.503-511.
Geeganage, CM, Diener, HC, Algra, A, Chen, C, Topol, EJ, Dengler, R, Markus, HS, Bath,
MW, Bath, PM & Acute Antiplatelet Stroke Trialists Collaboration 2012, ‘Dual or mono
antiplatelet therapy for patients with acute ischemic stroke or transient ischemic
attack’, Stroke, vol. 43, no. 4, pp.1058-1066.
Hickey, K 2012, ‘Anticoagulation management in clinical practice: preventing stroke in
patients with atrial fibrillation’, Heart & Lung: The Journal of Acute and Critical Care,
vol. 41, no. 2, pp.146-156.
Ihle‐Hansen, H, Thommessen, B, Fagerland, MW, Øksengård, AR, Wyller, TB, Engedal, K
& Fure, B 2014, ‘Multifactorial vascular risk factor intervention to prevent cognitive
impairment after stroke and TIA: a 12‐month randomized controlled trial’, International
Journal of Stroke, vol. 9, no. 7, pp.932-938.
4. References:
Bunker, J 2014, ‘Hypertension: diagnosis, assessment and management’, Nursing
Standard, vol. 28, no. 42, pp.50-59.
Daniels, EC, Powe, BD, Metoyer, MT, McCray, MG, Baltrus, P & Rust, GS 2012,
‘Increasing knowledge of cardiovascular risk factors among African Americans by use of
community health workers: the ABCD community intervention pilot project’, Journal of the
National Medical Association, vol. 104, p.179.
Easton, JD, Lopes, RD, Bahit, MC, Wojdyla, DM, Granger, CB, Wallentin, L, Alings, M,
Goto, S, Lewis, BS, Rosenqvist, M & Hanna, M 2012, ‘Apixaban compared with warfarin in
patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup
analysis of the ARISTOTLE trial’, The Lancet Neurology, vol. 11, no. 6, pp.503-511.
Geeganage, CM, Diener, HC, Algra, A, Chen, C, Topol, EJ, Dengler, R, Markus, HS, Bath,
MW, Bath, PM & Acute Antiplatelet Stroke Trialists Collaboration 2012, ‘Dual or mono
antiplatelet therapy for patients with acute ischemic stroke or transient ischemic
attack’, Stroke, vol. 43, no. 4, pp.1058-1066.
Hickey, K 2012, ‘Anticoagulation management in clinical practice: preventing stroke in
patients with atrial fibrillation’, Heart & Lung: The Journal of Acute and Critical Care,
vol. 41, no. 2, pp.146-156.
Ihle‐Hansen, H, Thommessen, B, Fagerland, MW, Øksengård, AR, Wyller, TB, Engedal, K
& Fure, B 2014, ‘Multifactorial vascular risk factor intervention to prevent cognitive
impairment after stroke and TIA: a 12‐month randomized controlled trial’, International
Journal of Stroke, vol. 9, no. 7, pp.932-938.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
Peters, SA, Huxley, RR & Woodward, M 2013, ‘Smoking as a risk factor for stroke in
women compared with men,’ Stroke, vol. 44, no. 10, pp.2821-2828.
Rabar, S, Harker, M, O'flynn, N & Wierzbicki, AS 2014, ‘Lipid modification and
cardiovascular risk assessment for the primary and secondary prevention of cardiovascular
disease: summary of updated NICE guidance’, BMJ: British Medical Journal (Online), 349.
Riccio, PM, Klein, FR, Cassará, FP, Giacomelli, FM, Toledo, MEG, Racosta, JM, Delfitto,
M, Roberts, ES, Bahit, MC & Sposato, LA, 2013, ‘Newly diagnosed atrial fibrillation linked
to wake-up stroke and TIA Hypothetical implications’, Neurology, vol. 80, no. 20, pp.1834-
1840.
Rosenberg, GA 2012, ‘Neurological diseases in relation to the blood–brain barrier’, Journal
of Cerebral Blood Flow & Metabolism’, vol. 32, no. 7, pp.1139-1151.
Sanders, LM, Srikanth, VK, Blacker, DJ, Jolley, DJ, Cooper, KA & Phan, TG ‘2012.
Performance of the ABCD2 score for stroke risk post TIA Meta-analysis and probability
modeling’, Neurology, vol. 79, no. 10, pp.971-980.
