Culture as a Determinant of Health: Strategies and Implications
VerifiedAdded on 2020/04/07
|10
|3370
|84
Essay
AI Summary
This essay examines the critical role of culture as a determinant of health, particularly focusing on the indigenous populations in Australia. It highlights the historical suppression faced by these communities, leading to adverse health outcomes like high mortality rates, chronic diseases, and mental health issues. The paper discusses how traditional healthcare approaches often fail to address cultural complexities and indigenous healing processes. It emphasizes the importance of a population health approach, considering non-medical determinants like cultural identity, socioeconomic status, and access to healthcare. The essay explores human rights-based health approaches, empowerment dynamics, and the influence of power and culture on health and well-being. It also delves into the links between poverty, chronic stress, and health disparities, as well as the impact of community control over health services. Finally, the paper outlines strategies to promote cultural health determinants and bridge the health gap between indigenous and non-indigenous communities, emphasizing the need for cultural sensitivity and tailored interventions.

Culture as a determinant of health
Name
Title
University Affiliation
Name
Title
University Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Culture as a determinant of health 2
Culture as a determinant of health
Abstract
Indigenous populations in Australia are subject to venerable outcomes of historical
suppression. These consequences result to high mortality rates, poor health conditions n
comparison to non indigenous populations and inexplicably high levels of diseases like
diabetes, mental health problems and alcoholism. There extreme poverty levels translate
directly to low levels of education that reflect to economic adversity, lower attainment in
education, no access or little access to high quality healthcare and social dysfunction
(Iwelunmor et al., 2014).
Traditional Medicare approaches primarily focus on disease treatment and
progression, therefore cultural complexities and indigenous healing processes are not captured
in plan designs meant to improve healthcare and change health behaviors’ in these
communities. These papers role hence is to describe the role of culture as a determinant of
health and strategies to work effectively with these cultures.
Summary
Modern medical science views health as primarily lack of defect or disease in the
body, whereby, the body systems are operating normally. These poses limitations as new
technology, new drug and treatment discoveries increase the cost of Medicare. This has
continued to rise in the recent past. In practice, this materialistic approach therefore results in
symptomatic and piecemeal approach to ill health. Specific cures fix symptoms and cure
diseases without dealing with symptom causes and individuals as a whole.
Focusing only on aspects measured and observed in the laboratory leaves a large blind
spot that the medical model cannot solve as it views people like body systems working
together. Using an approach that takes into account human spirit, emotions and mind brings
about other factors that determine healthcare. The population health approach insists on a
state of complete mental, social wellbeing. In analyzing individual and populations’ health,
non medical determinants come into play. Cultural identity, equity, safety, education, social
economic status, infrastructure, social integration, inclusions, community and geography
influences provision of or access to medical services (Basnyat & Dutta, 2012). Important
determinants of Australians indigenous populations’ health is inequality; including the lower
standards of infrastructures of health and healthcare equal access when compared to other
Culture as a determinant of health
Abstract
Indigenous populations in Australia are subject to venerable outcomes of historical
suppression. These consequences result to high mortality rates, poor health conditions n
comparison to non indigenous populations and inexplicably high levels of diseases like
diabetes, mental health problems and alcoholism. There extreme poverty levels translate
directly to low levels of education that reflect to economic adversity, lower attainment in
education, no access or little access to high quality healthcare and social dysfunction
(Iwelunmor et al., 2014).
Traditional Medicare approaches primarily focus on disease treatment and
progression, therefore cultural complexities and indigenous healing processes are not captured
in plan designs meant to improve healthcare and change health behaviors’ in these
communities. These papers role hence is to describe the role of culture as a determinant of
health and strategies to work effectively with these cultures.
Summary
Modern medical science views health as primarily lack of defect or disease in the
body, whereby, the body systems are operating normally. These poses limitations as new
technology, new drug and treatment discoveries increase the cost of Medicare. This has
continued to rise in the recent past. In practice, this materialistic approach therefore results in
symptomatic and piecemeal approach to ill health. Specific cures fix symptoms and cure
diseases without dealing with symptom causes and individuals as a whole.
Focusing only on aspects measured and observed in the laboratory leaves a large blind
spot that the medical model cannot solve as it views people like body systems working
together. Using an approach that takes into account human spirit, emotions and mind brings
about other factors that determine healthcare. The population health approach insists on a
state of complete mental, social wellbeing. In analyzing individual and populations’ health,
non medical determinants come into play. Cultural identity, equity, safety, education, social
economic status, infrastructure, social integration, inclusions, community and geography
influences provision of or access to medical services (Basnyat & Dutta, 2012). Important
determinants of Australians indigenous populations’ health is inequality; including the lower
standards of infrastructures of health and healthcare equal access when compared to other
Culture as a determinant of health 3
Australians. The National Strategic Framework for Aboriginal and Torres Strait Islander
Health 2003-2013 guides Australia’s indigenous health policy. The main concern therefore is
to bridge the gap between the indigenous people and the other population.
Human rights and empowerment practice
Rights inherent to all human beings are termed as human rights. No matter what our
place of dwelling, nationality, color, national or ethnic group, language, religion or other
status, human rights are entitled to all without discrimination. These rights are indivisible,
interdependent and interrelated. They are guaranteed and expressed by law in forms of
customary international law and treaties. The ICESCR (International Covenant on Economic,
Social and Cultural Rights) includes the right to education, the right to adequate living
standards i.e. adequate food, housing and clothing and the right to enjoyment of the highest
attainable standard of mental and physical health in articles 13, 11 and 12 consecutively. The
covenant in article 2 requires that governments to the maximum of their resource will take
steps to make realizable all the rights in the covenant. In addition to that non discriminatory
enjoyment of the rights should apply. The human rights based health approach has a set
framework that is focused to offset inequalities and ensure people enjoy the highest health
standards attainable (Dutta et al., 2015).
It emphasis governments accountability for outcomes of social economic nature in
different sectors as legal obligations measured against human rights system norms.
Fundamental principles are established that guide development of policies that ensure equal
opportunity provision to indigenous people and that there is no discrimination against through
distinctive cultural status recognition. It outlines a criteria used to asses program interventions
and health policy to ascertain that services are of sufficient quality, appropriate, available and
accessible by ensuring they don’t fall below the essential minimum level for human rights.
Requires the government to demonstrate; targeted approach of issues in collaboration with
indigenous people; to achieve within a timeframe the defined goals (Rubincam et al., 215). It
places on the government a burden to justify use of all resources in its disposal as a matter of
priority to satisfy the right to health.
