CNA344: Practice Portfolio - Clinical Encounter Analysis and Goals
VerifiedAdded on 2022/09/02
|8
|2675
|43
Project
AI Summary
This assignment presents a detailed clinical encounter analysis focusing on a patient experiencing delirium. The analysis begins with an overview of the patient's situation, including how the patient was found unconscious and unresponsive. The assignment then reviews available information, such as the patient's medical history and initial assessments, and gathers new information through additional assessments, including vital signs and laboratory results. The student recalls relevant knowledge to understand the patient's condition, identifying signs and symptoms of delirium. The assignment then processes the gathered information to determine two primary nursing problems: the increased risk of harm to the patient experiencing delirium and the identification of the cause of delirium. Goals are established for each problem, along with rationales for nursing actions based on scholarly literature and clinical guidelines. The assignment concludes with an evaluation of the outcomes of the clinical encounter, highlighting the interventions used to manage the patient's condition, and emphasizes the importance of early detection and intervention for delirium.
CNA344: Becoming a RN: Practice consolidation
Practice Portfolio of Evidence PART B:Clinical Encounter Analysis
Consider the patient
situation/context
(@150 words)
Provide an overview
of the encounter.
What happened, how
it occurred, what was
it that alerted you to
that fact that you
needed to take action
in the encounter.
All these things began when Hanna went on to talk to her father in the shed she found him unconscious and unresponsive and also ran
to call the ambulance. After that she pulled her father out of the shed in order to get some fresh air. Lars De Jong arrived in the
hospital in an ambulance and was not breathing or responding to the changes. However, the ambulance could feel a slight carotid
pulse. After arriving in the hospital the patient was still unconscious and was breathing at a faster rate. Then after the registrar arrived,
he put the patient on mechanical ventilation and after that the patient was admitted to ICU. Her daughter, Hanna was terribly worried
and tensed about Lars De Jongand wanted to know the medical state of her father. After that the healthcare staff in the ambulance
inserted an oropharyngeal airway, intravenous (IV) cannula and provided ventilation with bag/valve/mask using 100% oxygen.
Review(@150 words)
What key information
was already available
to you and how did
this influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
Gather(@150 words)
What was the new
information you
gathered from
Review:
After the analysis it was found that when Lars was admitted to the hospital due to unconsciousness and breathing problems. He also
had a problem of high blood pressure that created a lot of problems in the treatment. The previous history of Lars showed that he was
a migrant to Australia and used to work very hard in order to earn money. After Hanna’s child Charlie developed Autism Lars used to
take care of him. Lars also took care of his wife Isa, after she developed COPD and was suffering from type 2 diabetes. This made the
patient much more tensed and worried that created high blood pressure as well as mental stress. The constant stress upon the patient
about sharing the responsibility of the house deteriorated his condition that went unnoticed by the family members especially by
Hanna and resulted in a severe health condition of Lars.
Relevant medications (where relevant):(not included in word count)
Gather:
After the assessment the doctor mentioned that Lars was subjected to carbon monoxide and that could have damaged his brain. Thus, it was
important for him to regain consciousness in order to detect the amount of brain damage. When he regained consciousness it was found that he
1
Practice Portfolio of Evidence PART B:Clinical Encounter Analysis
Consider the patient
situation/context
(@150 words)
Provide an overview
of the encounter.
What happened, how
it occurred, what was
it that alerted you to
that fact that you
needed to take action
in the encounter.
All these things began when Hanna went on to talk to her father in the shed she found him unconscious and unresponsive and also ran
to call the ambulance. After that she pulled her father out of the shed in order to get some fresh air. Lars De Jong arrived in the
hospital in an ambulance and was not breathing or responding to the changes. However, the ambulance could feel a slight carotid
pulse. After arriving in the hospital the patient was still unconscious and was breathing at a faster rate. Then after the registrar arrived,
he put the patient on mechanical ventilation and after that the patient was admitted to ICU. Her daughter, Hanna was terribly worried
and tensed about Lars De Jongand wanted to know the medical state of her father. After that the healthcare staff in the ambulance
inserted an oropharyngeal airway, intravenous (IV) cannula and provided ventilation with bag/valve/mask using 100% oxygen.
