Research Paper: Cognitive Therapy's Role in Treating Eating Disorders
VerifiedAdded on 2022/10/12
|12
|3008
|290
Report
AI Summary
This research paper is a comprehensive literature review exploring the efficacy of Cognitive Behavioral Therapy (CBT) in treating eating disorders. The paper begins with an introduction to eating disorders and the principles of CBT, followed by a detailed analysis of various studies. The review examines the effectiveness of CBT-E (enhanced CBT) in both inpatient and outpatient settings, focusing on its application to anorexia nervosa (AN) and other eating disorders. The paper discusses factors influencing treatment outcomes, such as the severity and duration of the disorder, and the importance of personalized therapy. The review highlights the positive impact of CBT on patients' behavioral changes and overall well-being. The research paper also identifies gaps in current knowledge and suggests areas for further study, emphasizing the need for more research on parameters to measure the outcome of CBT and the need for more research on different types of eating disorders. The paper concludes by synthesizing the findings and providing insights into the future direction of CBT in treating eating disorders.

Running head: RESEARCH PAPER
Role of Cognitive Therapy in Treating Eating Disorder (literature review)
Name of the Student
Name of the University
Author Note
Role of Cognitive Therapy in Treating Eating Disorder (literature review)
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
RESEARCH PAPER
Introduction (150)
According to Mental Health America (2019), eating disorders are regarded as
complex psychiatric illness that has serious health-related outcomes. Nearly 20 million
women and 10 million in the U.S execute significant symptom of eating disorder during any-
point of time in their life. Low self-esteem, cultural norms of attractiveness, sexual abuse and
over-controlling parents are some of the reason behind eating disorder. The long-term effects
of eating disorders are fata and this includes malnutrition, cardiovascular disease,
neurological and renal complications. There are no specific pharmacological interventions for
eating disorders, the health care professionals mainly rely over non-pharmacological
interventions in order to treat eating disorders. The following research paper aimed towards
identifying the role of cognitive behavioral therapy (CBT) as a potent non-pharmacological
intervention for the treatment of eating disorder. The paper will initiate with a brief
description of eating disorders and the concept underlying CBT. This will be followed by a
detailed literature review and discussion. Review will help in highlighting the current gaps in
knowledge about CBT treatment in eating disorders and thus will be helpful in giving a
direction for further studies.
Cognitive Behavioral Therapy
According to the American Psychological Association [APA] (2018), cognitive
behavior therapy (CBT) is defined as a form of psychological treatment that has
demonstrated efficacy in treating a range of psychological problems like depression, anxiety,
drug abuse, marital problems, eating disorder (anorexia and bulimia) and severe mental
illness. Numerous research conducted so far have helped in highlighting significant
improvements in the quality of life of the people upon application of the cognitive therapy.
The application of CBT is based on the concept that the thoughts, feelings, actions and
RESEARCH PAPER
Introduction (150)
According to Mental Health America (2019), eating disorders are regarded as
complex psychiatric illness that has serious health-related outcomes. Nearly 20 million
women and 10 million in the U.S execute significant symptom of eating disorder during any-
point of time in their life. Low self-esteem, cultural norms of attractiveness, sexual abuse and
over-controlling parents are some of the reason behind eating disorder. The long-term effects
of eating disorders are fata and this includes malnutrition, cardiovascular disease,
neurological and renal complications. There are no specific pharmacological interventions for
eating disorders, the health care professionals mainly rely over non-pharmacological
interventions in order to treat eating disorders. The following research paper aimed towards
identifying the role of cognitive behavioral therapy (CBT) as a potent non-pharmacological
intervention for the treatment of eating disorder. The paper will initiate with a brief
description of eating disorders and the concept underlying CBT. This will be followed by a
detailed literature review and discussion. Review will help in highlighting the current gaps in
knowledge about CBT treatment in eating disorders and thus will be helpful in giving a
direction for further studies.
Cognitive Behavioral Therapy
According to the American Psychological Association [APA] (2018), cognitive
behavior therapy (CBT) is defined as a form of psychological treatment that has
demonstrated efficacy in treating a range of psychological problems like depression, anxiety,
drug abuse, marital problems, eating disorder (anorexia and bulimia) and severe mental
illness. Numerous research conducted so far have helped in highlighting significant
improvements in the quality of life of the people upon application of the cognitive therapy.
The application of CBT is based on the concept that the thoughts, feelings, actions and
2
RESEARCH PAPER
physical sensations are all interconnected and constant channelization of negative thoughts
trap an individual under a vicious cycle of pessimism. CBT aims to understand these negative
thoughts by focusing in the current problems rather than understanding the past. Upon
understanding the root-cause of the negative thoughts, CBT aims to replace those negative
thoughts with positive thoughts (Verywellmind, 2019).
Eating disorders
Nurturing an unhealthy attitude towards food intake is referred to as eating disorders.
