A Comparative Analysis of Kuru, Variant CJD, and Iatrogenic CJD
VerifiedAdded on 2020/04/13
|9
|1776
|48
Report
AI Summary
This report provides a comprehensive analysis of Creutzfeldt-Jakob disease (CJD), focusing on the distinctions between Kuru, variant CJD (vCJD), and iatrogenic CJD (iCJD). The report begins by defining CJD as a neurodegenerative disorder caused by misfolded prion proteins, leading to severe dementia, motor impairments, and ultimately, death. It highlights the different origins of these prion diseases: Kuru, historically linked to cannibalistic practices; vCJD, associated with the consumption of contaminated beef; and iatrogenic CJD, resulting from medical procedures involving infected tissues or instruments. The report details the common symptoms, such as dementia, muscle twitching, and loss of coordination, while also noting the unique features of each form. For example, vCJD is characterized by earlier onset and the presence of florid plaques. The report also discusses the pathophysiology, biological mechanisms, and diagnostic methods, including neuropathological examinations and biopsy, for each type of CJD. Finally, it references several studies to support the information provided. This analysis aims to provide a clear understanding of the similarities and differences among these forms of CJD and their implications.

Running head: CREUTZFELDT- JAKOB DISEASE
CREUTZFELDT- JAKOB DISEASE
Name of the Student
Name of the university
Author’s note
CREUTZFELDT- JAKOB DISEASE
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CREUTZFELDT- JAKOB DISEASE
Differences between kuru, variant CJD and iatrogenic CJD
JCD is a neurodegenerative disorder which is caused due to the altered folding of the host
prion proteins.
People suffering from CJD suffer from severe dementia, slurred speech, twitching of
muscles and tremors, slurred speech, loss of speech, blindness. Finally the person becomes
bedridden. Most of the people end up dying due to pneumonia (Head and Ironside 2012).
Human prion diseases can be hereditary, acquired or sporadic. The cause of the sporadic
Creutzfeldt-Jakob disease (CJD) is not known, but hereditary cases are associated with mutations
in the prion protein gene (PRNP) (Siroska et al.2012). The infections can also be transferred
from infected humans to other. vCJD is a new form of prion disease and resembles Bovine
spongioform encephalopathy (Lacroux et al. 2014).
Classic CJD is not related to vCJD and shows difference in many respects.
Kuru, vCJD, iCJD all are caused by the proteinacious infected particle formed due to the
altered folding of the host prion protein PrPc to infectious PrPsc (Siroska et al.2012). The
common signs and symptoms of al the prion diseases are almost same such as severe dementia,
insomnia, twitching of muscles, neuronal loss, loss of physical coordination, distorted speaking,
loss of speech, blindness, coma followed by death. Symptoms of Kuru involve compulsive
crying or laughing (Sikorska and Liberski 2012).
Kuru is a fatal nervous system disease and is highly prevalent during the 1950s and 1960
in people residing in the highlands of New Guinea. The fore people contracted this disease on
Differences between kuru, variant CJD and iatrogenic CJD
JCD is a neurodegenerative disorder which is caused due to the altered folding of the host
prion proteins.
People suffering from CJD suffer from severe dementia, slurred speech, twitching of
muscles and tremors, slurred speech, loss of speech, blindness. Finally the person becomes
bedridden. Most of the people end up dying due to pneumonia (Head and Ironside 2012).
Human prion diseases can be hereditary, acquired or sporadic. The cause of the sporadic
Creutzfeldt-Jakob disease (CJD) is not known, but hereditary cases are associated with mutations
in the prion protein gene (PRNP) (Siroska et al.2012). The infections can also be transferred
from infected humans to other. vCJD is a new form of prion disease and resembles Bovine
spongioform encephalopathy (Lacroux et al. 2014).
Classic CJD is not related to vCJD and shows difference in many respects.
Kuru, vCJD, iCJD all are caused by the proteinacious infected particle formed due to the
altered folding of the host prion protein PrPc to infectious PrPsc (Siroska et al.2012). The
common signs and symptoms of al the prion diseases are almost same such as severe dementia,
insomnia, twitching of muscles, neuronal loss, loss of physical coordination, distorted speaking,
loss of speech, blindness, coma followed by death. Symptoms of Kuru involve compulsive
crying or laughing (Sikorska and Liberski 2012).
Kuru is a fatal nervous system disease and is highly prevalent during the 1950s and 1960
in people residing in the highlands of New Guinea. The fore people contracted this disease on
2CREUTZFELDT- JAKOB DISEASE
eating the infected brains of the dead people as the funeral rites (Siroska et al.2012). Kuru
mainly occurs as a result of cannibalism or coming in to contact with open wounds or sores of
somebody with kuru. Many years later it was found that in this disease the infected brain
resembles sponges with holes (Sikorska and Liberski 2012).