Review(@150 words)
What key information
was already available
to you and how did
this influence your
thinking? (eg:
handover, history,
charts, result of test,
assessments, medical
orders
etc.).
Gather(@150 words)
What was the new
information you
gathered from
Review:
After the analysis it was found that when Lars was admitted to the hospital due to unconsciousness and breathing problems. He also
had a problem of high blood pressure that created a lot of problems in the treatment. The previous history of Lars showed that he was
a migrant to Australia and used to work very hard in order to earn money. After Hanna’s child Charlie developed Autism Lars used to
take care of him. Lars also took care of his wife Isa, after she developed COPD and was suffering from type 2 diabetes. This made the
patient much more tensed and worried that created high blood pressure as well as mental stress. The constant stress upon the patient
about sharing the responsibility of the house deteriorated his condition that went unnoticed by the family members especially by
Hanna and resulted in a severe health condition of Lars.
Relevant medications (where relevant):(not included in word count)
Gather:
After the assessment the doctor mentioned that Lars was subjected to carbon monoxide and that could have damaged his brain. Thus, it was
important for him to regain consciousness in order to detect the amount of brain damage. When he regained consciousness it was found that he
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
additional
assessment?
Dot points are fine for
this section
Recall(@200 words)
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
was not able to move his legs and hands properly. His heart rate and the respiratory were both increased. Thus, the healthcare staff and the
nurses had to work very hard in order to maintain the heart rate as well as the respiratory rate. After that there was urine assessment
performed for the patient as his urine output was continuously decreasing (Maldonado 2017; Maldonado 2018).
After that a new series of blood tests were also performed that included bilirubin, creatinine and platelet tests that will give additional
information about the patient. It highlighted that the creatinine was 420 mg/dL, bilirubin 83 mg/dL and platelets of 90 (x10³/uL).
Recall:
After the assessment, it was found that the site of insertion of the CVC was warm and red and there was no other sign of infection. Thus there
was a diagnosis for the Central Line Associated Bloodstream Infection (CLABSI) that will help in the identification and determination of the
infection sites in the blood. Along with this, it was observed that the patient was becoming extremely aggressive and agitated and continuously
tried to remove the pipes and tubes that were used for the treatment of the patient. All these signs and symptoms showed that the patient
needed solution as well as a new approach to the treatment process. Whenever, he was not showing this behaviour he was withdrawn,
apathetic, avoiding conversations and eye contact (ATG 2019).
Thus, it can be assumed that he was suffering from delirium and thus applied non-pharmacological protocols on him in order to assure Lars and
also to orient him back into the environment. All these information were gathered by the nursing professionals and they also tried to give the
proper treatment practice that included encouraging communication and repeated reorientation, ensuring visible daylight, consistency of
nursing staff, mobilisation activities and range of motion exercises. As per the NSQHS standards it is important that the healthcare professionals
have the ability to cover the incidents that can result in adverse events and can also help in the prevention of the deterioration of the clinical
condition.
2
assessment?
Dot points are fine for
this section
Recall(@200 words)
Recall and apply your
existing knowledge to
the above situation to
ensure you have a
broad understanding
of what is/may be
occurring before
proceeding with the
rest of the cycle.
What was telling you
that the encounter
was presenting you
with a problem that
required resolution?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
was not able to move his legs and hands properly. His heart rate and the respiratory were both increased. Thus, the healthcare staff and the
nurses had to work very hard in order to maintain the heart rate as well as the respiratory rate. After that there was urine assessment
performed for the patient as his urine output was continuously decreasing (Maldonado 2017; Maldonado 2018).
After that a new series of blood tests were also performed that included bilirubin, creatinine and platelet tests that will give additional
information about the patient. It highlighted that the creatinine was 420 mg/dL, bilirubin 83 mg/dL and platelets of 90 (x10³/uL).