Men and women of any age can get affected with eating disorders. However, young adults or
adolescents between the age group of 13 to 17 years are considered as the main victims of
eating disorders. There are two types of eating disorders namely anorexia nervosa (AN),
bulimia, binge eating disorder (BED) and other specified feeding or eating disorder
(OSFED). AN patients try to keep their weight as low as possible by avoiding consumption
of food or conducting excessive exercise. The patients suffering from bulimia suffer from
frequent loss of control over the carving of food and end up consuming gamut meal during a
short span of time (binging) and as a result, they fall sick followed by deliberate use of
laxatives in order to excrete the consumed food. Unlike bulimia, BED patients regularly loose
control over eating. They consume controlled food until they feel uncomfortable and this is
followed by a sense of guilt. OSFED patients execute symptoms different from AN, bulimia
or BED (National Health Service [NHS], 2019).
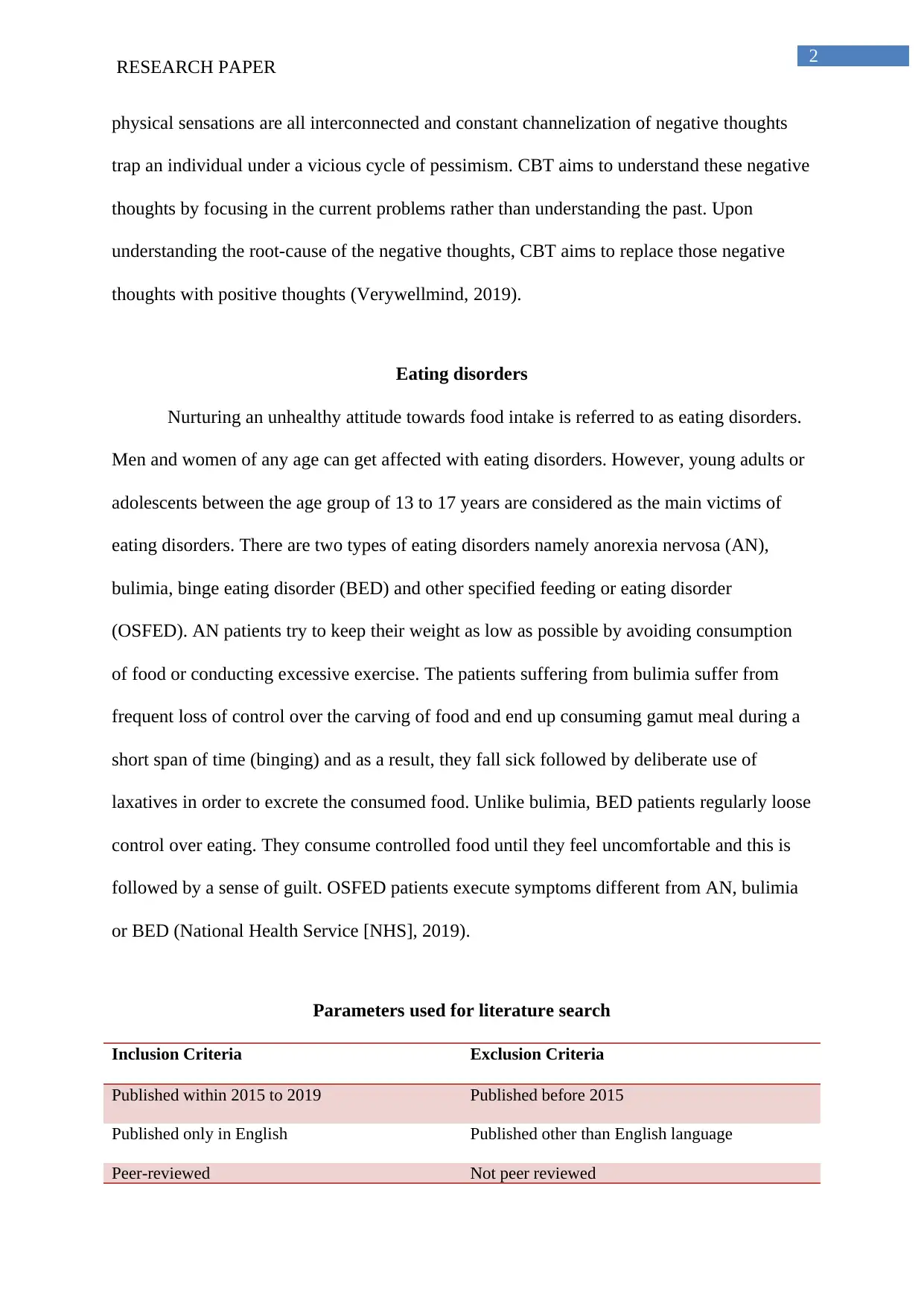
Parameters used for literature search
Inclusion Criteria Exclusion Criteria
Published within 2015 to 2019 Published before 2015
Published only in English Published other than English language
Peer-reviewed Not peer reviewed
RESEARCH PAPER
physical sensations are all interconnected and constant channelization of negative thoughts
trap an individual under a vicious cycle of pessimism. CBT aims to understand these negative
thoughts by focusing in the current problems rather than understanding the past. Upon
understanding the root-cause of the negative thoughts, CBT aims to replace those negative
thoughts with positive thoughts (Verywellmind, 2019).
