NURBN2000: Comprehensive Health Assessment & Care Plan for Kevin Jones
VerifiedAdded on 2023/06/15
|15
|4629
|193
Report
AI Summary
This assignment presents a comprehensive health assessment and nursing care plan developed for Mr. Kevin Jones, a 75-year-old patient with a history of hypertension, alcoholism, and a recent stroke leading to right-side paralysis. The assessment identifies key health issues including impaired physical mobility, anxiety, ineffective breathing patterns due to lower lobe pneumonia, and deficit fluid volume related to dehydration. The nursing care plan outlines prioritized nursing diagnoses with goals, interventions, rationales, and evaluation methods for each problem. The document also covers Kevin's social history, highlighting his isolation and limited family support, and summarizes the overall assessment, emphasizing the need to address his physical and emotional distress to improve his quality of life. This student document is available on Desklib, a platform offering a wide range of study tools and resources for students.
School of Nursing, Midwifery and
Healthcare
Faculty of Health
Bachelor of Nursing
NURBN2000
Transition to Nursing Studies
Semester 1, 2018
Assessment 2 Part B
Health Assessment & Nursing
Care Plan Workbook
Healthcare
Faculty of Health
Bachelor of Nursing
NURBN2000
Transition to Nursing Studies
Semester 1, 2018
Assessment 2 Part B
Health Assessment & Nursing
Care Plan Workbook
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Student Name:
Student Number:
CRICOS Provider Number 00103D
Introduction
In Assessment Task 2 –Part B you are required to complete a comprehensive health
assessment and nursing care plan on information given to you in the case study- Mr. Kevin
Jones. The case study information is located in the Book – Case Study Guidelines for
Assessment Task 2 (B).
Using the information gathered from the case study of Mr. Kevin Jones, you are expected to
document the assessment you have undertaken. You are also asked to identify four (4)
priority issues, develop, implement and evaluate your nursing care plan for Mr. Kevin Jones.
All information is to be recorded in this Health Assessment & Nursing Care Plan Workbook.
Your completed Health Assessment & Nursing Care Plan Workbook will be assessed using
the marking guide in the NURBN2000 Moodle shell. Print a copy of the marking guide and
keep it with you while writing your Care Plan to ensure you answer the questions correctly.
Guidelines for Health Assessment and Nursing Care plan (Total: 2000 words)
This assessment relies on students being familiar with the nursing process as you
will be required to follow the steps outlined in this process. If you are not familiar with
this, review in any recommended nursing textbook – however, this has been covered
in your prior EN training.
Complete the workbook, ensuring you have answered all the questions
Students will demonstrate clinical decision making skills in:
1. The Nursing Process.
2. Identification/ assessment of nursing problems (nursing diagnosis)
3. Planning and Implementation of nursing care
4. Documentation of nursing data.
5. Evaluation of nursing care
Read this plan for the assessment task:
Activity-Assessment Task 2: Total 2000 words
Student Number:
CRICOS Provider Number 00103D
Introduction
In Assessment Task 2 –Part B you are required to complete a comprehensive health
assessment and nursing care plan on information given to you in the case study- Mr. Kevin
Jones. The case study information is located in the Book – Case Study Guidelines for
Assessment Task 2 (B).
Using the information gathered from the case study of Mr. Kevin Jones, you are expected to
document the assessment you have undertaken. You are also asked to identify four (4)
priority issues, develop, implement and evaluate your nursing care plan for Mr. Kevin Jones.
All information is to be recorded in this Health Assessment & Nursing Care Plan Workbook.
Your completed Health Assessment & Nursing Care Plan Workbook will be assessed using
the marking guide in the NURBN2000 Moodle shell. Print a copy of the marking guide and
keep it with you while writing your Care Plan to ensure you answer the questions correctly.
Guidelines for Health Assessment and Nursing Care plan (Total: 2000 words)
This assessment relies on students being familiar with the nursing process as you
will be required to follow the steps outlined in this process. If you are not familiar with
this, review in any recommended nursing textbook – however, this has been covered
in your prior EN training.
Complete the workbook, ensuring you have answered all the questions
Students will demonstrate clinical decision making skills in:
1. The Nursing Process.
2. Identification/ assessment of nursing problems (nursing diagnosis)
3. Planning and Implementation of nursing care
4. Documentation of nursing data.
5. Evaluation of nursing care
Read this plan for the assessment task:
Activity-Assessment Task 2: Total 2000 words
600 word assessment
Nursing Care Plan
3 Diagnosis/Problems
Expected outcomes
Interventions
Rationale
Evaluation
Referenced 600 word assessment identifying physical & mental health
components e.g. dehydration may result in anxiety & confusion (Gulanick
& Myers, 2012)
Remaining word count utilised in the rest of document (1400 words)
Your care planning will be based on your assessment data
Develop a Care Plan based on data gathered in your assessment (a,b,c).
Then, identify three (3) main nursing problems and provide goals,
interventions, rationale and implementation of that care.
Evaluate (how successful was the care for each of the 3 problems
identified)
Submit Workbook
Adult Health Assessment – Total: 2000 words
Outline:
1. Students are required to discuss the physical and mental health
components for the assessment (600 words). This will need to be written &
referenced according to academic writing & referencing standards.
2. Identify 4 major issues for Kevin Jones, his social history and provide a
summary of your overall assessment of him. Ensure that you use ‘objective’
language. This would be similar to what you would write in nursing notes as
an admission history.
3. Using the Nursing diagnosis section, select the three (3) health nursing
diagnosis that you think are a priority for Kevin and include the evidence from
your assessment that supports this.
4. Now prioritise these 3 important nursing problems to formulate a nursing
care plan for Kevin
5. Develop a nursing care plan with rationale (referenced) and related
interventions that could be implemented for Kevin.
6. Complete the evaluation sections of the care plan - identify ways that you
could measure success in relation to each of these interventions.
1. Write your 600 words referenced assessment below discussing the
physical and mental health components for Kevin. This will need to be written
according to academic writing & referencing standards.(NB: your assessment
will roll on the next page).
Nursing Care Plan
3 Diagnosis/Problems
Expected outcomes
Interventions
Rationale
Evaluation
Referenced 600 word assessment identifying physical & mental health
components e.g. dehydration may result in anxiety & confusion (Gulanick
& Myers, 2012)
Remaining word count utilised in the rest of document (1400 words)
Your care planning will be based on your assessment data
Develop a Care Plan based on data gathered in your assessment (a,b,c).
Then, identify three (3) main nursing problems and provide goals,
interventions, rationale and implementation of that care.
Evaluate (how successful was the care for each of the 3 problems
identified)
Submit Workbook
Adult Health Assessment – Total: 2000 words
Outline:
1. Students are required to discuss the physical and mental health
components for the assessment (600 words). This will need to be written &
referenced according to academic writing & referencing standards.
2. Identify 4 major issues for Kevin Jones, his social history and provide a
summary of your overall assessment of him. Ensure that you use ‘objective’
language. This would be similar to what you would write in nursing notes as
an admission history.
3. Using the Nursing diagnosis section, select the three (3) health nursing
diagnosis that you think are a priority for Kevin and include the evidence from
your assessment that supports this.
4. Now prioritise these 3 important nursing problems to formulate a nursing
care plan for Kevin
5. Develop a nursing care plan with rationale (referenced) and related
interventions that could be implemented for Kevin.
6. Complete the evaluation sections of the care plan - identify ways that you
could measure success in relation to each of these interventions.
1. Write your 600 words referenced assessment below discussing the
physical and mental health components for Kevin. This will need to be written
according to academic writing & referencing standards.(NB: your assessment
will roll on the next page).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mr Kevin Jones is a 75-year-old gentleman, admitted under my care with the
history of hypertension, and alcoholism. He had stroke and paralysis. Assessment is
necessary to identify the risk factors and appropriate intervention for improving the
physical and mental health outcomes (Berman et al., 2014).