Recall:
After the assessment, it was found that the site of insertion of the CVC was warm and red and there was no other sign of infection. Thus there
was a diagnosis for the Central Line Associated Bloodstream Infection (CLABSI) that will help in the identification and determination of the
infection sites in the blood. Along with this, it was observed that the patient was becoming extremely aggressive and agitated and continuously
tried to remove the pipes and tubes that were used for the treatment of the patient. All these signs and symptoms showed that the patient
needed solution as well as a new approach to the treatment process. Whenever, he was not showing this behaviour he was withdrawn,
apathetic, avoiding conversations and eye contact (ATG 2019).
Thus, it can be assumed that he was suffering from delirium and thus applied non-pharmacological protocols on him in order to assure Lars and
also to orient him back into the environment. All these information were gathered by the nursing professionals and they also tried to give the
proper treatment practice that included encouraging communication and repeated reorientation, ensuring visible daylight, consistency of
nursing staff, mobilisation activities and range of motion exercises. As per the NSQHS standards it is important that the healthcare professionals
have the ability to cover the incidents that can result in adverse events and can also help in the prevention of the deterioration of the clinical
condition.
2
Process
Information(@400
words)
Interpret, relate and
infer from the
information gathered
Interpret, Relate and Infer:
The gathered information shows that the vital signs of the patient were high blood pressure without much change in the inotropic supports for
the patient. The increased heart rate was about 121 and the respiratory rate was 28 and there was a need to change the high flow nasal prong
support at 40L at 50% of Fi02 in order to maintain the Sp02 at more than 93%. After the diagnosis it was suspected that the patient might be
suffering from some blood infections and that caused a lot of problem in the diagnosis and further treatment of the patient. However, after
certain improvement in his condition he was shifted to the medical ward in order to continue with the IV antibiotics along with a psychiatric
3
Information(@400
words)
Interpret, relate and
infer from the
information gathered
Interpret, Relate and Infer:
The gathered information shows that the vital signs of the patient were high blood pressure without much change in the inotropic supports for
the patient. The increased heart rate was about 121 and the respiratory rate was 28 and there was a need to change the high flow nasal prong
support at 40L at 50% of Fi02 in order to maintain the Sp02 at more than 93%. After the diagnosis it was suspected that the patient might be
suffering from some blood infections and that caused a lot of problem in the diagnosis and further treatment of the patient. However, after
certain improvement in his condition he was shifted to the medical ward in order to continue with the IV antibiotics along with a psychiatric
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
to demonstrate an
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
Predict(@100 words)
What could/would
have happened in
your encounter if you
were to have taken
NO action and why?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
team.
It was supposed that the patient was suffering from delirium and that can be due to any abrupt changes inside the brain and can result either
due to dementia or any other action such as alcohol consumption. This was not assessed by the nursing staff that whether Lars was about to
develop dementia or not. They only consulted the psychiatrist about the aggressive state of the patient so that they can clam him down
whenever Lars is feeling withdrawn or was avoiding any kind of conversation (Fitzgerald et al. 2013; Williams 2013).
The reasons for the delirium of the patient can be attributed to a number of factors that included medications, infections, metabolic
disturbances, cardiac events, seizures, pain as well as discomfort. However, the pathophysiology of the disease is not well known. The main
principle for the management of the patient with delirium is to identify the key underlying reason for delirium and also to implement the non-
pharmacological measures. As it can arise from the medication problems and thus, it is important to review the medication history of the
patient along with implementing certain additional measure for handling the unpredictable behaviour or attitude of the patient (ATG 2019).
However, when Lars’s daughter wanted to talk or discuss about the various treatment or diagnosis that are opted for her father’s treatment
however, she was just calmed by the healthcare professionals about the treatment options. She was also told by the nurses not to worry as her
father was not having any kind of brain damage (Fong et al. 2015; NICE 2018).
The nurses also needed to keep the patient under continuous observation and that resulted in the slipping of the patient on the floor causing
him elbow tear. Thus, this was also the role of the nurse to take care of the fact that the patient was under continuous observation in order to
avoid any further clinical deterioration in the health of the patient (Inouye, Westendorp and Saczynski, 2014).
Predict:
It can be predicted that the patient was suffering from Delirium and thus it is important that the treatment is given in that manner only.
