A Case Study on the Intervention and Management of COPD
VerifiedAdded on 2023/06/15
|15
|3611
|188
Case Study
AI Summary
This case study provides a detailed analysis of the intervention and management strategies for Chronic Obstructive Pulmonary Disease (COPD), focusing on a patient named Robert, a long-time smoker. It delves into the pathophysiology of COPD, differentiating between emphysema and bronchitis, and highlights the impact of smoking and age on disease progression. The study examines the exacerbation of COPD, emphasizing the role of bacterial infections and environmental factors, and discusses the pathophysiology of pneumonia, distinguishing between community-acquired and hospital-acquired types. Furthermore, it explores the pharmacology of administered medications such as Salbutamol, Budesonide/efomoterol fumarate dehydrate (Symbicort), Tiotropium, Amoxicillin, Ceftriaxone, and Levoflaxone, detailing their mechanisms of action, contraindications, and nursing considerations. The case study also touches on the importance of psychosocial interventions for COPD patients. The rationale behind the doctor's decision to replace Symbicort with Tiotropium, considering the patient's pneumonia and potential adverse effects, is also discussed.

Running head: INTERVENTION AND MANAGEMENT OF COPD
Intervention and management of COPD.
Name of the student:
Name of the university:
Author note:
Intervention and management of COPD.
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
INTERVENTION AND MANAGEMENT OF COPD
Table of Contents
Introduction: 2
Pathophysiology: 2
Pathophysiology of COPD: 2
Exacerbation of the COPD: 3
Pathophysiology of pneumonia: 4
Pharmacology of the medications administered: 5
Salbutamol: 5
Budesonide/efomoterol fumarate dehydrate (symbicort): 6
Tiotropium: 7
Amoxicillin: 8
Ceftriaxone: 8
Levoflaxone: 9
Psychosocial interventions for COPD: 9
Conclusion: 10
References 11
INTERVENTION AND MANAGEMENT OF COPD
Table of Contents
Introduction: 2
Pathophysiology: 2
Pathophysiology of COPD: 2
Exacerbation of the COPD: 3
Pathophysiology of pneumonia: 4
Pharmacology of the medications administered: 5
Salbutamol: 5
Budesonide/efomoterol fumarate dehydrate (symbicort): 6
Tiotropium: 7
Amoxicillin: 8
Ceftriaxone: 8
Levoflaxone: 9
Psychosocial interventions for COPD: 9
Conclusion: 10
References 11
2
INTERVENTION AND MANAGEMENT OF COPD