Eating disorders
Nurturing an unhealthy attitude towards food intake is referred to as eating disorders.
Men and women of any age can get affected with eating disorders. However, young adults or
adolescents between the age group of 13 to 17 years are considered as the main victims of
eating disorders. There are two types of eating disorders namely anorexia nervosa (AN),
bulimia, binge eating disorder (BED) and other specified feeding or eating disorder
(OSFED). AN patients try to keep their weight as low as possible by avoiding consumption
of food or conducting excessive exercise. The patients suffering from bulimia suffer from
frequent loss of control over the carving of food and end up consuming gamut meal during a
short span of time (binging) and as a result, they fall sick followed by deliberate use of
laxatives in order to excrete the consumed food. Unlike bulimia, BED patients regularly loose
control over eating. They consume controlled food until they feel uncomfortable and this is
followed by a sense of guilt. OSFED patients execute symptoms different from AN, bulimia
or BED (National Health Service [NHS], 2019).
Parameters used for literature search
Inclusion Criteria Exclusion Criteria
Published within 2015 to 2019 Published before 2015
Published only in English Published other than English language
Peer-reviewed Not peer reviewed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
RESEARCH PAPER
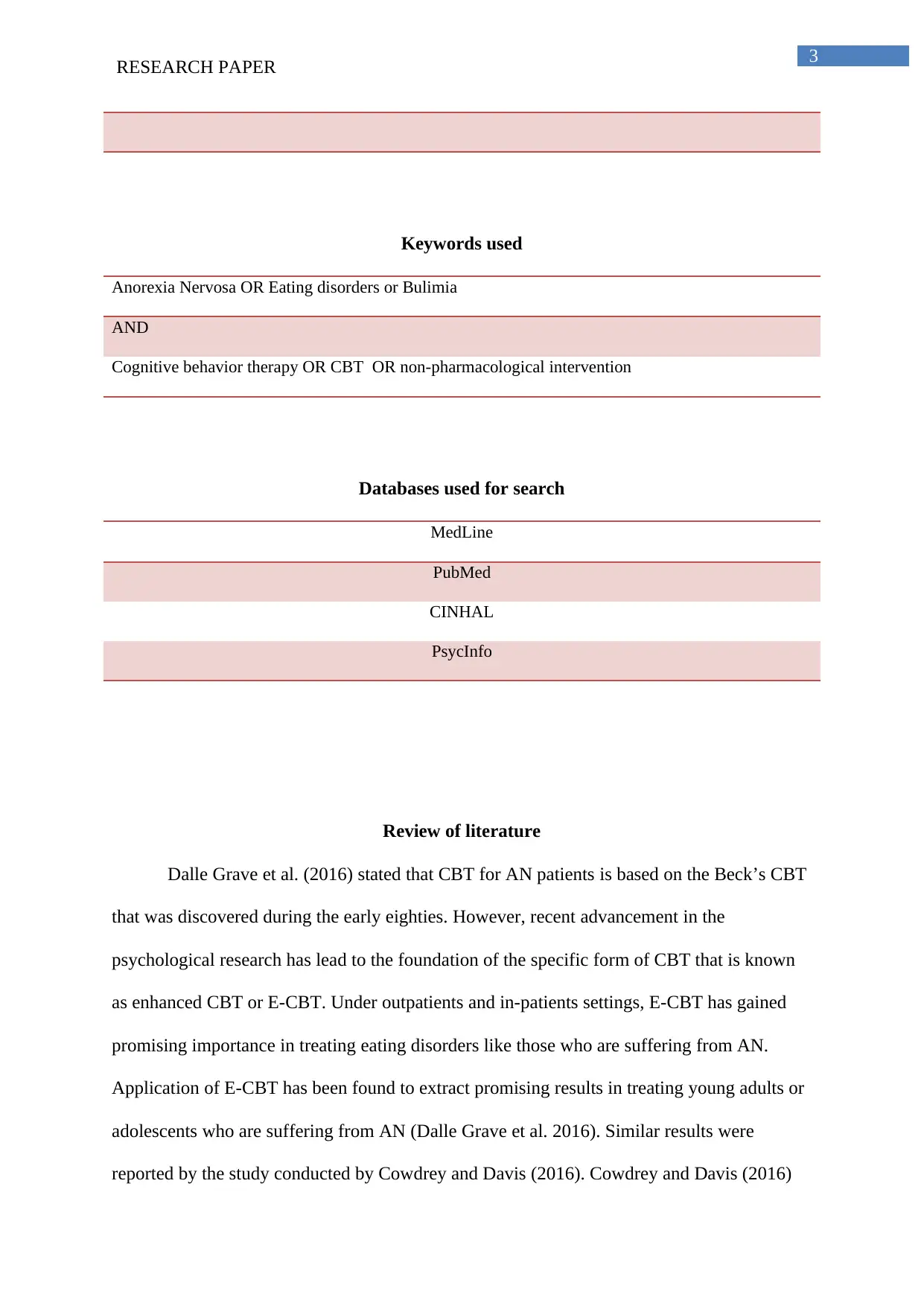
Keywords used
Anorexia Nervosa OR Eating disorders or Bulimia
AND
Cognitive behavior therapy OR CBT OR non-pharmacological intervention
Databases used for search
MedLine
PubMed
CINHAL
PsycInfo
Review of literature
Dalle Grave et al. (2016) stated that CBT for AN patients is based on the Beck’s CBT
that was discovered during the early eighties. However, recent advancement in the
psychological research has lead to the foundation of the specific form of CBT that is known
as enhanced CBT or E-CBT. Under outpatients and in-patients settings, E-CBT has gained
promising importance in treating eating disorders like those who are suffering from AN.
