Modern vs. Traditional CPR: A Study on Mortality in Hospital Adults
VerifiedAdded on 2023/06/15
|11
|2847
|61
Report
AI Summary
This report examines the effectiveness of modern CPR devices compared to traditional chest compression CPR techniques in preventing mortality among hospitalized adults experiencing cardiac arrest. The problem's significance lies in the high mortality rates associated with in-hospital cardiac arrests (IHCA) despite advancements in modern technology. Current practices often rely on modern resuscitation devices, but these devices have shown significant injuries to patients without substantial improvement in survival rates compared to traditional methods. Ethical considerations such as futility, withdrawing interventions, and communication also play a role. Based on the analysis of multiple research and non-research articles, the report recommends a shift back to manual CPR techniques due to their lower injury rates, cost-effectiveness, and comparable survival rates. Implementation of this change involves collaboration with nurses, supervisors, and clinical nurse educators, while addressing barriers such as cultural resistance and lack of motivation through education and support. The report concludes that traditional CPR methods offer a viable and efficient alternative for improving outcomes in cardiac arrest cases.

EVIDENCE BASED RESEARCH 1
Evidence Based Research Nursing
Name
Affiliation
Instructor
Date
Evidence Based Research Nursing
Name
Affiliation
Instructor
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED RESEARCH 2
Evidence-Based Research Nursing
A1. Summary
The healthcare problem under study regards the effectiveness of the use of modern CPR
devices versus the use conventional chest compression CPR technique in preventing mortality
amongst hospitalized adults under cardiac arrest. CPR means cardiopulmonary resuscitation. The
procedure is intended to maintain and support circulation and to breathe for an individual with
cardiac arrest. The process aims to preserve and restore breathing, circulation and provide blood
flow and oxygen to the brain, heart and other crucial organs amongst patients under cardiac
arrest. Sudden death can occur if the organs do not receive enough oxygen or blood. There are
different techniques used in carrying out the CPR procedure. Some of the most common
techniques include the traditional chest compression CPR technique as well as the use of the
modern CPR devices, though the effectiveness of each method varies.
A2.The significance of the Problem
The significance of the problem is the need to analyse the survival rates for adult
patients under cardiac in hospitals. In-hospital cardiac arrests (IHCA) is one of the world’s
leading causes of death. According to Raffee et al. (2017, p.26), an estimated 200,000 IHCAs are
reported every year in the US alone, with less 20% of the patients surviving to discharge. Other
economies such as the UK have also recorded low survival rate for adult patients in hospitals
who suffer cardiac arrest. Christ et al. (2014, p.320) report that only 35.4% of the patients
admitted daily for cardiac arrest survive. Amongst developing countries, the mortality rate for
cardiac arrest patients is higher with the majority of the deaths been unwitnessed by the
caregivers. The mortality rates for cardiac arrest patients have been increasing globally despite
developments in the modern technology. There is a need for the development of stringent
Evidence-Based Research Nursing
A1. Summary
The healthcare problem under study regards the effectiveness of the use of modern CPR
devices versus the use conventional chest compression CPR technique in preventing mortality
amongst hospitalized adults under cardiac arrest. CPR means cardiopulmonary resuscitation. The
procedure is intended to maintain and support circulation and to breathe for an individual with
cardiac arrest. The process aims to preserve and restore breathing, circulation and provide blood
flow and oxygen to the brain, heart and other crucial organs amongst patients under cardiac
arrest. Sudden death can occur if the organs do not receive enough oxygen or blood. There are
different techniques used in carrying out the CPR procedure. Some of the most common
techniques include the traditional chest compression CPR technique as well as the use of the
modern CPR devices, though the effectiveness of each method varies.
