Coronary Heart Disease: A Comprehensive Report on CHD (Course Name)
VerifiedAdded on 2020/03/28
|23
|5462
|49
Report
AI Summary
This report provides a comprehensive review of coronary heart disease (CHD), also known as ischemic heart disease or coronary artery disease, a prevalent condition characterized by the accumulation of fatty material in coronary arteries. The report delves into the anatomy and physiology of the involved systems, including the structure and function of coronary vessels, and explains the process of atherosclerosis. It explores the aetiology, detailing both modifiable and fixed risk factors such as smoking, hypertension, diabetes, and family history. The clinical presentation of CHD is discussed, covering symptoms like angina and myocardial infarction, alongside investigative procedures such as ECG, echocardiography, stress testing, and coronary angiography. Finally, the report touches upon the management and treatment of CHD, with a particular focus on pharmacological interventions. The report aims to provide a detailed overview of the disease, its causes, diagnostic methods, and treatment options.

Running head: CORONARY HEART DISEASE 1
Coronary Heart Disease
Name
Institution
Coronary Heart Disease
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CORONARY HEART DISEASE 2
Coronary Heart Disease
Introduction
Coronary heart disease (CHD), also known as ischaemic heart disease or coronary artery
disease is a common form of heart disease characterised by the gradual accumulation of fatty
material (plaque) within the walls of the coronary arteries. The build-up of plaque results
from a process known as atherosclerosis which is influenced by lifestyle habits such as high
cholesterol and smoking, and conditions such as diabetes and hypertension (Nichols,
Peterson, Herbert, & Allender, 2015). CHD in its two major clinical forms (angina and
myocardial infarction) is the largest contributor to cardiovascular disease (CVD) (Australian
Institute of Health and Welfare, 2012)
The condition is responsible for a significant amount of morbidity and mortality globally. In
2015 alone, CHD affected more than a hundred million people and resulted in close to nine
million deaths (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators,
2016); accounting for more than fifteen percent of all deaths worldwide. As a result, it ranks
at the most common cause of mortality worldwide (GBD 2015 Mortality and Causes of Death
Collaborators, 2016). CHD affects approximately 1.2 million Australians. It stands out as the
single leading cause of death in Australia, accounting for more than ten percent of all deaths
in the country. For instance, in 2015, it accounted for 19, 777 deaths, an equivalent of 12% of
all deaths in that year (Australian Bureau of Statistics, 2016).
This paper reviews various aspects of this condition including the anatomy and physiology of
the involved systems, its aetiology, clinical presentation, the investigative procedures adopted
Coronary Heart Disease
Introduction
Coronary heart disease (CHD), also known as ischaemic heart disease or coronary artery
disease is a common form of heart disease characterised by the gradual accumulation of fatty
material (plaque) within the walls of the coronary arteries. The build-up of plaque results
from a process known as atherosclerosis which is influenced by lifestyle habits such as high
cholesterol and smoking, and conditions such as diabetes and hypertension (Nichols,
Peterson, Herbert, & Allender, 2015). CHD in its two major clinical forms (angina and
myocardial infarction) is the largest contributor to cardiovascular disease (CVD) (Australian
Institute of Health and Welfare, 2012)
The condition is responsible for a significant amount of morbidity and mortality globally. In
2015 alone, CHD affected more than a hundred million people and resulted in close to nine
million deaths (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators,
2016); accounting for more than fifteen percent of all deaths worldwide. As a result, it ranks
at the most common cause of mortality worldwide (GBD 2015 Mortality and Causes of Death
Collaborators, 2016). CHD affects approximately 1.2 million Australians. It stands out as the
single leading cause of death in Australia, accounting for more than ten percent of all deaths
in the country. For instance, in 2015, it accounted for 19, 777 deaths, an equivalent of 12% of
all deaths in that year (Australian Bureau of Statistics, 2016).
