Analysis of Social Health Determinants in Mt Isa Community (3804NRS)
VerifiedAdded on 2023/01/18
|9
|2303
|53
Report
AI Summary
This report provides a community health assessment focusing on the social determinants of health in the Mt Isa community. It analyzes demographic data, including gender distribution, Aboriginal and Torres Strait Islander (ATSI) populations, education levels, employment rates, and income levels, comparing them to state and national averages. The report explores the impact of these determinants—education, employment, and income—on health outcomes, referencing relevant literature. It discusses the role of community nurses in addressing health disparities, particularly within vulnerable groups like the ATSI community, and outlines strategies for needs assessment, health promotion, and engagement. The report emphasizes the importance of early childhood education, adult education, and culturally sensitive approaches to improve health outcomes and reduce socioeconomic disparities. The report concludes by restating the importance of these social determinants and recommends collaborative efforts between healthcare providers and the government to support marginalized communities.
Running head: HEALTH
Student name
Student No
Unit
Title: Social Health Determinants
Student name
Student No
Unit
Title: Social Health Determinants
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH
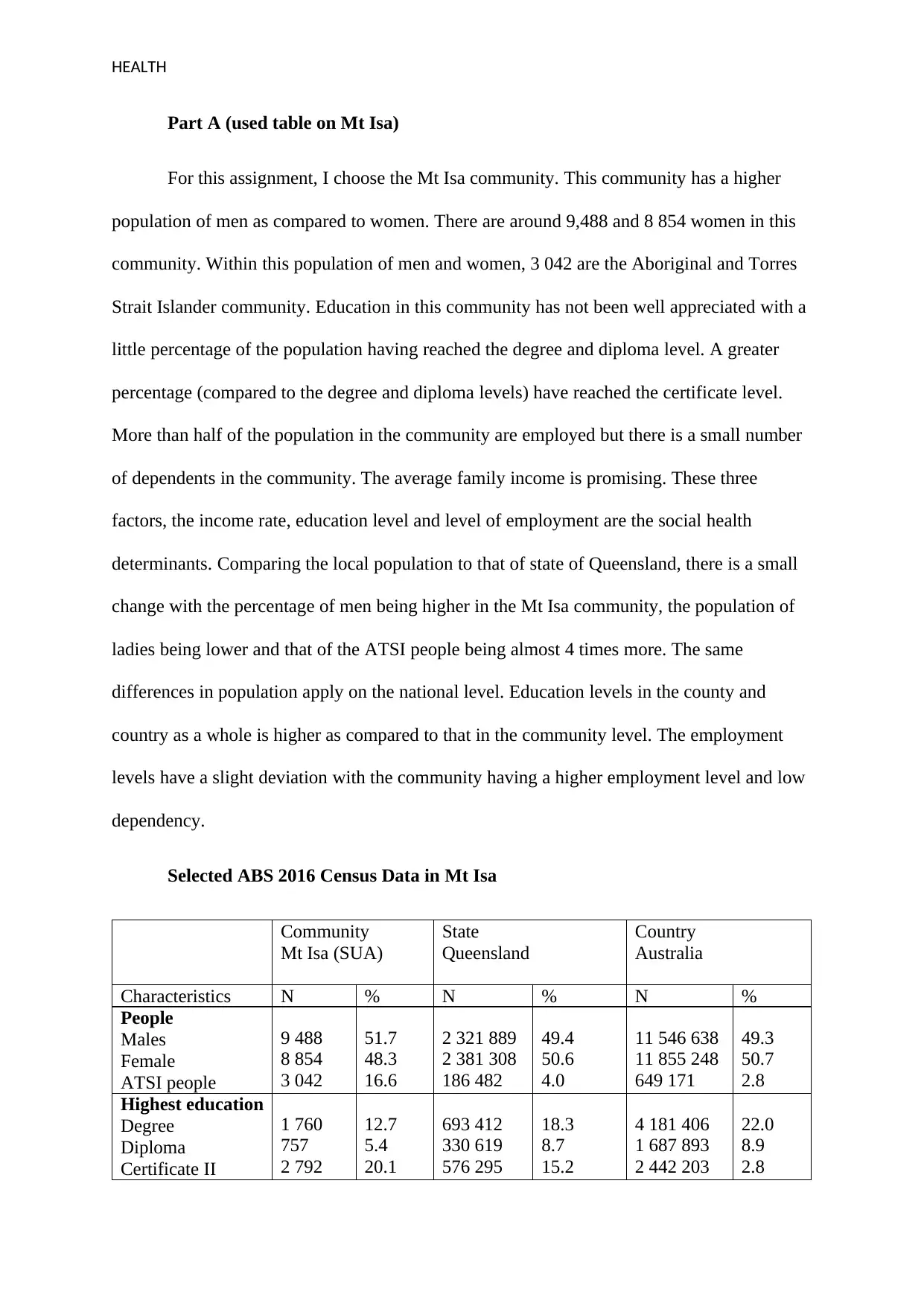
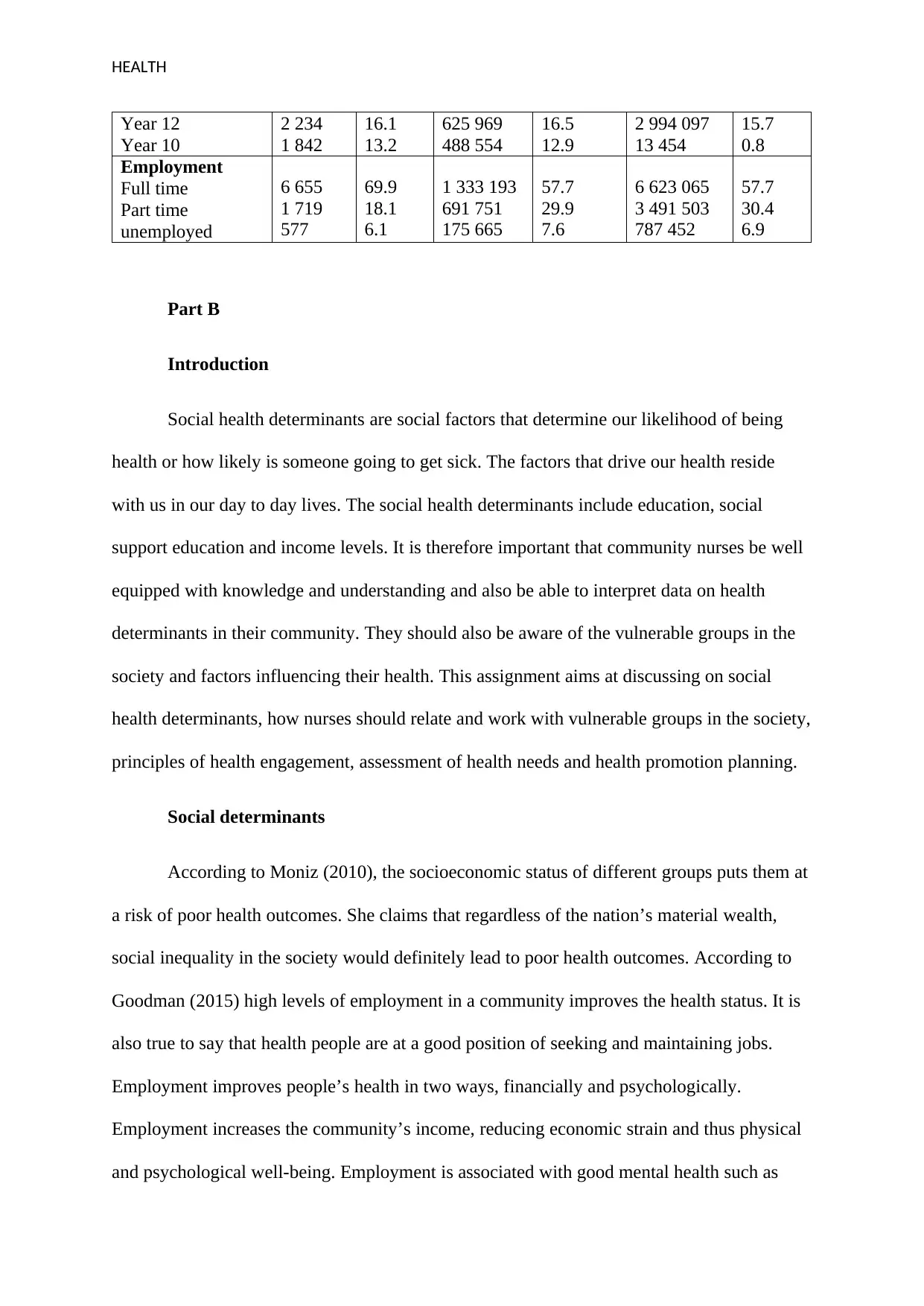
Part A (used table on Mt Isa)
For this assignment, I choose the Mt Isa community. This community has a higher
population of men as compared to women. There are around 9,488 and 8 854 women in this
community. Within this population of men and women, 3 042 are the Aboriginal and Torres
Strait Islander community. Education in this community has not been well appreciated with a
little percentage of the population having reached the degree and diploma level. A greater
percentage (compared to the degree and diploma levels) have reached the certificate level.
