CNA253 AT3: Scenario-Based Nursing Diagnosis and Care Plan
VerifiedAdded on 2023/04/23
|5
|1629
|53
Practical Assignment
AI Summary
This assignment details a nursing care plan for a 25-year-old male, Mr. X, admitted after a severe fall from a horse. The student identifies and prioritizes two nursing diagnoses: Ineffective tissue perfusion and Decreased intracranial adaptive capacity. Justifications for prioritization are provided, emphasizing the life-threatening nature of these conditions. The assignment outlines specific goals, related nursing actions with rationales, and evaluation methods for each diagnosis, demonstrating the application of the clinical reasoning cycle. The care plan includes interventions such as medication management, monitoring vital signs, and occupational therapy. The student reflects on the simulated episode, highlighting the importance of multidisciplinary care and clinical reasoning in achieving positive patient outcomes. The assignment adheres to the rubric requirements, utilizing current scholarly literature and textbooks to support clinical decisions and substantiating statements. References are provided to support the evidence-based practice.
Your student number:
CNA253 AT3
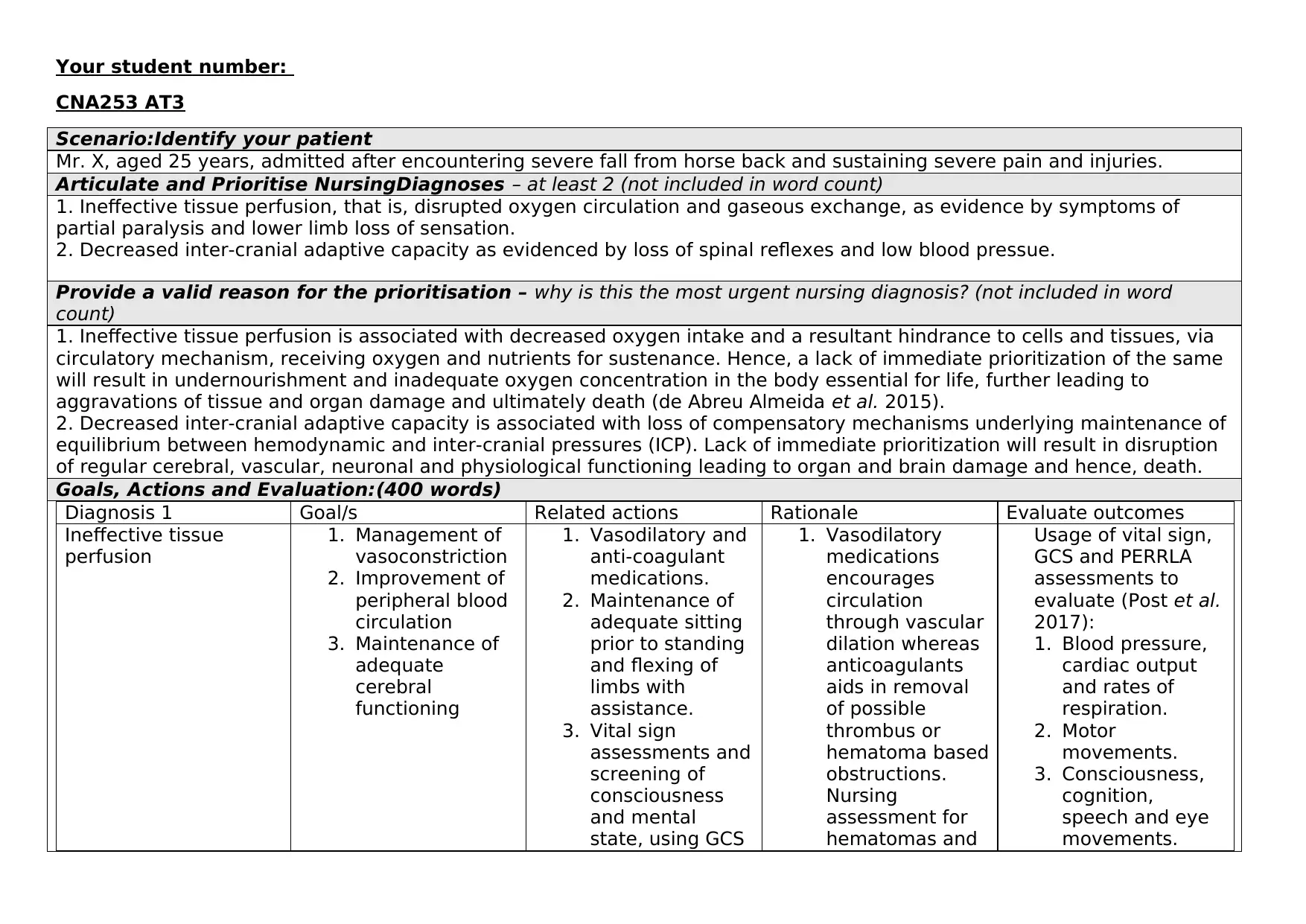
Scenario:Identify your patient
Mr. X, aged 25 years, admitted after encountering severe fall from horse back and sustaining severe pain and injuries.