Dynamics of power and culture that shape health and wellbeing
In the empowerment matrix, community health work terrain is multidimensional with
the health worker being the primary instrument that is involved in practice since the work is
Australians. The National Strategic Framework for Aboriginal and Torres Strait Islander
Health 2003-2013 guides Australia’s indigenous health policy. The main concern therefore is
to bridge the gap between the indigenous people and the other population.
Human rights and empowerment practice
Rights inherent to all human beings are termed as human rights. No matter what our
place of dwelling, nationality, color, national or ethnic group, language, religion or other
status, human rights are entitled to all without discrimination. These rights are indivisible,
interdependent and interrelated. They are guaranteed and expressed by law in forms of
customary international law and treaties. The ICESCR (International Covenant on Economic,
Social and Cultural Rights) includes the right to education, the right to adequate living
standards i.e. adequate food, housing and clothing and the right to enjoyment of the highest
attainable standard of mental and physical health in articles 13, 11 and 12 consecutively. The
covenant in article 2 requires that governments to the maximum of their resource will take
steps to make realizable all the rights in the covenant. In addition to that non discriminatory
enjoyment of the rights should apply. The human rights based health approach has a set
framework that is focused to offset inequalities and ensure people enjoy the highest health
standards attainable (Dutta et al., 2015).
It emphasis governments accountability for outcomes of social economic nature in
different sectors as legal obligations measured against human rights system norms.
Fundamental principles are established that guide development of policies that ensure equal
opportunity provision to indigenous people and that there is no discrimination against through
distinctive cultural status recognition. It outlines a criteria used to asses program interventions
and health policy to ascertain that services are of sufficient quality, appropriate, available and
accessible by ensuring they don’t fall below the essential minimum level for human rights.
Requires the government to demonstrate; targeted approach of issues in collaboration with
indigenous people; to achieve within a timeframe the defined goals (Rubincam et al., 215). It
places on the government a burden to justify use of all resources in its disposal as a matter of
priority to satisfy the right to health.
Dynamics of power and culture that shape health and wellbeing
In the empowerment matrix, community health work terrain is multidimensional with
the health worker being the primary instrument that is involved in practice since the work is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Culture as a determinant of health 4
about relationships and partnerships. Awareness of the dimensions puts one in a place to use
their power transformatively in power cultural dynamics disempowerment. This matrix
provides useful means of bringing into concept the relationships between empowerment
process, social identities and cultural systems. It refers to the elements landscape existing
outside and within an individual and its interaction make up communities or individuals
capacity to assume control over their wellbeing and health (Betsch et al., 2015).
Psychological elements or more subjective empowerment elements like identity,
consciousness and culture form the internal empowerment terrain. Identity embeds ones’ self
esteem, sense of belonging and self. Consciousness includes intuition, knowledge, critical
thinking ability and skills. These are basically individual capacities that they carry around
with them. They combine to bring out a person’s capacities.
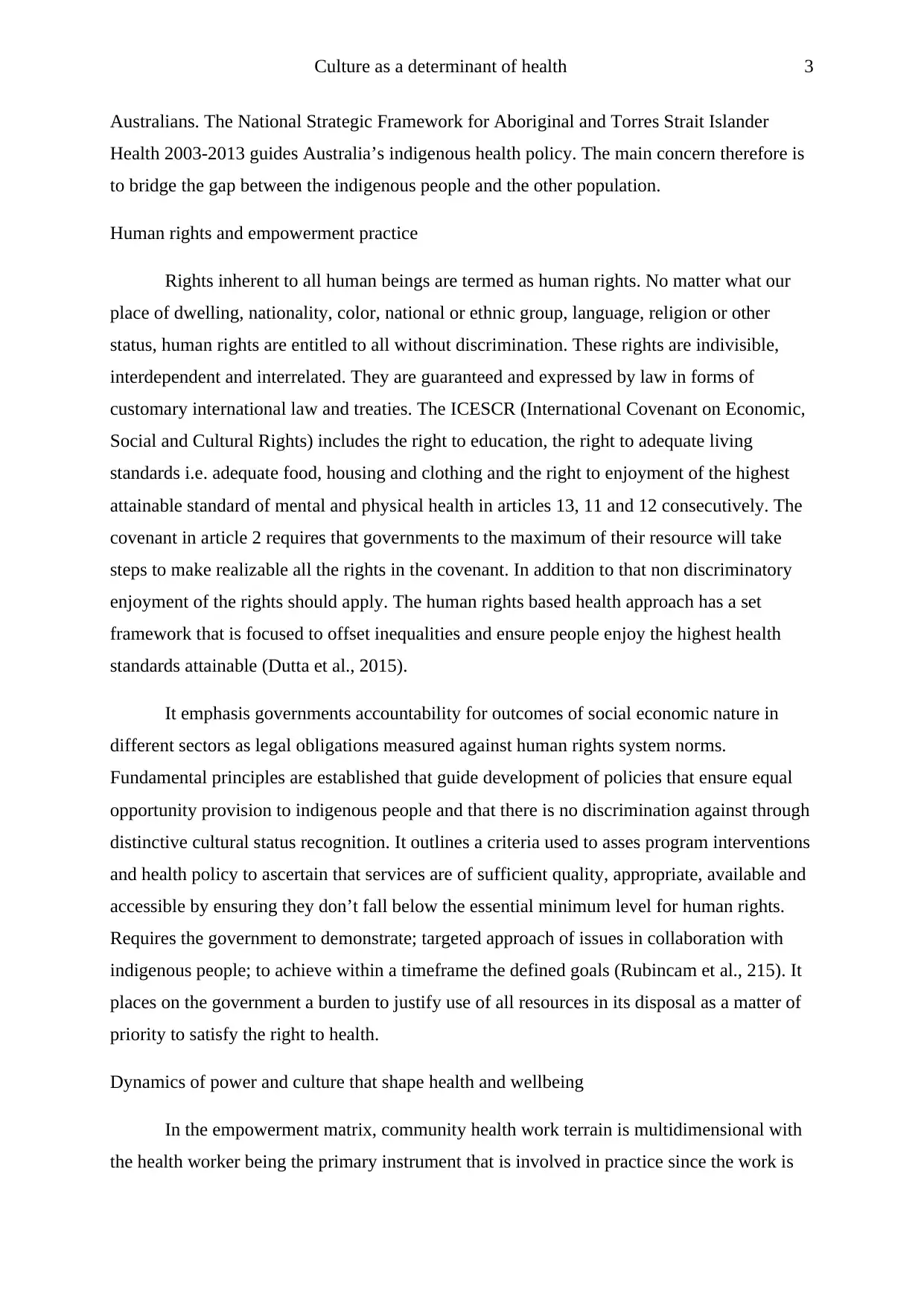
On the other hand, material elements that are outward oriented constitute external
empowerment terrain. These include strategic partnerships, social structures, community
cohesiveness, physical resources, community social networks and other economic resources.
