Case Study: Congestive Heart Failure and Nursing Care Strategies
VerifiedAdded on 2021/04/21
|10
|2744
|22
Case Study
AI Summary
This case study focuses on Mrs. McKenzie, who is suffering from congestive heart failure (CHF), a chronic condition where the heart cannot pump enough blood. The study explores the causes of CHF, including hypertension, myocardial infarction, and other risk factors. It details the pathophysiology, symptoms such as shortness of breath, fatigue, and swelling, and the two common drug classes used for treatment: Furosemide and ACE inhibitors (Lisinopril). The study also provides nursing care strategies, including the initial evaluation, monitoring of vital signs, and administration of medications. Furthermore, it emphasizes the importance of holistic care, including providing a calm environment and addressing the patient's emotional needs. The document references several research papers and guidelines to support the analysis and recommendations for patient care.

Running head: CONGESTIVE HEAR FAILURE
CONGESTIVE HEAR FAILURE
Name of the Student
Name of the university
Author’s note
CONGESTIVE HEAR FAILURE
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CONGESTIVE HEAR FAILURE
Answers
1. Congestive heart failure (CHF) is a chronic disease that is mainly caused due to the
inability of the heart to pump adequate amount of blood for meeting the oxygen demand
of various organs (Kemp & Conte, 2012). The case study reveals the fact that Mrs.
McKenzie has been suffering from diastolic cardiac failure as she has hypertension and
her respiratory rate is 30 bpm.
Congestive heart failure can be brought about by several causes. It can be caused
by cardiomyopathy (weakening of the heart muscles), damaged valves of the heart,
Ischemic cardiomyopathy, where the blood vessels supplying the coronary arteries gets
blocked (Kemp & Conte, 2012). Toxic exposure to alcohol and drugs can also cause this
disease. Left ventricular hypertrophy (thickening of the heart muscles) that is caused due
to hypertension may also act as the contributing factor. The risk factors contributing to
CHF are equal to the risk of stroke, coronary heart disease. According to Kemp & Conte,
(2012) hypertension is the most important risk factor accounting for about CHF in 59 %
of women and 39% of men (Dib, Matin, & Luckert, 2012). Elevated cholesterol, diabetes
and obesity are the other factors. It is evident that Mrs. Sharon McKenzie already had a
past history of Myocardial infarction at the age of 65. CHF occurs in about half of the
patients with MI. With CHF the stroke volume decreases but the cardiac index is
maintained by an increased heart rate. The minute work and the stroke work of the left
ventricles are decreased significantly further decreasing the end-diastolic pressure of the
left ventricle. This complicates the myocardial infarction causing CHF.
Answers
1. Congestive heart failure (CHF) is a chronic disease that is mainly caused due to the
inability of the heart to pump adequate amount of blood for meeting the oxygen demand
of various organs (Kemp & Conte, 2012). The case study reveals the fact that Mrs.
McKenzie has been suffering from diastolic cardiac failure as she has hypertension and
her respiratory rate is 30 bpm.
Congestive heart failure can be brought about by several causes. It can be caused
by cardiomyopathy (weakening of the heart muscles), damaged valves of the heart,
Ischemic cardiomyopathy, where the blood vessels supplying the coronary arteries gets
blocked (Kemp & Conte, 2012). Toxic exposure to alcohol and drugs can also cause this
disease. Left ventricular hypertrophy (thickening of the heart muscles) that is caused due
to hypertension may also act as the contributing factor. The risk factors contributing to
CHF are equal to the risk of stroke, coronary heart disease. According to Kemp & Conte,
(2012) hypertension is the most important risk factor accounting for about CHF in 59 %
of women and 39% of men (Dib, Matin, & Luckert, 2012). Elevated cholesterol, diabetes
and obesity are the other factors. It is evident that Mrs. Sharon McKenzie already had a
past history of Myocardial infarction at the age of 65. CHF occurs in about half of the
patients with MI. With CHF the stroke volume decreases but the cardiac index is
maintained by an increased heart rate. The minute work and the stroke work of the left
ventricles are decreased significantly further decreasing the end-diastolic pressure of the
left ventricle. This complicates the myocardial infarction causing CHF.
2CONGESTIVE HEAR FAILURE
The prevention and the treatment of CHF have risen to a burgeoning public health
problem. There are almost 20 million people worldwide who are affected by CHF.