More than half of the population in the community are employed but there is a small number
of dependents in the community. The average family income is promising. These three
factors, the income rate, education level and level of employment are the social health
determinants. Comparing the local population to that of state of Queensland, there is a small
change with the percentage of men being higher in the Mt Isa community, the population of
ladies being lower and that of the ATSI people being almost 4 times more. The same
differences in population apply on the national level. Education levels in the county and
country as a whole is higher as compared to that in the community level. The employment
levels have a slight deviation with the community having a higher employment level and low
dependency.
Selected ABS 2016 Census Data in Mt Isa
Community
Mt Isa (SUA)
State
Queensland
Country
Australia
Characteristics N % N % N %
People
Males
Female
ATSI people
9 488
8 854
3 042
51.7
48.3
16.6
2 321 889
2 381 308
186 482
49.4
50.6
4.0
11 546 638
11 855 248
649 171
49.3
50.7
2.8
Highest education
Degree
Diploma
Certificate II
1 760
757
2 792
12.7
5.4
20.1
693 412
330 619
576 295
18.3
8.7
15.2
4 181 406
1 687 893
2 442 203
22.0
8.9
2.8
Part A (used table on Mt Isa)
For this assignment, I choose the Mt Isa community. This community has a higher
population of men as compared to women. There are around 9,488 and 8 854 women in this
community. Within this population of men and women, 3 042 are the Aboriginal and Torres
Strait Islander community. Education in this community has not been well appreciated with a
little percentage of the population having reached the degree and diploma level. A greater
percentage (compared to the degree and diploma levels) have reached the certificate level.
More than half of the population in the community are employed but there is a small number
of dependents in the community. The average family income is promising. These three
factors, the income rate, education level and level of employment are the social health
determinants. Comparing the local population to that of state of Queensland, there is a small
change with the percentage of men being higher in the Mt Isa community, the population of
ladies being lower and that of the ATSI people being almost 4 times more. The same
differences in population apply on the national level. Education levels in the county and
country as a whole is higher as compared to that in the community level. The employment
levels have a slight deviation with the community having a higher employment level and low
dependency.
Selected ABS 2016 Census Data in Mt Isa
Community
Mt Isa (SUA)
State
Queensland
Country
Australia
Characteristics N % N % N %
People
Males
Female
ATSI people
9 488
8 854
3 042
51.7
48.3
16.6
2 321 889
2 381 308
186 482
49.4
50.6
4.0
11 546 638
11 855 248
649 171
49.3
50.7
2.8
Highest education
Degree
Diploma
Certificate II
1 760
757
2 792
12.7
5.4
20.1
693 412
330 619
576 295
18.3
8.7
15.2
4 181 406
1 687 893
2 442 203
22.0
8.9
2.8
HEALTH
Year 12
Year 10
2 234
1 842
16.1
13.2
625 969
488 554
16.5
12.9
2 994 097
13 454
15.7
0.8
Employment
Full time
Part time
unemployed
6 655
1 719
577
69.9
18.1
6.1
1 333 193
691 751
175 665
57.7
29.9
7.6
6 623 065
3 491 503
787 452
57.7
30.4
6.9
Part B
Introduction
Social health determinants are social factors that determine our likelihood of being
health or how likely is someone going to get sick. The factors that drive our health reside
with us in our day to day lives. The social health determinants include education, social
support education and income levels. It is therefore important that community nurses be well
equipped with knowledge and understanding and also be able to interpret data on health
determinants in their community. They should also be aware of the vulnerable groups in the
society and factors influencing their health. This assignment aims at discussing on social
health determinants, how nurses should relate and work with vulnerable groups in the society,
principles of health engagement, assessment of health needs and health promotion planning.