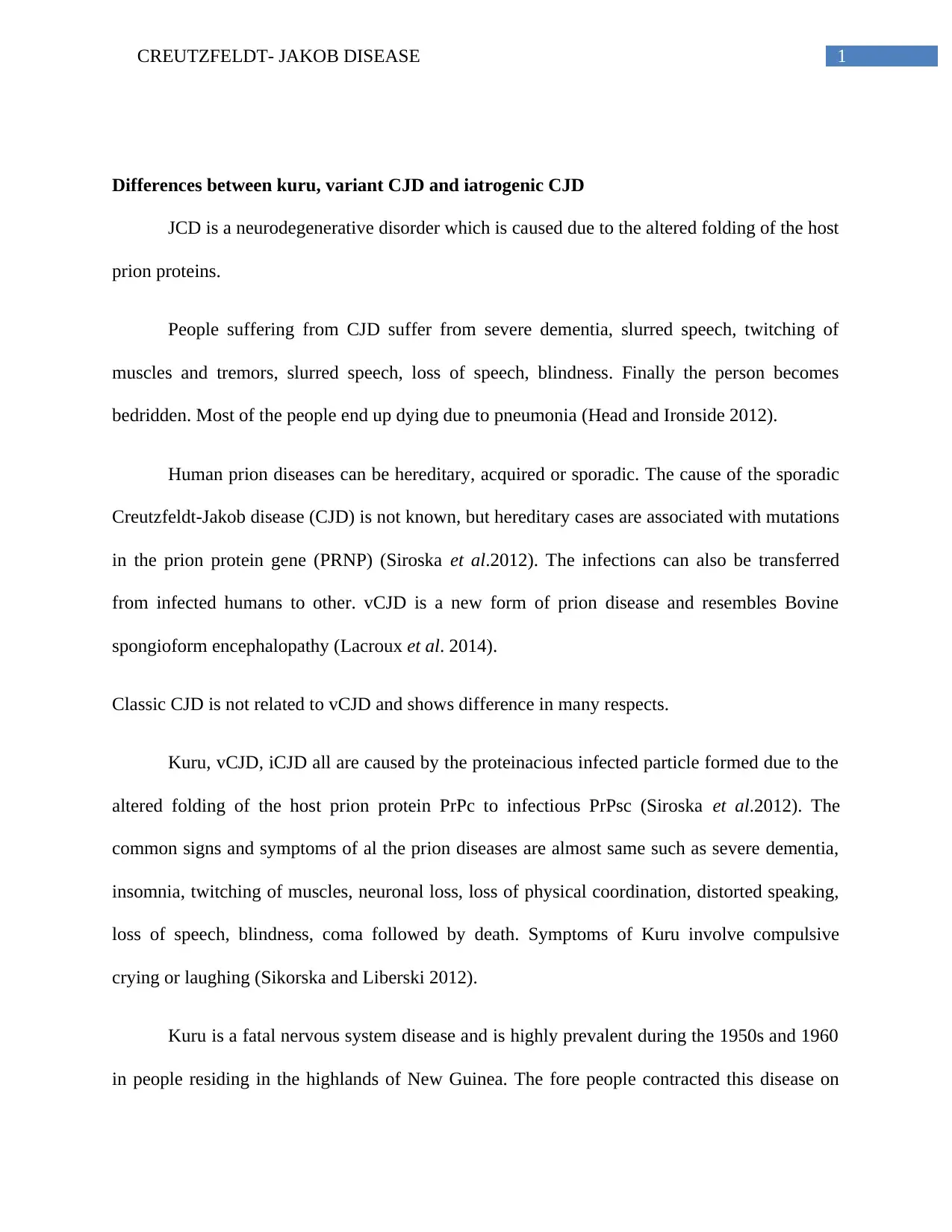
Figure 1: ( Hall et al. 2015)
Iatrogenic CJD is a neurodegenerative disorder that occurs due to the exposure to prion
infections (Siroska et al.2012). Exposure to the prion particles may occur due to medical
treatment that involves blood products or tissues from an infected individual. It can occur during
the organ transplants, preparation of hormones (Sikorska and Liberski 2012). One can be
contracted to this by unexpected incidents such as stab wounds by a needle that was in contact
with a brain or tissue infected with CJD.
Symptoms of Iatrogenic CJD are almost similar to that of sporadic CJD. It involves
depression, memory lapse with a rapid progression to dementia. iCJD is very rare in comparison
to kuru or variant CJD. Less than 1 percent of the cases have been found to contract acquired
CJD (Siroska et al.2012).
vCJD is a rare and fatal neurodegenerative disease. It belonged to the family of diseases
known as the transmissible spongiform encephalopathy (Lacroux et al.2014). vCJD is
eating the infected brains of the dead people as the funeral rites (Siroska et al.2012). Kuru
mainly occurs as a result of cannibalism or coming in to contact with open wounds or sores of
somebody with kuru. Many years later it was found that in this disease the infected brain
resembles sponges with holes (Sikorska and Liberski 2012).