A2.The significance of the Problem
The significance of the problem is the need to analyse the survival rates for adult
patients under cardiac in hospitals. In-hospital cardiac arrests (IHCA) is one of the world’s
leading causes of death. According to Raffee et al. (2017, p.26), an estimated 200,000 IHCAs are
reported every year in the US alone, with less 20% of the patients surviving to discharge. Other
economies such as the UK have also recorded low survival rate for adult patients in hospitals
who suffer cardiac arrest. Christ et al. (2014, p.320) report that only 35.4% of the patients
admitted daily for cardiac arrest survive. Amongst developing countries, the mortality rate for
cardiac arrest patients is higher with the majority of the deaths been unwitnessed by the
caregivers. The mortality rates for cardiac arrest patients have been increasing globally despite
developments in the modern technology. There is a need for the development of stringent
EVIDENCE BASED RESEARCH 3
guidelines and practices regarding CPR on cardiac arrest patients to help reduce the mortality
rates to the in-hospital adult patients.
A3. The Current Practice
The current practice which relates to the healthcare problem relies on the use of the
modern resuscitation devices. Majority of the clinicians are adopting the use of the new electric
resuscitation devices which are said to attain better perfusion of the heart and brain within
laboratory settings. However, these devices have shown significant injuries to patients with no
substantial improvement in the survival rate compared to the traditional resuscitation methods
which include chest compressions using hands (Smekal, 2013). Some of the most common
devices currently used for resuscitation for patients facing cardiac arrests include the AutoPulse
devices and Lund University Cardiac Assist System (LUCAS) as described by Remino et al.
(2017, P.3).
The LUCAS device is one of the methods which have proved in useful during
percutaneous coronary interventions (PCI). The use of the invention is challenging since the
hands of the rescuer are within the field vision of the angiography. Also, the fluoroscopic x-ray
detectors within the device mandate the rescuers to conduct resuscitation manoeuvers in
nonefficient and uncomfortable positions. The modern device challenges the process of
resuscitation as the height of the cardiac catheterization table is high making the rescuers
position themselves in a way where it would be difficult to conduct an efficient CPR procedure.
These drawbacks relating to the use of the modern CPR procedures particularly the LUCAS
device do not show any substantial reduction in mortality rates for adults hospitalized with
cardiac arrests. The tools are expensive to purchase and maintain, notwithstanding the training
guidelines and practices regarding CPR on cardiac arrest patients to help reduce the mortality
rates to the in-hospital adult patients.
A3. The Current Practice
The current practice which relates to the healthcare problem relies on the use of the
modern resuscitation devices. Majority of the clinicians are adopting the use of the new electric
resuscitation devices which are said to attain better perfusion of the heart and brain within
laboratory settings. However, these devices have shown significant injuries to patients with no
substantial improvement in the survival rate compared to the traditional resuscitation methods
which include chest compressions using hands (Smekal, 2013). Some of the most common
devices currently used for resuscitation for patients facing cardiac arrests include the AutoPulse
devices and Lund University Cardiac Assist System (LUCAS) as described by Remino et al.
(2017, P.3).
The LUCAS device is one of the methods which have proved in useful during
percutaneous coronary interventions (PCI). The use of the invention is challenging since the
hands of the rescuer are within the field vision of the angiography. Also, the fluoroscopic x-ray
detectors within the device mandate the rescuers to conduct resuscitation manoeuvers in
nonefficient and uncomfortable positions. The modern device challenges the process of
resuscitation as the height of the cardiac catheterization table is high making the rescuers
position themselves in a way where it would be difficult to conduct an efficient CPR procedure.
These drawbacks relating to the use of the modern CPR procedures particularly the LUCAS
device do not show any substantial reduction in mortality rates for adults hospitalized with
cardiac arrests. The tools are expensive to purchase and maintain, notwithstanding the training
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED RESEARCH 4
cost as health practitioners need to be trained on how to use the devices (Giraud & Siegenthaler,
2014, p.2).
A4. Ethical Considerations
CPR shares common goals with other health interventions, which is to restore health,
preserve life and relief suffering as well as limiting disability. When initiating and ending
resuscitation, differences in cultural norms and ethical perspectives have to be considered. Some
of the ethical issues that might affect the healthcare organization or the caregiver include matters
pertaining futility, withdrawing or withholding interventions, practicing procedures on the newly
dead as well as communication and palliative care. During cardiac arrest, CPR attempts are
conducted. Rapid decisions have to be made based on the available information which can be
erroneous or incomplete. There is an increasing concern of the high budgets spent on CPR when
mainly the results are analysed based on the high percentage of the death of cardiac arrest
patients (Rubulotta & Rubulotta, 2013, p. 266).