Application of E-CBT has been found to extract promising results in treating young adults or
adolescents who are suffering from AN (Dalle Grave et al. 2016). Similar results were
reported by the study conducted by Cowdrey and Davis (2016). Cowdrey and Davis (2016)
RESEARCH PAPER
Keywords used
Anorexia Nervosa OR Eating disorders or Bulimia
AND
Cognitive behavior therapy OR CBT OR non-pharmacological intervention
Databases used for search
MedLine
PubMed
CINHAL
PsycInfo
Review of literature
Dalle Grave et al. (2016) stated that CBT for AN patients is based on the Beck’s CBT
that was discovered during the early eighties. However, recent advancement in the
psychological research has lead to the foundation of the specific form of CBT that is known
as enhanced CBT or E-CBT. Under outpatients and in-patients settings, E-CBT has gained
promising importance in treating eating disorders like those who are suffering from AN.
Application of E-CBT has been found to extract promising results in treating young adults or
adolescents who are suffering from AN (Dalle Grave et al. 2016). Similar results were
reported by the study conducted by Cowdrey and Davis (2016). Cowdrey and Davis (2016)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
RESEARCH PAPER
conducted an observation study by self-monitoring of the records of both the baseline data
and after treatment data in order to ascertain the outcome of the application of CBT in
treating eating disorders. The analysis of the results highlighted that CBT is considered as
one of the important interventions among the young adults and adolescents for the treatment
eating disorders. The participants are of the opinion that CBT works by decreasing the fear of
body shaming or gaining weight and thus helping them to overcome the social stigma of
being fat and thereby helping to improve the eating habits. Similarly, like the study of
Cowdrey and Davis (2016), the study conducted by Onslow et al. (2016) aimed towards
addressing the experiences of the victims of eating disorders upon receiving the CBT-E.
Onslow et al. (2016) selected eight patients of bulimia who have completed CBT-E and use
semi-structured interview for the process of data collection. The interpretative
phenomenological analysis (IPA) highlighted that participants valued both the non-specific
and specific factors of CBT-E. The most important aspect of the therapy as highlighted by the
participants include, CBT helps in getting insight of the healthy lifestyle behaviors and
thereby helping to bring behavior change and improvement in the overall eating patterns.
However, in spite of the getting positive response from the patients who are suffering
from the eating disorders in relation to the CBT, there are studies that showed the overall
response of the CBT depends on the severity of the disease. The exploratory study conducted
by Cooper et al. (2016) reviewing the randomized control trial highlighted that outcome of
enhanced cognitive behavioral therapy (CBT-E) and interpersonal psychotherapy (IPT) over
the treatment of eating disorder depends on the severity of the eating disorder. The study
showed that patients with longer duration of the disorder are less likely to fetch benefit from
the both of the treatments. However, the study failed to highlight between CBT-E and IPT,
which therapy is more effective in fetching effective outcomes in the treatment process of
eating disorder. The study also failed to highlight how the treatment outcome can be
RESEARCH PAPER
conducted an observation study by self-monitoring of the records of both the baseline data
and after treatment data in order to ascertain the outcome of the application of CBT in
treating eating disorders. The analysis of the results highlighted that CBT is considered as
one of the important interventions among the young adults and adolescents for the treatment
eating disorders. The participants are of the opinion that CBT works by decreasing the fear of
body shaming or gaining weight and thus helping them to overcome the social stigma of
being fat and thereby helping to improve the eating habits. Similarly, like the study of
Cowdrey and Davis (2016), the study conducted by Onslow et al. (2016) aimed towards
addressing the experiences of the victims of eating disorders upon receiving the CBT-E.
