Culturally Safe Nursing Practice: A Self-Reflection Report
VerifiedAdded on 2022/10/17
|8
|1796
|8
Report
AI Summary
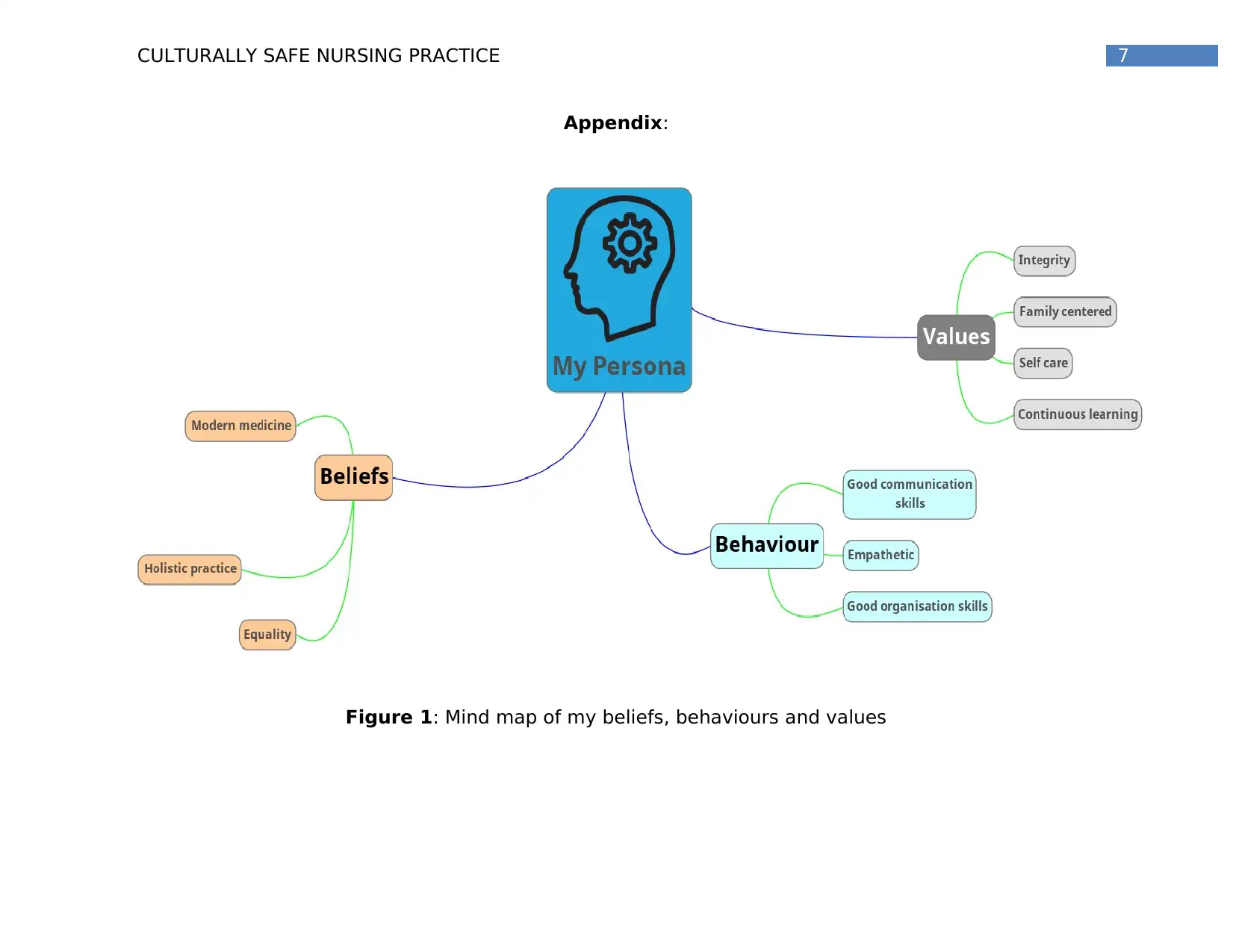
This report provides a comprehensive self-reflection on culturally safe nursing practice. It begins with an introduction emphasizing the importance of understanding personal beliefs, values, and behaviors in clinical practice to ensure quality patient care and avoid cultural discrimination. The report then delves into the author's beliefs, including a respect for evidence-based practices, acceptance of alternative therapies within a cultural context, and a commitment to health equality. Core values such as continuous learning, integrity, and self-care are examined, highlighting their impact on clinical practice and the importance of maintaining a balance to provide optimal patient care. The author's behaviors, including communication and empathy, are discussed as crucial elements of culturally safe practice. The conclusion reiterates the significance of cultural safety in healthcare, advocating for the eradication of inequalities and the effective use of personal values to facilitate patient recovery. The report is supported by a mind map illustrating the interrelation of beliefs, behaviors, and values, along with references to relevant literature.