Stroke in the patients may have caused Paralysis. It is the common disability.
Stroke and paralysis may cause impaired voluntary movement of muscles. It is due
to brain damage due to the permanent block of blood supply. Kevin leans on one
side. He has slurred speech as per assessment. He forgets where his right hand
may be. Slurred speech after a stroke may occur due to the damage to left
hemisphere of the brain called hemiplegic. Hemiplegia may have caused vision
problems and his swallowing and walking difficulties. It may become even severe if
neglected and walking difficulty increases the risk of fall (Ben Natan et al., 2016).
The patient seems to have impediments to mobility as a result of paralysis risk
assessment. Currently, the patient is using three-pronged stick, and he is anxious
about the balance. There may be a need to further assess the strength to perform
ROM. It will help determine if the patent can participate in the rehabilitative activities
and exercises. Further, assessment showed affect of paralysis on mental health
components. Lack of family members support may have caused anxiety and can be
due to independent nature of Kevin. He may not be able to perform his activities of
daily living. Fear of fall and injury in this situation can be due to anxiety. and is mainly
autonomic response (Berman et al., 2014). Kevin's agitated and irritated behaviour
with nurses and physiotherapist relates to severe anxiety. In this level of anxiety,
people are overwhelmed and report overloaded with stimuli. It needs immediate
treatment as Kevin has history of Depression and Anxiety (Kang et al., 2017).
The chest x-ray of Kevin revealed lower lobe pneumonia. It is the lower
respiratory tract infection (bacterial or viral). It is characterised by patchy
consolidation in the lower lobe. Fever, infection, or dehydration may have caused
disorientation in patient as per assessment. Dehydration and anxiety may have led
the patient to convey his needs poorly (Cacciatore et al., 2017). His case details
inform about fever, loss of appetite, taking fewer fluids, malaise and body ache over
the past few days. It may be the cause of loss of weight and dehydration. He is
complaining chronic cough with sputum. His vital signs are recorded as BP - 90/60,
Temp 38.3 (mild fever), O2 sats - 93%, Resp rate - 24/ min (indicating critical illness
and shortness of breath) (Berman et al., 2014). There are Crackles & wheezes on
auscultation, diminished breath sounds. Patient has low blood pressure that may
have increased the risk of another stroke. His auscultation reports indicate the
probability of pleural effusion. Thickening of the reactive airway wall and decreased
airway lumen may have caused Wheezes. Without treatment, it may lead to heart
failure (Manabe et al., 2015).
The loss of appetite and less fluid intake may have decreased urinary output.
Dehydration in Kevin has caused skin turgor dry, and mucous membranes dry.
Dehydration may have caused anxiety and confusion (Berman et al., 2014). The
excess protein intake by Kevin may have caused increased urine concentration. The
condition indicates excessive protein breakdown. Increased blood urea nitrogen is
history of hypertension, and alcoholism. He had stroke and paralysis. Assessment is
necessary to identify the risk factors and appropriate intervention for improving the
physical and mental health outcomes (Berman et al., 2014).
Stroke in the patients may have caused Paralysis. It is the common disability.
Stroke and paralysis may cause impaired voluntary movement of muscles. It is due
to brain damage due to the permanent block of blood supply. Kevin leans on one
side. He has slurred speech as per assessment. He forgets where his right hand
may be. Slurred speech after a stroke may occur due to the damage to left
hemisphere of the brain called hemiplegic. Hemiplegia may have caused vision
problems and his swallowing and walking difficulties. It may become even severe if
neglected and walking difficulty increases the risk of fall (Ben Natan et al., 2016).
The patient seems to have impediments to mobility as a result of paralysis risk
assessment. Currently, the patient is using three-pronged stick, and he is anxious
about the balance. There may be a need to further assess the strength to perform
ROM. It will help determine if the patent can participate in the rehabilitative activities
and exercises. Further, assessment showed affect of paralysis on mental health
components. Lack of family members support may have caused anxiety and can be
due to independent nature of Kevin. He may not be able to perform his activities of
daily living. Fear of fall and injury in this situation can be due to anxiety. and is mainly
autonomic response (Berman et al., 2014). Kevin's agitated and irritated behaviour
with nurses and physiotherapist relates to severe anxiety. In this level of anxiety,
people are overwhelmed and report overloaded with stimuli. It needs immediate
treatment as Kevin has history of Depression and Anxiety (Kang et al., 2017).
The chest x-ray of Kevin revealed lower lobe pneumonia. It is the lower
respiratory tract infection (bacterial or viral). It is characterised by patchy
consolidation in the lower lobe. Fever, infection, or dehydration may have caused
disorientation in patient as per assessment. Dehydration and anxiety may have led
the patient to convey his needs poorly (Cacciatore et al., 2017). His case details
inform about fever, loss of appetite, taking fewer fluids, malaise and body ache over
the past few days. It may be the cause of loss of weight and dehydration. He is
complaining chronic cough with sputum. His vital signs are recorded as BP - 90/60,
Temp 38.3 (mild fever), O2 sats - 93%, Resp rate - 24/ min (indicating critical illness
and shortness of breath) (Berman et al., 2014). There are Crackles & wheezes on
auscultation, diminished breath sounds. Patient has low blood pressure that may
have increased the risk of another stroke. His auscultation reports indicate the
probability of pleural effusion. Thickening of the reactive airway wall and decreased
airway lumen may have caused Wheezes. Without treatment, it may lead to heart
failure (Manabe et al., 2015).
The loss of appetite and less fluid intake may have decreased urinary output.
Dehydration in Kevin has caused skin turgor dry, and mucous membranes dry.
