UCL Assignment: Critical Appraisal of Wakefield et al. (Lancet) Paper
VerifiedAdded on 2023/01/03
|8
|6867
|79
Report
AI Summary
This report offers a critical appraisal of the Wakefield et al. paper, focusing on its relevance, originality, and research hypothesis. The analysis examines the paper's methodology, including the use of CASP checklists for qualitative research and randomized controlled trials. The appraisal assesses the study's validity, results, and local applicability, providing a systematic evaluation of the research. The report considers the importance of the topic, the study's originality, and the clarity of the research hypothesis. It evaluates the study's impact on healthcare and patient safety, highlighting the significance of critical appraisal in scientific publications. The report also includes an overview of the educational program that was conducted to improve patient safety culture. The study aimed to determine the effect of empowering nurses and supervisors through an educational program on patient safety culture in adult ICUs. The intervention consisted of a two-day workshop, hanging posters, and distributing pamphlets that covered topics such as patient safety, patient safety culture, speak up about safety issues, and the skills of Team Strategies and Tools to Enhance Performance and Patient Safety.
R E S E A R C H A R T I C L E Open Access
The effect of nurse empowerment
educationalprogram on patient safety
culture:a randomized controlled trial
Maryam Amiri1
, Zahra Khademian1* and Reza Nikandish2
Abstract
Background:The complexity of patients’condition and treatment processes in intensive care units (ICUs) predispo
patients to more hazardous events.Effective patient safety culture is related to lowering the rate of patients’
complications and fewer adverse events.The present study aimed to determine the effect of empowering nurses
and supervisors through an educationalprogram on patient safety culture in adult ICUs.
Methods:A randomized controlled trialwas conducted during April–September 2015 in 6 adult ICUs at Namazi
Hospital,Shiraz,Iran.A total of 60 nurses and 20 supervisors were selected through proportional stratified samp
census,respectively,and randomly assigned to the experimental and control groups.The intervention consisted of a
two-day workshop,hanging posters,and distributing pamphlets that covered topics such as patient safety,patient
safety culture,speak up about safety issues,and the skills of Team Strategies and Tools to Enhance Performance and
Patient Safety.Data were collected through a hospital survey on patient safety culture.Eventually,61 participants
completed the study.Data were analyzed using descriptive statistics,independent-samples t-test,paired-samples t-test,
and Chi-square test.P < 0.05 was considered statistically significant.
Results: In the experimentalgroup,the totalpost-test mean scores of the patient safety culture (3.46 ± 0.26) was
significantly higher than that of the controlgroup (2.84 ± 0.37,P < 0.001).It was also higher than that of the pre-
test (2.91 ± 0.4,P < 0.001).Additionally,significant improvements were observed in 5 out of 12 dimensions in the
experimentalgroup.However,dimensions such as non-punitive response to errors and the events reported did
not improve significantly.
Conclusion:Empowering nurses and supervisors could improve the overallpatient safety culture.Nonetheless,
additional actions are required to improve areas such as reporting the events and non-punitive response to
Trial registration: IRCT2015053122494N1.Date registered:March 2,2016.
Keywords: Culture,Intensive care units,Nursing,Supervisory,Nurses,Patient safety,Patient safety culture,Safety
Background
Patient safetyis an importantelementin offering
high-qualityhealth careservices.However,it is esti-
mated that approximately 400,000 annualdeaths are re-
lated to preventableharms [1]. The complexityof
patients’condition and treatment processes in Intensive
Care Unit (ICU) predisposes patients to more hazardous
events [2].In a prospective study,during 2013–2014,the
rate ofadverse events per 1000 patient-days in an ICU
was 80.5 in which 45% were preventable [3].The epi-
demiology ofmedicalerrors in Iran is ambiguous.Zar-
garzadeh hasestimated that24,500 annualdeathsare
related to medicalerrors[4]. In addition,in an ICU,
among 307 medication doses,214 (69.7%)errors were
identified during administration (n = 132,42.99%),pre-
scription (n = 74,24.1%),and transcription (n = 8,2.61%)
of medications [5].Moreover,48 medication errors per
100 orders were observed in a pediatric ICU [6].
* Correspondence:Zahrakhademian@yahoo.com;khademian@sums.ac.ir;
zahrakhademian@gmail.com
1Department of Nursing,Schoolof Nursing and Midwifery,Shiraz University
of MedicalSciences,Shiraz,Iran
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Amiri et al.BMC MedicalEducation (2018) 18:158
https://doi.org/10.1186/s12909-018-1255-6
The effect of nurse empowerment
educationalprogram on patient safety
culture:a randomized controlled trial
Maryam Amiri1
, Zahra Khademian1* and Reza Nikandish2
Abstract
Background:The complexity of patients’condition and treatment processes in intensive care units (ICUs) predispo
patients to more hazardous events.Effective patient safety culture is related to lowering the rate of patients’
complications and fewer adverse events.The present study aimed to determine the effect of empowering nurses
and supervisors through an educationalprogram on patient safety culture in adult ICUs.
Methods:A randomized controlled trialwas conducted during April–September 2015 in 6 adult ICUs at Namazi
Hospital,Shiraz,Iran.A total of 60 nurses and 20 supervisors were selected through proportional stratified samp
census,respectively,and randomly assigned to the experimental and control groups.The intervention consisted of a
two-day workshop,hanging posters,and distributing pamphlets that covered topics such as patient safety,patient
safety culture,speak up about safety issues,and the skills of Team Strategies and Tools to Enhance Performance and
Patient Safety.Data were collected through a hospital survey on patient safety culture.Eventually,61 participants
completed the study.Data were analyzed using descriptive statistics,independent-samples t-test,paired-samples t-test,
and Chi-square test.P < 0.05 was considered statistically significant.
Results: In the experimentalgroup,the totalpost-test mean scores of the patient safety culture (3.46 ± 0.26) was
significantly higher than that of the controlgroup (2.84 ± 0.37,P < 0.001).It was also higher than that of the pre-
test (2.91 ± 0.4,P < 0.001).Additionally,significant improvements were observed in 5 out of 12 dimensions in the
experimentalgroup.However,dimensions such as non-punitive response to errors and the events reported did
not improve significantly.
Conclusion:Empowering nurses and supervisors could improve the overallpatient safety culture.Nonetheless,
additional actions are required to improve areas such as reporting the events and non-punitive response to
Trial registration: IRCT2015053122494N1.Date registered:March 2,2016.
Keywords: Culture,Intensive care units,Nursing,Supervisory,Nurses,Patient safety,Patient safety culture,Safety
Background
Patient safetyis an importantelementin offering
high-qualityhealth careservices.However,it is esti-
mated that approximately 400,000 annualdeaths are re-
lated to preventableharms [1]. The complexityof
patients’condition and treatment processes in Intensive
Care Unit (ICU) predisposes patients to more hazardous
events [2].In a prospective study,during 2013–2014,the
rate ofadverse events per 1000 patient-days in an ICU
was 80.5 in which 45% were preventable [3].The epi-
demiology ofmedicalerrors in Iran is ambiguous.Zar-
garzadeh hasestimated that24,500 annualdeathsare
related to medicalerrors[4]. In addition,in an ICU,
among 307 medication doses,214 (69.7%)errors were
identified during administration (n = 132,42.99%),pre-
scription (n = 74,24.1%),and transcription (n = 8,2.61%)
of medications [5].Moreover,48 medication errors per
100 orders were observed in a pediatric ICU [6].
* Correspondence:Zahrakhademian@yahoo.com;khademian@sums.ac.ir;
zahrakhademian@gmail.com
1Department of Nursing,Schoolof Nursing and Midwifery,Shiraz University
of MedicalSciences,Shiraz,Iran
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Amiri et al.BMC MedicalEducation (2018) 18:158
https://doi.org/10.1186/s12909-018-1255-6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Poor communication and collaboration [7],lack of
knowledge,and inadequatetraining wereamongthe
main causes ofnursing errors in ICUs [8].Studies have
shown the lack ofcommunication skills in nurses and
nursing students [9,10].Hence,a training program for
nurses on patient safety alongside with strategies to im-
proveprofessionalcommunication isrequired to im-
prove patient safety.
High mortality and morbidity associated with medical
errors indicatethe importanceof promotingpatient
safety in critical care units.Nurses play a key role in im-
proving patientsafety due to their continuous presence
at patients’bedsides and interaction with their families
and otherhealthcareprofessionals[11].For instance,
criticalcare unitnurses have often reported thatthey
identified and corrected errors such as medication and
proceduralerrors related to nurses and other caregivers
[12].Henneman etal. identified multiple strategiesto
identify the patient,recognize other team members,and
the plan ofcare,which nurses used to detect,discon-
tinue,and correct errors in critical care settings [13].
Research findings indicated that a strong patient safety
culture is associated with a lower rate ofpatients’com-
plications and fewer adverse events [14,15].It is defined
as a culture whereby nurses are aware of errors and are
encouraged to discussthem.This, in turn, improves
their ability to learn from pastmistakes and take cor-
rective measures [16].
A meta-analysis,including 11 descriptive studieson
hospitalstaff,showed that only 8.3 and 32.3% of the re-
spondentsof the reviewed articleshave rated patient
safety culture in Iran as excellent and very good,respect-
ively [17].The importantrole of patientsafety culture
necessitates improvementof these strategies in clinical
settings.Nevertheless,interventionsthat may improve
patient safety culture are not adequately defined [18].In
a study,the positive effects ofsome interventions,such
as executive walk rounds[19] and the role of nurse
managersin regular assessmentand supportof the
safety culture were reported [20].Consequently,the par-
ticipation of nurse managers in the planning and imple-
mentationof strategies,to improve patient safety
culture,may reinforce these strategies [18].
Severalstudies have reported the effects ofnurse em-
powermentinterventionson patientsafety culture.A
type ofstrategy is an educationalprogram,such as on-
line module,addressing patientsafety which increases
positive scores ofnurses in two dimensions ofpatient
safety culture (i.e.“non-punitive response to errors” and
“frequency of event reporting”) [21].Teaching teamwork
also improves staff perception of patient safety culture in
the emergency department [22].Another empowerment
strategy is to encourage nurses to speak up.Sayre (2010)
reported thatnursesbehaviortowardspatientsafety
protection increased when encouraged to speak up in a
situation of a threat to patient safety [23].
In order to improve the quality ofcare and patient
safety,the Institute ofMedicine (2003)recommended a
reform in health profession education [24]. Accordingly,
the Quality and Safety Education for Nurses (QSEN) pro-
ject was introduced to train nurses on the required com-
petencies to improve the quality of care and patient safety
[25]. Considering the important role of nurses and leaders
in ensuring patient safety and in providing a strong patient
safety culture,we developed and studied the effects of an
innovative empowerment program on patient safety cul-
ture.This program is unique in a sense thatit involves
nurses and supervisors with an integrated exclusive educa-
tionalprogram which encourages them to speak up.The
present study aimed to determine the effect of empower-
ing nurses and supervisors through an educationalpro-
gram on patient safety culture in adult ICUs.