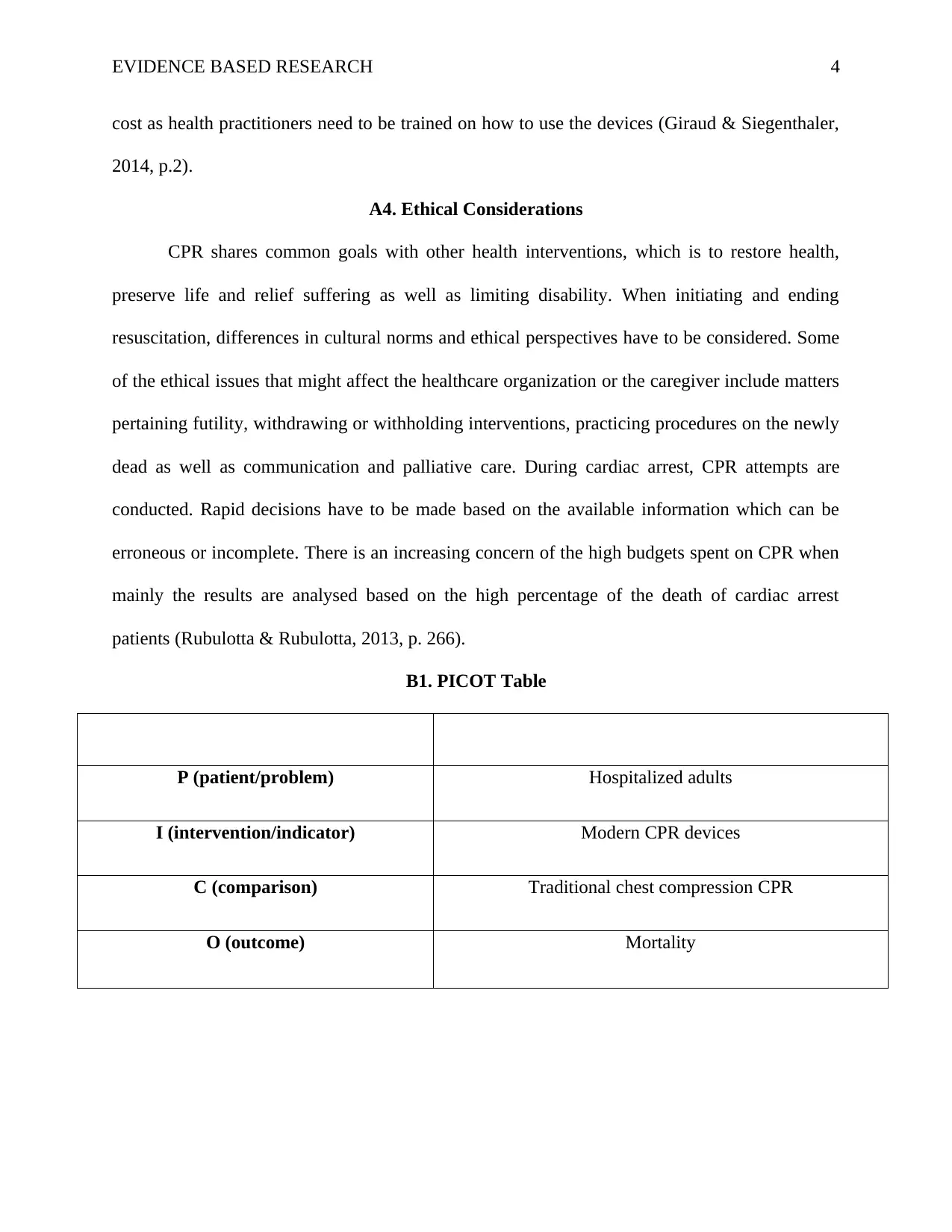
B1. PICOT Table
P (patient/problem) Hospitalized adults
I (intervention/indicator) Modern CPR devices
C (comparison) Traditional chest compression CPR
O (outcome) Mortality
cost as health practitioners need to be trained on how to use the devices (Giraud & Siegenthaler,
2014, p.2).
