Health Assessment: Analyzing Mr. Williams' Nursing Case Report
VerifiedAdded on 2022/10/10
|13
|2169
|102
Report
AI Summary
This report presents a comprehensive nursing assessment of Mr. Williams, a 48-year-old patient admitted after a workplace fall. The assessment begins with a detailed analysis of the provided ISBAR handover and video observations, including neurological, cardiovascular, respiratory, musculoskeletal, gastrointestinal, integument, endocrine, and psychosocial data/cues. Part B focuses on identifying actual and potential nursing problems such as pain, fluid and electrolyte imbalance, stress and anxiety, and breathing problems, along with their rationales. Open-ended questions are formulated for each problem to guide assessment and evaluation. Part C discusses the importance of accurate nursing assessments, highlighting the biomedical approach and the primary/secondary survey approach as essential frameworks. The report emphasizes the ethical responsibility of nurses to provide comprehensive care, adhering to NMBA standards, and the consequences of inadequate assessment. The report concludes with a discussion on the connection between pain and other medical conditions, such as tachypnea and tachycardia, differentiating the two conditions. References are provided to support the analysis.

Running head: NURSING ASSIGNMENT
NURSUNG ASSIGNMENT
Name of the Student
Name of the University
Author note
NURSUNG ASSIGNMENT
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING ASSIGNMENT
Table of Contents
Part A...............................................................................................................................................2
Part B...............................................................................................................................................2
Part C...............................................................................................................................................8
References......................................................................................................................................11
Table of Contents
Part A...............................................................................................................................................2
Part B...............................................................................................................................................2
Part C...............................................................................................................................................8
References......................................................................................................................................11
2NURSING ASSIGNMENT
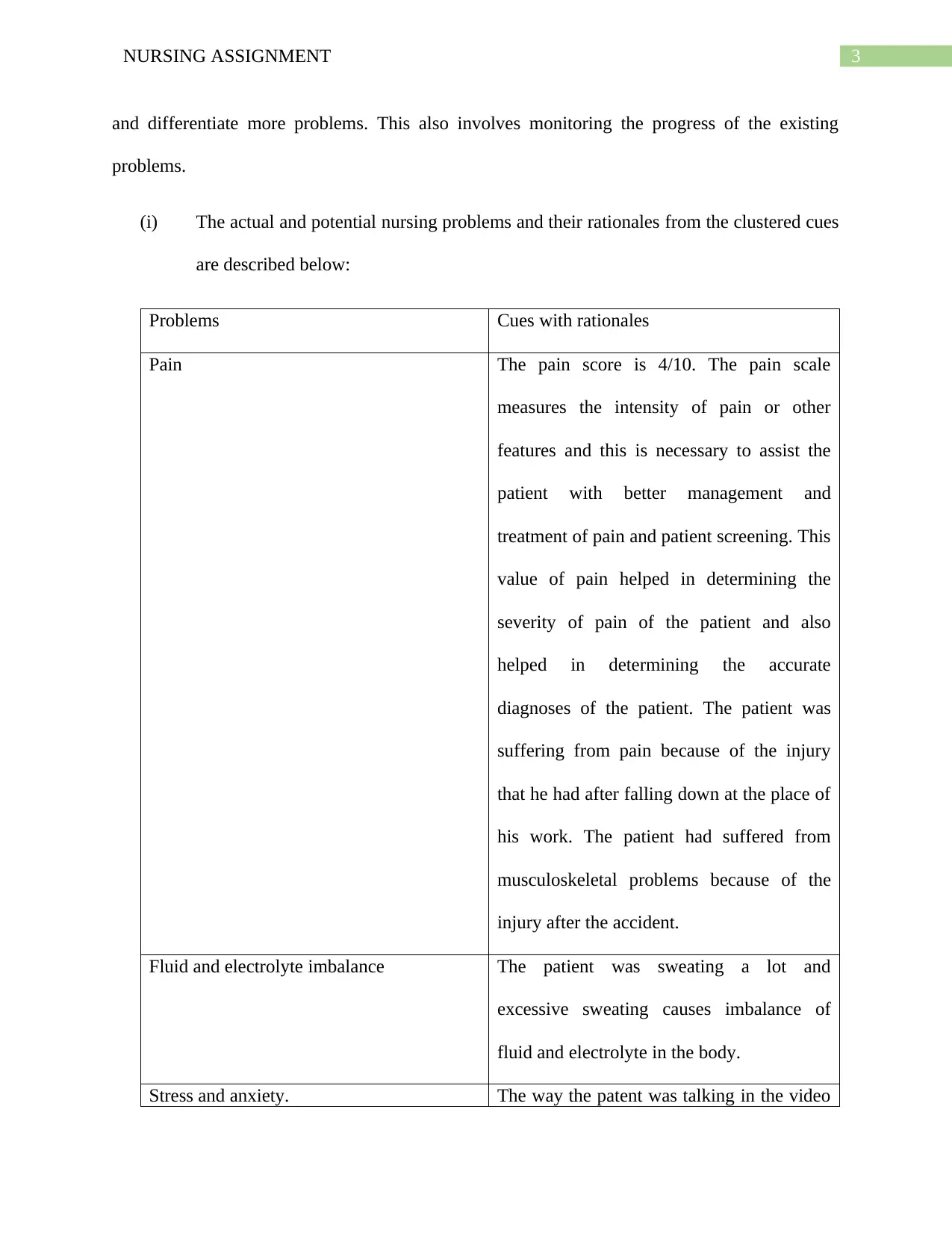
Part A
The data and cue available are described below:
Neurological- Both the subjective and objective symptoms are normal.