According to the Australian commission for health and safety, about 5.2 millions of
Australians suffer from CHF, much of which is due the obesity and diabetes (Australian
heart Foundation, 2018). The estimated mortality due to CHF is about 286000. It follows
an exponential pattern affecting 6-10 % of the population over the age of 65. The
expected cost to the disease in Australia has been recorded to be $34.8 billion (Australian
heart Foundation, 2018).
CHF have not only affected the physical health of Mrs. Mackenzie, but also
contribute to her emotional burden. Sense of inferiority complex or discontent may come
due to the inability to do daily chores. Furthermore it will also contribute to the emotional
burden. CHF failure requires regular monitoring and costly medications and even hospital
stay. Hence this would also affect the economic condition of the family. The patient’s
husband may suffer from anxiety and may be perturbed about her wellbeing. Some
people even face from high levels of depressive symptoms.
2.
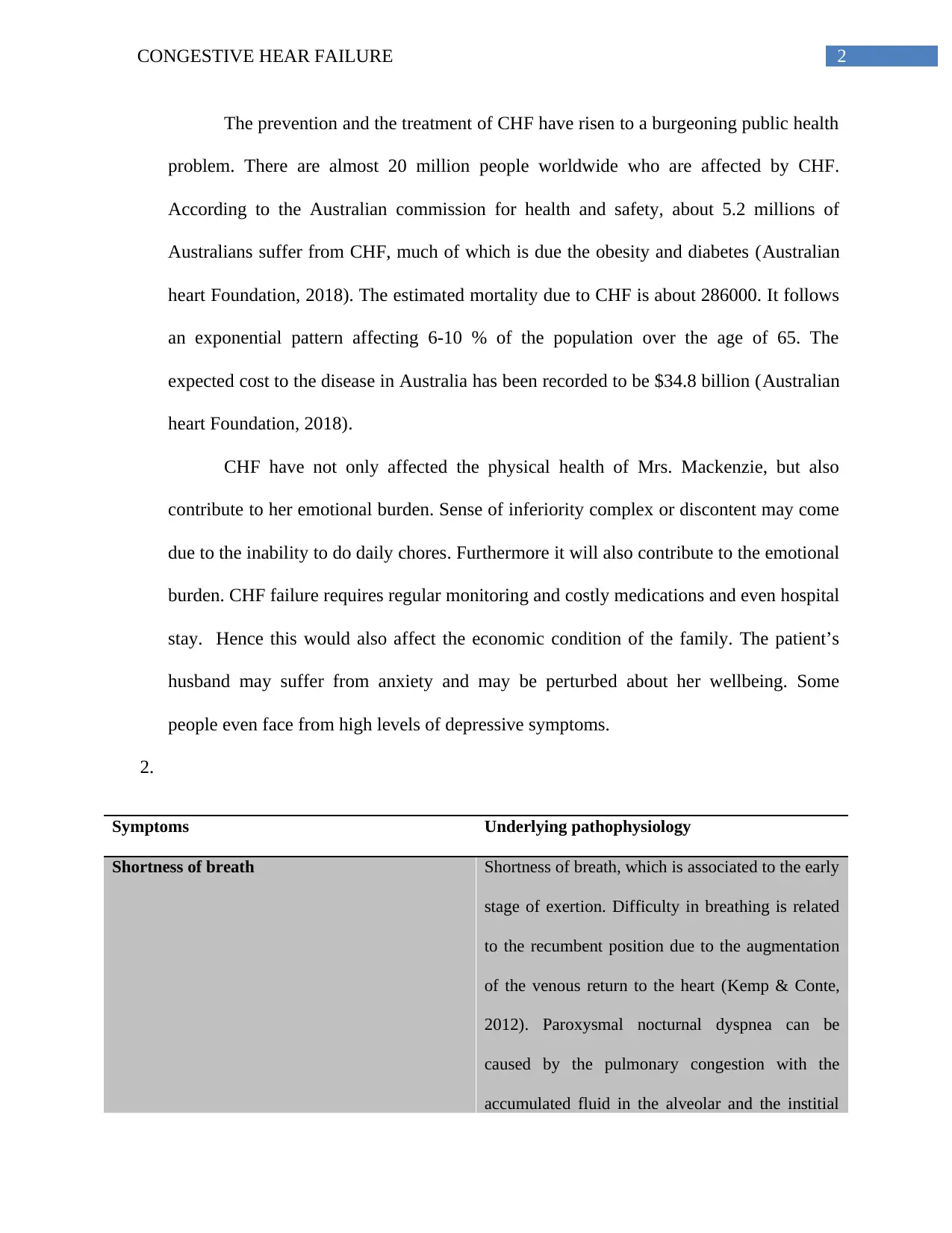
Symptoms Underlying pathophysiology
Shortness of breath Shortness of breath, which is associated to the early
stage of exertion. Difficulty in breathing is related
to the recumbent position due to the augmentation
of the venous return to the heart (Kemp & Conte,
2012). Paroxysmal nocturnal dyspnea can be
caused by the pulmonary congestion with the
accumulated fluid in the alveolar and the institial
The prevention and the treatment of CHF have risen to a burgeoning public health
problem. There are almost 20 million people worldwide who are affected by CHF.