Dehydration may have caused anxiety and confusion (Berman et al., 2014). The
excess protein intake by Kevin may have caused increased urine concentration. The
condition indicates excessive protein breakdown. Increased blood urea nitrogen is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
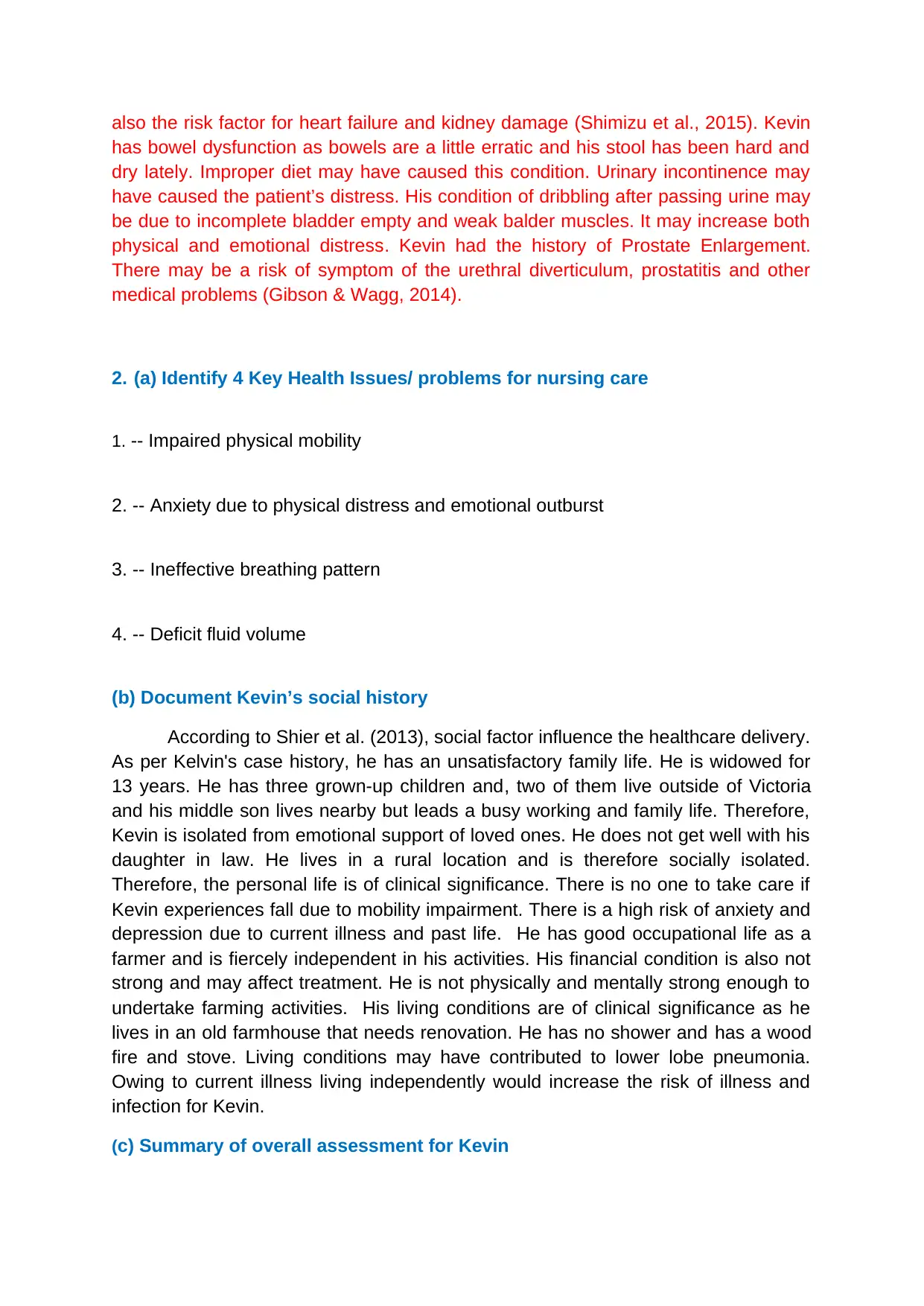
also the risk factor for heart failure and kidney damage (Shimizu et al., 2015). Kevin
has bowel dysfunction as bowels are a little erratic and his stool has been hard and
dry lately. Improper diet may have caused this condition. Urinary incontinence may
have caused the patient’s distress. His condition of dribbling after passing urine may
be due to incomplete bladder empty and weak balder muscles. It may increase both
physical and emotional distress. Kevin had the history of Prostate Enlargement.
There may be a risk of symptom of the urethral diverticulum, prostatitis and other
medical problems (Gibson & Wagg, 2014).
2. (a) Identify 4 Key Health Issues/ problems for nursing care
1. -- Impaired physical mobility
2. -- Anxiety due to physical distress and emotional outburst
3. -- Ineffective breathing pattern
4. -- Deficit fluid volume
(b) Document Kevin’s social history
According to Shier et al. (2013), social factor influence the healthcare delivery.
As per Kelvin's case history, he has an unsatisfactory family life. He is widowed for
13 years. He has three grown-up children and, two of them live outside of Victoria
and his middle son lives nearby but leads a busy working and family life. Therefore,
Kevin is isolated from emotional support of loved ones. He does not get well with his
daughter in law. He lives in a rural location and is therefore socially isolated.
Therefore, the personal life is of clinical significance. There is no one to take care if
Kevin experiences fall due to mobility impairment. There is a high risk of anxiety and
depression due to current illness and past life. He has good occupational life as a
farmer and is fiercely independent in his activities. His financial condition is also not
strong and may affect treatment. He is not physically and mentally strong enough to
undertake farming activities. His living conditions are of clinical significance as he
lives in an old farmhouse that needs renovation. He has no shower and has a wood
fire and stove. Living conditions may have contributed to lower lobe pneumonia.
Owing to current illness living independently would increase the risk of illness and
infection for Kevin.
(c) Summary of overall assessment for Kevin
has bowel dysfunction as bowels are a little erratic and his stool has been hard and
dry lately. Improper diet may have caused this condition. Urinary incontinence may
have caused the patient’s distress. His condition of dribbling after passing urine may
be due to incomplete bladder empty and weak balder muscles. It may increase both
physical and emotional distress. Kevin had the history of Prostate Enlargement.
There may be a risk of symptom of the urethral diverticulum, prostatitis and other
medical problems (Gibson & Wagg, 2014).
2. (a) Identify 4 Key Health Issues/ problems for nursing care
1. -- Impaired physical mobility
2. -- Anxiety due to physical distress and emotional outburst
3. -- Ineffective breathing pattern
4. -- Deficit fluid volume
(b) Document Kevin’s social history
According to Shier et al. (2013), social factor influence the healthcare delivery.
As per Kelvin's case history, he has an unsatisfactory family life. He is widowed for
13 years. He has three grown-up children and, two of them live outside of Victoria
and his middle son lives nearby but leads a busy working and family life. Therefore,
Kevin is isolated from emotional support of loved ones. He does not get well with his
daughter in law. He lives in a rural location and is therefore socially isolated.
Therefore, the personal life is of clinical significance. There is no one to take care if
Kevin experiences fall due to mobility impairment. There is a high risk of anxiety and
depression due to current illness and past life. He has good occupational life as a
farmer and is fiercely independent in his activities. His financial condition is also not
strong and may affect treatment. He is not physically and mentally strong enough to
undertake farming activities. His living conditions are of clinical significance as he
lives in an old farmhouse that needs renovation. He has no shower and has a wood
fire and stove. Living conditions may have contributed to lower lobe pneumonia.
Owing to current illness living independently would increase the risk of illness and
infection for Kevin.
(c) Summary of overall assessment for Kevin

In case of Kevin paralysis and pneumonia has been a major health issue.
Based on an overall assessment of Kevin it can be concluded that he is at high risk
of fall due to mobility impairment. His physical distress, respiratory infection and fluid
volume deficit have increased anxiety and emotional distress. Treating respiratory
infection is necessary to cure his ineffective breathing pattern. These are areas of
clinical significance. Dehydration and bowel elimination problem is an area of priority
care. Kevin needs a proper diet to decrease the high blood urea nitrogen as it also
includes the risk of heart and kidney failure.
Identifying Nursing Problems (Diagnosis)
Nursing Diagnosis
A nursing diagnosis is a statement that describes the PERSON'S actual or potential
response to a health problem that requires nursing care. It is a three-part statement with
diagnosis, cause and evidence.
Ref: Berman, A., Snyder, S., J., Levett-Jones, T., Dwyer, T., Hales, M., Harvey, N. Luxford,
Y., Moxham, L., Park, T., Parker, B., Reid-Searl, K., Stanley, D. (2014). Kozier &
Erb’s Fundamentals of Nursing (3r Australian Ed.). Pearson: NSW, Australia. 2012, Ch. 13
Page 233 -249
Based on Assessment data you have gathered, select the three (3) priority
diagnoses that you feel are the most appropriate for Kevin.
Ensure you include what evidence you have to support this.
(1) Impaired mobility due to paralysis
Evidenced by: Kevin's anxiety related to balance, mobilising with three-pronged stick,
patient unable to sense his right hand and evident from the patient leaning one side
(2) Ineffective airway breathing due to lower lobe pneumonia
Evidenced by: cough with sputum production, crackles and wheezes, diminished breath
sound in the auscultation report, changes in the respiratory and pulse rate
(3 Deficit fluid volume due to dehydration
Evidenced by: dry skin turgor, bowel elimination problem, dry mucus’s membrane, high
blood urea nitrogen, concentrated urine
Based on an overall assessment of Kevin it can be concluded that he is at high risk
of fall due to mobility impairment. His physical distress, respiratory infection and fluid
volume deficit have increased anxiety and emotional distress. Treating respiratory
infection is necessary to cure his ineffective breathing pattern. These are areas of
clinical significance. Dehydration and bowel elimination problem is an area of priority
care. Kevin needs a proper diet to decrease the high blood urea nitrogen as it also
includes the risk of heart and kidney failure.