Social determinants
According to Moniz (2010), the socioeconomic status of different groups puts them at
a risk of poor health outcomes. She claims that regardless of the nation’s material wealth,
social inequality in the society would definitely lead to poor health outcomes. According to
Goodman (2015) high levels of employment in a community improves the health status. It is
also true to say that health people are at a good position of seeking and maintaining jobs.
Employment improves people’s health in two ways, financially and psychologically.
Employment increases the community’s income, reducing economic strain and thus physical
and psychological well-being. Employment is associated with good mental health such as
Year 12
Year 10
2 234
1 842
16.1
13.2
625 969
488 554
16.5
12.9
2 994 097
13 454
15.7
0.8
Employment
Full time
Part time
unemployed
6 655
1 719
577
69.9
18.1
6.1
1 333 193
691 751
175 665
57.7
29.9
7.6
6 623 065
3 491 503
787 452
57.7
30.4
6.9
Part B
Introduction
Social health determinants are social factors that determine our likelihood of being
health or how likely is someone going to get sick. The factors that drive our health reside
with us in our day to day lives. The social health determinants include education, social
support education and income levels. It is therefore important that community nurses be well
equipped with knowledge and understanding and also be able to interpret data on health
determinants in their community. They should also be aware of the vulnerable groups in the
society and factors influencing their health. This assignment aims at discussing on social
health determinants, how nurses should relate and work with vulnerable groups in the society,
principles of health engagement, assessment of health needs and health promotion planning.
Social determinants
According to Moniz (2010), the socioeconomic status of different groups puts them at
a risk of poor health outcomes. She claims that regardless of the nation’s material wealth,
social inequality in the society would definitely lead to poor health outcomes. According to
Goodman (2015) high levels of employment in a community improves the health status. It is
also true to say that health people are at a good position of seeking and maintaining jobs.
Employment improves people’s health in two ways, financially and psychologically.
Employment increases the community’s income, reducing economic strain and thus physical
and psychological well-being. Employment is associated with good mental health such as
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH
self-worth and self esteem. Psychologists argue that unemployment is a threat to one’s
identity and destroys one’s sense of self worth.
Among the many relationships between education levels in a community and the
health of the residents is that educated individuals are predisposed to better health outcomes.
Zimmermann and Woolf (2014) think that education is a major health predictor in a
community, with economic trends in industrialized nations intensifying this relationship
between education and health. Goldman and Smith (2011) reported that the gradient in health
outcomes as a result of educational attainment in the United States has steepened as greater
heights in education are being attained. According to Montez and Berkman (2014) there is a
large gap in health status between people with high and low education. Low levels of
education also reduces the life expectancy in the society.
According to Khullar and Chokshi (2018), there exists a strong evidence that
associates a community’s income and health. This evidence suggests that policies and
strategies that promote economic equity affects health broadly. Low income in a community
leads to high mortality and morbidity, with more and more income associated challenges
growing day in day out. Over the years poverty has been recognized as among the leading
causes of diseases and deaths. Larrimore (2011) thinks that many researches have proven that
there exists a positive relationship between good socioeconomic status and improved health
outcomes. He claims that people with high income tend to have better health as compared to
those with low income. Arno, Sohler, Viola, Schechter (2009) claims that government policy
makers must understand the relationship existing between the income rate and health as they
lay down public policies and programs. Increasing the income support programs is thought to
bring a positive health effect. A research by Khullar and Chokshi (2018), showed that people
with low income are associate with high physical limitation, including diseases such as
diabetes, hypertension, heart diseases and other chronic infections. A family earning less than
self-worth and self esteem. Psychologists argue that unemployment is a threat to one’s
identity and destroys one’s sense of self worth.
Among the many relationships between education levels in a community and the
health of the residents is that educated individuals are predisposed to better health outcomes.
