Analysis: COVID-19 Impact on NHS Patient Care in England, July 2020
VerifiedAdded on 2021/09/02
|8
|2043
|72
Report
AI Summary
This report analyzes the significant impact of the COVID-19 pandemic on the National Health Service (NHS) in England, focusing on the period of April, May, and June 2020. Due to the pandemic, the NHS had to reduce or shut down non-COVID care, leading to a drastic decrease in elective procedures, urgent cancer referrals, first cancer treatments, and outpatient appointments. The report uses NHS England data to estimate the 'missing' activity compared to pre-COVID levels, revealing a substantial backlog of unmet patient needs. It highlights the potential long-term consequences of delayed treatments and diagnoses, emphasizing the need for increased funding, a credible plan for managing the backlog, and support for NHS staff. The BMA estimates that millions of patients have been affected, with up to 1.5 million fewer elective admissions, 2.6 million fewer outpatient attendances, and significant reductions in cancer-related services. The report concludes by stressing the importance of addressing these issues to ensure patient safety and restore the NHS to full operational capacity.
The hidden impact of COVID-19 on
patient care in the NHS in England
July 2020
patient care in the NHS in England
July 2020
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Page 2 of 8
The COVID-19 outbreak has had a huge impact on core NHS services. In order to free up enough
capacity to deal with the initial peak of the pandemic, the NHS was forced to shut down or
significantly reduce many areas of non-COVID care during April, May and June 2020.i This, combined
with fewer patients seeking care during lockdown, means that there has been a significant drop in
elective procedures, urgent cancer referrals, first cancer treatments and outpatient appointments.
The full impact of this drastic reduction in routine NHS care in England is only now emerging. Millions
of patients living with health problems (including life-threatening conditions such as cancer) have
been affected, with their treatment postponed or cancelled. And millions of patients will have missed
vital opportunities to receive initial assessment and diagnosis for health problems in the first place.
This is the hidden impact of the COVID crisis – patient safety is being severely compromised not just
by the virus itself, but by the knock-on effects of an unprecedented disruption to NHS services.
The BMA estimates that in April, May and June 2020 in England there were:
– between 1.32 and 1.50 million fewer elective admissions than would usually be expected
– between 2.47 million and 2.60 million fewer first outpatient attendances
– between 274,000 and 286,000 fewer urgent cancer referrals
– between 20,800 and 25,900 fewer patients starting first cancer treatments following a
decision to treat
– between 12,000 and 15,000 fewer patients starting first cancer treatments following an
urgent GP referral.
This outcome was avoidable. Although a pandemic on the scale of COVID-19 was always likely to
cause major disruption to health services, the drastic extent to which the NHS had to shut down
routine care is a consequence of over a decade of underinvestment and (in the case of public health
and social care) cuts to services. As a result, NHS capacity has lagged behind many other EU
countries, including in terms of bed numbers, critical care facilities, workforce numbers (with 10,000
medical vacancies in the NHS in England in 2019) and resources in primary and community care. The
NHS was already in crisis before the pandemic hit, as the BMA consistently warned.
As the NHS begins the vital task of reopening non-COVID services, it now faces a huge backlog of
unmet patient need, with patients now facing long waits for treatment. The commitment made by
the Chancellor of the Exchequer in March to give the NHS ‘whatever it needs’ to tackle the pandemic
must not end as the initial peak of the virus recedes. The NHS needs:
– honesty and clarity from government about the size of the backlog and how it is going to be
managed – in real practical terms
– assurances that there is a credible plan in place to the NHS through this incredibly difficult
period, including increasing funding for the coming years above previous spending plans
– a package of support for NHS staff, who have consistently gone ‘above and beyond’ so far
during the crisis.
The BMA has set out more detailed recommendations on restarting non-COVID care here.
The COVID-19 outbreak has had a huge impact on core NHS services. In order to free up enough
capacity to deal with the initial peak of the pandemic, the NHS was forced to shut down or
significantly reduce many areas of non-COVID care during April, May and June 2020.i This, combined
with fewer patients seeking care during lockdown, means that there has been a significant drop in
elective procedures, urgent cancer referrals, first cancer treatments and outpatient appointments.
The full impact of this drastic reduction in routine NHS care in England is only now emerging. Millions
of patients living with health problems (including life-threatening conditions such as cancer) have
been affected, with their treatment postponed or cancelled. And millions of patients will have missed
vital opportunities to receive initial assessment and diagnosis for health problems in the first place.
This is the hidden impact of the COVID crisis – patient safety is being severely compromised not just
by the virus itself, but by the knock-on effects of an unprecedented disruption to NHS services.
The BMA estimates that in April, May and June 2020 in England there were:
– between 1.32 and 1.50 million fewer elective admissions than would usually be expected
– between 2.47 million and 2.60 million fewer first outpatient attendances
– between 274,000 and 286,000 fewer urgent cancer referrals
– between 20,800 and 25,900 fewer patients starting first cancer treatments following a
decision to treat
– between 12,000 and 15,000 fewer patients starting first cancer treatments following an
urgent GP referral.
