NURSING 6: University Dissertation: COPD Patient Service Innovation
VerifiedAdded on 2022/10/12
|34
|10757
|51
Report
AI Summary
This assignment delves into patient service innovation within the context of COPD, focusing on a community-based intervention designed to reduce hospital readmission rates. The report begins with an introduction to patient service innovation and its importance in healthcare, particularly within the NHS framework. It explores the challenges faced by the NHS, including funding, staffing, and evolving healthcare demands. The report then outlines a project plan for a community-based intervention, a change management strategy to facilitate its implementation, and a leadership theory suitable for guiding the project. It highlights the significance of clinical governance principles and their role in improving patient care. The assignment also examines the role of nurses in this innovation, emphasizing their contributions to patient outcomes and service improvement. Furthermore, the assignment presents a theoretical background on the NHS, challenges faced, and clinical governance, which will be followed by how change management model will help to put the innovation into practice. Time management will also be explained in this essay, which will predict how long it will take to plan, realize and assess the innovation. Finally, the role of the nurse in innovation will also be explored in the essay.

Running head: NURSING
Patient Service innovation – Dissertation
Name of the Student
Name of the University
Author Note
Patient Service innovation – Dissertation
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
Part 1
Introduction
Patient service innovation refers to strategies that are adopted by the
healthcare organization and health department for continuous enhancement of
patient satisfaction and are generally promoted with the aim of enhancing patient
health outcomes. Furthermore, public sponsored healthcare has also been identified
as a crucial aspect of health innovation on a national and local level. Time and again
it has been proved that bringing about improvement in patient care has been
identified as a major priority for different healthcare providers who have the chief
objective of enhancing patient satisfaction (Dandoyet al. 2017). Furthermore, an
increase in awareness among the public, snowballingmandate for better care,
profound competition, increase in number of health care regulation, the growth in
medical misconduct litigation, and anxiety about poor health outcomes are some of
the factors that significantly contribute to patient service innovation.
The patient service innovation that will be discussed in the assignment
focuses on reducing the recurrent hospital admissions amid patients who suffer from
COPD.
The patient innovation program focuses on making the COPD affected
individuals use community service for lowering their admission rates. There are
several community services available for patients suffering from COPD that focus on
altering their behaviour, helping them deal with the physical and emotional impact of
the disease, and medication management. However, it has been found that not
many patients seek help from these community services, thus calling for the need of
implementing patient service innovation. Therefore, the service that will be discussed
in this assignment focuses on a community-based intervention that will address the
healthcare needs of patients who are suffering from COPD, thus lowering their
admission rates in healthcare settings. This assignment will contain a project plan,
followed by a suitable change management strategy, and leadership theory that fits
the intended project. Furthermore, the assignment will also elaborate on the role of
nurses in service innovation. This assignment will be divided in to two sections. The
first section will elaborate on the theory and include the general idea of the NHS and
contemporary challenges. The major principles of clinical governance and their role
Part 1
Introduction
Patient service innovation refers to strategies that are adopted by the
healthcare organization and health department for continuous enhancement of
patient satisfaction and are generally promoted with the aim of enhancing patient
health outcomes. Furthermore, public sponsored healthcare has also been identified
as a crucial aspect of health innovation on a national and local level. Time and again
it has been proved that bringing about improvement in patient care has been
identified as a major priority for different healthcare providers who have the chief
objective of enhancing patient satisfaction (Dandoyet al. 2017). Furthermore, an
increase in awareness among the public, snowballingmandate for better care,
profound competition, increase in number of health care regulation, the growth in
medical misconduct litigation, and anxiety about poor health outcomes are some of
the factors that significantly contribute to patient service innovation.
The patient service innovation that will be discussed in the assignment
focuses on reducing the recurrent hospital admissions amid patients who suffer from
COPD.
The patient innovation program focuses on making the COPD affected
individuals use community service for lowering their admission rates. There are
several community services available for patients suffering from COPD that focus on
altering their behaviour, helping them deal with the physical and emotional impact of
the disease, and medication management. However, it has been found that not
many patients seek help from these community services, thus calling for the need of
implementing patient service innovation. Therefore, the service that will be discussed
in this assignment focuses on a community-based intervention that will address the
healthcare needs of patients who are suffering from COPD, thus lowering their
admission rates in healthcare settings. This assignment will contain a project plan,
followed by a suitable change management strategy, and leadership theory that fits
the intended project. Furthermore, the assignment will also elaborate on the role of
nurses in service innovation. This assignment will be divided in to two sections. The
first section will elaborate on the theory and include the general idea of the NHS and
contemporary challenges. The major principles of clinical governance and their role
2NURSING
in service improvement, quality improvement and clinical excellence will be also ne
discussed in this section. Part two will talk about how change management model
will help to put the innovation into practice. Time management will also be explained
in this essay, which will predict how long it will take to plan, realize and assess the
innovation. Finally, the role of the nurse in innovation will also be explored in the
essay.
Theory
The National Health Service (NHS) was created in England and refers to
a publicly subsidisednation-wide healthcare system and is one of the four NHS that
have been formulated for each constituent nation of the United Kingdom. The
foundation of this organisation can be associated to the enforcement of the National
Health Service Act 1946 on 5 July 1948 (Grimes 2016). Presence of a
national health service had been identified as an important expectation in
the Beveridge Report(Siddall2018). In addition, the establishment of the Emergency
Hospital Service in 1939 provided a clear overview of what the NHS would comprise
of. The initial structure of the NHS encompassed three crucial aspects namely, (i)
hospital services, (ii) primary care, and (iii) community services. The core principles
of the NHS that govern the delivery of healthcare facilities in England are based on
the long-held assumption that excellent quality healthcare must be available to every
resident, regardless of prosperity and socioeconomic condition (Guest et al. 2015).
Furthermore, some additional principles that also govern the work of NHS, in relation
to delivery of optimal healthcare services are namely, (i) care, (ii) communication, (iii)
compassion, (iv) competence, (v) commitment, and (vi) courage to be inadequate
(Lancet 2018). Furthermore, an early COPD diagnosis is often challenging for the
healthcare professionals, since patients who are affected with mild COPD, in
addition to smoker’s cough are not diagnosed properly (NHS England 2013).
in service improvement, quality improvement and clinical excellence will be also ne
discussed in this section. Part two will talk about how change management model
will help to put the innovation into practice. Time management will also be explained
in this essay, which will predict how long it will take to plan, realize and assess the
innovation. Finally, the role of the nurse in innovation will also be explored in the
essay.
