Detailed Analysis and Report on Creutzfeldt-Jakob Disease
VerifiedAdded on 2020/04/07
|10
|1840
|56
Report
AI Summary
This report provides a comprehensive overview of Creutzfeldt-Jakob Disease (CJD), a rare and invariably fatal neurodegenerative disorder caused by prions. It covers the causative agent, different categories like sporadic, hereditary, and acquired CJD, and the disease's history, including its discovery and transmission modes. The report details the epidemiology of CJD, its reservoir, and modes of transmission, highlighting the pathology, molecular basis of prions, and the signs and symptoms, which include cognitive impairment, involuntary movements, and eventual coma. The diagnosis involves neurological assessments, brain biopsies, and prion protein detection, while treatment focuses on managing symptoms. The report also touches upon the socio-politico-economic impact, including government policies related to blood transfusions and donor restrictions. References to key research papers are included to support the findings.

Running head: CREUTZFELDT- JAKOB DISEASE
CREUTZFELDT- JAKOB DISEASE
Name of the Student
Name of the university
Author’s note
CREUTZFELDT- JAKOB DISEASE
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CREUTZFELDT- JAKOB DISEASE
CREUTZFELDT- JAKOB- DISEASE
a) Causative agent
CJD is a degenerative, rare, invariably lethal brain disorder. It causes cognitive
impairment and with the progression of the illness, the deterioration of the mental health
occurs leading to blindness, incontinence, involuntary movement, and extreme weakness,
coma and death1.
CJD is caused by the aggregation of the toxic proteins called the prions. Prions are
proteinaceous infectious particles that are caused due to the abnormal folding of the
proteins. Prion protein can occur in normal form and are present in the body of the animals
and they normally play a protective part in the cells and help the cells to respond to the
oxygen deficiency1. The normal prion protein in a body may suddenly change in to
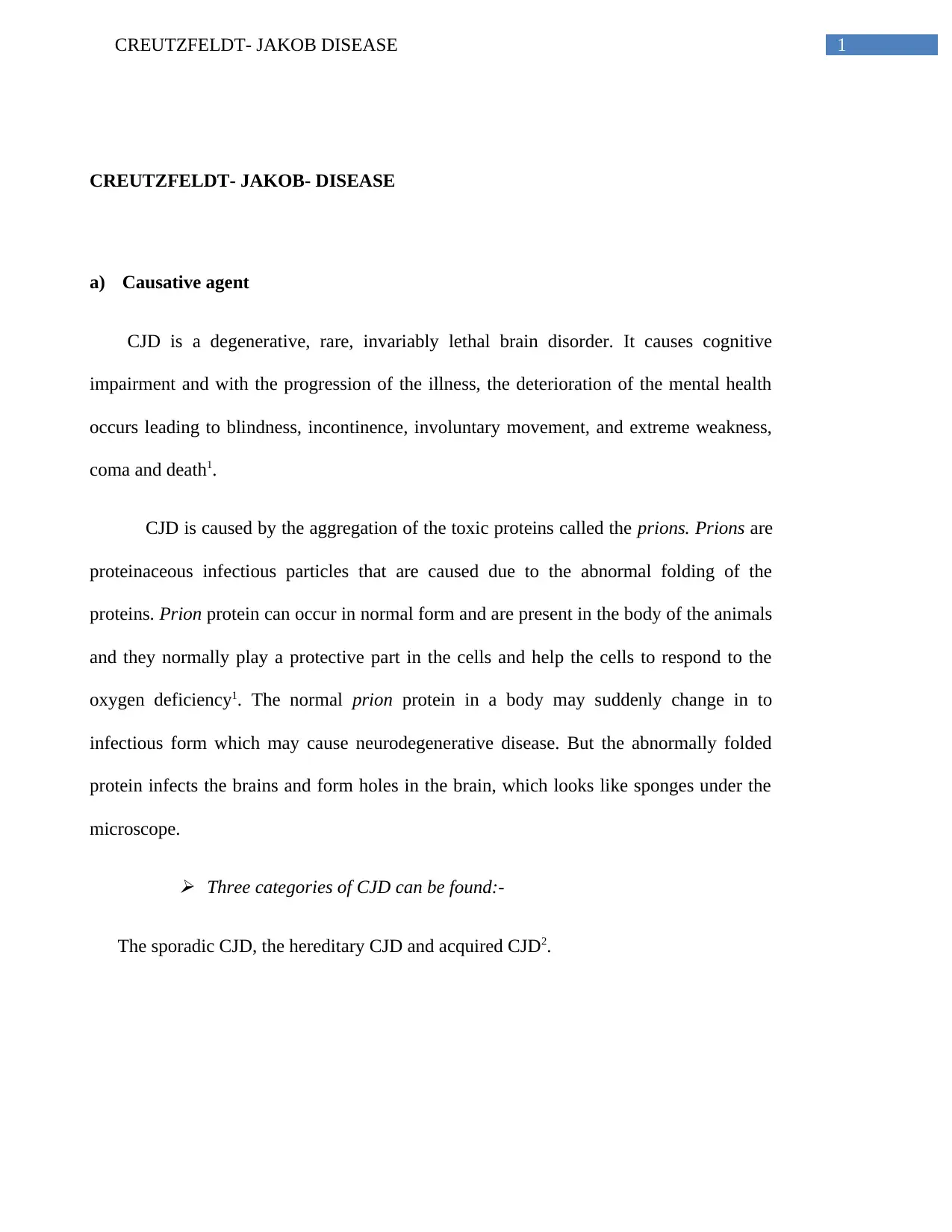
infectious form which may cause neurodegenerative disease. But the abnormally folded
protein infects the brains and form holes in the brain, which looks like sponges under the
microscope. Three categories of CJD can be found:-
The sporadic CJD, the hereditary CJD and acquired CJD2.