Pathophysiology:
Pathophysiology of COPD:
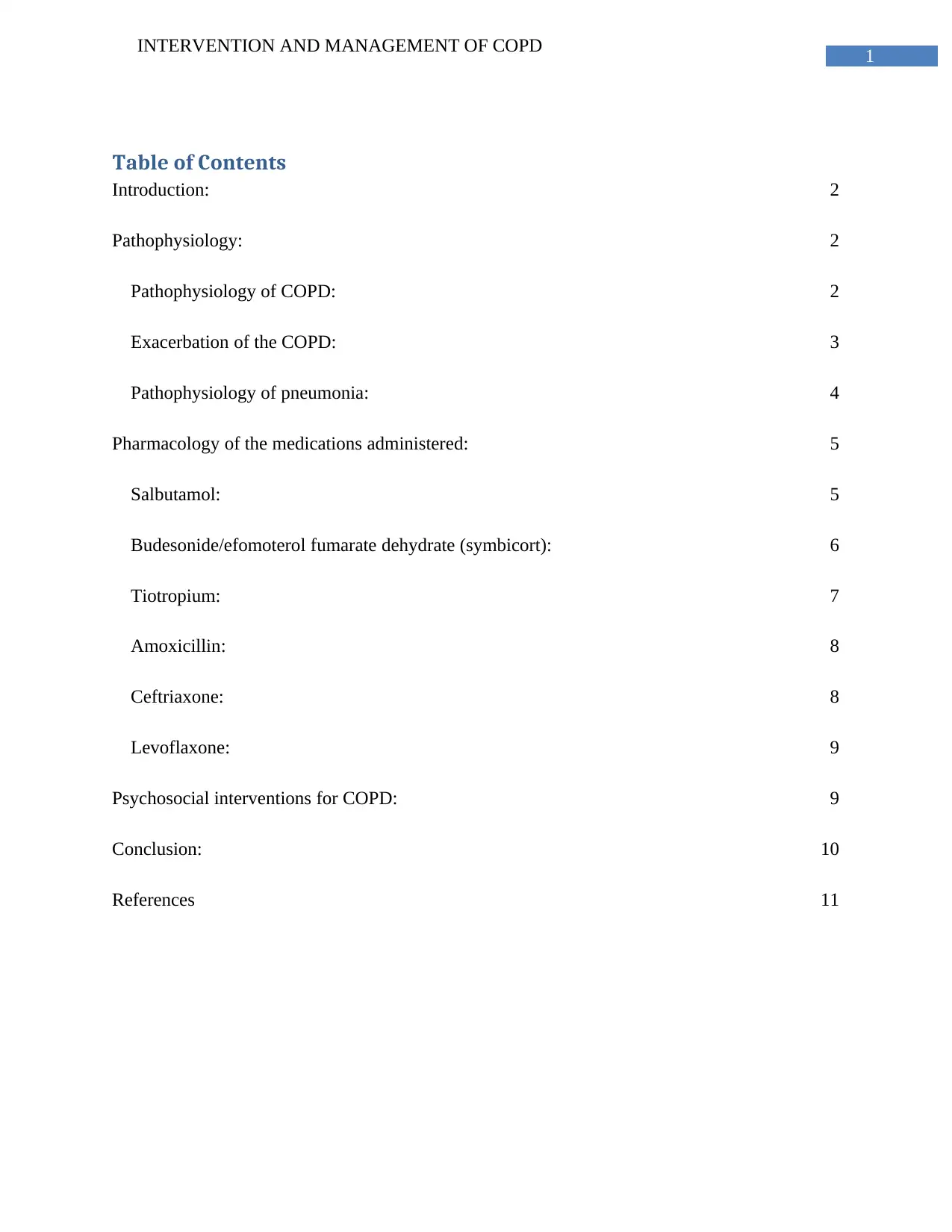
Pathophysiology can be defined by the detailed exploration and analysis of the
physiological processes and mechanisms that aid in development of the disease condition. COPD
can be defined as a chronic obstructive pulmonary disorder, and is a life-threatening respiratory
disease. The pathophysiological manifestation of the disease generally begins with affecting the
airways and air sacs of the patient, restricting smooth breathing process of the patient. It has to
be mentioned that COPD is an umbrella term, and it encompasses two key respiratory disorders,
chronic bronchitis and emphysema. During inhalation the air moves through the trachea through
2 tubes called bronchi, and these tubes branch out into smaller tubes called bronchioles, which
further diverge into small air sacs called alveoli. Emphysema can be categorized as an alveolar
disease, which mainly affects the walls of the alveoli. The damage to the wall fiber of the alveoli
that leads to lack of elasticity in the wall fiber and it effect stability of the patient of exhaling
(Albert et al., 2011).
Pathophysiology of COPD and correlation with smoking (Vogelmeier et al., 2011)
INTERVENTION AND MANAGEMENT OF COPD
Pathophysiology:
Pathophysiology of COPD:
Pathophysiology can be defined by the detailed exploration and analysis of the
physiological processes and mechanisms that aid in development of the disease condition. COPD
can be defined as a chronic obstructive pulmonary disorder, and is a life-threatening respiratory
disease. The pathophysiological manifestation of the disease generally begins with affecting the
airways and air sacs of the patient, restricting smooth breathing process of the patient. It has to
be mentioned that COPD is an umbrella term, and it encompasses two key respiratory disorders,
chronic bronchitis and emphysema. During inhalation the air moves through the trachea through
2 tubes called bronchi, and these tubes branch out into smaller tubes called bronchioles, which
further diverge into small air sacs called alveoli. Emphysema can be categorized as an alveolar
disease, which mainly affects the walls of the alveoli. The damage to the wall fiber of the alveoli
that leads to lack of elasticity in the wall fiber and it effect stability of the patient of exhaling
(Albert et al., 2011).