Methods
This randomized controlled trialwith a pre-testand
post-test control groups was conducted during
April–September2015 in 6 adult ICUs at Namazi
Hospital, Shiraz, Iran. All the above-mentioned ICUs were
similar in terms of patient safety policies. The study popu-
lation included 160 nurses and 20 supervisors. The nurse:-
patientratio in these wardswas 1:2.The sample size
consisted of60 nurses and 20 supervisors.The nurses
were selected based on proportionalstratified sampling.
Therefore,the number of selected nurses from each ICU
was proportionalto the total numberof its nurses.
Supervisors were nurses with atleasta Bachelor’s de-
gree and responsible for oversightnursing services in
the studied ICUs.Note that the supervisorsdid not
provide direct patient care.All supervisors at the hos-
pital participated in the study.To randomly allocate
nurses,a number was assigned to each ICU and catego-
rized into the controland experimentalgroups,based
on permuted block randomization.In total,30 nurses
from ICUs number 1,3, and 6 (surgical,neurosurgical,
and generalICU) were assigned to the experimental
group.In addition,30 nurses from ICUs number 2,4,
and 5 (medical,neurosurgical,and generalICU) were
assigned to thecontrol group. Based on permuted
block randomization,all supervisorsat the hospital
were assigned to the experimental(n = 10) and control
(n = 10)groups.The experimentalgroup,including 30
nurses (ICUs number 1,3, and 6)and 10 supervisors
received the educationalempowermentprogram.The
controlgroup included 30 nurses (ICUs number 2,4,
and 5) and 10 supervisorsthat did not receiveany
intervention.The inclusion criteria were having at least
6 monthsexperience in an adultICU and at leasta
Bachelor’sdegreein nursing. The exclusion criteria
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 2 of 8
knowledge,and inadequatetraining wereamongthe
main causes ofnursing errors in ICUs [8].Studies have
shown the lack ofcommunication skills in nurses and
nursing students [9,10].Hence,a training program for
nurses on patient safety alongside with strategies to im-
proveprofessionalcommunication isrequired to im-
prove patient safety.
High mortality and morbidity associated with medical
errors indicatethe importanceof promotingpatient
safety in critical care units.Nurses play a key role in im-
proving patientsafety due to their continuous presence
at patients’bedsides and interaction with their families
and otherhealthcareprofessionals[11].For instance,
criticalcare unitnurses have often reported thatthey
identified and corrected errors such as medication and
proceduralerrors related to nurses and other caregivers
[12].Henneman etal. identified multiple strategiesto
identify the patient,recognize other team members,and
the plan ofcare,which nurses used to detect,discon-
tinue,and correct errors in critical care settings [13].
Research findings indicated that a strong patient safety
culture is associated with a lower rate ofpatients’com-
plications and fewer adverse events [14,15].It is defined
as a culture whereby nurses are aware of errors and are
encouraged to discussthem.This, in turn, improves
their ability to learn from pastmistakes and take cor-
rective measures [16].
A meta-analysis,including 11 descriptive studieson
hospitalstaff,showed that only 8.3 and 32.3% of the re-
spondentsof the reviewed articleshave rated patient
safety culture in Iran as excellent and very good,respect-
ively [17].The importantrole of patientsafety culture
necessitates improvementof these strategies in clinical
settings.Nevertheless,interventionsthat may improve
patient safety culture are not adequately defined [18].In
a study,the positive effects ofsome interventions,such
as executive walk rounds[19] and the role of nurse
managersin regular assessmentand supportof the
safety culture were reported [20].Consequently,the par-
ticipation of nurse managers in the planning and imple-
mentationof strategies,to improve patient safety
culture,may reinforce these strategies [18].
Severalstudies have reported the effects ofnurse em-
powermentinterventionson patientsafety culture.A
type ofstrategy is an educationalprogram,such as on-
line module,addressing patientsafety which increases
positive scores ofnurses in two dimensions ofpatient
safety culture (i.e.“non-punitive response to errors” and
“frequency of event reporting”) [21].Teaching teamwork
also improves staff perception of patient safety culture in
the emergency department [22].Another empowerment
strategy is to encourage nurses to speak up.Sayre (2010)
reported thatnursesbehaviortowardspatientsafety
protection increased when encouraged to speak up in a
situation of a threat to patient safety [23].
In order to improve the quality ofcare and patient
safety,the Institute ofMedicine (2003)recommended a
reform in health profession education [24]. Accordingly,
the Quality and Safety Education for Nurses (QSEN) pro-
ject was introduced to train nurses on the required com-
petencies to improve the quality of care and patient safety
[25]. Considering the important role of nurses and leaders
in ensuring patient safety and in providing a strong patient
safety culture,we developed and studied the effects of an
innovative empowerment program on patient safety cul-
ture.This program is unique in a sense thatit involves
nurses and supervisors with an integrated exclusive educa-
tionalprogram which encourages them to speak up.The
present study aimed to determine the effect of empower-
ing nurses and supervisors through an educationalpro-
gram on patient safety culture in adult ICUs.
Methods
This randomized controlled trialwith a pre-testand
post-test control groups was conducted during
April–September2015 in 6 adult ICUs at Namazi
Hospital, Shiraz, Iran. All the above-mentioned ICUs were
similar in terms of patient safety policies. The study popu-
lation included 160 nurses and 20 supervisors. The nurse:-
patientratio in these wardswas 1:2.The sample size
consisted of60 nurses and 20 supervisors.The nurses
were selected based on proportionalstratified sampling.
Therefore,the number of selected nurses from each ICU
was proportionalto the total numberof its nurses.
Supervisors were nurses with atleasta Bachelor’s de-
gree and responsible for oversightnursing services in
the studied ICUs.Note that the supervisorsdid not
provide direct patient care.All supervisors at the hos-
pital participated in the study.To randomly allocate
nurses,a number was assigned to each ICU and catego-
rized into the controland experimentalgroups,based
on permuted block randomization.In total,30 nurses
from ICUs number 1,3, and 6 (surgical,neurosurgical,
and generalICU) were assigned to the experimental
group.In addition,30 nurses from ICUs number 2,4,
and 5 (medical,neurosurgical,and generalICU) were
assigned to thecontrol group. Based on permuted
block randomization,all supervisorsat the hospital
were assigned to the experimental(n = 10) and control
(n = 10)groups.The experimentalgroup,including 30
nurses (ICUs number 1,3, and 6)and 10 supervisors
received the educationalempowermentprogram.The
controlgroup included 30 nurses (ICUs number 2,4,
and 5) and 10 supervisorsthat did not receiveany
intervention.The inclusion criteria were having at least
6 monthsexperience in an adultICU and at leasta
Bachelor’sdegreein nursing. The exclusion criteria
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 2 of 8
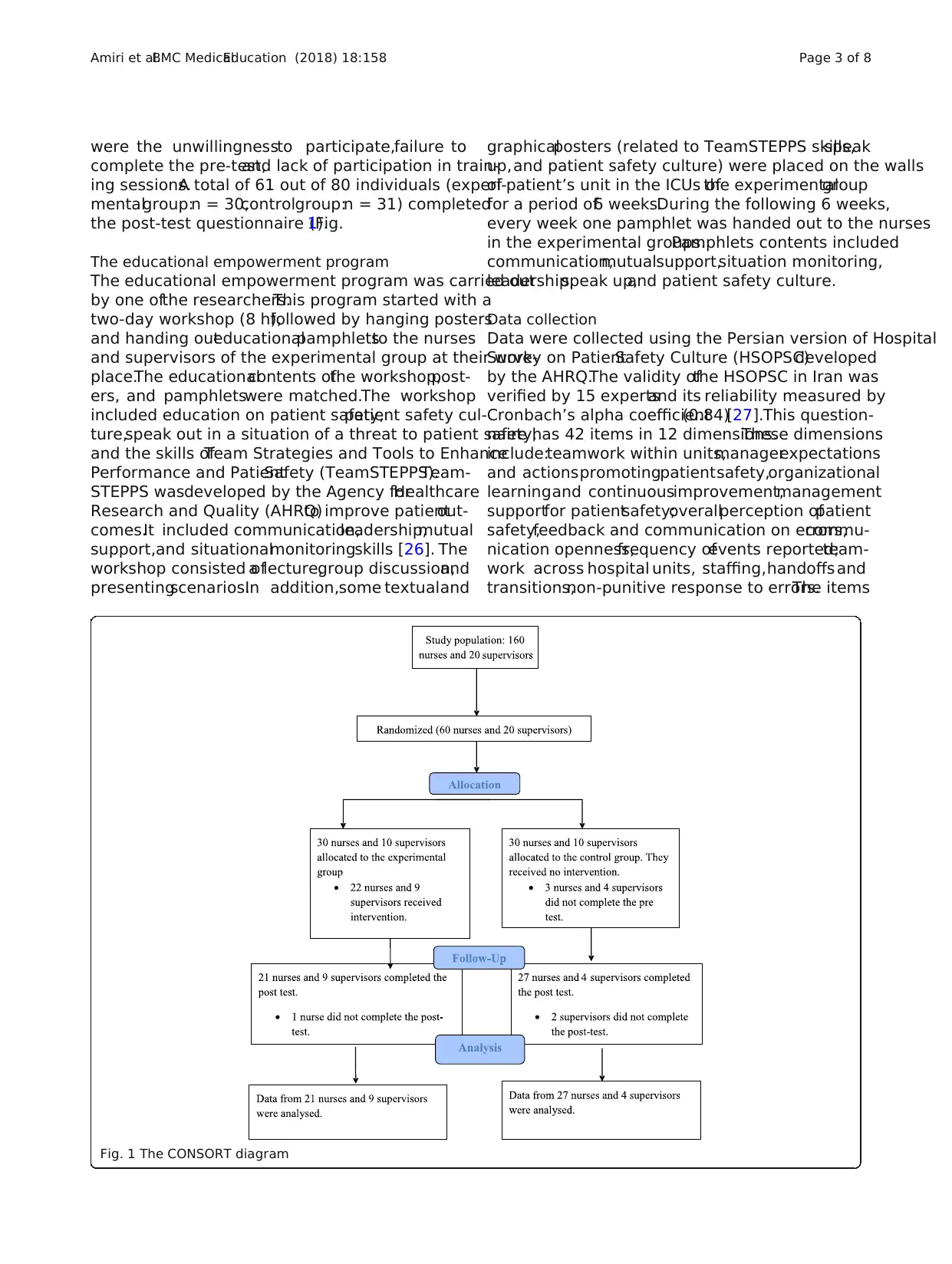
were the unwillingnessto participate,failure to
complete the pre-test,and lack of participation in train-
ing sessions.A total of 61 out of 80 individuals (experi-
mentalgroup:n = 30,controlgroup:n = 31) completed
the post-test questionnaire (Fig.1).