Identifying Nursing Problems (Diagnosis)
Nursing Diagnosis
A nursing diagnosis is a statement that describes the PERSON'S actual or potential
response to a health problem that requires nursing care. It is a three-part statement with
diagnosis, cause and evidence.
Ref: Berman, A., Snyder, S., J., Levett-Jones, T., Dwyer, T., Hales, M., Harvey, N. Luxford,
Y., Moxham, L., Park, T., Parker, B., Reid-Searl, K., Stanley, D. (2014). Kozier &
Erb’s Fundamentals of Nursing (3r Australian Ed.). Pearson: NSW, Australia. 2012, Ch. 13
Page 233 -249
Based on Assessment data you have gathered, select the three (3) priority
diagnoses that you feel are the most appropriate for Kevin.
Ensure you include what evidence you have to support this.
(1) Impaired mobility due to paralysis
Evidenced by: Kevin's anxiety related to balance, mobilising with three-pronged stick,
patient unable to sense his right hand and evident from the patient leaning one side
(2) Ineffective airway breathing due to lower lobe pneumonia
Evidenced by: cough with sputum production, crackles and wheezes, diminished breath
sound in the auscultation report, changes in the respiratory and pulse rate
(3 Deficit fluid volume due to dehydration
Evidenced by: dry skin turgor, bowel elimination problem, dry mucus’s membrane, high
blood urea nitrogen, concentrated urine
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
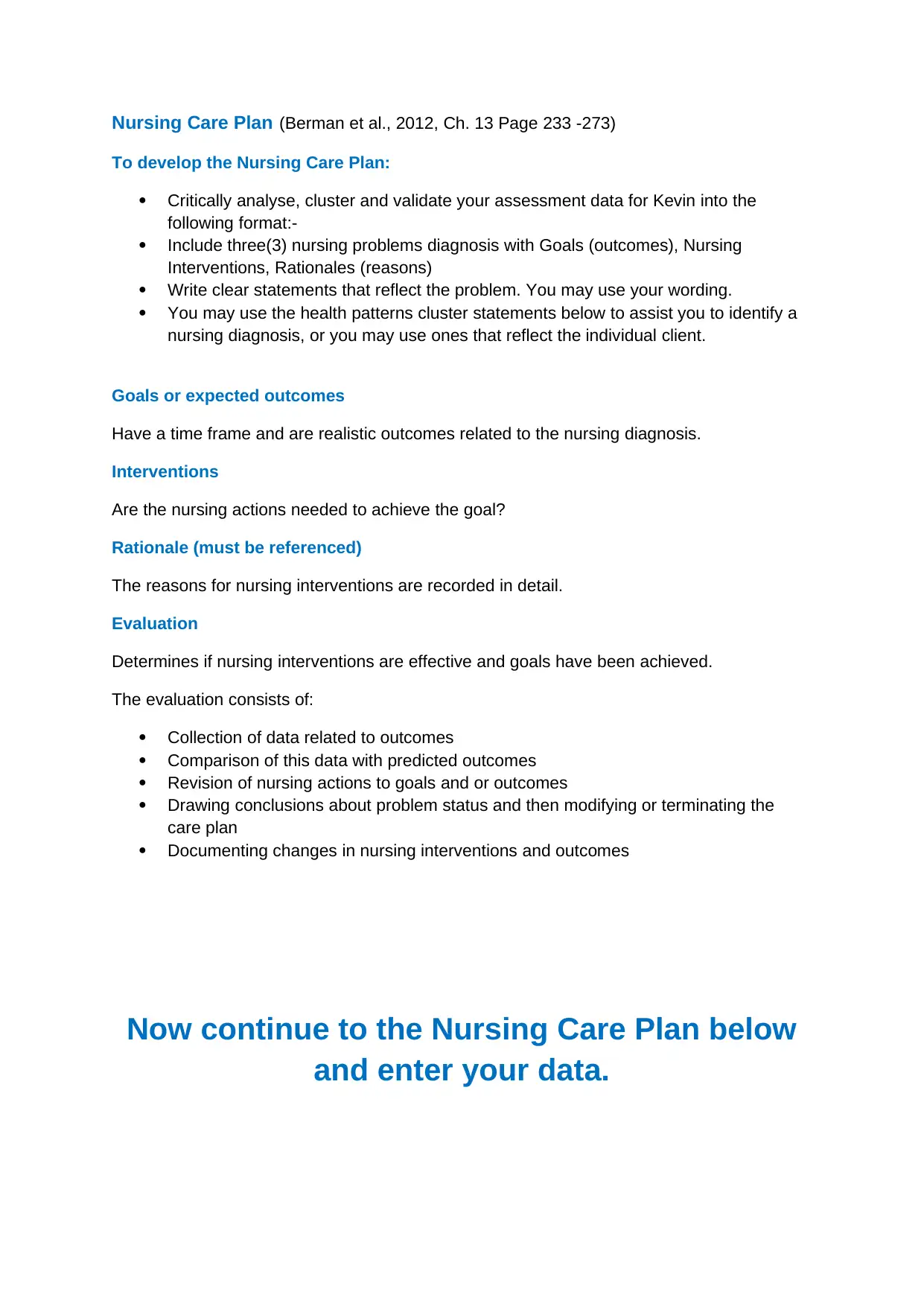
Nursing Care Plan (Berman et al., 2012, Ch. 13 Page 233 -273)
To develop the Nursing Care Plan:
Critically analyse, cluster and validate your assessment data for Kevin into the
following format:-
Include three(3) nursing problems diagnosis with Goals (outcomes), Nursing
Interventions, Rationales (reasons)
Write clear statements that reflect the problem. You may use your wording.
You may use the health patterns cluster statements below to assist you to identify a
nursing diagnosis, or you may use ones that reflect the individual client.
Goals or expected outcomes
Have a time frame and are realistic outcomes related to the nursing diagnosis.
Interventions
Are the nursing actions needed to achieve the goal?
Rationale (must be referenced)
The reasons for nursing interventions are recorded in detail.
Evaluation
Determines if nursing interventions are effective and goals have been achieved.
The evaluation consists of:
Collection of data related to outcomes
Comparison of this data with predicted outcomes
Revision of nursing actions to goals and or outcomes
Drawing conclusions about problem status and then modifying or terminating the
care plan
Documenting changes in nursing interventions and outcomes
Now continue to the Nursing Care Plan below
and enter your data.
To develop the Nursing Care Plan:
Critically analyse, cluster and validate your assessment data for Kevin into the
following format:-
Include three(3) nursing problems diagnosis with Goals (outcomes), Nursing
Interventions, Rationales (reasons)
Write clear statements that reflect the problem. You may use your wording.
You may use the health patterns cluster statements below to assist you to identify a
nursing diagnosis, or you may use ones that reflect the individual client.
Goals or expected outcomes
Have a time frame and are realistic outcomes related to the nursing diagnosis.
Interventions
Are the nursing actions needed to achieve the goal?
Rationale (must be referenced)
The reasons for nursing interventions are recorded in detail.
Evaluation
Determines if nursing interventions are effective and goals have been achieved.