Theory
The National Health Service (NHS) was created in England and refers to
a publicly subsidisednation-wide healthcare system and is one of the four NHS that
have been formulated for each constituent nation of the United Kingdom. The
foundation of this organisation can be associated to the enforcement of the National
Health Service Act 1946 on 5 July 1948 (Grimes 2016). Presence of a
national health service had been identified as an important expectation in
the Beveridge Report(Siddall2018). In addition, the establishment of the Emergency
Hospital Service in 1939 provided a clear overview of what the NHS would comprise
of. The initial structure of the NHS encompassed three crucial aspects namely, (i)
hospital services, (ii) primary care, and (iii) community services. The core principles
of the NHS that govern the delivery of healthcare facilities in England are based on
the long-held assumption that excellent quality healthcare must be available to every
resident, regardless of prosperity and socioeconomic condition (Guest et al. 2015).
Furthermore, some additional principles that also govern the work of NHS, in relation
to delivery of optimal healthcare services are namely, (i) care, (ii) communication, (iii)
compassion, (iv) competence, (v) commitment, and (vi) courage to be inadequate
(Lancet 2018). Furthermore, an early COPD diagnosis is often challenging for the
healthcare professionals, since patients who are affected with mild COPD, in
addition to smoker’s cough are not diagnosed properly (NHS England 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
Figure 1- 7 pillars of clinical governance
Source- (Routes Healthcare 2019)
Nonetheless, the NHS is facing several challenges in recent times. Some of
the key challenges that the NHS is currently facing are namely, (i) lack of adequate
funding, (ii) shortage of staffing, (iii) exit of the British from the European Union, (iv)
increase in social care costs, (v) evolving healthcare demands and needs, (vi)
centralisation drives that are causing closure of local health services, and (vii)
increased reliance of the public on privatised healthcare services (Mossialos et al.
2016). During the launch of the NHS in 1948 it had a financial plan of £437 million
(approximately £9 billion according to current price), which eventually increased to
£122.5 billion in 2016-17 (Burch 2019). Furthermore, the health spending was an
estimated 11.2% during 1955-56 that increased to a massive 29.7% during 2015-16
(Triggle 2017). Evidences also highlight the fact that the NHS performs well while
protecting individuals from huge monetary costs at the time of their illness (Pitchforth
et al. 2017).
As per the Griffiths Report outline, clinicians were expected to be more
involvement in patient management (Klein 2019). This report resulted in a major
change in the managerial culture in NHS. The organisation underwent several
changes in the past seven decades and is under the process of continuous evolution
(Ham 2018).The Berwick Report was another essential step in identification of the
significance of constant watchfulness, watching and knowledge acquisition to make
Figure 1- 7 pillars of clinical governance
Source- (Routes Healthcare 2019)
Nonetheless, the NHS is facing several challenges in recent times. Some of
the key challenges that the NHS is currently facing are namely, (i) lack of adequate
funding, (ii) shortage of staffing, (iii) exit of the British from the European Union, (iv)
increase in social care costs, (v) evolving healthcare demands and needs, (vi)
centralisation drives that are causing closure of local health services, and (vii)
increased reliance of the public on privatised healthcare services (Mossialos et al.
2016). During the launch of the NHS in 1948 it had a financial plan of £437 million
(approximately £9 billion according to current price), which eventually increased to
£122.5 billion in 2016-17 (Burch 2019). Furthermore, the health spending was an
estimated 11.2% during 1955-56 that increased to a massive 29.7% during 2015-16
(Triggle 2017). Evidences also highlight the fact that the NHS performs well while
protecting individuals from huge monetary costs at the time of their illness (Pitchforth
et al. 2017).
As per the Griffiths Report outline, clinicians were expected to be more
involvement in patient management (Klein 2019). This report resulted in a major
change in the managerial culture in NHS. The organisation underwent several
changes in the past seven decades and is under the process of continuous evolution
(Ham 2018).The Berwick Report was another essential step in identification of the
significance of constant watchfulness, watching and knowledge acquisition to make
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
sure that the patients were kept distant from any kind of avoidable harm (Gov.UK
2013).
The NHS Reorganisation Act also resulted in setting up of local NHS bodies
that had the responsibility of managing all community and general health services
(Lale and Temple 2016). Moreover, health disparities are still on the plan and
continue as a key precedence for public health services. This has eventually resulted
in the ‘Forward View’ assessment where some of the future strategies of the NHS
have been highlighted such as, (i) better health, (ii) better care, and (iii) financial
sustainability (NHS 2017). Furthermore, the King’s Fund is an independent public
health thinktank that focuses on health-related work in England. Moreover, efforts
are also been taken by the organisation for shaping practice and policy through
analysis and research (Ham 2018). According to the King’s Fund (2013) the national
leaders must be given credit for addressing quantifiable developments in health
outcomes.The King’s Fund has some values that underpin the work towards
excellence of care. It displays a commitment for maintaining independence, while
promoting collaborative practice and striving for excellence. The King’s fund also
states that management of care for individuals suffering from long-term health
complications must be holistic, preventive, proactive, and patient centred. Taking into
consideration the fact that there are almost 15 million individuals in England who
have been diagnosed with one or more long-term health condition, it is imperative to
implement personalised care planning where the patients and clinicians work
together for identifying the support needs and reaching a consensus (The King’s
Fund 2013).
