PUBH6003: Health System and Economics - Cost Benefit Analysis Report
VerifiedAdded on 2022/09/29
|5
|1197
|24
Report
AI Summary
This report provides an overview of health economics, focusing on cost-benefit analysis (CBA) and cost-effectiveness analysis (CEA) in healthcare. It explains how CBA compares health strategies using monetary terms, including discrete choice experiments and willingness to pay surveys. The report highlights the use of CBA in assessing interventions like infrastructure development and discusses input types such as costs and benefits. It explores methods like the value of a statistical life (VSL) and provides a case study of Colombia's health expenditure, comparing universal health insurance to private insurance. The report further explains CEA, contrasting new interventions with current practices and emphasizing sectoral cost-effective analysis for resource allocation. It also addresses the importance of financial sustainability in healthcare systems, using Colombia as an example, and suggests strategies to strengthen health system performance through primary care improvements and early detection programs.

Running head: PUBH6003 1
Health System and Economics
(Author’s name)
(Institutional Affiliation)
Health System and Economics
(Author’s name)
(Institutional Affiliation)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBH6003 2
In healthcare economics, cost-benefit analysis(CBA) is determined by comparing various
types of health strategies and their impacts which has both benefits and cost outcomes that are
usually expressed in monetary terms (S. I. Prada, Duarte, & Guerrero, 2015)This makes it
possible to compare several treatment interventions that can be used alternatively using the net
monetary benefit that is usually calculated by obtaining the difference between the benefits of
each treatment minus each cost. In most cases, discrete choice experiments(DCES) and
willingness to pay (WTP) surveys are the basic strategies used in CBA monetary evaluation.
This is due to the fact that there may be difficulties in associating some health outcomes such as
increased life span with monetary value(Juan López, Martínez Valle, & Aguilera, 2015). The
most common areas that CBA is used in healthcare is to assess interventions that increase access
services, waiting times reduction or improvement and development of infrastructure including
new hospitals.
There are two major types of inputs that are included in cost-benefit analysis. These
include the costs used in implementing a healthcare intervention and the benefits from those
interventions(CDC, 2019). The benefits include things such as medical cost averted, health
improvements in terms of monetary value and productivity gains calculated in terms of liquid
cash saved. The monetary evaluation of health benefits can be calculated using other methods
such as the value of a statistical life (VSL).(CDC, 2019) This method suggests that valuing one
saved life means finding an equivalent amount of money that someone is willing to accept for the
extra risk in an intervention that might lead to death. All benefits are calculated in each
intervention less than the cost in each to find the net cost-benefit analysis. CBA assumes that, if
an intervention uses less money, then there would be no reason for trying it out(CDC, 2019). For
instance, Colombia total health expenditure in 2012 was 6.8% of the total budget. Per capital
In healthcare economics, cost-benefit analysis(CBA) is determined by comparing various
types of health strategies and their impacts which has both benefits and cost outcomes that are
usually expressed in monetary terms (S. I. Prada, Duarte, & Guerrero, 2015)This makes it
possible to compare several treatment interventions that can be used alternatively using the net
monetary benefit that is usually calculated by obtaining the difference between the benefits of
each treatment minus each cost. In most cases, discrete choice experiments(DCES) and
willingness to pay (WTP) surveys are the basic strategies used in CBA monetary evaluation.
This is due to the fact that there may be difficulties in associating some health outcomes such as
increased life span with monetary value(Juan López, Martínez Valle, & Aguilera, 2015). The
most common areas that CBA is used in healthcare is to assess interventions that increase access
services, waiting times reduction or improvement and development of infrastructure including
new hospitals.