This outcome was avoidable. Although a pandemic on the scale of COVID-19 was always likely to
cause major disruption to health services, the drastic extent to which the NHS had to shut down
routine care is a consequence of over a decade of underinvestment and (in the case of public health
and social care) cuts to services. As a result, NHS capacity has lagged behind many other EU
countries, including in terms of bed numbers, critical care facilities, workforce numbers (with 10,000
medical vacancies in the NHS in England in 2019) and resources in primary and community care. The
NHS was already in crisis before the pandemic hit, as the BMA consistently warned.
As the NHS begins the vital task of reopening non-COVID services, it now faces a huge backlog of
unmet patient need, with patients now facing long waits for treatment. The commitment made by
the Chancellor of the Exchequer in March to give the NHS ‘whatever it needs’ to tackle the pandemic
must not end as the initial peak of the virus recedes. The NHS needs:
– honesty and clarity from government about the size of the backlog and how it is going to be
managed – in real practical terms
– assurances that there is a credible plan in place to the NHS through this incredibly difficult
period, including increasing funding for the coming years above previous spending plans
– a package of support for NHS staff, who have consistently gone ‘above and beyond’ so far
during the crisis.
The BMA has set out more detailed recommendations on restarting non-COVID care here.
Page 3 of 8
Background
The COVID-19 pandemic led to an extensive shift in the package of care provided by the NHS as
hospitals had to prepare for a large surge in patients requiring intensive care. With services already
under severe strain and functioning at maximum capacity in early 2020, unprecedented steps were
needed to ensure COVID-19 care was not rationed and the NHS did not become overwhelmed.
Sir Simon Stevens wrote to NHS bodies on 17 March to notify them that significant amounts of
capacity would have to immediately be created by cancelling planned operations, large numbers of
patients being discharged back into the community, and non-COVID-19 patients and staff conducting
GP consultations remotely.1
Whilst these changes meant that intensive care did not have to be rationed to COVID-19 patients,
data indicates that the shutdown of most non-COVID services, combined with drastic changes in
patient behaviour, mean the NHS is now facing a large backlog of non-COVID-19 care, storing up
greater problems for the future. This paper investigates the extent to which non-COVID care has
been disrupted over April, May and June 2020, and the likely impact this will have in the longer term.
BMA analysis
We used NHS England data to estimate the gap between NHS care provided during the pandemic
and the pre-COVID ‘norm’. To understand what level of activity would usually (pre-COVID) be
expected, we looked at data from the same period in 2018 and 2019.
We chose to focus on how many urgent GP cancer referrals, elective general & acute admissions,
first cancer treatments, and first general & acute outpatient attendances have not taken place during
the epidemic that we would usually have expected. Data is currently available for the months of April
and May 2020 – we therefore compared the activity recorded during these months in 2020 to the
average recorded during the same months in 2018 and 2019. We estimated ‘worst’ and ‘best’ case
scenarios for what activity may have been like in June based on the level activity was at in April and
May, a statement from Sir Simon Stevens, and our own surveys of BMA members (see Table 1).
1 https://www.england.nhs.uk/coronavirus/publication/next-steps-on-nhs-response-to-COVID-19-letter-from-
simon-stevens-and-amanda-pritchard/
Background
The COVID-19 pandemic led to an extensive shift in the package of care provided by the NHS as
hospitals had to prepare for a large surge in patients requiring intensive care. With services already
under severe strain and functioning at maximum capacity in early 2020, unprecedented steps were
needed to ensure COVID-19 care was not rationed and the NHS did not become overwhelmed.
Sir Simon Stevens wrote to NHS bodies on 17 March to notify them that significant amounts of
capacity would have to immediately be created by cancelling planned operations, large numbers of
patients being discharged back into the community, and non-COVID-19 patients and staff conducting
GP consultations remotely.1
Whilst these changes meant that intensive care did not have to be rationed to COVID-19 patients,
data indicates that the shutdown of most non-COVID services, combined with drastic changes in
patient behaviour, mean the NHS is now facing a large backlog of non-COVID-19 care, storing up
greater problems for the future. This paper investigates the extent to which non-COVID care has
been disrupted over April, May and June 2020, and the likely impact this will have in the longer term.
BMA analysis
We used NHS England data to estimate the gap between NHS care provided during the pandemic
and the pre-COVID ‘norm’. To understand what level of activity would usually (pre-COVID) be
expected, we looked at data from the same period in 2018 and 2019.
We chose to focus on how many urgent GP cancer referrals, elective general & acute admissions,
first cancer treatments, and first general & acute outpatient attendances have not taken place during
the epidemic that we would usually have expected. Data is currently available for the months of April
and May 2020 – we therefore compared the activity recorded during these months in 2020 to the
average recorded during the same months in 2018 and 2019. We estimated ‘worst’ and ‘best’ case
scenarios for what activity may have been like in June based on the level activity was at in April and
May, a statement from Sir Simon Stevens, and our own surveys of BMA members (see Table 1).