According to the Australian commission for health and safety, about 5.2 millions of
Australians suffer from CHF, much of which is due the obesity and diabetes (Australian
heart Foundation, 2018). The estimated mortality due to CHF is about 286000. It follows
an exponential pattern affecting 6-10 % of the population over the age of 65. The
expected cost to the disease in Australia has been recorded to be $34.8 billion (Australian
heart Foundation, 2018).
CHF have not only affected the physical health of Mrs. Mackenzie, but also
contribute to her emotional burden. Sense of inferiority complex or discontent may come
due to the inability to do daily chores. Furthermore it will also contribute to the emotional
burden. CHF failure requires regular monitoring and costly medications and even hospital
stay. Hence this would also affect the economic condition of the family. The patient’s
husband may suffer from anxiety and may be perturbed about her wellbeing. Some
people even face from high levels of depressive symptoms.
2.
Symptoms Underlying pathophysiology
Shortness of breath Shortness of breath, which is associated to the early
stage of exertion. Difficulty in breathing is related
to the recumbent position due to the augmentation
of the venous return to the heart (Kemp & Conte,
2012). Paroxysmal nocturnal dyspnea can be
caused by the pulmonary congestion with the
accumulated fluid in the alveolar and the institial
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CONGESTIVE HEAR FAILURE
spaces developing pulmonary edema.
Lack of appetite and nausea Fluid buildup around the liver and the gut can
interfere with the process of digestion that may
cause changes in the appetite (Katz & Konstam,
2012). Nausea is a complex act that needs central
neurologic coordination. The neurologic
coordination of the components of nausea is
provided by the emetic center. The onset of nausea
can also be due to the changes in the hormonal
levels of arginine vasopressin (Cowie & Poole-
Wilson, 2013).
Sleeping disorders and nocturia Accumulation of the extra fluid s may increase the
rate of urination at night leading to sleeping
disorders (Sobotka et al., 2013). Some finds it
difficult to sleep without sitting upright. Renal
perfusion may increase when the patient is in a
supine position as when a patient lies down the
blood that has been accumulated in the extremities
return back to the heart and the cardiac output
increases (Sobotka et al., 2013). Compared to the
daytime. The augmented cardiac output perfuses
the kidney to produce more urine for decreasing the
work load of the heart.