There are two major types of inputs that are included in cost-benefit analysis. These
include the costs used in implementing a healthcare intervention and the benefits from those
interventions(CDC, 2019). The benefits include things such as medical cost averted, health
improvements in terms of monetary value and productivity gains calculated in terms of liquid
cash saved. The monetary evaluation of health benefits can be calculated using other methods
such as the value of a statistical life (VSL).(CDC, 2019) This method suggests that valuing one
saved life means finding an equivalent amount of money that someone is willing to accept for the
extra risk in an intervention that might lead to death. All benefits are calculated in each
intervention less than the cost in each to find the net cost-benefit analysis. CBA assumes that, if
an intervention uses less money, then there would be no reason for trying it out(CDC, 2019). For
instance, Colombia total health expenditure in 2012 was 6.8% of the total budget. Per capital
PUBH6003 3
heath government expenditure was 402 dollars, with a GDP of 5.2%. Through the use of
universal health insurance, the government was able to raise around 80% of the total health
expenditure. The general public had to raise 14.8% only from out of the pocket money. Taking
into account to this, the universal health insurance has more cost benefit as compared to private
insurance(S. I. Prada et al., 2015).
On the other hand, the cost-effective analysis (CEA)evaluate the health effects and costs
of certain specific new interventions comparing with the current practice. In CEA, the estimated
cost and effectiveness of the targeted intervention for trial is compared by either the reported
interventions from researches or by the existing interventions that are in practice using a fixed set
price.The fixed cut of point is usually derived from Individuals’ willingness to pay for extra
health units provided(C. Prada & Chaves, 2019). The sectoral cost-effective analysis review
wide cost-effective perspectives using allocation of fixed health budgets to maximize the well-
being of a community. In this case, a number of curative, rehabilitative, and preventive strategies
that have benefits to various groups of individuals in a given population are compared to come
up with several interventions that produce maximum benefits.(Cost-Benefit Analysis, 2016)
However, sectoral cost-effective analysis can only be done at the national or regional level.
When evaluating the cost-effective analysis at a national level, more broadened policies
are used. This involves employing strategies that allocate resources that are used across a number
of interventions and in various population groups to provide an overall high level of population
healthcare.(WHO,2013) For instance, if calculations indicate that the current strategies are more
costly and number of interventions are not maximumly utilized, the available resources can be
distributed across all strategies to improve health outcomes . Although cost-effective analysis
majorly deals with allocation of resources, it is always better to include analysis that determines
heath government expenditure was 402 dollars, with a GDP of 5.2%. Through the use of
universal health insurance, the government was able to raise around 80% of the total health
expenditure. The general public had to raise 14.8% only from out of the pocket money. Taking
into account to this, the universal health insurance has more cost benefit as compared to private
insurance(S. I. Prada et al., 2015).
On the other hand, the cost-effective analysis (CEA)evaluate the health effects and costs
of certain specific new interventions comparing with the current practice. In CEA, the estimated
cost and effectiveness of the targeted intervention for trial is compared by either the reported
interventions from researches or by the existing interventions that are in practice using a fixed set
price.The fixed cut of point is usually derived from Individuals’ willingness to pay for extra
health units provided(C. Prada & Chaves, 2019). The sectoral cost-effective analysis review
wide cost-effective perspectives using allocation of fixed health budgets to maximize the well-
being of a community. In this case, a number of curative, rehabilitative, and preventive strategies
that have benefits to various groups of individuals in a given population are compared to come
up with several interventions that produce maximum benefits.(Cost-Benefit Analysis, 2016)
However, sectoral cost-effective analysis can only be done at the national or regional level.
When evaluating the cost-effective analysis at a national level, more broadened policies
are used. This involves employing strategies that allocate resources that are used across a number
of interventions and in various population groups to provide an overall high level of population
healthcare.(WHO,2013) For instance, if calculations indicate that the current strategies are more
costly and number of interventions are not maximumly utilized, the available resources can be
distributed across all strategies to improve health outcomes . Although cost-effective analysis
majorly deals with allocation of resources, it is always better to include analysis that determines
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PUBH6003 4
the allocation efficiency of the reallocated resources. The process can be evaluated alongside
other social objectives and any considered constraints among decision and policy-makers.