A4. Ethical Considerations
CPR shares common goals with other health interventions, which is to restore health,
preserve life and relief suffering as well as limiting disability. When initiating and ending
resuscitation, differences in cultural norms and ethical perspectives have to be considered. Some
of the ethical issues that might affect the healthcare organization or the caregiver include matters
pertaining futility, withdrawing or withholding interventions, practicing procedures on the newly
dead as well as communication and palliative care. During cardiac arrest, CPR attempts are
conducted. Rapid decisions have to be made based on the available information which can be
erroneous or incomplete. There is an increasing concern of the high budgets spent on CPR when
mainly the results are analysed based on the high percentage of the death of cardiac arrest
patients (Rubulotta & Rubulotta, 2013, p. 266).
B1. PICOT Table
P (patient/problem) Hospitalized adults
I (intervention/indicator) Modern CPR devices
C (comparison) Traditional chest compression CPR
O (outcome) Mortality
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED RESEARCH 5
B2. PICOT Question
Amongst hospitalized adults, how useful is the modern use day CPR devices compared to
traditional chest compression CPR at averting mortality?
C1a. Critical Words Used for the Search
When searching the articles, I used different keywords. Some of the keywords used for
the search of the materials include the following; cardiac arrest, cardiopulmonary resuscitation,
Hospital patients, Cardiac patients, Mechanical resuscitation, AutoPulse, Lund University
Cardiac Assist System (LUCAS), automatic devices and cardiopulmonary resuscitation.
C1b. Number and Types of Articles Found
Based on the above keywords, a total of 12, 348 articles populated. After narrowing
down the date requirement of articles published not less than five years ago, 1243 items filled.
An estimated 27 reports were reviewed for this paper. Some of the pieces that were seen from the
results after the search were quality improvement projects, evidence-based research articles,
health engineering articles, survival rates statistics, medicine expert opinions, review cases and
unique materials. Some of the review cases, survival rate statistics, and expert opinions were
excellent though they were not used due to instances of date limits and failure to answer the
PICO question.
C2a. Discussion of the 4 Articles
The first research article by (Smekal, 2013), gives information on the emergence of the
new mechanical CPR devices which have been developed. According to the author, though the
new tools are said to be better compared to the traditional CPR methods, the use of the new
devices has not shown any substantial increase in the survival rates for cardiac arrest patients.
B2. PICOT Question
Amongst hospitalized adults, how useful is the modern use day CPR devices compared to
traditional chest compression CPR at averting mortality?
C1a. Critical Words Used for the Search
When searching the articles, I used different keywords. Some of the keywords used for
the search of the materials include the following; cardiac arrest, cardiopulmonary resuscitation,
Hospital patients, Cardiac patients, Mechanical resuscitation, AutoPulse, Lund University
Cardiac Assist System (LUCAS), automatic devices and cardiopulmonary resuscitation.
C1b. Number and Types of Articles Found
Based on the above keywords, a total of 12, 348 articles populated. After narrowing
down the date requirement of articles published not less than five years ago, 1243 items filled.
An estimated 27 reports were reviewed for this paper. Some of the pieces that were seen from the
results after the search were quality improvement projects, evidence-based research articles,
health engineering articles, survival rates statistics, medicine expert opinions, review cases and
unique materials. Some of the review cases, survival rate statistics, and expert opinions were
excellent though they were not used due to instances of date limits and failure to answer the
PICO question.
C2a. Discussion of the 4 Articles
The first research article by (Smekal, 2013), gives information on the emergence of the
new mechanical CPR devices which have been developed. According to the author, though the
new tools are said to be better compared to the traditional CPR methods, the use of the new
devices has not shown any substantial increase in the survival rates for cardiac arrest patients.
EVIDENCE BASED RESEARCH 6
The research by Smekal gives me evidence that the new CPR devices have no significant benefit
of reducing mortality rates despite their high purchasing and operational costs.