Articulate and Prioritise NursingDiagnoses – at least 2 (not included in word count)
1. Ineffective tissue perfusion, that is, disrupted oxygen circulation and gaseous exchange, as evidence by symptoms of
partial paralysis and lower limb loss of sensation.
2. Decreased inter-cranial adaptive capacity as evidenced by loss of spinal reflexes and low blood pressue.
Provide a valid reason for the prioritisation – why is this the most urgent nursing diagnosis? (not included in word
count)
1. Ineffective tissue perfusion is associated with decreased oxygen intake and a resultant hindrance to cells and tissues, via
circulatory mechanism, receiving oxygen and nutrients for sustenance. Hence, a lack of immediate prioritization of the same
will result in undernourishment and inadequate oxygen concentration in the body essential for life, further leading to
aggravations of tissue and organ damage and ultimately death (de Abreu Almeida et al. 2015).
2. Decreased inter-cranial adaptive capacity is associated with loss of compensatory mechanisms underlying maintenance of
equilibrium between hemodynamic and inter-cranial pressures (ICP). Lack of immediate prioritization will result in disruption
of regular cerebral, vascular, neuronal and physiological functioning leading to organ and brain damage and hence, death.
Goals, Actions and Evaluation:(400 words)
Diagnosis 1 Goal/s Related actions Rationale Evaluate outcomes
Ineffective tissue
perfusion
1. Management of
vasoconstriction
2. Improvement of
peripheral blood
circulation
3. Maintenance of
adequate
cerebral
functioning
1. Vasodilatory and
anti-coagulant
medications.
2. Maintenance of
adequate sitting
prior to standing
and flexing of
limbs with
assistance.
3. Vital sign
assessments and
screening of
consciousness
and mental
state, using GCS
1. Vasodilatory
medications
encourages
circulation
through vascular
dilation whereas
anticoagulants
aids in removal
of possible
thrombus or
hematoma based
obstructions.
Nursing
assessment for
hematomas and
Usage of vital sign,
GCS and PERRLA
assessments to
evaluate (Post et al.
2017):
1. Blood pressure,
cardiac output
and rates of
respiration.
2. Motor
movements.
3. Consciousness,
cognition,
speech and eye
movements.
CNA253 AT3
Scenario:Identify your patient
Mr. X, aged 25 years, admitted after encountering severe fall from horse back and sustaining severe pain and injuries.
Articulate and Prioritise NursingDiagnoses – at least 2 (not included in word count)
1. Ineffective tissue perfusion, that is, disrupted oxygen circulation and gaseous exchange, as evidence by symptoms of
partial paralysis and lower limb loss of sensation.
2. Decreased inter-cranial adaptive capacity as evidenced by loss of spinal reflexes and low blood pressue.
Provide a valid reason for the prioritisation – why is this the most urgent nursing diagnosis? (not included in word
count)
1. Ineffective tissue perfusion is associated with decreased oxygen intake and a resultant hindrance to cells and tissues, via
circulatory mechanism, receiving oxygen and nutrients for sustenance. Hence, a lack of immediate prioritization of the same
will result in undernourishment and inadequate oxygen concentration in the body essential for life, further leading to
aggravations of tissue and organ damage and ultimately death (de Abreu Almeida et al. 2015).
2. Decreased inter-cranial adaptive capacity is associated with loss of compensatory mechanisms underlying maintenance of
equilibrium between hemodynamic and inter-cranial pressures (ICP). Lack of immediate prioritization will result in disruption
of regular cerebral, vascular, neuronal and physiological functioning leading to organ and brain damage and hence, death.
Goals, Actions and Evaluation:(400 words)
Diagnosis 1 Goal/s Related actions Rationale Evaluate outcomes
Ineffective tissue
perfusion
1. Management of
vasoconstriction
2. Improvement of
peripheral blood
circulation
3. Maintenance of
adequate
cerebral
functioning
1. Vasodilatory and
anti-coagulant
medications.