1 https://www.england.nhs.uk/coronavirus/publication/next-steps-on-nhs-response-to-COVID-19-letter-from-
simon-stevens-and-amanda-pritchard/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Page 4 of 8
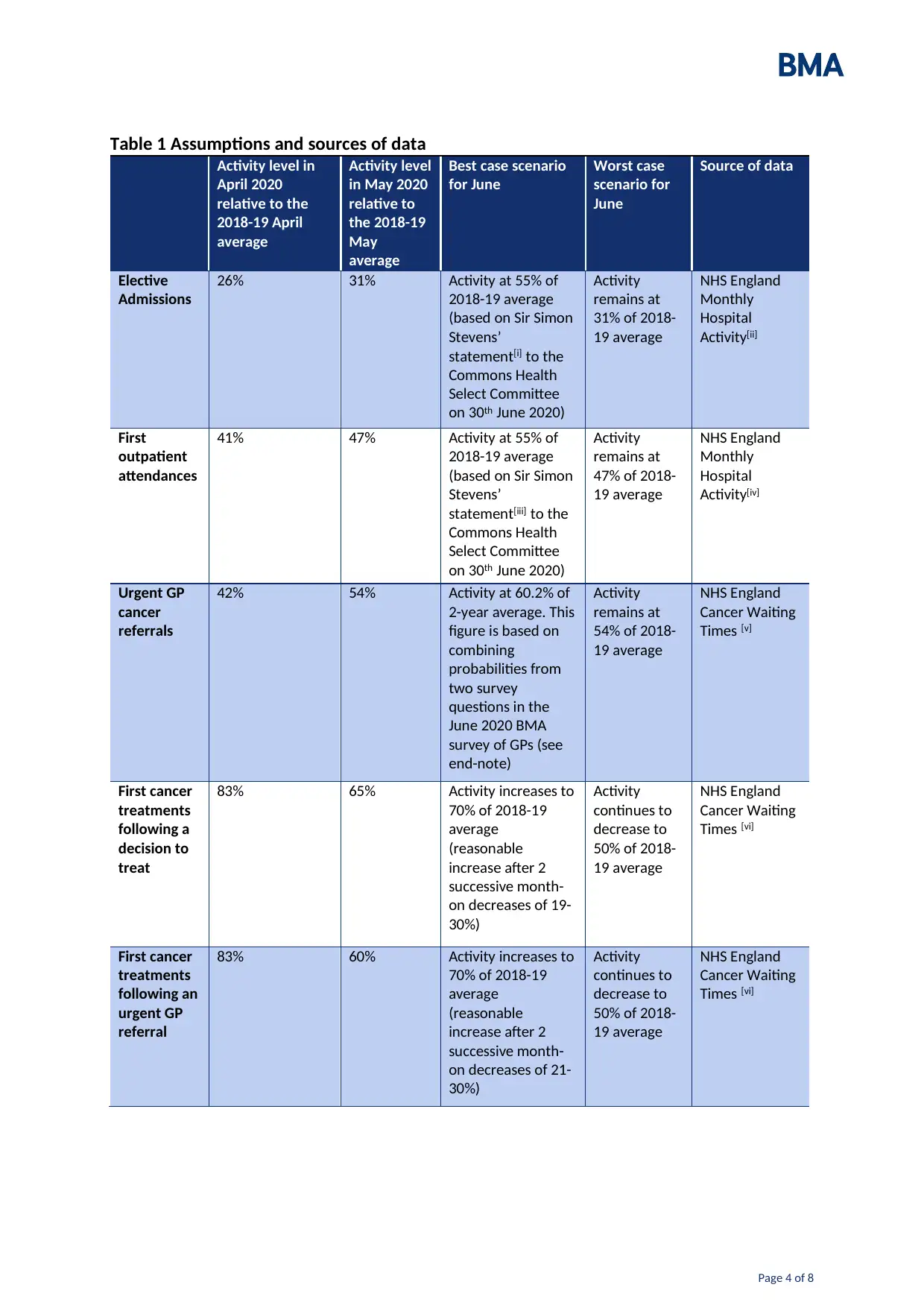
Table 1 Assumptions and sources of data
Activity level in
April 2020
relative to the
2018-19 April
average
Activity level
in May 2020
relative to
the 2018-19
May
average
Best case scenario
for June
Worst case
scenario for
June
Source of data
Elective
Admissions
26% 31% Activity at 55% of
2018-19 average
(based on Sir Simon
Stevens’
statement[i] to the
Commons Health
Select Committee
on 30th June 2020)
Activity
remains at
31% of 2018-
19 average
NHS England
Monthly
Hospital
Activity[ii]
First
outpatient
attendances
41% 47% Activity at 55% of
2018-19 average
(based on Sir Simon
Stevens’
statement[iii] to the
Commons Health
Select Committee
on 30th June 2020)
Activity
remains at
47% of 2018-
19 average
NHS England
Monthly
Hospital
Activity[iv]
Urgent GP
cancer
referrals
42% 54% Activity at 60.2% of
2-year average. This
figure is based on
combining
probabilities from
two survey
questions in the
June 2020 BMA
survey of GPs (see
end-note)
Activity
remains at
54% of 2018-
19 average
NHS England
Cancer Waiting
Times [v]
First cancer
treatments
following a
decision to
treat
83% 65% Activity increases to
70% of 2018-19
average
(reasonable
increase after 2
successive month-
on decreases of 19-
30%)
Activity
continues to
decrease to
50% of 2018-
19 average
NHS England
Cancer Waiting
Times [vi]
First cancer
treatments
following an
urgent GP
referral
83% 60% Activity increases to