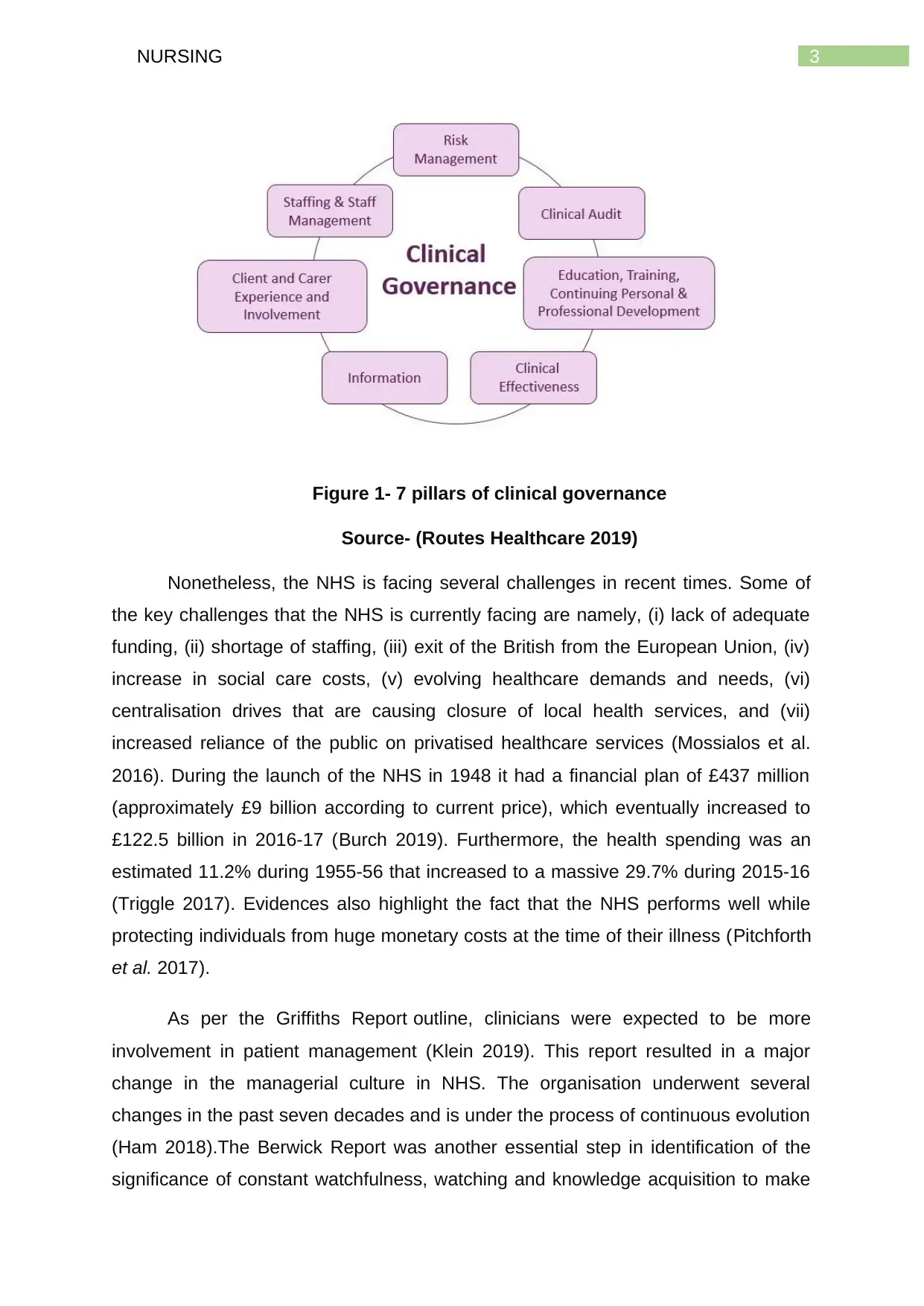
Some of the chief principles of clinical governance that have been associated
with high quality patient care are (a) training, education, and continuous professional
development, (b) evidence-based care, (c) patient and carer involvement and
experience, and (d) staff management (Donaldson 2018). It came into effect after the
Bristol heart scandalof 1995 and is defined as the framework through which NHS
organisations are answerable for repeatedlyrefining the quality of their care services,
while protecting high care standards by creating a setting in which superiority in
clinical care will display (Fox 2001).If clinical governance is to really function
successfully as a methodical approach to upholding and enhancing the excellence of
patient care in a health organisation, it necessitates advocates (Walshe and
sure that the patients were kept distant from any kind of avoidable harm (Gov.UK
2013).
The NHS Reorganisation Act also resulted in setting up of local NHS bodies
that had the responsibility of managing all community and general health services
(Lale and Temple 2016). Moreover, health disparities are still on the plan and
continue as a key precedence for public health services. This has eventually resulted
in the ‘Forward View’ assessment where some of the future strategies of the NHS
have been highlighted such as, (i) better health, (ii) better care, and (iii) financial
sustainability (NHS 2017). Furthermore, the King’s Fund is an independent public
health thinktank that focuses on health-related work in England. Moreover, efforts
are also been taken by the organisation for shaping practice and policy through
analysis and research (Ham 2018). According to the King’s Fund (2013) the national
leaders must be given credit for addressing quantifiable developments in health
outcomes.The King’s Fund has some values that underpin the work towards
excellence of care. It displays a commitment for maintaining independence, while
promoting collaborative practice and striving for excellence. The King’s fund also
states that management of care for individuals suffering from long-term health
complications must be holistic, preventive, proactive, and patient centred. Taking into
consideration the fact that there are almost 15 million individuals in England who