CREUTZFELDT- JAKOB- DISEASE
a) Causative agent
CJD is a degenerative, rare, invariably lethal brain disorder. It causes cognitive
impairment and with the progression of the illness, the deterioration of the mental health
occurs leading to blindness, incontinence, involuntary movement, and extreme weakness,
coma and death1.
CJD is caused by the aggregation of the toxic proteins called the prions. Prions are
proteinaceous infectious particles that are caused due to the abnormal folding of the
proteins. Prion protein can occur in normal form and are present in the body of the animals
and they normally play a protective part in the cells and help the cells to respond to the
oxygen deficiency1. The normal prion protein in a body may suddenly change in to
infectious form which may cause neurodegenerative disease. But the abnormally folded
protein infects the brains and form holes in the brain, which looks like sponges under the
microscope. Three categories of CJD can be found:-
The sporadic CJD, the hereditary CJD and acquired CJD2.
2CREUTZFELDT- JAKOB DISEASE
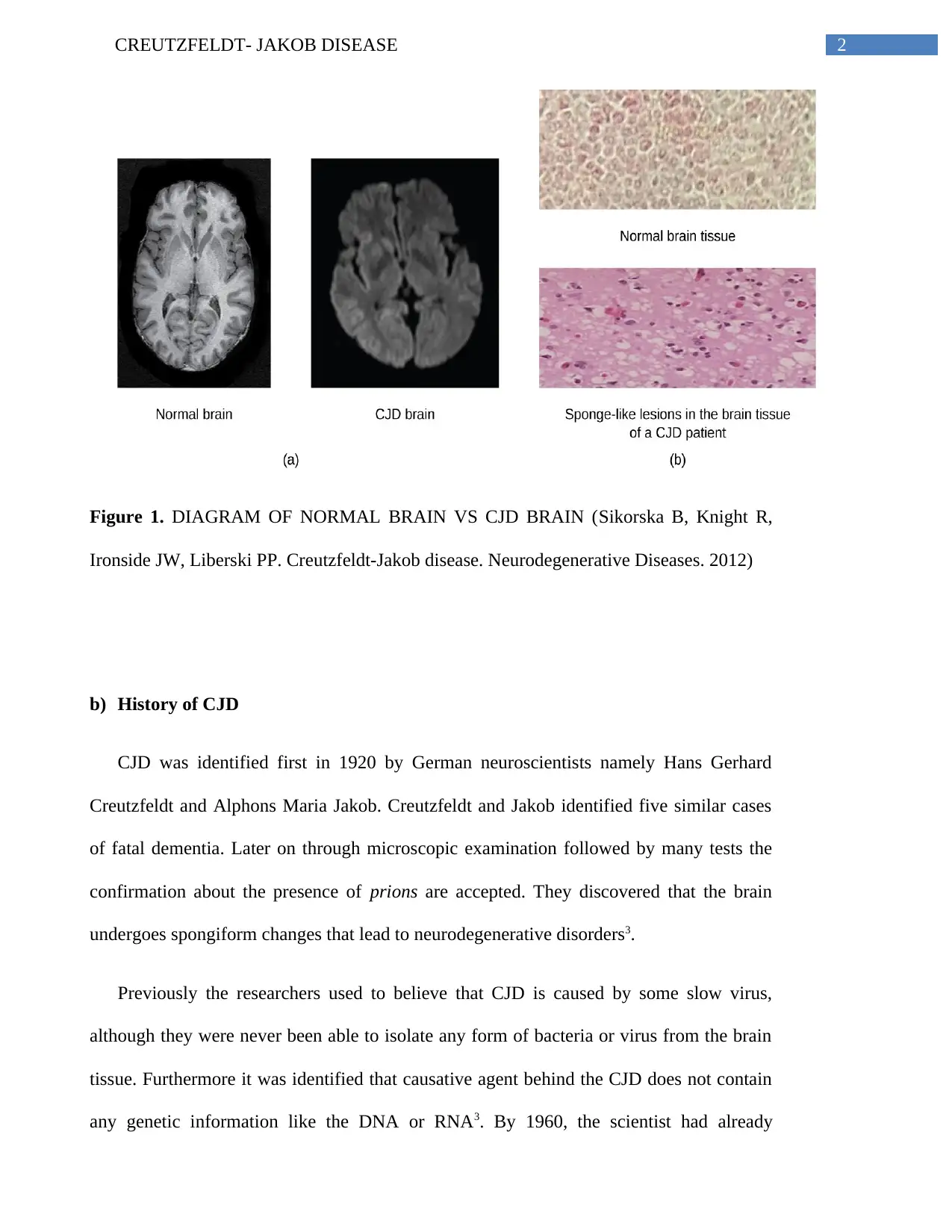
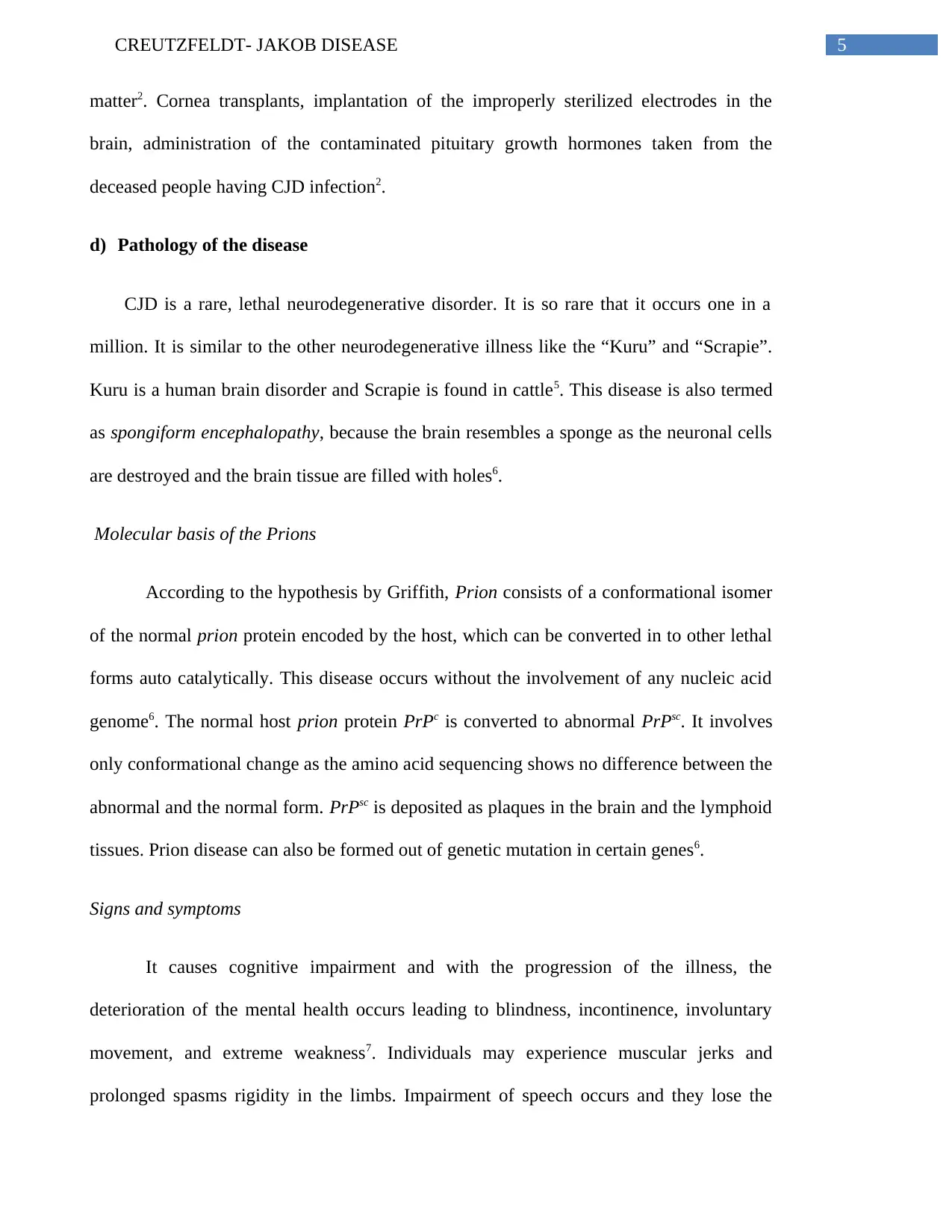
Figure 1. DIAGRAM OF NORMAL BRAIN VS CJD BRAIN (Sikorska B, Knight R,
Ironside JW, Liberski PP. Creutzfeldt-Jakob disease. Neurodegenerative Diseases. 2012)
b) History of CJD