70% of 2018-19
average
(reasonable
increase after 2
successive month-
on decreases of 21-
30%)
Activity
continues to
decrease to
50% of 2018-
19 average
NHS England
Cancer Waiting
Times [vi]
Table 1 Assumptions and sources of data
Activity level in
April 2020
relative to the
2018-19 April
average
Activity level
in May 2020
relative to
the 2018-19
May
average
Best case scenario
for June
Worst case
scenario for
June
Source of data
Elective
Admissions
26% 31% Activity at 55% of
2018-19 average
(based on Sir Simon
Stevens’
statement[i] to the
Commons Health
Select Committee
on 30th June 2020)
Activity
remains at
31% of 2018-
19 average
NHS England
Monthly
Hospital
Activity[ii]
First
outpatient
attendances
41% 47% Activity at 55% of
2018-19 average
(based on Sir Simon
Stevens’
statement[iii] to the
Commons Health
Select Committee
on 30th June 2020)
Activity
remains at
47% of 2018-
19 average
NHS England
Monthly
Hospital
Activity[iv]
Urgent GP
cancer
referrals
42% 54% Activity at 60.2% of
2-year average. This
figure is based on
combining
probabilities from
two survey
questions in the
June 2020 BMA
survey of GPs (see
end-note)
Activity
remains at
54% of 2018-
19 average
NHS England
Cancer Waiting
Times [v]
First cancer
treatments
following a
decision to
treat
83% 65% Activity increases to
70% of 2018-19
average
(reasonable
increase after 2
successive month-
on decreases of 19-
30%)
Activity
continues to
decrease to
50% of 2018-
19 average
NHS England
Cancer Waiting
Times [vi]
First cancer
treatments
following an
urgent GP
referral
83% 60% Activity increases to
70% of 2018-19
average
(reasonable