have been diagnosed with one or more long-term health condition, it is imperative to
implement personalised care planning where the patients and clinicians work
together for identifying the support needs and reaching a consensus (The King’s
Fund 2013).
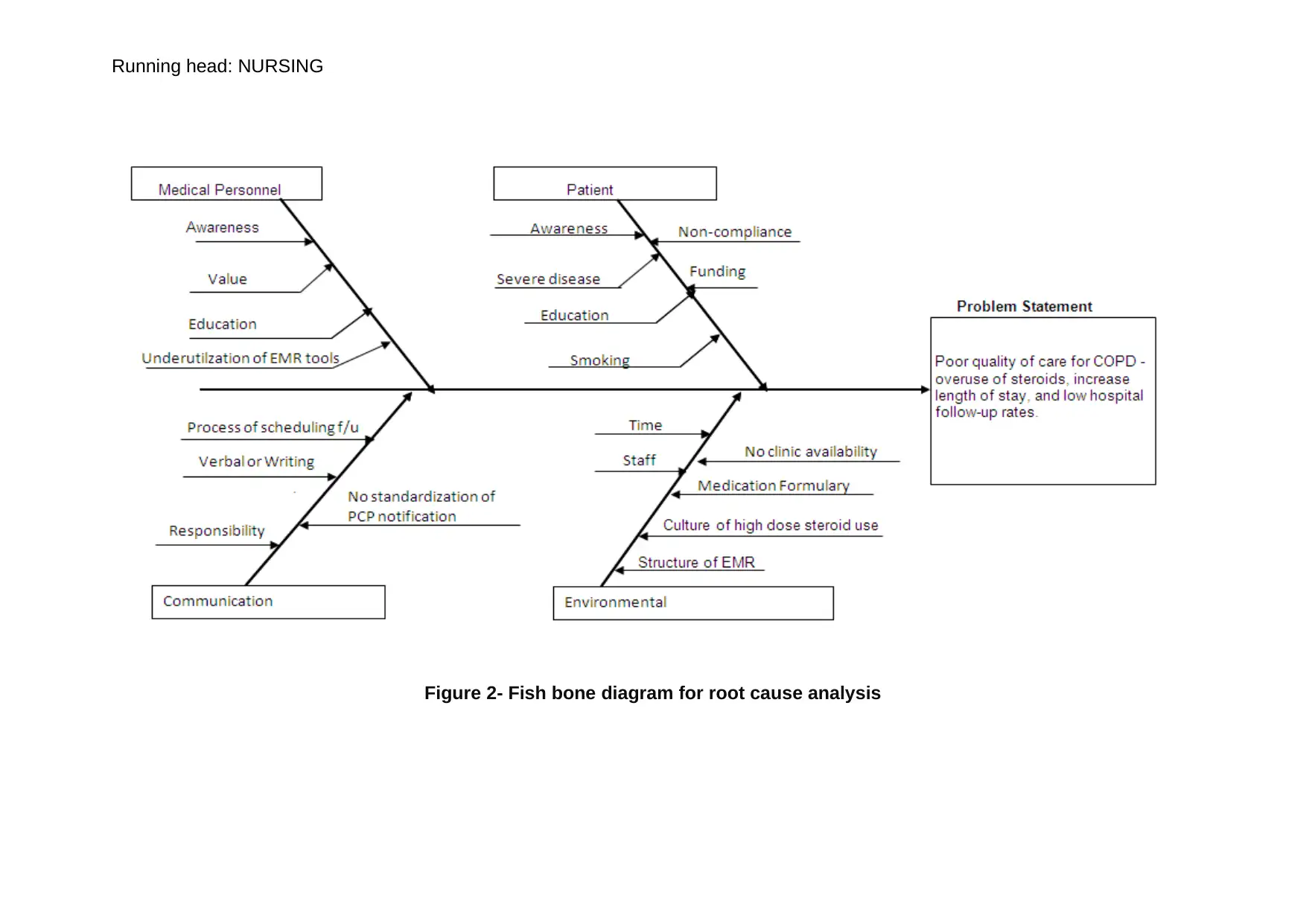
Some of the chief principles of clinical governance that have been associated
with high quality patient care are (a) training, education, and continuous professional
development, (b) evidence-based care, (c) patient and carer involvement and
experience, and (d) staff management (Donaldson 2018). It came into effect after the
Bristol heart scandalof 1995 and is defined as the framework through which NHS
organisations are answerable for repeatedlyrefining the quality of their care services,
while protecting high care standards by creating a setting in which superiority in
clinical care will display (Fox 2001).If clinical governance is to really function
successfully as a methodical approach to upholding and enhancing the excellence of
patient care in a health organisation, it necessitates advocates (Walshe and
5NURSING
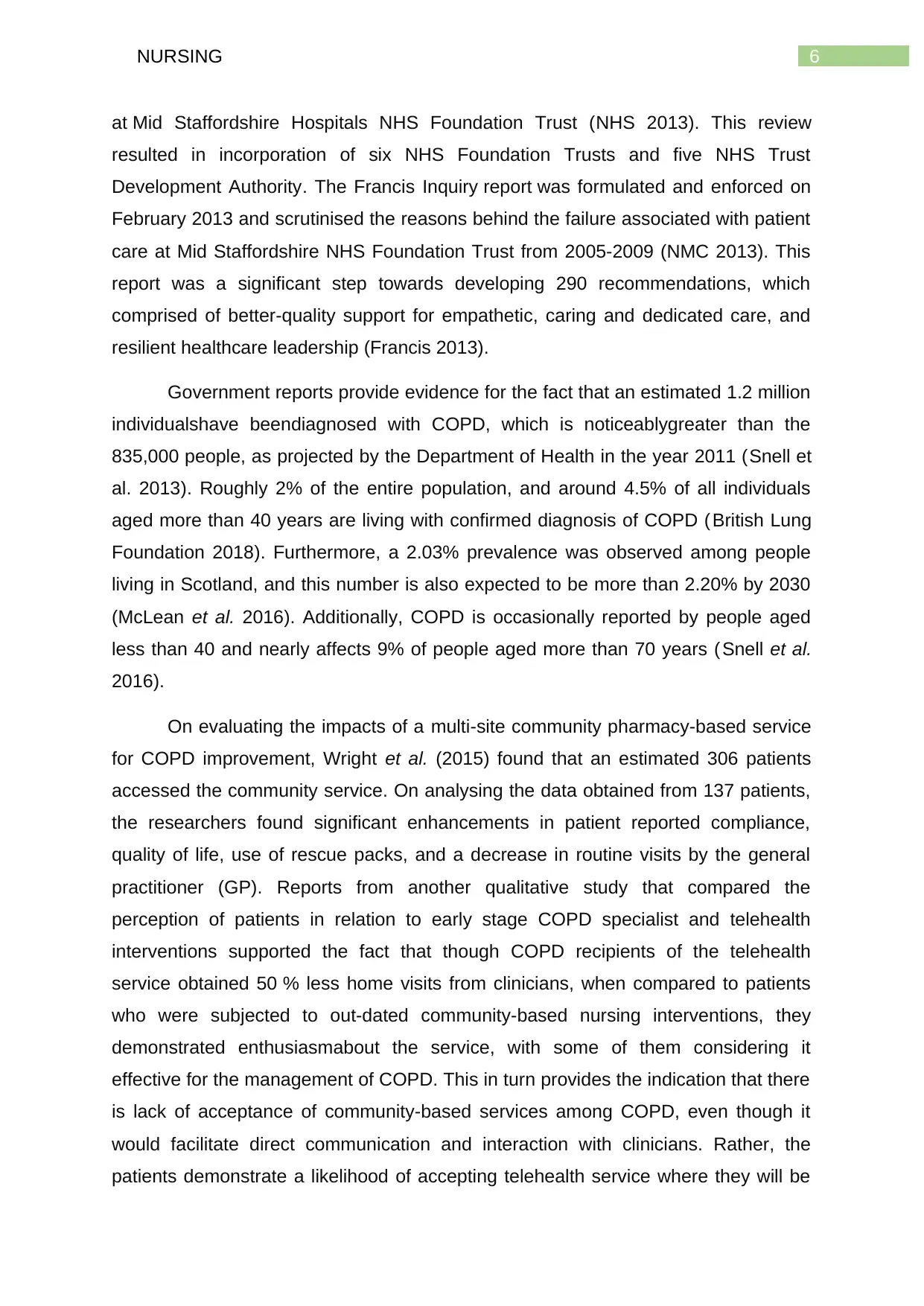
Chambers 2017). Furthermore, the NHS Outcomes Framework (NHS OF) has also
been developed in the form of several indicators by the Department of Health and
Social Care, with the aim of monitoring health outcomes of children and adults in
England (Roland and Guthrie 2016).
This in turn can be accomplished by implementing the NHS Healthcare
Leadership Model that states that professional skills, technical competence, and
managerial brillianceunderwrite good management, nonetheless the
actualassessment of what divides those individuals, in NHS, is the compassion,
care, and sincere investment in workers that great leaders identify as being the
importantvariance between satisfactory technical medical care and successful
healthcare service (NHS 2018). Another similar initiative that has been developed by
the NHS is the Leading Change, Adding Value (LCAV) that focuses on midwifery,
nursing and other care staff. According to this framework, efforts will be taken by the
NHS to address the target areas of health and wellbeing, care and quality, and
funding and efficiency (NHS 2016).