Onslow et al. (2016) selected eight patients of bulimia who have completed CBT-E and use
semi-structured interview for the process of data collection. The interpretative
phenomenological analysis (IPA) highlighted that participants valued both the non-specific
and specific factors of CBT-E. The most important aspect of the therapy as highlighted by the
participants include, CBT helps in getting insight of the healthy lifestyle behaviors and
thereby helping to bring behavior change and improvement in the overall eating patterns.
However, in spite of the getting positive response from the patients who are suffering
from the eating disorders in relation to the CBT, there are studies that showed the overall
response of the CBT depends on the severity of the disease. The exploratory study conducted
by Cooper et al. (2016) reviewing the randomized control trial highlighted that outcome of
enhanced cognitive behavioral therapy (CBT-E) and interpersonal psychotherapy (IPT) over
the treatment of eating disorder depends on the severity of the eating disorder. The study
showed that patients with longer duration of the disorder are less likely to fetch benefit from
the both of the treatments. However, the study failed to highlight between CBT-E and IPT,
which therapy is more effective in fetching effective outcomes in the treatment process of
eating disorder. The study also failed to highlight how the treatment outcome can be
5
RESEARCH PAPER
measured. Cooper et al. (2016) stated that use of DSM-IV failed to predict the positive health
outcome. The study conducted by Fairburn et al. (2015) helped in getting a detailed
perspective of CBT and IPT in treating eating disorder. Fairburn et al. (2015) screened 130
patients who are suffering from eating disorders. The follow-up was conducted for 20 weeks
and blinded assessors analyzed the results. The results highlighted that CBT-E is potent
treatment options for the significant number of the pout-patients for the treatment of eating
disorders. While IPT can be considered as an alternative therapy for the treatment of the
eating disorder eating disorder to CBT-E. However, the response of IPT is comparatively less
pronounced in comparison to the CBT-E and overall outcome of the therapy is expressed
slowly.
Lammers et al. (2015) study showed that not only the duration of the occurrence of
the disease, but the outcome of CBT in treating eating disorder also depends on various other
factors. The study further helped in gaining detailed insight of the outcome reported by
Cooper et al. (2016). Lammers et al. (2015) showed that outcome of the CBT-E also depends
on the mental drive of attaining slim or thin figure, degree of interoceptive awareness, the
lower levels of binge eating pathology and gender of the individuals. Lammers et al. (2015)
also reported that based on the gender and their craving for attaining slim of zero figure, the
CBT therapy must be personalized. However, the study was only directed towards treating
AN patients and not patients who are suffering from binge eating as binge eating individuals
are not inclined to slim or thin body type. The study conducted by Raykos et al. (2018)
opposed by outcomes Cooper et al. (2016). Raykos et al. (2018) stated that higher levels of
severity of the disease and duration of the occurrence of the disease are not directly
associated with the overall treatment outcomes. The outcome is mainly driven by the how
perosnlization of the therapy and the duration for which the therapy is being applied to the
patients who are suffering from AN.
RESEARCH PAPER
measured. Cooper et al. (2016) stated that use of DSM-IV failed to predict the positive health
outcome. The study conducted by Fairburn et al. (2015) helped in getting a detailed
perspective of CBT and IPT in treating eating disorder. Fairburn et al. (2015) screened 130
patients who are suffering from eating disorders. The follow-up was conducted for 20 weeks
and blinded assessors analyzed the results. The results highlighted that CBT-E is potent
treatment options for the significant number of the pout-patients for the treatment of eating
disorders. While IPT can be considered as an alternative therapy for the treatment of the
eating disorder eating disorder to CBT-E. However, the response of IPT is comparatively less
pronounced in comparison to the CBT-E and overall outcome of the therapy is expressed
slowly.
Lammers et al. (2015) study showed that not only the duration of the occurrence of
the disease, but the outcome of CBT in treating eating disorder also depends on various other
factors. The study further helped in gaining detailed insight of the outcome reported by
Cooper et al. (2016). Lammers et al. (2015) showed that outcome of the CBT-E also depends
on the mental drive of attaining slim or thin figure, degree of interoceptive awareness, the
lower levels of binge eating pathology and gender of the individuals. Lammers et al. (2015)
also reported that based on the gender and their craving for attaining slim of zero figure, the
CBT therapy must be personalized. However, the study was only directed towards treating
AN patients and not patients who are suffering from binge eating as binge eating individuals
are not inclined to slim or thin body type. The study conducted by Raykos et al. (2018)
opposed by outcomes Cooper et al. (2016). Raykos et al. (2018) stated that higher levels of
severity of the disease and duration of the occurrence of the disease are not directly
associated with the overall treatment outcomes. The outcome is mainly driven by the how
perosnlization of the therapy and the duration for which the therapy is being applied to the
patients who are suffering from AN.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
RESEARCH PAPER
The majority of the study analyzed for far mainly helped in understanding the role of
CBT-E with a special focus on the AN. Dalle Grave et al. (2015) study helps to gain a
completely different aspect underlying the role of CBT in treating eating disorder. Dalle
Grave et al. (2015) reported that there is a marked treatment response over the adolescents
who are suffering from eating disorder but are not underweight. Thus Dalle Grave et al.