2. Maintenance of
adequate sitting
prior to standing
and flexing of
limbs with
assistance.
3. Vital sign
assessments and
screening of
consciousness
and mental
state, using GCS
1. Vasodilatory
medications
encourages
circulation
through vascular
dilation whereas
anticoagulants
aids in removal
of possible
thrombus or
hematoma based
obstructions.
Nursing
assessment for
hematomas and
Usage of vital sign,
GCS and PERRLA
assessments to
evaluate (Post et al.
2017):
1. Blood pressure,
cardiac output
and rates of
respiration.
2. Motor
movements.
3. Consciousness,
cognition,
speech and eye
movements.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
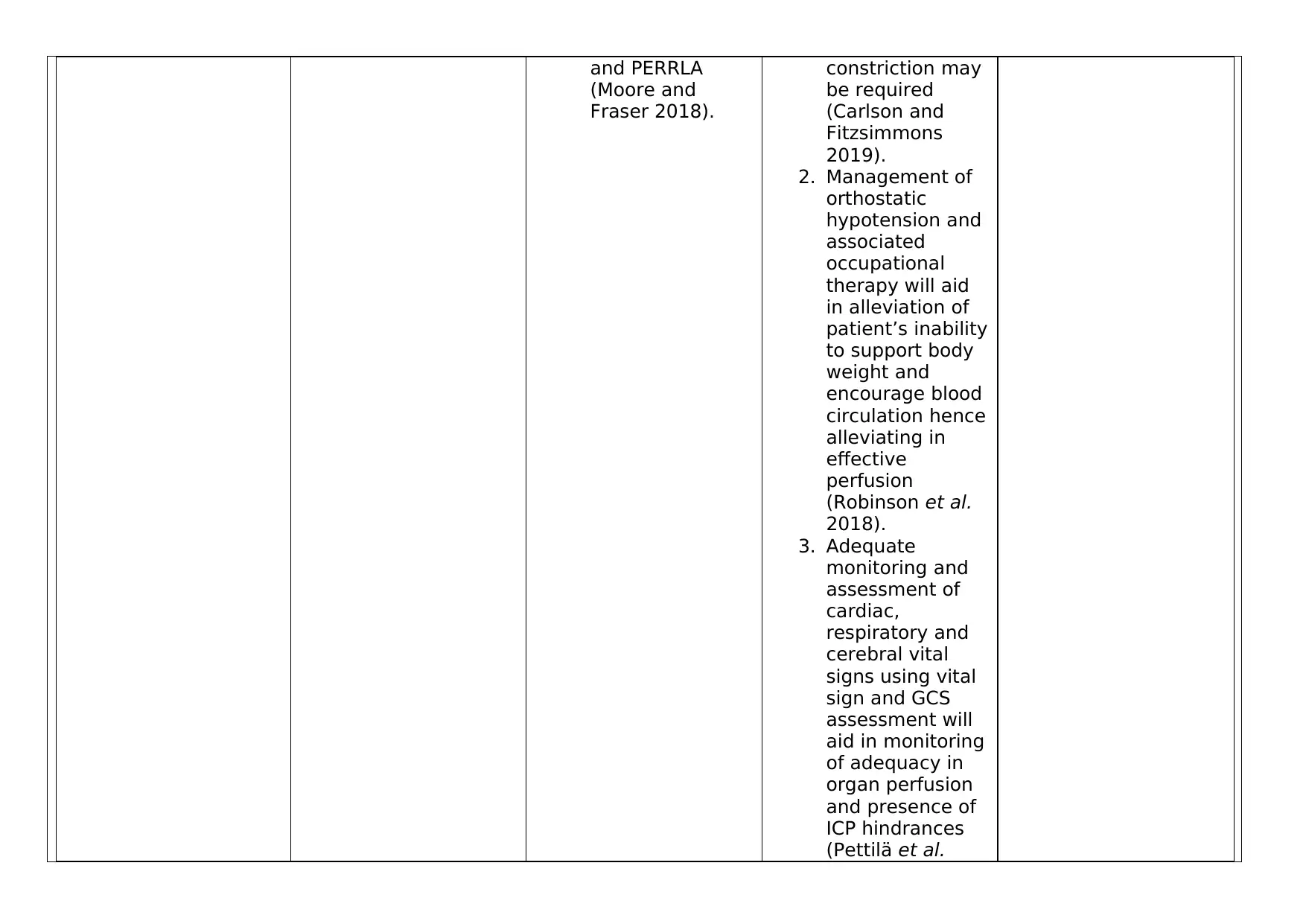
and PERRLA
(Moore and
Fraser 2018).
constriction may
be required
(Carlson and
Fitzsimmons
2019).