Cardiovascular- The objective symptoms were shortness of breath, sweating and anxiety. The
subjective symptom is increase in heart rate.
Respiratory- The objective symptom is breathlessness and the subjective symptoms are
respiratory rate 25, concentration of oxygen saturation – 94% on room air, high heart rate of 105,
high blood pressure of 150/80 and temperature 37.8.
Musculoskeletal- The objective symptom is his right arm is supported in a sling and the
subjective symptoms are three fractures on the right side of his ribs and dislocation of the right
shoulder.
Gastrointestinal – Both the subjective and objective symptoms are normal.
Integument- The symptom that was observed was that because of the accident the patient had a
significant bruising on the right upper thigh. The patient was suffering from pain because of this.
Endocrine- Both the symptoms are normal
Psychosocial- The objective symptom was that she was under severe stress and anxiety and the
subjective symptom was that his blood pressure had increased.
Part B
The nurse identify the possible nursing problems from the clustered cues and focus on how to do
the assessments. This means undertaking much more assessments on the patients for identifying
Part A
The data and cue available are described below:
Neurological- Both the subjective and objective symptoms are normal.
Cardiovascular- The objective symptoms were shortness of breath, sweating and anxiety. The
subjective symptom is increase in heart rate.
Respiratory- The objective symptom is breathlessness and the subjective symptoms are
respiratory rate 25, concentration of oxygen saturation – 94% on room air, high heart rate of 105,
high blood pressure of 150/80 and temperature 37.8.
Musculoskeletal- The objective symptom is his right arm is supported in a sling and the
subjective symptoms are three fractures on the right side of his ribs and dislocation of the right
shoulder.
Gastrointestinal – Both the subjective and objective symptoms are normal.
Integument- The symptom that was observed was that because of the accident the patient had a
significant bruising on the right upper thigh. The patient was suffering from pain because of this.
Endocrine- Both the symptoms are normal
Psychosocial- The objective symptom was that she was under severe stress and anxiety and the
subjective symptom was that his blood pressure had increased.
Part B
The nurse identify the possible nursing problems from the clustered cues and focus on how to do
the assessments. This means undertaking much more assessments on the patients for identifying
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING ASSIGNMENT
and differentiate more problems. This also involves monitoring the progress of the existing
problems.
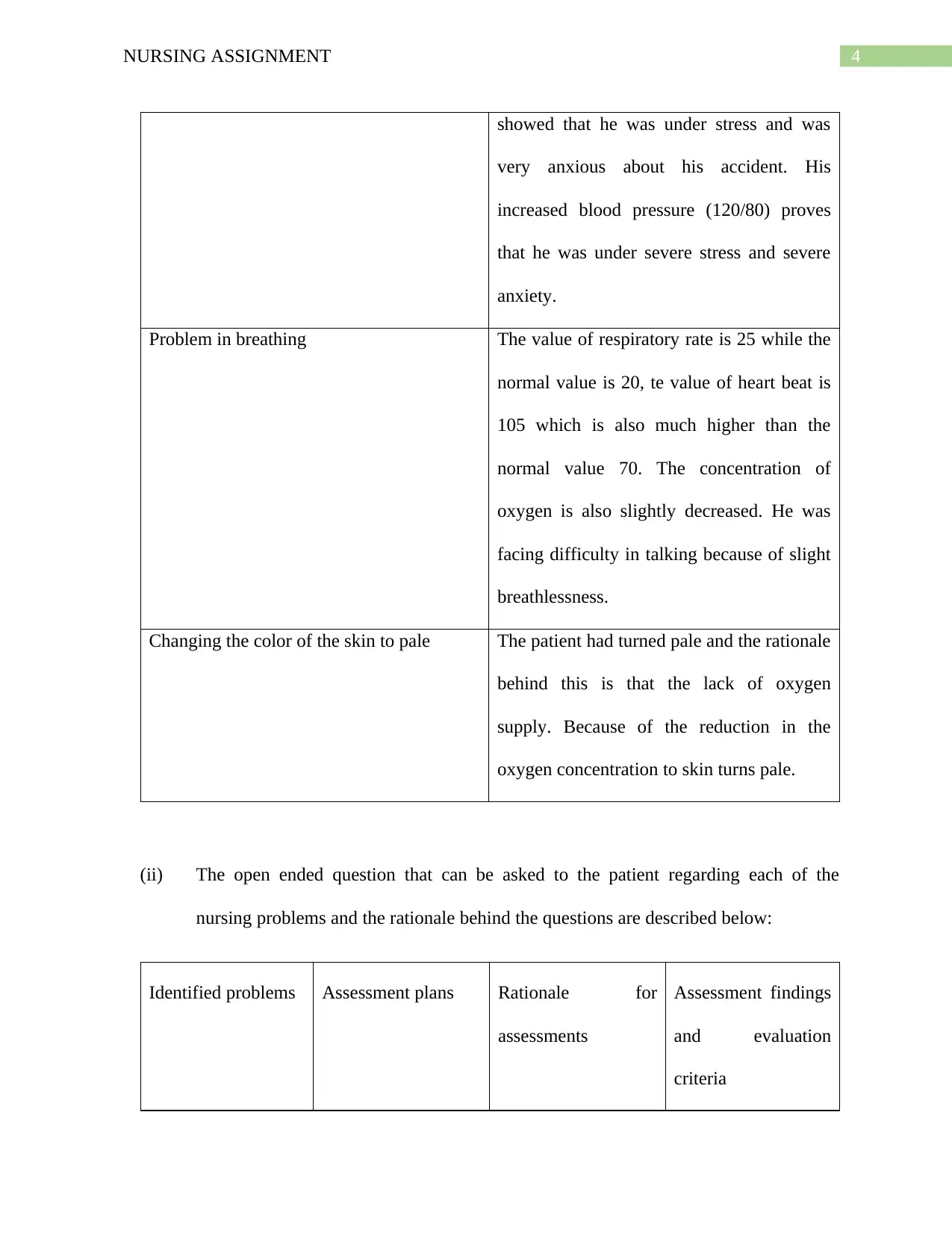
(i) The actual and potential nursing problems and their rationales from the clustered cues
are described below:
Problems Cues with rationales
Pain The pain score is 4/10. The pain scale
measures the intensity of pain or other
features and this is necessary to assist the
patient with better management and
treatment of pain and patient screening. This
value of pain helped in determining the