The educational empowerment program
The educational empowerment program was carried out
by one ofthe researchers.This program started with a
two-day workshop (8 h),followed by hanging posters
and handing outeducationalpamphletsto the nurses
and supervisors of the experimental group at their work-
place.The educationalcontents ofthe workshop,post-
ers, and pamphletswere matched.The workshop
included education on patient safety,patient safety cul-
ture,speak out in a situation of a threat to patient safety,
and the skills ofTeam Strategies and Tools to Enhance
Performance and PatientSafety (TeamSTEPPS).Team-
STEPPS wasdeveloped by the Agency forHealthcare
Research and Quality (AHRQ)to improve patientout-
comes.It included communication,leadership,mutual
support,and situationalmonitoringskills [26]. The
workshop consisted ofa lecture,group discussion,and
presentingscenarios.In addition,some textualand
graphicalposters (related to TeamSTEPPS skills,speak
up,and patient safety culture) were placed on the walls
of patient’s unit in the ICUs ofthe experimentalgroup
for a period of6 weeks.During the following 6 weeks,
every week one pamphlet was handed out to the nurses
in the experimental groups.Pamphlets contents included
communication,mutualsupport,situation monitoring,
leadership,speak up,and patient safety culture.
Data collection
Data were collected using the Persian version of Hospital
Survey on PatientSafety Culture (HSOPSC)developed
by the AHRQ.The validity ofthe HSOPSC in Iran was
verified by 15 expertsand its reliability measured by
Cronbach’s alpha coefficient(0.84)[27].This question-
naire has 42 items in 12 dimensions.These dimensions
include:teamwork within units,managerexpectations
and actionspromotingpatientsafety,organizational
learningand continuousimprovement,management
supportfor patientsafety;overallperception ofpatient
safety,feedback and communication on errors,commu-
nication openness,frequency ofevents reported;team-
work across hospital units, staffing,handoffs and
transitions,non-punitive response to errors.The items
Fig. 1 The CONSORT diagram
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 3 of 8
complete the pre-test,and lack of participation in train-
ing sessions.A total of 61 out of 80 individuals (experi-
mentalgroup:n = 30,controlgroup:n = 31) completed
the post-test questionnaire (Fig.1).
The educational empowerment program
The educational empowerment program was carried out
by one ofthe researchers.This program started with a
two-day workshop (8 h),followed by hanging posters
and handing outeducationalpamphletsto the nurses
and supervisors of the experimental group at their work-
place.The educationalcontents ofthe workshop,post-
ers, and pamphletswere matched.The workshop
included education on patient safety,patient safety cul-
ture,speak out in a situation of a threat to patient safety,
and the skills ofTeam Strategies and Tools to Enhance
Performance and PatientSafety (TeamSTEPPS).Team-
STEPPS wasdeveloped by the Agency forHealthcare
Research and Quality (AHRQ)to improve patientout-
comes.It included communication,leadership,mutual
support,and situationalmonitoringskills [26]. The
workshop consisted ofa lecture,group discussion,and
presentingscenarios.In addition,some textualand
graphicalposters (related to TeamSTEPPS skills,speak
up,and patient safety culture) were placed on the walls
of patient’s unit in the ICUs ofthe experimentalgroup
for a period of6 weeks.During the following 6 weeks,
every week one pamphlet was handed out to the nurses
in the experimental groups.Pamphlets contents included
communication,mutualsupport,situation monitoring,
leadership,speak up,and patient safety culture.
Data collection
Data were collected using the Persian version of Hospital
Survey on PatientSafety Culture (HSOPSC)developed
by the AHRQ.The validity ofthe HSOPSC in Iran was
verified by 15 expertsand its reliability measured by
Cronbach’s alpha coefficient(0.84)[27].This question-
naire has 42 items in 12 dimensions.These dimensions
include:teamwork within units,managerexpectations
and actionspromotingpatientsafety,organizational
learningand continuousimprovement,management
supportfor patientsafety;overallperception ofpatient
safety,feedback and communication on errors,commu-
nication openness,frequency ofevents reported;team-
work across hospital units, staffing,handoffs and
transitions,non-punitive response to errors.The items
Fig. 1 The CONSORT diagram
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 3 of 8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
were answered on a five-pointLikertscale,from com-
pletely disagree (1) to completely agree (5) or from never
(1) to always (5).There were a few negatively worded
items in the questionnaire thatwere reverse coded.If
the proportion of respondentswho answered “com-
pletely agree”/“agree”,or “always”/“most of the time” on
each item was more than 50%,this was considered as
strong,otherwise (below 50%) as the weak point ofthe
safety culture.In addition to these 42 questions,there
was a single item on patientsafety grading in the unit.
This item was answered on a five-point Likert scale from
excellent(score = 5)to failing (score = 1)and was ana-
lyzed separately as a single item [20,28].The pre-test
was completed individually before the workshop.Three
months after the workshop,the post-test was conducted
individually in both groups.
Data analysis
Statisticalanalysis was carried outusing the SPSS soft-
ware version 18.0. The results of One-Sample
Kolmogorov-Smirnovshowednormal distributionof
data before (P = 0.72)and after (P = 0.96)the interven-
tion,except for the single item on patient safety grading.
Descriptive statistics was used to describe age,sex,edu-
cation,position,and the total scores of the patient safety
culture and its dimensions.To compare the mean scores
between thetwo groupsand within each group,the
independent-samplest-test and paired-samplest-test
were used.The single item on patient safety grading was
compared between the controland experimentalgroups
using the Mann-Whitney test.This item was compared
before and after the intervention in each group using the
Wilcoxon test.The effect size for paired t-test was calcu-
lated by the Cohen (1988) equation as follows:
Effect size ¼ d ¼
M1‐M2
S pooled
; Spooled¼
ffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffi
S12 þ S22
2
r
Where M1 and M2 are post-test means of the experi-
mental and control groups,respectively.Spooled:Pooled
standard deviation,and S1 and S2:Post-teststandard
deviationsof the experimentaland control groups,
respectively.
The effectsize of 0.2,0.5,and 0.8 wasconsidered
small,medium,and large,respectively [29].P < 0.05 was
considered statistically significant.
Results
The sample size included 48 nurses and 13 supervisors.
The experimentaland controlgroupswere homoge-
neous in terms of age,sex,marital status,education,and
position (Table 1).
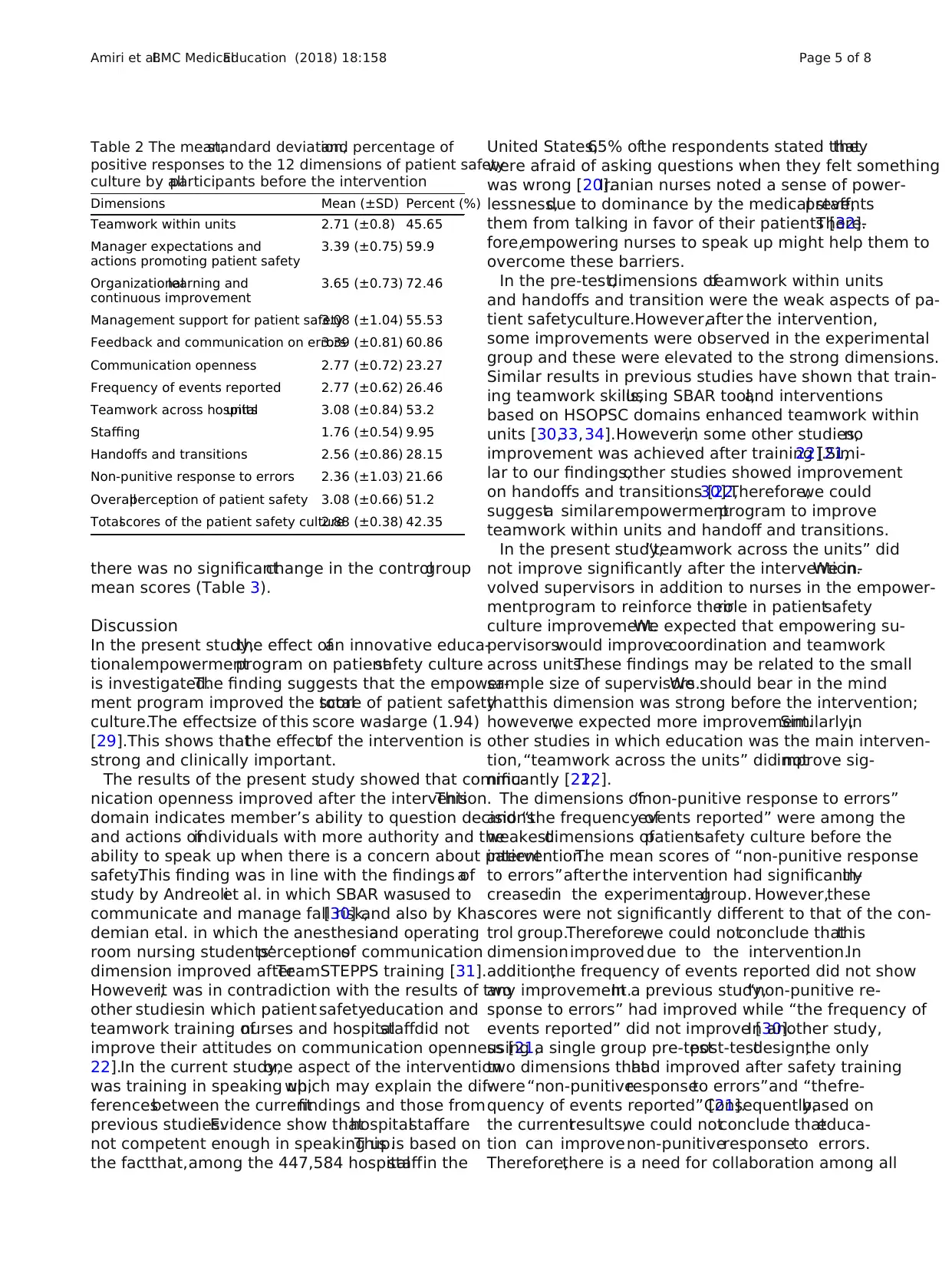
Table 2:The response ofall participants,both in the
experimentaland controlgroups,on patient safety cul-
ture prior to the intervention.The findings showed that
before the intervention,the organizationallearning and
continuous improvement (72.46% ofpositive responses)
and staffing (9.95% of positive responses) were the stron-
gest and the weakest dimensions of patient safety culture
(Table 2).