increase after 2
successive month-
on decreases of 21-
30%)
Activity
continues to
decrease to
50% of 2018-
19 average
NHS England
Cancer Waiting
Times [vi]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Page 5 of 8
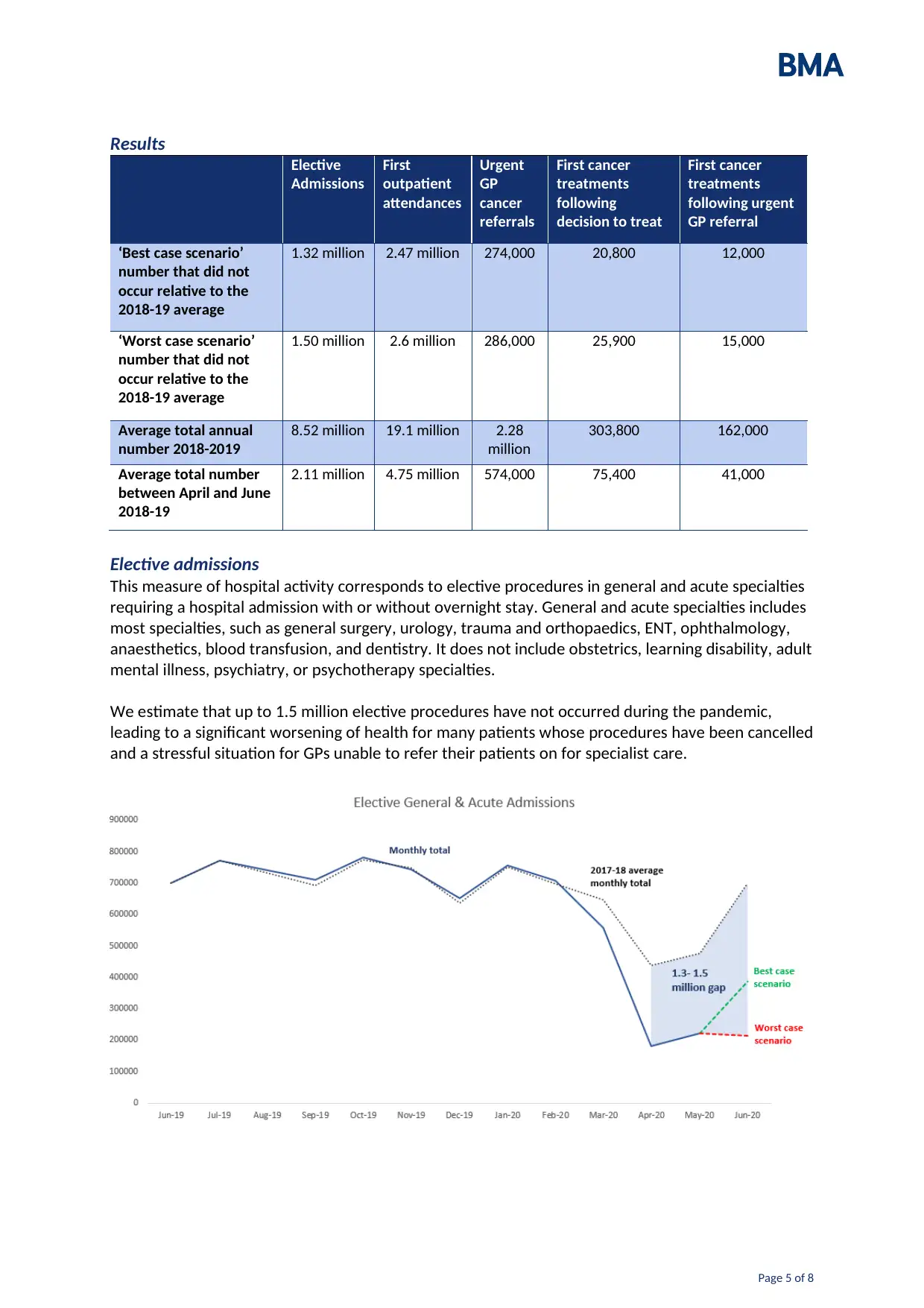
Results
Elective
Admissions
First
outpatient
attendances
Urgent
GP
cancer
referrals
First cancer
treatments
following
decision to treat
First cancer
treatments
following urgent
GP referral
‘Best case scenario’
number that did not
occur relative to the
2018-19 average
1.32 million 2.47 million 274,000 20,800 12,000
‘Worst case scenario’
number that did not
occur relative to the
2018-19 average
1.50 million 2.6 million 286,000 25,900 15,000
Average total annual
number 2018-2019
8.52 million 19.1 million 2.28
million
303,800 162,000
Average total number
between April and June
2018-19
2.11 million 4.75 million 574,000 75,400 41,000
Elective admissions
This measure of hospital activity corresponds to elective procedures in general and acute specialties
requiring a hospital admission with or without overnight stay. General and acute specialties includes
most specialties, such as general surgery, urology, trauma and orthopaedics, ENT, ophthalmology,
anaesthetics, blood transfusion, and dentistry. It does not include obstetrics, learning disability, adult
mental illness, psychiatry, or psychotherapy specialties.
We estimate that up to 1.5 million elective procedures have not occurred during the pandemic,
leading to a significant worsening of health for many patients whose procedures have been cancelled
and a stressful situation for GPs unable to refer their patients on for specialist care.