severity of pain of the patient and also
helped in determining the accurate
diagnoses of the patient. The patient was
suffering from pain because of the injury
that he had after falling down at the place of
his work. The patient had suffered from
musculoskeletal problems because of the
injury after the accident.
Fluid and electrolyte imbalance The patient was sweating a lot and
excessive sweating causes imbalance of
fluid and electrolyte in the body.
Stress and anxiety. The way the patent was talking in the video
and differentiate more problems. This also involves monitoring the progress of the existing
problems.
(i) The actual and potential nursing problems and their rationales from the clustered cues
are described below:
Problems Cues with rationales
Pain The pain score is 4/10. The pain scale
measures the intensity of pain or other
features and this is necessary to assist the
patient with better management and
treatment of pain and patient screening. This
value of pain helped in determining the
severity of pain of the patient and also
helped in determining the accurate
diagnoses of the patient. The patient was
suffering from pain because of the injury
that he had after falling down at the place of
his work. The patient had suffered from
musculoskeletal problems because of the
injury after the accident.
Fluid and electrolyte imbalance The patient was sweating a lot and
excessive sweating causes imbalance of
fluid and electrolyte in the body.
Stress and anxiety. The way the patent was talking in the video
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ASSIGNMENT
showed that he was under stress and was
very anxious about his accident. His
increased blood pressure (120/80) proves
that he was under severe stress and severe
anxiety.
Problem in breathing The value of respiratory rate is 25 while the
normal value is 20, te value of heart beat is
105 which is also much higher than the
normal value 70. The concentration of
oxygen is also slightly decreased. He was
facing difficulty in talking because of slight
breathlessness.
Changing the color of the skin to pale The patient had turned pale and the rationale
behind this is that the lack of oxygen
supply. Because of the reduction in the
oxygen concentration to skin turns pale.
(ii) The open ended question that can be asked to the patient regarding each of the
nursing problems and the rationale behind the questions are described below:
Identified problems Assessment plans Rationale for
assessments
Assessment findings
and evaluation
criteria
showed that he was under stress and was
very anxious about his accident. His
increased blood pressure (120/80) proves
that he was under severe stress and severe
anxiety.
Problem in breathing The value of respiratory rate is 25 while the
normal value is 20, te value of heart beat is
105 which is also much higher than the
normal value 70. The concentration of
oxygen is also slightly decreased. He was
facing difficulty in talking because of slight
breathlessness.
Changing the color of the skin to pale The patient had turned pale and the rationale
behind this is that the lack of oxygen
supply. Because of the reduction in the
oxygen concentration to skin turns pale.