2. Management of
orthostatic
hypotension and
associated
occupational
therapy will aid
in alleviation of
patient’s inability
to support body
weight and
encourage blood
circulation hence
alleviating in
effective
perfusion
(Robinson et al.
2018).
3. Adequate
monitoring and
assessment of
cardiac,
respiratory and
cerebral vital
signs using vital
sign and GCS
assessment will
aid in monitoring
of adequacy in
organ perfusion
and presence of
ICP hindrances
(Pettilä et al.
(Moore and
Fraser 2018).
constriction may
be required
(Carlson and
Fitzsimmons
2019).
2. Management of
orthostatic
hypotension and
associated
occupational
therapy will aid
in alleviation of
patient’s inability
to support body
weight and
encourage blood
circulation hence
alleviating in
effective
perfusion
(Robinson et al.
2018).
3. Adequate
monitoring and
assessment of
cardiac,
respiratory and
cerebral vital
signs using vital
sign and GCS
assessment will
aid in monitoring
of adequacy in
organ perfusion
and presence of
ICP hindrances
(Pettilä et al.
2016).
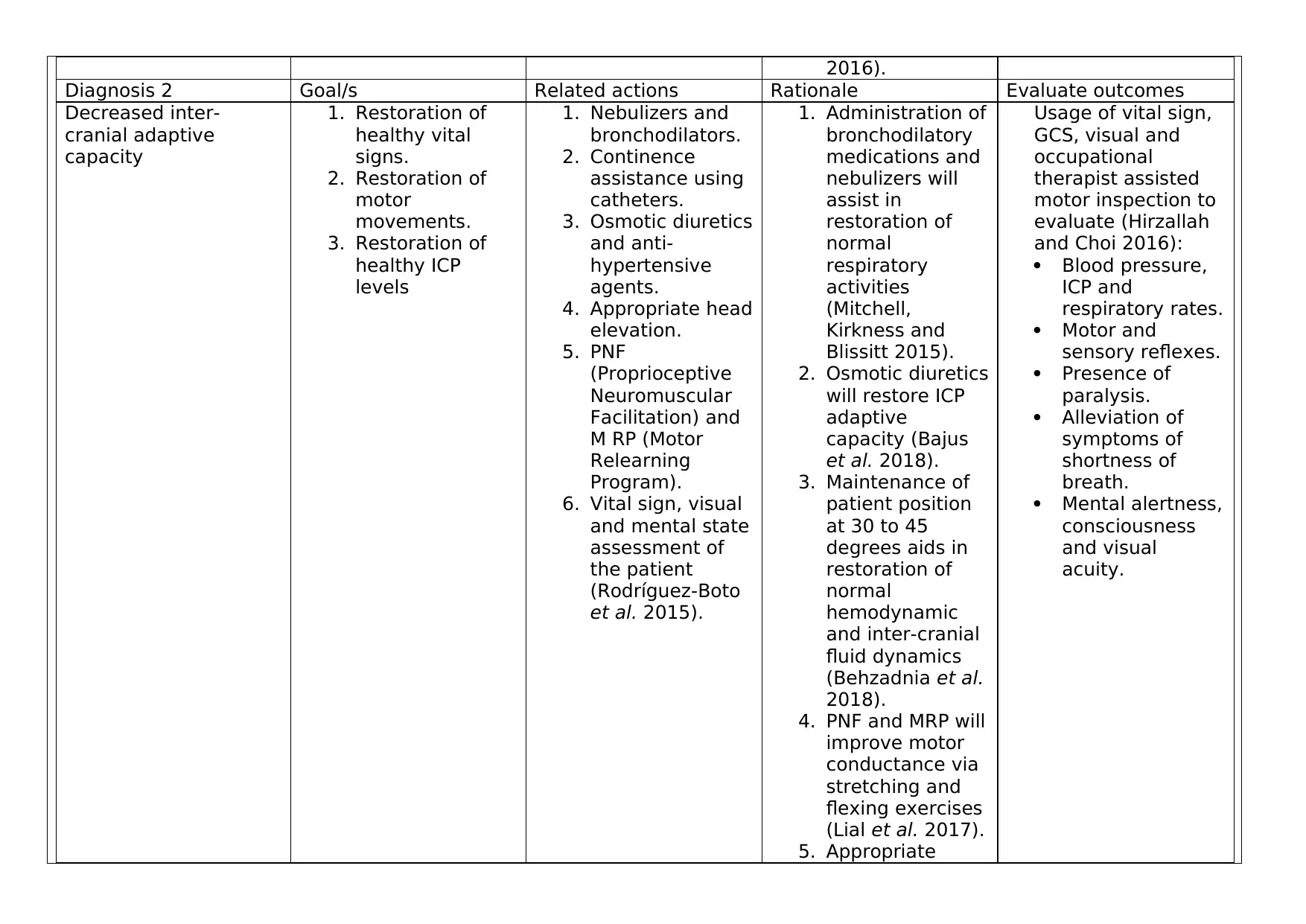
Diagnosis 2 Goal/s Related actions Rationale Evaluate outcomes
Decreased inter-
cranial adaptive
capacity
1. Restoration of
healthy vital
signs.