Delirium is a type of medical emergency that needs to be validated with the use of the proper treatment process (Cascella et al. 2018). If the
delirium of Lars was not detected at an early age by the nurses or was confused with that of dementia then it could have resulted in the further
deterioration of the patient. It can also be predicted that Lars had to stay for a longer time in the hospital and can also experience dementia
along with more hospital –acquired complications like fall or pressure sores and so on (ACSQHC 2016). This also happened to Lars as he had a
fall while staying at the hospital.
4
overall understanding
of the clinical
encounter to
determine the two
main nursing
problems.
Predict(@100 words)
What could/would
have happened in
your encounter if you
were to have taken
NO action and why?
Use scholarly,
evidence-based
literature/clinical
guidelines and/or
policy/NSQHS
materials to
substantiate your
discussion
team.
It was supposed that the patient was suffering from delirium and that can be due to any abrupt changes inside the brain and can result either
due to dementia or any other action such as alcohol consumption. This was not assessed by the nursing staff that whether Lars was about to
develop dementia or not. They only consulted the psychiatrist about the aggressive state of the patient so that they can clam him down
whenever Lars is feeling withdrawn or was avoiding any kind of conversation (Fitzgerald et al. 2013; Williams 2013).
The reasons for the delirium of the patient can be attributed to a number of factors that included medications, infections, metabolic
disturbances, cardiac events, seizures, pain as well as discomfort. However, the pathophysiology of the disease is not well known. The main
principle for the management of the patient with delirium is to identify the key underlying reason for delirium and also to implement the non-
pharmacological measures. As it can arise from the medication problems and thus, it is important to review the medication history of the
patient along with implementing certain additional measure for handling the unpredictable behaviour or attitude of the patient (ATG 2019).
However, when Lars’s daughter wanted to talk or discuss about the various treatment or diagnosis that are opted for her father’s treatment
however, she was just calmed by the healthcare professionals about the treatment options. She was also told by the nurses not to worry as her
father was not having any kind of brain damage (Fong et al. 2015; NICE 2018).
The nurses also needed to keep the patient under continuous observation and that resulted in the slipping of the patient on the floor causing