This paper reviews various aspects of this condition including the anatomy and physiology of
the involved systems, its aetiology, clinical presentation, the investigative procedures adopted
CORONARY HEART DISEASE 3
for the diagnosis, and its management and treatment with more focus on its pharmacology
treatment.
for the diagnosis, and its management and treatment with more focus on its pharmacology
treatment.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CORONARY HEART DISEASE 4
Overview of anatomy and physiology of systems involved
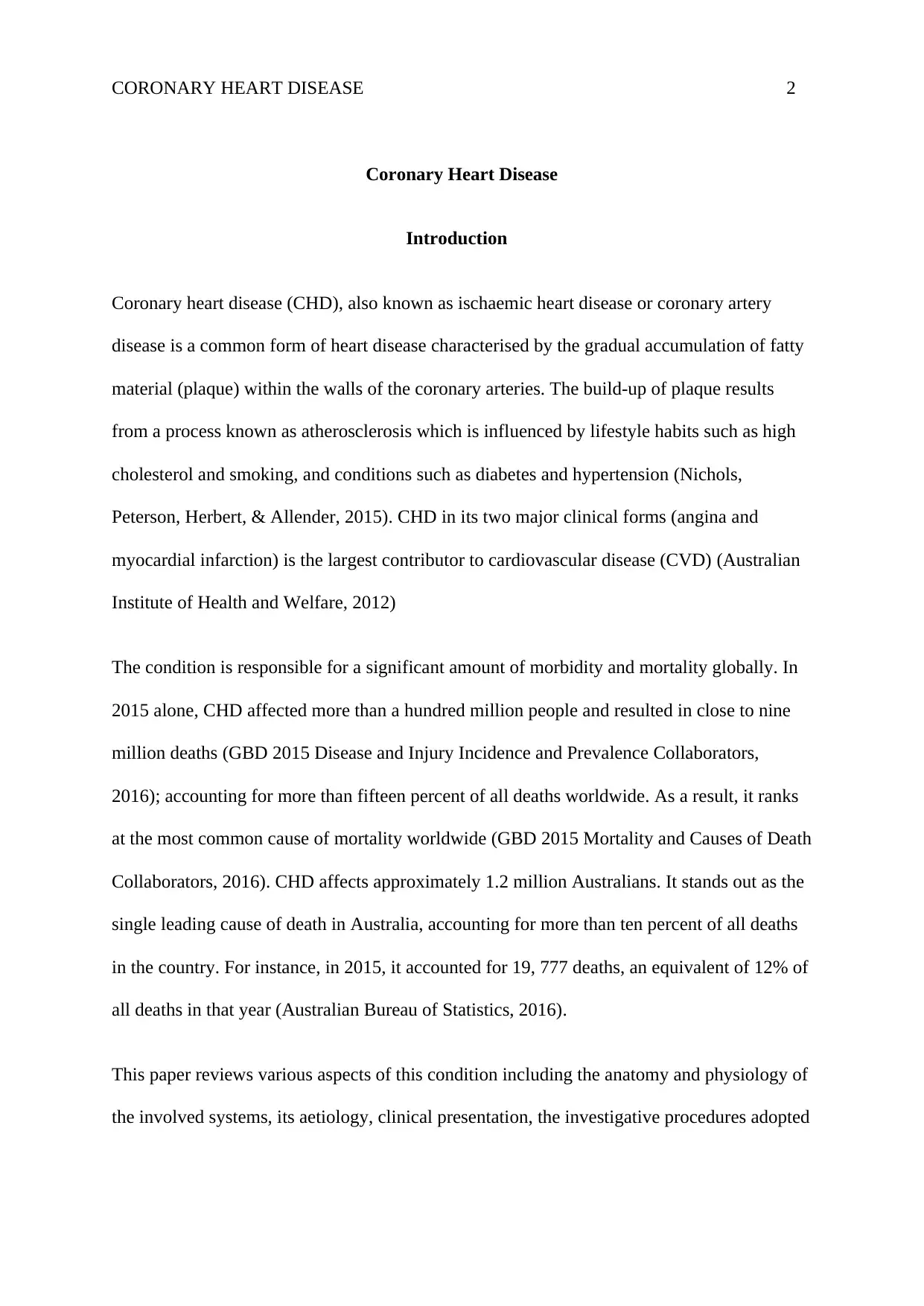
Coronary vessels have a different anatomy and physiology compared to the rest of the vessels
of the circulatory system. Coronary arteries are much smaller, tortuous vessels which supply
the myocardium with blood. The left main coronary artery (LCA) and the right coronary
artery (RCA) originate from the aorta as separate vessels and not as a single trunk
(Lüdinghausen, 2012). Whereas the LCA rises from the posterior coronary cusp, the RCA
arises from the anterior coronary cusp. The course taken by the two large vessels (RCA and
LCA) is also different as shown in Figure 1 below.