(ii) The open ended question that can be asked to the patient regarding each of the
nursing problems and the rationale behind the questions are described below:
Identified problems Assessment plans Rationale for
assessments
Assessment findings
and evaluation
criteria
5NURSING ASSIGNMENT
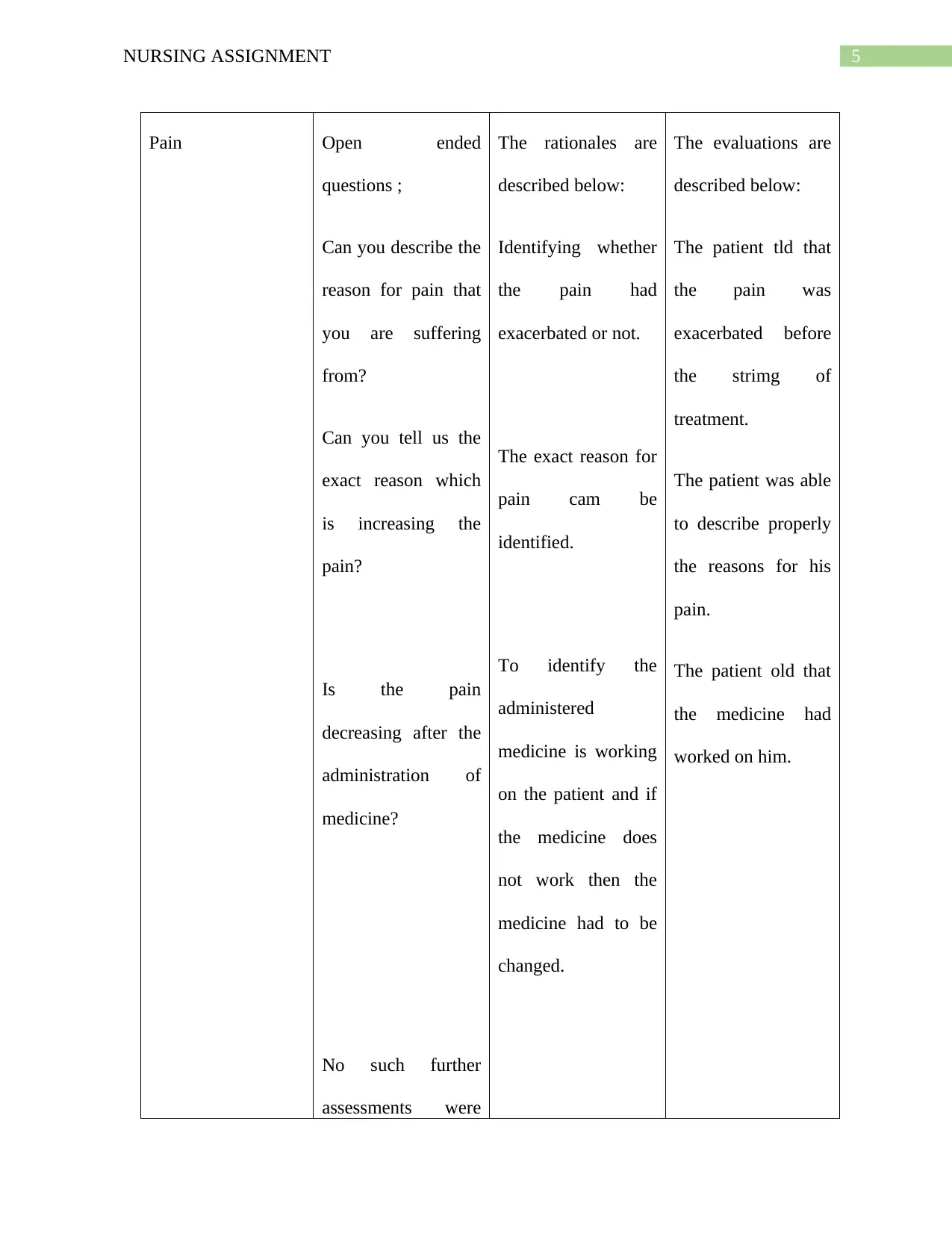
Pain Open ended
questions ;
Can you describe the
reason for pain that
you are suffering
from?
Can you tell us the
exact reason which
is increasing the
pain?
Is the pain
decreasing after the
administration of
medicine?
No such further
assessments were
The rationales are
described below:
Identifying whether
the pain had
exacerbated or not.
The exact reason for
pain cam be
identified.
To identify the
administered
medicine is working
on the patient and if
the medicine does
not work then the
medicine had to be
changed.
The evaluations are
described below:
The patient tld that
the pain was
exacerbated before
the strimg of
treatment.
The patient was able
to describe properly
the reasons for his
pain.
The patient old that
the medicine had
worked on him.
Pain Open ended
questions ;
Can you describe the
reason for pain that
you are suffering
from?
Can you tell us the
exact reason which
is increasing the
pain?
Is the pain
decreasing after the
administration of
medicine?
No such further
assessments were
The rationales are
described below:
Identifying whether
the pain had
exacerbated or not.
The exact reason for
pain cam be
identified.
To identify the
administered
medicine is working
on the patient and if
the medicine does
not work then the
medicine had to be
changed.
The evaluations are
described below:
The patient tld that
the pain was
exacerbated before
the strimg of
treatment.
The patient was able
to describe properly
the reasons for his
pain.
The patient old that
the medicine had
worked on him.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING ASSIGNMENT
required.