Figure 1: ( Hall et al. 2015)
Iatrogenic CJD is a neurodegenerative disorder that occurs due to the exposure to prion
infections (Siroska et al.2012). Exposure to the prion particles may occur due to medical
treatment that involves blood products or tissues from an infected individual. It can occur during
the organ transplants, preparation of hormones (Sikorska and Liberski 2012). One can be
contracted to this by unexpected incidents such as stab wounds by a needle that was in contact
with a brain or tissue infected with CJD.
Symptoms of Iatrogenic CJD are almost similar to that of sporadic CJD. It involves
depression, memory lapse with a rapid progression to dementia. iCJD is very rare in comparison
to kuru or variant CJD. Less than 1 percent of the cases have been found to contract acquired
CJD (Siroska et al.2012).
vCJD is a rare and fatal neurodegenerative disease. It belonged to the family of diseases
known as the transmissible spongiform encephalopathy (Lacroux et al.2014). vCJD is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CREUTZFELDT- JAKOB DISEASE
differentiated from kuru and other CJD in the context that vCJd shows its onset at a much
younger age than that of CJD. In vCJD the amount of the amyloid plaques is much more than
that of classical CJD (Siroska et al.2012). Unlike Kuru and iCJD, vCJD is caused from the
consumption of contaminated meat products from cattle having a disease called bovine
Spongiform encephalopathy or ' mad cow disease'. According to findings, the infectious particle
responsible for the BSE in cattles is the same as the causative agent of vCJD. Symptoms are
same as that of the other classes’ of CJD.
vCJD as first discovered in 1996, and was prevalent mainly in Great Britain along with
many other European countries. The initial symptom of vCJD is different from the other forms of
CJD. It occurs in typically younger patients as compared to the other forms, whereas in the other
forms, the median age is about 68 years (Urwin et al.2016). The incubation period of vCJD is
unknown (Siroska et al.2012). vCJD have typical unique features, having prominent clinical
manifestations. The neurologic abnormalities are delayed. The duration of the illness lasts for
about 6 months after which the patient dies. The presence of florid plaques is rarely found in
other forms of CJD, but in vCJD it is present in large numbers (Lacroux et al.2014). The
infectious agent is usually not determined in the other two forms of CJD but is readily found in
the lymphoid tissues (Sikorska and Liberski 2012).
Variant Creutzfeldt-Jakob disease
vCJD is a rare neurodegenerative disorder caused by the infectious prior protein that was
discovered in the United Kingdom in the year 1996. It is characterized by the formation of holes
in the brain due to the accumulation of the amyloid plaques in the brain (Davidson et al.2014).
differentiated from kuru and other CJD in the context that vCJd shows its onset at a much
younger age than that of CJD. In vCJD the amount of the amyloid plaques is much more than
that of classical CJD (Siroska et al.2012). Unlike Kuru and iCJD, vCJD is caused from the
consumption of contaminated meat products from cattle having a disease called bovine
Spongiform encephalopathy or ' mad cow disease'. According to findings, the infectious particle
responsible for the BSE in cattles is the same as the causative agent of vCJD. Symptoms are
same as that of the other classes’ of CJD.
vCJD as first discovered in 1996, and was prevalent mainly in Great Britain along with
many other European countries. The initial symptom of vCJD is different from the other forms of
CJD. It occurs in typically younger patients as compared to the other forms, whereas in the other
forms, the median age is about 68 years (Urwin et al.2016). The incubation period of vCJD is
unknown (Siroska et al.2012). vCJD have typical unique features, having prominent clinical
manifestations. The neurologic abnormalities are delayed. The duration of the illness lasts for
about 6 months after which the patient dies. The presence of florid plaques is rarely found in
other forms of CJD, but in vCJD it is present in large numbers (Lacroux et al.2014). The
infectious agent is usually not determined in the other two forms of CJD but is readily found in
the lymphoid tissues (Sikorska and Liberski 2012).
Variant Creutzfeldt-Jakob disease
vCJD is a rare neurodegenerative disorder caused by the infectious prior protein that was
discovered in the United Kingdom in the year 1996. It is characterized by the formation of holes
in the brain due to the accumulation of the amyloid plaques in the brain (Davidson et al.2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CREUTZFELDT- JAKOB DISEASE
The agent responsible for the prion diseases in cows, Bovine spongiform encephalopathy is the
same agent for causing vCJD in humans (Siroska et al.2012).
Pathophysiology of Variant Creutzfeldt-Jakob disease
vCJD is exclusively caused by the prion protein designated as PrPsc without any
encoding nucleic acid. PrPSc is nothing but an altered form of the normal host functional prion
protein PrPc. Abnormal prion proteins are generated due to the abnormal folding of the PrPc
protein (Sikorska and Liberski 2012). PrPc is protinease sensitive but PrPsc are resistant to
proteases and hence deposit as amyloid plaques. The infectious prion proteins are transmissible
and self propagating. More abnormal prion proteins are produced; it converts rest of the normal
proteins to its abnormal isoforms rapidly (Lacroux et al.2014). It has been found that the
conformational change in the PrPc is caused due to the mutation in the PRNP gene, which
modifies the sequence of the amino acids. A valine or methionine polymorphism at the codon
number 129 of the PRNP gene is the probable cause of the disease (Lacroux et al.2014).