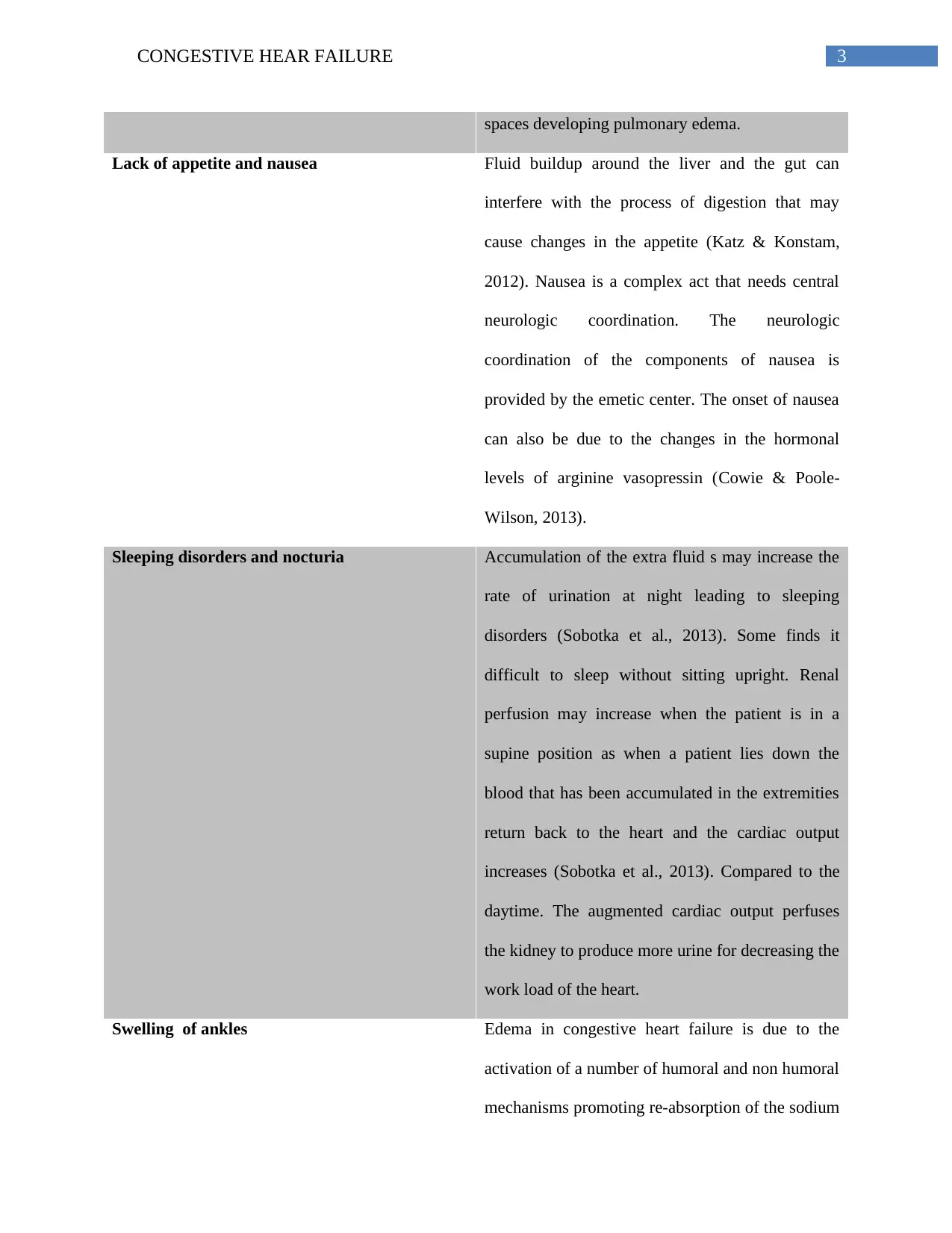
Swelling of ankles Edema in congestive heart failure is due to the
activation of a number of humoral and non humoral
mechanisms promoting re-absorption of the sodium
spaces developing pulmonary edema.
Lack of appetite and nausea Fluid buildup around the liver and the gut can
interfere with the process of digestion that may
cause changes in the appetite (Katz & Konstam,
2012). Nausea is a complex act that needs central
neurologic coordination. The neurologic
coordination of the components of nausea is
provided by the emetic center. The onset of nausea
can also be due to the changes in the hormonal
levels of arginine vasopressin (Cowie & Poole-
Wilson, 2013).
Sleeping disorders and nocturia Accumulation of the extra fluid s may increase the
rate of urination at night leading to sleeping
disorders (Sobotka et al., 2013). Some finds it
difficult to sleep without sitting upright. Renal
perfusion may increase when the patient is in a
supine position as when a patient lies down the
blood that has been accumulated in the extremities
return back to the heart and the cardiac output
increases (Sobotka et al., 2013). Compared to the
daytime. The augmented cardiac output perfuses
the kidney to produce more urine for decreasing the
work load of the heart.
Swelling of ankles Edema in congestive heart failure is due to the
activation of a number of humoral and non humoral
mechanisms promoting re-absorption of the sodium
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CONGESTIVE HEAR FAILURE
and water by the kidneys and the expansion of the
extracellular fluid (Kemp & Conte, 2012). As the
right ventricle of the heart begins to fail fluid
begins to collect in the feet (Kemp & Conte, 2012).