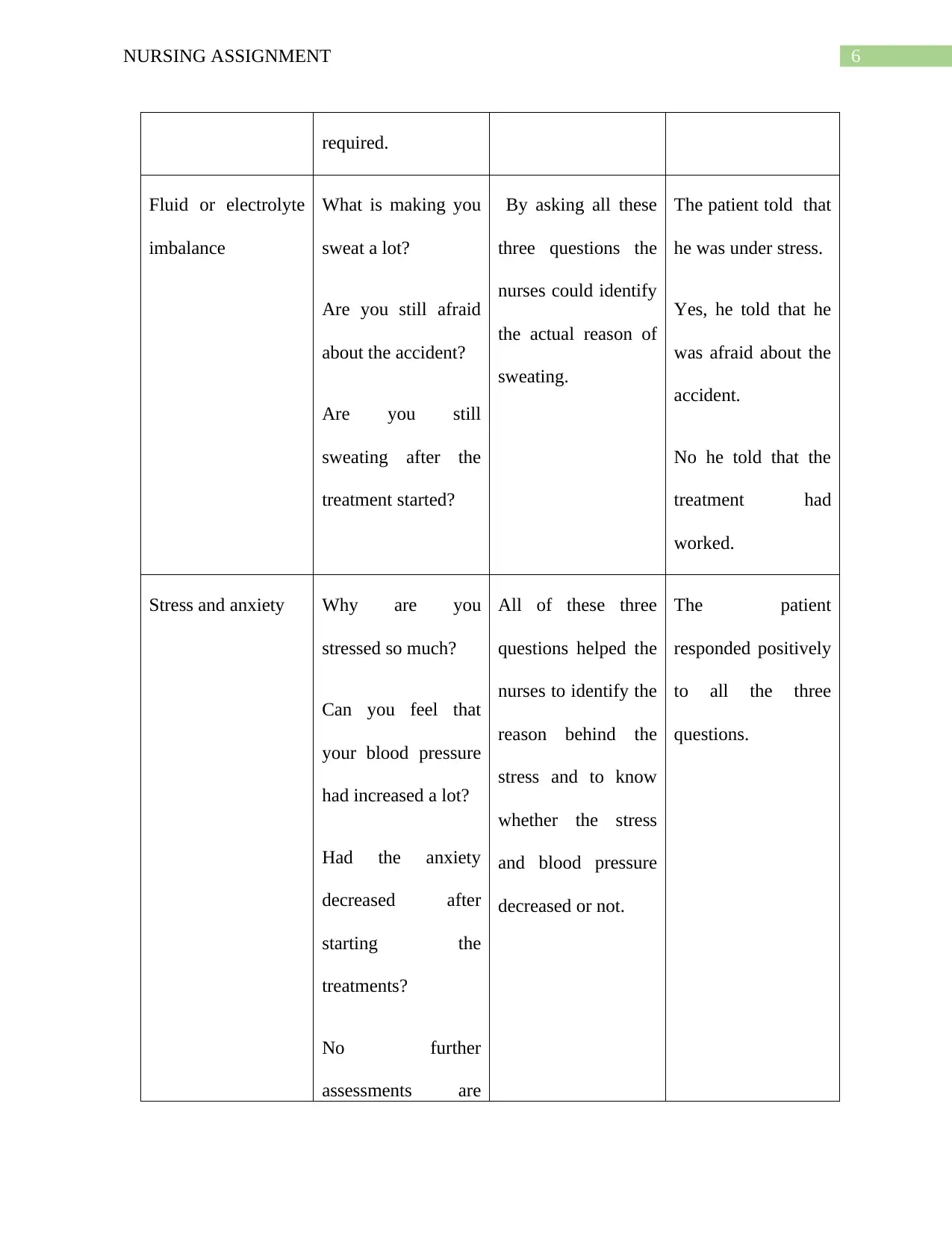
Fluid or electrolyte
imbalance
What is making you
sweat a lot?
Are you still afraid
about the accident?
Are you still
sweating after the
treatment started?
By asking all these
three questions the
nurses could identify
the actual reason of
sweating.
The patient told that
he was under stress.
Yes, he told that he
was afraid about the
accident.
No he told that the
treatment had
worked.
Stress and anxiety Why are you
stressed so much?
Can you feel that
your blood pressure
had increased a lot?
Had the anxiety
decreased after
starting the
treatments?
No further
assessments are
All of these three
questions helped the
nurses to identify the
reason behind the
stress and to know
whether the stress
and blood pressure
decreased or not.
The patient
responded positively
to all the three
questions.
required.
Fluid or electrolyte
imbalance
What is making you
sweat a lot?
Are you still afraid
about the accident?
Are you still
sweating after the
treatment started?
By asking all these
three questions the
nurses could identify
the actual reason of
sweating.
The patient told that
he was under stress.
Yes, he told that he
was afraid about the
accident.
No he told that the
treatment had
worked.
Stress and anxiety Why are you
stressed so much?
Can you feel that
your blood pressure
had increased a lot?
Had the anxiety
decreased after
starting the
treatments?
No further
assessments are
All of these three
questions helped the
nurses to identify the
reason behind the
stress and to know
whether the stress
and blood pressure
decreased or not.
