Cooperative Wound Clinic Model: Impact on Patient Outcomes & Care
VerifiedAdded on 2023/05/26
|7
|8008
|333
Report
AI Summary
This report evaluates the impact of a Cooperative Wound Clinic (CWC) model on improving patient outcomes through enhanced wound management practices in primary health care. The study, employing a longitudinal pre-post design across multiple Australian states, focused on coaching general practitioners and practice nurses in evidence-based wound care. Key findings revealed increased confidence among health professionals in managing various wound types, attributed to repetitive coaching over six months. The CWC model, inspired by the 'Leg Club' approach, fostered a holistic environment emphasizing social interaction, education, and peer support. The intervention, which incorporated local wound experts for training and coaching, demonstrated a positive impact on patient outcomes, knowledge, and satisfaction. The report concludes that expanding this model could empower nurses, improve wound management capabilities, and ultimately lead to better patient care within primary health settings. Task 1 involves answering questions related to the nurse's role in observing and documenting healing progress, as well as criteria for evaluating the effectiveness of wound management strategies and dressing products.

Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
Collegian xxx (2018) xxx–xxx
Contentslists available at ScienceDirect
Collegian
j o u rn a l h om e p a g e :w w w . e l s e v i e r . c o m / l o c a t e / c o l l
Improving patient outcomesby coachingprimary health general
practitioners and practice nurses in evidencebasedwound
managementat on-site wound clinics
K. Innes-Walkera,b, C.N. Parkera,b,∗, K.J. Finlaysona,b, M. Brooksc, L. Youngd, N. Morley e,
D. Maresco-Pennisif, H.E. Edwardsa,b
a Wound ManagementInnovationCooperativeResearchCentre,OxleyHouse,25 Donkin St West End,QLD,Australia
b Facultyof Health,Instituteof Health& BiomedicalInnovation,QueenslandUniversityof Technology,60 Musk Ave.Kelvin Grove,QLD 4059,Australia
c World of Wounds,LatrobeUniversity,Bundoora,Victoria3086,Australia
d Wound ManagementNursePractitioner,TasmanianHealthService,SouthernRegion,Hobart,Tasmania,Australia
e VascularNursePractitioner,QueenslandHealth,BrisbaneSouth,QLD,Australia
f UniversityQueenslandCentrefor Clinical Research,Facultyof Medicine,Royal Brisbaneand Women’sHospital,Brisbane,QLD,Australia
a r t i c l e i n f o
Articlehistory:
Received19 May 2017
Receivedin revised form 7 March 2018
Accepted18 March 2018
Available online xxx
Keywords:
Wound management
Primary health care
Wound clinic
Model of care
General practice
a b s t r a c t
Background:Wound management is frequently performed in the community and forms a large part
of daily activities of General Practice health professionals.However, previous research has acknowl-
edgeda need for further educationand training on evidencebasedwound managementfor these health
professionals.
Aim: The aim of this project was to develop and trial a CooperativeWound Clinic model of care in Gen-
eral Practices,using a nurse led, interdisciplinary, holistic approach; including training and coaching to
increasethe wound managementexpertiseand capacityof health professionalsworking in the primary
healthcareenvironment.
Methods:A longitudinal, pre-post design was used. Four CooperativeWound Clinic pilot sites and nine
wound clinics were establishedin General Practicesacrossthree Australian stateswith the intervention
of the study being the model of care and incorporating a local wound expert employed to provide the
training and coaching.Pre and post survey data were collectedon wound managementpractices,health
professional confidence in evidence based wound management,patient health, wellbeing and healing
outcomes.Longitudinal patient data were collectedfor 24 weeks.
Findings:Resultsincluded an increasein the confidenceof health professionalsto managewounds. Util-
isation of a repetitive coachingmodel over a six month period empowered the decision making process
and assessmentknowledge for a variety of wound types. A positive impact on patient outcomes for a
variety of wound types was also observed.
Conclusion:The potential for expandingthis model will bring many benefitsincluding: empowerment of
nurses’confidencein managingwounds, promoting the role of nurse led clinics; improved wound related
capabilityand confidenceof health professionals;improved wound management,patient knowledgeand
better patient satisfactionand outcomes.
© 2018 Australian Collegeof Nursing Ltd. Published by Elsevier Ltd.
Problem
Primary Health is a high priority area requiring more education
and training particularly around evidence based wound manage-
ment practice.
∗ Corresponding author at: QueenslandUniversity of Technology,Victoria Park
Rd. Kelvin Grove, QLD 4059, Australia.
E-mail address:christina.parker@qut.edu.au(C.N. Parker).
What is already known
Wound managementoccurs primarily in the community with
wounds being a common admission diagnosis to community
nursing services and general practice where patients are seen
for frequent on-going visits. There are many barriers to nurses
updating their evidence based wound management knowledge
and significant social and economic benefits would be gained if
resourcesand strategieswere directed to facilitating implementa-
https://doi.org/10.1016/j.colegn.2018.03.004
1322-7696/©2018 Australian Collegeof Nursing Ltd. Published by Elsevier Ltd.
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
Collegian xxx (2018) xxx–xxx
Contentslists available at ScienceDirect
Collegian
j o u rn a l h om e p a g e :w w w . e l s e v i e r . c o m / l o c a t e / c o l l
Improving patient outcomesby coachingprimary health general
practitioners and practice nurses in evidencebasedwound
managementat on-site wound clinics
K. Innes-Walkera,b, C.N. Parkera,b,∗, K.J. Finlaysona,b, M. Brooksc, L. Youngd, N. Morley e,
D. Maresco-Pennisif, H.E. Edwardsa,b
a Wound ManagementInnovationCooperativeResearchCentre,OxleyHouse,25 Donkin St West End,QLD,Australia
b Facultyof Health,Instituteof Health& BiomedicalInnovation,QueenslandUniversityof Technology,60 Musk Ave.Kelvin Grove,QLD 4059,Australia
c World of Wounds,LatrobeUniversity,Bundoora,Victoria3086,Australia
d Wound ManagementNursePractitioner,TasmanianHealthService,SouthernRegion,Hobart,Tasmania,Australia
e VascularNursePractitioner,QueenslandHealth,BrisbaneSouth,QLD,Australia
f UniversityQueenslandCentrefor Clinical Research,Facultyof Medicine,Royal Brisbaneand Women’sHospital,Brisbane,QLD,Australia
a r t i c l e i n f o
Articlehistory:
Received19 May 2017
Receivedin revised form 7 March 2018
Accepted18 March 2018
Available online xxx
Keywords:
Wound management
Primary health care
Wound clinic
Model of care
General practice
a b s t r a c t
Background:Wound management is frequently performed in the community and forms a large part
of daily activities of General Practice health professionals.However, previous research has acknowl-
edgeda need for further educationand training on evidencebasedwound managementfor these health
professionals.
Aim: The aim of this project was to develop and trial a CooperativeWound Clinic model of care in Gen-
eral Practices,using a nurse led, interdisciplinary, holistic approach; including training and coaching to
increasethe wound managementexpertiseand capacityof health professionalsworking in the primary
healthcareenvironment.
Methods:A longitudinal, pre-post design was used. Four CooperativeWound Clinic pilot sites and nine
wound clinics were establishedin General Practicesacrossthree Australian stateswith the intervention
of the study being the model of care and incorporating a local wound expert employed to provide the
training and coaching.Pre and post survey data were collectedon wound managementpractices,health
professional confidence in evidence based wound management,patient health, wellbeing and healing
outcomes.Longitudinal patient data were collectedfor 24 weeks.
Findings:Resultsincluded an increasein the confidenceof health professionalsto managewounds. Util-
isation of a repetitive coachingmodel over a six month period empowered the decision making process
and assessmentknowledge for a variety of wound types. A positive impact on patient outcomes for a
variety of wound types was also observed.
Conclusion:The potential for expandingthis model will bring many benefitsincluding: empowerment of
nurses’confidencein managingwounds, promoting the role of nurse led clinics; improved wound related
capabilityand confidenceof health professionals;improved wound management,patient knowledgeand
better patient satisfactionand outcomes.
© 2018 Australian Collegeof Nursing Ltd. Published by Elsevier Ltd.
Problem
Primary Health is a high priority area requiring more education
and training particularly around evidence based wound manage-
ment practice.
∗ Corresponding author at: QueenslandUniversity of Technology,Victoria Park
Rd. Kelvin Grove, QLD 4059, Australia.
E-mail address:christina.parker@qut.edu.au(C.N. Parker).
What is already known
Wound managementoccurs primarily in the community with
wounds being a common admission diagnosis to community
nursing services and general practice where patients are seen
for frequent on-going visits. There are many barriers to nurses
updating their evidence based wound management knowledge
and significant social and economic benefits would be gained if
resourcesand strategieswere directed to facilitating implementa-
https://doi.org/10.1016/j.colegn.2018.03.004
1322-7696/©2018 Australian Collegeof Nursing Ltd. Published by Elsevier Ltd.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
2 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
tion of strategies to increase evidence based practices in wound
managementin these health areas.
What this paper adds
The establishment of Cooperative Wound Clinics improved
patient outcomes by enhancing the capabilities of health profes-
sionals in primary health care settings to implement evidence
based wound management.
1. Introduction
The majority of wounds progress smoothly through the stages
of healing, however, some wounds will remain unhealed for
long periods of time. Wounds can occur as a disruption of skin
integrity, as part of a disease process, or from intentional or acci-
dental indications (Young & McNaught, 2011). Having a wound
can be debilitating and patients often suffer multiple symptoms
and effects,including pain, reduced mobility, lower limb oedema,
venous eczema, wound exudate, decreased quality of life and
depression (Jones, Barr, Robinson, & Carlisle, 2006; Parker, 2012).
The effects of chronic leg ulcers involves 1–3% of the population
(Briggs & Closs, 2003; Margolis, Bilker, Santanna, & Baumgarten,
2002) with many remaining unhealed for years or even decades.
Caring for acute and chronic wounds is a multi-billion dollar bur-
den on Australia’s health system with reported costs in excess of
A$3 billion (The Australian Wound Management Association Inc &
The New ZealandWound Care Society Inc, 2011).