(2015) concluded that CBT-E is a promising treatment options for adolescents who are
suffering from eating disorder and are not under-weight.
Though the study conducted by Cooper et al. (2016) stated that there are no specific
parameters in order to ascertain the outcome of the eating disorder upon application of CBT,
Friederich et al. (2017) stated that emotional expression can be used as a parameter.
Improvement in the positive state of mind helps to indicate the positive change in the
behavior of the patient who is suffering from eating disorder and is being administered with
CBT. However, the results are any tested over the patients who are suffering from AN and
not from other eating disorders. The study conducted by Resmark et al. (2018) stated that
standardized treatment manual facilitate planning of therapy and increase in the
comparability of the research process. The use of the manual CBT is effective in improving
the outcome of the patients suffering from AN and the results is opposed to the study
conducted by Dalle Grave et al. (2016) and goes in favor of the study conducted by Lammers
et al. (2015). The results of this study is based on the observation conducted over the
Anorexia Nervosa Treatment of Out Patients. However, the same study was not undertaken
over the in-patients and thus limiting the generalization of the data.The study further
explained that more the CBT-E or E-CBT is manualised or developed in a person centred
manner, more-likely the therapy plan will receive improved outcome.
RESEARCH PAPER
The majority of the study analyzed for far mainly helped in understanding the role of
CBT-E with a special focus on the AN. Dalle Grave et al. (2015) study helps to gain a
completely different aspect underlying the role of CBT in treating eating disorder. Dalle
Grave et al. (2015) reported that there is a marked treatment response over the adolescents
who are suffering from eating disorder but are not underweight. Thus Dalle Grave et al.
(2015) concluded that CBT-E is a promising treatment options for adolescents who are
suffering from eating disorder and are not under-weight.
Though the study conducted by Cooper et al. (2016) stated that there are no specific
parameters in order to ascertain the outcome of the eating disorder upon application of CBT,
Friederich et al. (2017) stated that emotional expression can be used as a parameter.
Improvement in the positive state of mind helps to indicate the positive change in the
behavior of the patient who is suffering from eating disorder and is being administered with
CBT. However, the results are any tested over the patients who are suffering from AN and
not from other eating disorders. The study conducted by Resmark et al. (2018) stated that
standardized treatment manual facilitate planning of therapy and increase in the
comparability of the research process. The use of the manual CBT is effective in improving
the outcome of the patients suffering from AN and the results is opposed to the study
conducted by Dalle Grave et al. (2016) and goes in favor of the study conducted by Lammers
et al. (2015). The results of this study is based on the observation conducted over the
Anorexia Nervosa Treatment of Out Patients. However, the same study was not undertaken
over the in-patients and thus limiting the generalization of the data.The study further
explained that more the CBT-E or E-CBT is manualised or developed in a person centred
manner, more-likely the therapy plan will receive improved outcome.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
RESEARCH PAPER
Discussion
Thus from the above discussion, it can be stated that E-CBT hold prominent
importance in the treatment of eating disorders however the majority of the studies are being
conducted over the AN patients (Dalle Grave et al., 2016). Increasing the aspect of
personalization of the therapy can help to increase the overall therapy outcome (Resmark et
al., 2018). The analysis of the review also helped in highlighting that the theory can be
applied over both in-patient and out-patient settings and is also cost-effective in nature
(Resmark et al., 2018; Friederich et al., 2017). The reported published in the Center for
Eating Disorder (2019), showed that in out-patient department the outcome is more
pronounced than the in-patients. Their facial expression can be used as a parameter to
measure the outcome (Friederich et al., 2017).
The review also showed that the patients who are undertaking the therapy also gave
positive response in favor of the CBT. The patients reported that the application of CBT
helped in promoting their behavioral change. However, increase in the severity of the disease,
decreases the efficacy of the disease, the efficacy is also modulated by the age, gender and
mental complications (Lammers et al., 2015; Cooper et al., 2016).