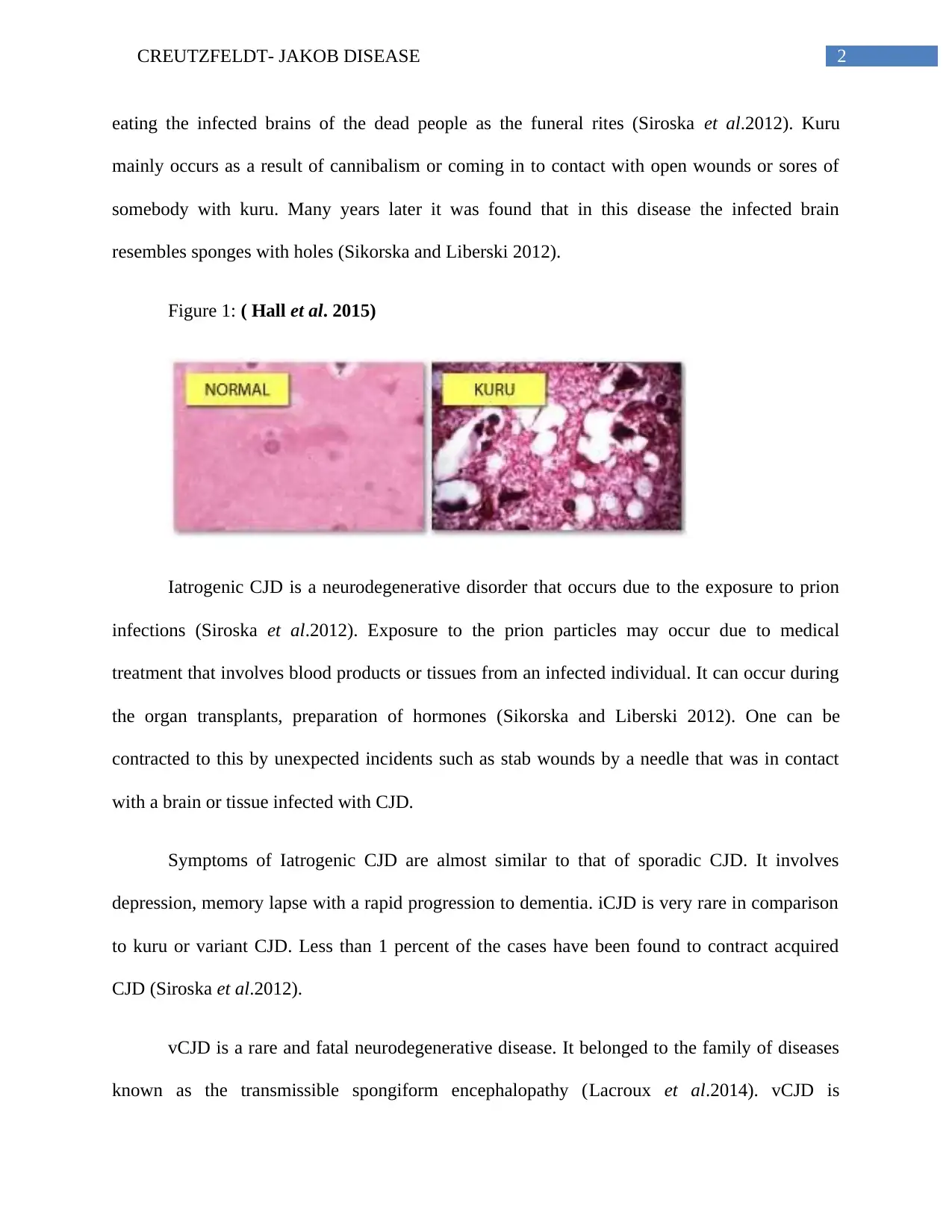
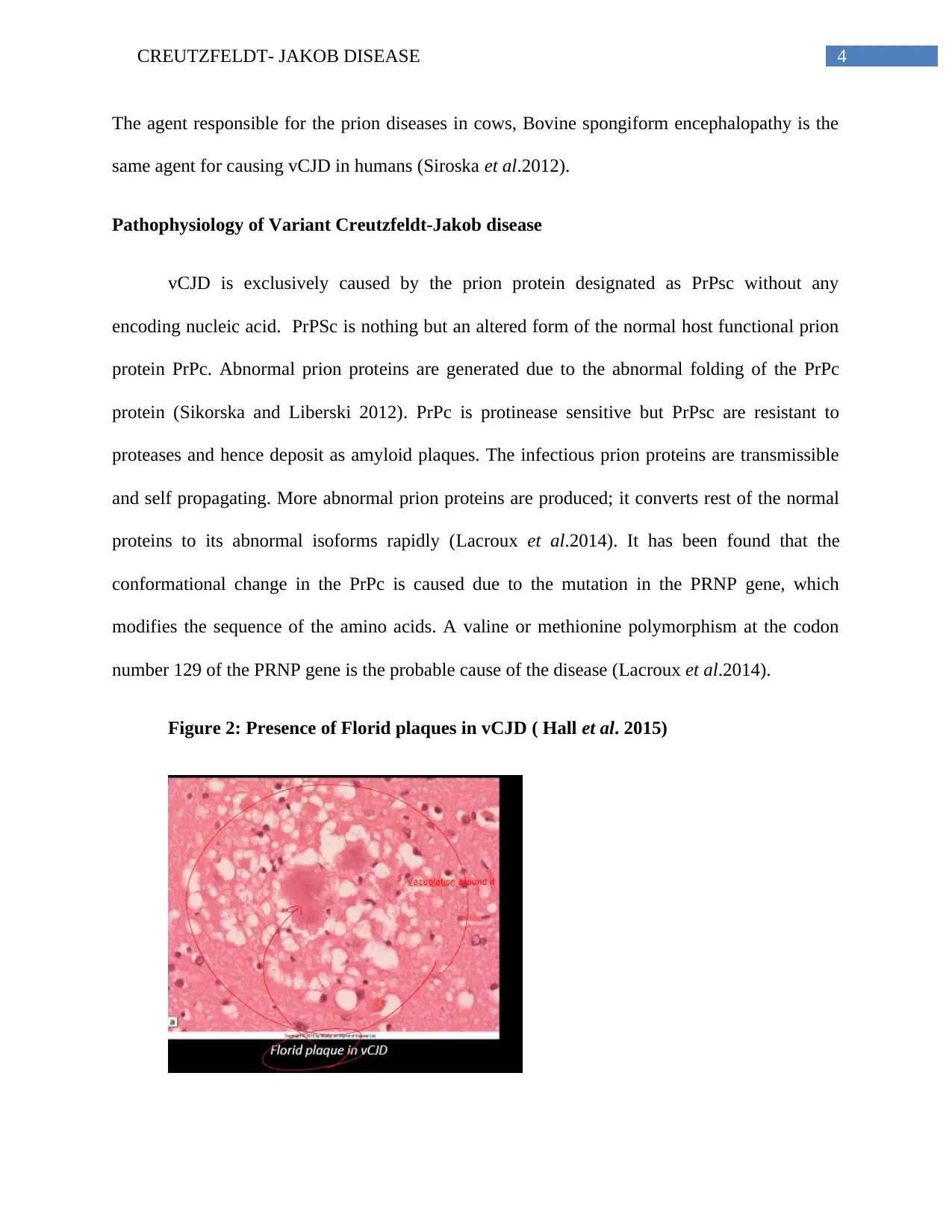
Figure 2: Presence of Florid plaques in vCJD ( Hall et al. 2015)
The agent responsible for the prion diseases in cows, Bovine spongiform encephalopathy is the
same agent for causing vCJD in humans (Siroska et al.2012).
Pathophysiology of Variant Creutzfeldt-Jakob disease
vCJD is exclusively caused by the prion protein designated as PrPsc without any
encoding nucleic acid. PrPSc is nothing but an altered form of the normal host functional prion
protein PrPc. Abnormal prion proteins are generated due to the abnormal folding of the PrPc
protein (Sikorska and Liberski 2012). PrPc is protinease sensitive but PrPsc are resistant to
proteases and hence deposit as amyloid plaques. The infectious prion proteins are transmissible
and self propagating. More abnormal prion proteins are produced; it converts rest of the normal
proteins to its abnormal isoforms rapidly (Lacroux et al.2014). It has been found that the
conformational change in the PrPc is caused due to the mutation in the PRNP gene, which
modifies the sequence of the amino acids. A valine or methionine polymorphism at the codon
number 129 of the PRNP gene is the probable cause of the disease (Lacroux et al.2014).