CJD was identified first in 1920 by German neuroscientists namely Hans Gerhard
Creutzfeldt and Alphons Maria Jakob. Creutzfeldt and Jakob identified five similar cases
of fatal dementia. Later on through microscopic examination followed by many tests the
confirmation about the presence of prions are accepted. They discovered that the brain
undergoes spongiform changes that lead to neurodegenerative disorders3.
Previously the researchers used to believe that CJD is caused by some slow virus,
although they were never been able to isolate any form of bacteria or virus from the brain
tissue. Furthermore it was identified that causative agent behind the CJD does not contain
any genetic information like the DNA or RNA3. By 1960, the scientist had already
Figure 1. DIAGRAM OF NORMAL BRAIN VS CJD BRAIN (Sikorska B, Knight R,
Ironside JW, Liberski PP. Creutzfeldt-Jakob disease. Neurodegenerative Diseases. 2012)
b) History of CJD
CJD was identified first in 1920 by German neuroscientists namely Hans Gerhard
Creutzfeldt and Alphons Maria Jakob. Creutzfeldt and Jakob identified five similar cases
of fatal dementia. Later on through microscopic examination followed by many tests the
confirmation about the presence of prions are accepted. They discovered that the brain
undergoes spongiform changes that lead to neurodegenerative disorders3.