Research gap
One of the research gaps that can be easily highlighted from the review is, all the
selected set of papers highlighted the efficacy of CBT over rating disorder, perception of the
patients and parameters of measure the outcome. The review helped in understanding that use
of CBT help in reducing eating disorder. However none of the study conducted so far have
examined whether after the completion of the CBT, eating disorder relapse. The
observational follow-p based study will help in ascertaining if the eating disorder is gets
RESEARCH PAPER
Discussion
Thus from the above discussion, it can be stated that E-CBT hold prominent
importance in the treatment of eating disorders however the majority of the studies are being
conducted over the AN patients (Dalle Grave et al., 2016). Increasing the aspect of
personalization of the therapy can help to increase the overall therapy outcome (Resmark et
al., 2018). The analysis of the review also helped in highlighting that the theory can be
applied over both in-patient and out-patient settings and is also cost-effective in nature
(Resmark et al., 2018; Friederich et al., 2017). The reported published in the Center for
Eating Disorder (2019), showed that in out-patient department the outcome is more
pronounced than the in-patients. Their facial expression can be used as a parameter to
measure the outcome (Friederich et al., 2017).
The review also showed that the patients who are undertaking the therapy also gave
positive response in favor of the CBT. The patients reported that the application of CBT
helped in promoting their behavioral change. However, increase in the severity of the disease,
decreases the efficacy of the disease, the efficacy is also modulated by the age, gender and
mental complications (Lammers et al., 2015; Cooper et al., 2016).
Research gap
One of the research gaps that can be easily highlighted from the review is, all the
selected set of papers highlighted the efficacy of CBT over rating disorder, perception of the
patients and parameters of measure the outcome. The review helped in understanding that use
of CBT help in reducing eating disorder. However none of the study conducted so far have
examined whether after the completion of the CBT, eating disorder relapse. The
observational follow-p based study will help in ascertaining if the eating disorder is gets

8
RESEARCH PAPER
relapsed even after application of CBT post 1 to 3 years. Such study will further help to
enlighten the efficacy of the CBT.
RESEARCH PAPER
relapsed even after application of CBT post 1 to 3 years. Such study will further help to
enlighten the efficacy of the CBT.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
RESEARCH PAPER
References
American Psychological Association [APA] (2019). What Is Cognitive Behavioral Therapy?.
Access date: 6th August 2019. Retrieved from:
https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
Cooper, Z., Allen, E., Bailey-Straebler, S., Basden, S., Murphy, R., O’Connor, M. E., &
Fairburn, C. G. (2016). Predictors and moderators of response to enhanced cognitive
behaviour therapy and interpersonal psychotherapy for the treatment of eating
disorders. Behaviour research and therapy, 84, 9-13.
Cowdrey, F. A., & Davis, J. (2016). Response to enhanced cognitive behavioural therapy in
an adolescent with anorexia nervosa. Behavioural and cognitive psychotherapy, 44(6),
717-722.
Dalle Grave, R., Calugi, S., Sartirana, M., & Fairburn, C. G. (2015). Transdiagnostic
cognitive behaviour therapy for adolescents with an eating disorder who are not
underweight. Behaviour research and therapy, 73, 79-82.
Dalle Grave, R., El Ghoch, M., Sartirana, M., & Calugi, S. (2016). Cognitive behavioral
therapy for anorexia nervosa: An update. Current psychiatry reports, 18(1), 2.
Fairburn, C. G., Bailey-Straebler, S., Basden, S., Doll, H. A., Jones, R., Murphy, R., ... &
Cooper, Z. (2015). A transdiagnostic comparison of enhanced cognitive behaviour
therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating
disorders. Behaviour research and therapy, 70, 64-71.
Friederich, H. C., Brockmeyer, T., Wild, B., Resmark, G., de Zwaan, M., Dinkel, A., ... &
Rothermund, E. (2017). Emotional expression predicts treatment outcome in focal
RESEARCH PAPER
References
American Psychological Association [APA] (2019). What Is Cognitive Behavioral Therapy?.
Access date: 6th August 2019. Retrieved from:
https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
Cooper, Z., Allen, E., Bailey-Straebler, S., Basden, S., Murphy, R., O’Connor, M. E., &
Fairburn, C. G. (2016). Predictors and moderators of response to enhanced cognitive
behaviour therapy and interpersonal psychotherapy for the treatment of eating
disorders. Behaviour research and therapy, 84, 9-13.
Cowdrey, F. A., & Davis, J. (2016). Response to enhanced cognitive behavioural therapy in
an adolescent with anorexia nervosa. Behavioural and cognitive psychotherapy, 44(6),
717-722.
Dalle Grave, R., Calugi, S., Sartirana, M., & Fairburn, C. G. (2015). Transdiagnostic
cognitive behaviour therapy for adolescents with an eating disorder who are not
underweight. Behaviour research and therapy, 73, 79-82.
Dalle Grave, R., El Ghoch, M., Sartirana, M., & Calugi, S. (2016). Cognitive behavioral
therapy for anorexia nervosa: An update. Current psychiatry reports, 18(1), 2.