The pre-testmeansof the experimentaland control
groups of the total scores of patient safety culture and its
dimensionswere notstatistically different.However,in
the experimental group,the total post-test mean scores of
patient safety culture was significantly higher than that of
the controlgroup (3.46 ± 0.26 vs.2.84 ± 0.37,P < 0.001),
and it was also higher than that of the pre-test (3.46 ± 0.26
vs.2.91 ± 0.4,P < 0.001,effect size (d) = 1.94).In addition,
significantimprovements were observed in 5 outof 12
dimensions in the experimentalgroup.The mean scores
of teamwork within units (3.95 ± 0.43 vs.2.91 ± 0.74,
P < 0.001,d = 1.03),manager expectations and actions
promoting patientsafety(4.22 ± 0.31 vs.3.48 ± 0.83,
P < 0.001,d = 0.84),and organizationallearning and
continuousimprovement(4.45 ± 0.45 vs.3.83 ± 0.65,
P < 0.001,d = 0.83)increased significantly in the ex-
perimentalgroup.Furthermore,the post-testmeans
of communication openness (4.22 ± 0.44 vs.2.72 ± 0.67,
P < 0.001,d = 1.82)and handoffs and transitions (4.23
± 0.69vs. 2.75 ± 0.9,P < 0.001,d = 1.30)increased
significantlyin the experimentalgroup. However,
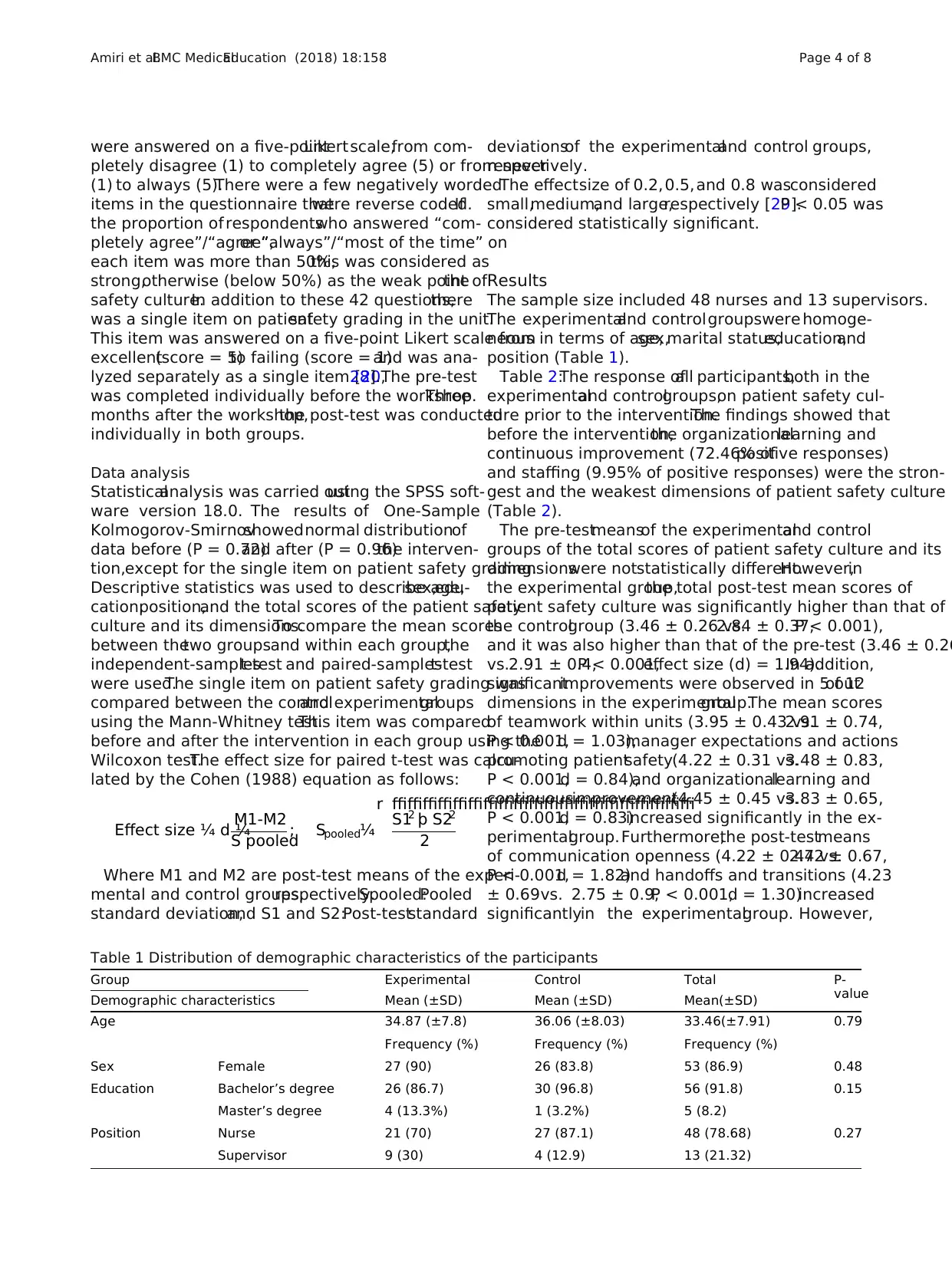
Table 1 Distribution of demographic characteristics of the participants
Group Experimental Control Total P-
value
Demographic characteristics Mean (±SD) Mean (±SD) Mean(±SD)
Age 34.87 (±7.8) 36.06 (±8.03) 33.46(±7.91) 0.79
Frequency (%) Frequency (%) Frequency (%)
Sex Female 27 (90) 26 (83.8) 53 (86.9) 0.48
Education Bachelor’s degree 26 (86.7) 30 (96.8) 56 (91.8) 0.15
Master’s degree 4 (13.3%) 1 (3.2%) 5 (8.2)
Position Nurse 21 (70) 27 (87.1) 48 (78.68) 0.27
Supervisor 9 (30) 4 (12.9) 13 (21.32)
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 4 of 8
pletely disagree (1) to completely agree (5) or from never
(1) to always (5).There were a few negatively worded
items in the questionnaire thatwere reverse coded.If
the proportion of respondentswho answered “com-
pletely agree”/“agree”,or “always”/“most of the time” on
each item was more than 50%,this was considered as
strong,otherwise (below 50%) as the weak point ofthe
safety culture.In addition to these 42 questions,there
was a single item on patientsafety grading in the unit.
This item was answered on a five-point Likert scale from
excellent(score = 5)to failing (score = 1)and was ana-
lyzed separately as a single item [20,28].The pre-test
was completed individually before the workshop.Three
months after the workshop,the post-test was conducted
individually in both groups.
Data analysis
Statisticalanalysis was carried outusing the SPSS soft-
ware version 18.0. The results of One-Sample
Kolmogorov-Smirnovshowednormal distributionof
data before (P = 0.72)and after (P = 0.96)the interven-
tion,except for the single item on patient safety grading.
Descriptive statistics was used to describe age,sex,edu-
cation,position,and the total scores of the patient safety
culture and its dimensions.To compare the mean scores
between thetwo groupsand within each group,the
independent-samplest-test and paired-samplest-test
were used.The single item on patient safety grading was
compared between the controland experimentalgroups
using the Mann-Whitney test.This item was compared
before and after the intervention in each group using the
Wilcoxon test.The effect size for paired t-test was calcu-
lated by the Cohen (1988) equation as follows:
Effect size ¼ d ¼
M1‐M2
S pooled
; Spooled¼
ffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffi
S12 þ S22
2
r
Where M1 and M2 are post-test means of the experi-
mental and control groups,respectively.Spooled:Pooled
standard deviation,and S1 and S2:Post-teststandard
deviationsof the experimentaland control groups,
respectively.
The effectsize of 0.2,0.5,and 0.8 wasconsidered
small,medium,and large,respectively [29].P < 0.05 was
considered statistically significant.
Results
The sample size included 48 nurses and 13 supervisors.
The experimentaland controlgroupswere homoge-
neous in terms of age,sex,marital status,education,and
position (Table 1).
Table 2:The response ofall participants,both in the
experimentaland controlgroups,on patient safety cul-
ture prior to the intervention.The findings showed that
before the intervention,the organizationallearning and
continuous improvement (72.46% ofpositive responses)
and staffing (9.95% of positive responses) were the stron-
gest and the weakest dimensions of patient safety culture
(Table 2).
The pre-testmeansof the experimentaland control
groups of the total scores of patient safety culture and its
dimensionswere notstatistically different.However,in
the experimental group,the total post-test mean scores of
patient safety culture was significantly higher than that of
the controlgroup (3.46 ± 0.26 vs.2.84 ± 0.37,P < 0.001),
and it was also higher than that of the pre-test (3.46 ± 0.26
vs.2.91 ± 0.4,P < 0.001,effect size (d) = 1.94).In addition,
significantimprovements were observed in 5 outof 12
dimensions in the experimentalgroup.The mean scores
of teamwork within units (3.95 ± 0.43 vs.2.91 ± 0.74,
P < 0.001,d = 1.03),manager expectations and actions
promoting patientsafety(4.22 ± 0.31 vs.3.48 ± 0.83,
P < 0.001,d = 0.84),and organizationallearning and
continuousimprovement(4.45 ± 0.45 vs.3.83 ± 0.65,
P < 0.001,d = 0.83)increased significantly in the ex-
perimentalgroup.Furthermore,the post-testmeans
of communication openness (4.22 ± 0.44 vs.2.72 ± 0.67,
P < 0.001,d = 1.82)and handoffs and transitions (4.23
± 0.69vs. 2.75 ± 0.9,P < 0.001,d = 1.30)increased
significantlyin the experimentalgroup. However,
Table 1 Distribution of demographic characteristics of the participants
Group Experimental Control Total P-
value
Demographic characteristics Mean (±SD) Mean (±SD) Mean(±SD)
Age 34.87 (±7.8) 36.06 (±8.03) 33.46(±7.91) 0.79
Frequency (%) Frequency (%) Frequency (%)
Sex Female 27 (90) 26 (83.8) 53 (86.9) 0.48
Education Bachelor’s degree 26 (86.7) 30 (96.8) 56 (91.8) 0.15
Master’s degree 4 (13.3%) 1 (3.2%) 5 (8.2)
Position Nurse 21 (70) 27 (87.1) 48 (78.68) 0.27
Supervisor 9 (30) 4 (12.9) 13 (21.32)
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 4 of 8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
there was no significantchange in the controlgroup
mean scores (Table 3).
