Comprehensive Health History and Assessment: NURS1004 Assignment
VerifiedAdded on 2021/05/31
|9
|2052
|24
Homework Assignment
AI Summary
This document presents a detailed health assessment of Robert Walker, an 83-year-old male, as part of a NURS1004 assignment. The assessment covers biographical data, reason for seeking care, present and past health history, family history, review of symptoms, and lifestyle management. It includes information on current medications, tobacco and alcohol use, environmental hazards, and activity levels. Furthermore, the assessment explores cardiovascular, respiratory, musculoskeletal, nutritional, renal, and mental status, along with a section on intimate partner violence. The patient's health goals are also outlined, reflecting his overall well-being and independence despite age-related issues like hearing loss and bronchitis. The assessment provides a comprehensive overview of Robert Walker's health, highlighting various aspects of his medical and personal history, making it a valuable resource for healthcare students studying patient assessment and documentation.
Date ............................................................
Interview conducted by ............................
Designation ................................................
1. Biographical data
Name: Robert Walker
Address: 15 Louis Avenue Brighton 5048
Date of birth: 7th November 1930
Birthplace: Australia
Age: 83 Gender Male Marital status: Married
Occupation: Technical person in a brewery
Employer: Not discussed
Interpreter required? No
Medicare number (Not required for the assignment) .............................................................
Private Heath Fund Details (Not required for the assignment) Not discussed........................
Advanced care directive?
Details: Not discussed
2. History obtained from: The patient himself
3. Reason/s for seeking care ..........................................................................................................
.........................................................................................................................................................
.........................................................................................................................................................
.........................................................................................................................................................
4. Present health or history of present illness At present, the patient is free from the illnesses
like cold and influenza but he is no longer strong enough as he used to be and that he feels tired
most of the times. No serious illness in childhood that dragged him to the hospital. In the last
year, he was appointed for an abdominal operation due to some bowel obstruction.
5. Past health
General health: General condition is good and suffered from no major illness or health issues
Childhood illnesses: No illness detected
Accidents or injuries: Once fell down from a tree and broke the left arm
...........................................................................................................................................................
Source: Jarvis, C & Denmead, E (Australian adapting author) 2012, chapter 7 ‘The health history’, in Student laboratory manual for physical
examination and health assessment, Australian and New Zealand edition, Saunders Elsevier, Sydney, pp. 65–73.
NURS1004 Part 1 Documentation for Health assessment
Interview conducted by ............................
Designation ................................................
1. Biographical data
Name: Robert Walker
Address: 15 Louis Avenue Brighton 5048
Date of birth: 7th November 1930
Birthplace: Australia
Age: 83 Gender Male Marital status: Married
Occupation: Technical person in a brewery
Employer: Not discussed
Interpreter required? No
Medicare number (Not required for the assignment) .............................................................
Private Heath Fund Details (Not required for the assignment) Not discussed........................
Advanced care directive?
Details: Not discussed
2. History obtained from: The patient himself
3. Reason/s for seeking care ..........................................................................................................
.........................................................................................................................................................
.........................................................................................................................................................
.........................................................................................................................................................
4. Present health or history of present illness At present, the patient is free from the illnesses
like cold and influenza but he is no longer strong enough as he used to be and that he feels tired
most of the times. No serious illness in childhood that dragged him to the hospital. In the last
year, he was appointed for an abdominal operation due to some bowel obstruction.
5. Past health
General health: General condition is good and suffered from no major illness or health issues
Childhood illnesses: No illness detected
Accidents or injuries: Once fell down from a tree and broke the left arm
...........................................................................................................................................................
Source: Jarvis, C & Denmead, E (Australian adapting author) 2012, chapter 7 ‘The health history’, in Student laboratory manual for physical
examination and health assessment, Australian and New Zealand edition, Saunders Elsevier, Sydney, pp. 65–73.
NURS1004 Part 1 Documentation for Health assessment
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Serious or chronic illnesses: No such illness. Once had an abdominal operation due to bowel
obstruction
Hospitalisations: For the operation of abdominal issue due to bowel obstruction and once due
to broken leg.
Operations: For the operation of abdominal issue due to bowel obstruction and once due to
broken leg. Cataract operation
Obstetric history ............................................................................................................................
Gravida ....................... Term ....................... Preterm ...........................
(# Pregnancies) (# Term pregnancies) (# Preterm
pregnancies)
Term / Incomplete .................. Children Living ......................................................................
(# Terminations / Miscarriages)
Course of pregnancy .....................................................................................................................
.........................................................................................................................................................
(Date delivery, length of pregnancy, length of labour, baby’s weight and sex, vaginal delivery /
caesarean section, complications, baby’s condition)
Immunisations
Tetanus Current Select Yes................................................................................
Influenza Current Select Yes................................................................................
Pneumococcus Current Select Yes................................................................................
Other ..................................................................................................................................
..............................................................................................................................................
Last GP visit date 20th February 2013..............................................................................................
Health Screening
Dentist Once or twice a year.................. Vision Last year (2012) for cataract
operation
Hearing Earlier this year......................... ECG A number of times..............................
CXR Yes............................................ Other ..........................................................
Allergies: Allergens and reaction – allergy bracelet applied Select .....................................
Drugs / medications No........................................................................................................
Food No...............................................................................................................................
Latex / other No...................................................................................................................
Comments No allergies to any specific thing......................................................................
...............................................................................................................................................
Infection control
Page 2 of 7
obstruction
Hospitalisations: For the operation of abdominal issue due to bowel obstruction and once due
to broken leg.
Operations: For the operation of abdominal issue due to bowel obstruction and once due to
broken leg. Cataract operation
Obstetric history ............................................................................................................................
Gravida ....................... Term ....................... Preterm ...........................
(# Pregnancies) (# Term pregnancies) (# Preterm
pregnancies)
Term / Incomplete .................. Children Living ......................................................................
(# Terminations / Miscarriages)
Course of pregnancy .....................................................................................................................
.........................................................................................................................................................
(Date delivery, length of pregnancy, length of labour, baby’s weight and sex, vaginal delivery /
caesarean section, complications, baby’s condition)
Immunisations
Tetanus Current Select Yes................................................................................