Results
Elective
Admissions
First
outpatient
attendances
Urgent
GP
cancer
referrals
First cancer
treatments
following
decision to treat
First cancer
treatments
following urgent
GP referral
‘Best case scenario’
number that did not
occur relative to the
2018-19 average
1.32 million 2.47 million 274,000 20,800 12,000
‘Worst case scenario’
number that did not
occur relative to the
2018-19 average
1.50 million 2.6 million 286,000 25,900 15,000
Average total annual
number 2018-2019
8.52 million 19.1 million 2.28
million
303,800 162,000
Average total number
between April and June
2018-19
2.11 million 4.75 million 574,000 75,400 41,000
Elective admissions
This measure of hospital activity corresponds to elective procedures in general and acute specialties
requiring a hospital admission with or without overnight stay. General and acute specialties includes
most specialties, such as general surgery, urology, trauma and orthopaedics, ENT, ophthalmology,
anaesthetics, blood transfusion, and dentistry. It does not include obstetrics, learning disability, adult
mental illness, psychiatry, or psychotherapy specialties.
We estimate that up to 1.5 million elective procedures have not occurred during the pandemic,
leading to a significant worsening of health for many patients whose procedures have been cancelled
and a stressful situation for GPs unable to refer their patients on for specialist care.
Page 6 of 8
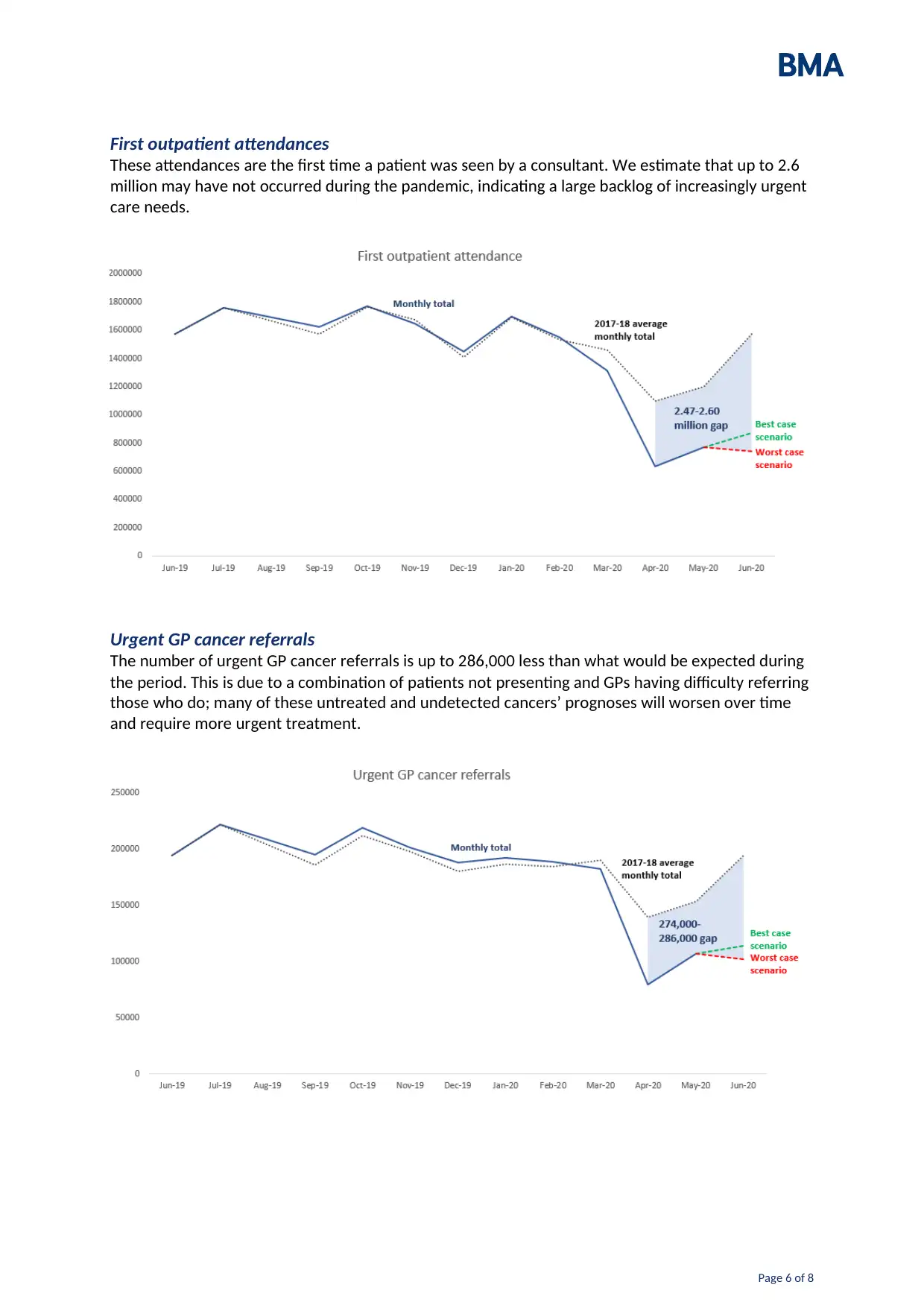
First outpatient attendances
These attendances are the first time a patient was seen by a consultant. We estimate that up to 2.6
