Evaluation of Practice: Communication in Critical Care Nursing
VerifiedAdded on 2023/01/16
|9
|2667
|76
Report
AI Summary
This report provides an evaluation of nursing practice within a critical care setting, specifically focusing on communication strategies for patients requiring ventilation. The report begins with an introduction to evidence-based practice and then identifies a specific area of practice, namely critical care nursing. The PICO format is used to develop a clinical question, and high-level evidence is gathered to answer it. The report compares this evidence to current clinical practices, highlighting differences and recommendations for improvement. Furthermore, it identifies barriers to evidence-based practice within the clinical setting, such as heavy workloads and lack of resources, and proposes strategies to overcome these barriers, including training and monitoring. The conclusion summarizes the key findings and emphasizes the importance of effective communication in improving patient outcomes.
TASK 3- EVALUATION OF
PRACTICE
PRACTICE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
INTRODUCTION...........................................................................................................................1
TASK 1............................................................................................................................................1
Specific area of practice with description....................................................................................1
TAKS 2............................................................................................................................................2
Development of questions using PICO format and search for evidence.....................................2
TAKS 3............................................................................................................................................3
Compare high-level evidence to current practice to clinical practice..........................................3
TASK 4............................................................................................................................................4
Barriers to EBP that exist in clinical setting................................................................................4
Strategies that promote EBP or overcome barriers......................................................................5
CONCLUSION................................................................................................................................5
REFERENCES................................................................................................................................7
INTRODUCTION...........................................................................................................................1
TASK 1............................................................................................................................................1
Specific area of practice with description....................................................................................1
TAKS 2............................................................................................................................................2
Development of questions using PICO format and search for evidence.....................................2
TAKS 3............................................................................................................................................3
Compare high-level evidence to current practice to clinical practice..........................................3
TASK 4............................................................................................................................................4
Barriers to EBP that exist in clinical setting................................................................................4
Strategies that promote EBP or overcome barriers......................................................................5
CONCLUSION................................................................................................................................5
REFERENCES................................................................................................................................7

Evaluation of Practice
INTRODUCTION
Evidence of practise is a kind of practise that relies on evidence for decision making and
guidance. It can also be defined as considering best evidence in decision making in order to
enhance care of patients (Cruccu and Truini, 2017). This assignment will help in focusing on
designing of specific question in the chosen area of clinical practise which nursing in critical care
unit using PICO format, high-level evidence will also be provided in order to answer the
question. Further in this current practise and high-level evidence will be compared in order to
provide clear recommendations to answer the question, further in this assignment barriers to
evidence-based practise will be identified and strategies though which these barriers can be
eliminated.
TASK 1
Specific area of practice with description
Specific area of clinical practise in which I am interested is nursing and even in nursing my
major area of interest is critical care services. Nurses play a vital role in providing critical care
services to the patients. Nurses in critical care team focuses on bringing improvement within
patients with most extreme or critical situation (Carruthers, Astin and Munro, 2017). Nurses who
provide critical care services to extreme situation patients helps in improving patients’ outcomes
in a much better manner. Other than this another interest in provision of care is nursing in
perioperative services in clinical based practise. Nurses within perioperative services provide
quality focused and compassionate care to patients who have undergone or will undergo surgical
procedures. Nurses within this service area are required to quite efficient in surgical techniques,
emergency procedures and medical technology. I am interested in both of these areas of nursing
in clinical practise but majorly I am interested in critical care services because role of nurses in
providing service to patients with critical situation is quite important. Improvement within
patient’s situation completely depend upon the type of services which is provided by the nurses
to them (Fernando, Gray and Gottlieb, 2017). Effectivity and efficiency of nurses and care which
is provided to such patients can enhance their overall treatment outcome.
1
INTRODUCTION
Evidence of practise is a kind of practise that relies on evidence for decision making and
guidance. It can also be defined as considering best evidence in decision making in order to
enhance care of patients (Cruccu and Truini, 2017). This assignment will help in focusing on
designing of specific question in the chosen area of clinical practise which nursing in critical care
unit using PICO format, high-level evidence will also be provided in order to answer the
question. Further in this current practise and high-level evidence will be compared in order to
provide clear recommendations to answer the question, further in this assignment barriers to
evidence-based practise will be identified and strategies though which these barriers can be
eliminated.