Discussion
In the present study,the effect ofan innovative educa-
tionalempowermentprogram on patientsafety culture
is investigated.The finding suggests that the empower-
ment program improved the totalscore of patient safety
culture.The effectsize of this score waslarge (1.94)
[29].This shows thatthe effectof the intervention is
strong and clinically important.
The results of the present study showed that commu-
nication openness improved after the intervention.This
domain indicates member’s ability to question decisions
and actions ofindividuals with more authority and the
ability to speak up when there is a concern about patient
safety.This finding was in line with the findings ofa
study by Andreoliet al. in which SBAR wasused to
communicate and manage fall risk,[30] and also by Kha-
demian etal. in which the anesthesiaand operating
room nursing students’perceptionsof communication
dimension improved afterTeamSTEPPS training [31].
However,it was in contradiction with the results of two
other studiesin which patient safetyeducation and
teamwork training ofnurses and hospitalstaffdid not
improve their attitudes on communication openness [21,
22].In the current study,one aspect of the intervention
was training in speaking up,which may explain the dif-
ferencesbetween the currentfindings and those from
previous studies.Evidence show thathospitalstaffare
not competent enough in speaking up.This is based on
the factthat,among the 447,584 hospitalstaffin the
United States,65% ofthe respondents stated thatthey
were afraid of asking questions when they felt something
was wrong [20].Iranian nurses noted a sense of power-
lessness,due to dominance by the medical staff,prevents
them from talking in favor of their patients [32].There-
fore,empowering nurses to speak up might help them to
overcome these barriers.
In the pre-test,dimensions ofteamwork within units
and handoffs and transition were the weak aspects of pa-
tient safetyculture.However,after the intervention,
some improvements were observed in the experimental
group and these were elevated to the strong dimensions.
Similar results in previous studies have shown that train-
ing teamwork skills,using SBAR tool,and interventions
based on HSOPSC domains enhanced teamwork within
units [30,33,34].However,in some other studies,no
improvement was achieved after training [21,22].Simi-
lar to our findings,other studies showed improvement
on handoffs and transitions [22,30].Therefore,we could
suggesta similarempowermentprogram to improve
teamwork within units and handoff and transitions.
In the present study,“teamwork across the units” did
not improve significantly after the intervention.We in-
volved supervisors in addition to nurses in the empower-
mentprogram to reinforce theirrole in patientsafety
culture improvement.We expected that empowering su-
pervisorswould improvecoordination and teamwork
across units.These findings may be related to the small
sample size of supervisors.We should bear in the mind
thatthis dimension was strong before the intervention;
however,we expected more improvement.Similarly,in
other studies in which education was the main interven-
tion,“teamwork across the units” did notimprove sig-
nificantly [21,22].
The dimensions of“non-punitive response to errors”
and “the frequency ofevents reported” were among the
weakestdimensions ofpatientsafety culture before the
intervention.The mean scores of “non-punitive response
to errors”after the intervention had significantlyin-
creasedin the experimentalgroup. However,these
scores were not significantly different to that of the con-
trol group.Therefore,we could notconclude thatthis
dimensionimproved due to the intervention.In
addition,the frequency of events reported did not show
any improvement.In a previous study,“non-punitive re-
sponse to errors” had improved while “the frequency of
events reported” did not improve [30].In another study,
using a single group pre-testpost-testdesign,the only
two dimensions thathad improved after safety training
were“non-punitiveresponseto errors”and “thefre-
quency of events reported” [21].Consequently,based on
the currentresults,we could notconclude thateduca-
tion can improvenon-punitiveresponseto errors.
Therefore,there is a need for collaboration among all
Table 2 The mean,standard deviation,and percentage of
positive responses to the 12 dimensions of patient safety
culture by allparticipants before the intervention
Dimensions Mean (±SD) Percent (%)
Teamwork within units 2.71 (±0.8) 45.65
Manager expectations and
actions promoting patient safety
3.39 (±0.75) 59.9
Organizationallearning and
continuous improvement
3.65 (±0.73) 72.46
Management support for patient safety3.08 (±1.04) 55.53
Feedback and communication on errors3.39 (±0.81) 60.86
Communication openness 2.77 (±0.72) 23.27
Frequency of events reported 2.77 (±0.62) 26.46
Teamwork across hospitalunits 3.08 (±0.84) 53.2
Staffing 1.76 (±0.54) 9.95
Handoffs and transitions 2.56 (±0.86) 28.15
Non-punitive response to errors 2.36 (±1.03) 21.66
Overallperception of patient safety 3.08 (±0.66) 51.2
Totalscores of the patient safety culture2.88 (±0.38) 42.35
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 5 of 8
mean scores (Table 3).
Discussion
In the present study,the effect ofan innovative educa-
tionalempowermentprogram on patientsafety culture
is investigated.The finding suggests that the empower-
ment program improved the totalscore of patient safety
culture.The effectsize of this score waslarge (1.94)
[29].This shows thatthe effectof the intervention is
strong and clinically important.
The results of the present study showed that commu-
nication openness improved after the intervention.This
domain indicates member’s ability to question decisions
and actions ofindividuals with more authority and the
ability to speak up when there is a concern about patient
safety.This finding was in line with the findings ofa
study by Andreoliet al. in which SBAR wasused to
communicate and manage fall risk,[30] and also by Kha-
demian etal. in which the anesthesiaand operating
room nursing students’perceptionsof communication
dimension improved afterTeamSTEPPS training [31].
However,it was in contradiction with the results of two
other studiesin which patient safetyeducation and
teamwork training ofnurses and hospitalstaffdid not
improve their attitudes on communication openness [21,
22].In the current study,one aspect of the intervention
was training in speaking up,which may explain the dif-
ferencesbetween the currentfindings and those from
previous studies.Evidence show thathospitalstaffare
not competent enough in speaking up.This is based on
the factthat,among the 447,584 hospitalstaffin the
United States,65% ofthe respondents stated thatthey
were afraid of asking questions when they felt something
was wrong [20].Iranian nurses noted a sense of power-
lessness,due to dominance by the medical staff,prevents
them from talking in favor of their patients [32].There-
fore,empowering nurses to speak up might help them to
overcome these barriers.
In the pre-test,dimensions ofteamwork within units
and handoffs and transition were the weak aspects of pa-
tient safetyculture.However,after the intervention,
some improvements were observed in the experimental
group and these were elevated to the strong dimensions.
Similar results in previous studies have shown that train-
ing teamwork skills,using SBAR tool,and interventions
based on HSOPSC domains enhanced teamwork within
units [30,33,34].However,in some other studies,no
improvement was achieved after training [21,22].Simi-
lar to our findings,other studies showed improvement
on handoffs and transitions [22,30].Therefore,we could
suggesta similarempowermentprogram to improve
teamwork within units and handoff and transitions.
In the present study,“teamwork across the units” did
not improve significantly after the intervention.We in-
volved supervisors in addition to nurses in the empower-
mentprogram to reinforce theirrole in patientsafety
culture improvement.We expected that empowering su-
pervisorswould improvecoordination and teamwork
across units.These findings may be related to the small
sample size of supervisors.We should bear in the mind
thatthis dimension was strong before the intervention;
however,we expected more improvement.Similarly,in
other studies in which education was the main interven-
tion,“teamwork across the units” did notimprove sig-
nificantly [21,22].
The dimensions of“non-punitive response to errors”
and “the frequency ofevents reported” were among the
weakestdimensions ofpatientsafety culture before the
intervention.The mean scores of “non-punitive response
to errors”after the intervention had significantlyin-
creasedin the experimentalgroup. However,these
scores were not significantly different to that of the con-
trol group.Therefore,we could notconclude thatthis
dimensionimproved due to the intervention.In
addition,the frequency of events reported did not show
any improvement.In a previous study,“non-punitive re-
sponse to errors” had improved while “the frequency of
events reported” did not improve [30].In another study,
using a single group pre-testpost-testdesign,the only
two dimensions thathad improved after safety training
were“non-punitiveresponseto errors”and “thefre-
quency of events reported” [21].Consequently,based on
the currentresults,we could notconclude thateduca-
tion can improvenon-punitiveresponseto errors.