Zimmermann and Woolf (2014) think that education is a major health predictor in a
community, with economic trends in industrialized nations intensifying this relationship
between education and health. Goldman and Smith (2011) reported that the gradient in health
outcomes as a result of educational attainment in the United States has steepened as greater
heights in education are being attained. According to Montez and Berkman (2014) there is a
large gap in health status between people with high and low education. Low levels of
education also reduces the life expectancy in the society.
According to Khullar and Chokshi (2018), there exists a strong evidence that
associates a community’s income and health. This evidence suggests that policies and
strategies that promote economic equity affects health broadly. Low income in a community
leads to high mortality and morbidity, with more and more income associated challenges
growing day in day out. Over the years poverty has been recognized as among the leading
causes of diseases and deaths. Larrimore (2011) thinks that many researches have proven that
there exists a positive relationship between good socioeconomic status and improved health
outcomes. He claims that people with high income tend to have better health as compared to
those with low income. Arno, Sohler, Viola, Schechter (2009) claims that government policy
makers must understand the relationship existing between the income rate and health as they
lay down public policies and programs. Increasing the income support programs is thought to
bring a positive health effect. A research by Khullar and Chokshi (2018), showed that people
with low income are associate with high physical limitation, including diseases such as
diabetes, hypertension, heart diseases and other chronic infections. A family earning less than
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH
$ 35 000 per year is reported to be 4 times nervous and 5 times being sad most of the time as
compared to a family that earns over $ 100 000 per year.
Vulnerable group
According to the Australian Government (2016), socioeconomic status such as
education levels and one’s occupation are important in explaining the health disparities
existing between indigenous and non-indigenous Australians. A research by Zhao et al.
(2013) showed that the health gap existing between the ATSI community and the non-
indigenous Australians is as a result differences in the socioeconomic patterns. The
indigenous Australians are the lowest income group, has lower levels of education, has low
levels of employment and also reported to have poor health in Australia. Marmot (2011)
claims that health inequalities are as result of societal inequalities. He continues that health
and lifestyle differences in the Australian communities lead to social disparities but the core
causes of social differences among these communities are associated with where an
individual is born, lived, grew, works and also their ages.
Engagement and needs assessment
As the community nurse, there are different ways to carry out needs assessment and
engage the Aboriginal and Torres Strait Islanders community in an attempt to solve the
socioeconomic disparities between them and the non-aboriginal communities. Since
education is a social health determinant, encouraging early childhood and also adult
education would be a big step. It has been scientifically proven that positive early childhood
education creates a firm foundation for healthy life. Educating people on the consequences of
poor socioeconomic circumstances would help them know what and when to do. There is a
theory that suggests that slow growth and poor emotional health in a child increases the risk
of poor mental and physical health in their adulthood. People should be educated on the effect
$ 35 000 per year is reported to be 4 times nervous and 5 times being sad most of the time as
compared to a family that earns over $ 100 000 per year.
Vulnerable group
According to the Australian Government (2016), socioeconomic status such as
education levels and one’s occupation are important in explaining the health disparities
existing between indigenous and non-indigenous Australians. A research by Zhao et al.
(2013) showed that the health gap existing between the ATSI community and the non-
indigenous Australians is as a result differences in the socioeconomic patterns. The
indigenous Australians are the lowest income group, has lower levels of education, has low
levels of employment and also reported to have poor health in Australia. Marmot (2011)
claims that health inequalities are as result of societal inequalities. He continues that health
and lifestyle differences in the Australian communities lead to social disparities but the core
causes of social differences among these communities are associated with where an
individual is born, lived, grew, works and also their ages.
Engagement and needs assessment
As the community nurse, there are different ways to carry out needs assessment and
engage the Aboriginal and Torres Strait Islanders community in an attempt to solve the
socioeconomic disparities between them and the non-aboriginal communities. Since
education is a social health determinant, encouraging early childhood and also adult
education would be a big step. It has been scientifically proven that positive early childhood
education creates a firm foundation for healthy life. Educating people on the consequences of
poor socioeconomic circumstances would help them know what and when to do. There is a
theory that suggests that slow growth and poor emotional health in a child increases the risk
of poor mental and physical health in their adulthood. People should be educated on the effect
HEALTH
of substance and drug abuse as pertains their health and foetal outcomes (for women). The
ATSI people knowing the importance of sufficient exercise and prenatal care would help
improve their health (Reading and Wien, 2014). As a community nurse I would partner with
the relevant authorities in promoting achieving of school readiness, engaging the community,
providing a relationship between the community’s culture with education, develop pride in
children achievement, enhancing familiarity with school work and promoting culturally
sensitive teaching.