The RCA supplies blood to the right ventricle and atrium, and the atrioventricular and nodes
which serve the role of regulating the heart’s rhythm (Spaan, 2012). The RCA further
branches into smaller branches which include the acute marginal artery and the right posterior
descending artery. It also teams up with left anterior descending anterior to form the septal
perforator (SP) which supplies blood to the septum. The LCA supplies blood to the left
ventricle and atrium. It further branches into the left anterior descending artery that supplies
blood to the front of the left side of the heart, and the circumflex artery which supplies blood
to the back and outer side of the heart. Other smaller branches of the coronary arteries include
diagonals, and the obtuse marginal (OM).
Overview of anatomy and physiology of systems involved
Coronary vessels have a different anatomy and physiology compared to the rest of the vessels
of the circulatory system. Coronary arteries are much smaller, tortuous vessels which supply
the myocardium with blood. The left main coronary artery (LCA) and the right coronary
artery (RCA) originate from the aorta as separate vessels and not as a single trunk
(Lüdinghausen, 2012). Whereas the LCA rises from the posterior coronary cusp, the RCA
arises from the anterior coronary cusp. The course taken by the two large vessels (RCA and
LCA) is also different as shown in Figure 1 below.
The RCA supplies blood to the right ventricle and atrium, and the atrioventricular and nodes
which serve the role of regulating the heart’s rhythm (Spaan, 2012). The RCA further
branches into smaller branches which include the acute marginal artery and the right posterior
descending artery. It also teams up with left anterior descending anterior to form the septal
perforator (SP) which supplies blood to the septum. The LCA supplies blood to the left
ventricle and atrium. It further branches into the left anterior descending artery that supplies
blood to the front of the left side of the heart, and the circumflex artery which supplies blood
to the back and outer side of the heart. Other smaller branches of the coronary arteries include
diagonals, and the obtuse marginal (OM).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CORONARY HEART DISEASE 5
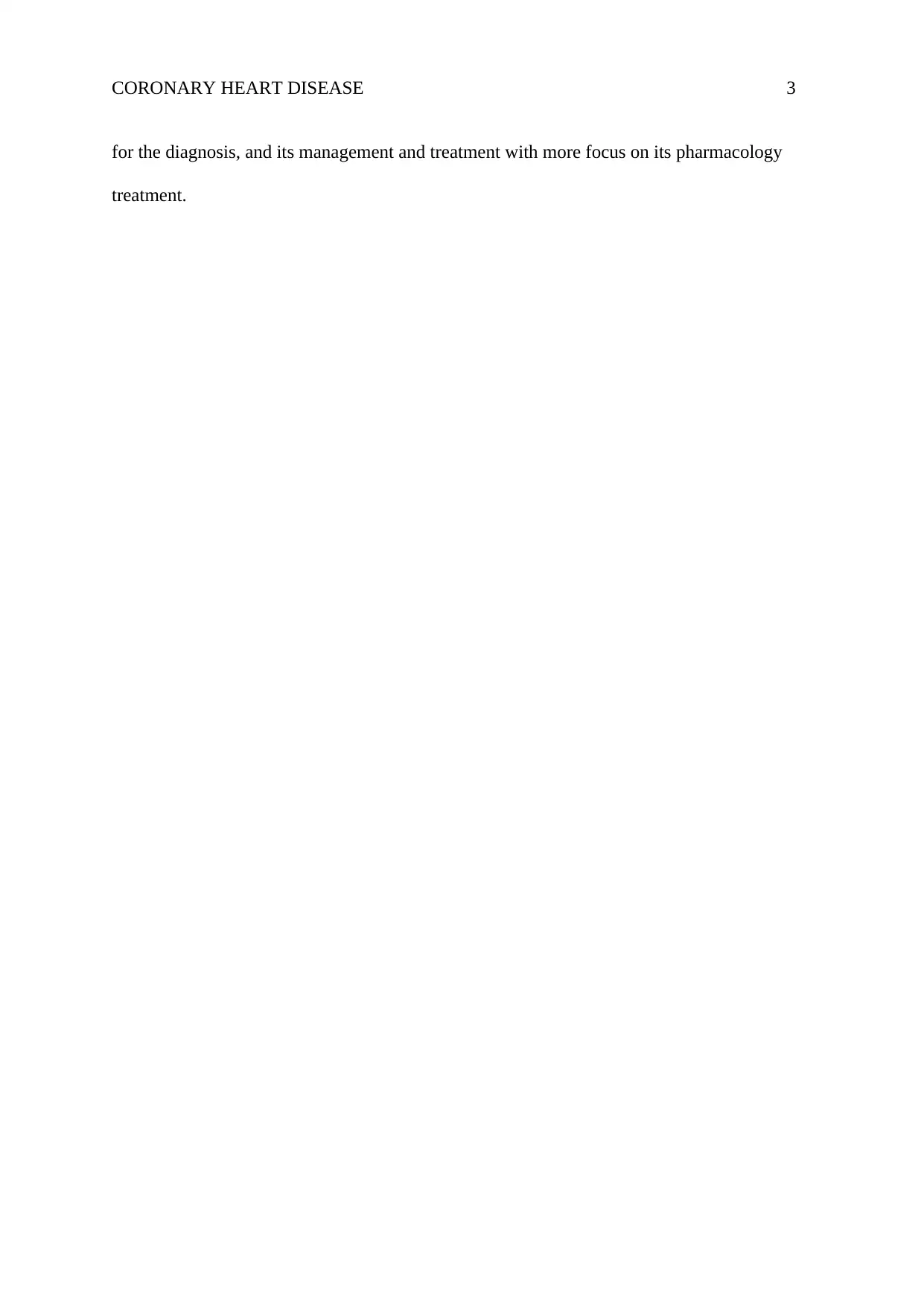
Atherosclerosis affects both the structure and function of the coronary arteries. Plaque
narrows the arteries (as shown in figure 2 above), and as a result, the blood flow to the
myocardium is also reduced. The build-up of plaque also increases the likelihood of blood
clots forming in the arteries. The clots can somewhat or totally block the blood flow to the