Currently, contemporary and social historic colonization process is considered an important
element characterizing external empowerment terrain and has real life effects on people
(Airhihenbuwa et al., 2016). The Australia’s indigenous cultural health determinants include;
Cultural determinants Sources/ bodies domain
Self determination UNDRIP; UDHR Social inclusion, HR, law and
justice (Basilio et al., 2016).
Freedom from being
discriminated against
ICESCR; ICERD Social policy, politics,
service delivery, law and
justice
Collective and individual
rights
ICCPR; UNDRIP Social policy, employment,
law and justice, economics
Freedom from culture
destruction and assimilation
ICCPR Politics, social policy,
education, service delivery,
law and justice
Protection from relocation CRC; UNDRIP; ICERD Service delivery, law and
justice
Connection and utilization of
traditional and country lands
ICESCR Environment and native title
land rights
about relationships and partnerships. Awareness of the dimensions puts one in a place to use
their power transformatively in power cultural dynamics disempowerment. This matrix
provides useful means of bringing into concept the relationships between empowerment
process, social identities and cultural systems. It refers to the elements landscape existing
outside and within an individual and its interaction make up communities or individuals
capacity to assume control over their wellbeing and health (Betsch et al., 2015).
Psychological elements or more subjective empowerment elements like identity,
consciousness and culture form the internal empowerment terrain. Identity embeds ones’ self
esteem, sense of belonging and self. Consciousness includes intuition, knowledge, critical
thinking ability and skills. These are basically individual capacities that they carry around
with them. They combine to bring out a person’s capacities.
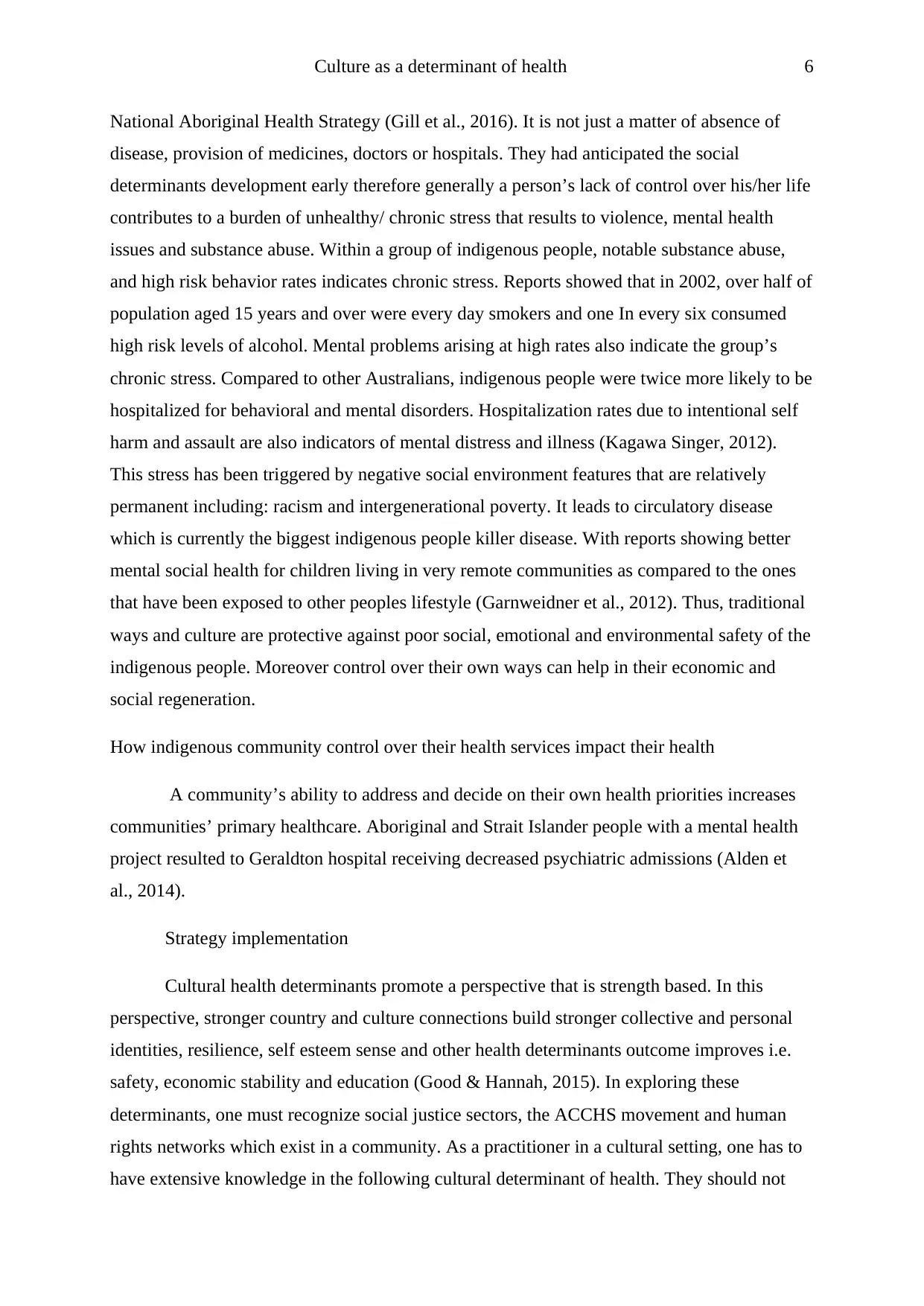
On the other hand, material elements that are outward oriented constitute external
empowerment terrain. These include strategic partnerships, social structures, community
cohesiveness, physical resources, community social networks and other economic resources.
Currently, contemporary and social historic colonization process is considered an important
element characterizing external empowerment terrain and has real life effects on people
(Airhihenbuwa et al., 2016). The Australia’s indigenous cultural health determinants include;
Cultural determinants Sources/ bodies domain
Self determination UNDRIP; UDHR Social inclusion, HR, law and
justice (Basilio et al., 2016).