Sanderson, TH, Reynolds, CA, Kumar, R, Przyklenk, K & Hüttemann, M 2013, ‘Molecular
mechanisms of ischemia–reperfusion injury in brain: pivotal role of the mitochondrial
membrane potential in reactive oxygen species generation’, Molecular neurobiology, vol. 47,
no. 1, pp.9-23.
Schnell, O, Erbach, M & Hummel, M, 2012, ‘Primary and secondary prevention of
cardiovascular disease in diabetes with aspirin’, Diabetes and Vascular Disease
Research, vol. 9, no. 4, pp.245-255.
Somford, DM, Hoeks, CM, Hulsbergen-van de Kaa, CA, Hambrock, T, Fütterer, JJ, Witjes,
JA, Bangma, CH, Vergunst, H, Smits, GA, Oddens, JR & van Oort, IM 2013, ‘Evaluation of
Peters, SA, Huxley, RR & Woodward, M 2013, ‘Smoking as a risk factor for stroke in
women compared with men,’ Stroke, vol. 44, no. 10, pp.2821-2828.
Rabar, S, Harker, M, O'flynn, N & Wierzbicki, AS 2014, ‘Lipid modification and
cardiovascular risk assessment for the primary and secondary prevention of cardiovascular
disease: summary of updated NICE guidance’, BMJ: British Medical Journal (Online), 349.
Riccio, PM, Klein, FR, Cassará, FP, Giacomelli, FM, Toledo, MEG, Racosta, JM, Delfitto,
M, Roberts, ES, Bahit, MC & Sposato, LA, 2013, ‘Newly diagnosed atrial fibrillation linked
to wake-up stroke and TIA Hypothetical implications’, Neurology, vol. 80, no. 20, pp.1834-
1840.
Rosenberg, GA 2012, ‘Neurological diseases in relation to the blood–brain barrier’, Journal
of Cerebral Blood Flow & Metabolism’, vol. 32, no. 7, pp.1139-1151.
Sanders, LM, Srikanth, VK, Blacker, DJ, Jolley, DJ, Cooper, KA & Phan, TG ‘2012.
Performance of the ABCD2 score for stroke risk post TIA Meta-analysis and probability
modeling’, Neurology, vol. 79, no. 10, pp.971-980.
Sanderson, TH, Reynolds, CA, Kumar, R, Przyklenk, K & Hüttemann, M 2013, ‘Molecular
mechanisms of ischemia–reperfusion injury in brain: pivotal role of the mitochondrial
membrane potential in reactive oxygen species generation’, Molecular neurobiology, vol. 47,
no. 1, pp.9-23.
Schnell, O, Erbach, M & Hummel, M, 2012, ‘Primary and secondary prevention of
cardiovascular disease in diabetes with aspirin’, Diabetes and Vascular Disease
Research, vol. 9, no. 4, pp.245-255.
Somford, DM, Hoeks, CM, Hulsbergen-van de Kaa, CA, Hambrock, T, Fütterer, JJ, Witjes,
JA, Bangma, CH, Vergunst, H, Smits, GA, Oddens, JR & van Oort, IM 2013, ‘Evaluation of
11CLINICAL ASSESSMENT OF TIA LEADING TO STROKE
diffusion-weighted MR imaging at inclusion in an active surveillance protocol for low-risk
prostate cancer’, Investigative radiology, vol. 48, no. 3, pp.152-157.
Spurgeon, L, Humphreys, G, James, G & Sackley, C, 2012, ‘A Q-methodology study of
patients’ subjective experiences of TIA’, Stroke research and treatment, 2012.
Tarola, G & Phillips, RB 2015, ‘Chiropractic response to a spontaneous vertebral artery
dissection’, Journal of chiropractic medicine, vol. 14, no. 3, pp.183-190.
diffusion-weighted MR imaging at inclusion in an active surveillance protocol for low-risk
prostate cancer’, Investigative radiology, vol. 48, no. 3, pp.152-157.
Spurgeon, L, Humphreys, G, James, G & Sackley, C, 2012, ‘A Q-methodology study of
patients’ subjective experiences of TIA’, Stroke research and treatment, 2012.
Tarola, G & Phillips, RB 2015, ‘Chiropractic response to a spontaneous vertebral artery
dissection’, Journal of chiropractic medicine, vol. 14, no. 3, pp.183-190.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