myocardium (ischemia). These processes lead to an imbalance between oxygen supply and
oxygen demand. With insufficient oxygen supply to meet the demand, the myocardium
becomes hypoxic and this often translates to angina (chest pain) or a heart attack.
(Source: John Hopkins Medicine) (Source: National Heart, Lung, and Blood Institute
Figure 1: Coronary arteries of the heart Figure 2: Normal artery vs narrowed artery following atherosclerosis
Figure A shows a normal artery, while figure B shows an artery
with plaque build-up
Atherosclerosis affects both the structure and function of the coronary arteries. Plaque
narrows the arteries (as shown in figure 2 above), and as a result, the blood flow to the
myocardium is also reduced. The build-up of plaque also increases the likelihood of blood
clots forming in the arteries. The clots can somewhat or totally block the blood flow to the
myocardium (ischemia). These processes lead to an imbalance between oxygen supply and
oxygen demand. With insufficient oxygen supply to meet the demand, the myocardium
becomes hypoxic and this often translates to angina (chest pain) or a heart attack.
(Source: John Hopkins Medicine) (Source: National Heart, Lung, and Blood Institute
Figure 1: Coronary arteries of the heart Figure 2: Normal artery vs narrowed artery following atherosclerosis
Figure A shows a normal artery, while figure B shows an artery
with plaque build-up
CORONARY HEART DISEASE 6
Summary of terms pertaining to the disease
a) Coronary heart disease (CHD) – The thinning of coronary arteries due to deposition
of plaques, resulting in reduced blood flow to cardiac muscles (Newton & Joyce,
2014).
b) Coronary artery disease (CAD) – Another name for coronary heart disease.
c) Ischemic heart disease - Another name for coronary heart disease
d) Ischemia – The inadequate supply of blood to the heart muscles causing a shortage of
oxygen and glucose necessary to cellular metabolism (Merck & Co, 2012).
e) Angina pectoris - is the feeling of chest pain, pressure, or squeezing, resulting from
inadequate blood supply to the myocardium (Newton & Joyce, 2014).
f) Stable angina – Classic type of angina which presents as chest discomfort often
precipitated by some physical activity.
g) Unstable angina - Angina pectoris that changes or worsens
h) Myocardial infarction (heart attack) – is the irreversible death (necrosis) of heart
muscle due to blockage in coronary arteries that completely blocks the flow of blood
to the cardiac muscles (Newton & Joyce, 2014).
i) CABG: Coronary artery bypass graft; and Coronary artery bypass grafting - a surgical
procedure that recovers blood supply to cardiac muscles (National Health Institutes,
2012).