The second research article by Christ et al. (2014, p.320), describes the increasing
mortality rate for adults with cardiac arrest. According to the authors, the survival rate for
cardiac arrest patients is increasing not only in the developed economies but also within the
developing economies. The research by the researchers helps me justify the need to address the
issue of adequate CPR procedures which will reduce adult mortality rates among patients in
hospitals
The first non- research article describes the current practices employed by healthcare
practitioners. According to Remino et al. (2017, P.3), currently, the majority of the health
practitioners attending to adults under cardiac arrest in hospitals are using the modern devices to
perform CPR. Some of the standard methods used as stated by the authors include AutoPulse
devices and Lund University Cardiac Assist System (LUCAS). The article helps justify my
earlier argument that currently, the majority of the rescuers are adopting the new CPR methods.
The second non-evidence article covers some of the ethical considerations that emanate from
CPR on patients facing cardiac arrest. Rubulotta & Rubulotta (2013, p. 266) describe some of the
ethical implications that might result in an organization due to the practice of the CPR amongst
in-hospital cardiac arrest patients. The authors help provide more insight on some of the ethical
considerations that need to be considered before performing a CPR.
E1. Recommended Practice Change
Based on the on evidence retrieved from the five articles, various recommendations are
touching on the change of the current CPR practices. According to Smekal (2013), the
mechanical CPR techniques which include the use of the LUCAS device has shown a high
The research by Smekal gives me evidence that the new CPR devices have no significant benefit
of reducing mortality rates despite their high purchasing and operational costs.
The second research article by Christ et al. (2014, p.320), describes the increasing
mortality rate for adults with cardiac arrest. According to the authors, the survival rate for
cardiac arrest patients is increasing not only in the developed economies but also within the
developing economies. The research by the researchers helps me justify the need to address the
issue of adequate CPR procedures which will reduce adult mortality rates among patients in
hospitals
The first non- research article describes the current practices employed by healthcare
practitioners. According to Remino et al. (2017, P.3), currently, the majority of the health
practitioners attending to adults under cardiac arrest in hospitals are using the modern devices to
perform CPR. Some of the standard methods used as stated by the authors include AutoPulse
devices and Lund University Cardiac Assist System (LUCAS). The article helps justify my
earlier argument that currently, the majority of the rescuers are adopting the new CPR methods.
The second non-evidence article covers some of the ethical considerations that emanate from
CPR on patients facing cardiac arrest. Rubulotta & Rubulotta (2013, p. 266) describe some of the
ethical implications that might result in an organization due to the practice of the CPR amongst
in-hospital cardiac arrest patients. The authors help provide more insight on some of the ethical
considerations that need to be considered before performing a CPR.
E1. Recommended Practice Change
Based on the on evidence retrieved from the five articles, various recommendations are
touching on the change of the current CPR practices. According to Smekal (2013), the
mechanical CPR techniques which include the use of the LUCAS device has shown a high
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED RESEARCH 7
number of injuries and fractures after autopsies of the patients who succumb. The evidence based
on the research indicates that there is need to shift towards the manual CPR techniques as they
have recorded fewer injuries or fractures to patients
Christ et al. (2014, p.320) analyze the survival rate for patients who are admitted with
cases of cardiac arrest. According to the research conducted by the researchers, the survival rates
for adults admitted with cardiac arrest is still high. There is no any significant difference in
regards to increased survival rates between the manual CPR and the mechanical CPR. The
authors find a 44.6% survival rate on the first day of admission with the rate reducing to 35.4%
on the seventh day. These rates do not justify the need to incur huge expenses on the new
devices. Manual CPR procedure which is cheap to source and more efficient to apply.
The new mechanical devices used are inefficient in delivering resuscitation to patients
under cardiac arrest. According to Giraud et al. (2014, p.2), the new device table height,
fluoroscopic x-ray detectors within the device mandate the rescuers to conduct resuscitation
manoeuvers in nonefficient and uncomfortable positions. The challenges which emanate from
the use of the equipment render the process of delivering resuscitation challenging hence a
recommendation for the manual methods is appropriate as the rescuers have a clear vision,
maintain right positions and do not have to deal with multi-tasking activities as seen with the
modern devices.