Background
The quality of care delivered to the patients is fundamentally determined by
the excellence of arrangement, worth of training, capability of staffs and competence
of the operational systems (Allan et al. 2017). The Keogh Review related to patient
safety was conducted, in relation to the Francis Inquiry that was based no poor care
NHS
outcomes
framework
Domain 1:
Preventing
people from
dying
prematurely
Domain 2:
Enhancing
quality of life for
people with
long-term
conditions
Domain 3:
Helping people
to recover from
episodes of ill
health or
following injury
Domain 4:
Ensuring that
people have a
positive
experience of
care
Domain 5:
Treating and
caring for
people in a safe
environment
and protecting
them from
avoidable harm
Chambers 2017). Furthermore, the NHS Outcomes Framework (NHS OF) has also
been developed in the form of several indicators by the Department of Health and
Social Care, with the aim of monitoring health outcomes of children and adults in
England (Roland and Guthrie 2016).
This in turn can be accomplished by implementing the NHS Healthcare
Leadership Model that states that professional skills, technical competence, and
managerial brillianceunderwrite good management, nonetheless the
actualassessment of what divides those individuals, in NHS, is the compassion,
care, and sincere investment in workers that great leaders identify as being the
importantvariance between satisfactory technical medical care and successful
healthcare service (NHS 2018). Another similar initiative that has been developed by
the NHS is the Leading Change, Adding Value (LCAV) that focuses on midwifery,
nursing and other care staff. According to this framework, efforts will be taken by the
NHS to address the target areas of health and wellbeing, care and quality, and
funding and efficiency (NHS 2016).
Background
The quality of care delivered to the patients is fundamentally determined by
the excellence of arrangement, worth of training, capability of staffs and competence
of the operational systems (Allan et al. 2017). The Keogh Review related to patient
safety was conducted, in relation to the Francis Inquiry that was based no poor care
NHS
outcomes
framework
Domain 1:
Preventing
people from
dying
prematurely
Domain 2:
Enhancing
quality of life for
people with
long-term
conditions
Domain 3:
Helping people
to recover from
episodes of ill
health or
following injury
Domain 4:
Ensuring that
people have a
positive
experience of
care
Domain 5:
Treating and
caring for
people in a safe
environment
and protecting
them from
avoidable harm
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING
at Mid Staffordshire Hospitals NHS Foundation Trust (NHS 2013). This review
resulted in incorporation of six NHS Foundation Trusts and five NHS Trust
Development Authority. The Francis Inquiry report was formulated and enforced on
February 2013 and scrutinised the reasons behind the failure associated with patient
care at Mid Staffordshire NHS Foundation Trust from 2005-2009 (NMC 2013). This
report was a significant step towards developing 290 recommendations, which
comprised of better-quality support for empathetic, caring and dedicated care, and
resilient healthcare leadership (Francis 2013).
Government reports provide evidence for the fact that an estimated 1.2 million
individualshave beendiagnosed with COPD, which is noticeablygreater than the
835,000 people, as projected by the Department of Health in the year 2011 (Snell et
al. 2013). Roughly 2% of the entire population, and around 4.5% of all individuals
aged more than 40 years are living with confirmed diagnosis of COPD ( British Lung
Foundation 2018). Furthermore, a 2.03% prevalence was observed among people
living in Scotland, and this number is also expected to be more than 2.20% by 2030
(McLean et al. 2016). Additionally, COPD is occasionally reported by people aged
less than 40 and nearly affects 9% of people aged more than 70 years (Snell et al.
2016).
On evaluating the impacts of a multi‐site community pharmacy-based service
for COPD improvement, Wright et al. (2015) found that an estimated 306 patients
accessed the community service. On analysing the data obtained from 137 patients,
the researchers found significant enhancements in patient reported compliance,
quality of life, use of rescue packs, and a decrease in routine visits by the general
practitioner (GP). Reports from another qualitative study that compared the
perception of patients in relation to early stage COPD specialist and telehealth
interventions supported the fact that though COPD recipients of the telehealth
service obtained 50 % less home visits from clinicians, when compared to patients
who were subjected to out-dated community-based nursing interventions, they
demonstrated enthusiasmabout the service, with some of them considering it
effective for the management of COPD. This in turn provides the indication that there
is lack of acceptance of community-based services among COPD, even though it
would facilitate direct communication and interaction with clinicians. Rather, the
patients demonstrate a likelihood of accepting telehealth service where they will be
at Mid Staffordshire Hospitals NHS Foundation Trust (NHS 2013). This review
resulted in incorporation of six NHS Foundation Trusts and five NHS Trust
Development Authority. The Francis Inquiry report was formulated and enforced on
February 2013 and scrutinised the reasons behind the failure associated with patient
care at Mid Staffordshire NHS Foundation Trust from 2005-2009 (NMC 2013). This
report was a significant step towards developing 290 recommendations, which
comprised of better-quality support for empathetic, caring and dedicated care, and
resilient healthcare leadership (Francis 2013).
Government reports provide evidence for the fact that an estimated 1.2 million
individualshave beendiagnosed with COPD, which is noticeablygreater than the
835,000 people, as projected by the Department of Health in the year 2011 (Snell et
al. 2013). Roughly 2% of the entire population, and around 4.5% of all individuals
aged more than 40 years are living with confirmed diagnosis of COPD ( British Lung
Foundation 2018). Furthermore, a 2.03% prevalence was observed among people
living in Scotland, and this number is also expected to be more than 2.20% by 2030
(McLean et al. 2016). Additionally, COPD is occasionally reported by people aged
less than 40 and nearly affects 9% of people aged more than 70 years (Snell et al.
2016).