Summary of terms pertaining to the disease
a) Coronary heart disease (CHD) – The thinning of coronary arteries due to deposition
of plaques, resulting in reduced blood flow to cardiac muscles (Newton & Joyce,
2014).
b) Coronary artery disease (CAD) – Another name for coronary heart disease.
c) Ischemic heart disease - Another name for coronary heart disease
d) Ischemia – The inadequate supply of blood to the heart muscles causing a shortage of
oxygen and glucose necessary to cellular metabolism (Merck & Co, 2012).
e) Angina pectoris - is the feeling of chest pain, pressure, or squeezing, resulting from
inadequate blood supply to the myocardium (Newton & Joyce, 2014).
f) Stable angina – Classic type of angina which presents as chest discomfort often
precipitated by some physical activity.
g) Unstable angina - Angina pectoris that changes or worsens
h) Myocardial infarction (heart attack) – is the irreversible death (necrosis) of heart
muscle due to blockage in coronary arteries that completely blocks the flow of blood
to the cardiac muscles (Newton & Joyce, 2014).
i) CABG: Coronary artery bypass graft; and Coronary artery bypass grafting - a surgical
procedure that recovers blood supply to cardiac muscles (National Health Institutes,
2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CORONARY HEART DISEASE 7
Aetiology
A review of literature demonstrates an association between coronary heart disease and certain
factors which contribute to atherosclerosis. These factors increase the intrusion of fat into the
walls of the arteries. The various risk factors create different risk associations and there is a
likelihood that they may be interacting together. The risk factors include both fixed risks
(gender, family history, age, ethnicity and lower and middle socioeconomic groups), and
modifiable risks (cigarette smoking, hypertension, diabetes mellitus, excessive alcohol intake,
central obesity, lipid abnormalities such (high LDL cholesterol and triglycerides, low HDL),
physical inactivity, and psychosocial issues (Gupta, Joshi, Mohan, Reddy, & Yusuf, 2013).
Research suggests that an individual’s risk is as a risk of the total risk and not just individual
risk factors as the existence of the risk factors has a synergistic effect.
Modifiable risk factors
Smoking leads to the exposure of heart and blood vessels to nicotine and carbon monoxide
which in turn causes constriction of blood vessels, increase in blood pressure and a rise in
cholesterol levels. It also deprives the body’s tissues of oxygen and this allows the growing of
plaques.
Hypertension can lead to the damage of blood vessels hence increasing the chances of
plaques forming. High blood pressure also causes arterial walls to thicken and stiffen, and
less able to undergo expansion and contraction in line with body activity and other physical
demands.
Diabetes is characterised by high levels of glucose in blood that can cause harm to blood
vessels, and this increases the risk of developing atherosclerotic plaques. Evidence from
Aetiology
A review of literature demonstrates an association between coronary heart disease and certain
factors which contribute to atherosclerosis. These factors increase the intrusion of fat into the
walls of the arteries. The various risk factors create different risk associations and there is a
likelihood that they may be interacting together. The risk factors include both fixed risks
(gender, family history, age, ethnicity and lower and middle socioeconomic groups), and
modifiable risks (cigarette smoking, hypertension, diabetes mellitus, excessive alcohol intake,
central obesity, lipid abnormalities such (high LDL cholesterol and triglycerides, low HDL),
physical inactivity, and psychosocial issues (Gupta, Joshi, Mohan, Reddy, & Yusuf, 2013).
Research suggests that an individual’s risk is as a risk of the total risk and not just individual
risk factors as the existence of the risk factors has a synergistic effect.
Modifiable risk factors
Smoking leads to the exposure of heart and blood vessels to nicotine and carbon monoxide
which in turn causes constriction of blood vessels, increase in blood pressure and a rise in
cholesterol levels. It also deprives the body’s tissues of oxygen and this allows the growing of
plaques.
Hypertension can lead to the damage of blood vessels hence increasing the chances of
plaques forming. High blood pressure also causes arterial walls to thicken and stiffen, and
less able to undergo expansion and contraction in line with body activity and other physical
demands.
Diabetes is characterised by high levels of glucose in blood that can cause harm to blood
vessels, and this increases the risk of developing atherosclerotic plaques. Evidence from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CORONARY HEART DISEASE 8
research studies actually shows that one out of every three persons with diabetes also has
CHD (Mohammed, Narayan, & Tandon, 2013).
Excessive alcohol intake – Individuals who drink moderately (3 units/day for males and 1
unit/day for females) have a lower mortality from CHD compared to non-drinkers (Mukamal
& Rimm, 2016), whereas binge drinking above these levels increases the risk for CHD due to
the increased risk for the development of high blood cholesterol and hypertension.