The evaluation consists of:
Collection of data related to outcomes
Comparison of this data with predicted outcomes
Revision of nursing actions to goals and or outcomes
Drawing conclusions about problem status and then modifying or terminating the
care plan
Documenting changes in nursing interventions and outcomes
Now continue to the Nursing Care Plan below
and enter your data.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
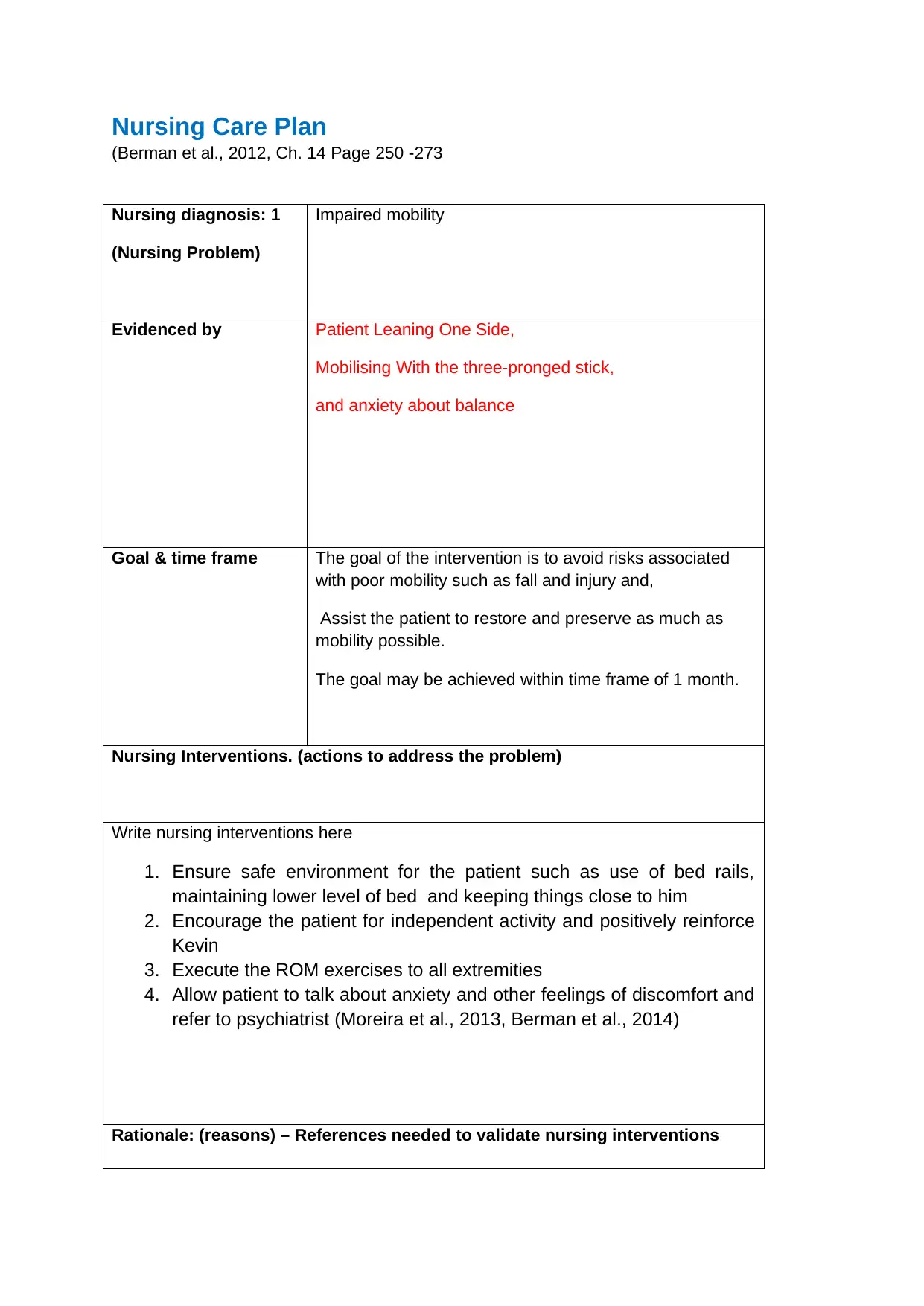
Nursing Care Plan
(Berman et al., 2012, Ch. 14 Page 250 -273
Nursing diagnosis: 1
(Nursing Problem)
Impaired mobility
Evidenced by Patient Leaning One Side,
Mobilising With the three-pronged stick,
and anxiety about balance
Goal & time frame The goal of the intervention is to avoid risks associated
with poor mobility such as fall and injury and,
Assist the patient to restore and preserve as much as
mobility possible.
The goal may be achieved within time frame of 1 month.
Nursing Interventions. (actions to address the problem)
Write nursing interventions here
1. Ensure safe environment for the patient such as use of bed rails,
maintaining lower level of bed and keeping things close to him
2. Encourage the patient for independent activity and positively reinforce
Kevin
3. Execute the ROM exercises to all extremities
4. Allow patient to talk about anxiety and other feelings of discomfort and
refer to psychiatrist (Moreira et al., 2013, Berman et al., 2014)
Rationale: (reasons) – References needed to validate nursing interventions
(Berman et al., 2012, Ch. 14 Page 250 -273
Nursing diagnosis: 1
(Nursing Problem)
Impaired mobility
Evidenced by Patient Leaning One Side,
Mobilising With the three-pronged stick,
and anxiety about balance
Goal & time frame The goal of the intervention is to avoid risks associated
with poor mobility such as fall and injury and,
Assist the patient to restore and preserve as much as
mobility possible.
The goal may be achieved within time frame of 1 month.
Nursing Interventions. (actions to address the problem)
Write nursing interventions here
1. Ensure safe environment for the patient such as use of bed rails,
maintaining lower level of bed and keeping things close to him
2. Encourage the patient for independent activity and positively reinforce
Kevin
3. Execute the ROM exercises to all extremities
4. Allow patient to talk about anxiety and other feelings of discomfort and
refer to psychiatrist (Moreira et al., 2013, Berman et al., 2014)
Rationale: (reasons) – References needed to validate nursing interventions
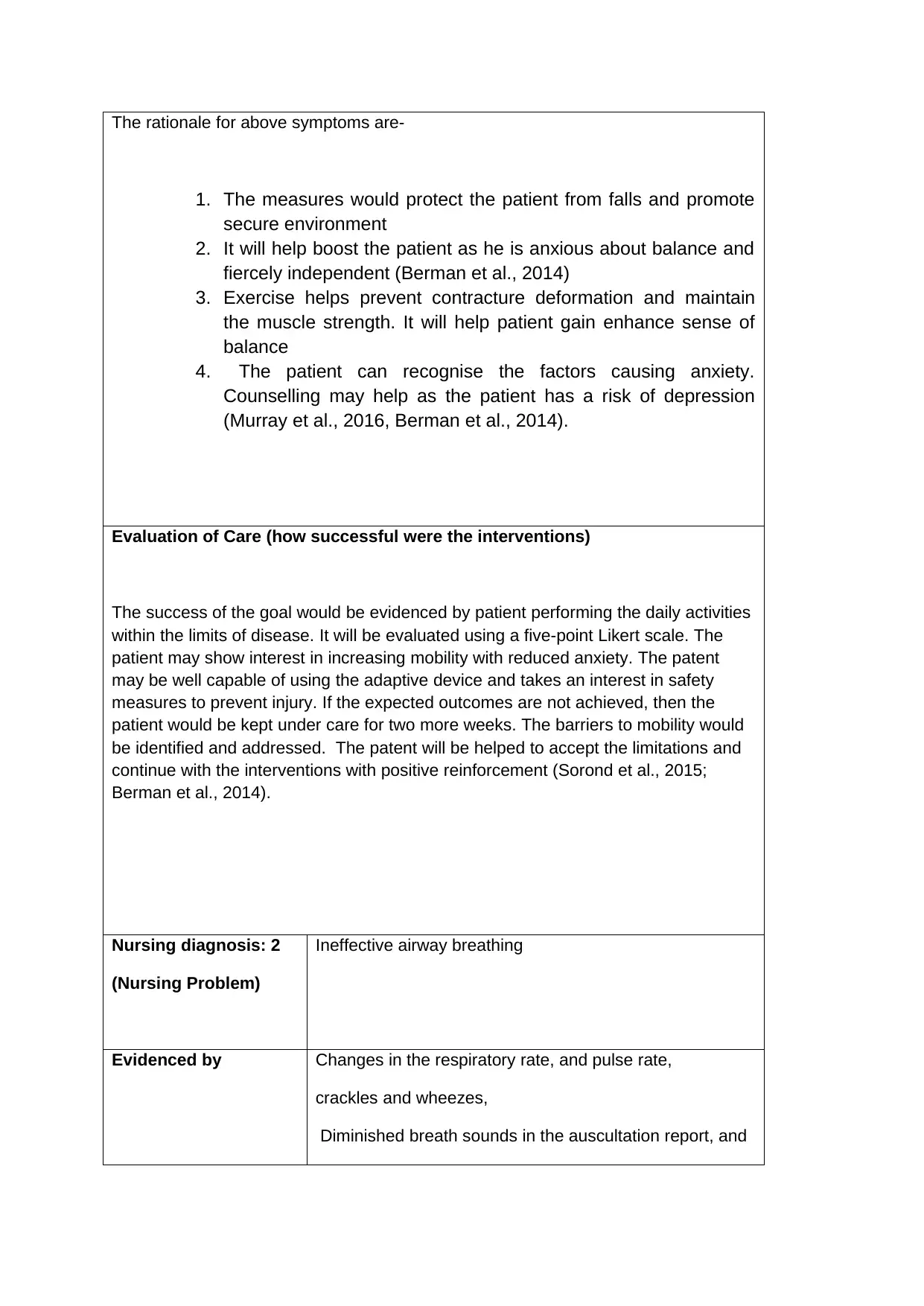
The rationale for above symptoms are-
1. The measures would protect the patient from falls and promote
secure environment
2. It will help boost the patient as he is anxious about balance and
fiercely independent (Berman et al., 2014)