TASK 1
Specific area of practice with description
Specific area of clinical practise in which I am interested is nursing and even in nursing my
major area of interest is critical care services. Nurses play a vital role in providing critical care
services to the patients. Nurses in critical care team focuses on bringing improvement within
patients with most extreme or critical situation (Carruthers, Astin and Munro, 2017). Nurses who
provide critical care services to extreme situation patients helps in improving patients’ outcomes
in a much better manner. Other than this another interest in provision of care is nursing in
perioperative services in clinical based practise. Nurses within perioperative services provide
quality focused and compassionate care to patients who have undergone or will undergo surgical
procedures. Nurses within this service area are required to quite efficient in surgical techniques,
emergency procedures and medical technology. I am interested in both of these areas of nursing
in clinical practise but majorly I am interested in critical care services because role of nurses in
providing service to patients with critical situation is quite important. Improvement within
patient’s situation completely depend upon the type of services which is provided by the nurses
to them (Fernando, Gray and Gottlieb, 2017). Effectivity and efficiency of nurses and care which
is provided to such patients can enhance their overall treatment outcome.
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
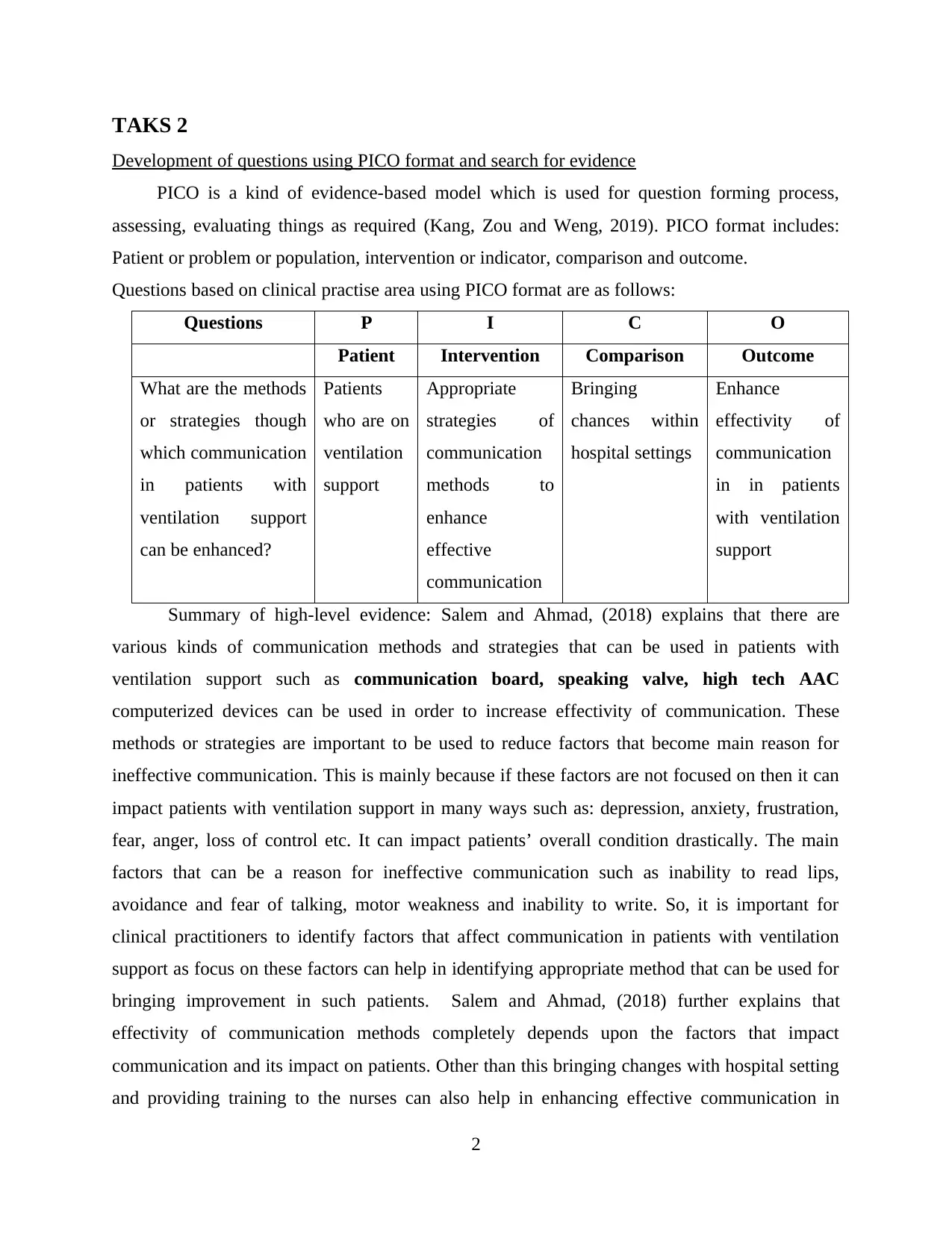
TAKS 2
Development of questions using PICO format and search for evidence
PICO is a kind of evidence-based model which is used for question forming process,
assessing, evaluating things as required (Kang, Zou and Weng, 2019). PICO format includes:
Patient or problem or population, intervention or indicator, comparison and outcome.