million may have not occurred during the pandemic, indicating a large backlog of increasingly urgent
care needs.
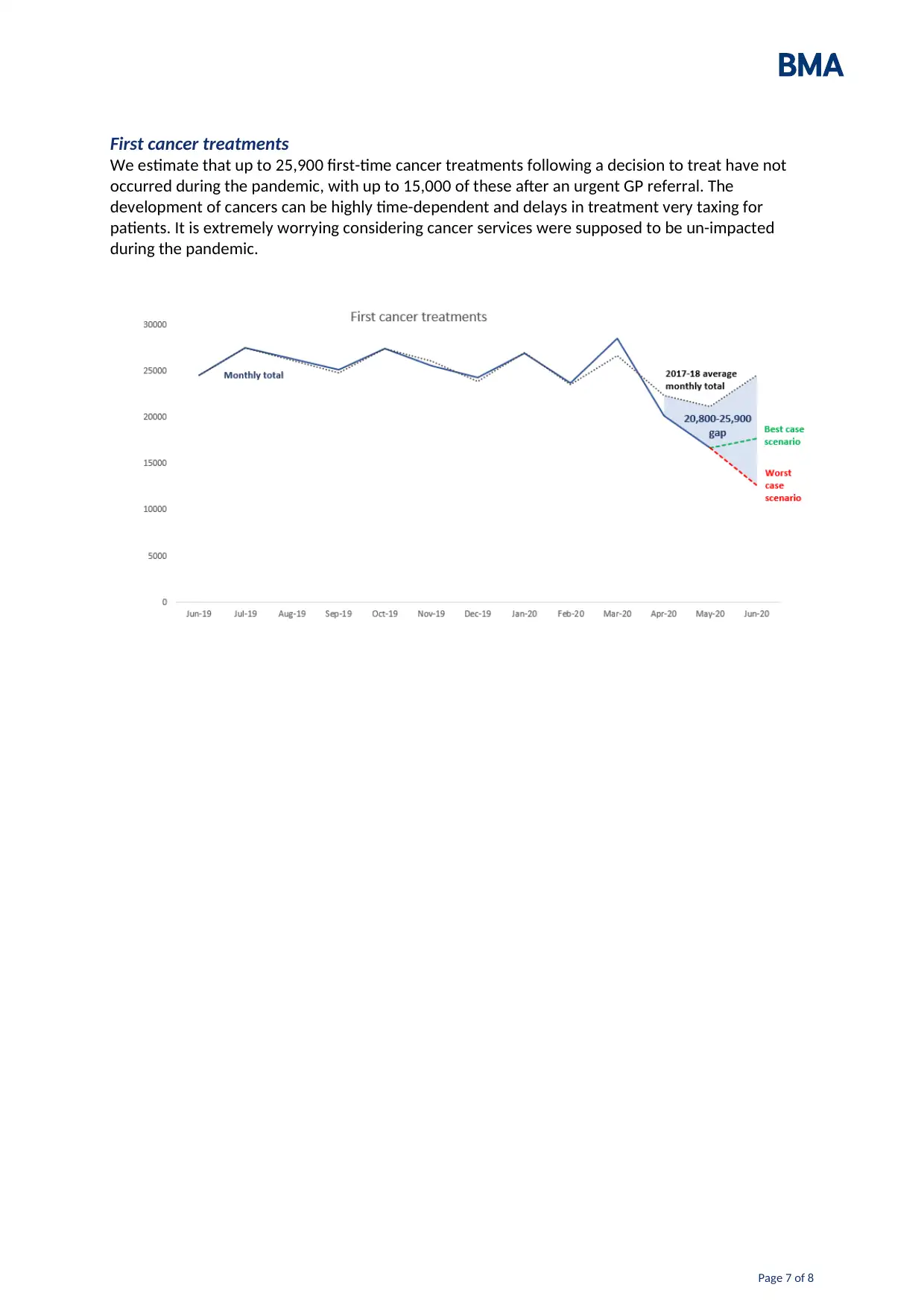
Urgent GP cancer referrals
The number of urgent GP cancer referrals is up to 286,000 less than what would be expected during
the period. This is due to a combination of patients not presenting and GPs having difficulty referring
those who do; many of these untreated and undetected cancers’ prognoses will worsen over time
and require more urgent treatment.
First outpatient attendances
These attendances are the first time a patient was seen by a consultant. We estimate that up to 2.6
million may have not occurred during the pandemic, indicating a large backlog of increasingly urgent
care needs.
Urgent GP cancer referrals
The number of urgent GP cancer referrals is up to 286,000 less than what would be expected during
the period. This is due to a combination of patients not presenting and GPs having difficulty referring
those who do; many of these untreated and undetected cancers’ prognoses will worsen over time
and require more urgent treatment.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Page 7 of 8
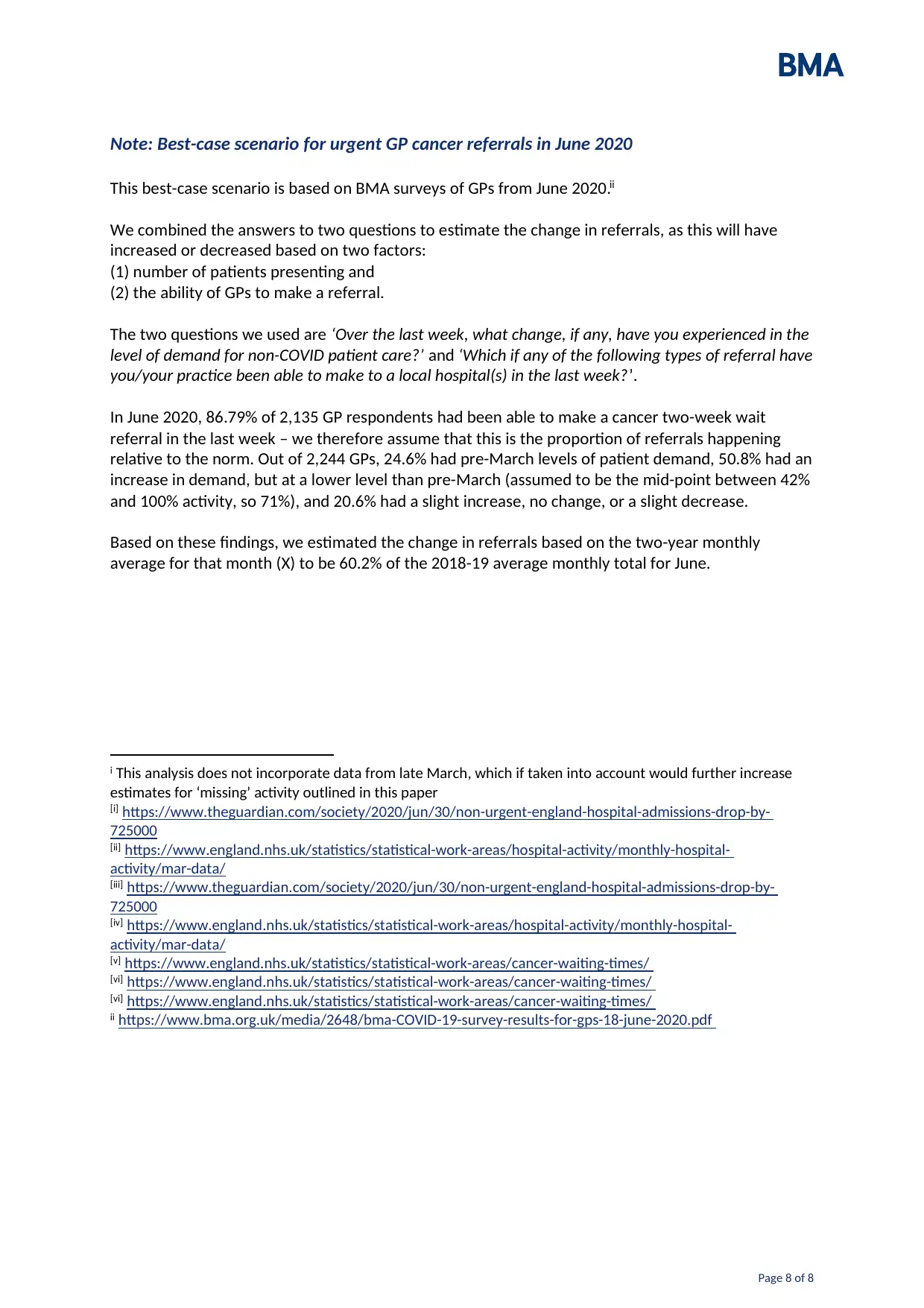
First cancer treatments
We estimate that up to 25,900 first-time cancer treatments following a decision to treat have not
occurred during the pandemic, with up to 15,000 of these after an urgent GP referral. The
development of cancers can be highly time-dependent and delays in treatment very taxing for
patients. It is extremely worrying considering cancer services were supposed to be un-impacted
during the pandemic.