Figure 2: Presence of Florid plaques in vCJD ( Hall et al. 2015)
5CREUTZFELDT- JAKOB DISEASE
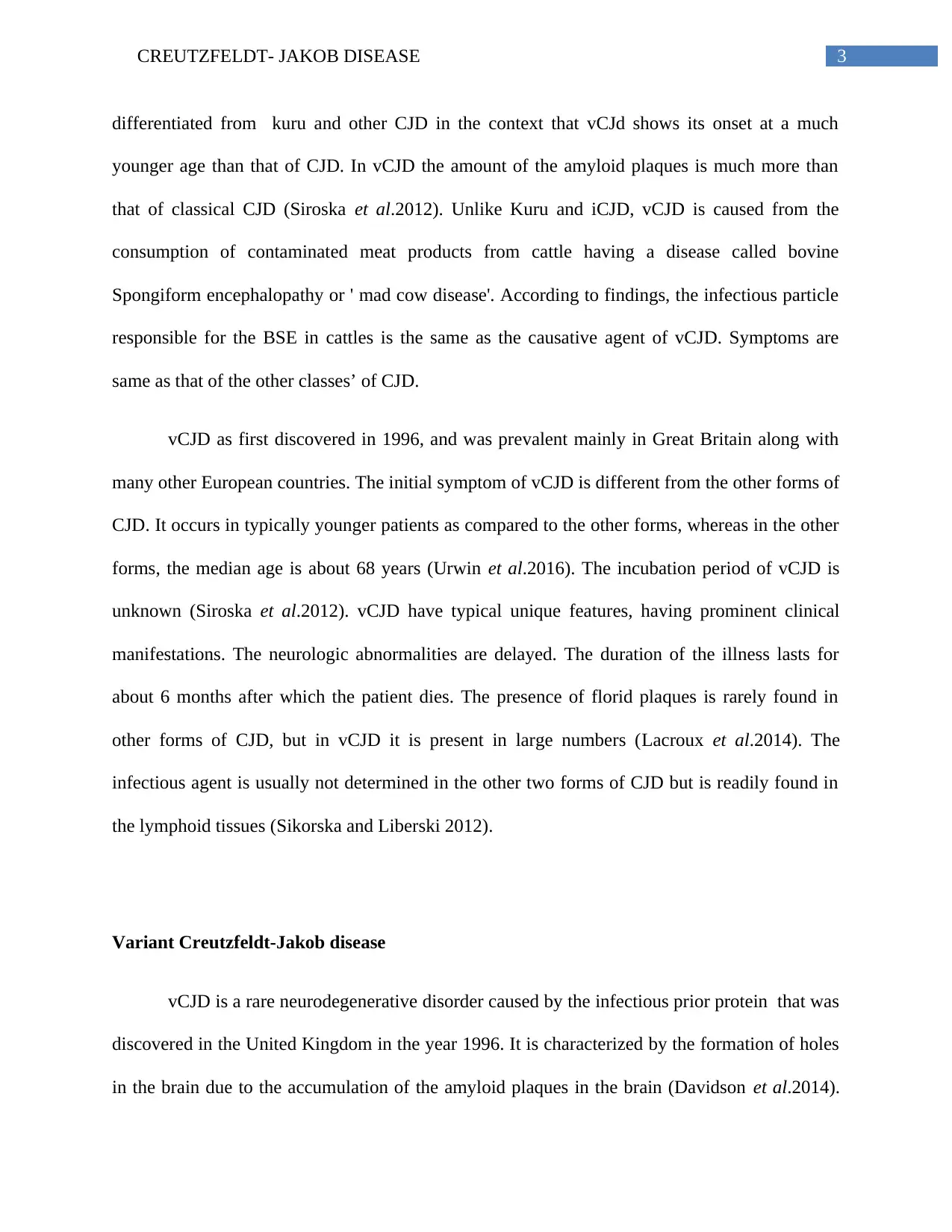
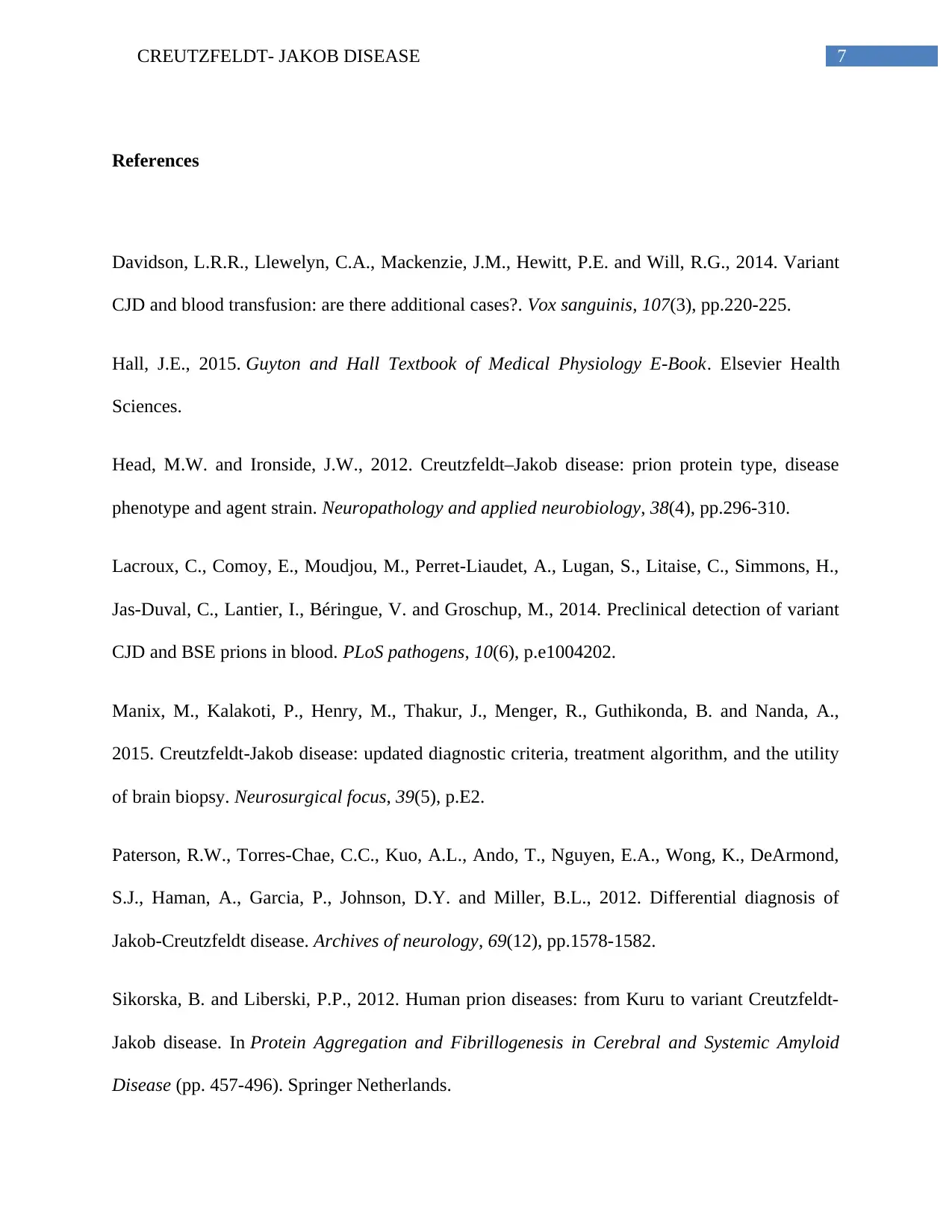
Figure 3: Altered protein conformation ( Hall et al. 2015)
Normally the host protein contains alpha helical structures, but in the altered protein beta
sheets are present.
Biological mechanism
According to Siroska et al.(2012) the time of the incubation period PrPsc is present in all
the tissue fluids, especially in the spinal fluids. At first intracytoplasmic vacuoles are formed in
the neurons. With the progression of the disease the vacuolization becomes more prominent and
the cortical neurophil resembles a sponge (Manix et al.2015). Advanced stage progresses with
neuronal loss, brain atrophy and gliosis. The purkinje cells of the brain are lost. In some diseases
related to prion infection, the PrPsc protein deposits as amyloid palques.
Diagnosis of Variant Creutzfeldt-Jakob disease
Variant CJD is normally diagnosed by neuropathology examination. At the initial stage
the disease remains asymptomatic with irreversible neurodegenerative loss (Siroska et al.2012).
The disease is diagnosed by autopsy, tonsil biopsy that exploits a vast tissue distribution of the
Figure 3: Altered protein conformation ( Hall et al. 2015)
Normally the host protein contains alpha helical structures, but in the altered protein beta
sheets are present.
Biological mechanism
According to Siroska et al.(2012) the time of the incubation period PrPsc is present in all
the tissue fluids, especially in the spinal fluids. At first intracytoplasmic vacuoles are formed in