The patient
responded positively
to all the three
questions.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
required.
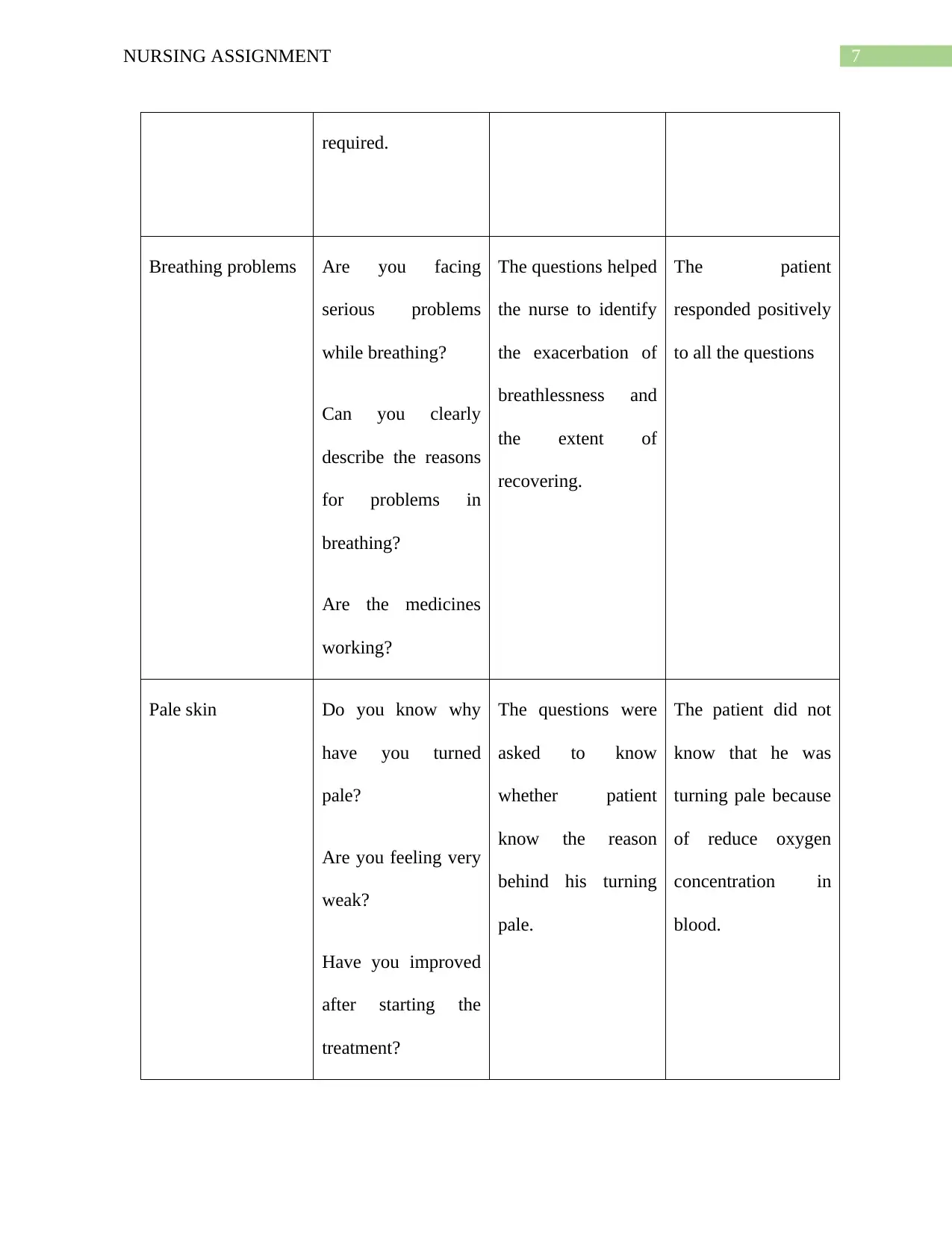
Breathing problems Are you facing
serious problems
while breathing?
Can you clearly
describe the reasons
for problems in
breathing?
Are the medicines
working?
The questions helped
the nurse to identify
the exacerbation of
breathlessness and
the extent of
recovering.
The patient
responded positively
to all the questions
Pale skin Do you know why
have you turned
pale?
Are you feeling very
weak?
Have you improved
after starting the
treatment?
The questions were
asked to know
whether patient
know the reason
behind his turning
pale.
The patient did not
know that he was
turning pale because
of reduce oxygen
concentration in
blood.
required.
Breathing problems Are you facing
serious problems
while breathing?
Can you clearly
describe the reasons
for problems in
breathing?
Are the medicines
working?
The questions helped
the nurse to identify
the exacerbation of
breathlessness and
the extent of
recovering.
The patient
responded positively
to all the questions
Pale skin Do you know why
have you turned
pale?
Are you feeling very
weak?
Have you improved
after starting the
treatment?
The questions were
asked to know
whether patient
know the reason
behind his turning
pale.