Freedom from being
discriminated against
ICESCR; ICERD Social policy, politics,
service delivery, law and
justice
Collective and individual
rights
ICCPR; UNDRIP Social policy, employment,
law and justice, economics
Freedom from culture
destruction and assimilation
ICCPR Politics, social policy,
education, service delivery,
law and justice
Protection from relocation CRC; UNDRIP; ICERD Service delivery, law and
justice
Connection and utilization of
traditional and country lands
ICESCR Environment and native title
land rights
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Culture as a determinant of health 5
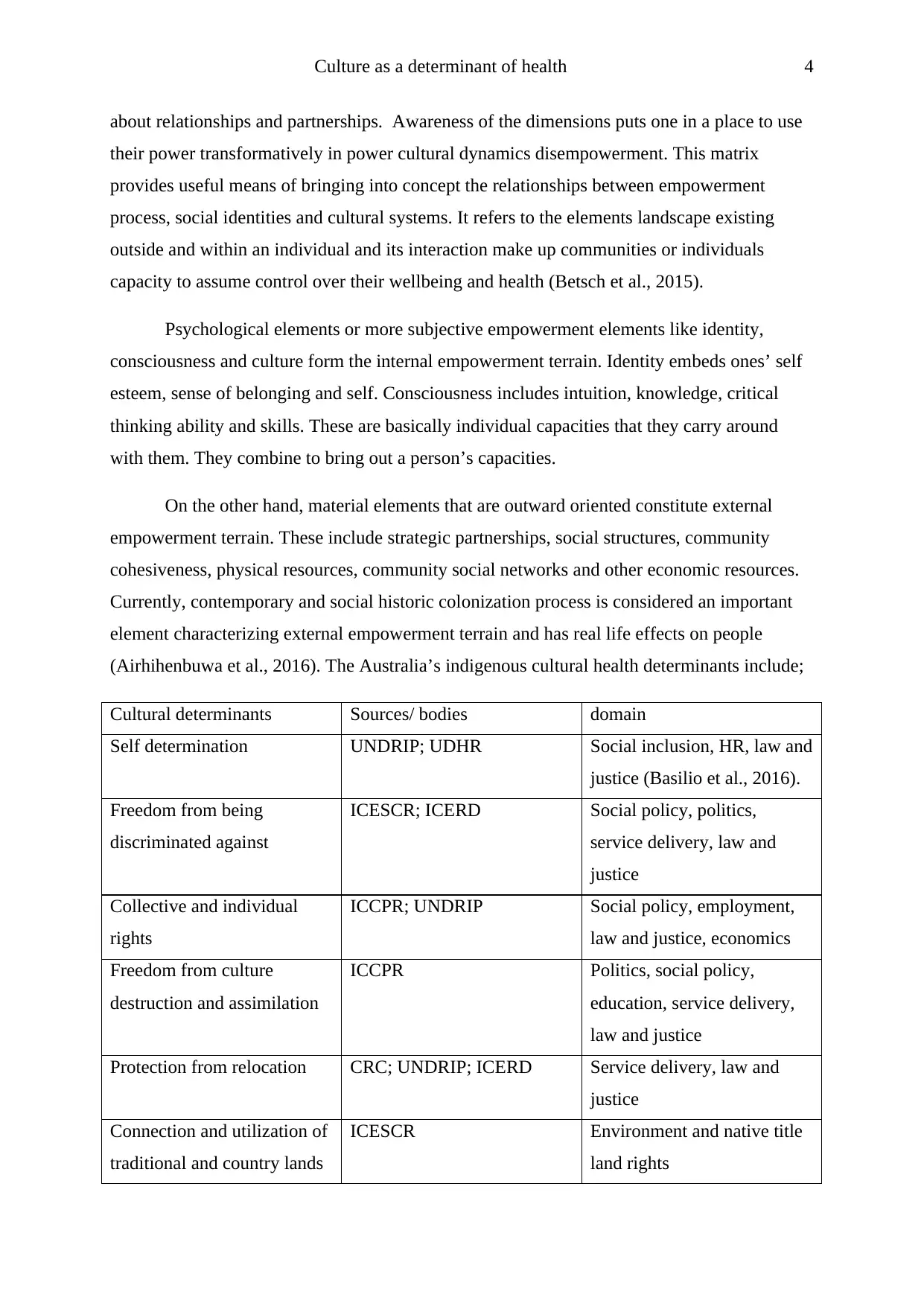
Promotion, reclamation,
preservation and
revitalization of cultural
practices and language
ICESCR;CRC Employment, education
Promotion and protection of
TK, IIP
ILO convention Ethics, law and justice
Understanding of law,
responsibilities and
traditional roles
UNDRIP education
Links between poverty and health status
There is a wide social economic gap between indigenous people and the other
population, averagely their gross household income is half that of the other population.
Indigenous people’s unemployment rate is three times that of the other non indigenous
population. By the year 2004 only half of indigenous students could continue their education
to their 12th year comparing to non- indigenous students. Poverty is hence related to poor
health (Thiam et al., 2015). Literacy and poor education contribute to poor health as it limits
the people’s capacity to use and benefit from health information. Accessibility to medicine
and health services is reduced by poor income. Poverty contributes to run down and
overcrowded housing that increase spread of communicable diseases, poor diet for infants and
future chronic diseases. High risk behaviors’ and smoking have been seen to be contributed
by low social economic status. Poor people have less forms of control over their lives i.e.
financial control, in many cases these contribute to a high unhealthy stress burden. They have
a high psychological demands exposure and limited possibilities to have power over the
situation (Currie et al., 2015). Chronic stress can impact on the bodies’ metabolic functions,
immune system and circulatory system through various hormonal pathways bringing rise to a
series of health problems e.g. heart disease, violence against women mental health and
dysfunction in the community.
Chronic stress and perceptions of control linkages
Indigenous people stated that there was a link between their control of community self
esteem, dignity, justice and their environmental control to their health as shown in their
Promotion, reclamation,
preservation and
revitalization of cultural
practices and language
ICESCR;CRC Employment, education
Promotion and protection of
TK, IIP
ILO convention Ethics, law and justice
Understanding of law,
responsibilities and
traditional roles
UNDRIP education
Links between poverty and health status
There is a wide social economic gap between indigenous people and the other
population, averagely their gross household income is half that of the other population.