Therefore,there is a need for collaboration among all
Table 2 The mean,standard deviation,and percentage of
positive responses to the 12 dimensions of patient safety
culture by allparticipants before the intervention
Dimensions Mean (±SD) Percent (%)
Teamwork within units 2.71 (±0.8) 45.65
Manager expectations and
actions promoting patient safety
3.39 (±0.75) 59.9
Organizationallearning and
continuous improvement
3.65 (±0.73) 72.46
Management support for patient safety3.08 (±1.04) 55.53
Feedback and communication on errors3.39 (±0.81) 60.86
Communication openness 2.77 (±0.72) 23.27
Frequency of events reported 2.77 (±0.62) 26.46
Teamwork across hospitalunits 3.08 (±0.84) 53.2
Staffing 1.76 (±0.54) 9.95
Handoffs and transitions 2.56 (±0.86) 28.15
Non-punitive response to errors 2.36 (±1.03) 21.66
Overallperception of patient safety 3.08 (±0.66) 51.2
Totalscores of the patient safety culture2.88 (±0.38) 42.35
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 5 of 8
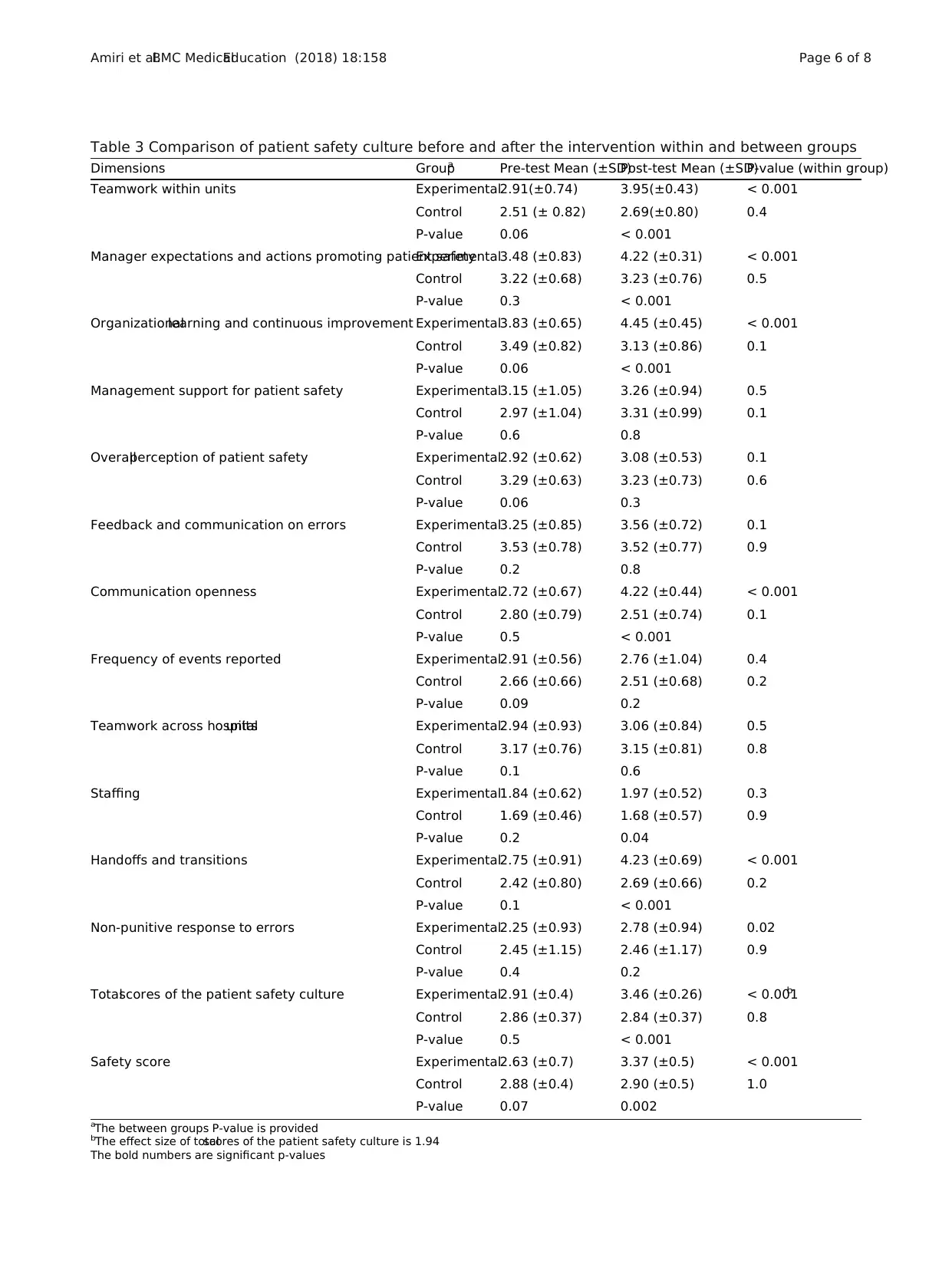
Table 3 Comparison of patient safety culture before and after the intervention within and between groups
Dimensions Groupa Pre-test Mean (±SD)Post-test Mean (±SD)P-value (within group)
Teamwork within units Experimental2.91(±0.74) 3.95(±0.43) < 0.001
Control 2.51 (± 0.82) 2.69(±0.80) 0.4
P-value 0.06 < 0.001
Manager expectations and actions promoting patient safetyExperimental3.48 (±0.83) 4.22 (±0.31) < 0.001
Control 3.22 (±0.68) 3.23 (±0.76) 0.5
P-value 0.3 < 0.001
Organizationallearning and continuous improvement Experimental3.83 (±0.65) 4.45 (±0.45) < 0.001
Control 3.49 (±0.82) 3.13 (±0.86) 0.1
P-value 0.06 < 0.001
Management support for patient safety Experimental3.15 (±1.05) 3.26 (±0.94) 0.5
Control 2.97 (±1.04) 3.31 (±0.99) 0.1
P-value 0.6 0.8
Overallperception of patient safety Experimental2.92 (±0.62) 3.08 (±0.53) 0.1
Control 3.29 (±0.63) 3.23 (±0.73) 0.6
P-value 0.06 0.3
Feedback and communication on errors Experimental3.25 (±0.85) 3.56 (±0.72) 0.1
Control 3.53 (±0.78) 3.52 (±0.77) 0.9
P-value 0.2 0.8
Communication openness Experimental2.72 (±0.67) 4.22 (±0.44) < 0.001
Control 2.80 (±0.79) 2.51 (±0.74) 0.1
P-value 0.5 < 0.001
Frequency of events reported Experimental2.91 (±0.56) 2.76 (±1.04) 0.4
Control 2.66 (±0.66) 2.51 (±0.68) 0.2
P-value 0.09 0.2
Teamwork across hospitalunits Experimental2.94 (±0.93) 3.06 (±0.84) 0.5
Control 3.17 (±0.76) 3.15 (±0.81) 0.8
P-value 0.1 0.6
Staffing Experimental1.84 (±0.62) 1.97 (±0.52) 0.3
Control 1.69 (±0.46) 1.68 (±0.57) 0.9
P-value 0.2 0.04
Handoffs and transitions Experimental2.75 (±0.91) 4.23 (±0.69) < 0.001
Control 2.42 (±0.80) 2.69 (±0.66) 0.2
P-value 0.1 < 0.001
Non-punitive response to errors Experimental2.25 (±0.93) 2.78 (±0.94) 0.02
Control 2.45 (±1.15) 2.46 (±1.17) 0.9
P-value 0.4 0.2
Totalscores of the patient safety culture Experimental2.91 (±0.4) 3.46 (±0.26) < 0.001b
Control 2.86 (±0.37) 2.84 (±0.37) 0.8
P-value 0.5 < 0.001
Safety score Experimental2.63 (±0.7) 3.37 (±0.5) < 0.001
Control 2.88 (±0.4) 2.90 (±0.5) 1.0
P-value 0.07 0.002
aThe between groups P-value is provided
bThe effect size of totalscores of the patient safety culture is 1.94
The bold numbers are significant p-values
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 6 of 8
Dimensions Groupa Pre-test Mean (±SD)Post-test Mean (±SD)P-value (within group)
Teamwork within units Experimental2.91(±0.74) 3.95(±0.43) < 0.001
Control 2.51 (± 0.82) 2.69(±0.80) 0.4
P-value 0.06 < 0.001
Manager expectations and actions promoting patient safetyExperimental3.48 (±0.83) 4.22 (±0.31) < 0.001
Control 3.22 (±0.68) 3.23 (±0.76) 0.5
P-value 0.3 < 0.001
Organizationallearning and continuous improvement Experimental3.83 (±0.65) 4.45 (±0.45) < 0.001
Control 3.49 (±0.82) 3.13 (±0.86) 0.1
P-value 0.06 < 0.001
Management support for patient safety Experimental3.15 (±1.05) 3.26 (±0.94) 0.5
Control 2.97 (±1.04) 3.31 (±0.99) 0.1
P-value 0.6 0.8
Overallperception of patient safety Experimental2.92 (±0.62) 3.08 (±0.53) 0.1
Control 3.29 (±0.63) 3.23 (±0.73) 0.6
P-value 0.06 0.3
Feedback and communication on errors Experimental3.25 (±0.85) 3.56 (±0.72) 0.1
Control 3.53 (±0.78) 3.52 (±0.77) 0.9
P-value 0.2 0.8
Communication openness Experimental2.72 (±0.67) 4.22 (±0.44) < 0.001
Control 2.80 (±0.79) 2.51 (±0.74) 0.1
P-value 0.5 < 0.001
Frequency of events reported Experimental2.91 (±0.56) 2.76 (±1.04) 0.4
Control 2.66 (±0.66) 2.51 (±0.68) 0.2
P-value 0.09 0.2
Teamwork across hospitalunits Experimental2.94 (±0.93) 3.06 (±0.84) 0.5
Control 3.17 (±0.76) 3.15 (±0.81) 0.8
P-value 0.1 0.6
Staffing Experimental1.84 (±0.62) 1.97 (±0.52) 0.3
Control 1.69 (±0.46) 1.68 (±0.57) 0.9
P-value 0.2 0.04
Handoffs and transitions Experimental2.75 (±0.91) 4.23 (±0.69) < 0.001
Control 2.42 (±0.80) 2.69 (±0.66) 0.2
P-value 0.1 < 0.001
Non-punitive response to errors Experimental2.25 (±0.93) 2.78 (±0.94) 0.02
Control 2.45 (±1.15) 2.46 (±1.17) 0.9
P-value 0.4 0.2
Totalscores of the patient safety culture Experimental2.91 (±0.4) 3.46 (±0.26) < 0.001b
Control 2.86 (±0.37) 2.84 (±0.37) 0.8
P-value 0.5 < 0.001
Safety score Experimental2.63 (±0.7) 3.37 (±0.5) < 0.001
Control 2.88 (±0.4) 2.90 (±0.5) 1.0
P-value 0.07 0.002
aThe between groups P-value is provided
bThe effect size of totalscores of the patient safety culture is 1.94
The bold numbers are significant p-values
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 6 of 8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
team members and leaders towards problem-solving and
to increase the number of events being reported.
It seems that the involvement of nurses and supervisors
in the empowermentprogram was notsufficientto im-
prove three important dimensions:staffing,error report-
ing,and non-punitive response to errors.Therefore,we
recommend that in the future higher-level hospital execu-
tives should also be involved in empowerment programs.
Limitations of the study
The main limitation ofthe present study was related to
the use of a self-reported instrument in order to explore
the effects ofempowermenton the patientsafety cul-
ture.It is recommended thatfurther studies should be
conducted using observationaldata collection methods.
Additionally,studies that assess the viewpoints ofother
parties such as patients are recommended.
Conclusion
This innovative empowermentprogram which involved
nursesand supervisorsresulted in improved patient
safety culture scores and developmentin some dimen-
sions.Communication openness,handoffsand transi-
tions,teamwork within units,learning and continuous
improvement,manager’s expectations and actions pro-
moting patientsafetyimproved significantlyafterthe
intervention.Therefore,this program can be utilized to
promote these importantdimensionsof patientsafety
culture.However,dimensions such as staffing,“non-pu-
nitive response to errors”,and “frequency of events that
were reported” continued to be the weak domains of the
patient safety culture throughout the study.Thus,to im-
prove these dimensions,conducting long-term studies
and additionalactions are also required.Given the im-
portance of reporting errors and adequate staffing in im-
proving patientsafety,it is recommended thatthese
items should be considered as a top priority for health-
care managers and hospital policymakers.
Abbreviations
AHRQ:Agency for Healthcare Research and Quality;HSOPSC:HospitalSurvey
on Patient Safety Culture;ICU:Intensive care units;SPSS:StatisticalPackage
for SocialScience;TeamSTEPPS:Team Strategies and Tools to Enhance
Performance and Patient Safety
Acknowledgments
This article was extracted from the MSc thesis by Maryam Amiri,and
approved by Vice Chancellor of Research of Shiraz University of Medical
Sciences,Shiraz,Iran.Hereby,the officials in NamaziHospital,Ms.Somayeh
Zahraei and Fatemeh Azadi,ICU nurses and supervisors are highly appreciated.