On evaluating the impacts of a multi‐site community pharmacy-based service
for COPD improvement, Wright et al. (2015) found that an estimated 306 patients
accessed the community service. On analysing the data obtained from 137 patients,
the researchers found significant enhancements in patient reported compliance,
quality of life, use of rescue packs, and a decrease in routine visits by the general
practitioner (GP). Reports from another qualitative study that compared the
perception of patients in relation to early stage COPD specialist and telehealth
interventions supported the fact that though COPD recipients of the telehealth
service obtained 50 % less home visits from clinicians, when compared to patients
who were subjected to out-dated community-based nursing interventions, they
demonstrated enthusiasmabout the service, with some of them considering it
effective for the management of COPD. This in turn provides the indication that there
is lack of acceptance of community-based services among COPD, even though it
would facilitate direct communication and interaction with clinicians. Rather, the
patients demonstrate a likelihood of accepting telehealth service where they will be
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
remotely governed by a healthcare professional (Fitzsimmons et al. 2016). The need
for increasing patient acceptance of community-based service for COPD was further
elucidated by Cope, Fowler and Pogson (2015) who postulated that on developing a
COPD in-reach service, the average length of hospitalisation for the patients reduced
significantly by 2.53 days, which in turn was concomitant with reduction in
readmission rates by a mean value of 4.5 per month. Furthermore, the service lead
to early discharge of 17% of patients, and also brought about an increased
preparedness and readiness among them for discharge from hospital. Thus, the
findings helped in illustrating the effectiveness of community-based service in
reducing COPD admission.
These findings are in accordance to those published by Hermizet al. (2002)
who stated that on subjecting randomised patients to a community-based COPD
intervention, no significant differences were observed in the rate of hospital
presentation, admission, or general functional status, Nonetheless, patients
subjected to community-based interventions were able to demonstrate improved
activity scores, while the control group manifested deterioration of their health
symptoms. Visits from the community nurses also increased patient satisfaction, in
comparison to general practitioner visits, and the patients in the intervention group
also reported improved awareness and knowledge about their health status, thus
highlighting the role of community-based care program in reducing COPD admission
to hospitals. This calls for the need of implementing changes where patients
diagnosed with COPD will be subjected to education and advice on different lifestyle
modifications that can help reduce their COPD symptoms.
Hall (2016) have also elaborated that on implementing Chronic Respiratory
Disease Nurse Practitioner (CRD NP) Model of Care (MOC) among patients, a
statistically noteworthyupsurgefrom 7.7% in 2009 to 45% in 2011was noted in the
number of patients, who had beenevaluated with arterial blood gas examination for
eligibility of STOT. Creating provisions for accessing the facility of STOT on patient
discharge also augmented from 26.7% to 44.4%. Furthermore, this MOC was also
associated with a reduction in the hospital re-admission rates, within 28 days of
release for the patients with STOT, from 25% to 12.5% (2009 and 2011,
respectively). Strategies to avoid hospital admission of COPD patients were also
illustrated by Cox et al. (2017) who stated that professionalexpertise of respiratory
remotely governed by a healthcare professional (Fitzsimmons et al. 2016). The need
for increasing patient acceptance of community-based service for COPD was further
elucidated by Cope, Fowler and Pogson (2015) who postulated that on developing a
COPD in-reach service, the average length of hospitalisation for the patients reduced
significantly by 2.53 days, which in turn was concomitant with reduction in
readmission rates by a mean value of 4.5 per month. Furthermore, the service lead
to early discharge of 17% of patients, and also brought about an increased
preparedness and readiness among them for discharge from hospital. Thus, the
findings helped in illustrating the effectiveness of community-based service in
reducing COPD admission.
These findings are in accordance to those published by Hermizet al. (2002)
who stated that on subjecting randomised patients to a community-based COPD
intervention, no significant differences were observed in the rate of hospital
presentation, admission, or general functional status, Nonetheless, patients
subjected to community-based interventions were able to demonstrate improved
activity scores, while the control group manifested deterioration of their health
symptoms. Visits from the community nurses also increased patient satisfaction, in
comparison to general practitioner visits, and the patients in the intervention group
also reported improved awareness and knowledge about their health status, thus
highlighting the role of community-based care program in reducing COPD admission
to hospitals. This calls for the need of implementing changes where patients
diagnosed with COPD will be subjected to education and advice on different lifestyle
modifications that can help reduce their COPD symptoms.
Hall (2016) have also elaborated that on implementing Chronic Respiratory
Disease Nurse Practitioner (CRD NP) Model of Care (MOC) among patients, a
statistically noteworthyupsurgefrom 7.7% in 2009 to 45% in 2011was noted in the
number of patients, who had beenevaluated with arterial blood gas examination for
eligibility of STOT. Creating provisions for accessing the facility of STOT on patient
discharge also augmented from 26.7% to 44.4%. Furthermore, this MOC was also
associated with a reduction in the hospital re-admission rates, within 28 days of
release for the patients with STOT, from 25% to 12.5% (2009 and 2011,
respectively). Strategies to avoid hospital admission of COPD patients were also
illustrated by Cox et al. (2017) who stated that professionalexpertise of respiratory
8NURSING
nurse specialists were an importantinfluential factor in the accomplishment of the
objective, predominantly the capability to commence and understand CBG
assessments amid patients, while initiating emergency oxygen upon them. It was
also suggested that providing a holistic and individual assessment, besides making
patient referral to community service also creates a longer-term influence on the
COPD related health outcomes.
According to the NICE guidelines (2018) it is essential to review COPD
patients at least once in a year, and if necessary, more often, to keep a track on their
health status. The guidelines highlight that for most individuals suffering from severe
COPD, consistent hospital review is not essential, nonetheless there must be locally
decided mechanisms to permit quick access to hospital examination, as and when
desired (NHS 2018). These guidelines also emphasise on the need for specialists to
frequently review individualsdiagnosed with severe COPD who require the
administration of interventions such as, non-invasive ventilation. Further reports from
the Care Quality Commission (2019) also elaborated on the fact that of all people
who are diagnosed with long-term health ailments, 88% patients who experienced
poor health did not complain since they were concerned about making trouble.
Nonetheless, 81% of patients with COPD lamented for not registering a complaint
about receiving poor care. Hence, this calls for the need of implementing a patient
innovation service that will address the concern of recurrent hospital admission that
patients suffering from COPD.
Rationale/aims and objectives
The fishbone diagram has been used for categorising the possible causes of
the health problem in order to classify its root causes, based on their hierarchy and
level of importance. It also facilitated identification of bottleneck in the entire
procedure, thus highlighting the strategies that can be adopted to address the
problem (Coccia 2018). It has been identified that not all patients who have been
diagnosed with COPD are able to utilise the community-based healthcare services
that are able to address their healthcare demands. Furthermore, patients have also
been found to demonstrate lack of adequate understanding and knowledge on the
available community service, and the potential health benefits that they can gain, by
using them. Hence, the primary aim of this patient innovation program is to create
and disseminate leaflets to patients, containing exhaustive and comprehensive
nurse specialists were an importantinfluential factor in the accomplishment of the
objective, predominantly the capability to commence and understand CBG
assessments amid patients, while initiating emergency oxygen upon them. It was
also suggested that providing a holistic and individual assessment, besides making
patient referral to community service also creates a longer-term influence on the
COPD related health outcomes.