3. Exercise helps prevent contracture deformation and maintain
the muscle strength. It will help patient gain enhance sense of
balance
4. The patient can recognise the factors causing anxiety.
Counselling may help as the patient has a risk of depression
(Murray et al., 2016, Berman et al., 2014).
Evaluation of Care (how successful were the interventions)
The success of the goal would be evidenced by patient performing the daily activities
within the limits of disease. It will be evaluated using a five-point Likert scale. The
patient may show interest in increasing mobility with reduced anxiety. The patent
may be well capable of using the adaptive device and takes an interest in safety
measures to prevent injury. If the expected outcomes are not achieved, then the
patient would be kept under care for two more weeks. The barriers to mobility would
be identified and addressed. The patent will be helped to accept the limitations and
continue with the interventions with positive reinforcement (Sorond et al., 2015;
Berman et al., 2014).
Nursing diagnosis: 2
(Nursing Problem)
Ineffective airway breathing
Evidenced by Changes in the respiratory rate, and pulse rate,
crackles and wheezes,
Diminished breath sounds in the auscultation report, and
1. The measures would protect the patient from falls and promote
secure environment
2. It will help boost the patient as he is anxious about balance and
fiercely independent (Berman et al., 2014)
3. Exercise helps prevent contracture deformation and maintain
the muscle strength. It will help patient gain enhance sense of
balance
4. The patient can recognise the factors causing anxiety.
Counselling may help as the patient has a risk of depression
(Murray et al., 2016, Berman et al., 2014).
Evaluation of Care (how successful were the interventions)
The success of the goal would be evidenced by patient performing the daily activities
within the limits of disease. It will be evaluated using a five-point Likert scale. The
patient may show interest in increasing mobility with reduced anxiety. The patent
may be well capable of using the adaptive device and takes an interest in safety
measures to prevent injury. If the expected outcomes are not achieved, then the
patient would be kept under care for two more weeks. The barriers to mobility would
be identified and addressed. The patent will be helped to accept the limitations and
continue with the interventions with positive reinforcement (Sorond et al., 2015;
Berman et al., 2014).
Nursing diagnosis: 2
(Nursing Problem)
Ineffective airway breathing
Evidenced by Changes in the respiratory rate, and pulse rate,
crackles and wheezes,
Diminished breath sounds in the auscultation report, and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
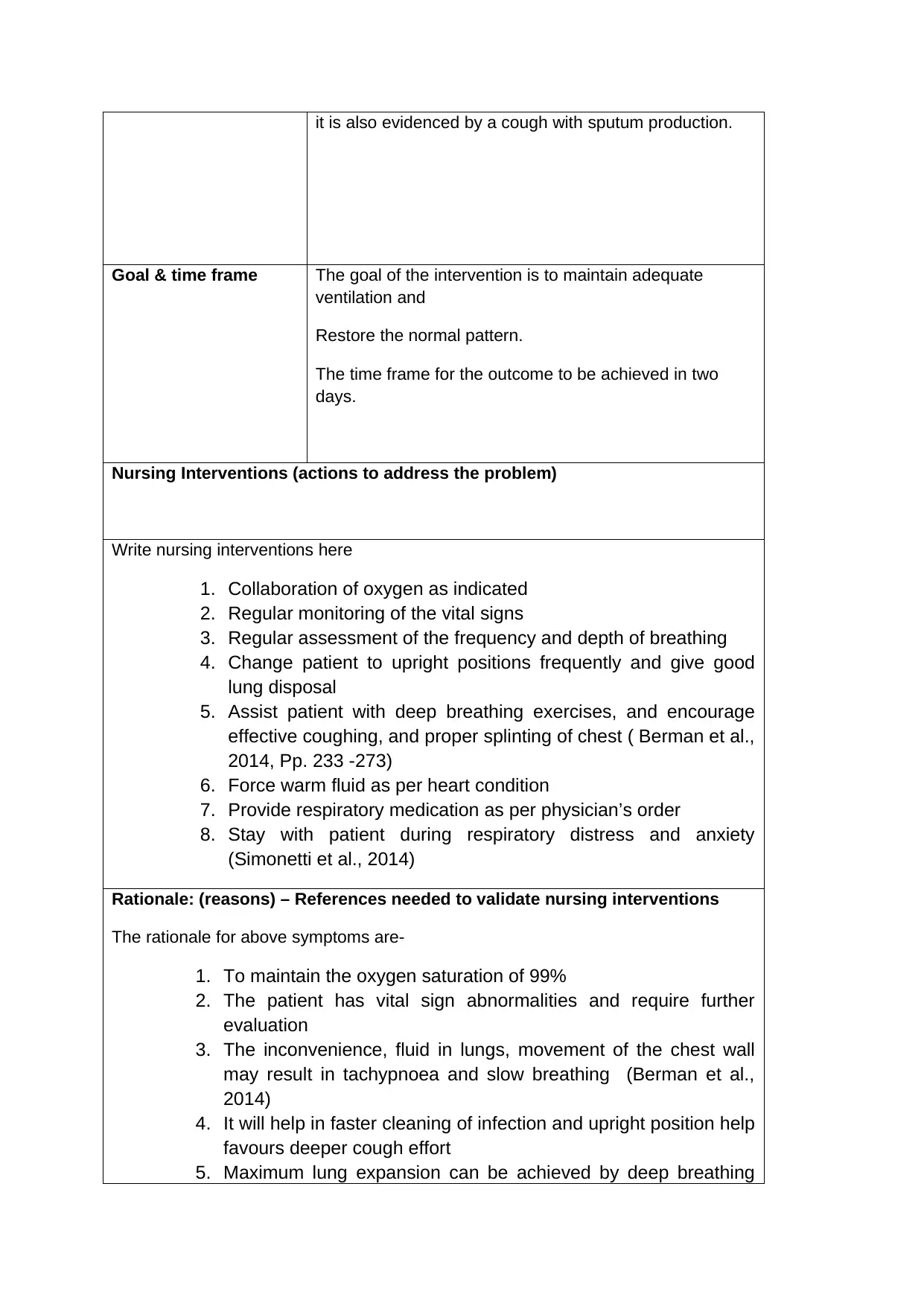
it is also evidenced by a cough with sputum production.