Pathophysiology of COPD and correlation with smoking (Vogelmeier et al., 2011)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
INTERVENTION AND MANAGEMENT OF COPD
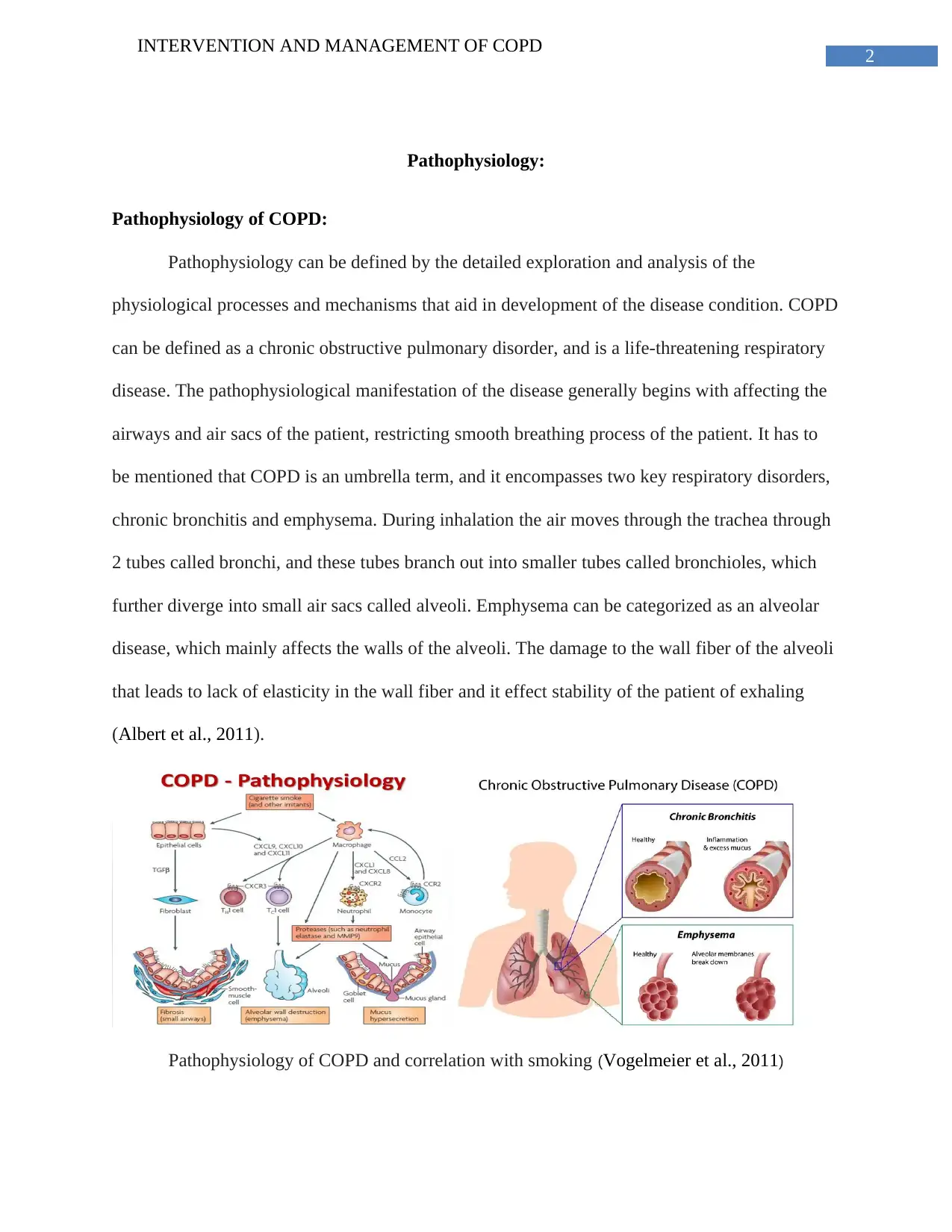
Bronchitis on the other hand is developed due to the inflammation of the bronchial tubes
accompanied by the over secretion of mucus. The over secretion of mucus eventually leads to
blocking of the airways and contribute to difficult air passage during the process of respiration. It
has to be understood that smoking is a very important contributing factor that has a profound role
in the pathophysiologic development of this respiratory disorder. For the case study, Robert, the
patient under consideration had been a chain-smoker for 40 years, smoking can be considered as
the origin of the disease he had developed. According to the case study, Robert had been
diagnosed with COPD 18 months ago and had been feeling unwell for months befire that as well.
Hence, it can be concluded that the onset of manifestations brnchitics and emphysema had begun
since a long time. The added burden of smoking excessively had contributed effectively to
further deteriorating the disease, along with the age factor of the patient in the case study.
COPD pathway (Vogelmeier et al., 2011) impact of age on COPD (Erb-Downward et al., 2011)
Exacerbation of the COPD:
An exacerbation can be defined as the sudden worsening or deterioration of the
conditions that the patient is going through. In case of COPD, exacerbation can be due to many
factors; however the most common contributor is bacterial infection. It generally comprises of
INTERVENTION AND MANAGEMENT OF COPD
Bronchitis on the other hand is developed due to the inflammation of the bronchial tubes
accompanied by the over secretion of mucus. The over secretion of mucus eventually leads to
blocking of the airways and contribute to difficult air passage during the process of respiration. It
has to be understood that smoking is a very important contributing factor that has a profound role
in the pathophysiologic development of this respiratory disorder. For the case study, Robert, the
patient under consideration had been a chain-smoker for 40 years, smoking can be considered as
the origin of the disease he had developed. According to the case study, Robert had been
diagnosed with COPD 18 months ago and had been feeling unwell for months befire that as well.
Hence, it can be concluded that the onset of manifestations brnchitics and emphysema had begun
since a long time. The added burden of smoking excessively had contributed effectively to
further deteriorating the disease, along with the age factor of the patient in the case study.