According to the NICE guidelines (2018) it is essential to review COPD
patients at least once in a year, and if necessary, more often, to keep a track on their
health status. The guidelines highlight that for most individuals suffering from severe
COPD, consistent hospital review is not essential, nonetheless there must be locally
decided mechanisms to permit quick access to hospital examination, as and when
desired (NHS 2018). These guidelines also emphasise on the need for specialists to
frequently review individualsdiagnosed with severe COPD who require the
administration of interventions such as, non-invasive ventilation. Further reports from
the Care Quality Commission (2019) also elaborated on the fact that of all people
who are diagnosed with long-term health ailments, 88% patients who experienced
poor health did not complain since they were concerned about making trouble.
Nonetheless, 81% of patients with COPD lamented for not registering a complaint
about receiving poor care. Hence, this calls for the need of implementing a patient
innovation service that will address the concern of recurrent hospital admission that
patients suffering from COPD.
Rationale/aims and objectives
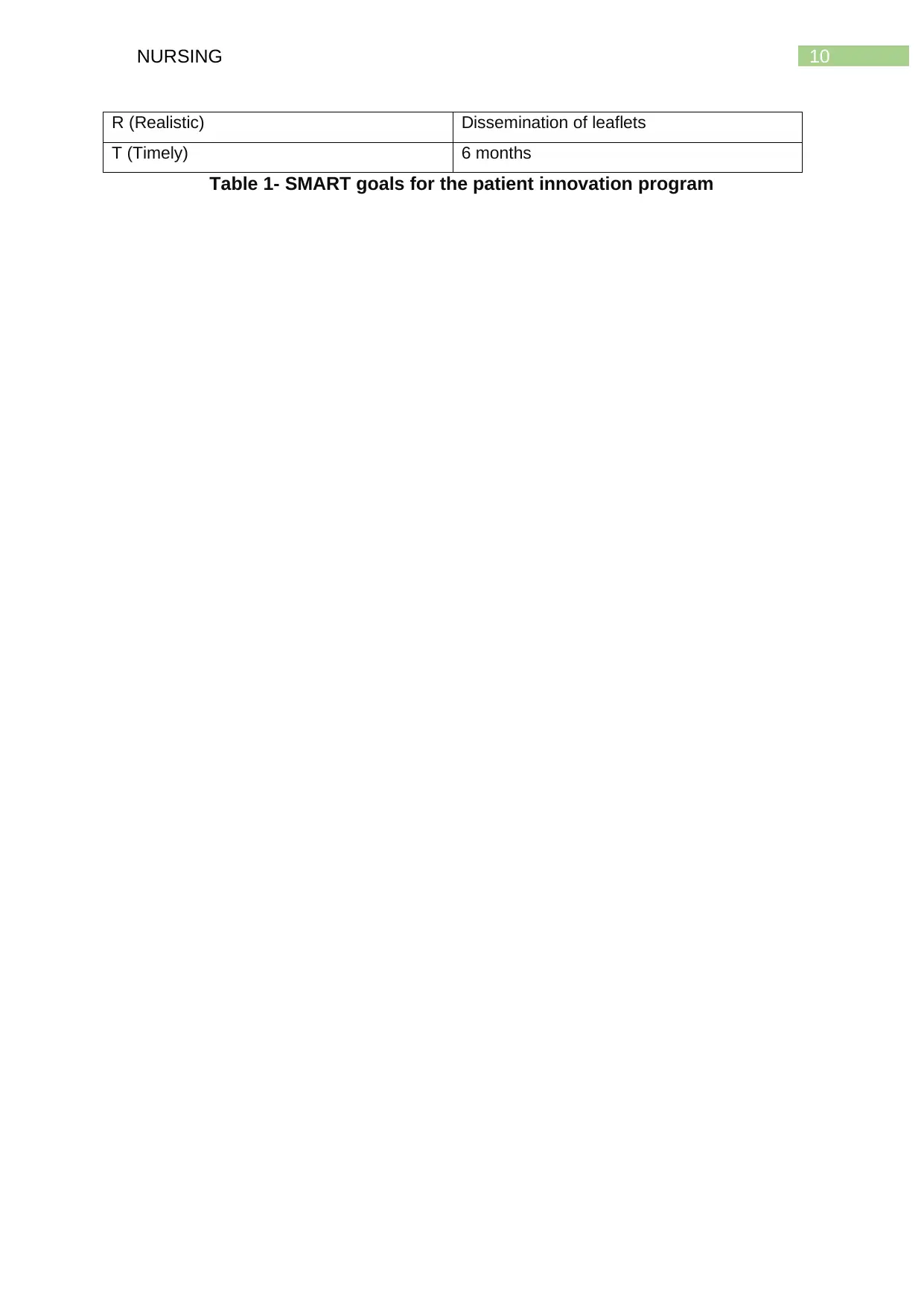
The fishbone diagram has been used for categorising the possible causes of
the health problem in order to classify its root causes, based on their hierarchy and
level of importance. It also facilitated identification of bottleneck in the entire
procedure, thus highlighting the strategies that can be adopted to address the
problem (Coccia 2018). It has been identified that not all patients who have been
diagnosed with COPD are able to utilise the community-based healthcare services
that are able to address their healthcare demands. Furthermore, patients have also
been found to demonstrate lack of adequate understanding and knowledge on the
available community service, and the potential health benefits that they can gain, by
using them. Hence, the primary aim of this patient innovation program is to create
and disseminate leaflets to patients, containing exhaustive and comprehensive
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
information on different respiratory health ailments namely, COPD, pneumothorax,
type 1 and type 2 respiratory failure, pulmonary embolism, their symptoms, causative
factors and treatment options. The leaflet will also provide the patients with
necessary information on when and whom to contact under emergency situations
such as respiratory specialist nurses and other healthcare personnel.
The major objective of distributing leaflets to patients is to increase their health
literacy, which will help the patients to understand and utilise the information
provided in a manner that prevents exacerbation of COPD symptoms, helps in
effective management of the condition, thereby reducing hospital readmission rates.