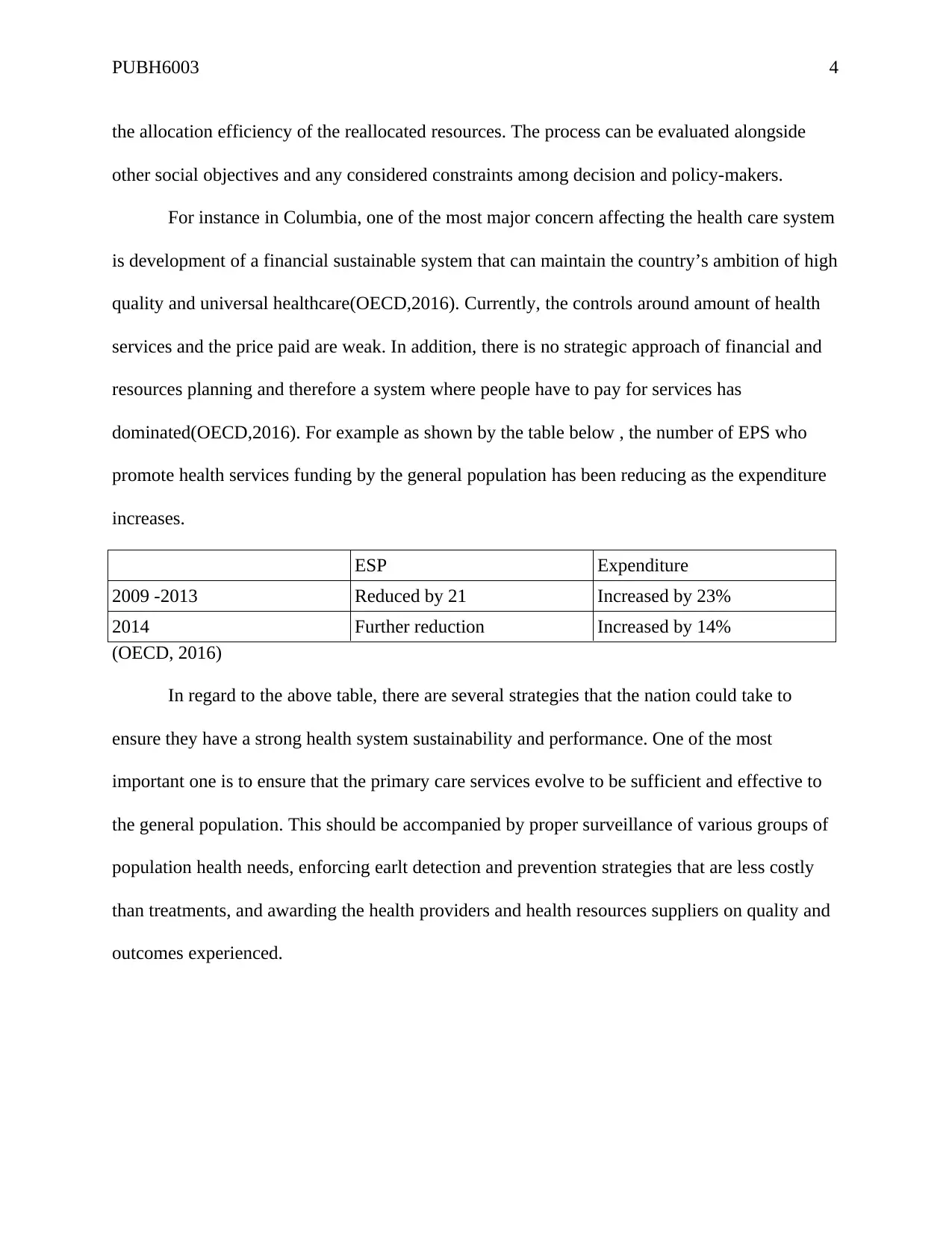
For instance in Columbia, one of the most major concern affecting the health care system
is development of a financial sustainable system that can maintain the country’s ambition of high
quality and universal healthcare(OECD,2016). Currently, the controls around amount of health
services and the price paid are weak. In addition, there is no strategic approach of financial and
resources planning and therefore a system where people have to pay for services has
dominated(OECD,2016). For example as shown by the table below , the number of EPS who
promote health services funding by the general population has been reducing as the expenditure
increases.