Appreciation goes to the Center for Development of Clinical Research at
Namazi Hospital and Dr.Nasrin Shokrpour,Mrs.Sareh Keshavarzi,Dr.Najaf Zare,
and Dr.Jamali for their collaboration in editorial assistance,design,statistics,and
data analysis.The authors would also like to thank the Research Consultation
Center at Shiraz University of Medical Sciences and Mr.Argasi and Dr.N.Pakshir
for their editorial assistance.
Funding
The present study was financially supported by the Vice Chancellor of Resea
Shiraz University of Medical Sciences,Shiraz,Iran (Grant No.5793).The funding
body did not play any roles in the design of the study and collection,analysis,
and interpretation of data and in writing the manuscript.
Availability of data and materials
The dataset of the present study is available upon request.
Authors’contributions
Allauthors made substantialcontributions to the conception and design of
the study.Data was collected by MA.Data analysis and interpretation were
done by ZKh and MA.RNN also participated in data interpretation.MA,RNN,
and ZKh conducted the intervention.ZKh and MA participated in drafting
the manuscript.Allauthors revised the manuscript critically for important
intellectualcontent and finalapprovalof the manuscript.
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of Shiraz
University of MedicalSciences (Shiraz,Iran) and the authorities at Namazi
Hospital(No.93–7397).Written informed consent was obtained from all
participants and confidentiality of the information was assured.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in publis
maps and institutional affiliations.
Author details
1Department of Nursing,Schoolof Nursing and Midwifery,Shiraz University
of MedicalSciences,Shiraz,Iran.2Anesthesia and CriticalCare Emergency
Medicine Department,NamaziHospital,Shiraz University of MedicalSciences,
Shiraz,Iran.
Received:18 July 2017 Accepted:12 June 2018
References
1. James JT.A new evidence-based estimate of patient harms associated with
hospitalcare.J Patient Saf.2013;9(3):122–8.
2. Lyle-Edrosolo G,Waxman K.Aligning healthcare safety and quality
competencies:quality and safety education for nurses (QSEN),The Joint
Commission,and American Nurses Credentialing Center (ANCC) magnet®
standards crosswalk.Nurse Leader.2016;14(1):70–5.
3. Ravi P,Vijai M.Errors in ICU:how safe is the patient? A prospective
observational study in a tertiary care hospital.J Anesth Clin Res.2015;6(6):535.
4. Zargarzadeh AH.Medication safety in Iran.J Pharm Care.2013;1(4):125–6.
5. Vazin A,FereidooniM.Determining frequency of prescription,
administration and transcription errors in internalintensive care unit of
Shahid FaghihiHospitalin Shiraz with direct observation approach.Iran J
Pharm Sci.2012;8(3):189–94.
6. Haghbin S,Shahsavari S,Vazin A.Medication errors in pediatric intensive care
unit:incidence,types and outcome.Trends Pharm Sci.2016;2(2):109–16.
7. FarziS,Irajpour A,SaghaeiM,RavaghiH.Causes of medication errors in
intensive care units from the perspective of healthcare professionals.J Res
Pharm Pract.2017;6(3):158–63.
8. NezamodiniZ,KhodamoradiF,Malekzadeh M,VaziriH.Nursing errors in
intensive care unit by human error identification in systems tool:a case
study.Jundishapur J Health Sci.2016;8(3):e36055.
9. Khademian Z,SharifiF,TabeiZ,Bolandparvaz S,Abbaszadeh A,AbbasiHR.
Teamwork improvement in emergency trauma department.Iran J Nurse
Midwifery Res.2013;18(4):333–9.
10. Shafakhah M,Zarshenas L,Sharif F,SarvestaniR.Evaluation of nursing
students’communication abilities in clinicalcourses in hospitals.Glob J
Health Sci.2015;7(4):323–8.
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 7 of 8
to increase the number of events being reported.
It seems that the involvement of nurses and supervisors
in the empowermentprogram was notsufficientto im-
prove three important dimensions:staffing,error report-
ing,and non-punitive response to errors.Therefore,we
recommend that in the future higher-level hospital execu-
tives should also be involved in empowerment programs.
Limitations of the study
The main limitation ofthe present study was related to
the use of a self-reported instrument in order to explore
the effects ofempowermenton the patientsafety cul-
ture.It is recommended thatfurther studies should be
conducted using observationaldata collection methods.
Additionally,studies that assess the viewpoints ofother
parties such as patients are recommended.
Conclusion
This innovative empowermentprogram which involved
nursesand supervisorsresulted in improved patient
safety culture scores and developmentin some dimen-
sions.Communication openness,handoffsand transi-
tions,teamwork within units,learning and continuous
improvement,manager’s expectations and actions pro-
moting patientsafetyimproved significantlyafterthe
intervention.Therefore,this program can be utilized to
promote these importantdimensionsof patientsafety
culture.However,dimensions such as staffing,“non-pu-
nitive response to errors”,and “frequency of events that
were reported” continued to be the weak domains of the
patient safety culture throughout the study.Thus,to im-
prove these dimensions,conducting long-term studies
and additionalactions are also required.Given the im-
portance of reporting errors and adequate staffing in im-
proving patientsafety,it is recommended thatthese
items should be considered as a top priority for health-
care managers and hospital policymakers.
Abbreviations
AHRQ:Agency for Healthcare Research and Quality;HSOPSC:HospitalSurvey
on Patient Safety Culture;ICU:Intensive care units;SPSS:StatisticalPackage
for SocialScience;TeamSTEPPS:Team Strategies and Tools to Enhance
Performance and Patient Safety
Acknowledgments
This article was extracted from the MSc thesis by Maryam Amiri,and
approved by Vice Chancellor of Research of Shiraz University of Medical
Sciences,Shiraz,Iran.Hereby,the officials in NamaziHospital,Ms.Somayeh
Zahraei and Fatemeh Azadi,ICU nurses and supervisors are highly appreciated.
Appreciation goes to the Center for Development of Clinical Research at
Namazi Hospital and Dr.Nasrin Shokrpour,Mrs.Sareh Keshavarzi,Dr.Najaf Zare,
and Dr.Jamali for their collaboration in editorial assistance,design,statistics,and
data analysis.The authors would also like to thank the Research Consultation
Center at Shiraz University of Medical Sciences and Mr.Argasi and Dr.N.Pakshir
for their editorial assistance.
Funding
The present study was financially supported by the Vice Chancellor of Resea
Shiraz University of Medical Sciences,Shiraz,Iran (Grant No.5793).The funding
body did not play any roles in the design of the study and collection,analysis,
and interpretation of data and in writing the manuscript.
Availability of data and materials
The dataset of the present study is available upon request.
Authors’contributions
Allauthors made substantialcontributions to the conception and design of
the study.Data was collected by MA.Data analysis and interpretation were
done by ZKh and MA.RNN also participated in data interpretation.MA,RNN,
and ZKh conducted the intervention.ZKh and MA participated in drafting
the manuscript.Allauthors revised the manuscript critically for important
intellectualcontent and finalapprovalof the manuscript.
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of Shiraz
University of MedicalSciences (Shiraz,Iran) and the authorities at Namazi
Hospital(No.93–7397).Written informed consent was obtained from all
participants and confidentiality of the information was assured.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in publis
maps and institutional affiliations.
Author details
1Department of Nursing,Schoolof Nursing and Midwifery,Shiraz University
of MedicalSciences,Shiraz,Iran.2Anesthesia and CriticalCare Emergency
Medicine Department,NamaziHospital,Shiraz University of MedicalSciences,
Shiraz,Iran.
Received:18 July 2017 Accepted:12 June 2018
References
1. James JT.A new evidence-based estimate of patient harms associated with
hospitalcare.J Patient Saf.2013;9(3):122–8.
2. Lyle-Edrosolo G,Waxman K.Aligning healthcare safety and quality
competencies:quality and safety education for nurses (QSEN),The Joint
Commission,and American Nurses Credentialing Center (ANCC) magnet®
standards crosswalk.Nurse Leader.2016;14(1):70–5.
3. Ravi P,Vijai M.Errors in ICU:how safe is the patient? A prospective
observational study in a tertiary care hospital.J Anesth Clin Res.2015;6(6):535.
4. Zargarzadeh AH.Medication safety in Iran.J Pharm Care.2013;1(4):125–6.
5. Vazin A,FereidooniM.Determining frequency of prescription,
administration and transcription errors in internalintensive care unit of
Shahid FaghihiHospitalin Shiraz with direct observation approach.Iran J
Pharm Sci.2012;8(3):189–94.
6. Haghbin S,Shahsavari S,Vazin A.Medication errors in pediatric intensive care
unit:incidence,types and outcome.Trends Pharm Sci.2016;2(2):109–16.
7. FarziS,Irajpour A,SaghaeiM,RavaghiH.Causes of medication errors in
intensive care units from the perspective of healthcare professionals.J Res
Pharm Pract.2017;6(3):158–63.
8. NezamodiniZ,KhodamoradiF,Malekzadeh M,VaziriH.Nursing errors in
intensive care unit by human error identification in systems tool:a case
study.Jundishapur J Health Sci.2016;8(3):e36055.
9. Khademian Z,SharifiF,TabeiZ,Bolandparvaz S,Abbaszadeh A,AbbasiHR.
Teamwork improvement in emergency trauma department.Iran J Nurse
Midwifery Res.2013;18(4):333–9.
10. Shafakhah M,Zarshenas L,Sharif F,SarvestaniR.Evaluation of nursing
students’communication abilities in clinicalcourses in hospitals.Glob J
Health Sci.2015;7(4):323–8.
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 7 of 8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11. Patient Safety Network.Nursing and Patient Safety.2017.https://psnet.ahrq.
gov/primers/primer/22/nursing-and-patient-safety.Accessed 25 Nov 2017.
12. Rogers AE,Dean GE,Hwang WT,Scott.Role ofregistered nurses in
errorprevention,discovery and correction.QualSafHealth Care.2008;
17(2):117–21.
13. Henneman EA,GawlinskiA,Blank FS,Henneman PL,Jordan D,McKenzie JB.
Strategies used by criticalcare nurses to identify,interrupt,and correct
medicalerrors.Am J Crit Care.2010;19(6):500–9.
14. Mardon RE,Khanna K,Sorra J,Dyer N,Famolaro T.Exploring relationships
between hospitalpatient safety culture and adverse events.J Patient Saf.
2010;6(4):226–32.
15. Wang X,Liu K,You L,Xiang J,Hu H,Zhang L.The relationship between
patient safety culture and adverse events:a questionnaire survey.Int J Nurs
Stud.2014;51(8):1114–22.