2. Restoration of
motor
movements.
3. Restoration of
healthy ICP
levels
1. Nebulizers and
bronchodilators.
2. Continence
assistance using
catheters.
3. Osmotic diuretics
and anti-
hypertensive
agents.
4. Appropriate head
elevation.
5. PNF
(Proprioceptive
Neuromuscular
Facilitation) and
M RP (Motor
Relearning
Program).
6. Vital sign, visual
and mental state
assessment of
the patient
(Rodríguez-Boto
et al. 2015).
1. Administration of
bronchodilatory
medications and
nebulizers will
assist in
restoration of
normal
respiratory
activities
(Mitchell,
Kirkness and
Blissitt 2015).
2. Osmotic diuretics
will restore ICP
adaptive
capacity (Bajus
et al. 2018).
3. Maintenance of
patient position
at 30 to 45
degrees aids in
restoration of
normal
hemodynamic
and inter-cranial
fluid dynamics
(Behzadnia et al.
2018).
4. PNF and MRP will
improve motor
conductance via
stretching and
flexing exercises
(Lial et al. 2017).
5. Appropriate
Usage of vital sign,
GCS, visual and
occupational
therapist assisted
motor inspection to
evaluate (Hirzallah
and Choi 2016):
Blood pressure,
ICP and
respiratory rates.
Motor and
sensory reflexes.
Presence of
paralysis.
Alleviation of
symptoms of
shortness of
breath.
Mental alertness,
consciousness
and visual
acuity.
Diagnosis 2 Goal/s Related actions Rationale Evaluate outcomes
Decreased inter-
cranial adaptive
capacity
1. Restoration of
healthy vital
signs.
2. Restoration of
motor
movements.
3. Restoration of
healthy ICP
levels
1. Nebulizers and
bronchodilators.
2. Continence
assistance using
catheters.
3. Osmotic diuretics
and anti-
hypertensive
agents.
4. Appropriate head
elevation.
5. PNF
(Proprioceptive
Neuromuscular
Facilitation) and
M RP (Motor
Relearning
Program).
6. Vital sign, visual
and mental state
assessment of
the patient
(Rodríguez-Boto
et al. 2015).
1. Administration of
bronchodilatory
medications and
nebulizers will
assist in
restoration of
normal
respiratory
activities
(Mitchell,
Kirkness and
Blissitt 2015).
2. Osmotic diuretics
will restore ICP
adaptive
capacity (Bajus
et al. 2018).
3. Maintenance of
patient position
at 30 to 45
degrees aids in
restoration of
normal
hemodynamic
and inter-cranial
fluid dynamics
(Behzadnia et al.
2018).
4. PNF and MRP will
improve motor
conductance via
stretching and
flexing exercises
(Lial et al. 2017).
5. Appropriate
Usage of vital sign,
GCS, visual and
occupational
therapist assisted
motor inspection to
evaluate (Hirzallah
and Choi 2016):
Blood pressure,
ICP and
respiratory rates.
Motor and
sensory reflexes.
Presence of
paralysis.
Alleviation of
symptoms of
shortness of
breath.