I would encourage the adults in the community to secure some employment so as to
maintain a regular income which is essential in improving the health outcomes of the ATSI
community. This would also prevent them from mental illness (depression and anxiety), heart
diseases and other physical health complications. Andermann (2018) thinks that during
medical processes, failure to know the social challenges of an individual would lead to
inappropriate diagnosis and care plans. Health professional who ask their patients about their
challenges are more likely to help their patients through their issues (Hutt and Gilmour,
2010). A nurse should ask the patient about their challenges in a culturally sensitive manner.
Coming up with a connected community school initiative could increase children attendance
in school. This initiative will be community based and involves parents and teachers
partnership whereby children would be monitored since birth, to school and other higher
levels of education.
Conclusion
It is clear now that educations levels, income and levels of employment in the society
are core social health determinants. Research by different scholars have shown the
relationship between these three factors and health. High levels of education leads to good
income. People with high levels of education show good health outcomes as compared to the
of substance and drug abuse as pertains their health and foetal outcomes (for women). The
ATSI people knowing the importance of sufficient exercise and prenatal care would help
improve their health (Reading and Wien, 2014). As a community nurse I would partner with
the relevant authorities in promoting achieving of school readiness, engaging the community,
providing a relationship between the community’s culture with education, develop pride in
children achievement, enhancing familiarity with school work and promoting culturally
sensitive teaching.
I would encourage the adults in the community to secure some employment so as to
maintain a regular income which is essential in improving the health outcomes of the ATSI
community. This would also prevent them from mental illness (depression and anxiety), heart
diseases and other physical health complications. Andermann (2018) thinks that during
medical processes, failure to know the social challenges of an individual would lead to
inappropriate diagnosis and care plans. Health professional who ask their patients about their
challenges are more likely to help their patients through their issues (Hutt and Gilmour,
2010). A nurse should ask the patient about their challenges in a culturally sensitive manner.
Coming up with a connected community school initiative could increase children attendance
in school. This initiative will be community based and involves parents and teachers
partnership whereby children would be monitored since birth, to school and other higher
levels of education.
Conclusion
It is clear now that educations levels, income and levels of employment in the society
are core social health determinants. Research by different scholars have shown the
relationship between these three factors and health. High levels of education leads to good
income. People with high levels of education show good health outcomes as compared to the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH
poor. Families with a good income are said to live more happily as compared to those with
low income. With good income, one has access to quality health care. Employment is a
source of self-esteem. It also give on a sense of social belonging. It is believed that lack of
employment leads to physical and mental challenges. It is important that the health care and
the government work hand in hand to help the marginalized groups in the society fight these
factors influencing their health.
poor. Families with a good income are said to live more happily as compared to those with
low income. With good income, one has access to quality health care. Employment is a
source of self-esteem. It also give on a sense of social belonging. It is believed that lack of
employment leads to physical and mental challenges. It is important that the health care and
the government work hand in hand to help the marginalized groups in the society fight these
factors influencing their health.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH
References
Australian Government: Australian Institute of Health and Welfare. (2016). Social
determinants of indigenous health. New Delhi” Australia Health
Andermann, A., & CLEAR Collaboration (2016). Taking action on the social determinants of
health in clinical practice: a framework for health professionals. CMAJ : Canadian
Medical Association journal, 188(17-18), E474–E483 Naz, A., Rosenberg, E.,
Andersson, N., Labonté, R., & Andermann, A. (2016). Health workers who ask about
social determinants of health are more likely to report helping patients: mixed-
methods study. Canadian Family Physician, 62(11), e684-e693.
doi:10.1503/cmaj.160177
Arno, P. S., Sohler, N., Viola, D., & Schechter, C. (2009). Bringing health and social policy
together: the case of the earned income tax credit. Journal of public health policy,
30(2), 198-207.