The mechanical CPR devices have indicated a weaker ability to deliver a return of
spontaneous circulation. According to Li et al. (2016), the automatic CPR devices cannot replace
the conventional CPR procedures. My recommendation majors on the use of the traditional CPR
procedures which have recorded a high return of spontaneous circulation (ROSC) among patients
with cardiac arrest.
number of injuries and fractures after autopsies of the patients who succumb. The evidence based
on the research indicates that there is need to shift towards the manual CPR techniques as they
have recorded fewer injuries or fractures to patients
Christ et al. (2014, p.320) analyze the survival rate for patients who are admitted with
cases of cardiac arrest. According to the research conducted by the researchers, the survival rates
for adults admitted with cardiac arrest is still high. There is no any significant difference in
regards to increased survival rates between the manual CPR and the mechanical CPR. The
authors find a 44.6% survival rate on the first day of admission with the rate reducing to 35.4%
on the seventh day. These rates do not justify the need to incur huge expenses on the new
devices. Manual CPR procedure which is cheap to source and more efficient to apply.
The new mechanical devices used are inefficient in delivering resuscitation to patients
under cardiac arrest. According to Giraud et al. (2014, p.2), the new device table height,
fluoroscopic x-ray detectors within the device mandate the rescuers to conduct resuscitation
manoeuvers in nonefficient and uncomfortable positions. The challenges which emanate from
the use of the equipment render the process of delivering resuscitation challenging hence a
recommendation for the manual methods is appropriate as the rescuers have a clear vision,
maintain right positions and do not have to deal with multi-tasking activities as seen with the
modern devices.
The mechanical CPR devices have indicated a weaker ability to deliver a return of
spontaneous circulation. According to Li et al. (2016), the automatic CPR devices cannot replace
the conventional CPR procedures. My recommendation majors on the use of the traditional CPR
procedures which have recorded a high return of spontaneous circulation (ROSC) among patients
with cardiac arrest.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED RESEARCH 8
Lastly, I would recommend the use of the traditional resuscitation procedure because of
its simplicity to use, low cost and efficiency of the technique as one can conduct it anywhere.
The method does not require high skills to perform. The survival rates of the manual procedure
are no different from the mechanical CPR procedures as indicated by Perkins et al. (21014).
F1. Implementation of the Change
The implementation of the change will involve different stakeholders. Some of-of the
stakeholders include nurses, my supervisor, and clinical nurse educator. I would suggest the
stakeholders in the decision to implement the change through different strategies. I will involve
my supervisor in the decision through requesting him to further elaborate on the different
traditional CPR procedures available as well as helping me access more educational materials
which give more insight on the best conventional practices which can improve the survival rate. I
would involve a clinical nurse educator in the decision through submitting inquiries on cost,
safety, and complications of adopting traditional CPR methods. In regards incorporating the
nurse in the decision to implement the change, I would inquire from him or her the effectiveness,
efficiency, and reliability of manual chest compression techniques. Based on the information
retrieved from the stakeholders, I will be able to make an informed decision pertaining the
implementation of the change from the use of the modern CPR devices to use of the traditional
CPR procedures.
F2. Barriers to Adoption of the Evidence-Based Practice
There exist various barriers which might hinder the adoption of the evidence-based
practice. Some of the obstacles include cultural or institutional barriers. Some of the factors
within this barriers include lack of an existing culture within institutions which encourages the
use of traditional CPR procedures. Other factors include traditional norms and a strong influence
Lastly, I would recommend the use of the traditional resuscitation procedure because of
its simplicity to use, low cost and efficiency of the technique as one can conduct it anywhere.
The method does not require high skills to perform. The survival rates of the manual procedure
are no different from the mechanical CPR procedures as indicated by Perkins et al. (21014).
F1. Implementation of the Change
The implementation of the change will involve different stakeholders. Some of-of the
stakeholders include nurses, my supervisor, and clinical nurse educator. I would suggest the
stakeholders in the decision to implement the change through different strategies. I will involve
my supervisor in the decision through requesting him to further elaborate on the different
traditional CPR procedures available as well as helping me access more educational materials
which give more insight on the best conventional practices which can improve the survival rate. I
would involve a clinical nurse educator in the decision through submitting inquiries on cost,
safety, and complications of adopting traditional CPR methods. In regards incorporating the
nurse in the decision to implement the change, I would inquire from him or her the effectiveness,
efficiency, and reliability of manual chest compression techniques. Based on the information
retrieved from the stakeholders, I will be able to make an informed decision pertaining the
implementation of the change from the use of the modern CPR devices to use of the traditional
CPR procedures.