Influenza Current Select Yes................................................................................
Pneumococcus Current Select Yes................................................................................
Other ..................................................................................................................................
..............................................................................................................................................
Last GP visit date 20th February 2013..............................................................................................
Health Screening
Dentist Once or twice a year.................. Vision Last year (2012) for cataract
operation
Hearing Earlier this year......................... ECG A number of times..............................
CXR Yes............................................ Other ..........................................................
Allergies: Allergens and reaction – allergy bracelet applied Select .....................................
Drugs / medications No........................................................................................................
Food No...............................................................................................................................
Latex / other No...................................................................................................................
Comments No allergies to any specific thing......................................................................
...............................................................................................................................................
Infection control
Page 2 of 7
Transmission-based precautions .......................................................................................
Notifiable disease ..............................................................................................................
6. Family history
Heart disease Not known.................................................................................................................
High blood pressure No...................................................................................................................
Stroke No.........................................................................................................................................
Diabetes No......................................................................................................................................
Blood disorders No..........................................................................................................................
Breast cancer No..............................................................................................................................
Cancer (other) Mother died of lung cancer .....................................................................................
Sickle cell No...................................................................................................................................
Arthritis Father might have..............................................................................................................
Allergies No ...................................................................................................................................
Asthma No.......................................................................................................................................
Obesity No one was grossly overweighed.......................................................................................
Alcoholism No.................................................................................................................................
Mental illness No.............................................................................................................................
Seizure disorder No.........................................................................................................................
Kidney disease No............................................................................................................................
Tuberculosis No...............................................................................................................................
Other .............................................................................................................................................
Review of symptoms, function and risks
There is no such risk or symptoms observed regarding the ill health of Robert. Robert has been
doing OK and that he can drive a bike or ride a car. There is no severe health issues identified.
The present condition is due to the old age like loss of hearing.
7. General overall health and wellbeing
Perception of health ........................................................................................................................
Interpersonal relationships / resources ..........................................................................................
Education (last level achieved) Bachelor degree in chemical technology from University
of Adelaide.........................................................................................................................................
Current employment Retired since 1st Jan 1993...................................................................
Family role? ......................................................................................................................
Support systems? Daughters are very supportive, receives pensions from Government
because his wife is blind and gets blind benefit pension...................................................................
Values and beliefs / spiritual resources Believes in cultural practices.............................................
Page 3 of 7
Notifiable disease ..............................................................................................................
6. Family history
Heart disease Not known.................................................................................................................
High blood pressure No...................................................................................................................
Stroke No.........................................................................................................................................
Diabetes No......................................................................................................................................
Blood disorders No..........................................................................................................................
Breast cancer No..............................................................................................................................
Cancer (other) Mother died of lung cancer .....................................................................................
Sickle cell No...................................................................................................................................
Arthritis Father might have..............................................................................................................
Allergies No ...................................................................................................................................
Asthma No.......................................................................................................................................
Obesity No one was grossly overweighed.......................................................................................
Alcoholism No.................................................................................................................................
Mental illness No.............................................................................................................................
Seizure disorder No.........................................................................................................................
Kidney disease No............................................................................................................................
Tuberculosis No...............................................................................................................................
Other .............................................................................................................................................
Review of symptoms, function and risks
There is no such risk or symptoms observed regarding the ill health of Robert. Robert has been
doing OK and that he can drive a bike or ride a car. There is no severe health issues identified.
The present condition is due to the old age like loss of hearing.
7. General overall health and wellbeing
Perception of health ........................................................................................................................
Interpersonal relationships / resources ..........................................................................................
Education (last level achieved) Bachelor degree in chemical technology from University
of Adelaide.........................................................................................................................................
Current employment Retired since 1st Jan 1993...................................................................
Family role? ......................................................................................................................
Support systems? Daughters are very supportive, receives pensions from Government
because his wife is blind and gets blind benefit pension...................................................................
Values and beliefs / spiritual resources Believes in cultural practices.............................................
Page 3 of 7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Cultural background Australian Caucasian..........................................................................
Cultural health practices Nothing mentioned.......................................................................
Religious / spiritual beliefs Goes to Church during Easters................................................
Coping and stress management .....................................................................................................
Stressors in life? Bottle around everything to relive stress..................................................
Methods to relieve stress Go for a walk to overcome stress................................................
Self-concept ..................................................................................................................................
Personal strengths? Still being alive and lively...................................................................
Life values and belief Good sense of humour......................................................................
Sleep / rest .....................................................................................................................................
Sleep pattern? Do not sleep during day but sleeps by 10 PM and read some news before
sleeping. ............................................................................................................................................
Aids used? No......................................................................................................................
8. Health and lifestyles management
Current medications: (prescribed and OTC). Note name, purpose, dose and daily schedule.
Ask specially about vitamins, oral contraceptives, aspirin, sedatives and antacids.
Name of the medicines or the drugs were not properly heard. .........................................................
Tobacco, alcohol and recreational / street drugs
Smoke cigarettes? Yes............................ Number of packs per day Not known........................
Daily use for how many years .. Age started 18............................................................
Ever tried to quit? yes Succeed? Yes...............................................................................
Comments After breathing problem, he left........................................................................
Drink alcohol? Yes Date last alcohol use The very day...............................................................
Amount of alcohol that episode 25 mils of whiskey.............................................................
Out of the last 30 days, how many days had alcohol? 25 days............................................
Ever had a drinking problem? No........................................................................................
Comments Got opportunity during employment in a brewery............................................
Any use of recreational drugs? (reinforce confidentiality of information disclosed)
Which ones No........................................
Marijuana? ............................................ Cocaine? ........................................................
Crack cocaine? ...................................... Amphetamines? ...........................................
Barbiturates? ........................................ LSD? ..............................................................
Heroin? ................................................ Other? ...........................................................
Ever had treatment for drugs or alcohol? ............................................................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
Page 4 of 7
Cultural health practices Nothing mentioned.......................................................................
Religious / spiritual beliefs Goes to Church during Easters................................................
Coping and stress management .....................................................................................................
Stressors in life? Bottle around everything to relive stress..................................................
Methods to relieve stress Go for a walk to overcome stress................................................
Self-concept ..................................................................................................................................