Questions based on clinical practise area using PICO format are as follows:
Questions P I C O
Patient Intervention Comparison Outcome
What are the methods
or strategies though
which communication
in patients with
ventilation support
can be enhanced?
Patients
who are on
ventilation
support
Appropriate
strategies of
communication
methods to
enhance
effective
communication
Bringing
chances within
hospital settings
Enhance
effectivity of
communication
in in patients
with ventilation
support
Summary of high-level evidence: Salem and Ahmad, (2018) explains that there are
various kinds of communication methods and strategies that can be used in patients with
ventilation support such as communication board, speaking valve, high tech AAC
computerized devices can be used in order to increase effectivity of communication. These
methods or strategies are important to be used to reduce factors that become main reason for
ineffective communication. This is mainly because if these factors are not focused on then it can
impact patients with ventilation support in many ways such as: depression, anxiety, frustration,
fear, anger, loss of control etc. It can impact patients’ overall condition drastically. The main
factors that can be a reason for ineffective communication such as inability to read lips,
avoidance and fear of talking, motor weakness and inability to write. So, it is important for
clinical practitioners to identify factors that affect communication in patients with ventilation
support as focus on these factors can help in identifying appropriate method that can be used for
bringing improvement in such patients. Salem and Ahmad, (2018) further explains that
effectivity of communication methods completely depends upon the factors that impact
communication and its impact on patients. Other than this bringing changes with hospital setting
and providing training to the nurses can also help in enhancing effective communication in
2
Development of questions using PICO format and search for evidence
PICO is a kind of evidence-based model which is used for question forming process,
assessing, evaluating things as required (Kang, Zou and Weng, 2019). PICO format includes:
Patient or problem or population, intervention or indicator, comparison and outcome.
Questions based on clinical practise area using PICO format are as follows:
Questions P I C O
Patient Intervention Comparison Outcome
What are the methods
or strategies though
which communication
in patients with
ventilation support
can be enhanced?
Patients
who are on
ventilation
support
Appropriate
strategies of
communication
methods to
enhance
effective
communication
Bringing
chances within
hospital settings
Enhance
effectivity of
communication
in in patients
with ventilation
support
Summary of high-level evidence: Salem and Ahmad, (2018) explains that there are
various kinds of communication methods and strategies that can be used in patients with
ventilation support such as communication board, speaking valve, high tech AAC
computerized devices can be used in order to increase effectivity of communication. These
methods or strategies are important to be used to reduce factors that become main reason for
ineffective communication. This is mainly because if these factors are not focused on then it can
impact patients with ventilation support in many ways such as: depression, anxiety, frustration,
fear, anger, loss of control etc. It can impact patients’ overall condition drastically. The main
factors that can be a reason for ineffective communication such as inability to read lips,
avoidance and fear of talking, motor weakness and inability to write. So, it is important for
clinical practitioners to identify factors that affect communication in patients with ventilation
support as focus on these factors can help in identifying appropriate method that can be used for
bringing improvement in such patients. Salem and Ahmad, (2018) further explains that
effectivity of communication methods completely depends upon the factors that impact
communication and its impact on patients. Other than this bringing changes with hospital setting
and providing training to the nurses can also help in enhancing effective communication in
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
patients with ventilation system. As per the view of Holm and Dreyer, (2018) another strategy
that can help in enhancing effective communication is by focus on bringing improvement within
hospital setting or focusing on level of sedation provided to patients, their muscle power,
effective use of tool or technology used for communication such as high-tech AAC
communicative too.