COPD pathway (Vogelmeier et al., 2011) impact of age on COPD (Erb-Downward et al., 2011)
Exacerbation of the COPD:
An exacerbation can be defined as the sudden worsening or deterioration of the
conditions that the patient is going through. In case of COPD, exacerbation can be due to many
factors; however the most common contributor is bacterial infection. It generally comprises of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
INTERVENTION AND MANAGEMENT OF COPD
sudden acute shortness of breath and altered quantity and consistency of the phlegm. In case of
COPD, an exacerbation event can last up-to several days and can effectively complicate the
health condition of the patient. In case of an exacerbation of COPD, the airways of the patient go
through enhanced inflammation, and coupled with increased mucous production, the gas
exchange is impaired effectively (Vogelmeier et al., 2011).
There can be many contributing factors that lead to an exacerbation event, along with
bacterial, infection, environmental pollution is also another reason for the sudden worsening.
With respect to the case study, for Robert, the most important risk factor that might have had a
profound role in the development of the exacerbation of the disease is infection. Infection by
Streptococcus pneumoniae often leads to further blockage of the airways which contributes to
impaired gas exchange and leads to dyspnea. According to the case study, Robert had been a
smoker for 40 years and continues to smoke in the present. Hence, the second risk factor for
Robert that might have led to exacerbation is smoking (Erb-Downward et al., 2011). It has to be
understood that allergens, especially smoke, can irritate the inflamed airways and air sacs
resulting in further inflammation. Hence these are the two risk factors behind the exacerbation of
COPD experienced by Robert in the case study.
Pathophysiology of pneumonia:
Pneumonia can be described as the infectious disease facilitates the inflammation of the air
sacs and results in overproduction of phlegm. The infection can have either bacterial or viral
Origin. During aspiration process the bacterial pathogen enters the body through the airways and
colonize the lung parenchyma. On a more elaborative note, it has to be mentioned that the
infection mechanism is facilitated by the invasion of the lung parenchyma. The overgrowth of
the bacteria in the lung parenchyma provokes the overproduction of intra-alveolar exudates like
INTERVENTION AND MANAGEMENT OF COPD
sudden acute shortness of breath and altered quantity and consistency of the phlegm. In case of
COPD, an exacerbation event can last up-to several days and can effectively complicate the
health condition of the patient. In case of an exacerbation of COPD, the airways of the patient go
through enhanced inflammation, and coupled with increased mucous production, the gas
exchange is impaired effectively (Vogelmeier et al., 2011).
There can be many contributing factors that lead to an exacerbation event, along with
bacterial, infection, environmental pollution is also another reason for the sudden worsening.
With respect to the case study, for Robert, the most important risk factor that might have had a
profound role in the development of the exacerbation of the disease is infection. Infection by
Streptococcus pneumoniae often leads to further blockage of the airways which contributes to
impaired gas exchange and leads to dyspnea. According to the case study, Robert had been a
smoker for 40 years and continues to smoke in the present. Hence, the second risk factor for
Robert that might have led to exacerbation is smoking (Erb-Downward et al., 2011). It has to be
understood that allergens, especially smoke, can irritate the inflamed airways and air sacs
resulting in further inflammation. Hence these are the two risk factors behind the exacerbation of
COPD experienced by Robert in the case study.
Pathophysiology of pneumonia:
Pneumonia can be described as the infectious disease facilitates the inflammation of the air
sacs and results in overproduction of phlegm. The infection can have either bacterial or viral
Origin. During aspiration process the bacterial pathogen enters the body through the airways and
colonize the lung parenchyma. On a more elaborative note, it has to be mentioned that the
infection mechanism is facilitated by the invasion of the lung parenchyma. The overgrowth of
the bacteria in the lung parenchyma provokes the overproduction of intra-alveolar exudates like
5
INTERVENTION AND MANAGEMENT OF COPD
mucous. It has to be mentioned in this context that the pneumonia infection manifests further as
soon as the pathogen reaches the alveoli, the host defences at this point are usually overwhelmed
by either the virulence or the inoculum size of the pathogen, and the infection spreads (Musher &
Thorner, 2014).
The community acquired pneumonia (CAP) can be considered as the most commonly
reported type and the mechanism of the infection in case of the community acquired pneumonia
differs from the other types significantly. The community acquired pneumonia is fundamentally
unique from any other type of pneumonia by the fact that it is not associated with the health care
facility at all. In case of CAP, the causing organism can be over 100 different types. The most
common types of infectious agents in case of the community acquired pneumonia, are bacteria,
virus, fungi and even allergens. However, in case of hospital acquired pneumonia is often more
severe as it is acquired by the patient during hospice stay, and the causing agent is often
antibiotic resistant strains. The patients on ventilators and intensive care units are at the most risk
of this type of pneumonia. In case of the health care associated pneumonia the point of acquiring
the infection is due to a long term stay in any community care setting or any outpatient clinics
(Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund, 2010).