Personal strengths? Still being alive and lively...................................................................
Life values and belief Good sense of humour......................................................................
Sleep / rest .....................................................................................................................................
Sleep pattern? Do not sleep during day but sleeps by 10 PM and read some news before
sleeping. ............................................................................................................................................
Aids used? No......................................................................................................................
8. Health and lifestyles management
Current medications: (prescribed and OTC). Note name, purpose, dose and daily schedule.
Ask specially about vitamins, oral contraceptives, aspirin, sedatives and antacids.
Name of the medicines or the drugs were not properly heard. .........................................................
Tobacco, alcohol and recreational / street drugs
Smoke cigarettes? Yes............................ Number of packs per day Not known........................
Daily use for how many years .. Age started 18............................................................
Ever tried to quit? yes Succeed? Yes...............................................................................
Comments After breathing problem, he left........................................................................
Drink alcohol? Yes Date last alcohol use The very day...............................................................
Amount of alcohol that episode 25 mils of whiskey.............................................................
Out of the last 30 days, how many days had alcohol? 25 days............................................
Ever had a drinking problem? No........................................................................................
Comments Got opportunity during employment in a brewery............................................
Any use of recreational drugs? (reinforce confidentiality of information disclosed)
Which ones No........................................
Marijuana? ............................................ Cocaine? ........................................................
Crack cocaine? ...................................... Amphetamines? ...........................................
Barbiturates? ........................................ LSD? ..............................................................
Heroin? ................................................ Other? ...........................................................
Ever had treatment for drugs or alcohol? ............................................................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
Page 4 of 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
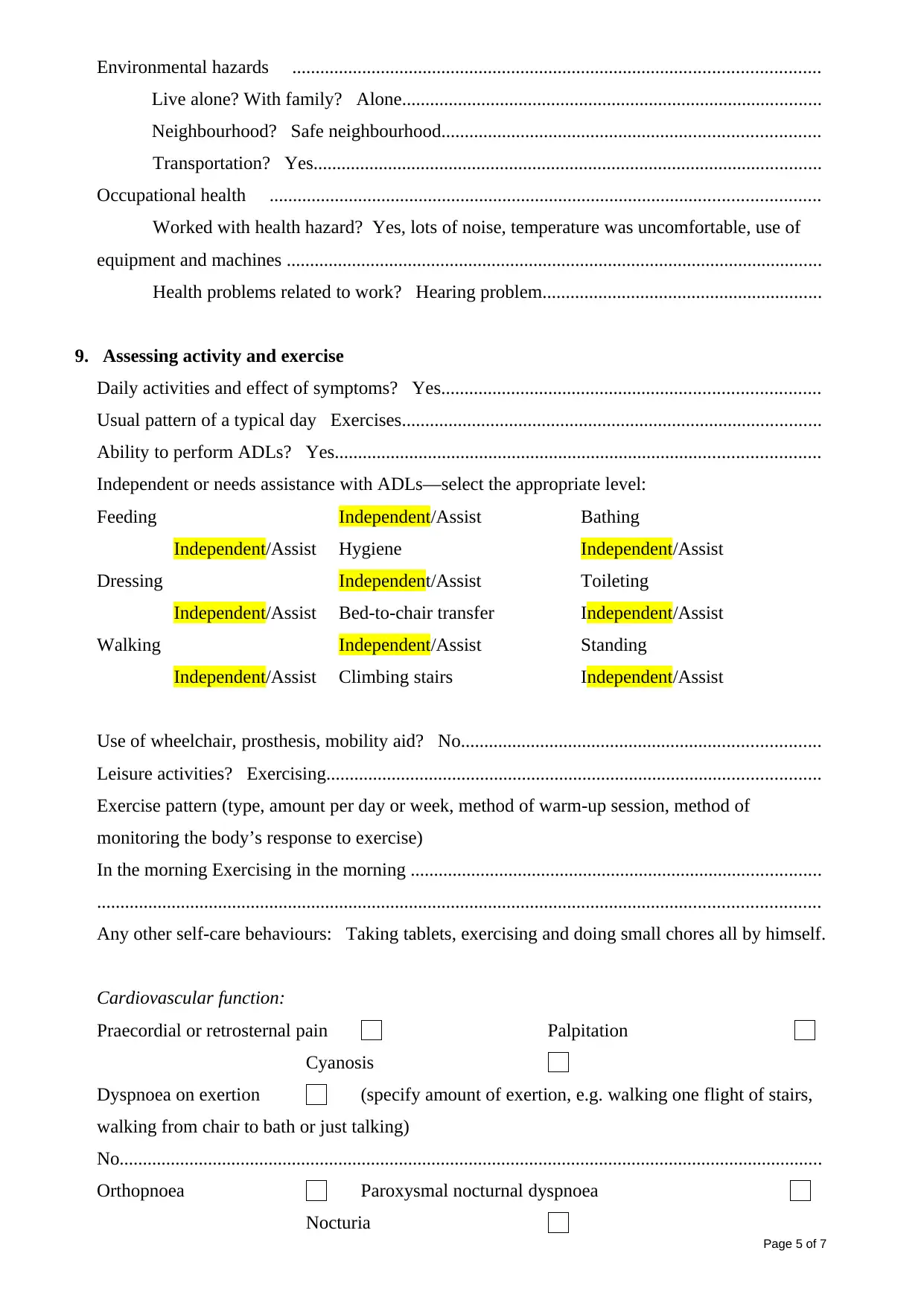
Environmental hazards .................................................................................................................
Live alone? With family? Alone..........................................................................................
Neighbourhood? Safe neighbourhood.................................................................................
Transportation? Yes.............................................................................................................
Occupational health ......................................................................................................................
Worked with health hazard? Yes, lots of noise, temperature was uncomfortable, use of
equipment and machines ...................................................................................................................
Health problems related to work? Hearing problem............................................................
9. Assessing activity and exercise
Daily activities and effect of symptoms? Yes.................................................................................
Usual pattern of a typical day Exercises..........................................................................................
Ability to perform ADLs? Yes........................................................................................................