Hyperlipidaemia – The risk of CHD is increased with the level of cholesterol in the blood.
Cholesterol levels, on the other hand, are dependent on factors such as diet, exercise,
genetics, and some diseases.
Obesity puts more strain on the heart, and also makes it difficult in controlling blood
pressure, diabetes and high cholesterol levels. According to Khosravi, et al., (2012), obesity
increases the risk for cardiovascular disease by 46% in males and 645 in females.
Physical inactivity weakens the muscles and makes it harder to control other risk factors for
cardiovascular disease which include obesity, diabetes, blood pressure and cholesterol levels.
Psychosocial issues such as stress, anxiety, depression and social isolation are also claimed
to be risk factors for CHD (Khayyam-Nekouei, Neshatdoost, Yousefy, Sadeghi, & Manshaee,
2013). Symptomatic CHD can be triggered by acute events such as the loss of a loved one,
and catastrophic events such as a terrorist attack.
Fixed risks
research studies actually shows that one out of every three persons with diabetes also has
CHD (Mohammed, Narayan, & Tandon, 2013).
Excessive alcohol intake – Individuals who drink moderately (3 units/day for males and 1
unit/day for females) have a lower mortality from CHD compared to non-drinkers (Mukamal
& Rimm, 2016), whereas binge drinking above these levels increases the risk for CHD due to
the increased risk for the development of high blood cholesterol and hypertension.
Hyperlipidaemia – The risk of CHD is increased with the level of cholesterol in the blood.
Cholesterol levels, on the other hand, are dependent on factors such as diet, exercise,
genetics, and some diseases.
Obesity puts more strain on the heart, and also makes it difficult in controlling blood
pressure, diabetes and high cholesterol levels. According to Khosravi, et al., (2012), obesity
increases the risk for cardiovascular disease by 46% in males and 645 in females.
Physical inactivity weakens the muscles and makes it harder to control other risk factors for
cardiovascular disease which include obesity, diabetes, blood pressure and cholesterol levels.
Psychosocial issues such as stress, anxiety, depression and social isolation are also claimed
to be risk factors for CHD (Khayyam-Nekouei, Neshatdoost, Yousefy, Sadeghi, & Manshaee,
2013). Symptomatic CHD can be triggered by acute events such as the loss of a loved one,
and catastrophic events such as a terrorist attack.
Fixed risks
CORONARY HEART DISEASE 9
Gender – Males are at increased risk of developing cardiovascular disease than females, but
the difference seems to disappear after the onset of menopause (National Institutes of Health,
2016).
Family history – An individual’s risk for CHD is doubled if a parent or sibling developed
cardiovascular disease early in life (before age 55 for males, and 65 for females) (National
Institutes of Health, 2016).
Age – The risk of CHD increases with the increase in age (National Institutes of Health,
2016). For males, the risk is heightened from about 45 years and above and is doubled at 55
upwards. For females, the risk is heightened as from age 55 upwards.
Ethnicity – The risk for CHD has shown to be increased among persons of African Caribbean
heritage, followed by Hispanics and South Asians (Leigh, Alvarez, & Rodriguez, 2016)
Socioeconomic status - It is an established fact that socioeconomically disadvantaged groups
have a higher prevalence of CHD and CVD mortality (Psaltopoulou, et al., 2017). The
gradient incidence of this morbidity and mortality is attributed to differences in income,
occupation, and educational status.
Signs and symptoms
a. Angina
The most prevalent CHD symptom is angina pectoris/chest pain. Approximately thirty
percent of adults who present o the emergency department with an unclear cause of pain, the
pain is often attributed to CHD (Kontos, Diercks, & Kirk, 2013). Angina is also described as
“chest discomfort, heaviness, tightness, pressure, aching, burning, numbness, fullness, or
Gender – Males are at increased risk of developing cardiovascular disease than females, but
the difference seems to disappear after the onset of menopause (National Institutes of Health,
2016).
Family history – An individual’s risk for CHD is doubled if a parent or sibling developed
cardiovascular disease early in life (before age 55 for males, and 65 for females) (National
Institutes of Health, 2016).
Age – The risk of CHD increases with the increase in age (National Institutes of Health,
2016). For males, the risk is heightened from about 45 years and above and is doubled at 55
upwards. For females, the risk is heightened as from age 55 upwards.