Fatigue Fatigue during congestive heart failure is mainly
caused due to the reduced cardiac output. CHF is
linked with the disruptive perfusion of the vital
organs, vasoconstrictive drive and diversion of the
blood flow away from the skin and muscle
circulations. This diversion causes muscular
fatigue. Reduced oxygen delivery can fatigue and
exhaustion (Mebazaa et al., 2015).
3. 2 common classes of drugs
Furosemide is a diuretic drug that is normally used for eliminating the water and salt
from the body (Bikdeli et al., 2013). It is used against the accumulation of the fluid in
the blood. It inhibits the re-absorption of the water in the nephron by the blockage of
the potassium- chloride co-transporters (NKCC22) in the Henle's loop of the nephron.
This mainly occurs due to the competitive inhibition occurring in the chloride binding
site of the cotransporter (Felker & Mentz, 2012). It prevents the transport of the
sodium from the Henle's loop in the basolateral interstitium. As a result the lumen
becomes hypertonic and the interstitium becomes less hypertonic, diminishing the
osmotic gradient for the absorption of the water in the nephron. The salt, water and
other molecules are normally filtered out of the blood in the kidneys and the filtered
and water by the kidneys and the expansion of the
extracellular fluid (Kemp & Conte, 2012). As the
right ventricle of the heart begins to fail fluid
begins to collect in the feet (Kemp & Conte, 2012).
Fatigue Fatigue during congestive heart failure is mainly
caused due to the reduced cardiac output. CHF is
linked with the disruptive perfusion of the vital
organs, vasoconstrictive drive and diversion of the
blood flow away from the skin and muscle
circulations. This diversion causes muscular
fatigue. Reduced oxygen delivery can fatigue and
exhaustion (Mebazaa et al., 2015).
3. 2 common classes of drugs
Furosemide is a diuretic drug that is normally used for eliminating the water and salt
from the body (Bikdeli et al., 2013). It is used against the accumulation of the fluid in
the blood. It inhibits the re-absorption of the water in the nephron by the blockage of
the potassium- chloride co-transporters (NKCC22) in the Henle's loop of the nephron.
This mainly occurs due to the competitive inhibition occurring in the chloride binding
site of the cotransporter (Felker & Mentz, 2012). It prevents the transport of the
sodium from the Henle's loop in the basolateral interstitium. As a result the lumen
becomes hypertonic and the interstitium becomes less hypertonic, diminishing the
osmotic gradient for the absorption of the water in the nephron. The salt, water and
other molecules are normally filtered out of the blood in the kidneys and the filtered
5CONGESTIVE HEAR FAILURE
fluid ultimately becomes the urine (Bikdeli et al., 2013). The sodium, chloride that
has been filtered out of the blood is reabsorbed in the blood and before the conversion
of the filtered fluid in to urine. Furosemide blocks the absorption of sodium, chloride
and water from the filtered fluid from the kidney leading to a profound increase of
urine. Thus this medicine can be used to cure the edema in the patient with CHF and
fluid retention (Felker & Mentz, 2012).
ACE inhibitors like lisinopril, can be used for patients having CHF, as Angiostenin
converting enzymes reduce the formation of the heart damaging hormones
(McMurray et al., 2013). It dilates the blood vessels to lower the blood pressure in
order to lessen the heart workload. It helps in blocking the formation of angiostenin
II, which narrows the blood vessels and increases the blood pressure. It works by
controlling the activity of the renin- angiostenin-aldosterone system (RAAS). RAAS
controls the bllod pressure fluctuations. Renin in secreted in the juxtaglomerular
structure of the kidney and this then produces the angieostenin. The angiostenin is
converted in to angiostenin II by the ACE which increases the fluid retention and
increased blood pressure. The ACE inhibitor blocks the conversion of the angiostenin
I to angeostenin II. Thus it can be considered as a suitable class of medication for Mrs
Mackenzie (McMurray et al., 2013).
4. Nursing care strategies: - At the time of admission a registered nurse should first
evaluate and treat the precipitating factors that have caused the heart failure right after the
admission the patient, the cardiac status of the patients should be evaluated by
electrocardiogram, echocardiogram (Krim et al., 2015).
fluid ultimately becomes the urine (Bikdeli et al., 2013). The sodium, chloride that
has been filtered out of the blood is reabsorbed in the blood and before the conversion
of the filtered fluid in to urine. Furosemide blocks the absorption of sodium, chloride
and water from the filtered fluid from the kidney leading to a profound increase of
urine. Thus this medicine can be used to cure the edema in the patient with CHF and
fluid retention (Felker & Mentz, 2012).