Wound managementoccurs primarily in the community with
wounds being a common reason for admission to community nurs-
ing services (RDNS, 2008) and/or General Practice (GP), where
patients are seen for frequent, on-going visits. One study investi-
gating adults with leg ulcers who were visiting GPs for care of their
ulcers, found that 82%attended1–2 times/week for a median of 21
weeks (Edwards et al., 2014). The ageing of the Australian popula-
tion, the increasing incidence of chronic illnesses and recognised
inequities in accessto health care have prompted governmentsto
look for new ways to fund care that has more of a focus on pre-
vention and ongoing disease management (Jolly, 2007). This has
resulted in current health care policy that aims to transfer health
services from the hospital sector to primary care where possible.
With the number of nurses in GPs rapidly increasing from 7728 in
2007 to 10,683 in 2012 (Australian Medicare Local Alliance, 2012),
nursesare well placedto play a lead role in redesigningcareto meet
these challenges.
Wound managementis a large and important part of the daily
activities for most primary health care nurses (Australian Medicare
Local Alliance, 2012). The treatment of people with wounds is an
important issue for nearly every GP in Australia (Britt et al., 2012).
In 2011–12, a considerable proportion (33%) of Medicare claims
were for wound management item numbers (Britt et al., 2012).
Dressings accounted for 20%of all procedures performed by prac-
tice nurses and three of the five most common procedures in GPs
involved wound management(Britt et al., 2012).An education and
training needs analysis performed by the Wound Management
Innovation Cooperative Research Centre indicated that primary
health care was a high priority area requiring more education and
training around evidencebased best wound managementpractice
(Innes-Walker & Edwards,2013).There are many well documented
barriers to nurses updating their evidence based wound manage-
ment knowledge (Coyer, Edwards, & Finlayson, 2005), however, it
has been indicated that significant social and economic benefits
would be gained if resourcesand strategieswere directed to facil-
itating implementation of these strategies in GP (Edwards et al.,
2013; Graves,Finlayson, Gibb, O’Reilly, & Edwards, 2014).
This project implemented a Cooperative Wound Clinic (CWC)
model of care which was underpinned by the principles of the “Leg
Club®
” model of care, developed in the United Kingdom (Lindsay,
2004),and utilising a coachingmodel of education.The “LegClub®”
model provides wound managementfor patients with an emphasis
on social interaction, education,participation and peer support for
patients (Lindsay,2004).A randomised controlled trial in Australia
that compared this model of care to in-home wound care reported
significant improved outcomes in patient quality of life, morale,
self-esteem, healing, pain and functional ability of the patient
(Edwards,Courtney,Finlayson,Shuter,& Lindsay,2009).It was pro-
posed that a service delivery model based on the Leg Club® model
undertaken in a primary health care environment would also offer
improved outcomes for patients and the health care system.
The CWC model of care also utilised coaching strategies
designed to provide holistic, evidence based care and dedicated
wound management clinic time to patients through the utilisa-
tion of a coaching model of education with a wound care expert.
A coaching role in the delivery of education and clinical skills has
been used effectively and has been noted to encouragecommuni-
cation, leadership and adaptability (Johnson, Hamilton, Delaney,
& Pennington, 2011), while utilising skills in facilitation, prac-
tice development principles, adult learning strategies to support
a person centred approach to care (Faithfull-Byrne et al., 2016).
The successful utilisation of a coaching model has also been
shown to increase documented assessments and knowledge in
chronic conditions (Johnston et al., 2007) and health organisa-
tions (Faithfull-Byrne et al., 2016). The role of a practice nurse
in today’s medical environment often occurs in rapidly changing
circumstancesand contemporary demandsfor workplace learning
have been supported by coachingroles in teaching(Faithfull-Byrne
et al., 2016). One-on-one or small group coaching allows for health
professionals to be able to coach other staff through the wound
assessmentand managementprocess,allowing for questions to be
asked and critical decision making to be discussedthroughout the
process.This included staff developmenttraining, work integrated
learning and the development of organised referral pathways for
multidisciplinary care as appropriate.
Specifically, the expert attended the clinic and simultaneously
led education to the health professionals and care to patients to
facilitate the transfer of learning into practice. The wound expert
used a patient centred approach incorporating holistic assessment
and the development of plans with the health professional and
patients and families while also encouraging the socialisation of
patients and/or families and carerswith other patients and/or fam-
ilies and carers in the wound clinic environment as per the Leg
Club® model of care.
2. Aim
The aim of this project was to evaluateoutcomes following the
implementation of the CWC model on:
• Health professionals’knowledge and patients’satisfaction about
evidencebased practice in wound management;
• Feasibility and sustainability within the primary care setting; and
• Patient outcomes (healing and quality of life).
3. Methods
3.1. Design
A longitudinal, pre-post design was used where survey data
from health professionals and patients were collected prior
to implementation of the intervention and 24 weeks post-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
2 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
tion of strategies to increase evidence based practices in wound
managementin these health areas.
What this paper adds
The establishment of Cooperative Wound Clinics improved
patient outcomes by enhancing the capabilities of health profes-
sionals in primary health care settings to implement evidence
based wound management.
1. Introduction
The majority of wounds progress smoothly through the stages
of healing, however, some wounds will remain unhealed for
long periods of time. Wounds can occur as a disruption of skin
integrity, as part of a disease process, or from intentional or acci-
dental indications (Young & McNaught, 2011). Having a wound
can be debilitating and patients often suffer multiple symptoms
and effects,including pain, reduced mobility, lower limb oedema,
venous eczema, wound exudate, decreased quality of life and
depression (Jones, Barr, Robinson, & Carlisle, 2006; Parker, 2012).
The effects of chronic leg ulcers involves 1–3% of the population
(Briggs & Closs, 2003; Margolis, Bilker, Santanna, & Baumgarten,
2002) with many remaining unhealed for years or even decades.
Caring for acute and chronic wounds is a multi-billion dollar bur-
den on Australia’s health system with reported costs in excess of
A$3 billion (The Australian Wound Management Association Inc &
The New ZealandWound Care Society Inc, 2011).
Wound managementoccurs primarily in the community with
wounds being a common reason for admission to community nurs-
ing services (RDNS, 2008) and/or General Practice (GP), where
patients are seen for frequent, on-going visits. One study investi-
gating adults with leg ulcers who were visiting GPs for care of their
ulcers, found that 82%attended1–2 times/week for a median of 21
weeks (Edwards et al., 2014). The ageing of the Australian popula-
tion, the increasing incidence of chronic illnesses and recognised
inequities in accessto health care have prompted governmentsto
look for new ways to fund care that has more of a focus on pre-
vention and ongoing disease management (Jolly, 2007). This has
resulted in current health care policy that aims to transfer health
services from the hospital sector to primary care where possible.
With the number of nurses in GPs rapidly increasing from 7728 in
2007 to 10,683 in 2012 (Australian Medicare Local Alliance, 2012),
nursesare well placedto play a lead role in redesigningcareto meet
these challenges.
Wound managementis a large and important part of the daily
activities for most primary health care nurses (Australian Medicare
Local Alliance, 2012). The treatment of people with wounds is an
important issue for nearly every GP in Australia (Britt et al., 2012).
In 2011–12, a considerable proportion (33%) of Medicare claims
were for wound management item numbers (Britt et al., 2012).
Dressings accounted for 20%of all procedures performed by prac-
tice nurses and three of the five most common procedures in GPs
involved wound management(Britt et al., 2012).An education and
training needs analysis performed by the Wound Management
Innovation Cooperative Research Centre indicated that primary
health care was a high priority area requiring more education and
training around evidencebased best wound managementpractice
(Innes-Walker & Edwards,2013).There are many well documented
barriers to nurses updating their evidence based wound manage-
ment knowledge (Coyer, Edwards, & Finlayson, 2005), however, it
has been indicated that significant social and economic benefits
would be gained if resourcesand strategieswere directed to facil-
itating implementation of these strategies in GP (Edwards et al.,
2013; Graves,Finlayson, Gibb, O’Reilly, & Edwards, 2014).
This project implemented a Cooperative Wound Clinic (CWC)
model of care which was underpinned by the principles of the “Leg
Club®
” model of care, developed in the United Kingdom (Lindsay,
2004),and utilising a coachingmodel of education.The “LegClub®”
model provides wound managementfor patients with an emphasis
on social interaction, education,participation and peer support for
patients (Lindsay,2004).A randomised controlled trial in Australia
that compared this model of care to in-home wound care reported
significant improved outcomes in patient quality of life, morale,
self-esteem, healing, pain and functional ability of the patient
(Edwards,Courtney,Finlayson,Shuter,& Lindsay,2009).It was pro-
posed that a service delivery model based on the Leg Club® model
undertaken in a primary health care environment would also offer
improved outcomes for patients and the health care system.
The CWC model of care also utilised coaching strategies
designed to provide holistic, evidence based care and dedicated
wound management clinic time to patients through the utilisa-
tion of a coaching model of education with a wound care expert.
A coaching role in the delivery of education and clinical skills has
been used effectively and has been noted to encouragecommuni-
cation, leadership and adaptability (Johnson, Hamilton, Delaney,
& Pennington, 2011), while utilising skills in facilitation, prac-
tice development principles, adult learning strategies to support
a person centred approach to care (Faithfull-Byrne et al., 2016).
The successful utilisation of a coaching model has also been
shown to increase documented assessments and knowledge in
chronic conditions (Johnston et al., 2007) and health organisa-
tions (Faithfull-Byrne et al., 2016). The role of a practice nurse
in today’s medical environment often occurs in rapidly changing
circumstancesand contemporary demandsfor workplace learning
have been supported by coachingroles in teaching(Faithfull-Byrne
et al., 2016). One-on-one or small group coaching allows for health
professionals to be able to coach other staff through the wound
assessmentand managementprocess,allowing for questions to be
asked and critical decision making to be discussedthroughout the
process.This included staff developmenttraining, work integrated
learning and the development of organised referral pathways for
multidisciplinary care as appropriate.
Specifically, the expert attended the clinic and simultaneously
led education to the health professionals and care to patients to
facilitate the transfer of learning into practice. The wound expert
used a patient centred approach incorporating holistic assessment
and the development of plans with the health professional and
patients and families while also encouraging the socialisation of
patients and/or families and carerswith other patients and/or fam-
ilies and carers in the wound clinic environment as per the Leg
Club® model of care.