The patient did not
know that he was
turning pale because
of reduce oxygen
concentration in
blood.
8NURSING ASSIGNMENT
(v) a. Tachypnea and tachycardia are the common nursing assessments findings and the
connection of these two medical problems with pain is that one of the symptom of
tachycardia is pain but tachypnea does not cause pain (Moon et al., 2016).
b. The other problem that is present with both the medical conditions is shortness of breath.
c. The assessments that can be used to differentiate the two medical conditions are:
In tachypnea blue tint in the fingers and lips occur but in tachycardia the fingers and
lips do not turn pink (van Vugt et al., 2015).
A patient may get faint if he is suffering from tachycardia but a patient suffering from
tachypnea does not become faint.
Part C
The nurses are responsible for assessing accurately a patient so that the doctors and
nurses can provide treatments to their best but in most of the cases the nurses in providing acute
care undertake very few assessments apart from checking the vital signs. The nurses should
follow certain frameworks for assessing the patients. The two most important frameworks are the
biomedical approach and the primary/secondary survey approach.
According to the biomedical model, health is considered to be freedom from pain, disease
and making the patients healthy. This method completely focusses on the physical processes like
pathology, physiology and biochemistry of any disease and does not consider the social factors
(v) a. Tachypnea and tachycardia are the common nursing assessments findings and the
connection of these two medical problems with pain is that one of the symptom of
tachycardia is pain but tachypnea does not cause pain (Moon et al., 2016).
b. The other problem that is present with both the medical conditions is shortness of breath.
c. The assessments that can be used to differentiate the two medical conditions are:
In tachypnea blue tint in the fingers and lips occur but in tachycardia the fingers and
lips do not turn pink (van Vugt et al., 2015).
A patient may get faint if he is suffering from tachycardia but a patient suffering from
tachypnea does not become faint.
Part C
The nurses are responsible for assessing accurately a patient so that the doctors and
nurses can provide treatments to their best but in most of the cases the nurses in providing acute
care undertake very few assessments apart from checking the vital signs. The nurses should
follow certain frameworks for assessing the patients. The two most important frameworks are the
biomedical approach and the primary/secondary survey approach.
According to the biomedical model, health is considered to be freedom from pain, disease
and making the patients healthy. This method completely focusses on the physical processes like
pathology, physiology and biochemistry of any disease and does not consider the social factors
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING ASSIGNMENT
and the individual subjectivity (Artioli, Foà and Taffurelli, 2016). However the disadvantage of
this model is that it does not consider the diagnoses of the disease. The nurses should consider
this model because the nurses focus on the vital signs without knowing in details about the
pathophysiology of the disease (Marafino, Boscardin and Dudley, 2015). So if the nurses follow
this model along with the regularly assessing the vital signs, a comprehensive care can be
provide to the patient. The next framework which is appropriate, is primary and secondary
assessment. The primary assessment helps the nurses to recognize the life threatening conditions
and implementing the correct treatment methods. The acronym ABCDE provide the patient with
primary assessment and this is the correct order for doing the assessment of the patient while
presenting in the emergency department (Harris et al., 2015). The ABCDE involves airway,
breathing, circulation and disability and exposure. The secondary assessment includes exploring
the specific medical conditions that the patient may have. The secondary assessment must be
methodical and must involve inspection, auscultation, palpitation and percussion. The
components of the secondary assessments are A, B, C, D, E.F, G, H, I, where F means full set of
vital signs, G means giving comfort, H means history and I means inspect posterior surfaces. So
by following the framework of primary and secondary assessments the nurses will be able to
provide a comprehensive treatment to the patient (Coventry et al., 2015). The standard 4 of
NMBA nursing standards says that the registered nurses are conduct a comprehensive and
systematic assessment procedure (Nursingmidwiferyboard.gov.au, 2019). They must conduct
assessments which are holistic and at the same time culturally appropriate. The nurses should use
a range of techniques of assessments for collecting relevant information and they should also
work in partnerships to potentially effect the well-being of the patient.
and the individual subjectivity (Artioli, Foà and Taffurelli, 2016). However the disadvantage of
this model is that it does not consider the diagnoses of the disease. The nurses should consider
this model because the nurses focus on the vital signs without knowing in details about the
pathophysiology of the disease (Marafino, Boscardin and Dudley, 2015). So if the nurses follow
this model along with the regularly assessing the vital signs, a comprehensive care can be
provide to the patient. The next framework which is appropriate, is primary and secondary
assessment. The primary assessment helps the nurses to recognize the life threatening conditions
and implementing the correct treatment methods. The acronym ABCDE provide the patient with
primary assessment and this is the correct order for doing the assessment of the patient while
presenting in the emergency department (Harris et al., 2015). The ABCDE involves airway,
breathing, circulation and disability and exposure. The secondary assessment includes exploring
the specific medical conditions that the patient may have. The secondary assessment must be
methodical and must involve inspection, auscultation, palpitation and percussion. The
components of the secondary assessments are A, B, C, D, E.F, G, H, I, where F means full set of
vital signs, G means giving comfort, H means history and I means inspect posterior surfaces. So
by following the framework of primary and secondary assessments the nurses will be able to
provide a comprehensive treatment to the patient (Coventry et al., 2015). The standard 4 of
NMBA nursing standards says that the registered nurses are conduct a comprehensive and
systematic assessment procedure (Nursingmidwiferyboard.gov.au, 2019). They must conduct
assessments which are holistic and at the same time culturally appropriate. The nurses should use
a range of techniques of assessments for collecting relevant information and they should also
work in partnerships to potentially effect the well-being of the patient.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING ASSIGNMENT
So it can be concluded that if the nurses want to provide a comprehensive therapeutic
treatment to the patient then they have to follow the nursing assessment framework. It is an
unethical act for the nurses to not providing comprehensive treatment to the patients. The nurse
are disobeying the codes of nursing conducts if they fail to provide the necessary treatments
required by the patients. If the nursing assessments are not done correctly then the doctors will
follow incorrect treatment procedures and the patients will not recover from their health issues.