Pharmacology of the medications administered:
2.1
Salbutamol:
It is a selective Beta 2 adrenergic receptor stimulating drug, and the most important function
of this medication in case of COPD is of bronchodilation. It has to be mentioned that the
stimulation by salbutamol activates the adenyl cyclase which is then transformed into cyclic
INTERVENTION AND MANAGEMENT OF COPD
mucous. It has to be mentioned in this context that the pneumonia infection manifests further as
soon as the pathogen reaches the alveoli, the host defences at this point are usually overwhelmed
by either the virulence or the inoculum size of the pathogen, and the infection spreads (Musher &
Thorner, 2014).
The community acquired pneumonia (CAP) can be considered as the most commonly
reported type and the mechanism of the infection in case of the community acquired pneumonia
differs from the other types significantly. The community acquired pneumonia is fundamentally
unique from any other type of pneumonia by the fact that it is not associated with the health care
facility at all. In case of CAP, the causing organism can be over 100 different types. The most
common types of infectious agents in case of the community acquired pneumonia, are bacteria,
virus, fungi and even allergens. However, in case of hospital acquired pneumonia is often more
severe as it is acquired by the patient during hospice stay, and the causing agent is often
antibiotic resistant strains. The patients on ventilators and intensive care units are at the most risk
of this type of pneumonia. In case of the health care associated pneumonia the point of acquiring
the infection is due to a long term stay in any community care setting or any outpatient clinics
(Johansson, Kalin, Tiveljung-Lindell, Giske & Hedlund, 2010).
Pharmacology of the medications administered:
2.1
Salbutamol:
It is a selective Beta 2 adrenergic receptor stimulating drug, and the most important function
of this medication in case of COPD is of bronchodilation. It has to be mentioned that the
stimulation by salbutamol activates the adenyl cyclase which is then transformed into cyclic
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
INTERVENTION AND MANAGEMENT OF COPD
AMP. The increased concentration of cyclic AMP then in turn relaxes the bronchial smooth
muscles and reduces the airway resistance by relaxing the bronchial tubes from trachea to
terminal bronchioles (Albert et al., 2011).
The contraindications for salbutamol include any patient with a history of hypersensitivity
reaction along with any patient with fast history of cardiac tachyarrhythmias. Hence if Robert
has had any history of hypersensitivity, Salbutamol will be contraindicated for him.
Also salbutamol is a well tolerated drug. yet side effects may occur due to any dosage or
administration route error. With respect to this case study, the nursing professional should also
be careful if Robert exhibits any signs of tremors special in the hands or any preparation of
tachycardia, which is the most frequently reported side effects of salbutamol (Bischoff et al.,
2011).
Budesonide/efomoterol fumarate dehydrate (symbicort):
This medication is a combination of a long acting Beta 2 adrenergic receptor agonist and
an inhaled corticosteroid. This medication is considered to be a maintenance therapy for the
COPD patients. The inhaled corticosteroid or budesonide, has anti-inflammatory properties
which help to reduce the inflammation of the bronchial airways and facilities better air passage.
And formoterol is the long acting beta agonist bronchodilator which relaxes the muscles and
prevents any bronchospasm, hence it will help relaxing respiratory muscles of Robert and wil
evade any chances of him going through bronchospasm (Agusti, 2014).
There are two major contraindications of this medication, with any acute episodes of
COPD where intensive measures are required this medication cannot be administered. In case of
Robert, any hypersensitivity reaction to the components of this medication will be harmful as
INTERVENTION AND MANAGEMENT OF COPD
AMP. The increased concentration of cyclic AMP then in turn relaxes the bronchial smooth
muscles and reduces the airway resistance by relaxing the bronchial tubes from trachea to
terminal bronchioles (Albert et al., 2011).
The contraindications for salbutamol include any patient with a history of hypersensitivity
reaction along with any patient with fast history of cardiac tachyarrhythmias. Hence if Robert
has had any history of hypersensitivity, Salbutamol will be contraindicated for him.
Also salbutamol is a well tolerated drug. yet side effects may occur due to any dosage or
administration route error. With respect to this case study, the nursing professional should also
be careful if Robert exhibits any signs of tremors special in the hands or any preparation of
tachycardia, which is the most frequently reported side effects of salbutamol (Bischoff et al.,
2011).
Budesonide/efomoterol fumarate dehydrate (symbicort):
This medication is a combination of a long acting Beta 2 adrenergic receptor agonist and
an inhaled corticosteroid. This medication is considered to be a maintenance therapy for the
COPD patients. The inhaled corticosteroid or budesonide, has anti-inflammatory properties
which help to reduce the inflammation of the bronchial airways and facilities better air passage.