Above question has been answered with the help of nursing journals, articles, books and
previous research papers. Nursing journals, articles and research papers has not only help in
gathering required data to answer these questions in a better manner but it has also help in
analysing the question and factors that can be improve to enhance effective communication.
TAKS 3
Compare high-level evidence to current practice to clinical practice
Currently within current clinical practises communication is one of the most important
things which is required by the nurses to be focused on especially with the patients with
ventilation system support. It has been observed that there are various kinds of issues that are
faced in patients with ventilation support (Hollinger, Harting and Lally, 2017). Most of the times
in clinical practises communication board is used to enhance or improve communication in
patients specifically patients with ventilation system support and further if there is requirement to
bring improvement within communication then changes within hospital or clinical settings are
done. But according to the high-level evidence that has been gathered there are many more ways
to bring improvement within communication in patients with ventilation system such as speaking
valve, high tech AAC communication board. But high-tech evidence collected also explains that
effectiveness of type of communication method or strategies used completely depends upon the
factors of ineffective communication and their impact on patients. According to the evidence
gathered resolving ore reducing factors of ineffective communication can also help in enhancing
chances of improvement within effectivity of communication. One of the major differences
between current clinical practise and evidence-based practise is that in clinical practises does not
focus on using high tech technology to improve effective communication. As per the findings of
high level evidence it has been observed that one of the main strategy that can be used by clinical
practitioners is to reduce factors that makes communication ineffective and after reducing such
factors efficiency of communication methods increases that can also help patients to improve
their overall treatment outcome in a much better manner. improving communication can also
3
that can help in enhancing effective communication is by focus on bringing improvement within
hospital setting or focusing on level of sedation provided to patients, their muscle power,
effective use of tool or technology used for communication such as high-tech AAC
communicative too.
Above question has been answered with the help of nursing journals, articles, books and
previous research papers. Nursing journals, articles and research papers has not only help in
gathering required data to answer these questions in a better manner but it has also help in
analysing the question and factors that can be improve to enhance effective communication.
TAKS 3
Compare high-level evidence to current practice to clinical practice
Currently within current clinical practises communication is one of the most important
things which is required by the nurses to be focused on especially with the patients with
ventilation system support. It has been observed that there are various kinds of issues that are
faced in patients with ventilation support (Hollinger, Harting and Lally, 2017). Most of the times
in clinical practises communication board is used to enhance or improve communication in
patients specifically patients with ventilation system support and further if there is requirement to
bring improvement within communication then changes within hospital or clinical settings are
done. But according to the high-level evidence that has been gathered there are many more ways
to bring improvement within communication in patients with ventilation system such as speaking
valve, high tech AAC communication board. But high-tech evidence collected also explains that
effectiveness of type of communication method or strategies used completely depends upon the
factors of ineffective communication and their impact on patients. According to the evidence
gathered resolving ore reducing factors of ineffective communication can also help in enhancing
chances of improvement within effectivity of communication. One of the major differences
between current clinical practise and evidence-based practise is that in clinical practises does not
focus on using high tech technology to improve effective communication. As per the findings of
high level evidence it has been observed that one of the main strategy that can be used by clinical
practitioners is to reduce factors that makes communication ineffective and after reducing such
factors efficiency of communication methods increases that can also help patients to improve
their overall treatment outcome in a much better manner. improving communication can also
3

help in increasing patient satisfaction level for the treatment as well. Other than this providing
special training to the nurses of critical care unit can also help in enhancing communication in
patients who are on ventilating system support.