Running head: CULTURALLY SAFE NURSING PRACTICE
Culturally Safe Nursing Practice
Name of the Student
Name of the University
Author’s Note:
Culturally Safe Nursing Practice
Name of the Student
Name of the University
Author’s Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CULTURALLY SAFE NURSING PRACTICE
Introduction:
Reflecting upon personal beliefs, values, and behaviours may influence
clinical practice and influence patient quality of care. It is essential to
recognize that patients are distinct from my own values, views and
behaviours (Repo, Vahlberg, Salminen, Papadopoulos, & Leino-Kilpi, 2017).
Understanding why I value something and think it can reveal a cultural
distinction or a precondition that I have for clinical exercise. Reflecting upon
the differences and their impact on patients’ cultural safety may safeguard
patients and refine my clinical practice from cultural discrimination (Douglas
et al., 2013). Specific values, beliefs and behaviours, which may require
further development and bias regions that may lead to unsafe cultural care,
must be studied and reflected (Crawford & Candlin, 2013). Keeping that in
mind, I will be reflecting upon my beliefs, values and behaviours in the
following section and how they might affect my culturally safe practice.
Beliefs:
I respect methods based on evidence that are the outcome of extensive
studies. Patients in my care can trust that only understanding and practice
based on proof from thorough studies influences my practice. However,
additional treatments are accepted and are recognized as additional
therapies for conventional medicine, and a wide range of alternative
therapies are offered that patients can think of as being healthy (Douglas et
al., 2014). Alternative therapies, whether they work with placebo, or
genuinely help patients, are component of their religious cultural identity.
For the restoration of physical health, the cultural well-being of the patient is
essential. The holistic treatment of a patient includes including your religious
convictions in your health plan (Duff, 2013). This is an area where I need to
focus on the continuing growth of culturally safe practice.
I, personally, advocate for all Australians the idealist perspective of health
equality. Social health conditions like the way in which a person receives
Introduction:
Reflecting upon personal beliefs, values, and behaviours may influence
clinical practice and influence patient quality of care. It is essential to
recognize that patients are distinct from my own values, views and
behaviours (Repo, Vahlberg, Salminen, Papadopoulos, & Leino-Kilpi, 2017).
Understanding why I value something and think it can reveal a cultural
distinction or a precondition that I have for clinical exercise. Reflecting upon
the differences and their impact on patients’ cultural safety may safeguard
patients and refine my clinical practice from cultural discrimination (Douglas
et al., 2013). Specific values, beliefs and behaviours, which may require
further development and bias regions that may lead to unsafe cultural care,
must be studied and reflected (Crawford & Candlin, 2013). Keeping that in
mind, I will be reflecting upon my beliefs, values and behaviours in the
following section and how they might affect my culturally safe practice.
Beliefs:
I respect methods based on evidence that are the outcome of extensive
studies. Patients in my care can trust that only understanding and practice
based on proof from thorough studies influences my practice. However,
additional treatments are accepted and are recognized as additional
therapies for conventional medicine, and a wide range of alternative
therapies are offered that patients can think of as being healthy (Douglas et
al., 2014). Alternative therapies, whether they work with placebo, or
genuinely help patients, are component of their religious cultural identity.
For the restoration of physical health, the cultural well-being of the patient is
essential. The holistic treatment of a patient includes including your religious
convictions in your health plan (Duff, 2013). This is an area where I need to
focus on the continuing growth of culturally safe practice.
I, personally, advocate for all Australians the idealist perspective of health
equality. Social health conditions like the way in which a person receives
2CULTURALLY SAFE NURSING PRACTICE
equal health care in Australia are affected by lifestyle, ethnicity,
socioeconomic status, education levels and a geographic place. As a health
professional, I am responsible for providing affordable health services data
and references. Studies have shown that health practitioners have a duty to
tackle inequality between Australians in the social determinants of health
(Kellett & Fitton, 2017). Knowledge of health facilities accessible and the
status of a patient with regard to the social determinants of the health can
be used to better serve the patient and will allow me to develop health plans
that include references to facilities that meet the requirements of the
patient. In addition, through equal access to facilities the patients will
receive cultural secure care (Kellett & Fitton, 2017). The awareness of
accessible services will involve further growth, as I will need to acquire
understanding of the services that are available.