And formoterol is the long acting beta agonist bronchodilator which relaxes the muscles and
prevents any bronchospasm, hence it will help relaxing respiratory muscles of Robert and wil
evade any chances of him going through bronchospasm (Agusti, 2014).
There are two major contraindications of this medication, with any acute episodes of
COPD where intensive measures are required this medication cannot be administered. In case of
Robert, any hypersensitivity reaction to the components of this medication will be harmful as
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
INTERVENTION AND MANAGEMENT OF COPD
well if taking this medication. Adverse reactions to this medication include allergic reaction,
adrenal insufficiency and even an increased risk of infection such as pneumonia.
There are 2 nursing considerations for this medication when administering to Robert, risk
for infection and hypersensitivity. Patient education includes explaining to Robert to never use
budesonide or formoterol in case of acute bronchospasm. In case of exceeding wheezing, Robert
should be instructed to seek out immediate medical attention due to the possibility of acute
asthmatic attack (Agusti, 2014).
Tiotropium:
Tiotropium is another bronchial muscle relaxant which is used to prevent any wheezing
or shortness of breath. This medication is an anticholinergic and it relaxes the muscles around the
bronchi and will facilitate smoother air passage in case of Robert.
The contraindication for this medication includes any hypersensitivity to anticholinergics.
Along with that renal diseases in glaucoma also contraindicated against the administration of this
medication (Wise et al., 2013).
The adverse effects of this medication are constipation, nausea, muscular pain, and
nosebleed. Robert will need to be educated about the possible side effects of this medication all
diseases are the most plausible adverse reaction to this medicine. The nursing considerations
include the fact that this medicine should only be taken to prevent bronchospasm for an ongoing
broncos ransom attack this medication should not be taken (Wise et al., 2013).
The main contributing factor behind the doctor changing Robert’s medicine chart by
replacing the symbicort with tritopium can be the fact that symbicort can only be used in regular
cases of COPD, it has no noticeable effect on exception of subdivision patient had been going
INTERVENTION AND MANAGEMENT OF COPD
well if taking this medication. Adverse reactions to this medication include allergic reaction,
adrenal insufficiency and even an increased risk of infection such as pneumonia.
There are 2 nursing considerations for this medication when administering to Robert, risk
for infection and hypersensitivity. Patient education includes explaining to Robert to never use
budesonide or formoterol in case of acute bronchospasm. In case of exceeding wheezing, Robert
should be instructed to seek out immediate medical attention due to the possibility of acute
asthmatic attack (Agusti, 2014).
Tiotropium:
Tiotropium is another bronchial muscle relaxant which is used to prevent any wheezing
or shortness of breath. This medication is an anticholinergic and it relaxes the muscles around the
bronchi and will facilitate smoother air passage in case of Robert.
The contraindication for this medication includes any hypersensitivity to anticholinergics.
Along with that renal diseases in glaucoma also contraindicated against the administration of this
medication (Wise et al., 2013).
The adverse effects of this medication are constipation, nausea, muscular pain, and
nosebleed. Robert will need to be educated about the possible side effects of this medication all
diseases are the most plausible adverse reaction to this medicine. The nursing considerations
include the fact that this medicine should only be taken to prevent bronchospasm for an ongoing
broncos ransom attack this medication should not be taken (Wise et al., 2013).
The main contributing factor behind the doctor changing Robert’s medicine chart by
replacing the symbicort with tritopium can be the fact that symbicort can only be used in regular
cases of COPD, it has no noticeable effect on exception of subdivision patient had been going
8
INTERVENTION AND MANAGEMENT OF COPD
through. Along with that, the major side effects of symbicort is pneumonia, and as the patient has
already been suffering with community-acquired pneumonia continuing symbicort can be very
harmful for the patient. Hence, the doctor replaced Symbicort with Tiotropium, which is a more
targeted and fast action relieving medicine mainly used for treating bronchospasm attacks and
exacerbations that Robert has been having (Wise et al., 2013).
2.2.
Amoxicillin:
Amoxicillin is a penicillin type antibiotic that is used to treat many bacterial infections
including pneumonia by Streptococcus pneumonia, and it can be used to treat Robert. It is
usually administered orally every 8 to 12 hours and dosage is dependent on the severity of the
infection.
The contraindications include any allergies to penicillin type antibiotics and any renal disease
which can be aggravated due to administration of this medicine. As Robert had no past history of
renal diseases mentioned, this antibiotic can be easily used for Robert.
Adverse effects that Robert might encounter include nausea, vomiting, and diarrhea.
Nursing considerations include patients with mononucleosis not been given this medication
along with patients with any hepatic impairment. Care should also be taken to ensure that
phenylalanine is present in the oral chewable tablets and suspensions given to Robert.