2. Aim
The aim of this project was to evaluateoutcomes following the
implementation of the CWC model on:
• Health professionals’knowledge and patients’satisfaction about
evidencebased practice in wound management;
• Feasibility and sustainability within the primary care setting; and
• Patient outcomes (healing and quality of life).
3. Methods
3.1. Design
A longitudinal, pre-post design was used where survey data
from health professionals and patients were collected prior
to implementation of the intervention and 24 weeks post-

Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 3
implementation of the intervention. The outcome measures
included health professionals’ knowledge, confidence and prac-
tices re evidencebased wound management,and patient outcome
measures of wound healing and prevention measures and satis-
faction with care.The health professional survey collected data on
demographics,education, clinical practice details, confidence lev-
els and barriers and limitations in assessment,managementand
prevention of wounds. Patient data collected when attending the
wound clinic at the first visit with a wound or for prevention strate-
giesincluded demographic,medical history, wound characteristics,
wound managementand prevention strategies; and then further
data (wound characteristics)were collected from patients attend-
ing the clinic at least every two weeks or until healing for open
wounds.
3.2. Procedure
Nine nurse-led CWCs were established in a variety of GP
practices which were located across three Australian states
(Queensland,Victoria and Tasmania).A local wound expert in each
state was employed to assist health professionals to consult with
patients and to provide training and coachingat each of thesesites.
The role of the expert trainer was to provide evidence-basedwound
managementtraining and coaching for general health profession-
als as well as playing an active clinical role in the clinic for the time
that they were there. The expert trainer was in most casesa Nurse
Practitioner in wound management.
The expert trainer as part of the intervention in this study was
involved in the initial training of health professionals within each
of the clinics and then attended the clinic once/fortnight to coach
and mentor staff in clinical practice.The initial training in the prac-
tice included a workshop that covered the implementation of the
model of care,wound aetiologies,wound assessment,management
and prevention principles and evidence based practice including
the need for good documentation.The need for a multidisciplinary
approach to wound care was enforced and a referral pathway was
provided to health professionalsin chart form that included details
of specialist clinics and health professionals within the area that
could offer specialist wound care advice. This workshop utilised
PowerPoint presentationsthat also included case studies and real
life scenarios. To assist with staff education, a wound education
and training material package named the CWC ResourceKit was
developed as part of the project and was made available to health
professionals and patients. The training content was also specifi-
cally directed towards GP with the necessaryincorporation of the
relevant MBS item numbers that may be relevant to wound care
practice.
This was followed up by the wound expert attending wound
care appointmentsonce/fortnight where the wound expert worked
with the health professionalstaff to treat the patientsusing a coach-
ing model of teaching. The wound expert would work with the
health professionalsto complete an assessmentof a patient with a
wound followed by the planning and implementation of evidence
based care for that patient. The health professionals were encour-
aged over time to complete all skills themselveswith the ability to
ask questions and discuss options with the wound expert. Sociali-
sation of patients and carerswas encouragedby scheduling at least
two visits at the same time and in the same room. Referral path-
ways were developedin consultation with GP health professionals
and utilised for referral on to specialists as appropriate.
Follow up attendance at clinical appointments by the wound
expert, in conjunction with the health professional staff, ensured
repetitive coaching in a nurturing, safe non-judgemental learn-
ing environment while incorporating the patient and family/carer
within the plan of care.
3.3. Sample
As places were limited, General Practices were invited to sub-
mit expressions of interest and were recruited if they fitted the
following inclusion criteria:
– Clinic was large enough to accommodate two or more wound
patients simultaneously
– Clinic had an interest in wound managementand support from
GPs and practice managers.
– Clinic was willing to collect patient clinical and satisfaction data
and health professional surveys
Patients were recruited if they fitted the inclusion criteria:
– Patientswith an open wound of any type or who visited the clinic
specifically for prevention of a wound
3.4. Data collectionand measures
3.4.1. Health professionals
Data were collected from March 2013 to June 2015 to gather
information before implementation of the CWC model and after
implementation of the CWC model. The health professional survey
was developed to obtain data including demographic information
(i.e.ageand gender)and qualifications (i.e.what is the highest level
of school you have completed or the highest qualification you have
received)and current wound practices(i.e.what percentageof your
work time is currently taken up with providing clinical care or pre-
ventativemanagementto patients at risk of developing wounds or
with current wounds). The survey also asked questions in relation
to evidence based practice based on the validated Self-Efficacy in
EvidenceBasedPractice scale (Chang & Crowe, 2011) and included
items on attitudes (i.e. please indicate your level of agreementor
disagreementwith the following statement: An interprofessional
collaborative approach to wound management results in better
patient outcomes), confidence levels in assessment,management
and prevention of wounds as well as transfer of learning and evi-
dence based wound managementguidelines (i.e., please rate your
confidence level to undertake the following: Finding evidence on
wound managementand clinical practice)and barriers to education
and training.
3.4.2. Patients
Data were collected from March 2013 to June 2015 and con-
tained baselineand follow up data for up to 24 weeks obtainedfrom
medical records, clinical assessment and surveys. This informa-
tion included demographic (age, gender, medical characteristics),
health (medical history, medications, nutrition), clinical charac-
teristics of any wounds (aetiology, area, tissue type, progress in
healing), managementand socioeconomic information. The Pres-
sure Ulcer Scale for Healing (PUSH) tool (National Pressure Ulcer
Advisory Panel, 2013) was used to document ulcer severity in all
wounds as this scale has demonstratedreliability and found to be
responsive in different types of leg ulcers and diabetic ulcers (Hon
et al., 2010; Ratliff & Rodeheaver,2005; Santos,Sellmer,& Massulo,
2007). The PUSH tool takes into account the area, the amount of
exudate and wound bed tissue type/surface appearanceas deter-
mined by the clinician. The PUSH scalewas scoredfrom 0 to 17 with
an increasing score indicating deterioration of a wound (National
Pressure Ulcer Advisory Panel, 2013). Self-reported survey data
were collected on health-related quality of life (SF-12 v2) (Ware
et al., 1996) and the Patient Enablement and Satisfaction Survey
(PESS)(Desborough,Banfield, & Parker, 2014).
All clinics operatedby appointment only. Patients receivededu-
cation and wound treatment, which was documented; patients
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 3
implementation of the intervention. The outcome measures
included health professionals’ knowledge, confidence and prac-
tices re evidencebased wound management,and patient outcome
measures of wound healing and prevention measures and satis-
faction with care.The health professional survey collected data on
demographics,education, clinical practice details, confidence lev-
els and barriers and limitations in assessment,managementand
prevention of wounds. Patient data collected when attending the
wound clinic at the first visit with a wound or for prevention strate-
giesincluded demographic,medical history, wound characteristics,
wound managementand prevention strategies; and then further
data (wound characteristics)were collected from patients attend-
ing the clinic at least every two weeks or until healing for open
wounds.
3.2. Procedure
Nine nurse-led CWCs were established in a variety of GP
practices which were located across three Australian states
(Queensland,Victoria and Tasmania).A local wound expert in each
state was employed to assist health professionals to consult with
patients and to provide training and coachingat each of thesesites.
The role of the expert trainer was to provide evidence-basedwound
managementtraining and coaching for general health profession-
als as well as playing an active clinical role in the clinic for the time
that they were there. The expert trainer was in most casesa Nurse
Practitioner in wound management.
The expert trainer as part of the intervention in this study was
involved in the initial training of health professionals within each
of the clinics and then attended the clinic once/fortnight to coach
and mentor staff in clinical practice.The initial training in the prac-
tice included a workshop that covered the implementation of the
model of care,wound aetiologies,wound assessment,management
and prevention principles and evidence based practice including
the need for good documentation.The need for a multidisciplinary
approach to wound care was enforced and a referral pathway was
provided to health professionalsin chart form that included details
of specialist clinics and health professionals within the area that
could offer specialist wound care advice. This workshop utilised
PowerPoint presentationsthat also included case studies and real
life scenarios. To assist with staff education, a wound education
and training material package named the CWC ResourceKit was
developed as part of the project and was made available to health
professionals and patients. The training content was also specifi-
cally directed towards GP with the necessaryincorporation of the
relevant MBS item numbers that may be relevant to wound care
practice.
This was followed up by the wound expert attending wound
care appointmentsonce/fortnight where the wound expert worked
with the health professionalstaff to treat the patientsusing a coach-
ing model of teaching. The wound expert would work with the
health professionalsto complete an assessmentof a patient with a
wound followed by the planning and implementation of evidence
based care for that patient. The health professionals were encour-
aged over time to complete all skills themselveswith the ability to
ask questions and discuss options with the wound expert. Sociali-
sation of patients and carerswas encouragedby scheduling at least
two visits at the same time and in the same room. Referral path-
ways were developedin consultation with GP health professionals
and utilised for referral on to specialists as appropriate.
Follow up attendance at clinical appointments by the wound
expert, in conjunction with the health professional staff, ensured
repetitive coaching in a nurturing, safe non-judgemental learn-
ing environment while incorporating the patient and family/carer
within the plan of care.
3.3. Sample
As places were limited, General Practices were invited to sub-
mit expressions of interest and were recruited if they fitted the
following inclusion criteria:
– Clinic was large enough to accommodate two or more wound
patients simultaneously
– Clinic had an interest in wound managementand support from
GPs and practice managers.
– Clinic was willing to collect patient clinical and satisfaction data
and health professional surveys
Patients were recruited if they fitted the inclusion criteria:
– Patientswith an open wound of any type or who visited the clinic
specifically for prevention of a wound
3.4. Data collectionand measures
3.4.1. Health professionals
Data were collected from March 2013 to June 2015 to gather
information before implementation of the CWC model and after
implementation of the CWC model. The health professional survey
was developed to obtain data including demographic information
(i.e.ageand gender)and qualifications (i.e.what is the highest level
of school you have completed or the highest qualification you have
received)and current wound practices(i.e.what percentageof your
work time is currently taken up with providing clinical care or pre-
ventativemanagementto patients at risk of developing wounds or
with current wounds). The survey also asked questions in relation
to evidence based practice based on the validated Self-Efficacy in
EvidenceBasedPractice scale (Chang & Crowe, 2011) and included
items on attitudes (i.e. please indicate your level of agreementor
disagreementwith the following statement: An interprofessional
collaborative approach to wound management results in better
patient outcomes), confidence levels in assessment,management
and prevention of wounds as well as transfer of learning and evi-
dence based wound managementguidelines (i.e., please rate your
confidence level to undertake the following: Finding evidence on
wound managementand clinical practice)and barriers to education
and training.