Fairburn, C. G., Bailey-Straebler, S., Basden, S., Doll, H. A., Jones, R., Murphy, R., ... &
Cooper, Z. (2015). A transdiagnostic comparison of enhanced cognitive behaviour
therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating
disorders. Behaviour research and therapy, 70, 64-71.
Friederich, H. C., Brockmeyer, T., Wild, B., Resmark, G., de Zwaan, M., Dinkel, A., ... &
Rothermund, E. (2017). Emotional expression predicts treatment outcome in focal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
RESEARCH PAPER
psychodynamic and cognitive behavioural therapy for anorexia nervosa: findings
from the ANTOP study. Psychotherapy and psychosomatics, 86(2), 108-110.
Lammers, M. W., Vroling, M. S., Ouwens, M. A., Engels, R. C., & van Strien, T. (2015).
Predictors of outcome for cognitive behaviour therapy in binge eating
disorder. European Eating Disorders Review, 23(3), 219-228.
Mental Health America. (2019). Eating Disorders. Access date: 6th August 2019. Retrieved
from: https://www.mentalhealthamerica.net/conditions/eating-disorders
National Health Service. (2019). Overview of Eating Disorders. Access date: 6th August
2019. Retrieved from: https://www.nhs.uk/conditions/eating-disorders/
Onslow, L., Woodward, D., Hoefkens, T., & Waddington, L. (2016). Experiences of
Enhanced cognitive Behaviour therapy for Bulimia nervosa. Behavioural and
cognitive psychotherapy, 44(2), 168-178.
Raykos, B. C., Erceg-Hurn, D. M., McEvoy, P. M., Fursland, A., & Waller, G. (2018).
Severe and enduring anorexia nervosa? Illness severity and duration are unrelated to
outcomes from cognitive behaviour therapy. Journal of consulting and clinical
psychology, 86(8), 702.
References
Resmark, G., Kennedy, B., Mayer, M., Giel, K., Junne, F., Teufel, M., ... & Zipfel, S. (2018).
Manualised Cognitive Behaviour Therapy for Anorexia Nervosa: Use of Treatment
Modules in the ANTOP Study. Journal of clinical medicine, 7(11), 398.
The Center for Eating Disorder. (2019). The Outpatient Dialectical Behavior Therapy (DBT)
Program. Access date: 6th August 2019. Retrieved from:
RESEARCH PAPER
psychodynamic and cognitive behavioural therapy for anorexia nervosa: findings
from the ANTOP study. Psychotherapy and psychosomatics, 86(2), 108-110.
Lammers, M. W., Vroling, M. S., Ouwens, M. A., Engels, R. C., & van Strien, T. (2015).
Predictors of outcome for cognitive behaviour therapy in binge eating
disorder. European Eating Disorders Review, 23(3), 219-228.
Mental Health America. (2019). Eating Disorders. Access date: 6th August 2019. Retrieved
from: https://www.mentalhealthamerica.net/conditions/eating-disorders
National Health Service. (2019). Overview of Eating Disorders. Access date: 6th August
2019. Retrieved from: https://www.nhs.uk/conditions/eating-disorders/
Onslow, L., Woodward, D., Hoefkens, T., & Waddington, L. (2016). Experiences of
Enhanced cognitive Behaviour therapy for Bulimia nervosa. Behavioural and
cognitive psychotherapy, 44(2), 168-178.
Raykos, B. C., Erceg-Hurn, D. M., McEvoy, P. M., Fursland, A., & Waller, G. (2018).
Severe and enduring anorexia nervosa? Illness severity and duration are unrelated to
outcomes from cognitive behaviour therapy. Journal of consulting and clinical
psychology, 86(8), 702.
References
Resmark, G., Kennedy, B., Mayer, M., Giel, K., Junne, F., Teufel, M., ... & Zipfel, S. (2018).
Manualised Cognitive Behaviour Therapy for Anorexia Nervosa: Use of Treatment
Modules in the ANTOP Study. Journal of clinical medicine, 7(11), 398.
The Center for Eating Disorder. (2019). The Outpatient Dialectical Behavior Therapy (DBT)
Program. Access date: 6th August 2019. Retrieved from:

11
RESEARCH PAPER
https://eatingdisorder.org/treatment-and-support/specialized-treatment-tracks/
outpatient-dbt-program/
Verywellmind. (2019). Cognitive Behavioral Therapy (CBT). Access date: 6th August 2019.
Retrieved from: https://www.verywellmind.com/what-is-cognitive-behavior-therapy-
2795747
RESEARCH PAPER
https://eatingdisorder.org/treatment-and-support/specialized-treatment-tracks/
outpatient-dbt-program/
Verywellmind. (2019). Cognitive Behavioral Therapy (CBT). Access date: 6th August 2019.
Retrieved from: https://www.verywellmind.com/what-is-cognitive-behavior-therapy-
2795747
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