him elbow tear. Thus, this was also the role of the nurse to take care of the fact that the patient was under continuous observation in order to
avoid any further clinical deterioration in the health of the patient (Inouye, Westendorp and Saczynski, 2014).
Predict:
It can be predicted that the patient was suffering from Delirium and thus it is important that the treatment is given in that manner only.
Delirium is a type of medical emergency that needs to be validated with the use of the proper treatment process (Cascella et al. 2018). If the
delirium of Lars was not detected at an early age by the nurses or was confused with that of dementia then it could have resulted in the further
deterioration of the patient. It can also be predicted that Lars had to stay for a longer time in the hospital and can also experience dementia
along with more hospital –acquired complications like fall or pressure sores and so on (ACSQHC 2016). This also happened to Lars as he had a
fall while staying at the hospital.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Identify the
Problem/s
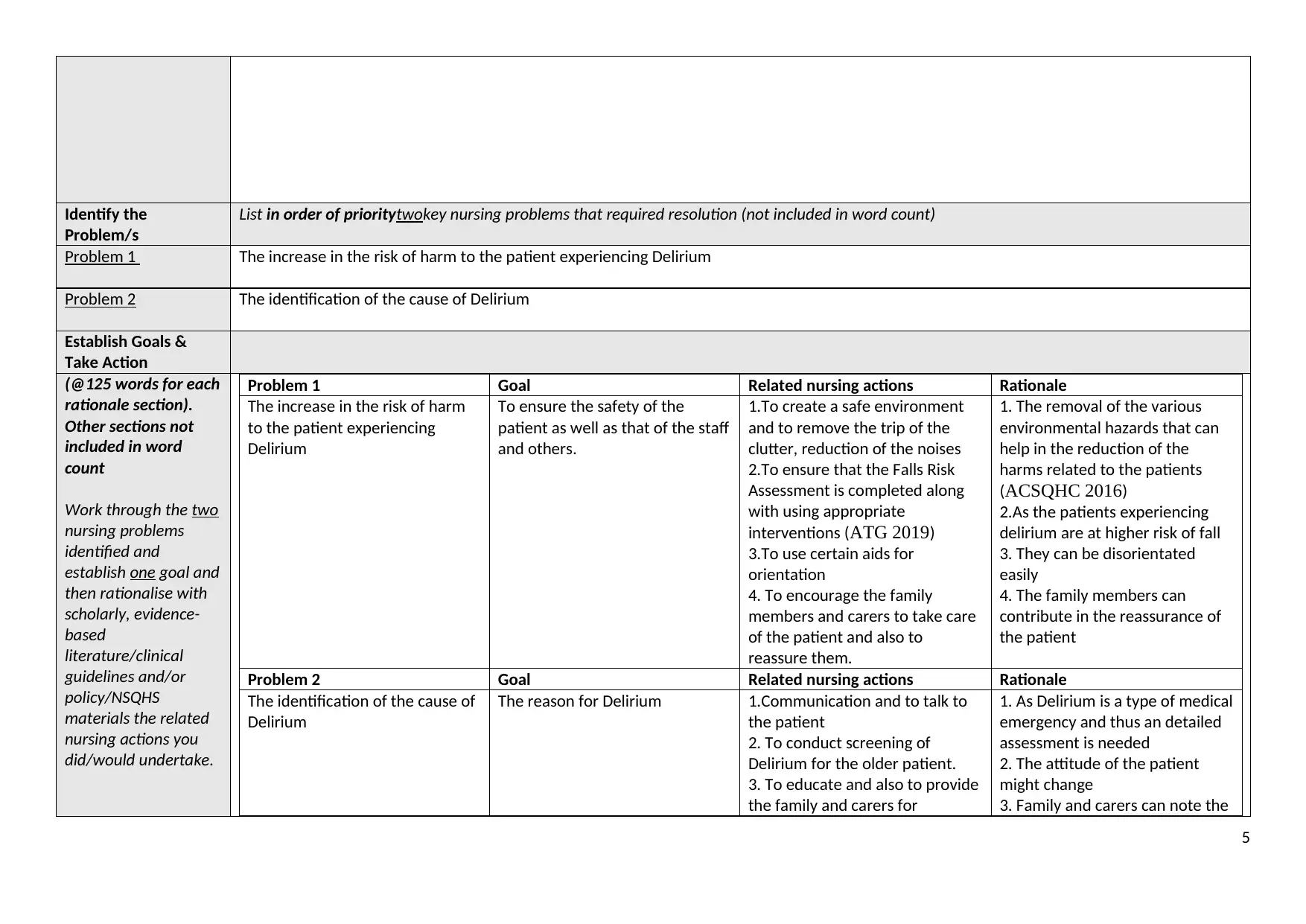
List in order of prioritytwokey nursing problems that required resolution (not included in word count)
Problem 1 The increase in the risk of harm to the patient experiencing Delirium
Problem 2 The identification of the cause of Delirium
Establish Goals &
Take Action
(@125 words for each
rationale section).
Other sections not
included in word
count
Work through the two
nursing problems
identified and
establish one goal and
then rationalise with
scholarly, evidence-
based
literature/clinical
guidelines and/or
policy/NSQHS
materials the related
nursing actions you
did/would undertake.
Problem 1 Goal Related nursing actions Rationale
The increase in the risk of harm
to the patient experiencing
Delirium
To ensure the safety of the
patient as well as that of the staff
and others.
1.To create a safe environment
and to remove the trip of the
clutter, reduction of the noises
2.To ensure that the Falls Risk
Assessment is completed along
with using appropriate
interventions (ATG 2019)
3.To use certain aids for
orientation
4. To encourage the family
members and carers to take care
of the patient and also to
reassure them.
1. The removal of the various
environmental hazards that can
help in the reduction of the
harms related to the patients
(ACSQHC 2016)
2.As the patients experiencing
delirium are at higher risk of fall
3. They can be disorientated
easily
4. The family members can
contribute in the reassurance of
the patient
Problem 2 Goal Related nursing actions Rationale
The identification of the cause of
Delirium
The reason for Delirium 1.Communication and to talk to
the patient
2. To conduct screening of
Delirium for the older patient.