3.4.2. Patients
Data were collected from March 2013 to June 2015 and con-
tained baselineand follow up data for up to 24 weeks obtainedfrom
medical records, clinical assessment and surveys. This informa-
tion included demographic (age, gender, medical characteristics),
health (medical history, medications, nutrition), clinical charac-
teristics of any wounds (aetiology, area, tissue type, progress in
healing), managementand socioeconomic information. The Pres-
sure Ulcer Scale for Healing (PUSH) tool (National Pressure Ulcer
Advisory Panel, 2013) was used to document ulcer severity in all
wounds as this scale has demonstratedreliability and found to be
responsive in different types of leg ulcers and diabetic ulcers (Hon
et al., 2010; Ratliff & Rodeheaver,2005; Santos,Sellmer,& Massulo,
2007). The PUSH tool takes into account the area, the amount of
exudate and wound bed tissue type/surface appearanceas deter-
mined by the clinician. The PUSH scalewas scoredfrom 0 to 17 with
an increasing score indicating deterioration of a wound (National
Pressure Ulcer Advisory Panel, 2013). Self-reported survey data
were collected on health-related quality of life (SF-12 v2) (Ware
et al., 1996) and the Patient Enablement and Satisfaction Survey
(PESS)(Desborough,Banfield, & Parker, 2014).
All clinics operatedby appointment only. Patients receivededu-
cation and wound treatment, which was documented; patients
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
4 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
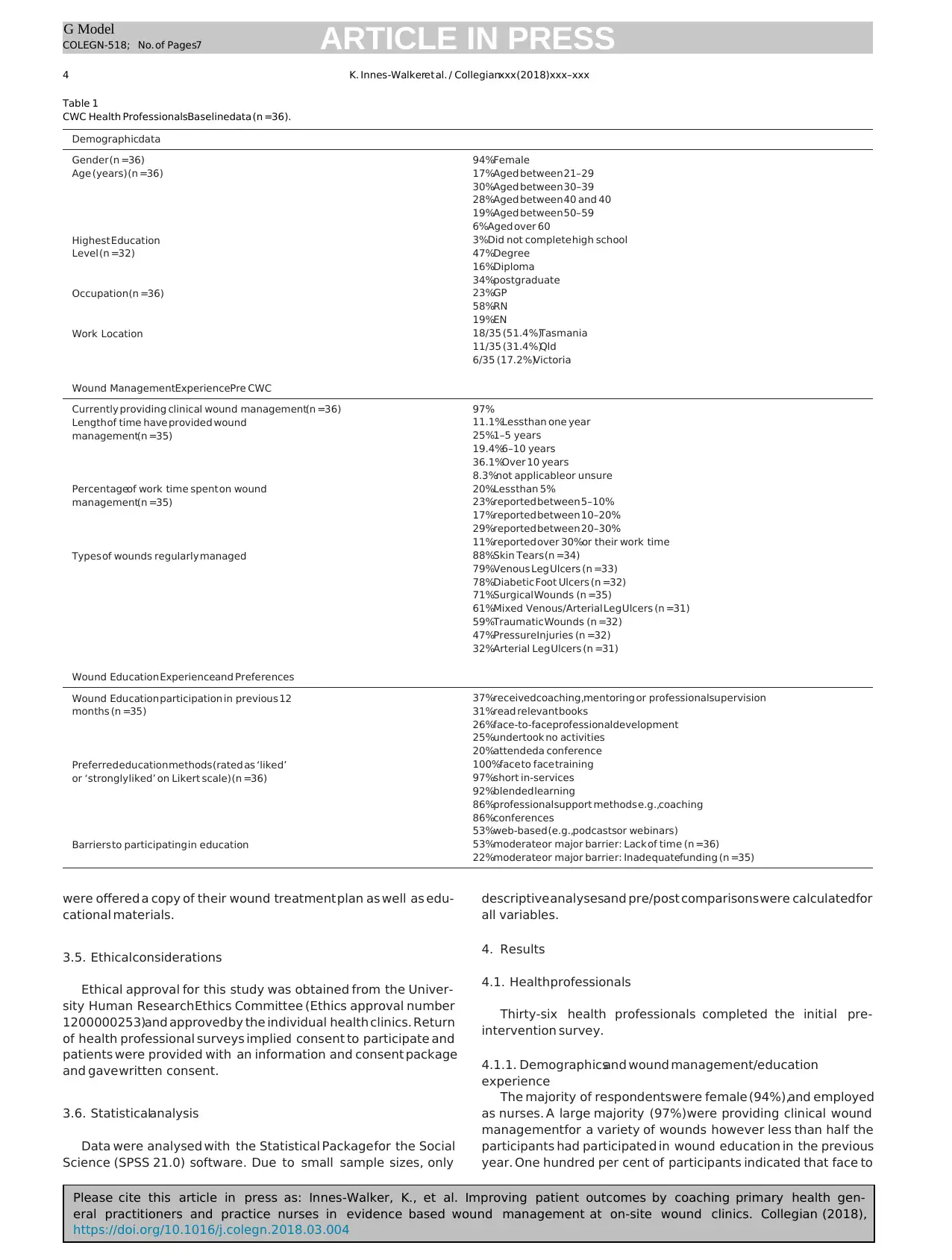
Table 1
CWC Health ProfessionalsBaselinedata (n =36).
Demographicdata
Gender (n =36) 94%Female
Age (years) (n =36) 17%Aged between 21–29
30%Aged between 30–39
28%Aged between 40 and 40
19%Aged between 50–59
6%Aged over 60
Highest Education
Level (n =32)
3%Did not complete high school
47%Degree
16%Diploma
34%postgraduate
Occupation(n =36) 23%GP
58%RN
19%EN
Work Location 18/35 (51.4%)Tasmania
11/35 (31.4%)Qld
6/35 (17.2%)Victoria
Wound ManagementExperiencePre CWC
Currently providing clinical wound management(n =36) 97%
Length of time have provided wound
management(n =35)
11.1%Lessthan one year
25%1–5 years
19.4%6–10 years
36.1%Over 10 years
8.3%not applicableor unsure
Percentageof work time spent on wound
management(n =35)
20%Lessthan 5%
23%reported between 5–10%
17%reported between 10–20%
29%reported between 20–30%
11%reported over 30%or their work time
Types of wounds regularly managed 88%Skin Tears (n =34)
79%Venous Leg Ulcers (n =33)
78%Diabetic Foot Ulcers (n =32)
71%Surgical Wounds (n =35)
61%Mixed Venous/Arterial Leg Ulcers (n =31)
59%Traumatic Wounds (n =32)
47%PressureInjuries (n =32)
32%Arterial Leg Ulcers (n =31)
Wound Education Experienceand Preferences
Wound Education participation in previous 12
months (n =35)
37%receivedcoaching,mentoring or professionalsupervision
31%read relevant books
26%face-to-faceprofessionaldevelopment
25%undertook no activities
20%attendeda conference
Preferred education methods (rated as ‘liked’
or ‘strongly liked’ on Likert scale) (n =36)
100%face to face training
97%short in-services
92%blended learning
86%professionalsupport methods e.g.,coaching
86%conferences
53%web-based (e.g.,podcastsor webinars)
Barriers to participating in education 53%moderateor major barrier: Lack of time (n =36)
22%moderateor major barrier: Inadequatefunding (n =35)
were offered a copy of their wound treatment plan as well as edu-
cational materials.
3.5. Ethicalconsiderations
Ethical approval for this study was obtained from the Univer-
sity Human Research Ethics Committee (Ethics approval number
1200000253)and approved by the individual health clinics. Return
of health professional surveys implied consent to participate and
patients were provided with an information and consent package
and gave written consent.
3.6. Statisticalanalysis
Data were analysed with the Statistical Package for the Social
Science (SPSS 21.0) software. Due to small sample sizes, only
descriptive analysesand pre/post comparisons were calculatedfor
all variables.
4. Results
4.1. Healthprofessionals
Thirty-six health professionals completed the initial pre-
intervention survey.
4.1.1. Demographicsand wound management/education
experience
The majority of respondentswere female (94%),and employed
as nurses. A large majority (97%)were providing clinical wound
managementfor a variety of wounds however less than half the
participants had participated in wound education in the previous
year. One hundred per cent of participants indicated that face to
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
4 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
Table 1
CWC Health ProfessionalsBaselinedata (n =36).
Demographicdata
Gender (n =36) 94%Female
Age (years) (n =36) 17%Aged between 21–29
30%Aged between 30–39
28%Aged between 40 and 40
19%Aged between 50–59
6%Aged over 60
Highest Education
Level (n =32)
3%Did not complete high school
47%Degree
16%Diploma
34%postgraduate
Occupation(n =36) 23%GP
58%RN
19%EN
Work Location 18/35 (51.4%)Tasmania
11/35 (31.4%)Qld
6/35 (17.2%)Victoria
Wound ManagementExperiencePre CWC
Currently providing clinical wound management(n =36) 97%
Length of time have provided wound
management(n =35)
11.1%Lessthan one year
25%1–5 years
19.4%6–10 years
36.1%Over 10 years
8.3%not applicableor unsure
Percentageof work time spent on wound
management(n =35)
20%Lessthan 5%
23%reported between 5–10%
17%reported between 10–20%
29%reported between 20–30%
11%reported over 30%or their work time
Types of wounds regularly managed 88%Skin Tears (n =34)
79%Venous Leg Ulcers (n =33)
78%Diabetic Foot Ulcers (n =32)
71%Surgical Wounds (n =35)
61%Mixed Venous/Arterial Leg Ulcers (n =31)
59%Traumatic Wounds (n =32)
47%PressureInjuries (n =32)
32%Arterial Leg Ulcers (n =31)
Wound Education Experienceand Preferences
Wound Education participation in previous 12
months (n =35)
37%receivedcoaching,mentoring or professionalsupervision
31%read relevant books
26%face-to-faceprofessionaldevelopment
25%undertook no activities
20%attendeda conference
Preferred education methods (rated as ‘liked’
or ‘strongly liked’ on Likert scale) (n =36)
100%face to face training
97%short in-services
92%blended learning
86%professionalsupport methods e.g.,coaching
86%conferences
53%web-based (e.g.,podcastsor webinars)
Barriers to participating in education 53%moderateor major barrier: Lack of time (n =36)
22%moderateor major barrier: Inadequatefunding (n =35)
were offered a copy of their wound treatment plan as well as edu-
cational materials.