Contrary to verbal information, the difficulty of interpretation of any written material is
permanent and consequently must be prepared in a manner that is understood by
the patients (Schmitz et al. 2017). Patients will therefore gain benefit from this
innovation program since it is in accordance to two indicators of the NHS Outcomes
Framework that are given below:
1.2 Under 75 mortality rate from respiratory disease
3b Emergency readmissions within 30 days of discharge from hospital (NHS
2019)
Owing to the fact that respiratory diseases, when left untreated, have been
associated with high mortality and morbidity rate, the patient leaflet will prove
effective in ensuring that health outcomes of COPD diagnosed patients aged under
75 will improve, thus decreasing their mortality. In addition, readmissions are
generally used by the NHS in the form of an indicator for determining the efficacy
and success of healthcare amenities, in relation to recovery of the patients. Thus,
leaflet dissemination will also help in increasing awareness among the patients,
thereby improving their health outcomes, and preventing emergency readmissions,
after discharge from the hospitals. The SMART goals for the patient innovation
program are given below (Bjerke and Renger 2017):
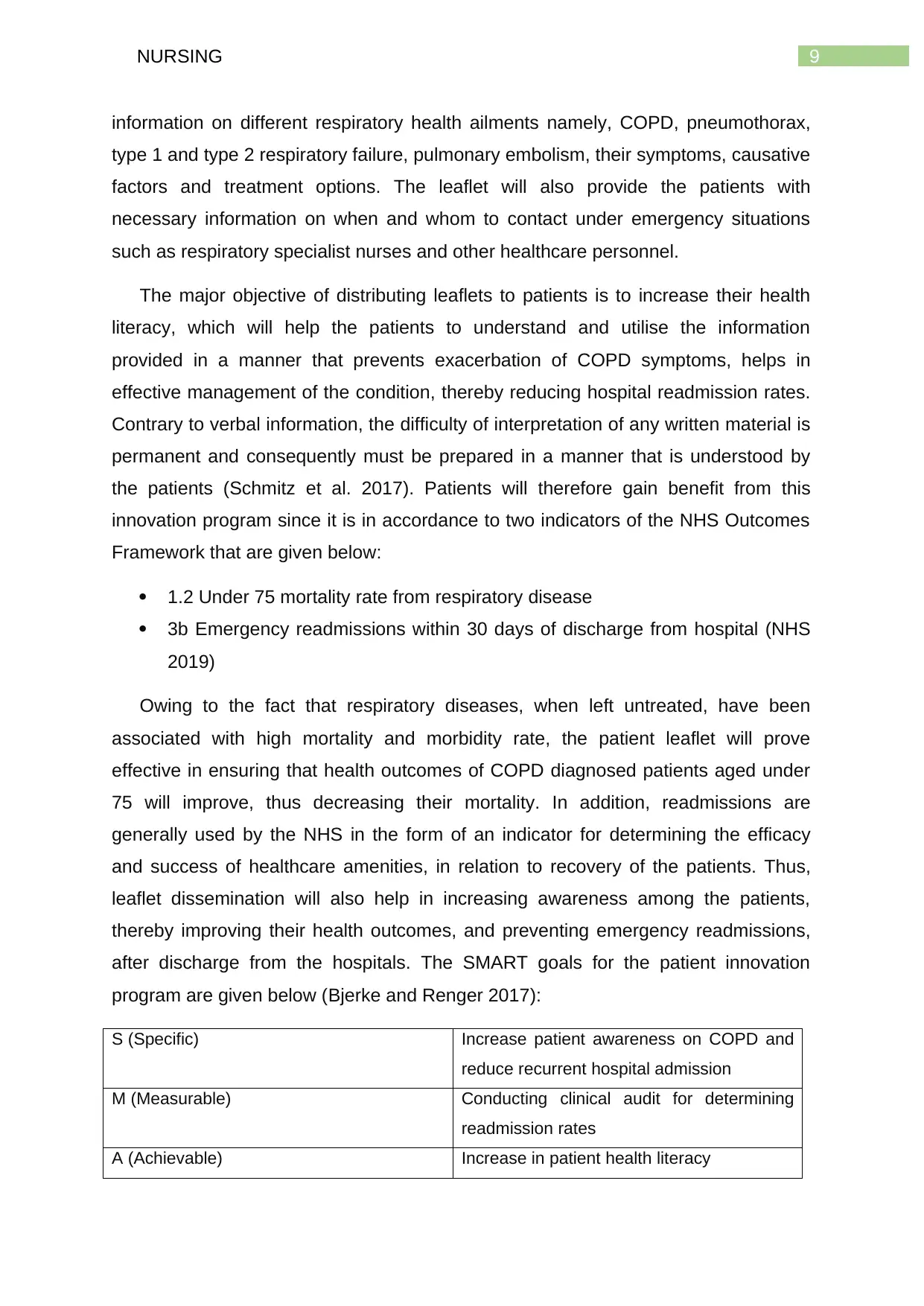
S (Specific) Increase patient awareness on COPD and
reduce recurrent hospital admission
M (Measurable) Conducting clinical audit for determining
readmission rates
A (Achievable) Increase in patient health literacy
information on different respiratory health ailments namely, COPD, pneumothorax,
type 1 and type 2 respiratory failure, pulmonary embolism, their symptoms, causative
factors and treatment options. The leaflet will also provide the patients with
necessary information on when and whom to contact under emergency situations
such as respiratory specialist nurses and other healthcare personnel.
The major objective of distributing leaflets to patients is to increase their health
literacy, which will help the patients to understand and utilise the information
provided in a manner that prevents exacerbation of COPD symptoms, helps in
effective management of the condition, thereby reducing hospital readmission rates.
Contrary to verbal information, the difficulty of interpretation of any written material is
permanent and consequently must be prepared in a manner that is understood by
the patients (Schmitz et al. 2017). Patients will therefore gain benefit from this
innovation program since it is in accordance to two indicators of the NHS Outcomes
Framework that are given below:
1.2 Under 75 mortality rate from respiratory disease
3b Emergency readmissions within 30 days of discharge from hospital (NHS
2019)
Owing to the fact that respiratory diseases, when left untreated, have been
associated with high mortality and morbidity rate, the patient leaflet will prove
effective in ensuring that health outcomes of COPD diagnosed patients aged under
75 will improve, thus decreasing their mortality. In addition, readmissions are
generally used by the NHS in the form of an indicator for determining the efficacy
and success of healthcare amenities, in relation to recovery of the patients. Thus,
leaflet dissemination will also help in increasing awareness among the patients,
thereby improving their health outcomes, and preventing emergency readmissions,
after discharge from the hospitals. The SMART goals for the patient innovation
program are given below (Bjerke and Renger 2017):
S (Specific) Increase patient awareness on COPD and
reduce recurrent hospital admission
M (Measurable) Conducting clinical audit for determining
readmission rates
A (Achievable) Increase in patient health literacy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
R (Realistic) Dissemination of leaflets
T (Timely) 6 months
Table 1- SMART goals for the patient innovation program
R (Realistic) Dissemination of leaflets
T (Timely) 6 months
Table 1- SMART goals for the patient innovation program
Running head: NURSING
Figure 2- Fish bone diagram for root cause analysis
Figure 2- Fish bone diagram for root cause analysis
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 34
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