Goldman, D., and J. P. Smith. (2011). The increasing value of education to health. Social
Science and Medicine 72:1728–1737
. Khullar, D. and Chokshi, D. A. (2018). Health, Income, & Poverty: Where We Are & What
Could Help. Health Affairs, 319(13):1312-1313. Doi: 10.1377/hpb20180817.901935
Larrimore J. (2011). Does a higher income have positive health effects? Using the earned
income tax credit to explore the income-health gradient. The Milbank quarterly,
89(4), 694–727. doi:10.1111/j.1468-0009.2011.00647.x
Goodman, N. (2015). The Impact of Employment on the Health Status and Health Care Costs
of Working-age People with Disabilities. New York: Lead Centre.
References
Australian Government: Australian Institute of Health and Welfare. (2016). Social
determinants of indigenous health. New Delhi” Australia Health
Andermann, A., & CLEAR Collaboration (2016). Taking action on the social determinants of
health in clinical practice: a framework for health professionals. CMAJ : Canadian
Medical Association journal, 188(17-18), E474–E483 Naz, A., Rosenberg, E.,
Andersson, N., Labonté, R., & Andermann, A. (2016). Health workers who ask about
social determinants of health are more likely to report helping patients: mixed-
methods study. Canadian Family Physician, 62(11), e684-e693.
doi:10.1503/cmaj.160177
Arno, P. S., Sohler, N., Viola, D., & Schechter, C. (2009). Bringing health and social policy
together: the case of the earned income tax credit. Journal of public health policy,
30(2), 198-207.
Goldman, D., and J. P. Smith. (2011). The increasing value of education to health. Social
Science and Medicine 72:1728–1737
. Khullar, D. and Chokshi, D. A. (2018). Health, Income, & Poverty: Where We Are & What
Could Help. Health Affairs, 319(13):1312-1313. Doi: 10.1377/hpb20180817.901935
Larrimore J. (2011). Does a higher income have positive health effects? Using the earned
income tax credit to explore the income-health gradient. The Milbank quarterly,
89(4), 694–727. doi:10.1111/j.1468-0009.2011.00647.x
Goodman, N. (2015). The Impact of Employment on the Health Status and Health Care Costs
of Working-age People with Disabilities. New York: Lead Centre.
HEALTH
Marmot, M. (2011). Social determinants and the health of indigenous Australians. Med. J.
Aust. 194(10): 512-513. Doi: 10.5694/j.1326-5377.2011.tb03086.x
Montez, J. K., R. A. Hummer, and M. D. Hayward. (2012). Educational attainment and adult
mortality in the United States: A systematic assessment of functional form.
Demography 45:315–336
Moniz, C. (2010). Social Work and the Social Determinants of Health Perspective: A Good
Fit, Health & Social Work, Volume 35, Issue 4, pp. 310–313. Doi:
https://doi.org/10.1093/hsw/35.4.310
Reading, C. L. and Wien, F. (2014). Health inequalities ad social determinants of Aboriginal
people’s health. Prince George, BC: National Collaborating Centre for Aboriginal
Health
Zimmerman, E. and Woolf, S. H. (2014). Understanding the relationship between education
and health. Washington DC: National Academy of Health.
Marmot, M. (2011). Social determinants and the health of indigenous Australians. Med. J.
Aust. 194(10): 512-513. Doi: 10.5694/j.1326-5377.2011.tb03086.x
Montez, J. K., R. A. Hummer, and M. D. Hayward. (2012). Educational attainment and adult
mortality in the United States: A systematic assessment of functional form.
Demography 45:315–336
Moniz, C. (2010). Social Work and the Social Determinants of Health Perspective: A Good
Fit, Health & Social Work, Volume 35, Issue 4, pp. 310–313. Doi:
https://doi.org/10.1093/hsw/35.4.310
Reading, C. L. and Wien, F. (2014). Health inequalities ad social determinants of Aboriginal
people’s health. Prince George, BC: National Collaborating Centre for Aboriginal
Health
Zimmerman, E. and Woolf, S. H. (2014). Understanding the relationship between education
and health. Washington DC: National Academy of Health.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