First cancer treatments
We estimate that up to 25,900 first-time cancer treatments following a decision to treat have not
occurred during the pandemic, with up to 15,000 of these after an urgent GP referral. The
development of cancers can be highly time-dependent and delays in treatment very taxing for
patients. It is extremely worrying considering cancer services were supposed to be un-impacted
during the pandemic.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Page 8 of 8
Note: Best-case scenario for urgent GP cancer referrals in June 2020
This best-case scenario is based on BMA surveys of GPs from June 2020.ii
We combined the answers to two questions to estimate the change in referrals, as this will have
increased or decreased based on two factors:
(1) number of patients presenting and
(2) the ability of GPs to make a referral.
The two questions we used are ‘Over the last week, what change, if any, have you experienced in the
level of demand for non-COVID patient care?’ and ‘Which if any of the following types of referral have
you/your practice been able to make to a local hospital(s) in the last week?’.
In June 2020, 86.79% of 2,135 GP respondents had been able to make a cancer two-week wait
referral in the last week – we therefore assume that this is the proportion of referrals happening
relative to the norm. Out of 2,244 GPs, 24.6% had pre-March levels of patient demand, 50.8% had an
increase in demand, but at a lower level than pre-March (assumed to be the mid-point between 42%
and 100% activity, so 71%), and 20.6% had a slight increase, no change, or a slight decrease.
Based on these findings, we estimated the change in referrals based on the two-year monthly
average for that month (X) to be 60.2% of the 2018-19 average monthly total for June.
i This analysis does not incorporate data from late March, which if taken into account would further increase
estimates for ‘missing’ activity outlined in this paper
[i] https://www.theguardian.com/society/2020/jun/30/non-urgent-england-hospital-admissions-drop-by-
725000
[ii] https://www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/monthly-hospital-
activity/mar-data/
[iii] https://www.theguardian.com/society/2020/jun/30/non-urgent-england-hospital-admissions-drop-by-
725000
[iv] https://www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/monthly-hospital-
activity/mar-data/
[v] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
[vi] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
[vi] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
ii https://www.bma.org.uk/media/2648/bma-COVID-19-survey-results-for-gps-18-june-2020.pdf
Note: Best-case scenario for urgent GP cancer referrals in June 2020
This best-case scenario is based on BMA surveys of GPs from June 2020.ii
We combined the answers to two questions to estimate the change in referrals, as this will have
increased or decreased based on two factors:
(1) number of patients presenting and
(2) the ability of GPs to make a referral.
The two questions we used are ‘Over the last week, what change, if any, have you experienced in the
level of demand for non-COVID patient care?’ and ‘Which if any of the following types of referral have
you/your practice been able to make to a local hospital(s) in the last week?’.
In June 2020, 86.79% of 2,135 GP respondents had been able to make a cancer two-week wait
referral in the last week – we therefore assume that this is the proportion of referrals happening
relative to the norm. Out of 2,244 GPs, 24.6% had pre-March levels of patient demand, 50.8% had an
increase in demand, but at a lower level than pre-March (assumed to be the mid-point between 42%
and 100% activity, so 71%), and 20.6% had a slight increase, no change, or a slight decrease.
Based on these findings, we estimated the change in referrals based on the two-year monthly
average for that month (X) to be 60.2% of the 2018-19 average monthly total for June.
i This analysis does not incorporate data from late March, which if taken into account would further increase
estimates for ‘missing’ activity outlined in this paper
[i] https://www.theguardian.com/society/2020/jun/30/non-urgent-england-hospital-admissions-drop-by-
725000
[ii] https://www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/monthly-hospital-
activity/mar-data/
[iii] https://www.theguardian.com/society/2020/jun/30/non-urgent-england-hospital-admissions-drop-by-
725000
[iv] https://www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/monthly-hospital-
activity/mar-data/
[v] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
[vi] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
[vi] https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
ii https://www.bma.org.uk/media/2648/bma-COVID-19-survey-results-for-gps-18-june-2020.pdf
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