3.5. Ethicalconsiderations
Ethical approval for this study was obtained from the Univer-
sity Human Research Ethics Committee (Ethics approval number
1200000253)and approved by the individual health clinics. Return
of health professional surveys implied consent to participate and
patients were provided with an information and consent package
and gave written consent.
3.6. Statisticalanalysis
Data were analysed with the Statistical Package for the Social
Science (SPSS 21.0) software. Due to small sample sizes, only
descriptive analysesand pre/post comparisons were calculatedfor
all variables.
4. Results
4.1. Healthprofessionals
Thirty-six health professionals completed the initial pre-
intervention survey.
4.1.1. Demographicsand wound management/education
experience
The majority of respondentswere female (94%),and employed
as nurses. A large majority (97%)were providing clinical wound
managementfor a variety of wounds however less than half the
participants had participated in wound education in the previous
year. One hundred per cent of participants indicated that face to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 5
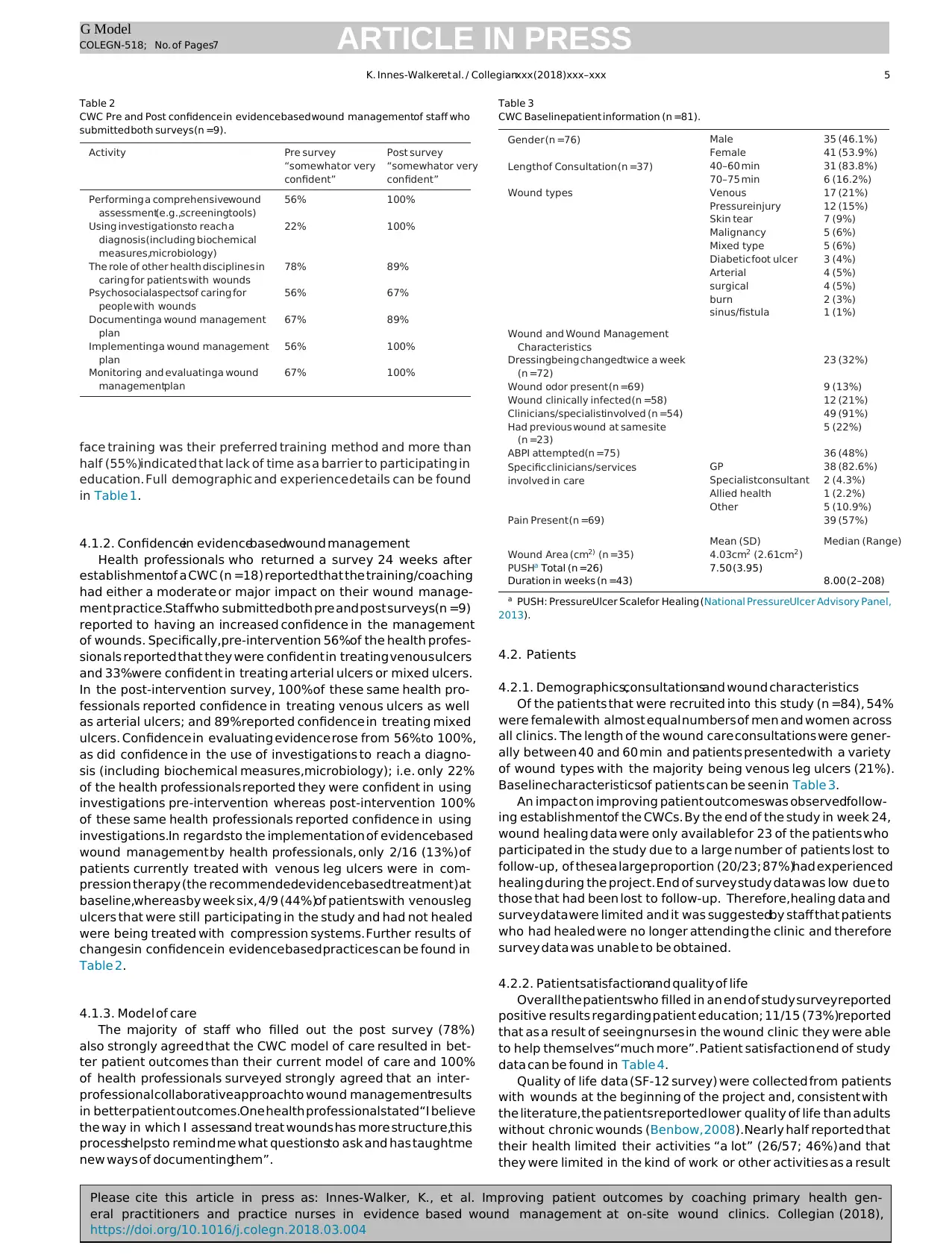
Table 2
CWC Pre and Post confidence in evidencebased wound managementof staff who
submitted both surveys(n =9).
Activity Pre survey
“somewhat or very
confident”
Post survey
“somewhat or very
confident”
Performing a comprehensivewound
assessment(e.g.,screeningtools)
56% 100%
Using investigationsto reach a
diagnosis(including biochemical
measures,microbiology)
22% 100%
The role of other health disciplines in
caring for patients with wounds
78% 89%
Psychosocialaspectsof caring for
people with wounds
56% 67%
Documentinga wound management
plan
67% 89%
Implementing a wound management
plan
56% 100%
Monitoring and evaluatinga wound
managementplan
67% 100%
face training was their preferred training method and more than
half (55%)indicated that lack of time as a barrier to participating in
education. Full demographic and experience details can be found
in Table 1.
4.1.2. Confidencein evidencebasedwound management
Health professionals who returned a survey 24 weeks after
establishmentof a CWC (n =18) reported that the training/coaching
had either a moderate or major impact on their wound manage-
ment practice.Staffwho submitted both pre and post surveys(n =9)
reported to having an increased confidence in the management
of wounds. Specifically,pre-intervention 56%of the health profes-
sionals reported that they were confident in treating venous ulcers
and 33%were confident in treating arterial ulcers or mixed ulcers.
In the post-intervention survey, 100%of these same health pro-
fessionals reported confidence in treating venous ulcers as well
as arterial ulcers; and 89%reported confidence in treating mixed
ulcers. Confidence in evaluating evidence rose from 56%to 100%,
as did confidence in the use of investigations to reach a diagno-
sis (including biochemical measures,microbiology); i.e. only 22%
of the health professionals reported they were confident in using
investigations pre-intervention whereas post-intervention 100%
of these same health professionals reported confidence in using
investigations.In regardsto the implementation of evidencebased
wound management by health professionals, only 2/16 (13%) of
patients currently treated with venous leg ulcers were in com-
pression therapy (the recommendedevidencebased treatment) at
baseline,whereasby week six, 4/9 (44%)of patientswith venousleg
ulcers that were still participating in the study and had not healed
were being treated with compression systems. Further results of
changesin confidence in evidence based practices can be found in
Table 2.
4.1.3. Model of care
The majority of staff who filled out the post survey (78%)
also strongly agreed that the CWC model of care resulted in bet-
ter patient outcomes than their current model of care and 100%
of health professionals surveyed strongly agreed that an inter-
professionalcollaborativeapproachto wound managementresults
in better patient outcomes.One health professionalstated“I believe
the way in which I assessand treat wounds has more structure,this
processhelpsto remind me what questionsto ask and has taughtme
new ways of documentingthem”.
Table 3
CWC Baselinepatient information (n =81).
Gender (n =76) Male 35 (46.1%)
Female 41 (53.9%)
Length of Consultation (n =37) 40–60 min 31 (83.8%)
70–75 min 6 (16.2%)
Wound types Venous 17 (21%)
Pressureinjury 12 (15%)
Skin tear 7 (9%)
Malignancy 5 (6%)
Mixed type 5 (6%)
Diabetic foot ulcer 3 (4%)
Arterial 4 (5%)
surgical 4 (5%)
burn 2 (3%)
sinus/fistula 1 (1%)
Wound and Wound Management
Characteristics
Dressingbeing changedtwice a week
(n =72)
23 (32%)
Wound odor present (n =69) 9 (13%)
Wound clinically infected (n =58) 12 (21%)
Clinicians/specialistinvolved (n =54) 49 (91%)
Had previous wound at same site
(n =23)
5 (22%)
ABPI attempted(n =75) 36 (48%)
Specific clinicians/services
involved in care
GP 38 (82.6%)
Specialistconsultant 2 (4.3%)
Allied health 1 (2.2%)
Other 5 (10.9%)
Pain Present (n =69) 39 (57%)
Mean (SD) Median (Range)
Wound Area (cm2) (n =35) 4.03cm2 (2.61cm2)
PUSHa Total (n =26) 7.50 (3.95)
Duration in weeks (n =43) 8.00 (2–208)
a PUSH: PressureUlcer Scalefor Healing (National PressureUlcer Advisory Panel,
2013).
4.2. Patients
4.2.1. Demographics,consultationsand wound characteristics
Of the patients that were recruited into this study (n =84), 54%
were female with almost equal numbers of men and women across
all clinics. The length of the wound care consultations were gener-
ally between 40 and 60 min and patients presented with a variety
of wound types with the majority being venous leg ulcers (21%).
Baseline characteristicsof patients can be seen in Table 3.
An impact on improving patient outcomeswas observedfollow-
ing establishmentof the CWCs. By the end of the study in week 24,
wound healing data were only available for 23 of the patients who
participated in the study due to a large number of patients lost to
follow-up, of thesea large proportion (20/23; 87%)had experienced
healing during the project. End of survey study data was low due to
those that had been lost to follow-up. Therefore,healing data and
survey data were limited and it was suggestedby staff that patients
who had healed were no longer attending the clinic and therefore
survey data was unable to be obtained.
4.2.2. Patientsatisfactionand quality of life
Overall the patientswho filled in an end of study surveyreported
positive results regarding patient education; 11/15 (73%)reported
that as a result of seeingnurses in the wound clinic they were able
to help themselves“much more”. Patient satisfaction end of study
data can be found in Table 4.
