CNA253 - Patient Scenario, Nursing Diagnosis, and Care Plan Assignment
VerifiedAdded on 2022/12/01
|5
|908
|283
Homework Assignment
AI Summary
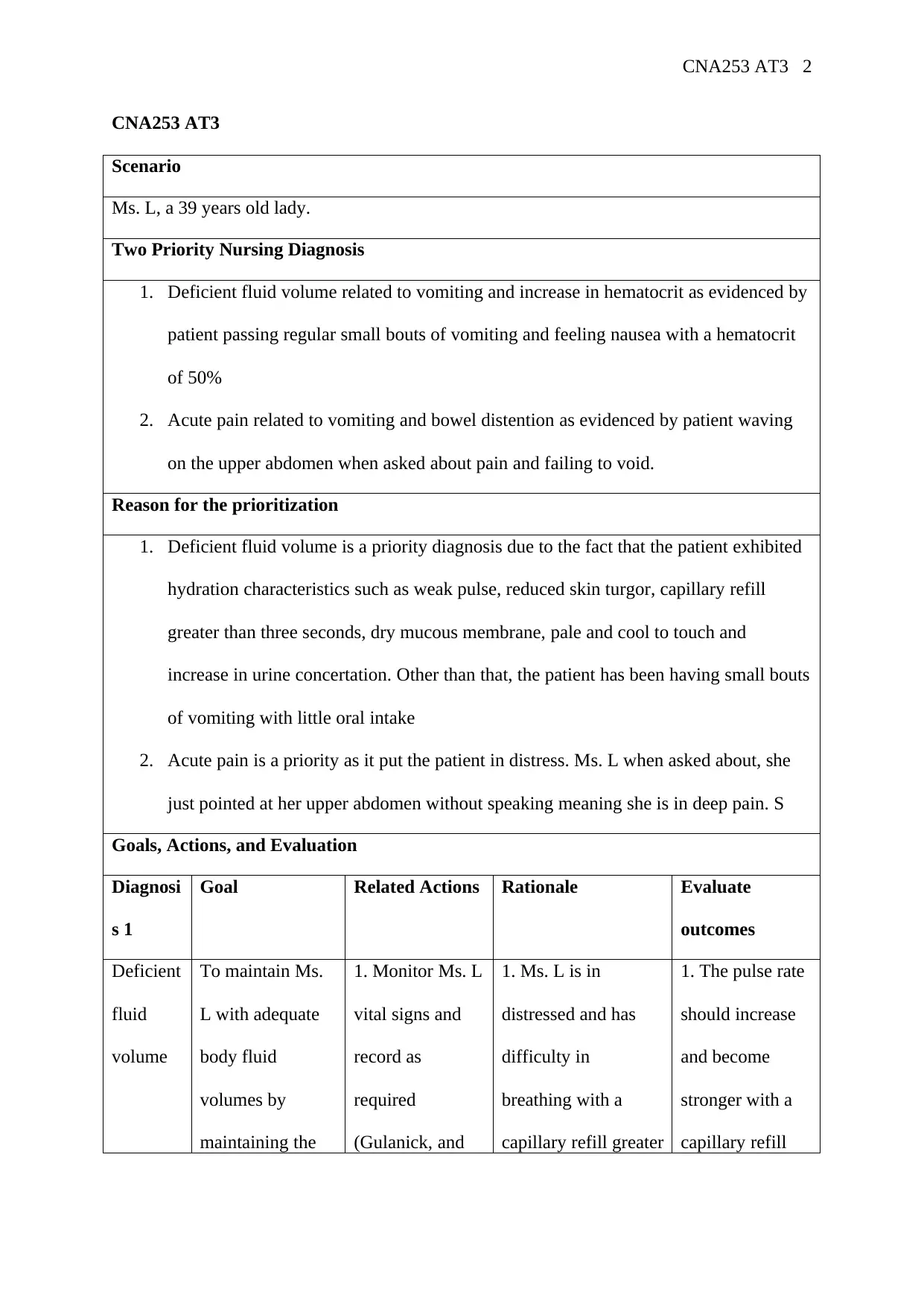
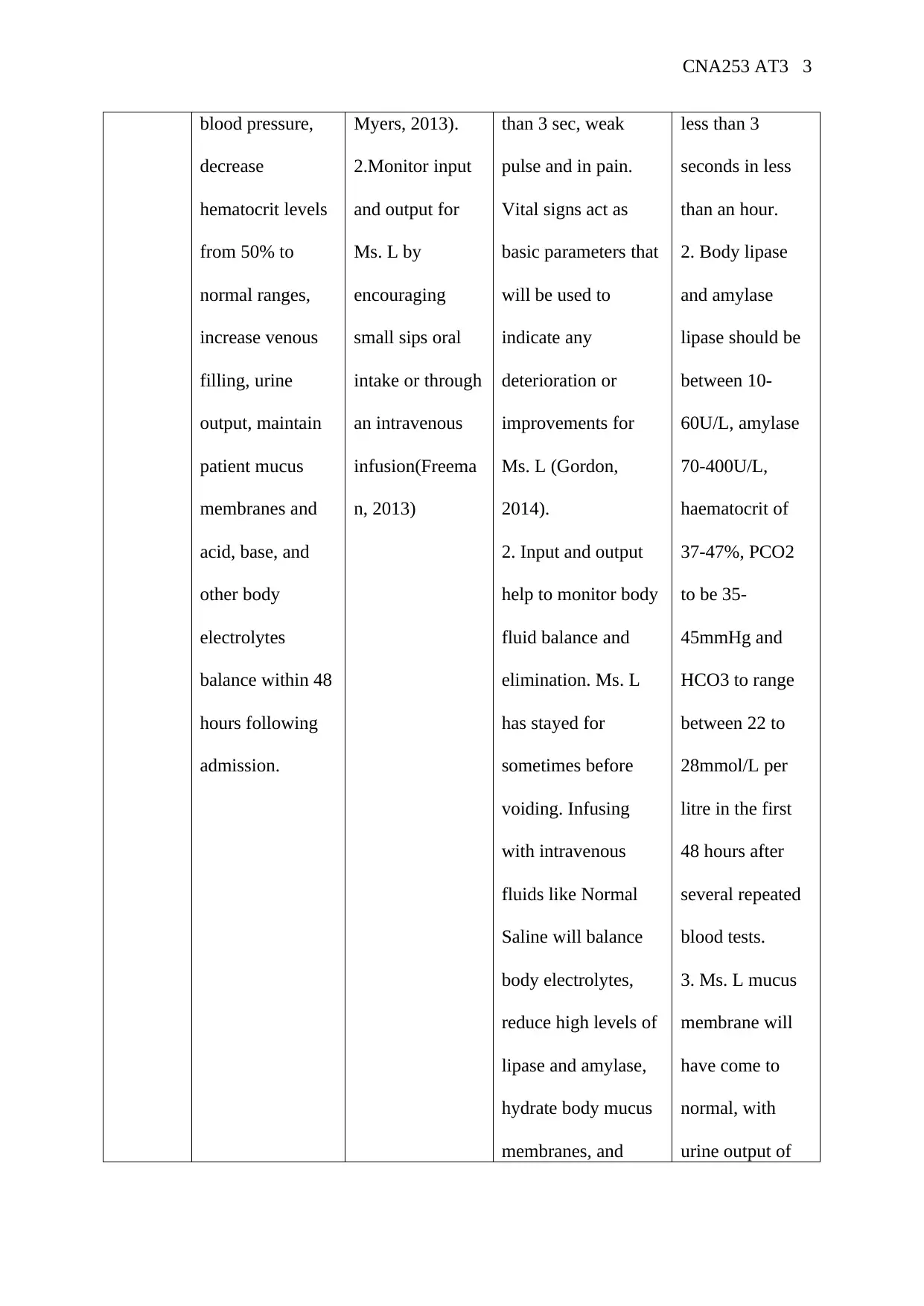
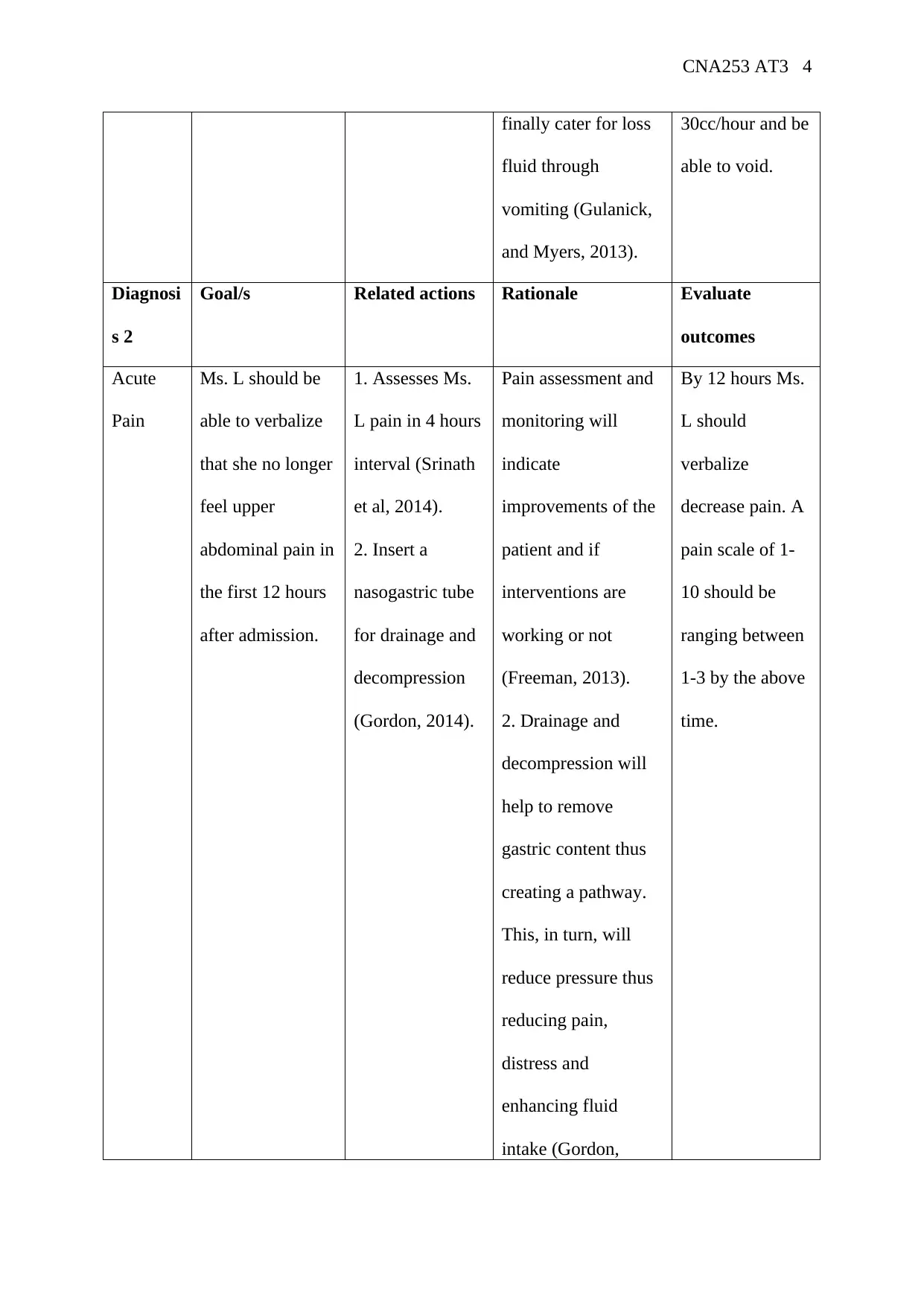
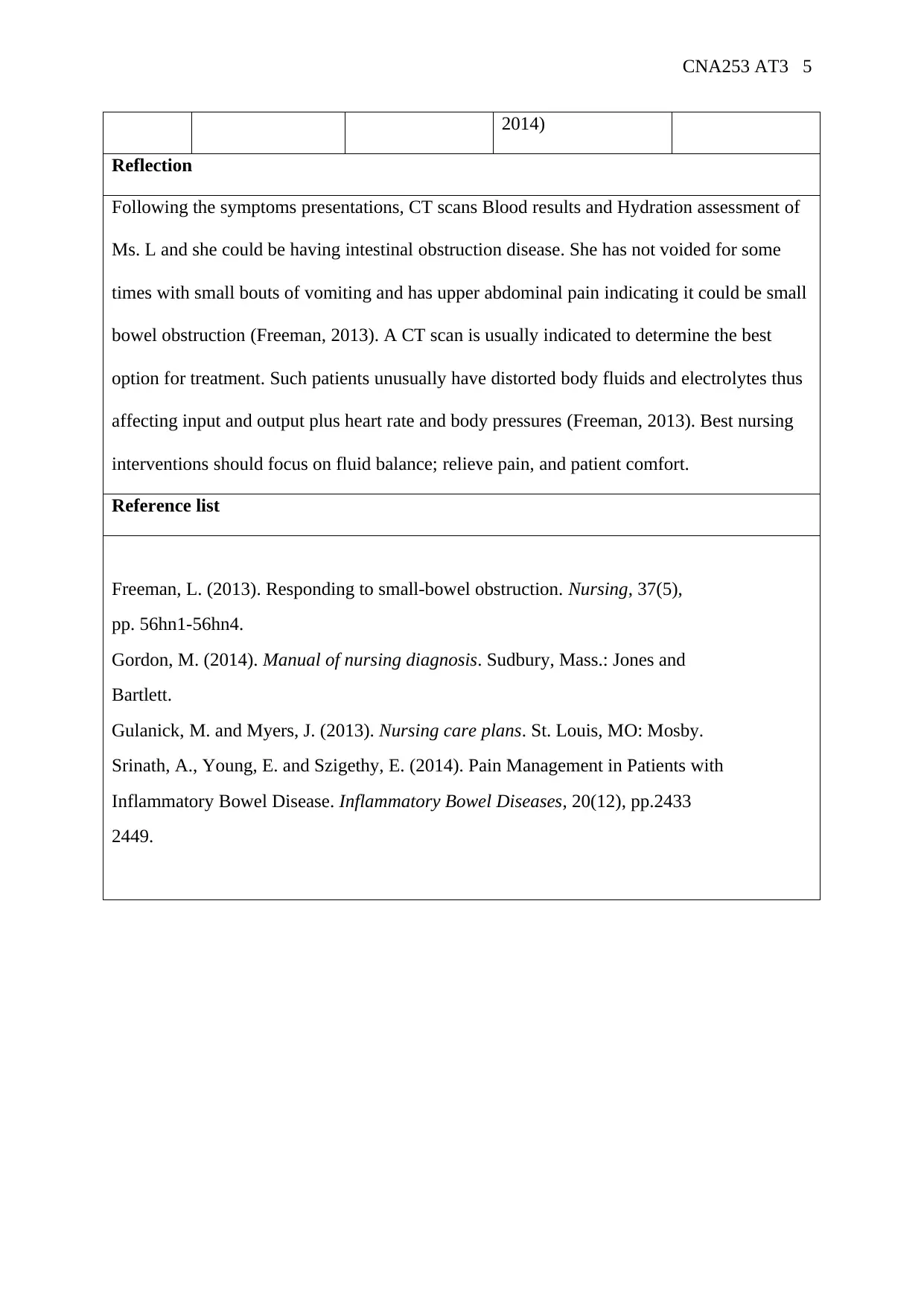
This CNA253 assignment focuses on a patient case study, Ms. L, a 39-year-old woman presenting with nausea, vomiting, and abdominal pain. The student identifies and prioritizes two nursing diagnoses: deficient fluid volume and acute pain, providing rationale based on patient assessment findings such as weak pulses, reduced skin turgor, and elevated hematocrit and lipase levels. The assignment includes goals, related nursing actions with rationales, and expected outcomes for each diagnosis. The student also reflects on the case, suggesting a possible diagnosis of intestinal obstruction and the need for further investigation with CT scans, emphasizing the importance of fluid balance, pain management, and patient comfort. References are also provided. The assignment demonstrates understanding of patient assessment, nursing diagnosis, care planning, and evaluation of outcomes.
1 out of 5




![[object Object]](/_next/static/media/star-bottom.7253800d.svg)