Independent or needs assistance with ADLs—select the appropriate level:
Feeding Independent/Assist Bathing
Independent/Assist Hygiene Independent/Assist
Dressing Independent/Assist Toileting
Independent/Assist Bed-to-chair transfer Independent/Assist
Walking Independent/Assist Standing
Independent/Assist Climbing stairs Independent/Assist
Use of wheelchair, prosthesis, mobility aid? No.............................................................................
Leisure activities? Exercising..........................................................................................................
Exercise pattern (type, amount per day or week, method of warm-up session, method of
monitoring the body’s response to exercise)
In the morning Exercising in the morning ........................................................................................
...........................................................................................................................................................
Any other self-care behaviours: Taking tablets, exercising and doing small chores all by himself.
Cardiovascular function:
Praecordial or retrosternal pain Palpitation
Cyanosis
Dyspnoea on exertion (specify amount of exertion, e.g. walking one flight of stairs,
walking from chair to bath or just talking)
No.......................................................................................................................................................
Orthopnoea Paroxysmal nocturnal dyspnoea
Nocturia
Page 5 of 7
Live alone? With family? Alone..........................................................................................
Neighbourhood? Safe neighbourhood.................................................................................
Transportation? Yes.............................................................................................................
Occupational health ......................................................................................................................
Worked with health hazard? Yes, lots of noise, temperature was uncomfortable, use of
equipment and machines ...................................................................................................................
Health problems related to work? Hearing problem............................................................
9. Assessing activity and exercise
Daily activities and effect of symptoms? Yes.................................................................................
Usual pattern of a typical day Exercises..........................................................................................
Ability to perform ADLs? Yes........................................................................................................
Independent or needs assistance with ADLs—select the appropriate level:
Feeding Independent/Assist Bathing
Independent/Assist Hygiene Independent/Assist
Dressing Independent/Assist Toileting
Independent/Assist Bed-to-chair transfer Independent/Assist
Walking Independent/Assist Standing
Independent/Assist Climbing stairs Independent/Assist
Use of wheelchair, prosthesis, mobility aid? No.............................................................................
Leisure activities? Exercising..........................................................................................................
Exercise pattern (type, amount per day or week, method of warm-up session, method of
monitoring the body’s response to exercise)
In the morning Exercising in the morning ........................................................................................
...........................................................................................................................................................
Any other self-care behaviours: Taking tablets, exercising and doing small chores all by himself.
Cardiovascular function:
Praecordial or retrosternal pain Palpitation
Cyanosis
Dyspnoea on exertion (specify amount of exertion, e.g. walking one flight of stairs,
walking from chair to bath or just talking)
No.......................................................................................................................................................
Orthopnoea Paroxysmal nocturnal dyspnoea
Nocturia
Page 5 of 7
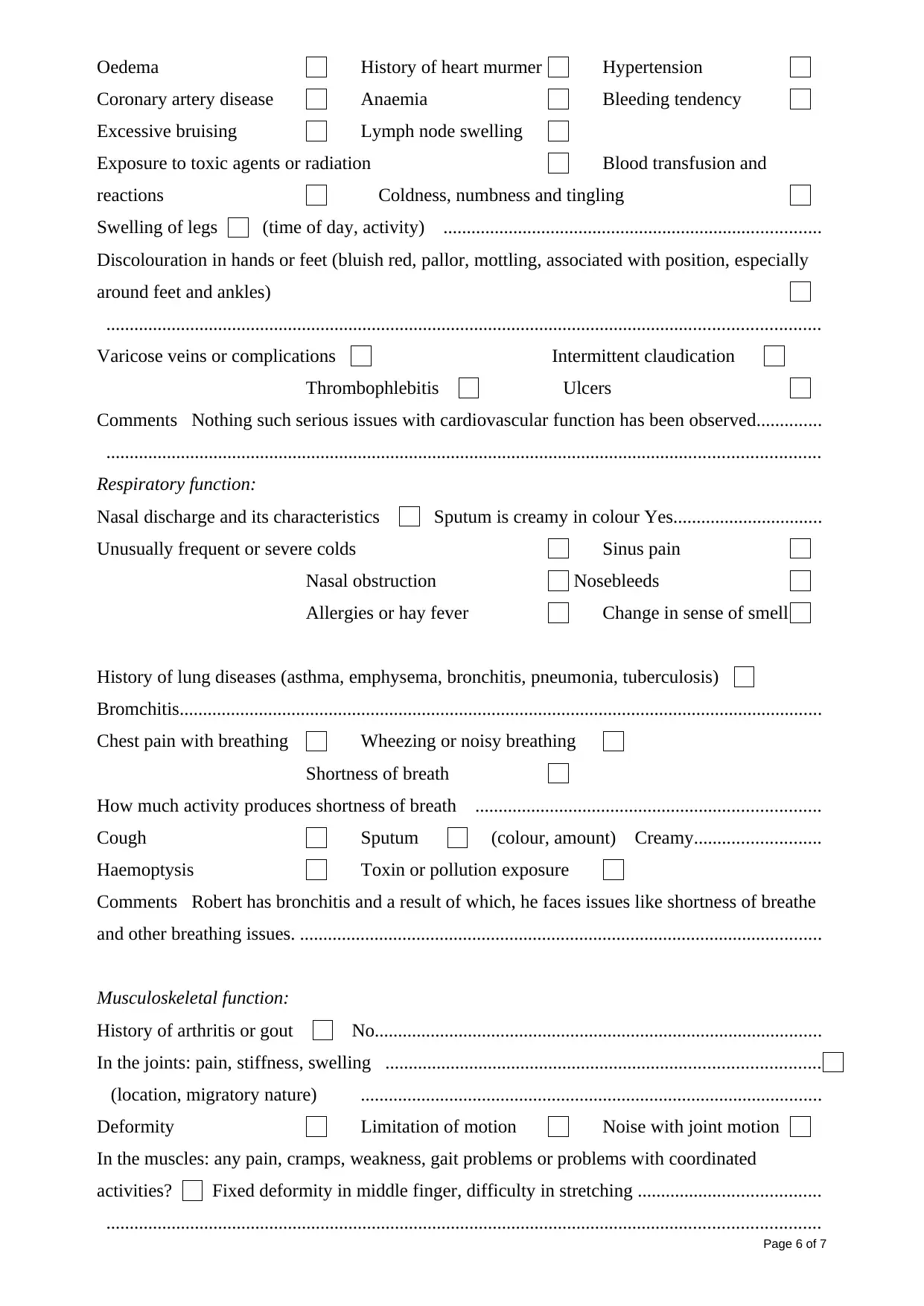
Oedema History of heart murmer Hypertension
Coronary artery disease Anaemia Bleeding tendency
Excessive bruising Lymph node swelling
Exposure to toxic agents or radiation Blood transfusion and
reactions Coldness, numbness and tingling
Swelling of legs (time of day, activity) .................................................................................