Quality of life data (SF-12 survey) were collected from patients
with wounds at the beginning of the project and, consistent with
the literature,the patients reported lower quality of life than adults
without chronic wounds (Benbow, 2008).Nearly half reported that
their health limited their activities “a lot” (26/57; 46%) and that
they were limited in the kind of work or other activities as a result
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 5
Table 2
CWC Pre and Post confidence in evidencebased wound managementof staff who
submitted both surveys(n =9).
Activity Pre survey
“somewhat or very
confident”
Post survey
“somewhat or very
confident”
Performing a comprehensivewound
assessment(e.g.,screeningtools)
56% 100%
Using investigationsto reach a
diagnosis(including biochemical
measures,microbiology)
22% 100%
The role of other health disciplines in
caring for patients with wounds
78% 89%
Psychosocialaspectsof caring for
people with wounds
56% 67%
Documentinga wound management
plan
67% 89%
Implementing a wound management
plan
56% 100%
Monitoring and evaluatinga wound
managementplan
67% 100%
face training was their preferred training method and more than
half (55%)indicated that lack of time as a barrier to participating in
education. Full demographic and experience details can be found
in Table 1.
4.1.2. Confidencein evidencebasedwound management
Health professionals who returned a survey 24 weeks after
establishmentof a CWC (n =18) reported that the training/coaching
had either a moderate or major impact on their wound manage-
ment practice.Staffwho submitted both pre and post surveys(n =9)
reported to having an increased confidence in the management
of wounds. Specifically,pre-intervention 56%of the health profes-
sionals reported that they were confident in treating venous ulcers
and 33%were confident in treating arterial ulcers or mixed ulcers.
In the post-intervention survey, 100%of these same health pro-
fessionals reported confidence in treating venous ulcers as well
as arterial ulcers; and 89%reported confidence in treating mixed
ulcers. Confidence in evaluating evidence rose from 56%to 100%,
as did confidence in the use of investigations to reach a diagno-
sis (including biochemical measures,microbiology); i.e. only 22%
of the health professionals reported they were confident in using
investigations pre-intervention whereas post-intervention 100%
of these same health professionals reported confidence in using
investigations.In regardsto the implementation of evidencebased
wound management by health professionals, only 2/16 (13%) of
patients currently treated with venous leg ulcers were in com-
pression therapy (the recommendedevidencebased treatment) at
baseline,whereasby week six, 4/9 (44%)of patientswith venousleg
ulcers that were still participating in the study and had not healed
were being treated with compression systems. Further results of
changesin confidence in evidence based practices can be found in
Table 2.
4.1.3. Model of care
The majority of staff who filled out the post survey (78%)
also strongly agreed that the CWC model of care resulted in bet-
ter patient outcomes than their current model of care and 100%
of health professionals surveyed strongly agreed that an inter-
professionalcollaborativeapproachto wound managementresults
in better patient outcomes.One health professionalstated“I believe
the way in which I assessand treat wounds has more structure,this
processhelpsto remind me what questionsto ask and has taughtme
new ways of documentingthem”.
Table 3
CWC Baselinepatient information (n =81).
Gender (n =76) Male 35 (46.1%)
Female 41 (53.9%)
Length of Consultation (n =37) 40–60 min 31 (83.8%)
70–75 min 6 (16.2%)
Wound types Venous 17 (21%)
Pressureinjury 12 (15%)
Skin tear 7 (9%)
Malignancy 5 (6%)
Mixed type 5 (6%)
Diabetic foot ulcer 3 (4%)
Arterial 4 (5%)
surgical 4 (5%)
burn 2 (3%)
sinus/fistula 1 (1%)
Wound and Wound Management
Characteristics
Dressingbeing changedtwice a week
(n =72)
23 (32%)
Wound odor present (n =69) 9 (13%)
Wound clinically infected (n =58) 12 (21%)
Clinicians/specialistinvolved (n =54) 49 (91%)
Had previous wound at same site
(n =23)
5 (22%)
ABPI attempted(n =75) 36 (48%)
Specific clinicians/services
involved in care
GP 38 (82.6%)
Specialistconsultant 2 (4.3%)
Allied health 1 (2.2%)
Other 5 (10.9%)
Pain Present (n =69) 39 (57%)
Mean (SD) Median (Range)
Wound Area (cm2) (n =35) 4.03cm2 (2.61cm2)
PUSHa Total (n =26) 7.50 (3.95)
Duration in weeks (n =43) 8.00 (2–208)
a PUSH: PressureUlcer Scalefor Healing (National PressureUlcer Advisory Panel,
2013).
4.2. Patients
4.2.1. Demographics,consultationsand wound characteristics
Of the patients that were recruited into this study (n =84), 54%
were female with almost equal numbers of men and women across
all clinics. The length of the wound care consultations were gener-
ally between 40 and 60 min and patients presented with a variety
of wound types with the majority being venous leg ulcers (21%).
Baseline characteristicsof patients can be seen in Table 3.
An impact on improving patient outcomeswas observedfollow-
ing establishmentof the CWCs. By the end of the study in week 24,
wound healing data were only available for 23 of the patients who
participated in the study due to a large number of patients lost to
follow-up, of thesea large proportion (20/23; 87%)had experienced
healing during the project. End of survey study data was low due to
those that had been lost to follow-up. Therefore,healing data and
survey data were limited and it was suggestedby staff that patients
who had healed were no longer attending the clinic and therefore
survey data was unable to be obtained.
4.2.2. Patientsatisfactionand quality of life
Overall the patientswho filled in an end of study surveyreported
positive results regarding patient education; 11/15 (73%)reported
that as a result of seeingnurses in the wound clinic they were able
to help themselves“much more”. Patient satisfaction end of study
data can be found in Table 4.
Quality of life data (SF-12 survey) were collected from patients
with wounds at the beginning of the project and, consistent with
the literature,the patients reported lower quality of life than adults
without chronic wounds (Benbow, 2008).Nearly half reported that
their health limited their activities “a lot” (26/57; 46%) and that
they were limited in the kind of work or other activities as a result

Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
6 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
Table 4
CWC Patient End of study survey Data (Week 24).
Percent that “strongly agreed”
Patient reported that the treatmentsthey receivedwere of high quality 93%(n =15)
Patient reported that the decisionsregardingtheir health care were of high quality 87%(n =15)
Patient reported that overall they were satisfied with their wound care 87%(n =15)
Patient reported that the wound care they receivedfrom the nurse/s was of high quality 87%(n =15)
Patient reported they felt much more able to help themselvesas a result of seeingthe nurses 73%(n =15)
Patient’sulcer had healed by week 24 the end of the study 87%(n =23)
of their physical health 24/55 (43%).Quality of life data at the end
of the intervention period was collected and returned from a lim-
ited number of patients (n =5), however, within this group of 5
patients, there was a notable improvement in the overall health-
related Quality of Life score from a mean of 37.2 (SD 13.9) at the
beginning of the project, up to 47.3 (SD 9.7) after 24 weeks (total
scalefrom 0 to 100). In this small group at the end of the study only
one patient of the five reported their health limited their activities.
5. Discussion
GP settings are a central point of access for patients into the
health caresystem(Yelland, 2014) and health professionalsin these
settings are well placed to make a difference in the area of wound
care.Having specialistNurse Practitioners as leaderswithin wound
management are key to empowering and nurturing the skill set
capabilitiesfor health professionals.Support and guidancefor prac-
tice health professionals’ decision making processes, gains their
confidence through repetitive learning and coaching, this enables
autonomy, continuity in care and overall improvement in both
nurses and patient’s decision for optimal evidence based wound
care outcomes. This project has been able to provide evidence on
the different types of wounds cared for at GPs and a model to
educate health professionals and patients about evidence based
practice in wound management using a training and modelling
(coaching) model to facilitate research translation in the GP set-
ting. This model has been effective in being able to increasehealth
professionals’confidencein the assessment,managementand pre-
vention of a variety of wounds while also being able to facilitate
uptake of evidence based,best practice within the primary health
caresettingas required.The baselinedata supportedprevious stud-
ies (Edwards et al., 2013,2014) in that evidencebasedpracticesare
often not performed in general practice and has shown increased
rates of evidencebased practice post study.
6. Limitations
The participant and clinicians’ commitment to this project may
have influenced results, possibly indicating bias. There was sig-
nificant missing documentation in relation to follow up data on
patients and health professionals.The time that health profession-
als had with patients was often not considered adequategiven the
complexities of the patients referred i.e. medical history, language
barriers,if there were multiple wounds present,and lack of practice
nurse item numbers and remuneration limited what could reason-
ably be done. The GP setting is always very busy and finding the
time to ensure accuratedocumentation was often a challenge.
Referral pathways were developed specific for each area how-
ever in some cases,ensuring health professionalsfollowed this was
a challenge.A barrier to uptake of best practicewas the cost of some
treatments,where some treatmentswere not an affordable option
for the patient to purchase.One of the original aims of the project,
to increasesocialisation for patients,was difficult to managein the
general practice setting; as even when a treatment room was allo-
cated for a wound care clinic, emergencyadmissions often needed
to be accommodatedand therefore only one patient could be seen
at a time.
Although we note that an increase in staff confidence in this
study appears to have been accompanied by improved patient
outcomes, it is important to note that an increase in practitioner
confidence does always correlate with an increase in evidence
based practices (Flanagan,2005) or in wound healing. Education
has limited value if it is not sustained and applied to practice
(Flanagan,2005) in an appropriateway. This project shows encour-
aging results in regard to increasing confidence levels of health
practitioners as well as an increase in some evidence based prac-
tices. Further examination of other evidence-based practices is
necessaryand long term investigation of sustainability of this con-
fidence and use of evidence based practices would be beneficial.
7. Conclusion
The establishment of CWCs led to improved patient outcomes
by enhancing the capabilities of health professionals in primary
health care settingsto implement evidencebasedwound manage-
ment. Further uptake and evaluation of this model could benefit
patients in the community by facilitating the implementation of
evidence based wound care leading to improved health outcomes
and ultimately decreasingthe costs to the patients and the health
care system.The use of wound experts,mainly Nurse Practitioners
in wound care, was essential to this process and the use of Nurse
Practitioners in GP requires further exploration of the benefits to
practice and patient outcomes.