16. Sammer CE,Lykens K,Singh KP,Mains DA,Lackan NA.What is patient safety
culture? A review of the literature.J Nurs Scholarsh.2010;42(2):156–65.
17. Azami-Aghdash S,Ebadifard Azar F,Rezapour A,AzamiA,RasiV,Klvany K.
Patient safety culture in hospitals of Iran:a systematic review and meta-
analysis.Med J Islam Repub Iran.2015;23(29):251.
18. Weaver SJ,LubomksiLH,Wilson RF,Pfoh ER,Martinez KA,Dy SM.
Promoting a culture of safety.In:Making health care safer II:An updated
criticalanalysis of the evidence for patient safety practices.Rockville:
Agency for Healthcare Research and Quality;2013.https://www.ncbi.nlm.
nih.gov/books/NBK133394/ .Accessed 23 Jun 2017.
19. Morello RT,Lowthian JA,Barker AL,McGinnes R,Dunt D,Brand C.Strategies
for improving patient safety culture in hospitals:a systematic review.BMJ
QualSaf.2013;22(1):8–11.
20. Famolaro T,Yount ND,Burns W,Flashner E,Liu H,Sorra J.Hospitalsurvey
on patient safety culture:2016 user comparative database report.2016.
(Prepared by Westat,Rockville,MD,under Contract No.HHSA
290201300003C).Rockville:Agency for Healthcare Research and Quality.
AHRQ Publication No.16–0021-EF
21. AbuAlRub RF,Abualhaja AA.The impact of educationalinterventions on
enhancing perceptions of patient safety culture among Jordanian senior
nurses.Nurs Forum.2014;49(2):139–50.
22. Jones F,Podila F,Power C.Creating a culture of safety in the emergency
department:The Value of Team Training.J Nurse Adm.2013;93(4):194–200.
23. Sayre MM.Improving collaboration and patient safety by encouraging
nurses to speak-up:Overcoming personaland organizationalobstacles
through self-reflection and collaboration .Available from ProQuest
Dissertations and Theses Global.(753487229).http://search.proquest.com/
docview/753487229?accountid=41313 .2010.Accessed 10 Jun 2016.
24. Institute of Medicine.Committee on the Health Professions Education
Summit.Health professions education:a bridge to quality.2003.https://
www.ncbi.nlm.nih.gov/books/NBK221528/ [Internet].NationalAcademies
Press (US).Accessed 15 Jun 2017.
25. Cronenwett L,Sherwood G,Barnsteiner J,Disch J,Johnson J,MitchellP.
Quality and safety education for nurses.Nurs Outlook.2007;55(3):112–31.
26. AHRQ.About TeamSTEPPS®.2016.https://www.ahrq.gov/teamstepps/about-
teamstepps/index.html.Accessed 10 Mar 2017.
27. IzadiAR,Drikvand J,Ebrazeh A.The patientsafety culture in Fatemeh
Zahra Hospitalof Najafabad,Iran.Health Information Management.
2013;9(6):895–907.
28. Agency for Healthcare Research and Quality,Rockville.Surveys on Patient
Safety Culture™.https://www.ahrq.gov/sites/default/files/wysiwyg/sops/
quality-patient-safety/patientsafetyculture/hospitalscanform.pdf .Accessed
10 Mar 2018.
29. Nakagawa S,CuthillIC:Effectsize,confidence intervaland statistical
significance:a practicalguide forbiologists.Biologicalreviews 2007,
82(4):591–605.
30. AndreoliA,Fancott C,VeljiK,Baker GR,Solway S,Aimone E.Using SBAR to
communicate falls risk and management in interprofessionalrehabilitation
teams.Healthc Q.2010;13:94–101.
31. Khademian Z,PishgarZ, Torabizadeh C.Effectof training on the
attitude and knowledge ofteamwork among anesthesia and operating
room nursing students:a quasi-experimentalstudy.Shiraz E Med J.
2018;19(4):e61079.
32. Negarandeh R,Oskouie F,AhmadiF,Nikravesh M,Hallberg IR.Patient
advocacy:barriers and facilitators.BMC Nurs.2006;5(1):3.
33. Adams-Pizarro I,Walker Z,Robinson J,Kelly S,Toth M:Using the AHRQ
HospitalSurvey on patient safety culture as an intervention toolfor regional
clinicalimprovement collaboratives.In:Henriksen K,Battles JB,Keyes MA,
et al.,editors.Advances in patient safety:new directions and alternative
approaches (vol.2:culture and redesign).Rockville:Agency for Healthcare
Research and Quality (US);2008.Available from:https://www.ncbi.nlm.nih.
gov/books/NBK43728/ .Accessed 10 Mar 2017.
34. Mayer CM,Cluff L,Lin WT,Willis TS,Stafford RE,Williams C:Evaluating
efforts to optimize TeamSTEPPS implementation in surgicaland pediatric
intensive care units.Jt Comm J QualPatient Saf 2011,37(8):365–374.
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 8 of 8
gov/primers/primer/22/nursing-and-patient-safety.Accessed 25 Nov 2017.
12. Rogers AE,Dean GE,Hwang WT,Scott.Role ofregistered nurses in
errorprevention,discovery and correction.QualSafHealth Care.2008;
17(2):117–21.
13. Henneman EA,GawlinskiA,Blank FS,Henneman PL,Jordan D,McKenzie JB.
Strategies used by criticalcare nurses to identify,interrupt,and correct
medicalerrors.Am J Crit Care.2010;19(6):500–9.
14. Mardon RE,Khanna K,Sorra J,Dyer N,Famolaro T.Exploring relationships
between hospitalpatient safety culture and adverse events.J Patient Saf.
2010;6(4):226–32.
15. Wang X,Liu K,You L,Xiang J,Hu H,Zhang L.The relationship between
patient safety culture and adverse events:a questionnaire survey.Int J Nurs
Stud.2014;51(8):1114–22.
16. Sammer CE,Lykens K,Singh KP,Mains DA,Lackan NA.What is patient safety
culture? A review of the literature.J Nurs Scholarsh.2010;42(2):156–65.
17. Azami-Aghdash S,Ebadifard Azar F,Rezapour A,AzamiA,RasiV,Klvany K.
Patient safety culture in hospitals of Iran:a systematic review and meta-
analysis.Med J Islam Repub Iran.2015;23(29):251.
18. Weaver SJ,LubomksiLH,Wilson RF,Pfoh ER,Martinez KA,Dy SM.
Promoting a culture of safety.In:Making health care safer II:An updated
criticalanalysis of the evidence for patient safety practices.Rockville:
Agency for Healthcare Research and Quality;2013.https://www.ncbi.nlm.
nih.gov/books/NBK133394/ .Accessed 23 Jun 2017.
19. Morello RT,Lowthian JA,Barker AL,McGinnes R,Dunt D,Brand C.Strategies
for improving patient safety culture in hospitals:a systematic review.BMJ
QualSaf.2013;22(1):8–11.
20. Famolaro T,Yount ND,Burns W,Flashner E,Liu H,Sorra J.Hospitalsurvey
on patient safety culture:2016 user comparative database report.2016.
(Prepared by Westat,Rockville,MD,under Contract No.HHSA
290201300003C).Rockville:Agency for Healthcare Research and Quality.
AHRQ Publication No.16–0021-EF
21. AbuAlRub RF,Abualhaja AA.The impact of educationalinterventions on
enhancing perceptions of patient safety culture among Jordanian senior
nurses.Nurs Forum.2014;49(2):139–50.
22. Jones F,Podila F,Power C.Creating a culture of safety in the emergency
department:The Value of Team Training.J Nurse Adm.2013;93(4):194–200.
23. Sayre MM.Improving collaboration and patient safety by encouraging
nurses to speak-up:Overcoming personaland organizationalobstacles
through self-reflection and collaboration .Available from ProQuest
Dissertations and Theses Global.(753487229).http://search.proquest.com/
docview/753487229?accountid=41313 .2010.Accessed 10 Jun 2016.
24. Institute of Medicine.Committee on the Health Professions Education
Summit.Health professions education:a bridge to quality.2003.https://
www.ncbi.nlm.nih.gov/books/NBK221528/ [Internet].NationalAcademies
Press (US).Accessed 15 Jun 2017.
25. Cronenwett L,Sherwood G,Barnsteiner J,Disch J,Johnson J,MitchellP.
Quality and safety education for nurses.Nurs Outlook.2007;55(3):112–31.
26. AHRQ.About TeamSTEPPS®.2016.https://www.ahrq.gov/teamstepps/about-
teamstepps/index.html.Accessed 10 Mar 2017.
27. IzadiAR,Drikvand J,Ebrazeh A.The patientsafety culture in Fatemeh
Zahra Hospitalof Najafabad,Iran.Health Information Management.
2013;9(6):895–907.
28. Agency for Healthcare Research and Quality,Rockville.Surveys on Patient
Safety Culture™.https://www.ahrq.gov/sites/default/files/wysiwyg/sops/
quality-patient-safety/patientsafetyculture/hospitalscanform.pdf .Accessed
10 Mar 2018.
29. Nakagawa S,CuthillIC:Effectsize,confidence intervaland statistical
significance:a practicalguide forbiologists.Biologicalreviews 2007,
82(4):591–605.
30. AndreoliA,Fancott C,VeljiK,Baker GR,Solway S,Aimone E.Using SBAR to
communicate falls risk and management in interprofessionalrehabilitation
teams.Healthc Q.2010;13:94–101.
31. Khademian Z,PishgarZ, Torabizadeh C.Effectof training on the
attitude and knowledge ofteamwork among anesthesia and operating
room nursing students:a quasi-experimentalstudy.Shiraz E Med J.
2018;19(4):e61079.
32. Negarandeh R,Oskouie F,AhmadiF,Nikravesh M,Hallberg IR.Patient
advocacy:barriers and facilitators.BMC Nurs.2006;5(1):3.
33. Adams-Pizarro I,Walker Z,Robinson J,Kelly S,Toth M:Using the AHRQ
HospitalSurvey on patient safety culture as an intervention toolfor regional
clinicalimprovement collaboratives.In:Henriksen K,Battles JB,Keyes MA,
et al.,editors.Advances in patient safety:new directions and alternative
approaches (vol.2:culture and redesign).Rockville:Agency for Healthcare
Research and Quality (US);2008.Available from:https://www.ncbi.nlm.nih.
gov/books/NBK43728/ .Accessed 10 Mar 2017.
34. Mayer CM,Cluff L,Lin WT,Willis TS,Stafford RE,Williams C:Evaluating
efforts to optimize TeamSTEPPS implementation in surgicaland pediatric
intensive care units.Jt Comm J QualPatient Saf 2011,37(8):365–374.
Amiri et al.BMC MedicalEducation (2018) 18:158 Page 8 of 8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