Values:
Continuous learning and time spent on education are a significant personal
value and are taken as a profession by the Australian Nursing and Midwifery
Board (NMBA) (2016). Standard 3.3 is the necessity for improved nursing
practices and good practices results for exercise as a licensed nurse (Nursing
& Midwifery Committee of Australia [NMBA], 2016). Lifelong learning in order
to improve nursing practices, knowledge of developments in medicine,
technology and research must be learned and examined. As a virtue of this,
my understanding stays current and culturally secure for patients. The
difference in medical know-how concentrations, however, could lead to a
power imbalance that would result in culturally unsafe patient circumstances
(NMBA, 2016). As an avid learner, I tend to learn new things every day and
my urge continuous learning will help me in my future nursing practice.
Integrity is an impact on my clinical practice. Honesty and accountability and
responsibility are included in integrity. The preservation of professional
integrity includes renewal of registration, continuous professional growth,
equal health care in Australia are affected by lifestyle, ethnicity,
socioeconomic status, education levels and a geographic place. As a health
professional, I am responsible for providing affordable health services data
and references. Studies have shown that health practitioners have a duty to
tackle inequality between Australians in the social determinants of health
(Kellett & Fitton, 2017). Knowledge of health facilities accessible and the
status of a patient with regard to the social determinants of the health can
be used to better serve the patient and will allow me to develop health plans
that include references to facilities that meet the requirements of the
patient. In addition, through equal access to facilities the patients will
receive cultural secure care (Kellett & Fitton, 2017). The awareness of
accessible services will involve further growth, as I will need to acquire
understanding of the services that are available.
Values:
Continuous learning and time spent on education are a significant personal
value and are taken as a profession by the Australian Nursing and Midwifery
Board (NMBA) (2016). Standard 3.3 is the necessity for improved nursing
practices and good practices results for exercise as a licensed nurse (Nursing
& Midwifery Committee of Australia [NMBA], 2016). Lifelong learning in order
to improve nursing practices, knowledge of developments in medicine,
technology and research must be learned and examined. As a virtue of this,
my understanding stays current and culturally secure for patients. The
difference in medical know-how concentrations, however, could lead to a
power imbalance that would result in culturally unsafe patient circumstances
(NMBA, 2016). As an avid learner, I tend to learn new things every day and
my urge continuous learning will help me in my future nursing practice.
Integrity is an impact on my clinical practice. Honesty and accountability and
responsibility are included in integrity. The preservation of professional
integrity includes renewal of registration, continuous professional growth,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CULTURALLY SAFE NURSING PRACTICE
exercise and reflective practice (NMBA, 2016). Integrity in care will involve
continuous growth as my repertoire grows and as my skills grows personally
and professionally (Kangasniemi, Vaismoradi, Jasper, & Turunen, 2013).
Self-care remains a continuing task and is needed for equilibrium of life. A
balance of life maintains commitment to clinical practice and enhances my
ability to offer patients the best possible care (Everson et al., 2015). My
private needs are aware of patients, requirements when admitted to a health
facility. During admission, a patient can be restrictive and weakening when
they are unable to schedule their day and take part in operations considered
important to their cultural identity (Repo et al., 2017). For secure clinical
practice in a multicultural society, continuous reflection and growth will be
necessary. Language obstacles and family distinctions are challenging in
different societies and are needed for continuous growth.
Behaviours:
Good communication is essential to the development of therapeutic
relations. It is also important for patient evaluation and for attaining patient
involvement nursing objectives (Almutairi, McCarthy, & Gardner, 2015). But
communication with patients will constantly bring fresh difficulties and
involve constant reflection and adaptation, as I practice with advanced
communicational abilities. In addition, cultural variations in communication,
including verbal and non verbal distinctions, could be viewed differently. If
the patients are aware of possible variations in communication, and
consideration of these and adjusting clinical practices could be critical to
offering culturally secure practices, they could feel secure from culture
(Crawford & Candlin, 2013).
Empathy practices are behaviour essential for secure cultural care. Empathy
is an expression of identity in reaction to experiences or occurrences with
emotions or attitudes. A therapeutic relationship is improved when the nurse
communicates with the patient with empathy. Studies have shown that the
exercise and reflective practice (NMBA, 2016). Integrity in care will involve
continuous growth as my repertoire grows and as my skills grows personally
and professionally (Kangasniemi, Vaismoradi, Jasper, & Turunen, 2013).