Funding statement
This study was supported by the Wound Management Inno-
vation CRC (established and supported under the Australian
Government’sCooperativeResearchCentresProgram).
Conflict of interest
No conflict of interest has been declared by the authors.
Acknowledgements
The authors would like to acknowledge the support of the Aus-
tralian Government’sCooperative ResearchCentres Program. The
authors would like to acknowledge and thank all the staff and par-
ticipants who were involved in contributing to the study. Namely,
South West Melbourne Medical Local (SWMML), Victoria; North-
ern Melbourne Medicare Local (NMML), Victoria; WestgateHealth
Co-op, Victoria; RosannaMedical Group, Victoria; Viewbank Med-
ical Group, Victoria; Tasmania Medicare Local (TML); Bellerive
Medical Centre,Tasmania; The Lindisfarne Clinic, Tasmania; Sandy
Bay Medical Centre, Tasmania; Lauderdale Doctors Surgery, Tas-
mania; Greater Brisbane Metro South Medicare Local (GBMSML),
Queensland; Calamvale Medical Centre, Queensland and Garden
City Medical Centre,Queensland.
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
6 K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx
Table 4
CWC Patient End of study survey Data (Week 24).
Percent that “strongly agreed”
Patient reported that the treatmentsthey receivedwere of high quality 93%(n =15)
Patient reported that the decisionsregardingtheir health care were of high quality 87%(n =15)
Patient reported that overall they were satisfied with their wound care 87%(n =15)
Patient reported that the wound care they receivedfrom the nurse/s was of high quality 87%(n =15)
Patient reported they felt much more able to help themselvesas a result of seeingthe nurses 73%(n =15)
Patient’sulcer had healed by week 24 the end of the study 87%(n =23)
of their physical health 24/55 (43%).Quality of life data at the end
of the intervention period was collected and returned from a lim-
ited number of patients (n =5), however, within this group of 5
patients, there was a notable improvement in the overall health-
related Quality of Life score from a mean of 37.2 (SD 13.9) at the
beginning of the project, up to 47.3 (SD 9.7) after 24 weeks (total
scalefrom 0 to 100). In this small group at the end of the study only
one patient of the five reported their health limited their activities.
5. Discussion
GP settings are a central point of access for patients into the
health caresystem(Yelland, 2014) and health professionalsin these
settings are well placed to make a difference in the area of wound
care.Having specialistNurse Practitioners as leaderswithin wound
management are key to empowering and nurturing the skill set
capabilitiesfor health professionals.Support and guidancefor prac-
tice health professionals’ decision making processes, gains their
confidence through repetitive learning and coaching, this enables
autonomy, continuity in care and overall improvement in both
nurses and patient’s decision for optimal evidence based wound
care outcomes. This project has been able to provide evidence on
the different types of wounds cared for at GPs and a model to
educate health professionals and patients about evidence based
practice in wound management using a training and modelling
(coaching) model to facilitate research translation in the GP set-
ting. This model has been effective in being able to increasehealth
professionals’confidencein the assessment,managementand pre-
vention of a variety of wounds while also being able to facilitate
uptake of evidence based,best practice within the primary health
caresettingas required.The baselinedata supportedprevious stud-
ies (Edwards et al., 2013,2014) in that evidencebasedpracticesare
often not performed in general practice and has shown increased
rates of evidencebased practice post study.
6. Limitations
The participant and clinicians’ commitment to this project may
have influenced results, possibly indicating bias. There was sig-
nificant missing documentation in relation to follow up data on
patients and health professionals.The time that health profession-
als had with patients was often not considered adequategiven the
complexities of the patients referred i.e. medical history, language
barriers,if there were multiple wounds present,and lack of practice
nurse item numbers and remuneration limited what could reason-
ably be done. The GP setting is always very busy and finding the
time to ensure accuratedocumentation was often a challenge.
Referral pathways were developed specific for each area how-
ever in some cases,ensuring health professionalsfollowed this was
a challenge.A barrier to uptake of best practicewas the cost of some
treatments,where some treatmentswere not an affordable option
for the patient to purchase.One of the original aims of the project,
to increasesocialisation for patients,was difficult to managein the
general practice setting; as even when a treatment room was allo-
cated for a wound care clinic, emergencyadmissions often needed
to be accommodatedand therefore only one patient could be seen
at a time.
Although we note that an increase in staff confidence in this
study appears to have been accompanied by improved patient
outcomes, it is important to note that an increase in practitioner
confidence does always correlate with an increase in evidence
based practices (Flanagan,2005) or in wound healing. Education
has limited value if it is not sustained and applied to practice
(Flanagan,2005) in an appropriateway. This project shows encour-
aging results in regard to increasing confidence levels of health
practitioners as well as an increase in some evidence based prac-
tices. Further examination of other evidence-based practices is
necessaryand long term investigation of sustainability of this con-
fidence and use of evidence based practices would be beneficial.
7. Conclusion
The establishment of CWCs led to improved patient outcomes
by enhancing the capabilities of health professionals in primary
health care settingsto implement evidencebasedwound manage-
ment. Further uptake and evaluation of this model could benefit
patients in the community by facilitating the implementation of
evidence based wound care leading to improved health outcomes
and ultimately decreasingthe costs to the patients and the health
care system.The use of wound experts,mainly Nurse Practitioners
in wound care, was essential to this process and the use of Nurse
Practitioners in GP requires further exploration of the benefits to
practice and patient outcomes.
Funding statement
This study was supported by the Wound Management Inno-
vation CRC (established and supported under the Australian
Government’sCooperativeResearchCentresProgram).
Conflict of interest
No conflict of interest has been declared by the authors.
Acknowledgements
The authors would like to acknowledge the support of the Aus-
tralian Government’sCooperative ResearchCentres Program. The
authors would like to acknowledge and thank all the staff and par-
ticipants who were involved in contributing to the study. Namely,
South West Melbourne Medical Local (SWMML), Victoria; North-
ern Melbourne Medicare Local (NMML), Victoria; WestgateHealth
Co-op, Victoria; RosannaMedical Group, Victoria; Viewbank Med-
ical Group, Victoria; Tasmania Medicare Local (TML); Bellerive
Medical Centre,Tasmania; The Lindisfarne Clinic, Tasmania; Sandy
Bay Medical Centre, Tasmania; Lauderdale Doctors Surgery, Tas-
mania; Greater Brisbane Metro South Medicare Local (GBMSML),
Queensland; Calamvale Medical Centre, Queensland and Garden
City Medical Centre,Queensland.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Please cite this article in press as: Innes-Walker, K., et al. Improving patient outcomes by coaching primary health gen-
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 7
References
Australian Medicare Local Alliance. (2012).GeneralPracticeNurseNational Survey
Report.
Benbow, M. (2008).Exploring wound managementand measuringquality of life.
Journal of CommunityNursing,22(6) http://dx.doi.org/10.1186/1477-7525-5-
44, 14–14,16,18
Briggs,M., & Closs,S. (2003).The prevalenceof leg ulceration: A review of the
literature. EWMA Journal,3(2), 14–20.
Britt, H., Miller, G. C., Henderson,J., Charles,J., Valenti, L., Harrison, C., & Pan, Y.
(2012).General practice activity in Australia 2011–12 (Family Medicine
ResearchCentre,Trans.).In Generalpracticeseries.Sydney: SydneyUniversity.
Chang,A. M., & Crowe, L. (2011).Validation of scalesmeasuringself-efficacyand
outcome expectancyin evidence-basedpractice.Worldviewson Evidence-Based
Nursing,8(2), 106–115. http://dx.doi.org/10.1111/j.1741-6787.2011.00215.x
Coyer,F., Edwards, H., & Finlayson, K. (2005).Bestpracticecommunitycarefor
clientswith chronicvenousleg ulcers:National Institutefor Clinical Studies(NICS)
reportfor phase1 evidenceuptakenetwork.Brisbane: QueenslandUniversity of
Technology.
Desborough,J., Banfield, M., & Parker, R. (2014).A tool to evaluatepatients’
experiencesof nursing care in Australian generalpractice: Developmentof the
patient enablementand satisfactionsurvey.AustralianJournal of Primary
Health,20(2),209–215. http://dx.doi.org/10.1071/PY12121
Edwards, H., Courtney,M., Finlayson, K., Shuter,P., & Lindsay,E. (2009).A
randomised controlled trial of a community nursing intervention: Improved
quality of life and healing for clients with chronic leg ulcers.Journal of Clinical
Nursing,18(11),1541–1549.http://dx.doi.org/10.1111/j.1365-2702.2008.
02648.x
Edwards, H., Finlayson, K., Courtney,M., Graves,N., Gibb, M., & Parker, C. (2013).
Health service pathways for patients with chronic leg ulcers: Identifying
effectivepathways for facilitation of evidencebasedwound care.BMC Health
ServicesResearch,13(1),86.
Edwards, H., Finlayson, K., Maresco-Pennisi,D., Gibb, M., Parker, C.,& Graves,N.
(2014).The long and winding road: Health servicesfor clients with chronic leg
ulcers in the community. Wound Practice& Research:Journal of the Australian
Wound ManagementAssociation,22(4),226–233.
Faithfull-Byrne, A., Thompson,L., Schafer,K. W., Elks, M., Jaspers,J., Welch, A., &
Moss, C. (2016).Clinical coachesin nursing and midwifery practice:
Facilitating point of care workplace learning and development.Collegian,24(4),
403. http://dx.doi.org/10.1016/j.colegn.2016.06.001
Flanagan,M. (2005).Barriers to the implementationof best practice in wound care.
WoundsUK, 1(3), 74–82.
Graves,N., Finlayson,K., Gibb, M., O’Reilly,M., & Edwards, H. (2014).Modelling the
economic benefitsof gold standard care for chronic wounds in a community
setting.Wound Practice& Research:Journal of the AustralianWound
ManagementAssociation,22(3),163–168.
Hon, J., Lagden,K., McLaren, A. M., O’Sullivan,D., Orr, L., Houghton, P. E., &
Woodbury, M. G. (2010).A prospective,multicenter study to validate use of
the PUSH in patients with diabetic,venous,and pressureulcers.OstomyWound
Management,56(2),26–36.