the neurons. With the progression of the disease the vacuolization becomes more prominent and
the cortical neurophil resembles a sponge (Manix et al.2015). Advanced stage progresses with
neuronal loss, brain atrophy and gliosis. The purkinje cells of the brain are lost. In some diseases
related to prion infection, the PrPsc protein deposits as amyloid palques.
Diagnosis of Variant Creutzfeldt-Jakob disease
Variant CJD is normally diagnosed by neuropathology examination. At the initial stage
the disease remains asymptomatic with irreversible neurodegenerative loss (Siroska et al.2012).
The disease is diagnosed by autopsy, tonsil biopsy that exploits a vast tissue distribution of the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CREUTZFELDT- JAKOB DISEASE
infectious protein compared to other prion diseases. Biopsy is a 100% specific test for vCJD and
is specific and sensitive (Paterson et al.2012). Preclinical diagnosis is normally done by the
tonsil biopsy. Neuropathologic examination reveals amyloid plaques surrounded by vacuoles in
the brain which are known as florid plaques.
infectious protein compared to other prion diseases. Biopsy is a 100% specific test for vCJD and
is specific and sensitive (Paterson et al.2012). Preclinical diagnosis is normally done by the
tonsil biopsy. Neuropathologic examination reveals amyloid plaques surrounded by vacuoles in
the brain which are known as florid plaques.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CREUTZFELDT- JAKOB DISEASE
References
Davidson, L.R.R., Llewelyn, C.A., Mackenzie, J.M., Hewitt, P.E. and Will, R.G., 2014. Variant
CJD and blood transfusion: are there additional cases?. Vox sanguinis, 107(3), pp.220-225.