Self-care remains a continuing task and is needed for equilibrium of life. A
balance of life maintains commitment to clinical practice and enhances my
ability to offer patients the best possible care (Everson et al., 2015). My
private needs are aware of patients, requirements when admitted to a health
facility. During admission, a patient can be restrictive and weakening when
they are unable to schedule their day and take part in operations considered
important to their cultural identity (Repo et al., 2017). For secure clinical
practice in a multicultural society, continuous reflection and growth will be
necessary. Language obstacles and family distinctions are challenging in
different societies and are needed for continuous growth.
Behaviours:
Good communication is essential to the development of therapeutic
relations. It is also important for patient evaluation and for attaining patient
involvement nursing objectives (Almutairi, McCarthy, & Gardner, 2015). But
communication with patients will constantly bring fresh difficulties and
involve constant reflection and adaptation, as I practice with advanced
communicational abilities. In addition, cultural variations in communication,
including verbal and non verbal distinctions, could be viewed differently. If
the patients are aware of possible variations in communication, and
consideration of these and adjusting clinical practices could be critical to
offering culturally secure practices, they could feel secure from culture
(Crawford & Candlin, 2013).
Empathy practices are behaviour essential for secure cultural care. Empathy
is an expression of identity in reaction to experiences or occurrences with
emotions or attitudes. A therapeutic relationship is improved when the nurse
communicates with the patient with empathy. Studies have shown that the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CULTURALLY SAFE NURSING PRACTICE
care received by a patient depends on the child who exercises sensitivity
and comprehension for the variations between patients and emotions
concerning disease (Everson et al., 2015). Empathy is an innate behaviour
that I use in present nursing, but difficulties are to be overcome, and
circumstances where judgment is a first thought. This behaviour is an
ongoing area in my clinical practice for growth.
For this author, the organisation's private skills are developed well in my
career, but using this skill in the field of nursing is an ongoing job as I am
unable to handle patient care duties. The NMBA (2018) guideline states that
nurses need to exercise safely and competently in their professional
behaviour (NMBA 2018). The patient has a feeling of cultural security
through confidence in the clinical care that I provide, through effective and
well-prepared exercise.
Conclusion:
Cultural safety is a vital cog in health care service. Inequalities in the sector
of healthcare should be eroded. Planning for the elderly and the disabled
should be more suitable and suitable. Power and personal values should be
used effectively to bring the patient quick recovery and beneficial results.
The cultural safety guidelines give the nurses a clear overview of efficient
and culturally secure nursing procedures.
care received by a patient depends on the child who exercises sensitivity
and comprehension for the variations between patients and emotions
concerning disease (Everson et al., 2015). Empathy is an innate behaviour
that I use in present nursing, but difficulties are to be overcome, and
circumstances where judgment is a first thought. This behaviour is an
ongoing area in my clinical practice for growth.
For this author, the organisation's private skills are developed well in my
career, but using this skill in the field of nursing is an ongoing job as I am
unable to handle patient care duties. The NMBA (2018) guideline states that
nurses need to exercise safely and competently in their professional
behaviour (NMBA 2018). The patient has a feeling of cultural security
through confidence in the clinical care that I provide, through effective and
well-prepared exercise.
Conclusion:
Cultural safety is a vital cog in health care service. Inequalities in the sector
of healthcare should be eroded. Planning for the elderly and the disabled
should be more suitable and suitable. Power and personal values should be
used effectively to bring the patient quick recovery and beneficial results.
The cultural safety guidelines give the nurses a clear overview of efficient
and culturally secure nursing procedures.
5CULTURALLY SAFE NURSING PRACTICE
References:
Almutairi, A. F., McCarthy, A., & Gardner, G. E. (2015). Understanding cultural
competence in a multicultural nursing workforce: Registered nurses’
experience in Saudi Arabia. Journal of Transcultural Nursing, 26(1), 16–
23.
Crawford, T., & Candlin, S. (2013). Investigating the language needs of
culturally and linguistically diverse nursing students to assist their
completion of the bachelor of nursing programme to become safe and
effective practitioners. Nurse Education Today, 33(8), 796–801.
Douglas, M. K., Pierce, J. U., Rosenkoetter, M., Pacquiao, D., Callister, L. C.,
Hattar-Pollara, M., … Purnell, L. (2013). Standards of practice for
culturally competent nursing care: 2011 update. SALUTE E SOCIETÀ.