The nurses must keep in mind that they have to provide holistic and comprehensive care to the
patient by following accurate nursing frameworks.
So it can be concluded that if the nurses want to provide a comprehensive therapeutic
treatment to the patient then they have to follow the nursing assessment framework. It is an
unethical act for the nurses to not providing comprehensive treatment to the patients. The nurse
are disobeying the codes of nursing conducts if they fail to provide the necessary treatments
required by the patients. If the nursing assessments are not done correctly then the doctors will
follow incorrect treatment procedures and the patients will not recover from their health issues.
The nurses must keep in mind that they have to provide holistic and comprehensive care to the
patient by following accurate nursing frameworks.
11NURSING ASSIGNMENT
References
Artioli, G., Foà, C. and Taffurelli, C., 2016. An integrated narrative nursing model: towards a
new healthcare paradigm. Acta Bio Medica Atenei Parmensis, 87(4-S), pp.13-22.
Coventry, P., Lovell, K., Dickens, C., Bower, P., Chew-Graham, C., McElvenny, D., Hann, M.,
Cherrington, A., Garrett, C., Gibbons, C.J. and Baguley, C., 2015. Integrated primary care for
patients with mental and physical multimorbidity: cluster randomised controlled trial of
collaborative care for patients with depression comorbid with diabetes or cardiovascular
disease. bmj, 350, p.h638.
Harris, T., Kerry, S.M., Victor, C.R., Ekelund, U., Woodcock, A., Iliffe, S., Whincup, P.H.,
Beighton, C., Ussher, M., Limb, E.S. and David, L., 2015. A primary care nurse-delivered
walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-
Lift cluster randomised controlled trial. PLoS medicine, 12(2), p.e1001783.
Marafino, B.J., Boscardin, W.J. and Dudley, R.A., 2015. Efficient and sparse feature selection
for biomedical text classification via the elastic net: Application to ICU risk stratification from
nursing notes. Journal of biomedical informatics, 54, pp.114-120.
Moon, J., Kim, D.Y., Byun, J.I., Sunwoo, J.S., Lim, J.A., Kim, T.J., Shin, J.W., Lee, W.J., Lee,
H.S., Jun, J.S. and Park, K.I., 2016. Orthostatic intolerance symptoms are associated with
depression and diminished quality of life in patients with postural tachycardia syndrome. Health
and quality of life outcomes, 14(1), p.144.
References
Artioli, G., Foà, C. and Taffurelli, C., 2016. An integrated narrative nursing model: towards a
new healthcare paradigm. Acta Bio Medica Atenei Parmensis, 87(4-S), pp.13-22.
Coventry, P., Lovell, K., Dickens, C., Bower, P., Chew-Graham, C., McElvenny, D., Hann, M.,
Cherrington, A., Garrett, C., Gibbons, C.J. and Baguley, C., 2015. Integrated primary care for
patients with mental and physical multimorbidity: cluster randomised controlled trial of
collaborative care for patients with depression comorbid with diabetes or cardiovascular
disease. bmj, 350, p.h638.
Harris, T., Kerry, S.M., Victor, C.R., Ekelund, U., Woodcock, A., Iliffe, S., Whincup, P.H.,
Beighton, C., Ussher, M., Limb, E.S. and David, L., 2015. A primary care nurse-delivered
walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-
Lift cluster randomised controlled trial. PLoS medicine, 12(2), p.e1001783.
Marafino, B.J., Boscardin, W.J. and Dudley, R.A., 2015. Efficient and sparse feature selection
for biomedical text classification via the elastic net: Application to ICU risk stratification from
nursing notes. Journal of biomedical informatics, 54, pp.114-120.
Moon, J., Kim, D.Y., Byun, J.I., Sunwoo, J.S., Lim, J.A., Kim, T.J., Shin, J.W., Lee, W.J., Lee,
H.S., Jun, J.S. and Park, K.I., 2016. Orthostatic intolerance symptoms are associated with
depression and diminished quality of life in patients with postural tachycardia syndrome. Health
and quality of life outcomes, 14(1), p.144.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