ACE inhibitors like lisinopril, can be used for patients having CHF, as Angiostenin
converting enzymes reduce the formation of the heart damaging hormones
(McMurray et al., 2013). It dilates the blood vessels to lower the blood pressure in
order to lessen the heart workload. It helps in blocking the formation of angiostenin
II, which narrows the blood vessels and increases the blood pressure. It works by
controlling the activity of the renin- angiostenin-aldosterone system (RAAS). RAAS
controls the bllod pressure fluctuations. Renin in secreted in the juxtaglomerular
structure of the kidney and this then produces the angieostenin. The angiostenin is
converted in to angiostenin II by the ACE which increases the fluid retention and
increased blood pressure. The ACE inhibitor blocks the conversion of the angiostenin
I to angeostenin II. Thus it can be considered as a suitable class of medication for Mrs
Mackenzie (McMurray et al., 2013).
4. Nursing care strategies: - At the time of admission a registered nurse should first
evaluate and treat the precipitating factors that have caused the heart failure right after the
admission the patient, the cardiac status of the patients should be evaluated by
electrocardiogram, echocardiogram (Krim et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CONGESTIVE HEAR FAILURE
The immediate drug that can be administered right after the hospital admissions
are furosemide, ethacrynic acid in order to inhibit the reabsorption of the sodium ,
potassium and the chloride from the Henle's loop (Australian heart Foundation, 2018).
Nurses should be careful regarding the dosing of the diuretics, as it is vital in
maintaining the normal volume status in patients with heart failure. After the initiation of
the diuretics, there should be a careful monitoring of the hemodynamics (Krim et al.,
2015). Bed rest is necessary during the hospital admission for improving the diuresis,
physical therapy with early ambulation is required in the first 24 hours of the admission.
Foley catheter can be used if the accurate assessment of urine cannot be done due to
factors such as incontinence (Krim et al., 2015).
The volume status should be assessed at least once in a day, including the
assessment of the peripheral edema, ascites, jugular venous pressure, hepatimegaly and
body weight (Feltner et al., 2014). The symptoms should be reevaluated and focus should
be given on the symptoms that triggered the hospital admission. There should be a close
monitoring of the vital signs in order to see the effects of diuretics in hypotension and
urine output (Bradley et al., 2013). The renal output and the balance in the electrolytes
should be maintained in order to ensure the replacements of the electrolytes. At the time
of the admission all the guideline directed therapies should be assessed and evaluated and
should be adjusted depending on the patient's condition (Bradley et al., 2013). Beta
blockers and ACE Inhibitors can be used to allow diuresis and perfusion of the target
organs (Feltner et al., 2014). ARBs can be used in patients who cannot tolerate ACE
inhibitors. The nurses should be cautious while applying the Beta blockers to the patients
The immediate drug that can be administered right after the hospital admissions
are furosemide, ethacrynic acid in order to inhibit the reabsorption of the sodium ,
potassium and the chloride from the Henle's loop (Australian heart Foundation, 2018).
Nurses should be careful regarding the dosing of the diuretics, as it is vital in
maintaining the normal volume status in patients with heart failure. After the initiation of
the diuretics, there should be a careful monitoring of the hemodynamics (Krim et al.,
2015). Bed rest is necessary during the hospital admission for improving the diuresis,
physical therapy with early ambulation is required in the first 24 hours of the admission.
Foley catheter can be used if the accurate assessment of urine cannot be done due to
factors such as incontinence (Krim et al., 2015).
The volume status should be assessed at least once in a day, including the
assessment of the peripheral edema, ascites, jugular venous pressure, hepatimegaly and
body weight (Feltner et al., 2014). The symptoms should be reevaluated and focus should
be given on the symptoms that triggered the hospital admission. There should be a close
monitoring of the vital signs in order to see the effects of diuretics in hypotension and
urine output (Bradley et al., 2013). The renal output and the balance in the electrolytes
should be maintained in order to ensure the replacements of the electrolytes. At the time
of the admission all the guideline directed therapies should be assessed and evaluated and
should be adjusted depending on the patient's condition (Bradley et al., 2013). Beta
blockers and ACE Inhibitors can be used to allow diuresis and perfusion of the target
organs (Feltner et al., 2014). ARBs can be used in patients who cannot tolerate ACE
inhibitors. The nurses should be cautious while applying the Beta blockers to the patients
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CONGESTIVE HEAR FAILURE
who have taken inotropic therapy at the time of their index hospitalisation and those with
newly diagnosed cardiac failure (Bradley et al., 2013).