Discolouration in hands or feet (bluish red, pallor, mottling, associated with position, especially
around feet and ankles)
.........................................................................................................................................................
Varicose veins or complications Intermittent claudication
Thrombophlebitis Ulcers
Comments Nothing such serious issues with cardiovascular function has been observed..............
.........................................................................................................................................................
Respiratory function:
Nasal discharge and its characteristics Sputum is creamy in colour Yes................................
Unusually frequent or severe colds Sinus pain
Nasal obstruction Nosebleeds
Allergies or hay fever Change in sense of smell
History of lung diseases (asthma, emphysema, bronchitis, pneumonia, tuberculosis)
Bromchitis..........................................................................................................................................
Chest pain with breathing Wheezing or noisy breathing
Shortness of breath
How much activity produces shortness of breath ..........................................................................
Cough Sputum (colour, amount) Creamy...........................
Haemoptysis Toxin or pollution exposure
Comments Robert has bronchitis and a result of which, he faces issues like shortness of breathe
and other breathing issues. ................................................................................................................
Musculoskeletal function:
History of arthritis or gout No................................................................................................
In the joints: pain, stiffness, swelling .............................................................................................
(location, migratory nature) ...................................................................................................
Deformity Limitation of motion Noise with joint motion
In the muscles: any pain, cramps, weakness, gait problems or problems with coordinated
activities? Fixed deformity in middle finger, difficulty in stretching .......................................
.........................................................................................................................................................
Page 6 of 7
Coronary artery disease Anaemia Bleeding tendency
Excessive bruising Lymph node swelling
Exposure to toxic agents or radiation Blood transfusion and
reactions Coldness, numbness and tingling
Swelling of legs (time of day, activity) .................................................................................
Discolouration in hands or feet (bluish red, pallor, mottling, associated with position, especially
around feet and ankles)
.........................................................................................................................................................
Varicose veins or complications Intermittent claudication
Thrombophlebitis Ulcers
Comments Nothing such serious issues with cardiovascular function has been observed..............
.........................................................................................................................................................
Respiratory function:
Nasal discharge and its characteristics Sputum is creamy in colour Yes................................
Unusually frequent or severe colds Sinus pain
Nasal obstruction Nosebleeds
Allergies or hay fever Change in sense of smell
History of lung diseases (asthma, emphysema, bronchitis, pneumonia, tuberculosis)
Bromchitis..........................................................................................................................................
Chest pain with breathing Wheezing or noisy breathing
Shortness of breath
How much activity produces shortness of breath ..........................................................................
Cough Sputum (colour, amount) Creamy...........................
Haemoptysis Toxin or pollution exposure
Comments Robert has bronchitis and a result of which, he faces issues like shortness of breathe
and other breathing issues. ................................................................................................................
Musculoskeletal function:
History of arthritis or gout No................................................................................................
In the joints: pain, stiffness, swelling .............................................................................................
(location, migratory nature) ...................................................................................................
Deformity Limitation of motion Noise with joint motion
In the muscles: any pain, cramps, weakness, gait problems or problems with coordinated
activities? Fixed deformity in middle finger, difficulty in stretching .......................................
.........................................................................................................................................................
Page 6 of 7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
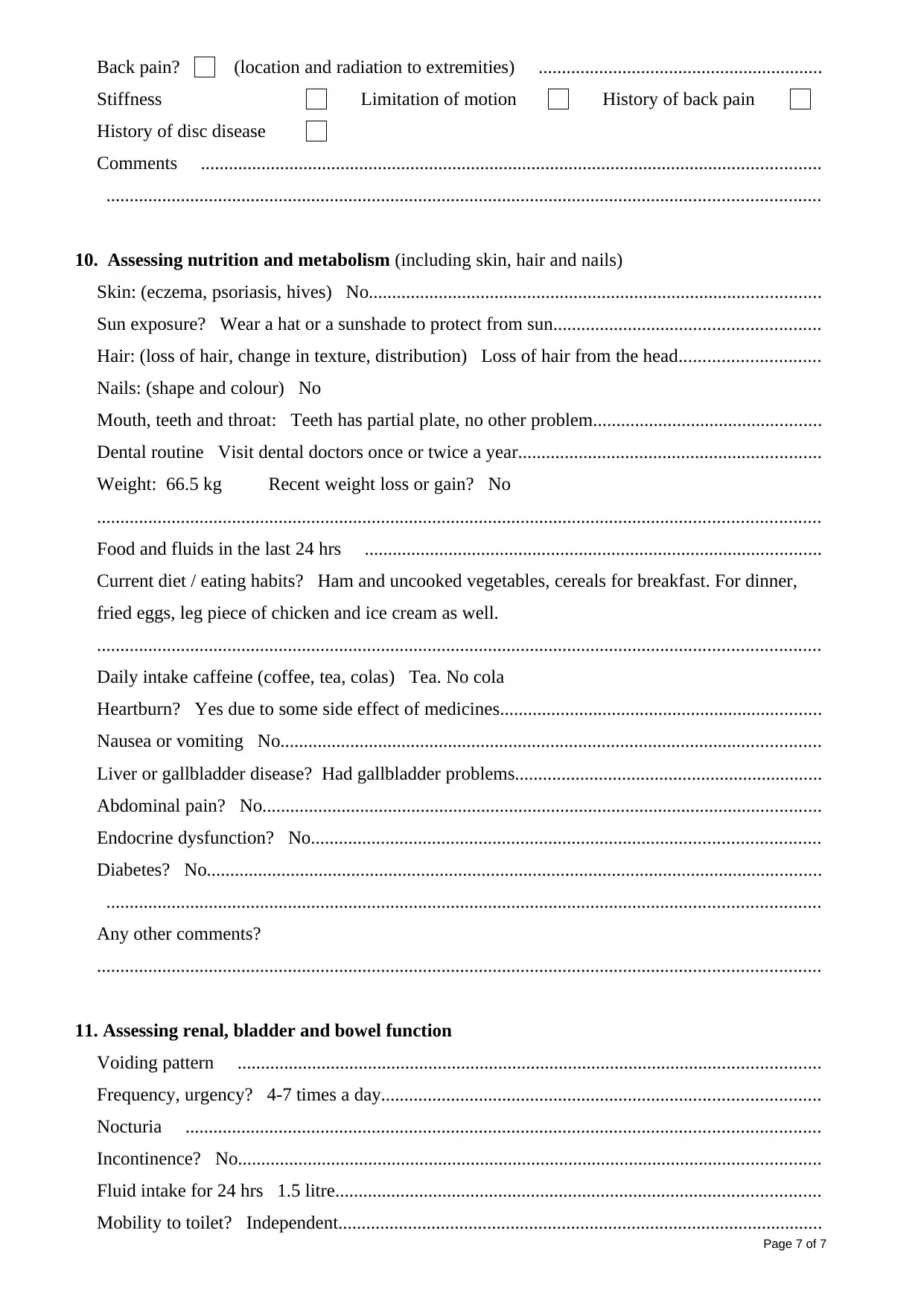
Back pain? (location and radiation to extremities) .............................................................