Previously the researchers used to believe that CJD is caused by some slow virus,
although they were never been able to isolate any form of bacteria or virus from the brain
tissue. Furthermore it was identified that causative agent behind the CJD does not contain
any genetic information like the DNA or RNA3. By 1960, the scientist had already
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CREUTZFELDT- JAKOB DISEASE
discovered the spongiform structure of the diseased brain. They found that the disease is
almost similar to the disease that has occurred in the people dying from ‘kuru’4. Kuru was
known to be a result of cannibalism in the tribe of Papua New Guinea. CJD was also found
to be transmissible. Later on scientists found that a small amount of abnormal prion could
generate more abnormal prions by the abnormal folding3. By 1980 it was found that CJD
can be transmitted to the patients through the grafts of the dura matter as well as through
the hormones prepared from the deceased people infected with CJD. Later on it was also
discovered that the cattle are also susceptible to the infected proteins, causing ‘mad cow
disease’ in the cattle. Later on by the year 2013, the effect of the variant CJD seemed to be
over or very few cases have been found worldwide3.
c) Epidemiology of the disease
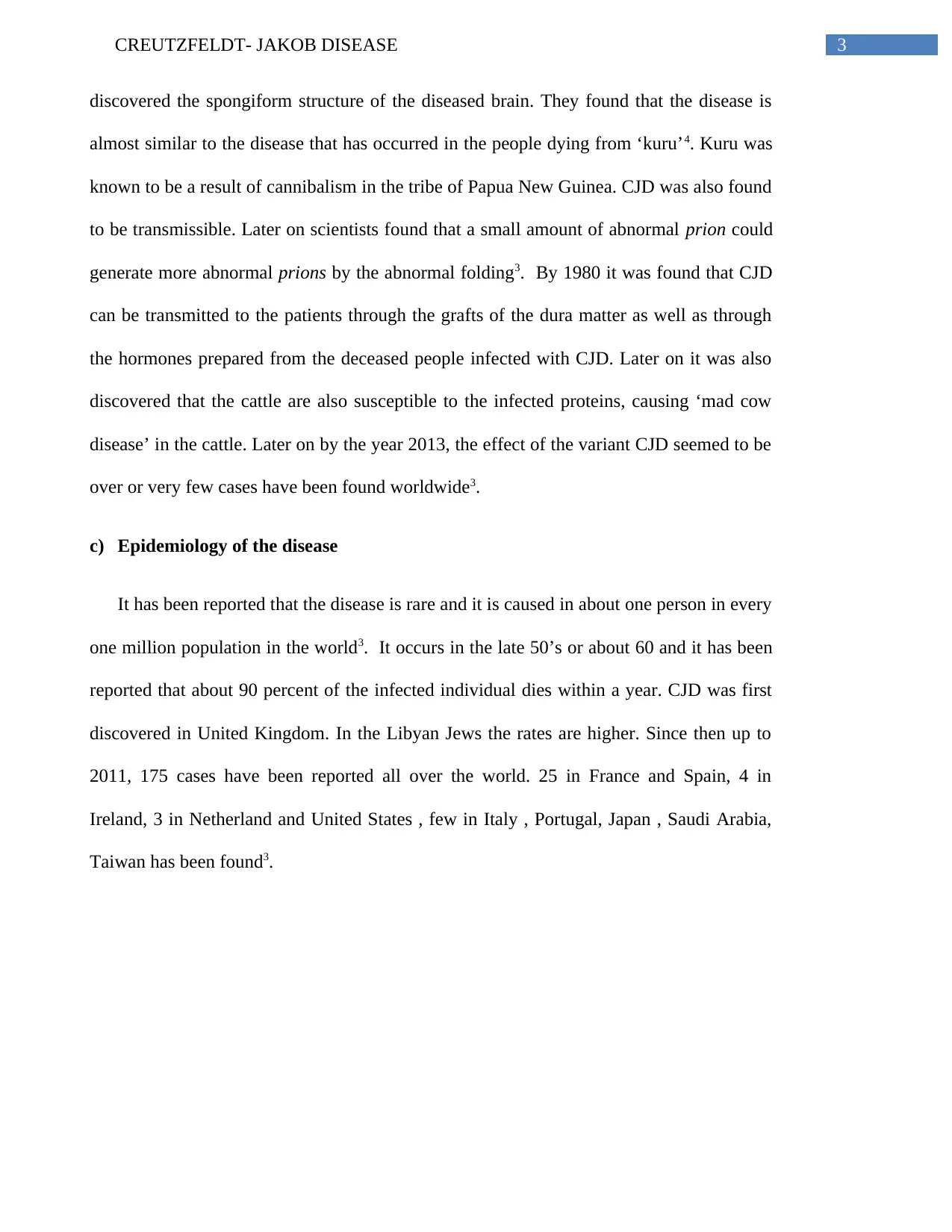
It has been reported that the disease is rare and it is caused in about one person in every
one million population in the world3. It occurs in the late 50’s or about 60 and it has been
reported that about 90 percent of the infected individual dies within a year. CJD was first
discovered in United Kingdom. In the Libyan Jews the rates are higher. Since then up to
2011, 175 cases have been reported all over the world. 25 in France and Spain, 4 in
Ireland, 3 in Netherland and United States , few in Italy , Portugal, Japan , Saudi Arabia,
Taiwan has been found3.