Reduced cardiac output, decreased ambulation increases the risk of
thromboembolic events. In order to mitigate the risk, thromboembolism prophylaxis has
to be administered to the patients (Feltner et al., 2014). Nurses should ausculate the
breathe sound frequently for any crackles or wheezes, assess the bowel sounds for
visceral congestion can change the intestinal function and hence any signs of anorexia
should be reported. Nurses should encourage the patient to verbalize the feelings
(Mebazaa et al., 2015). The abdomen should be palpated and any reports of right upper
quadrant pain and tenderness should be reported (Feltner et al., 2014). The dietician
should be consulted with for providing the necessary diet to the patient that meets her
caloric needs within restricted sodium level. Nurses should be able to provide a holistic
care approach to the patient, which involves provision of a calm and quite environment,
helping the patient to manage stressful conditions, listen and respond to their feelings
(Rustad et al., 2012).
who have taken inotropic therapy at the time of their index hospitalisation and those with
newly diagnosed cardiac failure (Bradley et al., 2013).
Reduced cardiac output, decreased ambulation increases the risk of
thromboembolic events. In order to mitigate the risk, thromboembolism prophylaxis has
to be administered to the patients (Feltner et al., 2014). Nurses should ausculate the
breathe sound frequently for any crackles or wheezes, assess the bowel sounds for
visceral congestion can change the intestinal function and hence any signs of anorexia
should be reported. Nurses should encourage the patient to verbalize the feelings
(Mebazaa et al., 2015). The abdomen should be palpated and any reports of right upper
quadrant pain and tenderness should be reported (Feltner et al., 2014). The dietician
should be consulted with for providing the necessary diet to the patient that meets her
caloric needs within restricted sodium level. Nurses should be able to provide a holistic
care approach to the patient, which involves provision of a calm and quite environment,
helping the patient to manage stressful conditions, listen and respond to their feelings
(Rustad et al., 2012).
8CONGESTIVE HEAR FAILURE
References
Alt, E. (2014). U.S. Patent No. 8,777,851. Washington, DC: U.S. Patent and Trademark Office.
Australian Foundation, T. (2018). Heart attack treatment. The Heart Foundation. Retrieved 24
March 2018, from https://www.heartfoundation.org.au/after-my-heart-attack/heart-attack-
treatment
Bikdeli, B., Strait, K. M., Dharmarajan, K., Partovian, C., Coca, S. G., Kim, N., ... & Krumholz,
H. M. (2013). Dominance of furosemide for loop diuretic therapy in heart failure: time to
revisit the alternatives?. Journal of the American College of Cardiology, 61(14), 1549-
1550.
Bradley, E. H., Curry, L., Horwitz, L. I., Sipsma, H., Wang, Y., Walsh, M. N., ... & Krumholz,
H. M. (2013). Hospital strategies associated with 30-day readmission rates for patients
with heart failure. Circulation: Cardiovascular Quality and Outcomes, 6(4), 444-450.
Cowie, M. R., & Poole-Wilson, P. A. (2013). Pathophysiology of heart failure. In Essential
cardiology (pp. 327-345). Springer, New York, NY.
Dib, J. E., Matin, S. A., & Luckert, A. (2012). Prehospital use of continuous positive airway
pressure for acute severe congestive heart failure. Journal of Emergency Medicine, 42(5),
553-558.
Felker, G. M., & Mentz, R. J. (2012). Diuretics and ultrafiltration in acute decompensated heart
failure. Journal of the American College of Cardiology, 59(24), 2145-2153.
References
Alt, E. (2014). U.S. Patent No. 8,777,851. Washington, DC: U.S. Patent and Trademark Office.