Stiffness Limitation of motion History of back pain
History of disc disease
Comments .....................................................................................................................................
.........................................................................................................................................................
10. Assessing nutrition and metabolism (including skin, hair and nails)
Skin: (eczema, psoriasis, hives) No.................................................................................................
Sun exposure? Wear a hat or a sunshade to protect from sun.........................................................
Hair: (loss of hair, change in texture, distribution) Loss of hair from the head..............................
Nails: (shape and colour) No
Mouth, teeth and throat: Teeth has partial plate, no other problem.................................................
Dental routine Visit dental doctors once or twice a year.................................................................
Weight: 66.5 kg Recent weight loss or gain? No
...........................................................................................................................................................
Food and fluids in the last 24 hrs ..................................................................................................
Current diet / eating habits? Ham and uncooked vegetables, cereals for breakfast. For dinner,
fried eggs, leg piece of chicken and ice cream as well.
...........................................................................................................................................................
Daily intake caffeine (coffee, tea, colas) Tea. No cola
Heartburn? Yes due to some side effect of medicines.....................................................................
Nausea or vomiting No....................................................................................................................
Liver or gallbladder disease? Had gallbladder problems..................................................................
Abdominal pain? No........................................................................................................................
Endocrine dysfunction? No.............................................................................................................
Diabetes? No....................................................................................................................................
.........................................................................................................................................................
Any other comments?
...........................................................................................................................................................
11. Assessing renal, bladder and bowel function
Voiding pattern .............................................................................................................................
Frequency, urgency? 4-7 times a day..............................................................................................
Nocturia ........................................................................................................................................
Incontinence? No.............................................................................................................................
Fluid intake for 24 hrs 1.5 litre........................................................................................................
Mobility to toilet? Independent........................................................................................................
Page 7 of 7
Stiffness Limitation of motion History of back pain
History of disc disease
Comments .....................................................................................................................................
.........................................................................................................................................................
10. Assessing nutrition and metabolism (including skin, hair and nails)
Skin: (eczema, psoriasis, hives) No.................................................................................................
Sun exposure? Wear a hat or a sunshade to protect from sun.........................................................
Hair: (loss of hair, change in texture, distribution) Loss of hair from the head..............................
Nails: (shape and colour) No
Mouth, teeth and throat: Teeth has partial plate, no other problem.................................................
Dental routine Visit dental doctors once or twice a year.................................................................
Weight: 66.5 kg Recent weight loss or gain? No
...........................................................................................................................................................
Food and fluids in the last 24 hrs ..................................................................................................
Current diet / eating habits? Ham and uncooked vegetables, cereals for breakfast. For dinner,
fried eggs, leg piece of chicken and ice cream as well.
...........................................................................................................................................................
Daily intake caffeine (coffee, tea, colas) Tea. No cola
Heartburn? Yes due to some side effect of medicines.....................................................................
Nausea or vomiting No....................................................................................................................
Liver or gallbladder disease? Had gallbladder problems..................................................................
Abdominal pain? No........................................................................................................................
Endocrine dysfunction? No.............................................................................................................
Diabetes? No....................................................................................................................................
.........................................................................................................................................................
Any other comments?
...........................................................................................................................................................
11. Assessing renal, bladder and bowel function
Voiding pattern .............................................................................................................................
Frequency, urgency? 4-7 times a day..............................................................................................
Nocturia ........................................................................................................................................
Incontinence? No.............................................................................................................................
Fluid intake for 24 hrs 1.5 litre........................................................................................................
Mobility to toilet? Independent........................................................................................................