Mental alertness,
consciousness
and visual
acuity.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
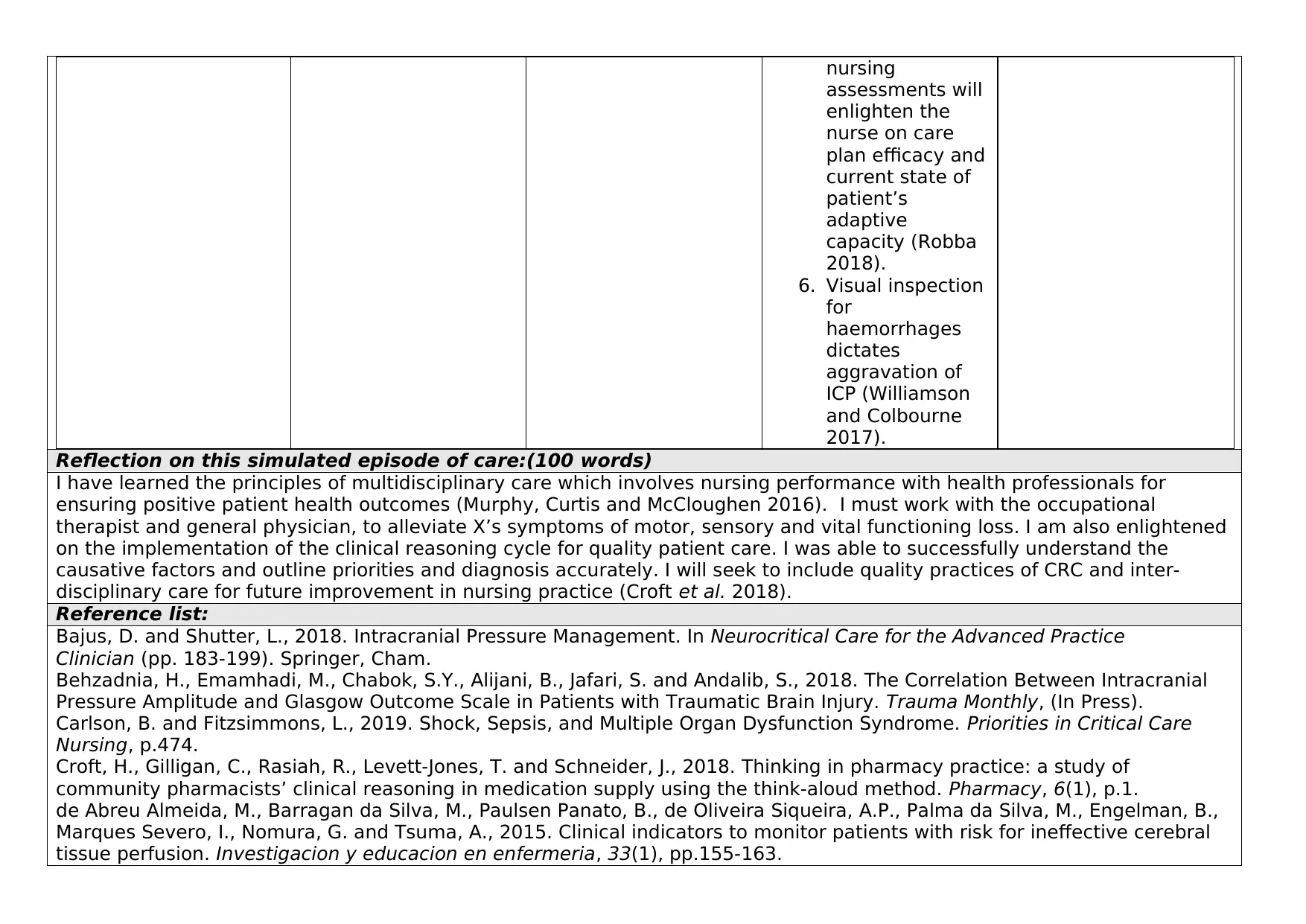
nursing
assessments will
enlighten the
nurse on care
plan efficacy and
current state of
patient’s
adaptive
capacity (Robba
2018).
6. Visual inspection
for
haemorrhages
dictates
aggravation of
ICP (Williamson
and Colbourne
2017).
Reflection on this simulated episode of care:(100 words)
I have learned the principles of multidisciplinary care which involves nursing performance with health professionals for
ensuring positive patient health outcomes (Murphy, Curtis and McCloughen 2016). I must work with the occupational
therapist and general physician, to alleviate X’s symptoms of motor, sensory and vital functioning loss. I am also enlightened
on the implementation of the clinical reasoning cycle for quality patient care. I was able to successfully understand the
causative factors and outline priorities and diagnosis accurately. I will seek to include quality practices of CRC and inter-
disciplinary care for future improvement in nursing practice (Croft et al. 2018).