Australian Foundation, T. (2018). Heart attack treatment. The Heart Foundation. Retrieved 24
March 2018, from https://www.heartfoundation.org.au/after-my-heart-attack/heart-attack-
treatment
Bikdeli, B., Strait, K. M., Dharmarajan, K., Partovian, C., Coca, S. G., Kim, N., ... & Krumholz,
H. M. (2013). Dominance of furosemide for loop diuretic therapy in heart failure: time to
revisit the alternatives?. Journal of the American College of Cardiology, 61(14), 1549-
1550.
Bradley, E. H., Curry, L., Horwitz, L. I., Sipsma, H., Wang, Y., Walsh, M. N., ... & Krumholz,
H. M. (2013). Hospital strategies associated with 30-day readmission rates for patients
with heart failure. Circulation: Cardiovascular Quality and Outcomes, 6(4), 444-450.
Cowie, M. R., & Poole-Wilson, P. A. (2013). Pathophysiology of heart failure. In Essential
cardiology (pp. 327-345). Springer, New York, NY.
Dib, J. E., Matin, S. A., & Luckert, A. (2012). Prehospital use of continuous positive airway
pressure for acute severe congestive heart failure. Journal of Emergency Medicine, 42(5),
553-558.
Felker, G. M., & Mentz, R. J. (2012). Diuretics and ultrafiltration in acute decompensated heart
failure. Journal of the American College of Cardiology, 59(24), 2145-2153.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CONGESTIVE HEAR FAILURE
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ... &
Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for persons
with heart failure: a systematic review and meta-analysis. Annals of internal medicine,
160(11), 774-784.
Katz, A. M., & Konstam, M. A. (2012). Heart failure: pathophysiology, molecular biology, and
clinical management. Lippincott Williams & Wilkins.
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371.
Krim, S. R., Campbell, P. T., Desai, S., Mandras, S., Patel, H., Eiswirth, C., & Ventura, H. O.
(2015). Management of Patients Admitted with Acute Decompensated Heart Failure. The
Ochsner Journal, 15(3), 284–289.
McMurray, J. J., Packer, M., Desai, A. S., Gong, J., Lefkowitz, M. P., Rizkala, A. R., ... & Zile,
M. R. (2014). Angiotensin–neprilysin inhibition versus enalapril in heart failure. New
England Journal of Medicine, 371(11), 993-1004.
Mebazaa, A., Yilmaz, M. B., Levy, P., Ponikowski, P., Peacock, W. F., Laribi, S., ... &
McDonagh, T. (2015). Recommendations on pre‐hospital & early hospital management
of acute heart failure: a consensus paper from the Heart Failure Association of the
European Society of Cardiology, the European Society of Emergency Medicine and the
Society of Academic Emergency Medicine. European journal of heart failure, 17(6),
544-558.
Rustad, J. K., Stern, T. A., Hebert, K. A., & Musselman, D. L. (2013). Diagnosis and treatment
of depression in patients with congestive heart failure: a review of the literature. The
primary care companion for CNS disorders, 15(4).
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ... &
Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for persons
with heart failure: a systematic review and meta-analysis. Annals of internal medicine,
160(11), 774-784.
Katz, A. M., & Konstam, M. A. (2012). Heart failure: pathophysiology, molecular biology, and
clinical management. Lippincott Williams & Wilkins.
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371.
Krim, S. R., Campbell, P. T., Desai, S., Mandras, S., Patel, H., Eiswirth, C., & Ventura, H. O.
(2015). Management of Patients Admitted with Acute Decompensated Heart Failure. The
Ochsner Journal, 15(3), 284–289.
McMurray, J. J., Packer, M., Desai, A. S., Gong, J., Lefkowitz, M. P., Rizkala, A. R., ... & Zile,
M. R. (2014). Angiotensin–neprilysin inhibition versus enalapril in heart failure. New
England Journal of Medicine, 371(11), 993-1004.
Mebazaa, A., Yilmaz, M. B., Levy, P., Ponikowski, P., Peacock, W. F., Laribi, S., ... &
McDonagh, T. (2015). Recommendations on pre‐hospital & early hospital management
of acute heart failure: a consensus paper from the Heart Failure Association of the
European Society of Cardiology, the European Society of Emergency Medicine and the
Society of Academic Emergency Medicine. European journal of heart failure, 17(6),
544-558.
Rustad, J. K., Stern, T. A., Hebert, K. A., & Musselman, D. L. (2013). Diagnosis and treatment
of depression in patients with congestive heart failure: a review of the literature. The
primary care companion for CNS disorders, 15(4).
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