Indigenous people’s unemployment rate is three times that of the other non indigenous
population. By the year 2004 only half of indigenous students could continue their education
to their 12th year comparing to non- indigenous students. Poverty is hence related to poor
health (Thiam et al., 2015). Literacy and poor education contribute to poor health as it limits
the people’s capacity to use and benefit from health information. Accessibility to medicine
and health services is reduced by poor income. Poverty contributes to run down and
overcrowded housing that increase spread of communicable diseases, poor diet for infants and
future chronic diseases. High risk behaviors’ and smoking have been seen to be contributed
by low social economic status. Poor people have less forms of control over their lives i.e.
financial control, in many cases these contribute to a high unhealthy stress burden. They have
a high psychological demands exposure and limited possibilities to have power over the
situation (Currie et al., 2015). Chronic stress can impact on the bodies’ metabolic functions,
immune system and circulatory system through various hormonal pathways bringing rise to a
series of health problems e.g. heart disease, violence against women mental health and
dysfunction in the community.
Chronic stress and perceptions of control linkages
Indigenous people stated that there was a link between their control of community self
esteem, dignity, justice and their environmental control to their health as shown in their
Culture as a determinant of health 6
National Aboriginal Health Strategy (Gill et al., 2016). It is not just a matter of absence of
disease, provision of medicines, doctors or hospitals. They had anticipated the social
determinants development early therefore generally a person’s lack of control over his/her life
contributes to a burden of unhealthy/ chronic stress that results to violence, mental health
issues and substance abuse. Within a group of indigenous people, notable substance abuse,
and high risk behavior rates indicates chronic stress. Reports showed that in 2002, over half of
population aged 15 years and over were every day smokers and one In every six consumed
high risk levels of alcohol. Mental problems arising at high rates also indicate the group’s
chronic stress. Compared to other Australians, indigenous people were twice more likely to be
hospitalized for behavioral and mental disorders. Hospitalization rates due to intentional self
harm and assault are also indicators of mental distress and illness (Kagawa Singer, 2012).
This stress has been triggered by negative social environment features that are relatively
permanent including: racism and intergenerational poverty. It leads to circulatory disease
which is currently the biggest indigenous people killer disease. With reports showing better
mental social health for children living in very remote communities as compared to the ones
that have been exposed to other peoples lifestyle (Garnweidner et al., 2012). Thus, traditional
ways and culture are protective against poor social, emotional and environmental safety of the
indigenous people. Moreover control over their own ways can help in their economic and
social regeneration.
How indigenous community control over their health services impact their health
A community’s ability to address and decide on their own health priorities increases
communities’ primary healthcare. Aboriginal and Strait Islander people with a mental health
project resulted to Geraldton hospital receiving decreased psychiatric admissions (Alden et
al., 2014).
Strategy implementation
Cultural health determinants promote a perspective that is strength based. In this
perspective, stronger country and culture connections build stronger collective and personal
identities, resilience, self esteem sense and other health determinants outcome improves i.e.
safety, economic stability and education (Good & Hannah, 2015). In exploring these
determinants, one must recognize social justice sectors, the ACCHS movement and human
rights networks which exist in a community. As a practitioner in a cultural setting, one has to
have extensive knowledge in the following cultural determinant of health. They should not
National Aboriginal Health Strategy (Gill et al., 2016). It is not just a matter of absence of
disease, provision of medicines, doctors or hospitals. They had anticipated the social
determinants development early therefore generally a person’s lack of control over his/her life
contributes to a burden of unhealthy/ chronic stress that results to violence, mental health
issues and substance abuse. Within a group of indigenous people, notable substance abuse,
and high risk behavior rates indicates chronic stress. Reports showed that in 2002, over half of
population aged 15 years and over were every day smokers and one In every six consumed
high risk levels of alcohol. Mental problems arising at high rates also indicate the group’s
chronic stress. Compared to other Australians, indigenous people were twice more likely to be
hospitalized for behavioral and mental disorders. Hospitalization rates due to intentional self
harm and assault are also indicators of mental distress and illness (Kagawa Singer, 2012).
This stress has been triggered by negative social environment features that are relatively
permanent including: racism and intergenerational poverty. It leads to circulatory disease
which is currently the biggest indigenous people killer disease. With reports showing better