Innes-Walker, K., & Edwards, H. (2013).A wound managementeducation and
training needsanalysis of health consumersand the relevant health workforce
and stocktakeof availableeducation and training activities and resources.
Wound Practice& Research:Journal of the AustralianWound Management
Association,21(3),104–109.
Johnson, M., Hamilton, M., Delaney,B., & Pennington,N. (2011).Developmentof
team skills in novice nurses through an athletic coachingmodel. Teachingand
Learningin Nursing,6(4),185–189.http://dx.doi.org/10.1016/j.teln.2011.05.005
Johnston, C. C.,Gagnon,A., Rennick,J., Rosmus,C., Patenaude,H., Ellis, J., & Byron, J.
(2007).One-on-one coaching to improve pain assessmentand management
practicesof pediatric nurses.Journal of PediatricNursing,22(6),467–478.
http://dx.doi.org/10.1016/j.pedn.2007.07.004
Jolly, R. (2007).Practicenursingin Australia.Parliament of Australia.
Jones, J., Barr, W., Robinson,J., & Carlisle,C. (2006).Depressionin patients with
chronic venous ulceration. British Journal of Nursing,15(11),S17–S23.
Lindsay,E. (2004).The Lindsay Leg Club®
Model: A model for evidence-basedleg
ulcer management.British Journal of CommunityNursing,9, 17–22.
Margolis, D. J., Bilker, W., Santanna,J., & Baumgarten,M. (2002).Venous leg ulcer:
Incidenceand prevalencein the elderly. Journal Of TheAmericanAcademyOf
Dermatology,46(3),381–386.
National PressureUlcer Advisory Panel. (2013).Educationaland clinical
resources—PUSHtool. Retrieved5th June, 2013, 2013,from. http://
wwwnpuaporg/wp-content/uploads/2012/03/push3pdf
Parker, K. (2012).Psychosocialeffectsof living with a leg ulcer. NursingStandard,
26(45),52.
RDNS.(2008).Royal districtnursingserviceannual report2008.
Ratliff, C. R., & Rodeheaver,G. T. (2005).Use of the PUSH tool to measurevenous
ulcer healing.OstomyWound Management,51(5),58.
Santos,V. L. C.,Sellmer,D., & Massulo, M. M. E. (2007).Inter rater reliability of
PressureUlcer Scalefor Healing (PUSH) in patients with chronic leg ulcers.
RevistaLatino-Americanade Enfermagem,15(3),391–396.
The Australian Wound ManagementAssociation Inc, & The New ZealandWound
Care SocietyInc (Eds.).(2011).Australianand New Zealandclinical practice
guidelinefor preventionand managementof venousleg ulcers.Cambridge
Publishing.
Ware, J., Jr., Kosinski, M., & Keller, S. D. (1996).A 12-Item Short-Form Health
Survey: Construction of scalesand preliminary tests of reliability and validity.
MedicalCare,34(3),220–233.
Yelland, S. (2014).General practice and primary care: Making a differenceat the
coalfaceof wound managementin Australia. Wound Practice& Research,22(2),
104–107.
Young, A., & McNaught, C.-E. (2011).The physiology of wound healing.Surgery
(Oxford),29(10),475–479. http://dx.doi.org/10.1016/j.mpsur.2011.06.011
eral practitioners and practice nurses in evidence based wound management at on-site wound clinics. Collegian (2018),
https://doi.org/10.1016/j.colegn.2018.03.004
ARTICLE IN PRESSG Model
COLEGN-518; No. of Pages7
K. Innes-Walkeret al. / Collegianxxx (2018)xxx–xxx 7
References
Australian Medicare Local Alliance. (2012).GeneralPracticeNurseNational Survey
Report.
Benbow, M. (2008).Exploring wound managementand measuringquality of life.
Journal of CommunityNursing,22(6) http://dx.doi.org/10.1186/1477-7525-5-
44, 14–14,16,18
Briggs,M., & Closs,S. (2003).The prevalenceof leg ulceration: A review of the
literature. EWMA Journal,3(2), 14–20.
Britt, H., Miller, G. C., Henderson,J., Charles,J., Valenti, L., Harrison, C., & Pan, Y.
(2012).General practice activity in Australia 2011–12 (Family Medicine
ResearchCentre,Trans.).In Generalpracticeseries.Sydney: SydneyUniversity.
Chang,A. M., & Crowe, L. (2011).Validation of scalesmeasuringself-efficacyand
outcome expectancyin evidence-basedpractice.Worldviewson Evidence-Based
Nursing,8(2), 106–115. http://dx.doi.org/10.1111/j.1741-6787.2011.00215.x
Coyer,F., Edwards, H., & Finlayson, K. (2005).Bestpracticecommunitycarefor
clientswith chronicvenousleg ulcers:National Institutefor Clinical Studies(NICS)
reportfor phase1 evidenceuptakenetwork.Brisbane: QueenslandUniversity of
Technology.
Desborough,J., Banfield, M., & Parker, R. (2014).A tool to evaluatepatients’
experiencesof nursing care in Australian generalpractice: Developmentof the
patient enablementand satisfactionsurvey.AustralianJournal of Primary
Health,20(2),209–215. http://dx.doi.org/10.1071/PY12121
Edwards, H., Courtney,M., Finlayson, K., Shuter,P., & Lindsay,E. (2009).A
randomised controlled trial of a community nursing intervention: Improved
quality of life and healing for clients with chronic leg ulcers.Journal of Clinical
Nursing,18(11),1541–1549.http://dx.doi.org/10.1111/j.1365-2702.2008.
02648.x
Edwards, H., Finlayson, K., Courtney,M., Graves,N., Gibb, M., & Parker, C. (2013).
Health service pathways for patients with chronic leg ulcers: Identifying
effectivepathways for facilitation of evidencebasedwound care.BMC Health
ServicesResearch,13(1),86.
Edwards, H., Finlayson, K., Maresco-Pennisi,D., Gibb, M., Parker, C.,& Graves,N.
(2014).The long and winding road: Health servicesfor clients with chronic leg
ulcers in the community. Wound Practice& Research:Journal of the Australian
Wound ManagementAssociation,22(4),226–233.
Faithfull-Byrne, A., Thompson,L., Schafer,K. W., Elks, M., Jaspers,J., Welch, A., &
Moss, C. (2016).Clinical coachesin nursing and midwifery practice:
Facilitating point of care workplace learning and development.Collegian,24(4),
403. http://dx.doi.org/10.1016/j.colegn.2016.06.001
Flanagan,M. (2005).Barriers to the implementationof best practice in wound care.
WoundsUK, 1(3), 74–82.
Graves,N., Finlayson,K., Gibb, M., O’Reilly,M., & Edwards, H. (2014).Modelling the
economic benefitsof gold standard care for chronic wounds in a community
setting.Wound Practice& Research:Journal of the AustralianWound
ManagementAssociation,22(3),163–168.
Hon, J., Lagden,K., McLaren, A. M., O’Sullivan,D., Orr, L., Houghton, P. E., &
Woodbury, M. G. (2010).A prospective,multicenter study to validate use of
the PUSH in patients with diabetic,venous,and pressureulcers.OstomyWound
Management,56(2),26–36.
Innes-Walker, K., & Edwards, H. (2013).A wound managementeducation and
training needsanalysis of health consumersand the relevant health workforce
and stocktakeof availableeducation and training activities and resources.
Wound Practice& Research:Journal of the AustralianWound Management
Association,21(3),104–109.
Johnson, M., Hamilton, M., Delaney,B., & Pennington,N. (2011).Developmentof
team skills in novice nurses through an athletic coachingmodel. Teachingand
Learningin Nursing,6(4),185–189.http://dx.doi.org/10.1016/j.teln.2011.05.005
Johnston, C. C.,Gagnon,A., Rennick,J., Rosmus,C., Patenaude,H., Ellis, J., & Byron, J.
(2007).One-on-one coaching to improve pain assessmentand management
practicesof pediatric nurses.Journal of PediatricNursing,22(6),467–478.
http://dx.doi.org/10.1016/j.pedn.2007.07.004
Jolly, R. (2007).Practicenursingin Australia.Parliament of Australia.
Jones, J., Barr, W., Robinson,J., & Carlisle,C. (2006).Depressionin patients with
chronic venous ulceration. British Journal of Nursing,15(11),S17–S23.
Lindsay,E. (2004).The Lindsay Leg Club®
Model: A model for evidence-basedleg
ulcer management.British Journal of CommunityNursing,9, 17–22.
Margolis, D. J., Bilker, W., Santanna,J., & Baumgarten,M. (2002).Venous leg ulcer:
Incidenceand prevalencein the elderly. Journal Of TheAmericanAcademyOf
Dermatology,46(3),381–386.
National PressureUlcer Advisory Panel. (2013).Educationaland clinical
resources—PUSHtool. Retrieved5th June, 2013, 2013,from. http://
wwwnpuaporg/wp-content/uploads/2012/03/push3pdf
Parker, K. (2012).Psychosocialeffectsof living with a leg ulcer. NursingStandard,
26(45),52.
RDNS.(2008).Royal districtnursingserviceannual report2008.
Ratliff, C. R., & Rodeheaver,G. T. (2005).Use of the PUSH tool to measurevenous
ulcer healing.OstomyWound Management,51(5),58.
Santos,V. L. C.,Sellmer,D., & Massulo, M. M. E. (2007).Inter rater reliability of
PressureUlcer Scalefor Healing (PUSH) in patients with chronic leg ulcers.
RevistaLatino-Americanade Enfermagem,15(3),391–396.
The Australian Wound ManagementAssociation Inc, & The New ZealandWound
Care SocietyInc (Eds.).(2011).Australianand New Zealandclinical practice
guidelinefor preventionand managementof venousleg ulcers.Cambridge
Publishing.
Ware, J., Jr., Kosinski, M., & Keller, S. D. (1996).A 12-Item Short-Form Health
Survey: Construction of scalesand preliminary tests of reliability and validity.
MedicalCare,34(3),220–233.
Yelland, S. (2014).General practice and primary care: Making a differenceat the
coalfaceof wound managementin Australia. Wound Practice& Research,22(2),
104–107.
Young, A., & McNaught, C.-E. (2011).The physiology of wound healing.Surgery
(Oxford),29(10),475–479. http://dx.doi.org/10.1016/j.mpsur.2011.06.011
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