Ethnicity – The risk for CHD has shown to be increased among persons of African Caribbean
heritage, followed by Hispanics and South Asians (Leigh, Alvarez, & Rodriguez, 2016)
Socioeconomic status - It is an established fact that socioeconomically disadvantaged groups
have a higher prevalence of CHD and CVD mortality (Psaltopoulou, et al., 2017). The
gradient incidence of this morbidity and mortality is attributed to differences in income,
occupation, and educational status.
Signs and symptoms
a. Angina
The most prevalent CHD symptom is angina pectoris/chest pain. Approximately thirty
percent of adults who present o the emergency department with an unclear cause of pain, the
pain is often attributed to CHD (Kontos, Diercks, & Kirk, 2013). Angina is also described as
“chest discomfort, heaviness, tightness, pressure, aching, burning, numbness, fullness, or
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CORONARY HEART DISEASE 10
squeezing” (WebMD, 2017). It is often felt in the chest but may radiate to other parts
including the shoulder, arms, neck or jaw. Angina results from the partial blockage of
coronary arteries. This symptom is usually triggered by physical activity or emotional
distress.
Angina may present in any of its variants. Stable angina is characterised by a short-term
discomfort resembling indigestion. A stable angina occurs when the heart is working harder
than usual such as in an event of physical activity. It has a regular pattern. Unstable angina,
on the other hand, occurs during rest, it is severe, last longer, and often worsens with time. It
is referred to as unstable owing to the changes in intensity, character, and frequency.
b. Dyspnoea
Shortness of breath may also result from the heart’s incapacity to pump adequate blood to
meet the body’s demands. This symptom may also be accompanied with extreme fatigue with
exertion.
c. Myocardial infarction (MI)
Heart attacks result if the arteries become completely blocked. Myocardial infarctions can
cause permanent damage to the heart muscles if they are not treated immediately, and can
also be fatal. Signs and symptoms of an MI include chest discomfort, dyspnoea, light-
headedness, sweating, nausea.
Investigations and tests
a) Electrocardiogram
squeezing” (WebMD, 2017). It is often felt in the chest but may radiate to other parts
including the shoulder, arms, neck or jaw. Angina results from the partial blockage of
coronary arteries. This symptom is usually triggered by physical activity or emotional
distress.
Angina may present in any of its variants. Stable angina is characterised by a short-term
discomfort resembling indigestion. A stable angina occurs when the heart is working harder
than usual such as in an event of physical activity. It has a regular pattern. Unstable angina,
on the other hand, occurs during rest, it is severe, last longer, and often worsens with time. It
is referred to as unstable owing to the changes in intensity, character, and frequency.
b. Dyspnoea
Shortness of breath may also result from the heart’s incapacity to pump adequate blood to
meet the body’s demands. This symptom may also be accompanied with extreme fatigue with
exertion.
c. Myocardial infarction (MI)
Heart attacks result if the arteries become completely blocked. Myocardial infarctions can
cause permanent damage to the heart muscles if they are not treated immediately, and can
also be fatal. Signs and symptoms of an MI include chest discomfort, dyspnoea, light-
headedness, sweating, nausea.
Investigations and tests
a) Electrocardiogram
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CORONARY HEART DISEASE 11
Electrocardiogram (ECG or EKG) detects and records the heart's electrical activity. An
ECG shows the heart beat rate, its rhythm, and also the strength and timing of electrical
signals passing through the heart (Saint Thomas Health, 2015).
b) Echocardiography (echo)
Echo is a procedure that uses sound waves for the evaluation o he heart’s structure and
function. Echo provides information on the systolic and diastolic function, condition and
function of valves, contractility, can also measure the pressure of pulmonary vessels (Heart
Foundation, 2014).
c) Stress testing
Stress testing is done with heart stimulation, using either exercise on a treadmill, with a
connection to an ECG. Stress testing helps identify possible signs and symptoms of CHD
including myocardial ischaemia, electrical instability or any other signs and symptoms related
to exertion (dyspnoea, abnormal changes in blood pressure and heart rate) (Garber, Hlatky,
Chareonthaitawee, & Askew, 2017). Stress testing can also be induced using medications in
cases where the patient cannot endure exercise tests.
d) Coronary angiography
It is the most accurate way of defining the presence and severity of CHD. The process
investigates the integrity of the coronary arteries by inserting a catheter into the coronary
vasculature and the use of a contrast medium to produce images. Coronary angiography
yields information on the extent of the vessel narrowing an also the culprit lesions (Gorenoi,
SchönermarK, & Hagen, 2012). This information is vital for the treatment and management
of the presentation.