discovered the spongiform structure of the diseased brain. They found that the disease is
almost similar to the disease that has occurred in the people dying from ‘kuru’4. Kuru was
known to be a result of cannibalism in the tribe of Papua New Guinea. CJD was also found
to be transmissible. Later on scientists found that a small amount of abnormal prion could
generate more abnormal prions by the abnormal folding3. By 1980 it was found that CJD
can be transmitted to the patients through the grafts of the dura matter as well as through
the hormones prepared from the deceased people infected with CJD. Later on it was also
discovered that the cattle are also susceptible to the infected proteins, causing ‘mad cow
disease’ in the cattle. Later on by the year 2013, the effect of the variant CJD seemed to be
over or very few cases have been found worldwide3.
c) Epidemiology of the disease
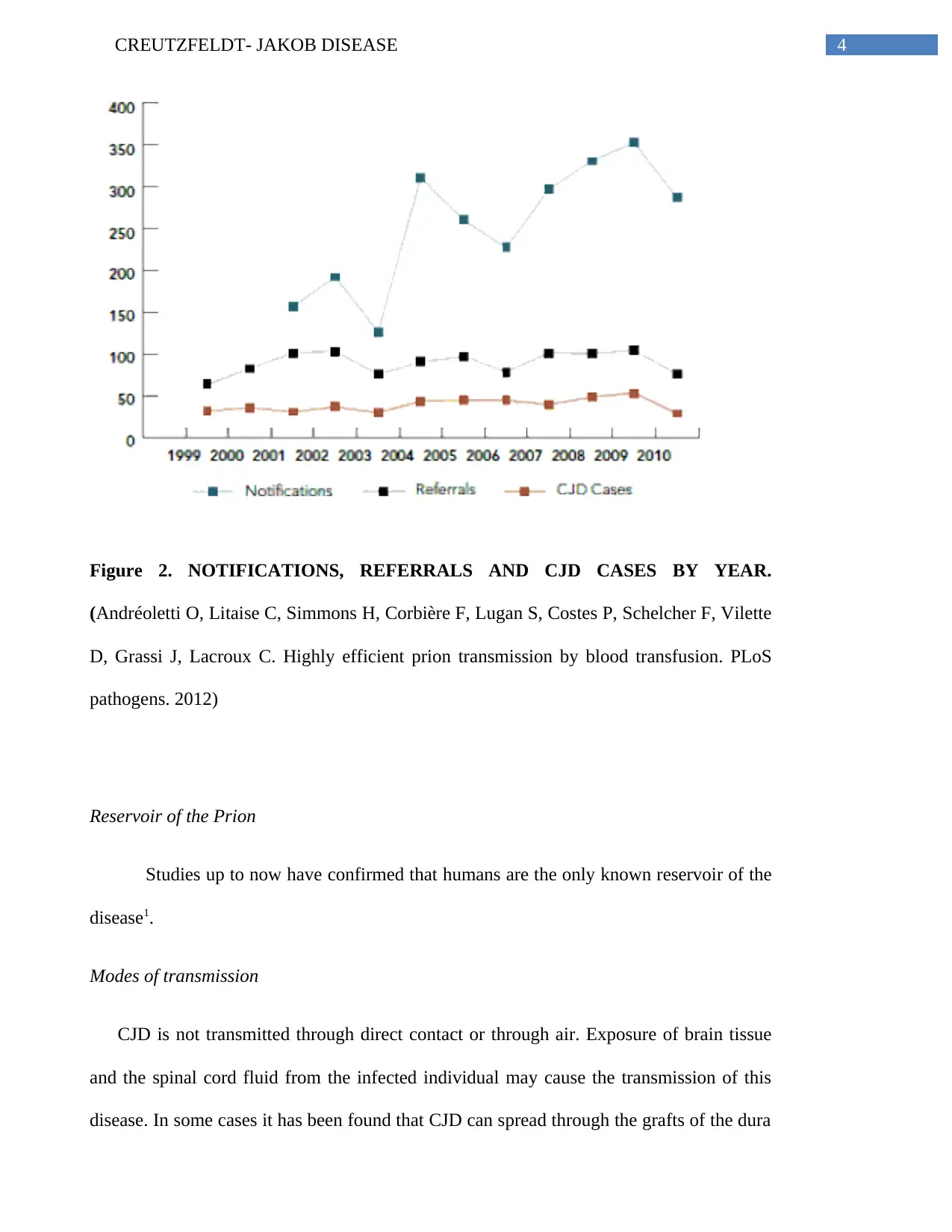
It has been reported that the disease is rare and it is caused in about one person in every
one million population in the world3. It occurs in the late 50’s or about 60 and it has been
reported that about 90 percent of the infected individual dies within a year. CJD was first
discovered in United Kingdom. In the Libyan Jews the rates are higher. Since then up to
2011, 175 cases have been reported all over the world. 25 in France and Spain, 4 in
Ireland, 3 in Netherland and United States , few in Italy , Portugal, Japan , Saudi Arabia,
Taiwan has been found3.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CREUTZFELDT- JAKOB DISEASE
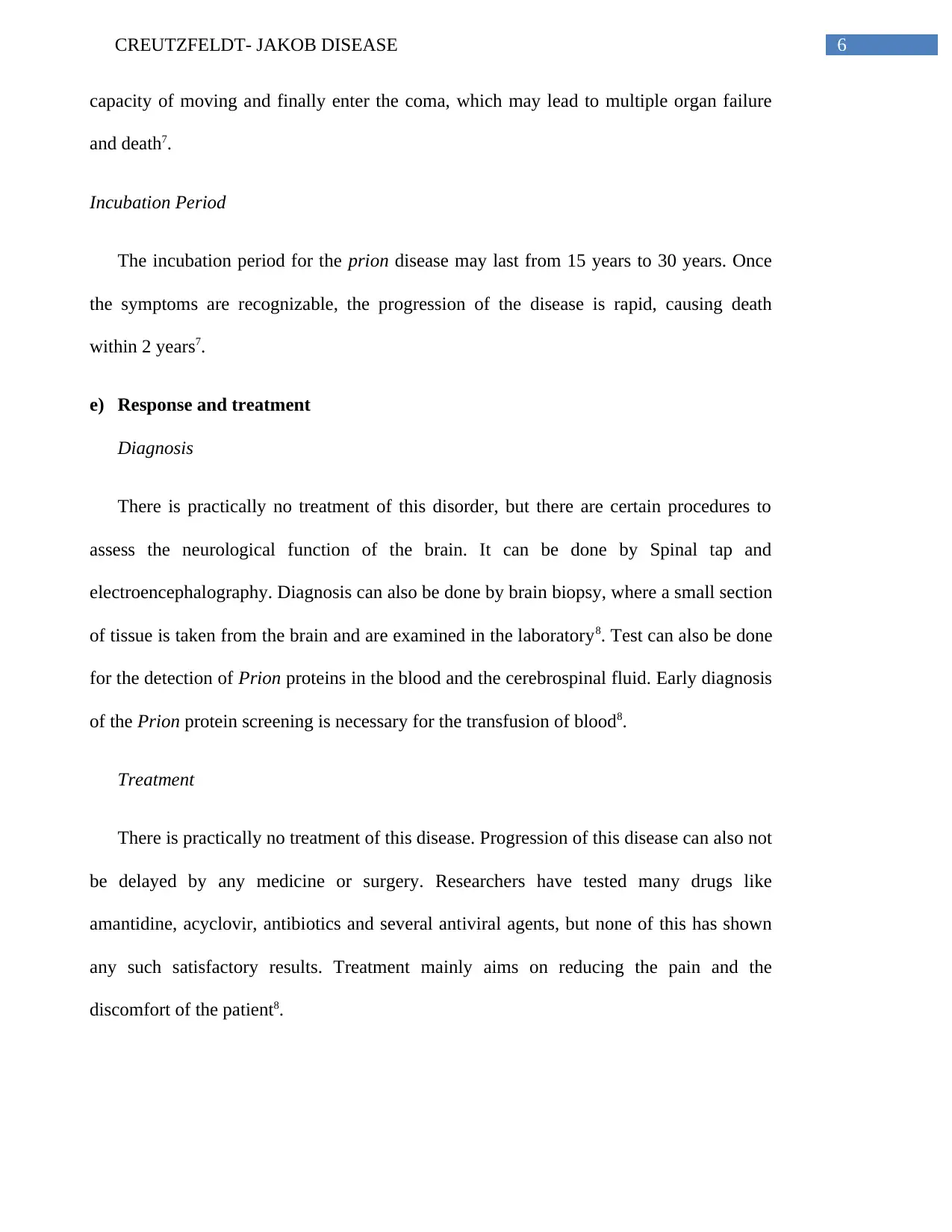
Figure 2. NOTIFICATIONS, REFERRALS AND CJD CASES BY YEAR.
(Andréoletti O, Litaise C, Simmons H, Corbière F, Lugan S, Costes P, Schelcher F, Vilette