ESP Expenditure
2009 -2013 Reduced by 21 Increased by 23%
2014 Further reduction Increased by 14%
(OECD, 2016)
In regard to the above table, there are several strategies that the nation could take to
ensure they have a strong health system sustainability and performance. One of the most
important one is to ensure that the primary care services evolve to be sufficient and effective to
the general population. This should be accompanied by proper surveillance of various groups of
population health needs, enforcing earlt detection and prevention strategies that are less costly
than treatments, and awarding the health providers and health resources suppliers on quality and
outcomes experienced.
the allocation efficiency of the reallocated resources. The process can be evaluated alongside
other social objectives and any considered constraints among decision and policy-makers.
For instance in Columbia, one of the most major concern affecting the health care system
is development of a financial sustainable system that can maintain the country’s ambition of high
quality and universal healthcare(OECD,2016). Currently, the controls around amount of health
services and the price paid are weak. In addition, there is no strategic approach of financial and
resources planning and therefore a system where people have to pay for services has
dominated(OECD,2016). For example as shown by the table below , the number of EPS who
promote health services funding by the general population has been reducing as the expenditure
increases.
ESP Expenditure
2009 -2013 Reduced by 21 Increased by 23%
2014 Further reduction Increased by 14%
(OECD, 2016)
In regard to the above table, there are several strategies that the nation could take to
ensure they have a strong health system sustainability and performance. One of the most
important one is to ensure that the primary care services evolve to be sufficient and effective to
the general population. This should be accompanied by proper surveillance of various groups of
population health needs, enforcing earlt detection and prevention strategies that are less costly
than treatments, and awarding the health providers and health resources suppliers on quality and
outcomes experienced.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBH6003 5
References.
CDC. (2019). Cost-Benefit Analysis. Retrieved August 16, 2019, from
https://www.cdc.gov/policy/polaris/economics/cost-benefit-analysis.html
Cost-Benefit Analysis. (2016). York; York Health Economics Consortium; 2016.
https://www.yhec.co.uk/glossary/cost-benefit-analysis/
OECD, (2016)OECD Reviews« Back to Glossary Index of Health Systems: Colombia
2016 .Assessment and recommendations
DOI:https://dx.doi.org/10.1787/9789264248908-4-en
WHO,(2013) WHO GUIDE TOCOST-EFFECTIVENESS ANALYSIS, Retrieved from https://
www.who.int/choice/publications/p_2003_generalised_cea.pdf
Prada, C., & Chaves, S. (2019). Health system structure and transformations in Colombia
between 1990 and 2013: a socio-historical study. Critical Public Health, 29(3), 314–324.
https://doi.org/10.1080/09581596.2018.1449943
Prada, S. I., Duarte, J. L., & Guerrero, R. (2015). Out-of-pocket health expenditure for poor and
non-poor older adults in Colombia: Composition and trends. International Journal of
Consumer Studies, 39(4), 362–368. https://doi.org/10.1111/ijcs.12203
References.
CDC. (2019). Cost-Benefit Analysis. Retrieved August 16, 2019, from
https://www.cdc.gov/policy/polaris/economics/cost-benefit-analysis.html
Cost-Benefit Analysis. (2016). York; York Health Economics Consortium; 2016.
https://www.yhec.co.uk/glossary/cost-benefit-analysis/
OECD, (2016)OECD Reviews« Back to Glossary Index of Health Systems: Colombia
2016 .Assessment and recommendations
DOI:https://dx.doi.org/10.1787/9789264248908-4-en
WHO,(2013) WHO GUIDE TOCOST-EFFECTIVENESS ANALYSIS, Retrieved from https://
www.who.int/choice/publications/p_2003_generalised_cea.pdf
Prada, C., & Chaves, S. (2019). Health system structure and transformations in Colombia
between 1990 and 2013: a socio-historical study. Critical Public Health, 29(3), 314–324.
https://doi.org/10.1080/09581596.2018.1449943
Prada, S. I., Duarte, J. L., & Guerrero, R. (2015). Out-of-pocket health expenditure for poor and
non-poor older adults in Colombia: Composition and trends. International Journal of
Consumer Studies, 39(4), 362–368. https://doi.org/10.1111/ijcs.12203
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