Hall, J.E., 2015. Guyton and Hall Textbook of Medical Physiology E-Book. Elsevier Health
Sciences.
Head, M.W. and Ironside, J.W., 2012. Creutzfeldt–Jakob disease: prion protein type, disease
phenotype and agent strain. Neuropathology and applied neurobiology, 38(4), pp.296-310.
Lacroux, C., Comoy, E., Moudjou, M., Perret-Liaudet, A., Lugan, S., Litaise, C., Simmons, H.,
Jas-Duval, C., Lantier, I., Béringue, V. and Groschup, M., 2014. Preclinical detection of variant
CJD and BSE prions in blood. PLoS pathogens, 10(6), p.e1004202.
Manix, M., Kalakoti, P., Henry, M., Thakur, J., Menger, R., Guthikonda, B. and Nanda, A.,
2015. Creutzfeldt-Jakob disease: updated diagnostic criteria, treatment algorithm, and the utility
of brain biopsy. Neurosurgical focus, 39(5), p.E2.
Paterson, R.W., Torres-Chae, C.C., Kuo, A.L., Ando, T., Nguyen, E.A., Wong, K., DeArmond,
S.J., Haman, A., Garcia, P., Johnson, D.Y. and Miller, B.L., 2012. Differential diagnosis of
Jakob-Creutzfeldt disease. Archives of neurology, 69(12), pp.1578-1582.
Sikorska, B. and Liberski, P.P., 2012. Human prion diseases: from Kuru to variant Creutzfeldt-
Jakob disease. In Protein Aggregation and Fibrillogenesis in Cerebral and Systemic Amyloid
Disease (pp. 457-496). Springer Netherlands.
References
Davidson, L.R.R., Llewelyn, C.A., Mackenzie, J.M., Hewitt, P.E. and Will, R.G., 2014. Variant
CJD and blood transfusion: are there additional cases?. Vox sanguinis, 107(3), pp.220-225.
Hall, J.E., 2015. Guyton and Hall Textbook of Medical Physiology E-Book. Elsevier Health
Sciences.
Head, M.W. and Ironside, J.W., 2012. Creutzfeldt–Jakob disease: prion protein type, disease
phenotype and agent strain. Neuropathology and applied neurobiology, 38(4), pp.296-310.
Lacroux, C., Comoy, E., Moudjou, M., Perret-Liaudet, A., Lugan, S., Litaise, C., Simmons, H.,
Jas-Duval, C., Lantier, I., Béringue, V. and Groschup, M., 2014. Preclinical detection of variant
CJD and BSE prions in blood. PLoS pathogens, 10(6), p.e1004202.
Manix, M., Kalakoti, P., Henry, M., Thakur, J., Menger, R., Guthikonda, B. and Nanda, A.,
2015. Creutzfeldt-Jakob disease: updated diagnostic criteria, treatment algorithm, and the utility
of brain biopsy. Neurosurgical focus, 39(5), p.E2.
Paterson, R.W., Torres-Chae, C.C., Kuo, A.L., Ando, T., Nguyen, E.A., Wong, K., DeArmond,
S.J., Haman, A., Garcia, P., Johnson, D.Y. and Miller, B.L., 2012. Differential diagnosis of
Jakob-Creutzfeldt disease. Archives of neurology, 69(12), pp.1578-1582.
Sikorska, B. and Liberski, P.P., 2012. Human prion diseases: from Kuru to variant Creutzfeldt-
Jakob disease. In Protein Aggregation and Fibrillogenesis in Cerebral and Systemic Amyloid
Disease (pp. 457-496). Springer Netherlands.
8CREUTZFELDT- JAKOB DISEASE
Sikorska, B., Knight, R., Ironside, J.W. and Liberski, P.P., 2012. Creutzfeldt-Jakob
disease. Neurodegenerative Diseases, pp.76-90.
Urwin, P.J.M., Mackenzie, J.M., Llewelyn, C.A., Will, R.G. and Hewitt, P.E., 2016. Creutzfeldt–
Jakob disease and blood transfusion: updated results of the UK Transfusion Medicine
Epidemiology Review Study. Vox sanguinis, 110(4), pp.310-316.
Sikorska, B., Knight, R., Ironside, J.W. and Liberski, P.P., 2012. Creutzfeldt-Jakob
disease. Neurodegenerative Diseases, pp.76-90.
Urwin, P.J.M., Mackenzie, J.M., Llewelyn, C.A., Will, R.G. and Hewitt, P.E., 2016. Creutzfeldt–
Jakob disease and blood transfusion: updated results of the UK Transfusion Medicine
Epidemiology Review Study. Vox sanguinis, 110(4), pp.310-316.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