F2. Barriers to Adoption of the Evidence-Based Practice
There exist various barriers which might hinder the adoption of the evidence-based
practice. Some of the obstacles include cultural or institutional barriers. Some of the factors
within this barriers include lack of an existing culture within institutions which encourages the
use of traditional CPR procedures. Other factors include traditional norms and a strong influence
EVIDENCE BASED RESEARCH 9
to fall back on habits learned before like use of the modern CPR devices. According to Tacia et
al. (2015, p.94), lack of motivation amongst nurses is a leading barrier towards the adoption of
EBP.
F3. Solution to the Barriers
Different initiatives can be implemented to address the barriers. Regarding cultural or
institutional boundaries, they can be solved through developing institutional values which will
determine the norms and conduct of employees within the healthcare organization. Pertaining
lack of motivation, this barrier can be addressed through creating trust amongst the healthcare
staff as well as recognition and training to ensure that they do not feel that they are not capable
of handling the change. Providing that there is efficient communication within the organization is
crucial in ensuring that the health practitioners do not feel like they lack any information which
might hinder them from making sure decisions pertaining CPR.
F4. Indicator to Measure the Outcome Related to the Recommendation
Based on the stated recommendation, there is one indicator which is crucial to be able to
determine the success of the evidence-based practice recommended. To measure how the
traditional CPR procedures reduce the mortality rate after implementation, there would be a need
to develop a chart audit at 7, 14 and 30 days. The chart will give a percentage of the mortality
rate or survival rate for cardiac arrest patients in hospitals who survive or succumb to cardiac
arrest when put under the traditional CPR procedures. An outcome of slightly below 50% of
above, would be an excellent outcome in saving lives.
to fall back on habits learned before like use of the modern CPR devices. According to Tacia et
al. (2015, p.94), lack of motivation amongst nurses is a leading barrier towards the adoption of
EBP.
F3. Solution to the Barriers
Different initiatives can be implemented to address the barriers. Regarding cultural or
institutional boundaries, they can be solved through developing institutional values which will
determine the norms and conduct of employees within the healthcare organization. Pertaining
lack of motivation, this barrier can be addressed through creating trust amongst the healthcare
staff as well as recognition and training to ensure that they do not feel that they are not capable
of handling the change. Providing that there is efficient communication within the organization is
crucial in ensuring that the health practitioners do not feel like they lack any information which
might hinder them from making sure decisions pertaining CPR.
F4. Indicator to Measure the Outcome Related to the Recommendation
Based on the stated recommendation, there is one indicator which is crucial to be able to
determine the success of the evidence-based practice recommended. To measure how the
traditional CPR procedures reduce the mortality rate after implementation, there would be a need
to develop a chart audit at 7, 14 and 30 days. The chart will give a percentage of the mortality
rate or survival rate for cardiac arrest patients in hospitals who survive or succumb to cardiac
arrest when put under the traditional CPR procedures. An outcome of slightly below 50% of
above, would be an excellent outcome in saving lives.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED RESEARCH 10
References
Christ, M., Dierschke, W., Von, K., & Bracht, M. (2014, June 30). Cardiac arrest teams and time
of day: effects. International Journal of General Medicine, 7, 319.
doi:10.2147/IJGM.S66609
Giraud, R., & Siegenthaler, N. (2014, February). The LUCAS 2 Chest Compression Device Is
Not Always Efficient: An Echographic Confirmation. RsearchGate.