3. To educate and also to provide
the family and carers for
1. As Delirium is a type of medical
emergency and thus an detailed
assessment is needed
2. The attitude of the patient
might change
3. Family and carers can note the
5
Problem/s
List in order of prioritytwokey nursing problems that required resolution (not included in word count)
Problem 1 The increase in the risk of harm to the patient experiencing Delirium
Problem 2 The identification of the cause of Delirium
Establish Goals &
Take Action
(@125 words for each
rationale section).
Other sections not
included in word
count
Work through the two
nursing problems
identified and
establish one goal and
then rationalise with
scholarly, evidence-
based
literature/clinical
guidelines and/or
policy/NSQHS
materials the related
nursing actions you
did/would undertake.
Problem 1 Goal Related nursing actions Rationale
The increase in the risk of harm
to the patient experiencing
Delirium
To ensure the safety of the
patient as well as that of the staff
and others.
1.To create a safe environment
and to remove the trip of the
clutter, reduction of the noises
2.To ensure that the Falls Risk
Assessment is completed along
with using appropriate
interventions (ATG 2019)
3.To use certain aids for
orientation
4. To encourage the family
members and carers to take care
of the patient and also to
reassure them.
1. The removal of the various
environmental hazards that can
help in the reduction of the
harms related to the patients
(ACSQHC 2016)
2.As the patients experiencing
delirium are at higher risk of fall
3. They can be disorientated
easily
4. The family members can
contribute in the reassurance of
the patient
Problem 2 Goal Related nursing actions Rationale
The identification of the cause of
Delirium
The reason for Delirium 1.Communication and to talk to
the patient
2. To conduct screening of
Delirium for the older patient.
3. To educate and also to provide
the family and carers for
1. As Delirium is a type of medical
emergency and thus an detailed
assessment is needed
2. The attitude of the patient
might change
3. Family and carers can note the
5
reporting any change in the
behaviour or attitude of the
patient (Cascella et al. 2018).
4. To monitor the patient closely
and also to communicate with
them about the pain, infection or
malnutrition or dehydration or
medication an alcohol
withdrawal
(Safetyandquality.gov.au 2019)
change in the attitude and can
provide best primary treatment
4. The factors are common in the
elderly patients experiencing
delirium.
Evaluate
outcomes(@100
words)
Evaluate the
outcomes of your
clinical encounter
including effectiveness
of the care provided
with supporting
evidence-based
literature