Reference list:
Bajus, D. and Shutter, L., 2018. Intracranial Pressure Management. In Neurocritical Care for the Advanced Practice
Clinician (pp. 183-199). Springer, Cham.
Behzadnia, H., Emamhadi, M., Chabok, S.Y., Alijani, B., Jafari, S. and Andalib, S., 2018. The Correlation Between Intracranial
Pressure Amplitude and Glasgow Outcome Scale in Patients with Traumatic Brain Injury. Trauma Monthly, (In Press).
Carlson, B. and Fitzsimmons, L., 2019. Shock, Sepsis, and Multiple Organ Dysfunction Syndrome. Priorities in Critical Care
Nursing, p.474.
Croft, H., Gilligan, C., Rasiah, R., Levett-Jones, T. and Schneider, J., 2018. Thinking in pharmacy practice: a study of
community pharmacists’ clinical reasoning in medication supply using the think-aloud method. Pharmacy, 6(1), p.1.
de Abreu Almeida, M., Barragan da Silva, M., Paulsen Panato, B., de Oliveira Siqueira, A.P., Palma da Silva, M., Engelman, B.,
Marques Severo, I., Nomura, G. and Tsuma, A., 2015. Clinical indicators to monitor patients with risk for ineffective cerebral
tissue perfusion. Investigacion y educacion en enfermeria, 33(1), pp.155-163.
assessments will
enlighten the
nurse on care
plan efficacy and
current state of
patient’s
adaptive
capacity (Robba
2018).
6. Visual inspection
for
haemorrhages
dictates
aggravation of
ICP (Williamson
and Colbourne
2017).
Reflection on this simulated episode of care:(100 words)
I have learned the principles of multidisciplinary care which involves nursing performance with health professionals for
ensuring positive patient health outcomes (Murphy, Curtis and McCloughen 2016). I must work with the occupational
therapist and general physician, to alleviate X’s symptoms of motor, sensory and vital functioning loss. I am also enlightened
on the implementation of the clinical reasoning cycle for quality patient care. I was able to successfully understand the
causative factors and outline priorities and diagnosis accurately. I will seek to include quality practices of CRC and inter-
disciplinary care for future improvement in nursing practice (Croft et al. 2018).
Reference list:
Bajus, D. and Shutter, L., 2018. Intracranial Pressure Management. In Neurocritical Care for the Advanced Practice
Clinician (pp. 183-199). Springer, Cham.
Behzadnia, H., Emamhadi, M., Chabok, S.Y., Alijani, B., Jafari, S. and Andalib, S., 2018. The Correlation Between Intracranial
Pressure Amplitude and Glasgow Outcome Scale in Patients with Traumatic Brain Injury. Trauma Monthly, (In Press).
Carlson, B. and Fitzsimmons, L., 2019. Shock, Sepsis, and Multiple Organ Dysfunction Syndrome. Priorities in Critical Care
Nursing, p.474.
Croft, H., Gilligan, C., Rasiah, R., Levett-Jones, T. and Schneider, J., 2018. Thinking in pharmacy practice: a study of
community pharmacists’ clinical reasoning in medication supply using the think-aloud method. Pharmacy, 6(1), p.1.
de Abreu Almeida, M., Barragan da Silva, M., Paulsen Panato, B., de Oliveira Siqueira, A.P., Palma da Silva, M., Engelman, B.,
Marques Severo, I., Nomura, G. and Tsuma, A., 2015. Clinical indicators to monitor patients with risk for ineffective cerebral
tissue perfusion. Investigacion y educacion en enfermeria, 33(1), pp.155-163.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Hirzallah, M.I. and Choi, H.A., 2016. The monitoring of brain edema and intracranial hypertension. Journal of Neurocritical
Care, 9(2), pp.92-104.
Lial, L., Moreira, R., Correia, L., Andrade, A., Pereira, A.C., Lira, R., Figueiredo, R., Silva-Júnior, F., Orsini, M., Ribeiro, P. and
Velasques, B., 2017. Proprioceptive neuromuscular facilitation increases alpha absolute power in the dorsolateral prefrontal
cortex and superior parietal cortex. Somatosensory & motor research, 34(3), pp.204-212.