Goal & time frame The goal of the intervention is to maintain adequate
ventilation and
Restore the normal pattern.
The time frame for the outcome to be achieved in two
days.
Nursing Interventions (actions to address the problem)
Write nursing interventions here
1. Collaboration of oxygen as indicated
2. Regular monitoring of the vital signs
3. Regular assessment of the frequency and depth of breathing
4. Change patient to upright positions frequently and give good
lung disposal
5. Assist patient with deep breathing exercises, and encourage
effective coughing, and proper splinting of chest ( Berman et al.,
2014, Pp. 233 -273)
6. Force warm fluid as per heart condition
7. Provide respiratory medication as per physician’s order
8. Stay with patient during respiratory distress and anxiety
(Simonetti et al., 2014)
Rationale: (reasons) – References needed to validate nursing interventions
The rationale for above symptoms are-
1. To maintain the oxygen saturation of 99%
2. The patient has vital sign abnormalities and require further
evaluation
3. The inconvenience, fluid in lungs, movement of the chest wall
may result in tachypnoea and slow breathing (Berman et al.,
2014)
4. It will help in faster cleaning of infection and upright position help
favours deeper cough effort
5. Maximum lung expansion can be achieved by deep breathing
Goal & time frame The goal of the intervention is to maintain adequate
ventilation and
Restore the normal pattern.
The time frame for the outcome to be achieved in two
days.
Nursing Interventions (actions to address the problem)
Write nursing interventions here
1. Collaboration of oxygen as indicated
2. Regular monitoring of the vital signs
3. Regular assessment of the frequency and depth of breathing
4. Change patient to upright positions frequently and give good
lung disposal
5. Assist patient with deep breathing exercises, and encourage
effective coughing, and proper splinting of chest ( Berman et al.,
2014, Pp. 233 -273)
6. Force warm fluid as per heart condition
7. Provide respiratory medication as per physician’s order
8. Stay with patient during respiratory distress and anxiety
(Simonetti et al., 2014)
Rationale: (reasons) – References needed to validate nursing interventions
The rationale for above symptoms are-
1. To maintain the oxygen saturation of 99%
2. The patient has vital sign abnormalities and require further
evaluation
3. The inconvenience, fluid in lungs, movement of the chest wall
may result in tachypnoea and slow breathing (Berman et al.,
2014)
4. It will help in faster cleaning of infection and upright position help
favours deeper cough effort
5. Maximum lung expansion can be achieved by deep breathing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
exercises. Chest discomfort can be prevented by splinting
(Berman et al., 2014, pp.273)
6. Warm fluid helps in expectoration of secretion and mobilisation
7. Air passage can be opened, Beta-adrenergic agonist
8. To reduce patient oxygen demand and anxiety (Hill et al., 2018,
Berman et al., 2014)
Evaluation of Care (how successful were the interventions)
The patient is expected to demonstrate the behaviour to achieve airway clearance
and show clear breath sound on auscultation. The vital signs may be normal with
reduced cough and sputum indicating airway clearance. Auscultation reports may
show clear breathing sound. A relaxed breathing is expected at the normal rate. The
patient is expected to breathe normally when carrying out the activities of daily living.
If the normal breathing pattern is not restored, then the GP would be consulted again
to revise the dosage of the medications (Quinn et al., 2014; Berman et al., 2014).
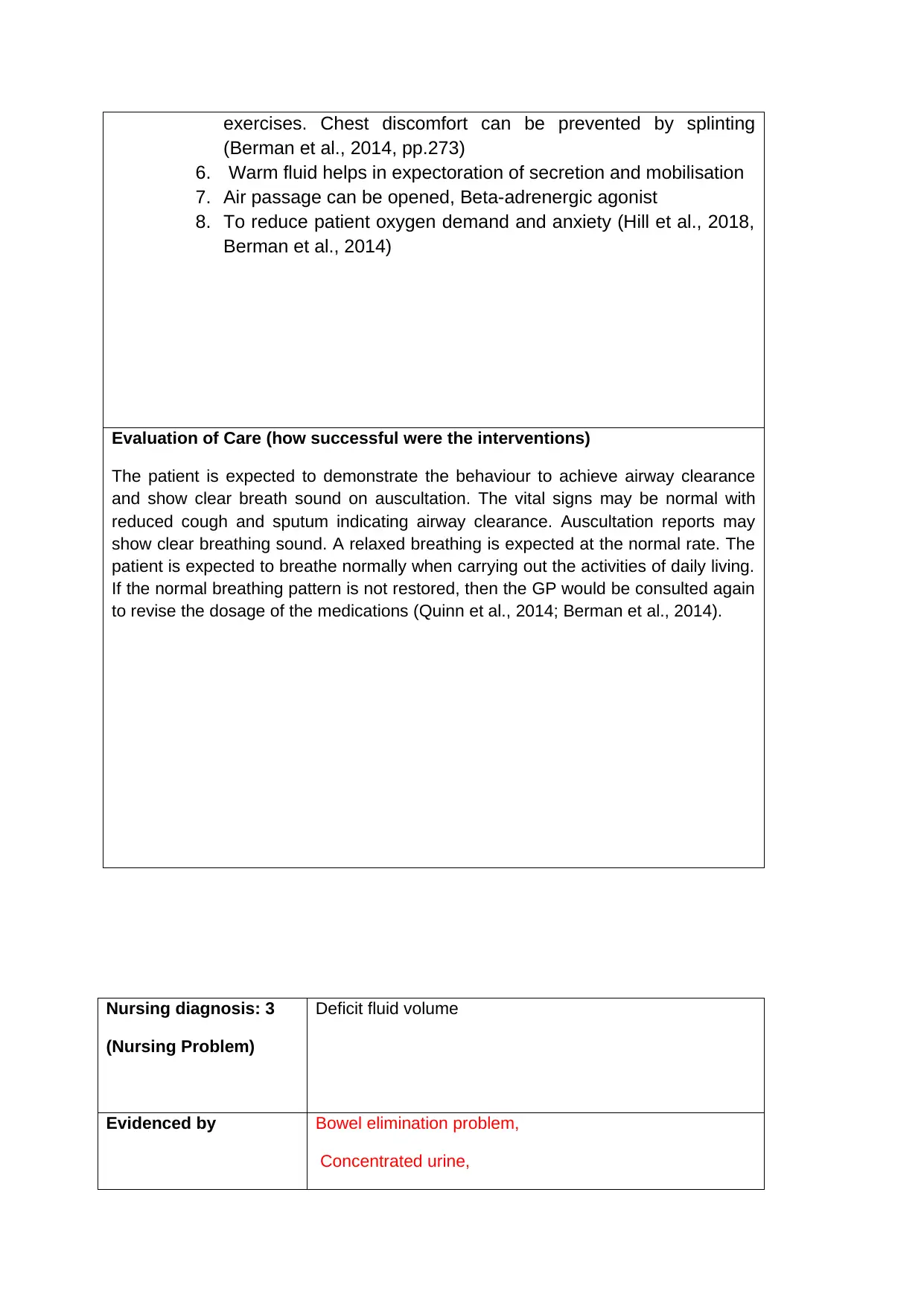
Nursing diagnosis: 3
(Nursing Problem)
Deficit fluid volume
Evidenced by Bowel elimination problem,
Concentrated urine,
(Berman et al., 2014, pp.273)
6. Warm fluid helps in expectoration of secretion and mobilisation
7. Air passage can be opened, Beta-adrenergic agonist
8. To reduce patient oxygen demand and anxiety (Hill et al., 2018,
Berman et al., 2014)
Evaluation of Care (how successful were the interventions)
The patient is expected to demonstrate the behaviour to achieve airway clearance
and show clear breath sound on auscultation. The vital signs may be normal with
reduced cough and sputum indicating airway clearance. Auscultation reports may
show clear breathing sound. A relaxed breathing is expected at the normal rate. The
patient is expected to breathe normally when carrying out the activities of daily living.