doi:10.1016/j.annemergmed.2014.01.020
Li, H., Wang, D., Yu, Y., & Zhao, X. (2016). Mechanical versus manual chest compressions for
cardiac arrest: a systematic review and meta-analysis. Scandinavian Journal of Trauma,
Resuscitation, 24(10). doi:10.1186/s13049-016-0202-y
Perkins, G. D., Lall, R., Quinn, T., & Deakin, C. (2015, March 14). Mechanical versus manual
chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic,cluster
randomised controlled trial. National Institute for Health Research HTA, 385. Retrieved
from
https://pdfs.semanticscholar.org/c3c6/a35d38b74c8c7a942febb47921e45a3c6f77.pdf
Raffee, L., Samrah, S., & Yousef, H. (2017, July). Incidence, Characteristics, and Survival Trend
of Cardiopulmonary Resuscitation Following In-hospital Comparedto Out-of-hospital
Cardiac Arrest in Northern Jordan. Comparing survival trend for in-hospital compared to
out-of-hospital cardiac arrest, 21(7), 436-441. doi:10.4103/ijccm.IJCCM_15_17
Remino, C., Baronio, M., Pellegrini1, N., & Aggogeri, F. (2018). Automatic and manual devices
for cardiopulmonary resuscitation: A review. 10(1), 1-14.
doi:10.1177/1687814017748749
References
Christ, M., Dierschke, W., Von, K., & Bracht, M. (2014, June 30). Cardiac arrest teams and time
of day: effects. International Journal of General Medicine, 7, 319.
doi:10.2147/IJGM.S66609
Giraud, R., & Siegenthaler, N. (2014, February). The LUCAS 2 Chest Compression Device Is
Not Always Efficient: An Echographic Confirmation. RsearchGate.
doi:10.1016/j.annemergmed.2014.01.020
Li, H., Wang, D., Yu, Y., & Zhao, X. (2016). Mechanical versus manual chest compressions for
cardiac arrest: a systematic review and meta-analysis. Scandinavian Journal of Trauma,
Resuscitation, 24(10). doi:10.1186/s13049-016-0202-y
Perkins, G. D., Lall, R., Quinn, T., & Deakin, C. (2015, March 14). Mechanical versus manual
chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic,cluster
randomised controlled trial. National Institute for Health Research HTA, 385. Retrieved
from
https://pdfs.semanticscholar.org/c3c6/a35d38b74c8c7a942febb47921e45a3c6f77.pdf
Raffee, L., Samrah, S., & Yousef, H. (2017, July). Incidence, Characteristics, and Survival Trend
of Cardiopulmonary Resuscitation Following In-hospital Comparedto Out-of-hospital
Cardiac Arrest in Northern Jordan. Comparing survival trend for in-hospital compared to
out-of-hospital cardiac arrest, 21(7), 436-441. doi:10.4103/ijccm.IJCCM_15_17
Remino, C., Baronio, M., Pellegrini1, N., & Aggogeri, F. (2018). Automatic and manual devices
for cardiopulmonary resuscitation: A review. 10(1), 1-14.
doi:10.1177/1687814017748749
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED RESEARCH 11
Rubulotta, F., & Rubulotta, G. (2013). Cardiopulmonary resuscitation and ethics. Rev Bras Ter
Intensiva., 25(4), 265-269. doi:10.5935/0103-507X.20130046
Smekal, D. (2013). Safety with Mechanical Chest. Digital Comprehensive Summaries of
Uppsala Dissertations, 1(1). Retrieved April 4, 2018, from http://www.hlr.nu/wp-
content/uploads/D.-Smekal.-CPR-and-LUCAS-2013.pdf
Tacia, L., Biskupski, K., Pheley, A., & Lehto, R. (2015, January 3). Identifying barriers to
evidence-based practice. Clinical Nursing Studies, 3(2). doi:10.5430/cns.v3n2p90
Rubulotta, F., & Rubulotta, G. (2013). Cardiopulmonary resuscitation and ethics. Rev Bras Ter
Intensiva., 25(4), 265-269. doi:10.5935/0103-507X.20130046
Smekal, D. (2013). Safety with Mechanical Chest. Digital Comprehensive Summaries of
Uppsala Dissertations, 1(1). Retrieved April 4, 2018, from http://www.hlr.nu/wp-
content/uploads/D.-Smekal.-CPR-and-LUCAS-2013.pdf
Tacia, L., Biskupski, K., Pheley, A., & Lehto, R. (2015, January 3). Identifying barriers to
evidence-based practice. Clinical Nursing Studies, 3(2). doi:10.5430/cns.v3n2p90
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