Few of the most common evidence-based recommendations for improving communication
in patients with ventilation system are: to reduce factors of ineffective communication, eliminate
negative impact of ineffective communication, use of high-tech technology like AAC
communication boards. There are many clinical practitioners that uses these kind of
communication boards to improve communication in patients with ventilation system. But there
is no clear evidence that can help in explaining that reducing factors of ineffective
communication can help in enhancing effective communication. No doubt the resolving or
reducing these factors can help in reducing inefficiency but it can also help in increasing
efficiency is not clear. Many researchers have been done in this field but none of them clearly
explains that these factors can improve communication. So, it can be said that it is poor quality
of evidence as there is no such proof of this evidence. It is only a theory that that claims that
resolving ineffective communication factors or changing hospital settings can improve
communication with patients with ventilation support. But there are many evidences that proves
that using advance technology communication methods or tools can help in improving
communication in patients with ventilation support. This recommendation can be used by
clinical practitioners to enhance their communication in patients with ventilation support.
TASK 4
Barriers to EBP that exist in clinical setting
There are various kinds of barriers that exist and can prevent use of evidence-based
practise (Asehnoune, Roquilly and Cinotti, 2018). Some of the most common barriers to
evidence-based practise that can become a barrier for nurses of critical care unit and can affect
effective communication in patients with ventilation support are: one of the main barriers that
exist if high workload. Heavy workload can reduce efficiency of nurses in critical care unit
because of which efficiency of effective communication in patients who are on ventilator
systems. Due to heavy workload they would spend less time on patients as their main focus will
be on fulfilling all of their roles and responsibilities in a much better and efficient manner.
Another barrier is lack of experience staff in EBP (Joyce, Berg and Bittner, 2017). It is extremely
important for nurses present in critical care unit to be experienced as experienced nurses will be
4
special training to the nurses of critical care unit can also help in enhancing communication in
patients who are on ventilating system support.
Few of the most common evidence-based recommendations for improving communication
in patients with ventilation system are: to reduce factors of ineffective communication, eliminate
negative impact of ineffective communication, use of high-tech technology like AAC
communication boards. There are many clinical practitioners that uses these kind of
communication boards to improve communication in patients with ventilation system. But there
is no clear evidence that can help in explaining that reducing factors of ineffective
communication can help in enhancing effective communication. No doubt the resolving or
reducing these factors can help in reducing inefficiency but it can also help in increasing
efficiency is not clear. Many researchers have been done in this field but none of them clearly
explains that these factors can improve communication. So, it can be said that it is poor quality
of evidence as there is no such proof of this evidence. It is only a theory that that claims that
resolving ineffective communication factors or changing hospital settings can improve
communication with patients with ventilation support. But there are many evidences that proves
that using advance technology communication methods or tools can help in improving
communication in patients with ventilation support. This recommendation can be used by
clinical practitioners to enhance their communication in patients with ventilation support.
TASK 4
Barriers to EBP that exist in clinical setting
There are various kinds of barriers that exist and can prevent use of evidence-based
practise (Asehnoune, Roquilly and Cinotti, 2018). Some of the most common barriers to
evidence-based practise that can become a barrier for nurses of critical care unit and can affect
effective communication in patients with ventilation support are: one of the main barriers that
exist if high workload. Heavy workload can reduce efficiency of nurses in critical care unit
because of which efficiency of effective communication in patients who are on ventilator
systems. Due to heavy workload they would spend less time on patients as their main focus will
be on fulfilling all of their roles and responsibilities in a much better and efficient manner.
Another barrier is lack of experience staff in EBP (Joyce, Berg and Bittner, 2017). It is extremely
important for nurses present in critical care unit to be experienced as experienced nurses will be
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

able to communicate with the patients in a much effective manner. Another one of the main
barriers is lack of required resources in EBP. In order to increase effectivity of efficient
communication in patients it is important to have all kinds of required resources (Sharpe and
Hemsley, 2016). For example, if resources kind communication board or high-tech AAC
communication board is required by patients with ventilation support but such kinds of resources
are not available then inefficiency of communication in such patients can increase which can
impact them in a negative manner and can also impact their treatment outcome. There is one
more barrier that exist among nurses of critical care unit is lack of knowledge i.e. many times
nurses do not have required knowledge to access resources to enhance communication or they
are not trained well or are not provided much knowledge about ways to enhance communication
in patients with ventilation support.