D, Grassi J, Lacroux C. Highly efficient prion transmission by blood transfusion. PLoS
pathogens. 2012)
Reservoir of the Prion
Studies up to now have confirmed that humans are the only known reservoir of the
disease1.
Modes of transmission
CJD is not transmitted through direct contact or through air. Exposure of brain tissue
and the spinal cord fluid from the infected individual may cause the transmission of this
disease. In some cases it has been found that CJD can spread through the grafts of the dura
Figure 2. NOTIFICATIONS, REFERRALS AND CJD CASES BY YEAR.
(Andréoletti O, Litaise C, Simmons H, Corbière F, Lugan S, Costes P, Schelcher F, Vilette
D, Grassi J, Lacroux C. Highly efficient prion transmission by blood transfusion. PLoS
pathogens. 2012)
Reservoir of the Prion
Studies up to now have confirmed that humans are the only known reservoir of the
disease1.
Modes of transmission
CJD is not transmitted through direct contact or through air. Exposure of brain tissue
and the spinal cord fluid from the infected individual may cause the transmission of this
disease. In some cases it has been found that CJD can spread through the grafts of the dura
5CREUTZFELDT- JAKOB DISEASE
matter2. Cornea transplants, implantation of the improperly sterilized electrodes in the
brain, administration of the contaminated pituitary growth hormones taken from the
deceased people having CJD infection2.
d) Pathology of the disease
CJD is a rare, lethal neurodegenerative disorder. It is so rare that it occurs one in a
million. It is similar to the other neurodegenerative illness like the “Kuru” and “Scrapie”.
Kuru is a human brain disorder and Scrapie is found in cattle5. This disease is also termed
as spongiform encephalopathy, because the brain resembles a sponge as the neuronal cells
are destroyed and the brain tissue are filled with holes6.