mental social health for children living in very remote communities as compared to the ones
that have been exposed to other peoples lifestyle (Garnweidner et al., 2012). Thus, traditional
ways and culture are protective against poor social, emotional and environmental safety of the
indigenous people. Moreover control over their own ways can help in their economic and
social regeneration.
How indigenous community control over their health services impact their health
A community’s ability to address and decide on their own health priorities increases
communities’ primary healthcare. Aboriginal and Strait Islander people with a mental health
project resulted to Geraldton hospital receiving decreased psychiatric admissions (Alden et
al., 2014).
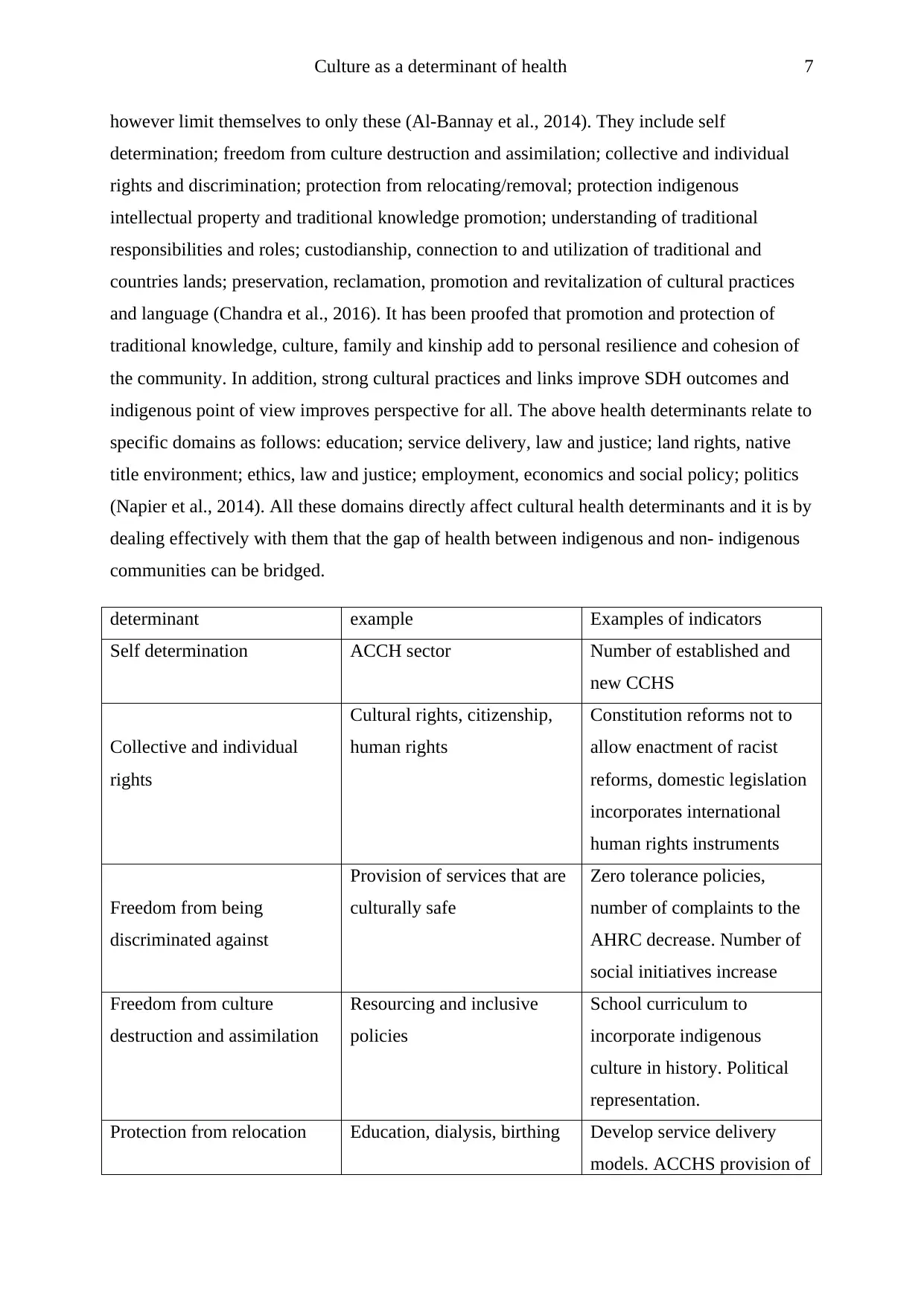
Strategy implementation
Cultural health determinants promote a perspective that is strength based. In this
perspective, stronger country and culture connections build stronger collective and personal
identities, resilience, self esteem sense and other health determinants outcome improves i.e.
safety, economic stability and education (Good & Hannah, 2015). In exploring these
determinants, one must recognize social justice sectors, the ACCHS movement and human
rights networks which exist in a community. As a practitioner in a cultural setting, one has to
have extensive knowledge in the following cultural determinant of health. They should not
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Culture as a determinant of health 7
however limit themselves to only these (Al-Bannay et al., 2014). They include self
determination; freedom from culture destruction and assimilation; collective and individual
rights and discrimination; protection from relocating/removal; protection indigenous
intellectual property and traditional knowledge promotion; understanding of traditional
responsibilities and roles; custodianship, connection to and utilization of traditional and
countries lands; preservation, reclamation, promotion and revitalization of cultural practices
and language (Chandra et al., 2016). It has been proofed that promotion and protection of
traditional knowledge, culture, family and kinship add to personal resilience and cohesion of
the community. In addition, strong cultural practices and links improve SDH outcomes and
indigenous point of view improves perspective for all. The above health determinants relate to
specific domains as follows: education; service delivery, law and justice; land rights, native
title environment; ethics, law and justice; employment, economics and social policy; politics
(Napier et al., 2014). All these domains directly affect cultural health determinants and it is by
dealing effectively with them that the gap of health between indigenous and non- indigenous
communities can be bridged.
determinant example Examples of indicators
Self determination ACCH sector Number of established and
new CCHS
Collective and individual
rights
Cultural rights, citizenship,
human rights
Constitution reforms not to
allow enactment of racist
reforms, domestic legislation
incorporates international
human rights instruments
Freedom from being
discriminated against
Provision of services that are
culturally safe
Zero tolerance policies,
number of complaints to the
AHRC decrease. Number of
social initiatives increase
Freedom from culture
destruction and assimilation
Resourcing and inclusive
policies
School curriculum to
incorporate indigenous
culture in history. Political
representation.
Protection from relocation Education, dialysis, birthing Develop service delivery
models. ACCHS provision of
however limit themselves to only these (Al-Bannay et al., 2014). They include self
determination; freedom from culture destruction and assimilation; collective and individual
rights and discrimination; protection from relocating/removal; protection indigenous
intellectual property and traditional knowledge promotion; understanding of traditional
responsibilities and roles; custodianship, connection to and utilization of traditional and
countries lands; preservation, reclamation, promotion and revitalization of cultural practices
and language (Chandra et al., 2016). It has been proofed that promotion and protection of
traditional knowledge, culture, family and kinship add to personal resilience and cohesion of
the community. In addition, strong cultural practices and links improve SDH outcomes and
indigenous point of view improves perspective for all. The above health determinants relate to
specific domains as follows: education; service delivery, law and justice; land rights, native
title environment; ethics, law and justice; employment, economics and social policy; politics
(Napier et al., 2014). All these domains directly affect cultural health determinants and it is by
dealing effectively with them that the gap of health between indigenous and non- indigenous
communities can be bridged.
determinant example Examples of indicators
Self determination ACCH sector Number of established and
new CCHS
Collective and individual
rights
Cultural rights, citizenship,
human rights
Constitution reforms not to
allow enactment of racist
reforms, domestic legislation
incorporates international
human rights instruments
Freedom from being
discriminated against
Provision of services that are
culturally safe
Zero tolerance policies,
number of complaints to the
AHRC decrease. Number of
social initiatives increase
Freedom from culture
destruction and assimilation
Resourcing and inclusive
policies
School curriculum to
incorporate indigenous
culture in history. Political
representation.