Page 7 of 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
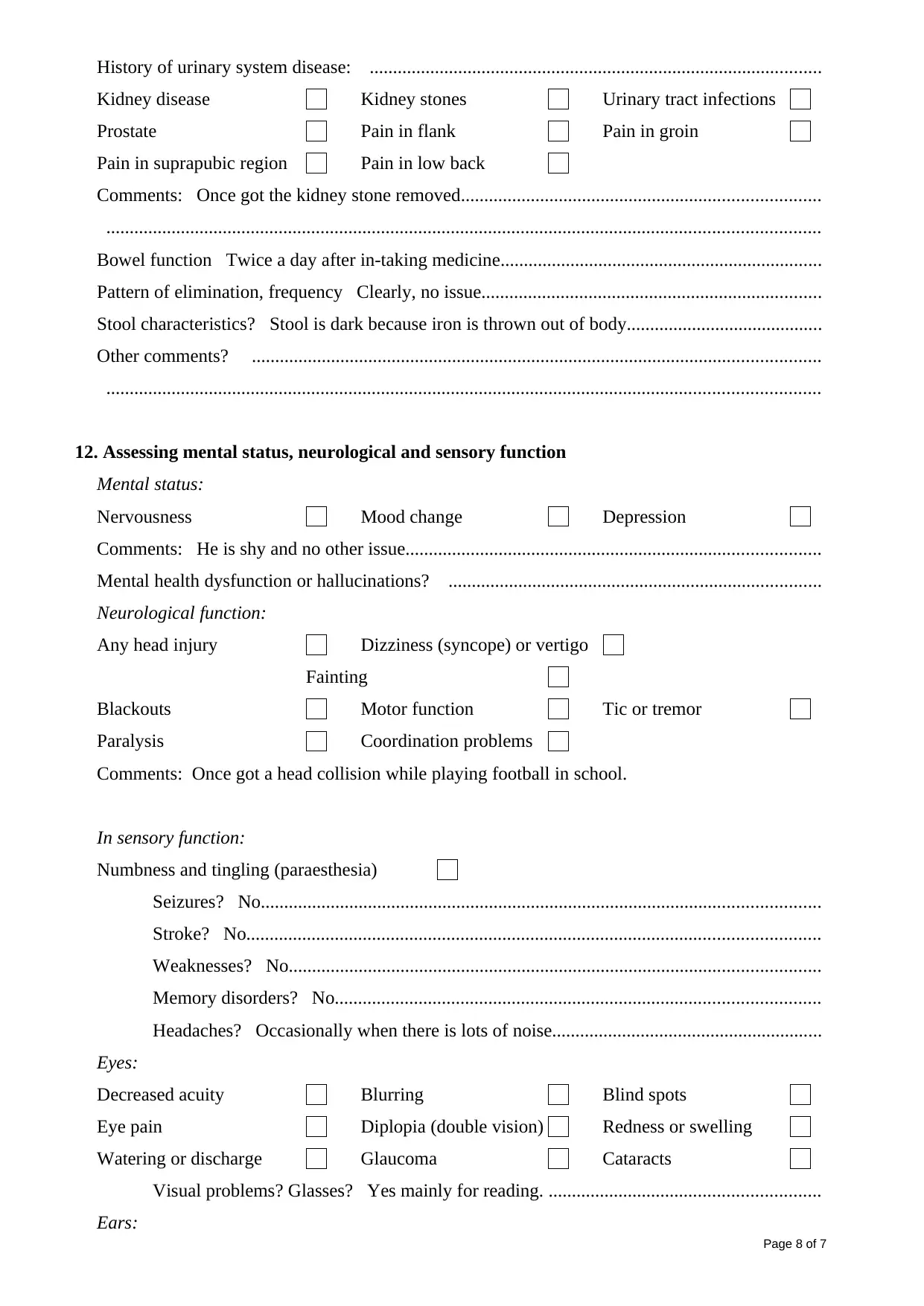
History of urinary system disease: .................................................................................................
Kidney disease Kidney stones Urinary tract infections
Prostate Pain in flank Pain in groin
Pain in suprapubic region Pain in low back
Comments: Once got the kidney stone removed.............................................................................
.........................................................................................................................................................
Bowel function Twice a day after in-taking medicine.....................................................................
Pattern of elimination, frequency Clearly, no issue.........................................................................
Stool characteristics? Stool is dark because iron is thrown out of body..........................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
12. Assessing mental status, neurological and sensory function
Mental status:
Nervousness Mood change Depression
Comments: He is shy and no other issue.........................................................................................
Mental health dysfunction or hallucinations? ................................................................................
Neurological function:
Any head injury Dizziness (syncope) or vertigo
Fainting
Blackouts Motor function Tic or tremor
Paralysis Coordination problems
Comments: Once got a head collision while playing football in school.
In sensory function:
Numbness and tingling (paraesthesia)
Seizures? No........................................................................................................................
Stroke? No...........................................................................................................................
Weaknesses? No..................................................................................................................
Memory disorders? No........................................................................................................
Headaches? Occasionally when there is lots of noise..........................................................
Eyes:
Decreased acuity Blurring Blind spots
Eye pain Diplopia (double vision) Redness or swelling
Watering or discharge Glaucoma Cataracts
Visual problems? Glasses? Yes mainly for reading. ..........................................................
Ears:
Page 8 of 7
Kidney disease Kidney stones Urinary tract infections
Prostate Pain in flank Pain in groin
Pain in suprapubic region Pain in low back
Comments: Once got the kidney stone removed.............................................................................
.........................................................................................................................................................
Bowel function Twice a day after in-taking medicine.....................................................................
Pattern of elimination, frequency Clearly, no issue.........................................................................
Stool characteristics? Stool is dark because iron is thrown out of body..........................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
12. Assessing mental status, neurological and sensory function
Mental status:
Nervousness Mood change Depression
Comments: He is shy and no other issue.........................................................................................
Mental health dysfunction or hallucinations? ................................................................................
Neurological function:
Any head injury Dizziness (syncope) or vertigo
Fainting
Blackouts Motor function Tic or tremor
Paralysis Coordination problems
Comments: Once got a head collision while playing football in school.
In sensory function:
Numbness and tingling (paraesthesia)
Seizures? No........................................................................................................................
Stroke? No...........................................................................................................................
Weaknesses? No..................................................................................................................
Memory disorders? No........................................................................................................
Headaches? Occasionally when there is lots of noise..........................................................
Eyes:
Decreased acuity Blurring Blind spots
Eye pain Diplopia (double vision) Redness or swelling
Watering or discharge Glaucoma Cataracts
Visual problems? Glasses? Yes mainly for reading. ..........................................................
