Case Study: Colon Cancer Patient Care Plan and Discharge
VerifiedAdded on 2023/06/07
|2
|752
|202
Case Study
AI Summary
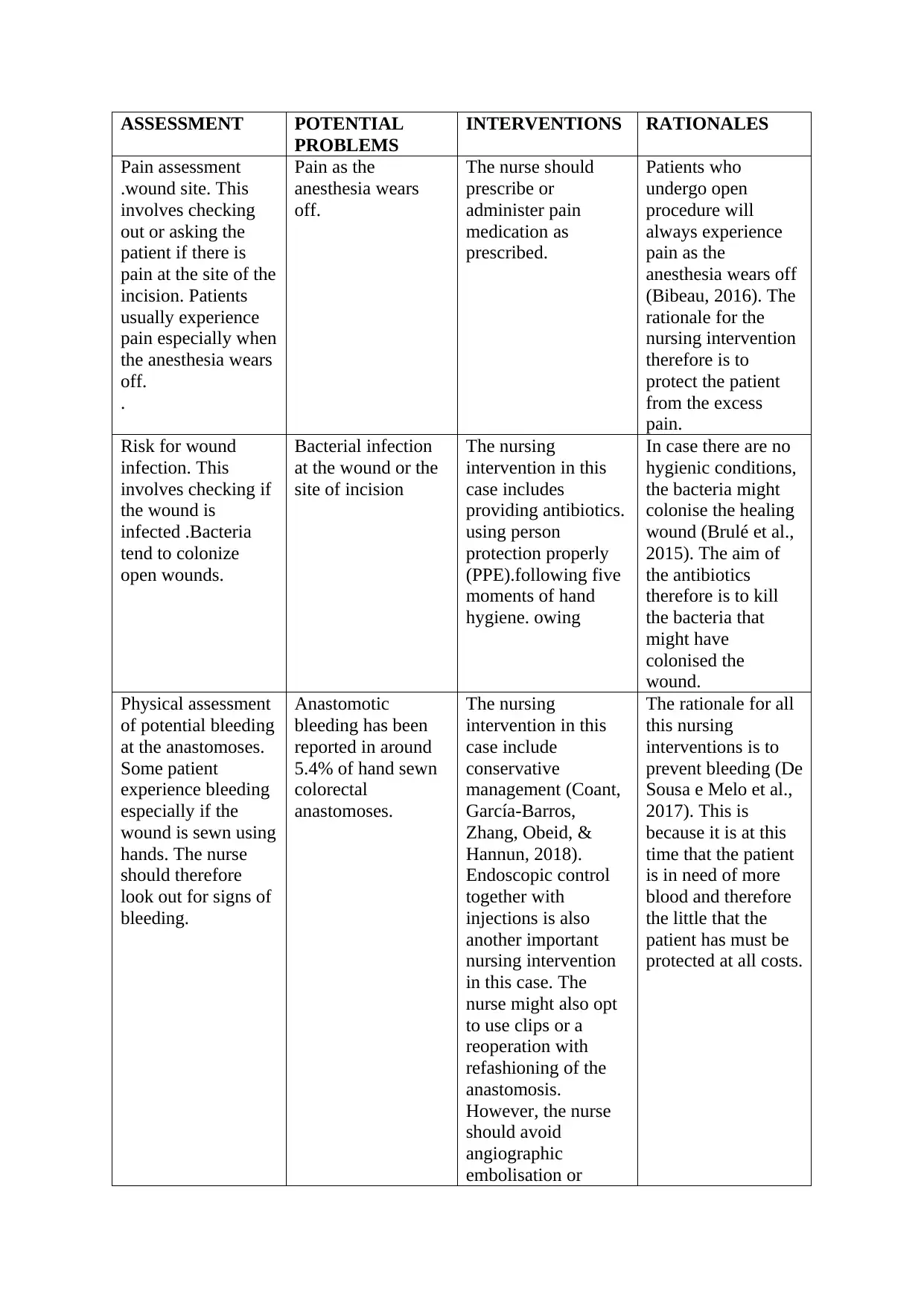
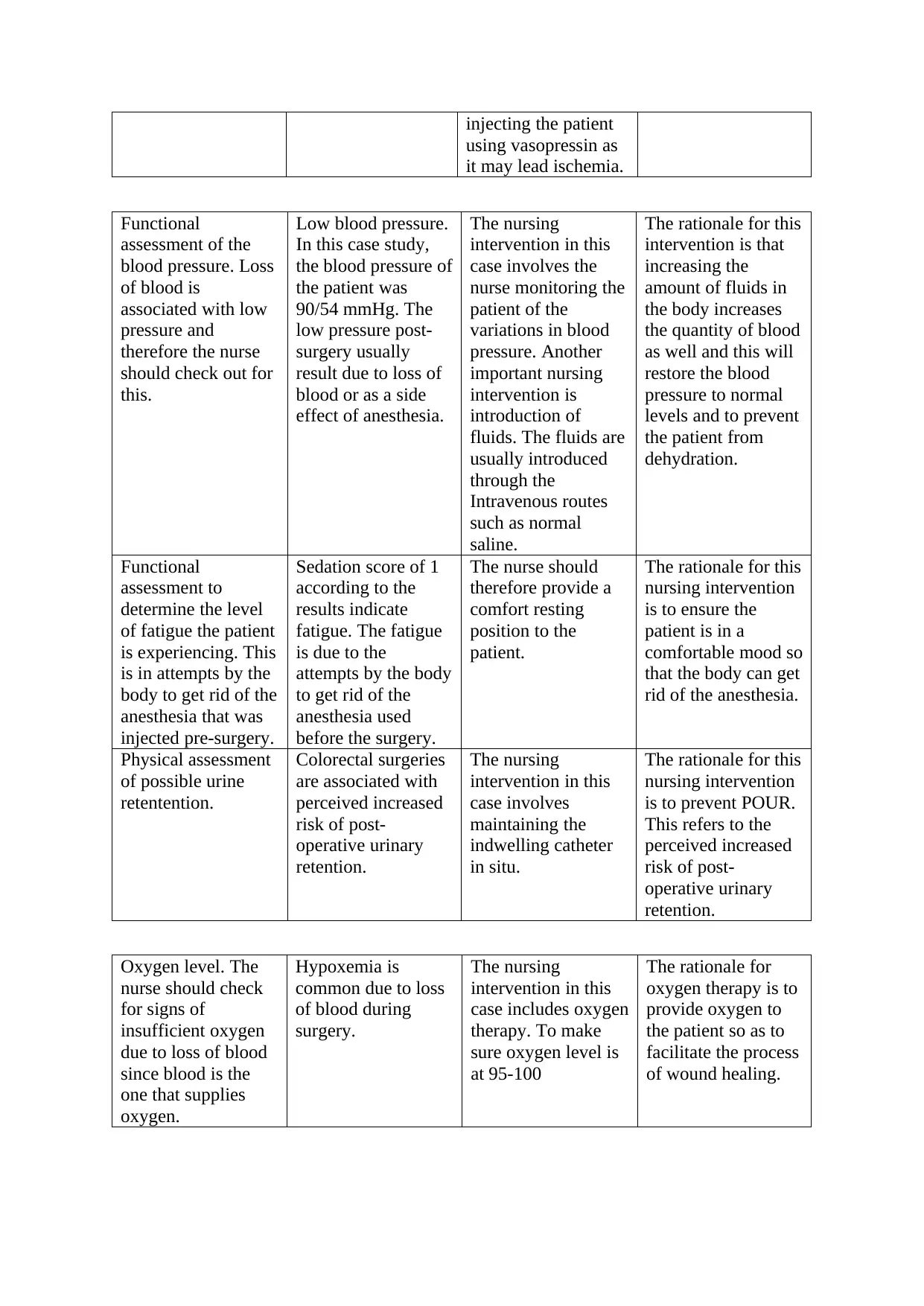
This case study focuses on a patient diagnosed with colon cancer, detailing the assessment of potential problems following surgery. It outlines a comprehensive care plan, addressing issues such as pain management as the anesthesia wears off, the risk of wound infection, potential bleeding, low blood pressure, fatigue, urine retention, and hypoxemia. The interventions include prescribing pain medication, administering antibiotics, monitoring for bleeding, fluid management, oxygen therapy, and maintaining an indwelling catheter. The rationales behind each intervention are provided, emphasizing patient comfort, preventing complications, and promoting healing. The assessment also includes functional assessments of blood pressure, fatigue, and oxygen levels. The study highlights the importance of thorough postoperative care, including a discharge plan to ensure the patient's successful recovery.
1 out of 2






![[object Object]](/_next/static/media/star-bottom.7253800d.svg)