Protection from relocation Education, dialysis, birthing Develop service delivery
models. ACCHS provision of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Culture as a determinant of health 8
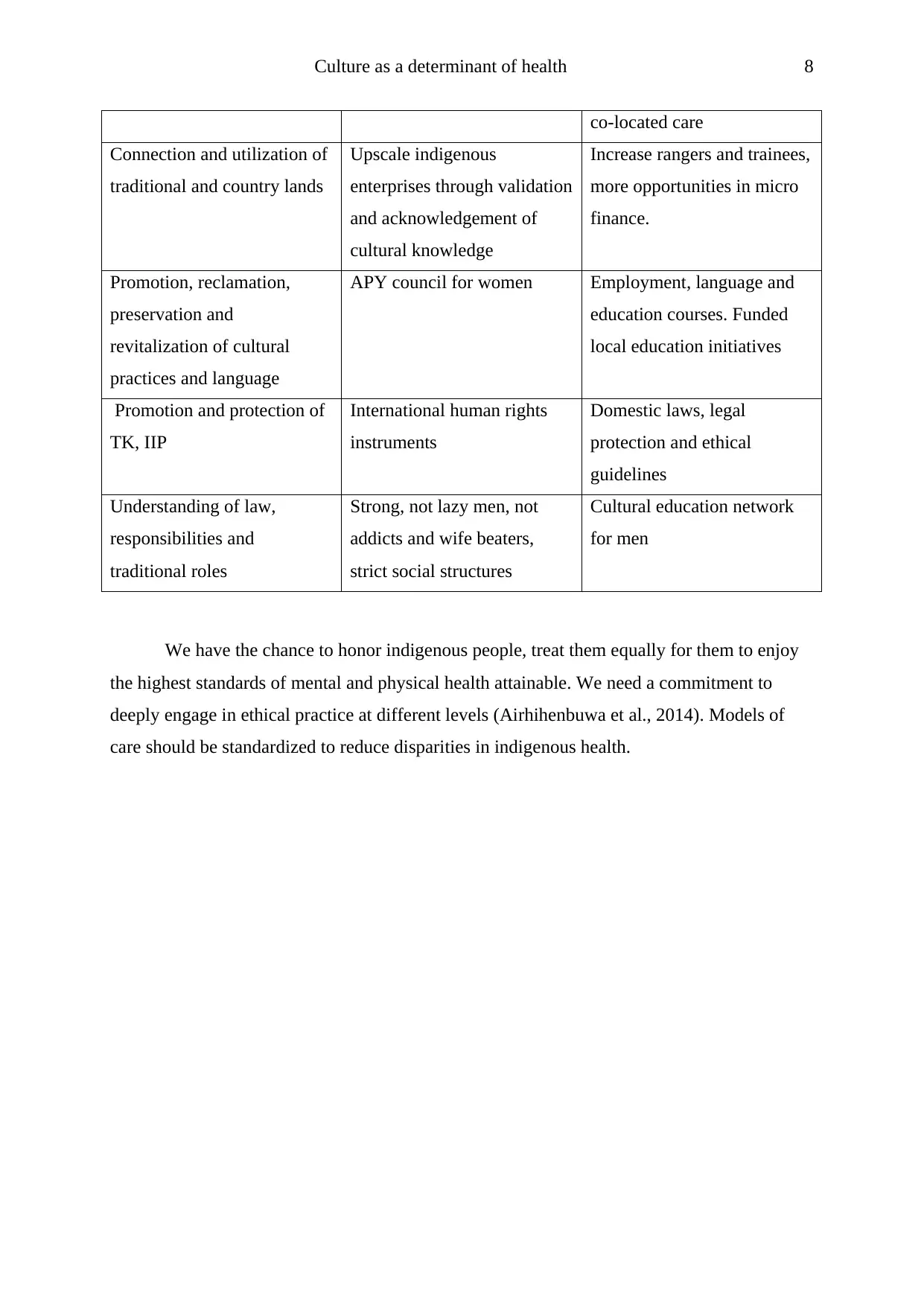
co-located care
Connection and utilization of
traditional and country lands
Upscale indigenous
enterprises through validation
and acknowledgement of
cultural knowledge
Increase rangers and trainees,
more opportunities in micro
finance.
Promotion, reclamation,
preservation and
revitalization of cultural
practices and language
APY council for women Employment, language and
education courses. Funded
local education initiatives
Promotion and protection of
TK, IIP
International human rights
instruments
Domestic laws, legal
protection and ethical
guidelines
Understanding of law,
responsibilities and
traditional roles
Strong, not lazy men, not
addicts and wife beaters,
strict social structures
Cultural education network
for men
We have the chance to honor indigenous people, treat them equally for them to enjoy
the highest standards of mental and physical health attainable. We need a commitment to
deeply engage in ethical practice at different levels (Airhihenbuwa et al., 2014). Models of
care should be standardized to reduce disparities in indigenous health.
co-located care
Connection and utilization of
traditional and country lands
Upscale indigenous
enterprises through validation
and acknowledgement of
cultural knowledge
Increase rangers and trainees,
more opportunities in micro
finance.
Promotion, reclamation,
preservation and
revitalization of cultural
practices and language
APY council for women Employment, language and
education courses. Funded
local education initiatives
Promotion and protection of
TK, IIP
International human rights
instruments
Domestic laws, legal
protection and ethical
guidelines
Understanding of law,
responsibilities and
traditional roles
Strong, not lazy men, not
addicts and wife beaters,
strict social structures
Cultural education network
for men
We have the chance to honor indigenous people, treat them equally for them to enjoy
the highest standards of mental and physical health attainable. We need a commitment to
deeply engage in ethical practice at different levels (Airhihenbuwa et al., 2014). Models of
care should be standardized to reduce disparities in indigenous health.
Culture as a determinant of health 9
References
Airhihenbuwa, C. O., Ford, C. L., & Iwelunmor, J. I. (2014). Why culture matters in health
interventions: Lessons from HIV/AIDS stigma and NCDs. Health Education
Behavior, 41, 78–84.
Airhihenbuwa, C. O., Iwelunmor J. I., Ezepue, C. J., Williams, N. J., & Jean-Louis, G. (2016).
I sleep, because we sleep: A synthesis on the role of culture in sleep behavior research.
Sleep Medicine, 18, 67–73.
Al-Bannay, H., Jarus, T., Jongbloed, L., Yazigi, M., & Dean, E. (2014). Culture as a variable
in health research: Perspectives and caveats. Health Promotion International, 29, 549–
557.
Alden, D. L., Friend, J., Schapira, M., & Stiggelbout, A. (2014). Cultural targeting and
tailoring of shared decision making technology: A theoretical framework for
improving the effectiveness of patient decision aids in culturally diverse groups. Social
Science & Medicine, 105, 1–8.
Basilio, C. D., Kwan, V. S., & Towers, M. J. (2016). Culture and risk assessments: Why
Latino Americans perceive greater risk for diabetes. Culturural Diversity & Ethnic
Minority Psychology, 22, 104–113.
Basnyat, I., & Dutta, M. J. (2012). Reframing motherhood through the culture-centered
approach: Articulations of agency among young Nepalese women. Health
Communication, 27, 273–283.
Betsch, C., Bohm, R., Airhihenbuwa, C. O., Butler, R., Chapman, G. B., Haase, N. B., et al.
(2015). Improving medical decision making and health promotion through culture-
sensitive health communication: An agenda for science and practice. Medical Decision
Making. 36, 811–833.