Ears:
Page 8 of 7
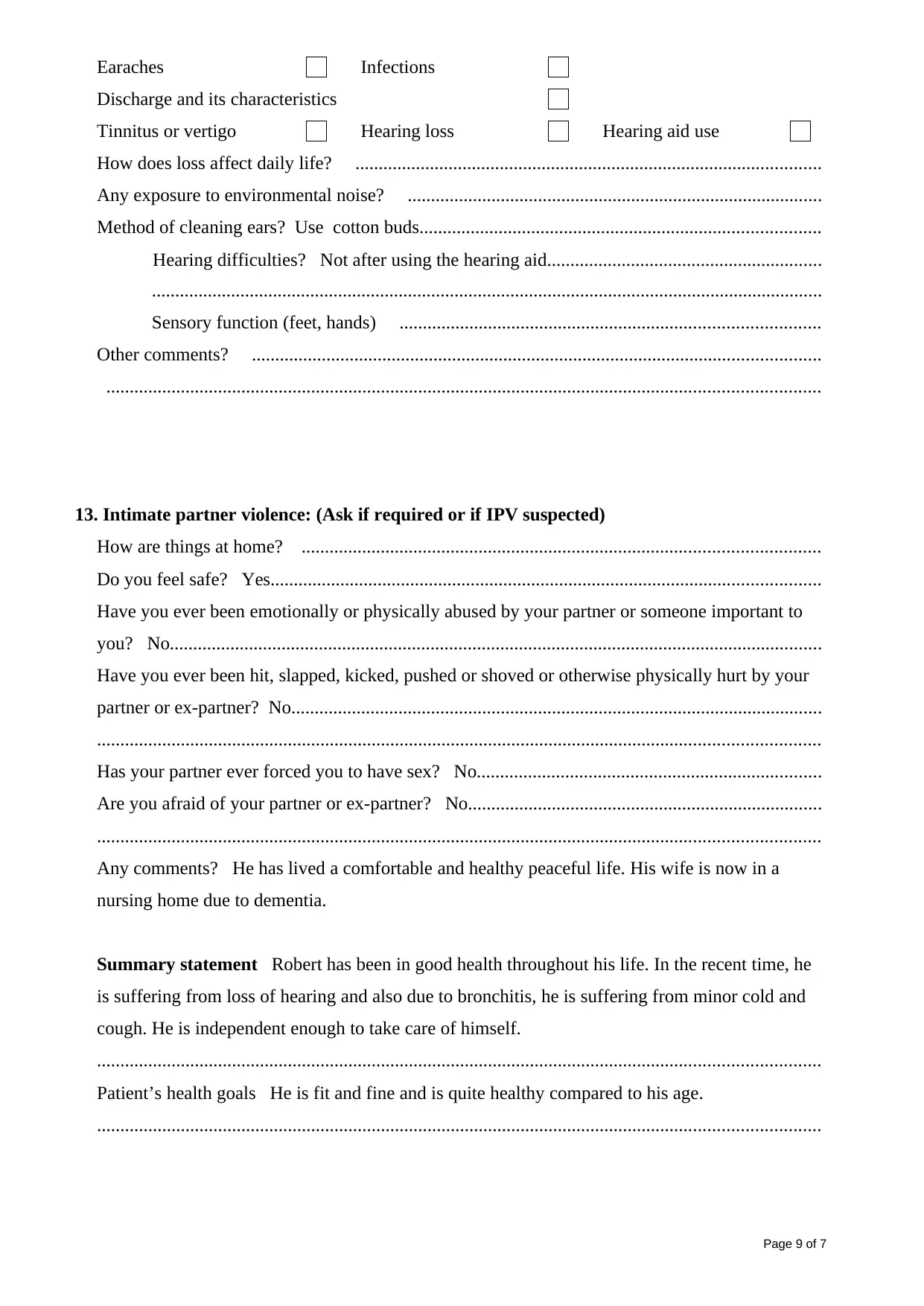
Earaches Infections
Discharge and its characteristics
Tinnitus or vertigo Hearing loss Hearing aid use
How does loss affect daily life? ....................................................................................................
Any exposure to environmental noise? .........................................................................................
Method of cleaning ears? Use cotton buds......................................................................................
Hearing difficulties? Not after using the hearing aid...........................................................
................................................................................................................................................
Sensory function (feet, hands) ..........................................................................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
13. Intimate partner violence: (Ask if required or if IPV suspected)
How are things at home? ...............................................................................................................
Do you feel safe? Yes......................................................................................................................
Have you ever been emotionally or physically abused by your partner or someone important to
you? No............................................................................................................................................
Have you ever been hit, slapped, kicked, pushed or shoved or otherwise physically hurt by your
partner or ex-partner? No..................................................................................................................
...........................................................................................................................................................
Has your partner ever forced you to have sex? No..........................................................................
Are you afraid of your partner or ex-partner? No............................................................................
...........................................................................................................................................................
Any comments? He has lived a comfortable and healthy peaceful life. His wife is now in a
nursing home due to dementia.
Summary statement Robert has been in good health throughout his life. In the recent time, he
is suffering from loss of hearing and also due to bronchitis, he is suffering from minor cold and
cough. He is independent enough to take care of himself.
...........................................................................................................................................................
Patient’s health goals He is fit and fine and is quite healthy compared to his age.
...........................................................................................................................................................
Page 9 of 7
Discharge and its characteristics
Tinnitus or vertigo Hearing loss Hearing aid use
How does loss affect daily life? ....................................................................................................
Any exposure to environmental noise? .........................................................................................
Method of cleaning ears? Use cotton buds......................................................................................
Hearing difficulties? Not after using the hearing aid...........................................................
................................................................................................................................................
Sensory function (feet, hands) ..........................................................................................
Other comments? ..........................................................................................................................
.........................................................................................................................................................
13. Intimate partner violence: (Ask if required or if IPV suspected)
How are things at home? ...............................................................................................................
Do you feel safe? Yes......................................................................................................................
Have you ever been emotionally or physically abused by your partner or someone important to
you? No............................................................................................................................................
Have you ever been hit, slapped, kicked, pushed or shoved or otherwise physically hurt by your
partner or ex-partner? No..................................................................................................................
...........................................................................................................................................................
Has your partner ever forced you to have sex? No..........................................................................
Are you afraid of your partner or ex-partner? No............................................................................
...........................................................................................................................................................
Any comments? He has lived a comfortable and healthy peaceful life. His wife is now in a
nursing home due to dementia.
Summary statement Robert has been in good health throughout his life. In the recent time, he
is suffering from loss of hearing and also due to bronchitis, he is suffering from minor cold and
cough. He is independent enough to take care of himself.
...........................................................................................................................................................
Patient’s health goals He is fit and fine and is quite healthy compared to his age.
...........................................................................................................................................................
Page 9 of 7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