*Do not ‘reflect on
new learning’ in this
section. This will
occur in your next
assessment (Part C).
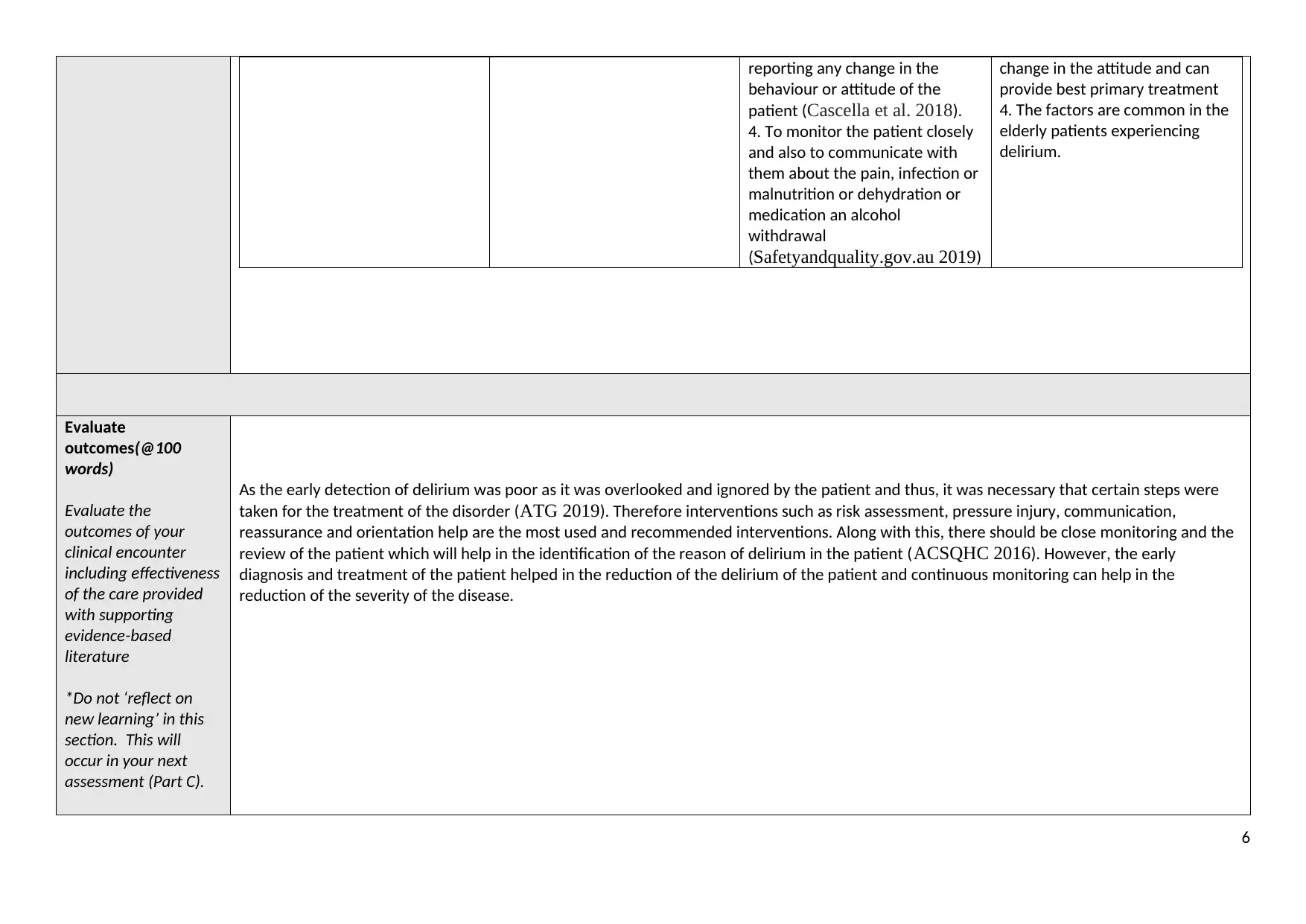
As the early detection of delirium was poor as it was overlooked and ignored by the patient and thus, it was necessary that certain steps were
taken for the treatment of the disorder (ATG 2019). Therefore interventions such as risk assessment, pressure injury, communication,
reassurance and orientation help are the most used and recommended interventions. Along with this, there should be close monitoring and the
review of the patient which will help in the identification of the reason of delirium in the patient (ACSQHC 2016). However, the early
diagnosis and treatment of the patient helped in the reduction of the delirium of the patient and continuous monitoring can help in the
reduction of the severity of the disease.
6
behaviour or attitude of the
patient (Cascella et al. 2018).
4. To monitor the patient closely
and also to communicate with
them about the pain, infection or
malnutrition or dehydration or
medication an alcohol
withdrawal
(Safetyandquality.gov.au 2019)
change in the attitude and can
provide best primary treatment
4. The factors are common in the
elderly patients experiencing
delirium.
Evaluate
outcomes(@100
words)
Evaluate the
outcomes of your
clinical encounter
including effectiveness
of the care provided
with supporting
evidence-based
literature
*Do not ‘reflect on
new learning’ in this
section. This will
occur in your next
assessment (Part C).
As the early detection of delirium was poor as it was overlooked and ignored by the patient and thus, it was necessary that certain steps were
taken for the treatment of the disorder (ATG 2019). Therefore interventions such as risk assessment, pressure injury, communication,
reassurance and orientation help are the most used and recommended interventions. Along with this, there should be close monitoring and the
review of the patient which will help in the identification of the reason of delirium in the patient (ACSQHC 2016). However, the early
diagnosis and treatment of the patient helped in the reduction of the delirium of the patient and continuous monitoring can help in the
reduction of the severity of the disease.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References:
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2016, Delirium Clinical Care Standard, ACSQHC, Sydney, viewed 5th January 2019,
< https://www.safetyandquality.gov.au/wp-content/uploads/2016/07/Delirium-Clinical-Care-Standard-Web-PDF.pdf>
Australian Therapeutic Guidelines (ATG) 2019b, Delirium, Therapeutic Guidelines, Melbourne, viewed 5th January 2019, Therapeutic Guidelines Database.