Patient education includes teaching Robert to chew or crush the chewable tablets rather than
swallowing it and to notify the carer in case of any aggravation or bloody urine (Torres et al.,
2015).
INTERVENTION AND MANAGEMENT OF COPD
through. Along with that, the major side effects of symbicort is pneumonia, and as the patient has
already been suffering with community-acquired pneumonia continuing symbicort can be very
harmful for the patient. Hence, the doctor replaced Symbicort with Tiotropium, which is a more
targeted and fast action relieving medicine mainly used for treating bronchospasm attacks and
exacerbations that Robert has been having (Wise et al., 2013).
2.2.
Amoxicillin:
Amoxicillin is a penicillin type antibiotic that is used to treat many bacterial infections
including pneumonia by Streptococcus pneumonia, and it can be used to treat Robert. It is
usually administered orally every 8 to 12 hours and dosage is dependent on the severity of the
infection.
The contraindications include any allergies to penicillin type antibiotics and any renal disease
which can be aggravated due to administration of this medicine. As Robert had no past history of
renal diseases mentioned, this antibiotic can be easily used for Robert.
Adverse effects that Robert might encounter include nausea, vomiting, and diarrhea.
Nursing considerations include patients with mononucleosis not been given this medication
along with patients with any hepatic impairment. Care should also be taken to ensure that
phenylalanine is present in the oral chewable tablets and suspensions given to Robert.
Patient education includes teaching Robert to chew or crush the chewable tablets rather than
swallowing it and to notify the carer in case of any aggravation or bloody urine (Torres et al.,
2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
INTERVENTION AND MANAGEMENT OF COPD
Ceftriaxone:
This is another cephalosporone type medication that is used to treat this infection, and is a
very common treatment option for pneumococcal infections for elderly patients like Robert.
The contraindications include hypersensitivity and the risk of calcium ceftriaxone interaction,
which is needed to be assessed before administering to Robert.
The adverse effects that Robert can have include bronchospasm, diarrhea, and nausea.
Nursing considerations include checking for any allergies reaction of shortness of breath that
Robert might experience.
In terms of patient education, Robert should be instructed to notify and seek attention in case
of hypersensitive reaction (Martin-Loeches et al., 2010).
Levoflaxone:
It s a quilonone used to treat pneumococcal infections in case of penicillin resistant strains.
The contraindications include hypersensitivity, diabetes, and renal disorders.
The adverse effects that Robert may have include nausea, insomnia, diarrhea and headache.
The nursing consideration for this are ensuring Robert not being allergic to quilonone
compounds and should be run slowly to avoid stinging.
The patient teaching must include informing Robert to refrain from taking vitamins and
supplements long with the possible side effects (Postma et al., 2015).
Psychosocial interventions for COPD:
.
INTERVENTION AND MANAGEMENT OF COPD
Ceftriaxone:
This is another cephalosporone type medication that is used to treat this infection, and is a
very common treatment option for pneumococcal infections for elderly patients like Robert.
The contraindications include hypersensitivity and the risk of calcium ceftriaxone interaction,
which is needed to be assessed before administering to Robert.
The adverse effects that Robert can have include bronchospasm, diarrhea, and nausea.
Nursing considerations include checking for any allergies reaction of shortness of breath that
Robert might experience.
In terms of patient education, Robert should be instructed to notify and seek attention in case
of hypersensitive reaction (Martin-Loeches et al., 2010).
Levoflaxone:
It s a quilonone used to treat pneumococcal infections in case of penicillin resistant strains.
The contraindications include hypersensitivity, diabetes, and renal disorders.
The adverse effects that Robert may have include nausea, insomnia, diarrhea and headache.
The nursing consideration for this are ensuring Robert not being allergic to quilonone
compounds and should be run slowly to avoid stinging.
The patient teaching must include informing Robert to refrain from taking vitamins and
supplements long with the possible side effects (Postma et al., 2015).
Psychosocial interventions for COPD:
.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
INTERVENTION AND MANAGEMENT OF COPD
According to the case study, Robert has been suffering from Exacerbation of COPD and
severe community acquired pneumonia which has is associated with suffering and restrictions
which can eventually have a significant psychological burden on the patient. Psychosocial
burden associated with co-mosbidities have been reported to have a huge impact on the recovery
statistics and wellbeing of the patient, and can even alter the response of the patient to the
treatment pathways.
Administering psychotherapic intervention can help the patient overcome the issues
effectively. The most common intervention is cognitive behavioral therapy which will help
Robert deal with the stress. However another psycho social intervention is mindfulness based
therapy, which is gaining popularity in case of such disorders as well according to Agusti (2014).
Moreover, relaxing therapies like yoga and meditation sessions can also help Robert find
strength to cope with the stress and regain control of his recovery with respect to the case study
(Wong et al., 2014). The next results can be yielded by an integrative psychotherapic plan
incorporating cognitive behavioral therapy, mindfulness based intervention and relaxation
technoques; which can address the differential psychotherapic need of a critical patient like
Robert.