Strategies that promote EBP or overcome barriers
There are various strategies that can be used to overcome above specified barriers and
promote EBP in nurses in critical care unit. One of the most commonly used strategy that can
help in overcoming barriers for nurses in critical care unit is to provide them with required
training (Joyce, Berg and Bittner, 2017). Providing appropriate training to nurses in this clinical
setting can help in enhancing their knowledge so that they can get to know about the resources
available or strategies that can be used by them to enhance effectivity of communication in
patients. Another strategy that can be used to overcome these barriers is conducting nursing
programs where nurses in critical care unit can attend such nursing programs so that they can
develop required skills that will be required them to attend their patients in a much better
manner. monitoring nurse’s performance and providing them with feedback can also help in
improving communication in patients who are on ventilator support. Monitoring their
performance will help their seniors to identify areas that are required to be developed or worked
on within nurses (Ranieri, Brodie and Vincent, 2017). Providing feedbacks to the nurses will
help them to understand areas where they lack so that if there is requirements to enhance their
skills or knowledge then they can work on themselves in order to bring improvement within
themselves and work on enhancing effective communication in patients.
CONCLUSION
From the above assignment it has been summarized that there are various ways through
which effective communication in patients with ventilators can be improved, however, there are
5
barriers is lack of required resources in EBP. In order to increase effectivity of efficient
communication in patients it is important to have all kinds of required resources (Sharpe and
Hemsley, 2016). For example, if resources kind communication board or high-tech AAC
communication board is required by patients with ventilation support but such kinds of resources
are not available then inefficiency of communication in such patients can increase which can
impact them in a negative manner and can also impact their treatment outcome. There is one
more barrier that exist among nurses of critical care unit is lack of knowledge i.e. many times
nurses do not have required knowledge to access resources to enhance communication or they
are not trained well or are not provided much knowledge about ways to enhance communication
in patients with ventilation support.
Strategies that promote EBP or overcome barriers
There are various strategies that can be used to overcome above specified barriers and
promote EBP in nurses in critical care unit. One of the most commonly used strategy that can
help in overcoming barriers for nurses in critical care unit is to provide them with required
training (Joyce, Berg and Bittner, 2017). Providing appropriate training to nurses in this clinical
setting can help in enhancing their knowledge so that they can get to know about the resources
available or strategies that can be used by them to enhance effectivity of communication in
patients. Another strategy that can be used to overcome these barriers is conducting nursing
programs where nurses in critical care unit can attend such nursing programs so that they can
develop required skills that will be required them to attend their patients in a much better
manner. monitoring nurse’s performance and providing them with feedback can also help in
improving communication in patients who are on ventilator support. Monitoring their
performance will help their seniors to identify areas that are required to be developed or worked
on within nurses (Ranieri, Brodie and Vincent, 2017). Providing feedbacks to the nurses will
help them to understand areas where they lack so that if there is requirements to enhance their
skills or knowledge then they can work on themselves in order to bring improvement within
themselves and work on enhancing effective communication in patients.
CONCLUSION
From the above assignment it has been summarized that there are various ways through
which effective communication in patients with ventilators can be improved, however, there are
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
n such clear evidences that can be used to support and answer the question. It has also been
analysed that it is important to have strong proof for evidence-based practise in order to answer
the question. It has also been analysed that there are various kinds of barriers to evidence-based
practise that can impact effective communication in chosen clinical setting. However, there are
various kinds of strategies that can be used to promote EBP in nursing in critical care unit.
6
analysed that it is important to have strong proof for evidence-based practise in order to answer
the question. It has also been analysed that there are various kinds of barriers to evidence-based
practise that can impact effective communication in chosen clinical setting. However, there are
various kinds of strategies that can be used to promote EBP in nursing in critical care unit.
6
REFERENCES
Books and Journals
Asehnoune, K., Roquilly, A. and Cinotti, R., 2018. Respiratory management in patients with
severe brain injury. Critical Care. 22(1). p.76.
Carruthers, H., Astin, F. and Munro, W., 2017. Which alternative communication methods are
effective for voiceless patients in Intensive Care Units? A systematic review. Intensive
and Critical Care Nursing. 42. pp.88-96.