Cascella, M., Muzio, M.R., Bimonte, S., Cuomo, A. and Jakobsson, J.G., 2018. Postoperative delirium and postoperative cognitive dysfunction: updates in
pathophysiology, potential translational approaches to clinical practice and further research perspectives. Minerva anestesiologica, 84(2), pp.246-260.
Fitzgerald, J.M., Adamis, D., Trzepacz, P.T., O’Regan, N., Timmons, S., Dunne, C. and Meagher, D.J., 2013. Delirium: a disturbance of circadian
integrity?. Medical hypotheses, 81(4), pp.568-576.
Fong, T.G., Davis, D., Growdon, M.E., Albuquerque, A. and Inouye, S.K., 2015. The interface between delirium and dementia in elderly adults. The Lancet
Neurology, 14(8), pp.823-832.
Inouye, S.K., Westendorp, R.G. and Saczynski, J.S., 2014. Delirium in elderly people. The Lancet, 383(9920), pp.911-922.
Maldonado, J.R., 2017. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Critical care clinics, 33(3), pp.461-519.
Maldonado, J.R., 2018. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. International journal of geriatric
psychiatry, 33(11), pp.1428-1457.
National Institute for Health and Clinical Excellence (NICE) 2018, Dementia: assessment, management and support for people living with dementia and their
carers, NICE, London, viewed 5th January 2019, < https://www.nice.org.uk/guidance/ng97/resources/dementia-assessment-management-and-support-for-
people-living-with-dementiaand-their-carers-pdf-1837760199109>
Safetyandquality.gov.au 2019. [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-
and-Quality-Health-Service-Standards-second-edition.pdf [Accessed 1 Jan. 2020].
7
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2016, Delirium Clinical Care Standard, ACSQHC, Sydney, viewed 5th January 2019,
< https://www.safetyandquality.gov.au/wp-content/uploads/2016/07/Delirium-Clinical-Care-Standard-Web-PDF.pdf>
Australian Therapeutic Guidelines (ATG) 2019b, Delirium, Therapeutic Guidelines, Melbourne, viewed 5th January 2019, Therapeutic Guidelines Database.
Cascella, M., Muzio, M.R., Bimonte, S., Cuomo, A. and Jakobsson, J.G., 2018. Postoperative delirium and postoperative cognitive dysfunction: updates in
pathophysiology, potential translational approaches to clinical practice and further research perspectives. Minerva anestesiologica, 84(2), pp.246-260.
Fitzgerald, J.M., Adamis, D., Trzepacz, P.T., O’Regan, N., Timmons, S., Dunne, C. and Meagher, D.J., 2013. Delirium: a disturbance of circadian
integrity?. Medical hypotheses, 81(4), pp.568-576.
Fong, T.G., Davis, D., Growdon, M.E., Albuquerque, A. and Inouye, S.K., 2015. The interface between delirium and dementia in elderly adults. The Lancet
Neurology, 14(8), pp.823-832.
Inouye, S.K., Westendorp, R.G. and Saczynski, J.S., 2014. Delirium in elderly people. The Lancet, 383(9920), pp.911-922.
Maldonado, J.R., 2017. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Critical care clinics, 33(3), pp.461-519.
Maldonado, J.R., 2018. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. International journal of geriatric
psychiatry, 33(11), pp.1428-1457.
National Institute for Health and Clinical Excellence (NICE) 2018, Dementia: assessment, management and support for people living with dementia and their
carers, NICE, London, viewed 5th January 2019, < https://www.nice.org.uk/guidance/ng97/resources/dementia-assessment-management-and-support-for-
people-living-with-dementiaand-their-carers-pdf-1837760199109>
Safetyandquality.gov.au 2019. [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-
and-Quality-Health-Service-Standards-second-edition.pdf [Accessed 1 Jan. 2020].
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Williams, S.T., 2013. Pathophysiology of encephalopathy and delirium. Journal of Clinical Neurophysiology, 30(5), pp.435-437.
8
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