Electrocardiogram (ECG or EKG) detects and records the heart's electrical activity. An
ECG shows the heart beat rate, its rhythm, and also the strength and timing of electrical
signals passing through the heart (Saint Thomas Health, 2015).
b) Echocardiography (echo)
Echo is a procedure that uses sound waves for the evaluation o he heart’s structure and
function. Echo provides information on the systolic and diastolic function, condition and
function of valves, contractility, can also measure the pressure of pulmonary vessels (Heart
Foundation, 2014).
c) Stress testing
Stress testing is done with heart stimulation, using either exercise on a treadmill, with a
connection to an ECG. Stress testing helps identify possible signs and symptoms of CHD
including myocardial ischaemia, electrical instability or any other signs and symptoms related
to exertion (dyspnoea, abnormal changes in blood pressure and heart rate) (Garber, Hlatky,
Chareonthaitawee, & Askew, 2017). Stress testing can also be induced using medications in
cases where the patient cannot endure exercise tests.
d) Coronary angiography
It is the most accurate way of defining the presence and severity of CHD. The process
investigates the integrity of the coronary arteries by inserting a catheter into the coronary
vasculature and the use of a contrast medium to produce images. Coronary angiography
yields information on the extent of the vessel narrowing an also the culprit lesions (Gorenoi,
SchönermarK, & Hagen, 2012). This information is vital for the treatment and management
of the presentation.
CORONARY HEART DISEASE 12
e) Chest X-Ray (CXR)
A chest x-ray aid in the investigation of the cause of dyspnoea (cardiac or respiratory) (Heart
Foundation, 2014). A CXR can help reveal causes of symptoms of CHD, alongside lung
disorders.
f) Blood Tests
Blood tests may also be carried out to check the levels of cholesterol, glucose, proteins, and
fats in the body. Abnormal levels are indicative of increased risk for CHD. Recommended
basic screening involves testing for fasting blood glucose, a full blood count, serum lipids
including high-density lipoproteins (HDL) and triglycerides, serum urates and blood urea and
electrolytes (Ministry of Health and Quality of Life; Mauritius Institute of Health; World
Health Organisation, 2015).
g) Ambulatory ECG Monitoring (Holter)
This procedure is used for the detection of abnormal electrical conduction, abnormal cardiac
rhythm, and ischaemic changes even in asymptomatic cases (Galli, Ambrosini, & Lombardi,
2016).
h) Thallium Scan
Thallium is a radioactive substance which is injected into a vein and then taken up by cardiac
muscles. In the case of narrowed coronary arteries, less thallium reaches the muscles (Saint
Thomas Health, 2015). This procedure helps detect significant coronary artery narrowing,
and also damage to cardiac muscles due to a heart attack.
i) Cardiac Magnetic Resonance (Cardiac MR)
e) Chest X-Ray (CXR)
A chest x-ray aid in the investigation of the cause of dyspnoea (cardiac or respiratory) (Heart
Foundation, 2014). A CXR can help reveal causes of symptoms of CHD, alongside lung
disorders.
f) Blood Tests
Blood tests may also be carried out to check the levels of cholesterol, glucose, proteins, and
fats in the body. Abnormal levels are indicative of increased risk for CHD. Recommended
basic screening involves testing for fasting blood glucose, a full blood count, serum lipids
including high-density lipoproteins (HDL) and triglycerides, serum urates and blood urea and
electrolytes (Ministry of Health and Quality of Life; Mauritius Institute of Health; World
Health Organisation, 2015).
g) Ambulatory ECG Monitoring (Holter)
This procedure is used for the detection of abnormal electrical conduction, abnormal cardiac
rhythm, and ischaemic changes even in asymptomatic cases (Galli, Ambrosini, & Lombardi,
2016).
h) Thallium Scan
Thallium is a radioactive substance which is injected into a vein and then taken up by cardiac
muscles. In the case of narrowed coronary arteries, less thallium reaches the muscles (Saint
Thomas Health, 2015). This procedure helps detect significant coronary artery narrowing,
and also damage to cardiac muscles due to a heart attack.
i) Cardiac Magnetic Resonance (Cardiac MR)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