Cruccu, G. and Truini, A., 2017. A review of neuropathic pain: from guidelines to clinical
practice. Pain and therapy. 6(1). pp.35-42.
Fernando, S.A., Gray, T.J. and Gottlieb, T., 2017. Healthcare‐acquired infections: prevention
strategies. Internal medicine journal. 47(12). pp.1341-1351.
Hollinger, L.E., Harting, M.T. and Lally, K.P., 2017, June. Long-term follow-up of congenital
diaphragmatic hernia. In Seminars in pediatric surgery (Vol. 26, No. 3, pp. 178-184).
WB Saunders.
Holm, A. and Dreyer, P., 2018. Nurse‐patient communication within the context of non‐sedated
mechanical ventilation: A hermeneutic‐phenomenological study. Nursing in critical care.
23(2). pp.88-94.
Joyce, M.F., Berg, S. and Bittner, E.A., 2017. Practical strategies for increasing efficiency and
effectiveness in critical care education. World journal of critical care medicine. 6(1). p.1.
Kang, T., Zou, S. and Weng, C., 2019. Pretraining to Recognize PICO Elements from
Randomized Controlled Trial Literature. Studies in health technology and informatics.
264. p.188.
Ranieri, V.M., Brodie, D. and Vincent, J.L., 2017. Extracorporeal organ support: from
technological tool to clinical strategy supporting severe organ failure. Jama. 318(12).
pp.1105-1106.
Salem, A. and Ahmad, M.M., 2018. Communication with invasive mechanically ventilated
patients and the use of alternative devices: integrative review. Journal of Research in
Nursing. 23(7). pp.614-630.
Sharpe, B. and Hemsley, B., 2016. Improving nurse–patient communication with patients with
communication impairments: hospital nurses' views on the feasibility of using mobile
communication technologies. Applied nursing research. 30. pp.228-236.
7
Books and Journals
Asehnoune, K., Roquilly, A. and Cinotti, R., 2018. Respiratory management in patients with
severe brain injury. Critical Care. 22(1). p.76.
Carruthers, H., Astin, F. and Munro, W., 2017. Which alternative communication methods are
effective for voiceless patients in Intensive Care Units? A systematic review. Intensive
and Critical Care Nursing. 42. pp.88-96.
Cruccu, G. and Truini, A., 2017. A review of neuropathic pain: from guidelines to clinical
practice. Pain and therapy. 6(1). pp.35-42.
Fernando, S.A., Gray, T.J. and Gottlieb, T., 2017. Healthcare‐acquired infections: prevention
strategies. Internal medicine journal. 47(12). pp.1341-1351.
Hollinger, L.E., Harting, M.T. and Lally, K.P., 2017, June. Long-term follow-up of congenital
diaphragmatic hernia. In Seminars in pediatric surgery (Vol. 26, No. 3, pp. 178-184).
WB Saunders.
Holm, A. and Dreyer, P., 2018. Nurse‐patient communication within the context of non‐sedated
mechanical ventilation: A hermeneutic‐phenomenological study. Nursing in critical care.
23(2). pp.88-94.
Joyce, M.F., Berg, S. and Bittner, E.A., 2017. Practical strategies for increasing efficiency and
effectiveness in critical care education. World journal of critical care medicine. 6(1). p.1.
Kang, T., Zou, S. and Weng, C., 2019. Pretraining to Recognize PICO Elements from
Randomized Controlled Trial Literature. Studies in health technology and informatics.
264. p.188.
Ranieri, V.M., Brodie, D. and Vincent, J.L., 2017. Extracorporeal organ support: from
technological tool to clinical strategy supporting severe organ failure. Jama. 318(12).
pp.1105-1106.
Salem, A. and Ahmad, M.M., 2018. Communication with invasive mechanically ventilated
patients and the use of alternative devices: integrative review. Journal of Research in
Nursing. 23(7). pp.614-630.
Sharpe, B. and Hemsley, B., 2016. Improving nurse–patient communication with patients with
communication impairments: hospital nurses' views on the feasibility of using mobile
communication technologies. Applied nursing research. 30. pp.228-236.
7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