INTERVENTION AND MANAGEMENT OF COPD
According to the case study, Robert has been suffering from Exacerbation of COPD and
severe community acquired pneumonia which has is associated with suffering and restrictions
which can eventually have a significant psychological burden on the patient. Psychosocial
burden associated with co-mosbidities have been reported to have a huge impact on the recovery
statistics and wellbeing of the patient, and can even alter the response of the patient to the
treatment pathways.
Administering psychotherapic intervention can help the patient overcome the issues
effectively. The most common intervention is cognitive behavioral therapy which will help
Robert deal with the stress. However another psycho social intervention is mindfulness based
therapy, which is gaining popularity in case of such disorders as well according to Agusti (2014).
Moreover, relaxing therapies like yoga and meditation sessions can also help Robert find
strength to cope with the stress and regain control of his recovery with respect to the case study
(Wong et al., 2014). The next results can be yielded by an integrative psychotherapic plan
incorporating cognitive behavioral therapy, mindfulness based intervention and relaxation
technoques; which can address the differential psychotherapic need of a critical patient like
Robert.
11
INTERVENTION AND MANAGEMENT OF COPD
References:
Agusti, A. (2014). The path to personalised medicine in COPD. Thorax, vol 69(9), pp 857-864.
DOi: 10.1136/thoraxjnl-2014-205507
Agustí, A., Edwards, L. D., Rennard, S. I., MacNee, W., Tal-Singer, R., Miller, B. E., ... & Crim,
C. (2012). Persistent systemic inflammation is associated with poor clinical outcomes in
COPD: a novel phenotype. PloS one, vol 7(5), e37483. Retrieved from
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037483
Albert, R. K., Connett, J., Bailey, W. C., Casaburi, R., Cooper Jr, J. A. D., Criner, G. J., ... &
Make, B. (2011). Azithromycin for prevention of exacerbations of COPD. New England
Journal of Medicine, 365(8), pp 689-698. DOI: 10.1056/NEJMoa1104623.
Almagro, P., Cabrera, F. J., Diez, J., Boixeda, R., Ortiz, M. B. A., Murio, C., & Soriano, J. B.
(2012). Comorbidities and short-term prognosis in patients hospitalized for acute
exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI)
study. Chest, vol 142(5), pp 1126-1133. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Bischoff, E. W., Hamd, D. H., Sedeno, M., Benedetti, A., Schermer, T. R., Bernard, S., ... &
Bourbeau, J. (2011). Effects of written action plan adherence on COPD exacerbation
recovery. Thorax, vol 66(1), pp 26-31. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Erb-Downward, J. R., Thompson, D. L., Han, M. K., Freeman, C. M., McCloskey, L., Schmidt,
L. A., ... & Martinez, F. J. (2011). Analysis of the lung microbiome in the “healthy”
INTERVENTION AND MANAGEMENT OF COPD
References:
Agusti, A. (2014). The path to personalised medicine in COPD. Thorax, vol 69(9), pp 857-864.
DOi: 10.1136/thoraxjnl-2014-205507
Agustí, A., Edwards, L. D., Rennard, S. I., MacNee, W., Tal-Singer, R., Miller, B. E., ... & Crim,
C. (2012). Persistent systemic inflammation is associated with poor clinical outcomes in
COPD: a novel phenotype. PloS one, vol 7(5), e37483. Retrieved from
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037483
Albert, R. K., Connett, J., Bailey, W. C., Casaburi, R., Cooper Jr, J. A. D., Criner, G. J., ... &
Make, B. (2011). Azithromycin for prevention of exacerbations of COPD. New England
Journal of Medicine, 365(8), pp 689-698. DOI: 10.1056/NEJMoa1104623.
Almagro, P., Cabrera, F. J., Diez, J., Boixeda, R., Ortiz, M. B. A., Murio, C., & Soriano, J. B.
(2012). Comorbidities and short-term prognosis in patients hospitalized for acute
exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI)
study. Chest, vol 142(5), pp 1126-1133. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Bischoff, E. W., Hamd, D. H., Sedeno, M., Benedetti, A., Schermer, T. R., Bernard, S., ... &
Bourbeau, J. (2011). Effects of written action plan adherence on COPD exacerbation
recovery. Thorax, vol 66(1), pp 26-31. Retrieved from
http://journal.chestnet.org/article/S0012-3692(12)60613-8/abstract
Erb-Downward, J. R., Thompson, D. L., Han, M. K., Freeman, C. M., McCloskey, L., Schmidt,
L. A., ... & Martinez, F. J. (2011). Analysis of the lung microbiome in the “healthy”
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