Chandra, A., Acosta, J., Carman, K. G., Dubowitz, T., Leviton, L., Martin, L. T., et al. (2016).
Building a national culture of health. Santa Monica, CA: RAND.
References
Airhihenbuwa, C. O., Ford, C. L., & Iwelunmor, J. I. (2014). Why culture matters in health
interventions: Lessons from HIV/AIDS stigma and NCDs. Health Education
Behavior, 41, 78–84.
Airhihenbuwa, C. O., Iwelunmor J. I., Ezepue, C. J., Williams, N. J., & Jean-Louis, G. (2016).
I sleep, because we sleep: A synthesis on the role of culture in sleep behavior research.
Sleep Medicine, 18, 67–73.
Al-Bannay, H., Jarus, T., Jongbloed, L., Yazigi, M., & Dean, E. (2014). Culture as a variable
in health research: Perspectives and caveats. Health Promotion International, 29, 549–
557.
Alden, D. L., Friend, J., Schapira, M., & Stiggelbout, A. (2014). Cultural targeting and
tailoring of shared decision making technology: A theoretical framework for
improving the effectiveness of patient decision aids in culturally diverse groups. Social
Science & Medicine, 105, 1–8.
Basilio, C. D., Kwan, V. S., & Towers, M. J. (2016). Culture and risk assessments: Why
Latino Americans perceive greater risk for diabetes. Culturural Diversity & Ethnic
Minority Psychology, 22, 104–113.
Basnyat, I., & Dutta, M. J. (2012). Reframing motherhood through the culture-centered
approach: Articulations of agency among young Nepalese women. Health
Communication, 27, 273–283.
Betsch, C., Bohm, R., Airhihenbuwa, C. O., Butler, R., Chapman, G. B., Haase, N. B., et al.
(2015). Improving medical decision making and health promotion through culture-
sensitive health communication: An agenda for science and practice. Medical Decision
Making. 36, 811–833.
Chandra, A., Acosta, J., Carman, K. G., Dubowitz, T., Leviton, L., Martin, L. T., et al. (2016).
Building a national culture of health. Santa Monica, CA: RAND.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Culture as a determinant of health 10
Currie, C. L., Wild, C. T., Schopflocher, D. P., Laing, L., & Veugelers, P. (2013). Illicit and
prescription drug problems among urban Aboriginal adults in Canada: The role of
traditional culture in protection and resilience. Social Science & Medicine, 88, 1–9.
Dutta, M. J. (2015). Communicating health: A culture-centered approach. West Sussex, U.K.:
John Wiley & Sons.
Garnweidner, L. M., Terragni, L., Pettersen, K. S., & Mosdol, A. (2012). Perceptions of the
host country’s food culture among female immigrants from Africa and Asia: Aspects
relevant for cultural sensitivity in nutrition communication. Journal of Nutrition
Education and Behavior, 44, 335–342.
Gill, S., Kuwahara, R., & Wilce, M. (2016). Through a culturally competent lens: Why the
program evaluation standards matter. Health Promotion Practice, 17, 5–8.
Good, M. J., & Hannah, S. D. (2015). “Shattering culture”: Perspectives on cultural
competence and evidence-based practice in mental health services. Transcultural
Psychiatry, 52, 198–221.
Iwelunmor, J., Newsome, V., & Airhihenbuwa, C. O. (2014). Framing the impact of culture
on health: A systematic review of the PEN-3 cultural model and its application in
public health research and interventions. Ethnicity & Health, 19, 20–46.
Kagawa Singer, M., Dressler, W., George, S., & Elwood, W. (2012a). The cultural framework
for health: An integrative approach for research and program design and evaluation.
Bethesda, MD: National Institutes of Health, Office of Behavioral and Social Science
Research.
Kagawa Singer, M (2012b). Applying the concept of culture to reduce health disparities
through health behavior research. Preventive Medicine, 55(5), 356–361.
Napier, A. D., Ancarno, C., Butler, B., Calabrese, J., Chater, A., Chatterjee, H., et al. (2014).
Culture and health. The Lancet, 384(9954), 1607–1639.
Rubincam, C., Lacombe-Duncan, A., & Newman, P. A. (2015). Taking culture seriously in
biomedical HIV prevention trials: A meta-synthesis of qualitative studies. Expert
Review of Vaccines, 15(3), 331–347.
Currie, C. L., Wild, C. T., Schopflocher, D. P., Laing, L., & Veugelers, P. (2013). Illicit and
prescription drug problems among urban Aboriginal adults in Canada: The role of
traditional culture in protection and resilience. Social Science & Medicine, 88, 1–9.
Dutta, M. J. (2015). Communicating health: A culture-centered approach. West Sussex, U.K.:
John Wiley & Sons.
Garnweidner, L. M., Terragni, L., Pettersen, K. S., & Mosdol, A. (2012). Perceptions of the
host country’s food culture among female immigrants from Africa and Asia: Aspects
relevant for cultural sensitivity in nutrition communication. Journal of Nutrition
Education and Behavior, 44, 335–342.
Gill, S., Kuwahara, R., & Wilce, M. (2016). Through a culturally competent lens: Why the
program evaluation standards matter. Health Promotion Practice, 17, 5–8.
Good, M. J., & Hannah, S. D. (2015). “Shattering culture”: Perspectives on cultural
competence and evidence-based practice in mental health services. Transcultural
Psychiatry, 52, 198–221.
Iwelunmor, J., Newsome, V., & Airhihenbuwa, C. O. (2014). Framing the impact of culture
on health: A systematic review of the PEN-3 cultural model and its application in
public health research and interventions. Ethnicity & Health, 19, 20–46.
Kagawa Singer, M., Dressler, W., George, S., & Elwood, W. (2012a). The cultural framework
for health: An integrative approach for research and program design and evaluation.
Bethesda, MD: National Institutes of Health, Office of Behavioral and Social Science
Research.
Kagawa Singer, M (2012b). Applying the concept of culture to reduce health disparities
through health behavior research. Preventive Medicine, 55(5), 356–361.
Napier, A. D., Ancarno, C., Butler, B., Calabrese, J., Chater, A., Chatterjee, H., et al. (2014).
Culture and health. The Lancet, 384(9954), 1607–1639.
Rubincam, C., Lacombe-Duncan, A., & Newman, P. A. (2015). Taking culture seriously in
biomedical HIV prevention trials: A meta-synthesis of qualitative studies. Expert
Review of Vaccines, 15(3), 331–347.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