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-
Pollara, M., Lauderdale, J., … Purnell, L. (2014). Guidelines for
implementing culturally competent nursing care. Journal of
Transcultural Nursing, 25(2), 109–121.
Duff, B. (2013). Creating a culture of safety by coaching clinicians to
competence. Elsevier.
Everson, N., Levett-Jones, T., Lapkin, S., Pitt, V., Van der Riet, P., Rossiter, R.,
… Courtney-Pratt, H. (2015). Measuring the impact of a 3D simulation
experience on nursing students’ cultural empathy using a modified
version of the Kiersma-Chen Empathy Scale. Journal of Clinical Nursing,
24(19–20), 2849–2858.
Kangasniemi, M., Vaismoradi, M., Jasper, M., & Turunen, H. (2013). Ethical
issues in patient safety: Implications for nursing management. Nursing
Ethics, 20(8), 904–916.
References:
Almutairi, A. F., McCarthy, A., & Gardner, G. E. (2015). Understanding cultural
competence in a multicultural nursing workforce: Registered nurses’
experience in Saudi Arabia. Journal of Transcultural Nursing, 26(1), 16–
23.
Crawford, T., & Candlin, S. (2013). Investigating the language needs of
culturally and linguistically diverse nursing students to assist their
completion of the bachelor of nursing programme to become safe and
effective practitioners. Nurse Education Today, 33(8), 796–801.
Douglas, M. K., Pierce, J. U., Rosenkoetter, M., Pacquiao, D., Callister, L. C.,
Hattar-Pollara, M., … Purnell, L. (2013). Standards of practice for
culturally competent nursing care: 2011 update. SALUTE E SOCIETÀ.
Douglas, M. K., Rosenkoetter, M., Pacquiao, D. F., Callister, L. C., Hattar-
Pollara, M., Lauderdale, J., … Purnell, L. (2014). Guidelines for
implementing culturally competent nursing care. Journal of
Transcultural Nursing, 25(2), 109–121.
Duff, B. (2013). Creating a culture of safety by coaching clinicians to
competence. Elsevier.
Everson, N., Levett-Jones, T., Lapkin, S., Pitt, V., Van der Riet, P., Rossiter, R.,
… Courtney-Pratt, H. (2015). Measuring the impact of a 3D simulation
experience on nursing students’ cultural empathy using a modified
version of the Kiersma-Chen Empathy Scale. Journal of Clinical Nursing,
24(19–20), 2849–2858.
Kangasniemi, M., Vaismoradi, M., Jasper, M., & Turunen, H. (2013). Ethical
issues in patient safety: Implications for nursing management. Nursing
Ethics, 20(8), 904–916.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CULTURALLY SAFE NURSING PRACTICE
Kellett, P., & Fitton, C. (2017). Supporting transvisibility and gender diversity
in nursing practice and education: Embracing cultural safety. Nursing
Inquiry, 24(1), e12146.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards
for practice.Retrieved from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/Professional-standards.aspx
Nursing and Midwifery Board of Australia. (2018). Code of conduct for nurses.
Retrieved from http://www.nursingmidwiferyboard.gov.au/Codes-
Guidelines-Statements/Professionalstandards.aspx
Repo, H., Vahlberg, T., Salminen, L., Papadopoulos, I., & Leino-Kilpi, H.
(2017). The cultural competence of graduating nursing students.
Journal of Transcultural Nursing, 28(1), 98–107.
Kellett, P., & Fitton, C. (2017). Supporting transvisibility and gender diversity
in nursing practice and education: Embracing cultural safety. Nursing
Inquiry, 24(1), e12146.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards
for practice.Retrieved from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/Professional-standards.aspx
Nursing and Midwifery Board of Australia. (2018). Code of conduct for nurses.
Retrieved from http://www.nursingmidwiferyboard.gov.au/Codes-
Guidelines-Statements/Professionalstandards.aspx
Repo, H., Vahlberg, T., Salminen, L., Papadopoulos, I., & Leino-Kilpi, H.
(2017). The cultural competence of graduating nursing students.
Journal of Transcultural Nursing, 28(1), 98–107.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CULTURALLY SAFE NURSING PRACTICE
Appendix:
Figure 1: Mind map of my beliefs, behaviours and values
Appendix:
Figure 1: Mind map of my beliefs, behaviours and values
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