Mitchell, P.H., Kirkness, C. and Blissitt, P.A., 2015. Cerebral Perfusion Pressure and Intracranial Pressure in Traumatic Brain
Injury. Annual Review of Nursing Research, Volume 33, 2015: Traumatic Brain Injury, p.111.
Moore, J. and Fraser, J.F., 2018. Clinical Implications of Monitoring Tissue Perfusion in Cardiogenic Shock. In Monitoring Tissue
Perfusion in Shock (pp. 193-206). Springer, Cham.
Murphy, M., Curtis, K. and McCloughen, A., 2016. What is the impact of multidisciplinary team simulation training on team
performance and efficiency of patient care? An integrative review. Australasian emergency nursing journal, 19(1), pp.44-53.
Pettilä, V., Merz, T., Wilkman, E., Perner, A., Karlsson, S., Lange, T., Hästbacka, J., Hjortrup, P.B., Kuitunen, A., Jakob, S.M. and
Takala, J., 2016. Targeted tissue perfusion versus macrocirculation-guided standard care in patients with septic shock
(TARTARE-2S): study protocol and statistical analysis plan for a randomized controlled trial. trials, 17(1), p.384.
Post, E.H., Kellum, J.A., Bellomo, R. and Vincent, J.L., 2017. Renal perfusion in sepsis: from macro-to microcirculation. Kidney
international, 91(1), pp.45-60.
Robba, C., 2018. Intracranial Pressure Monitoring. In Neuromonitoring Techniques (pp. 1-29). Academic Press.
Rodríguez-Boto, G., Rivero-Garvía, M., Gutiérrez-González, R. and Márquez-Rivas, J., 2015. Basic concepts about brain
pathophysiology and intracranial pressure monitoring. Neurología (English Edition), 30(1), pp.16-22.
Williamson, M.R. and Colbourne, F., 2017. Evidence for decreased brain parenchymal volume after large intracerebral
hemorrhages: a potential mechanism limiting intracranial pressure rises. Translational stroke research, 8(4), pp.386-396.
Care, 9(2), pp.92-104.
Lial, L., Moreira, R., Correia, L., Andrade, A., Pereira, A.C., Lira, R., Figueiredo, R., Silva-Júnior, F., Orsini, M., Ribeiro, P. and
Velasques, B., 2017. Proprioceptive neuromuscular facilitation increases alpha absolute power in the dorsolateral prefrontal
cortex and superior parietal cortex. Somatosensory & motor research, 34(3), pp.204-212.
Mitchell, P.H., Kirkness, C. and Blissitt, P.A., 2015. Cerebral Perfusion Pressure and Intracranial Pressure in Traumatic Brain
Injury. Annual Review of Nursing Research, Volume 33, 2015: Traumatic Brain Injury, p.111.
Moore, J. and Fraser, J.F., 2018. Clinical Implications of Monitoring Tissue Perfusion in Cardiogenic Shock. In Monitoring Tissue
Perfusion in Shock (pp. 193-206). Springer, Cham.
Murphy, M., Curtis, K. and McCloughen, A., 2016. What is the impact of multidisciplinary team simulation training on team
performance and efficiency of patient care? An integrative review. Australasian emergency nursing journal, 19(1), pp.44-53.
Pettilä, V., Merz, T., Wilkman, E., Perner, A., Karlsson, S., Lange, T., Hästbacka, J., Hjortrup, P.B., Kuitunen, A., Jakob, S.M. and
Takala, J., 2016. Targeted tissue perfusion versus macrocirculation-guided standard care in patients with septic shock
(TARTARE-2S): study protocol and statistical analysis plan for a randomized controlled trial. trials, 17(1), p.384.
Post, E.H., Kellum, J.A., Bellomo, R. and Vincent, J.L., 2017. Renal perfusion in sepsis: from macro-to microcirculation. Kidney
international, 91(1), pp.45-60.
Robba, C., 2018. Intracranial Pressure Monitoring. In Neuromonitoring Techniques (pp. 1-29). Academic Press.
Rodríguez-Boto, G., Rivero-Garvía, M., Gutiérrez-González, R. and Márquez-Rivas, J., 2015. Basic concepts about brain
pathophysiology and intracranial pressure monitoring. Neurología (English Edition), 30(1), pp.16-22.
Williamson, M.R. and Colbourne, F., 2017. Evidence for decreased brain parenchymal volume after large intracerebral
hemorrhages: a potential mechanism limiting intracranial pressure rises. Translational stroke research, 8(4), pp.386-396.
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