Molecular basis of the Prions
According to the hypothesis by Griffith, Prion consists of a conformational isomer
of the normal prion protein encoded by the host, which can be converted in to other lethal
forms auto catalytically. This disease occurs without the involvement of any nucleic acid
genome6. The normal host prion protein PrPc is converted to abnormal PrPsc. It involves
only conformational change as the amino acid sequencing shows no difference between the
abnormal and the normal form. PrPsc is deposited as plaques in the brain and the lymphoid
tissues. Prion disease can also be formed out of genetic mutation in certain genes6.
Signs and symptoms
It causes cognitive impairment and with the progression of the illness, the
deterioration of the mental health occurs leading to blindness, incontinence, involuntary
movement, and extreme weakness7. Individuals may experience muscular jerks and
prolonged spasms rigidity in the limbs. Impairment of speech occurs and they lose the
matter2. Cornea transplants, implantation of the improperly sterilized electrodes in the
brain, administration of the contaminated pituitary growth hormones taken from the
deceased people having CJD infection2.
d) Pathology of the disease
CJD is a rare, lethal neurodegenerative disorder. It is so rare that it occurs one in a
million. It is similar to the other neurodegenerative illness like the “Kuru” and “Scrapie”.
Kuru is a human brain disorder and Scrapie is found in cattle5. This disease is also termed
as spongiform encephalopathy, because the brain resembles a sponge as the neuronal cells
are destroyed and the brain tissue are filled with holes6.
Molecular basis of the Prions
According to the hypothesis by Griffith, Prion consists of a conformational isomer
of the normal prion protein encoded by the host, which can be converted in to other lethal
forms auto catalytically. This disease occurs without the involvement of any nucleic acid
genome6. The normal host prion protein PrPc is converted to abnormal PrPsc. It involves
only conformational change as the amino acid sequencing shows no difference between the
abnormal and the normal form. PrPsc is deposited as plaques in the brain and the lymphoid
tissues. Prion disease can also be formed out of genetic mutation in certain genes6.
Signs and symptoms
It causes cognitive impairment and with the progression of the illness, the
deterioration of the mental health occurs leading to blindness, incontinence, involuntary
movement, and extreme weakness7. Individuals may experience muscular jerks and
prolonged spasms rigidity in the limbs. Impairment of speech occurs and they lose the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CREUTZFELDT- JAKOB DISEASE
capacity of moving and finally enter the coma, which may lead to multiple organ failure
and death7.
Incubation Period
The incubation period for the prion disease may last from 15 years to 30 years. Once
the symptoms are recognizable, the progression of the disease is rapid, causing death
within 2 years7.
e) Response and treatment
Diagnosis
There is practically no treatment of this disorder, but there are certain procedures to
assess the neurological function of the brain. It can be done by Spinal tap and
electroencephalography. Diagnosis can also be done by brain biopsy, where a small section
of tissue is taken from the brain and are examined in the laboratory8. Test can also be done
for the detection of Prion proteins in the blood and the cerebrospinal fluid. Early diagnosis
of the Prion protein screening is necessary for the transfusion of blood8.
Treatment
There is practically no treatment of this disease. Progression of this disease can also not
be delayed by any medicine or surgery. Researchers have tested many drugs like
amantidine, acyclovir, antibiotics and several antiviral agents, but none of this has shown
any such satisfactory results. Treatment mainly aims on reducing the pain and the
discomfort of the patient8.
capacity of moving and finally enter the coma, which may lead to multiple organ failure
and death7.
Incubation Period
The incubation period for the prion disease may last from 15 years to 30 years. Once
the symptoms are recognizable, the progression of the disease is rapid, causing death
within 2 years7.
e) Response and treatment
Diagnosis
There is practically no treatment of this disorder, but there are certain procedures to
assess the neurological function of the brain. It can be done by Spinal tap and
electroencephalography. Diagnosis can also be done by brain biopsy, where a small section
of tissue is taken from the brain and are examined in the laboratory8. Test can also be done
for the detection of Prion proteins in the blood and the cerebrospinal fluid. Early diagnosis
of the Prion protein screening is necessary for the transfusion of blood8.
Treatment
There is practically no treatment of this disease. Progression of this disease can also not
be delayed by any medicine or surgery. Researchers have tested many drugs like
amantidine, acyclovir, antibiotics and several antiviral agents, but none of this has shown
any such satisfactory results. Treatment mainly aims on reducing the pain and the
discomfort of the patient8.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CREUTZFELDT- JAKOB DISEASE
f) Socio-politico-economic
In the Lancet medical journal it was reported that CJD can be transmitted by blood
transfusion. It was reported that the UK government banned any individual who have
received any blood transfusion since 1980 January9. In fact manufacturing of proteins like
albumin were being banned. In 2002, the United States food and drug administration
introduced a policy where blood donations were not accepted from the individuals who
have spent more than three months in the UK. Many policies were taken by the health care
organization of all the countries9. It was reported that at that time In U.S, the FDA had
imposed a ban on the donation of sperm due to the risk of the CJD.
Different measures can be taken while purifying artificial hormones, while installation
of the electrodes in the brain, cornea transplants8.
f) Socio-politico-economic
In the Lancet medical journal it was reported that CJD can be transmitted by blood
transfusion. It was reported that the UK government banned any individual who have
received any blood transfusion since 1980 January9. In fact manufacturing of proteins like
albumin were being banned. In 2002, the United States food and drug administration
introduced a policy where blood donations were not accepted from the individuals who
have spent more than three months in the UK. Many policies were taken by the health care
organization of all the countries9. It was reported that at that time In U.S, the FDA had
imposed a ban on the donation of sperm due to the risk of the CJD.