If the normal breathing pattern is not restored, then the GP would be consulted again
to revise the dosage of the medications (Quinn et al., 2014; Berman et al., 2014).
Nursing diagnosis: 3
(Nursing Problem)
Deficit fluid volume
Evidenced by Bowel elimination problem,
Concentrated urine,
Dry mucous membrane and
Dry Skin Turgor
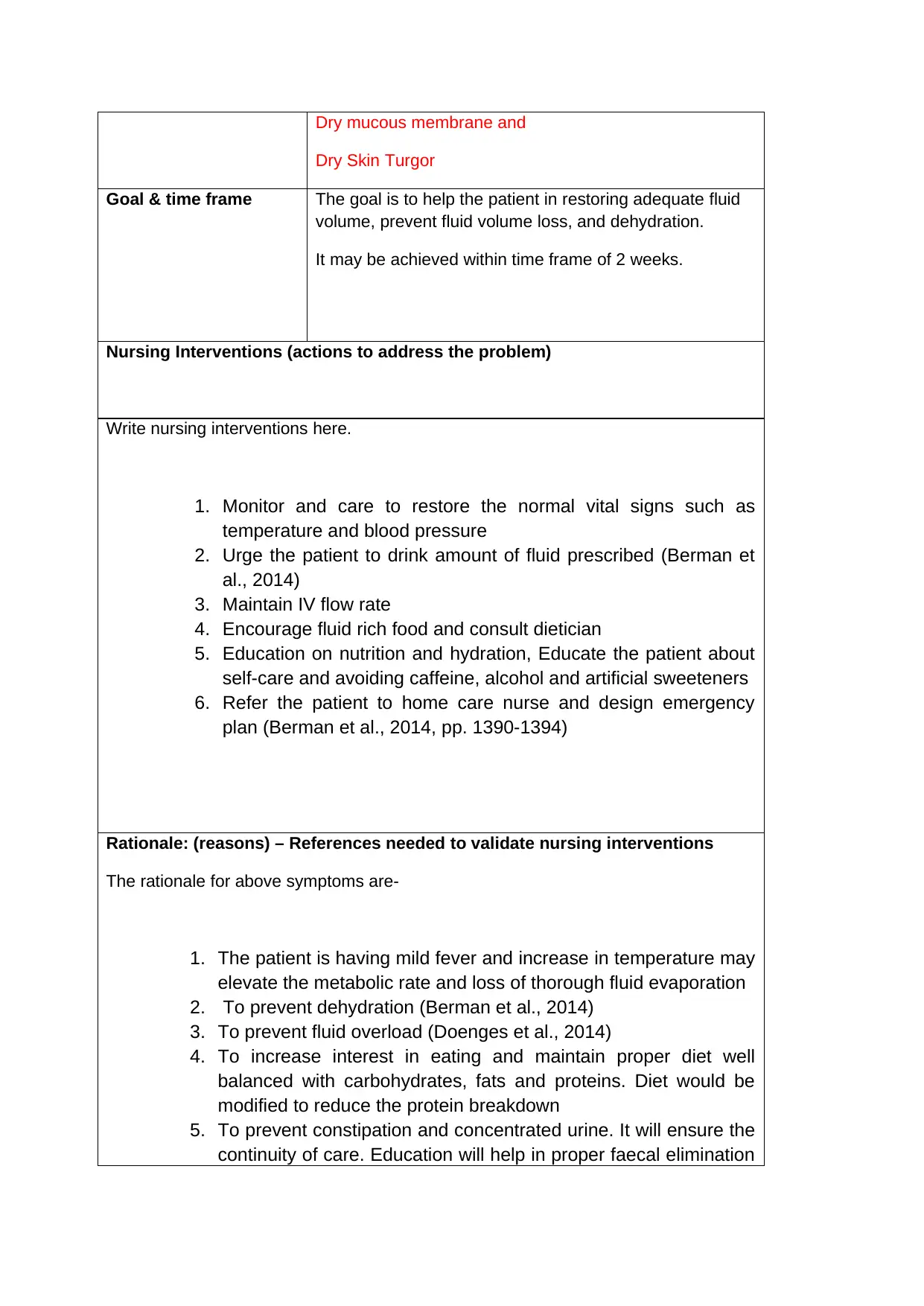
Goal & time frame The goal is to help the patient in restoring adequate fluid
volume, prevent fluid volume loss, and dehydration.
It may be achieved within time frame of 2 weeks.
Nursing Interventions (actions to address the problem)
Write nursing interventions here.
1. Monitor and care to restore the normal vital signs such as
temperature and blood pressure
2. Urge the patient to drink amount of fluid prescribed (Berman et
al., 2014)
3. Maintain IV flow rate
4. Encourage fluid rich food and consult dietician
5. Education on nutrition and hydration, Educate the patient about
self-care and avoiding caffeine, alcohol and artificial sweeteners
6. Refer the patient to home care nurse and design emergency
plan (Berman et al., 2014, pp. 1390-1394)
Rationale: (reasons) – References needed to validate nursing interventions
The rationale for above symptoms are-
1. The patient is having mild fever and increase in temperature may
elevate the metabolic rate and loss of thorough fluid evaporation
2. To prevent dehydration (Berman et al., 2014)
3. To prevent fluid overload (Doenges et al., 2014)
4. To increase interest in eating and maintain proper diet well
balanced with carbohydrates, fats and proteins. Diet would be
modified to reduce the protein breakdown
5. To prevent constipation and concentrated urine. It will ensure the
continuity of care. Education will help in proper faecal elimination
Dry Skin Turgor
Goal & time frame The goal is to help the patient in restoring adequate fluid
volume, prevent fluid volume loss, and dehydration.
It may be achieved within time frame of 2 weeks.
Nursing Interventions (actions to address the problem)
Write nursing interventions here.
1. Monitor and care to restore the normal vital signs such as
temperature and blood pressure
2. Urge the patient to drink amount of fluid prescribed (Berman et
al., 2014)
3. Maintain IV flow rate
4. Encourage fluid rich food and consult dietician
5. Education on nutrition and hydration, Educate the patient about
self-care and avoiding caffeine, alcohol and artificial sweeteners
6. Refer the patient to home care nurse and design emergency
plan (Berman et al., 2014, pp. 1390-1394)
Rationale: (reasons) – References needed to validate nursing interventions
The rationale for above symptoms are-
1. The patient is having mild fever and increase in temperature may
elevate the metabolic rate and loss of thorough fluid evaporation
2. To prevent dehydration (Berman et al., 2014)
3. To prevent fluid overload (Doenges et al., 2014)
4. To increase interest in eating and maintain proper diet well
balanced with carbohydrates, fats and proteins. Diet would be
modified to reduce the protein breakdown
5. To prevent constipation and concentrated urine. It will ensure the
continuity of care. Education will help in proper faecal elimination
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