Different measures can be taken while purifying artificial hormones, while installation
of the electrodes in the brain, cornea transplants8.
8CREUTZFELDT- JAKOB DISEASE
References
1. Sikorska B, Knight R, Ironside JW, Liberski PP. Creutzfeldt-Jakob disease.
Neurodegenerative Diseases. 2012:76-90.
2. Head MW, Ironside JW. Creutzfeldt–Jakob disease: prion protein type, disease
phenotype and agent strain. Neuropathology and applied neurobiology. 2012 Jun
1;38(4):296-310.
3. Urwin PJ, Mackenzie JM, Llewelyn CA, Will RG, Hewitt PE. Creutzfeldt–Jakob
disease and blood transfusion: updated results of the UK Transfusion Medicine
Epidemiology Review Study. Vox sanguinis. 2016 May 1;110(4):310-6.
4. Harrington MG, Merril CR, Asher DM, Gajdusek DC. Abnormal proteins in the
cerebrospinal fluid of patients with Creutzfeldt–Jakob disease. New England
Journal of Medicine. 1986 Jul 31;315(5):279-83.
5. Sikorska B, Liberski PP. Human prion diseases: from Kuru to variant Creutzfeldt-
Jakob disease. InProtein Aggregation and Fibrillogenesis in Cerebral and Systemic
Amyloid Disease 2012 (pp. 457-496). Springer Netherlands.
6. Torres M, Cartier L, Matamala JM, Hernández N, Woehlbier U, Hetz C. Altered
Prion protein expression pattern in CSF as a biomarker for Creutzfeldt-Jakob
disease. PloS one. 2012 Apr 27;7(4):e36159.
7. Zanusso G, Monaco S, Pocchiari M, Caughey B. Advanced tests for early and
accurate diagnosis of Creutzfeldt-Jakob disease. Nature reviews. Neurology. 2016
Jun 1;12(6):325.
References
1. Sikorska B, Knight R, Ironside JW, Liberski PP. Creutzfeldt-Jakob disease.
Neurodegenerative Diseases. 2012:76-90.
2. Head MW, Ironside JW. Creutzfeldt–Jakob disease: prion protein type, disease
phenotype and agent strain. Neuropathology and applied neurobiology. 2012 Jun
1;38(4):296-310.
3. Urwin PJ, Mackenzie JM, Llewelyn CA, Will RG, Hewitt PE. Creutzfeldt–Jakob
disease and blood transfusion: updated results of the UK Transfusion Medicine
Epidemiology Review Study. Vox sanguinis. 2016 May 1;110(4):310-6.
4. Harrington MG, Merril CR, Asher DM, Gajdusek DC. Abnormal proteins in the
cerebrospinal fluid of patients with Creutzfeldt–Jakob disease. New England
Journal of Medicine. 1986 Jul 31;315(5):279-83.
5. Sikorska B, Liberski PP. Human prion diseases: from Kuru to variant Creutzfeldt-
Jakob disease. InProtein Aggregation and Fibrillogenesis in Cerebral and Systemic
Amyloid Disease 2012 (pp. 457-496). Springer Netherlands.
6. Torres M, Cartier L, Matamala JM, Hernández N, Woehlbier U, Hetz C. Altered
Prion protein expression pattern in CSF as a biomarker for Creutzfeldt-Jakob
disease. PloS one. 2012 Apr 27;7(4):e36159.
7. Zanusso G, Monaco S, Pocchiari M, Caughey B. Advanced tests for early and
accurate diagnosis of Creutzfeldt-Jakob disease. Nature reviews. Neurology. 2016
Jun 1;12(6):325.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CREUTZFELDT- JAKOB DISEASE
8. Goodnough LT. Blood management: transfusion medicine comes of age. The
Lancet. 2013 May 25;381(9880):1791.
9. Andréoletti O, Litaise C, Simmons H, Corbière F, Lugan S, Costes P, Schelcher F,
Vilette D, Grassi J, Lacroux C. Highly efficient prion transmission by blood
transfusion. PLoS pathogens. 2012 Jun 21;8(6):e1002782.
10. Jackson GS, Burk-Rafel J, Edgeworth JA, Sicilia A, Abdilahi S, Korteweg J,
Mackey J, Thomas C, Wang G, Schott JM, Mummery C. Population screening for
variant Creutzfeldt-Jakob disease using a novel blood test: diagnostic accuracy and
feasibility study. JAMA neurology. 2014 Apr 1;71(4):421-8.
8. Goodnough LT. Blood management: transfusion medicine comes of age. The
Lancet. 2013 May 25;381(9880):1791.
9. Andréoletti O, Litaise C, Simmons H, Corbière F, Lugan S, Costes P, Schelcher F,
Vilette D, Grassi J, Lacroux C. Highly efficient prion transmission by blood
transfusion. PLoS pathogens. 2012 Jun 21;8(6):e1002782.
10. Jackson GS, Burk-Rafel J, Edgeworth JA, Sicilia A, Abdilahi S, Korteweg J,
Mackey J, Thomas C, Wang G, Schott JM, Mummery C. Population screening for
variant Creutzfeldt-Jakob disease using a novel blood test: diagnostic accuracy and
feasibility study. JAMA neurology. 2014 Apr 1;71(4):421-8.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




