Should Dementia Patients Be Involved in Healthcare Decisions?
VerifiedAdded on 2022/11/09
|12
|2830
|406
Report
AI Summary
This report is a comprehensive literature review examining the involvement of individuals with dementia in healthcare decision-making processes. The research question, framed using the PICO framework, investigates whether dementia patients should be involved in their healthcare decisions. The report details the search methodology, including the databases used (PubMed, CINAHL, and MEDLINE), search terms, and inclusion/exclusion criteria. A flowchart visually represents the search process and article selection. The study includes a literature review table summarizing key findings from ten articles, encompassing various study designs such as systematic reviews, qualitative studies, and case studies. The discussion section analyzes the capacity of dementia patients to make decisions, emphasizing the importance of patient autonomy and the impact of cognitive impairment. It explores themes such as informed consent, surrogate consent, assisted decision-making, and the challenges associated with involving dementia patients, including the burden on family and caregivers. The report highlights the need for tailored information aids and the role of healthcare professionals in assessing patient decision-making capacity. The review concludes by acknowledging the varying decision-making abilities across dementia stages and the importance of balancing patient autonomy with the limitations imposed by the condition.

Running head: DEMENTIA AND DECISION MAKING 1
Should a person living with dementia be involved in making decision regarding their health care?
Student’s Name
University
Should a person living with dementia be involved in making decision regarding their health care?
Student’s Name
University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
DEMENTIA AND DECISION MAKING 2
Should a person living with dementia be involved in making decision regarding their health
care?
P: Patient living with dementia
I: involvement in decision making
C: lack of involvement or partial involvement with family members
O: quality of decision made by dementia patient
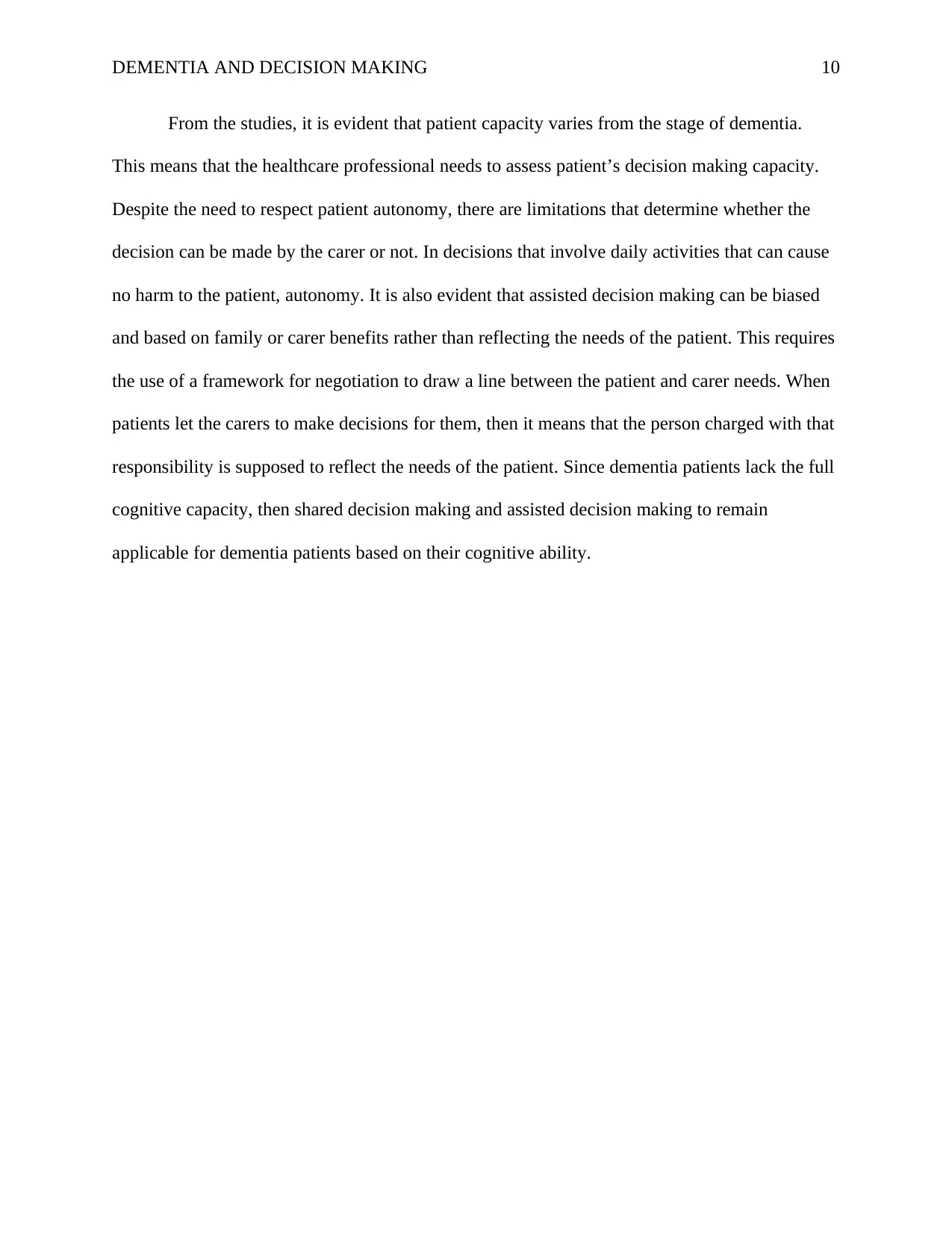
PART 1 - The Flow Chart
The databases used for this study were PubMed, CINAHL, and MEDLINE. The search for the
studies was based on the use of the terms “dementia” and “decision making” which led to 4213
studies. When the search was refined to set for year of publication to be 2010-2019, 318 papers
were found on the topic. The search was refined further to full text articles, academic language of
English and 103 articles were found. This led to the need for a review of the articles found to
pick the best articles that reflected the topic. This led to ten articles which were from different
study designs. The studies found were systematic reviews, rapid scoping review, qualitative
study with a prospective, multiperspective design, Case study and Qualitative multi-case design.
No study was found on randomized controlled trials, cross-sectional study and observational
studies
Should a person living with dementia be involved in making decision regarding their health
care?
P: Patient living with dementia
I: involvement in decision making
C: lack of involvement or partial involvement with family members
O: quality of decision made by dementia patient
PART 1 - The Flow Chart
The databases used for this study were PubMed, CINAHL, and MEDLINE. The search for the
studies was based on the use of the terms “dementia” and “decision making” which led to 4213
studies. When the search was refined to set for year of publication to be 2010-2019, 318 papers
were found on the topic. The search was refined further to full text articles, academic language of
English and 103 articles were found. This led to the need for a review of the articles found to
pick the best articles that reflected the topic. This led to ten articles which were from different
study designs. The studies found were systematic reviews, rapid scoping review, qualitative
study with a prospective, multiperspective design, Case study and Qualitative multi-case design.
No study was found on randomized controlled trials, cross-sectional study and observational
studies
DEMENTIA AND DECISION MAKING 3
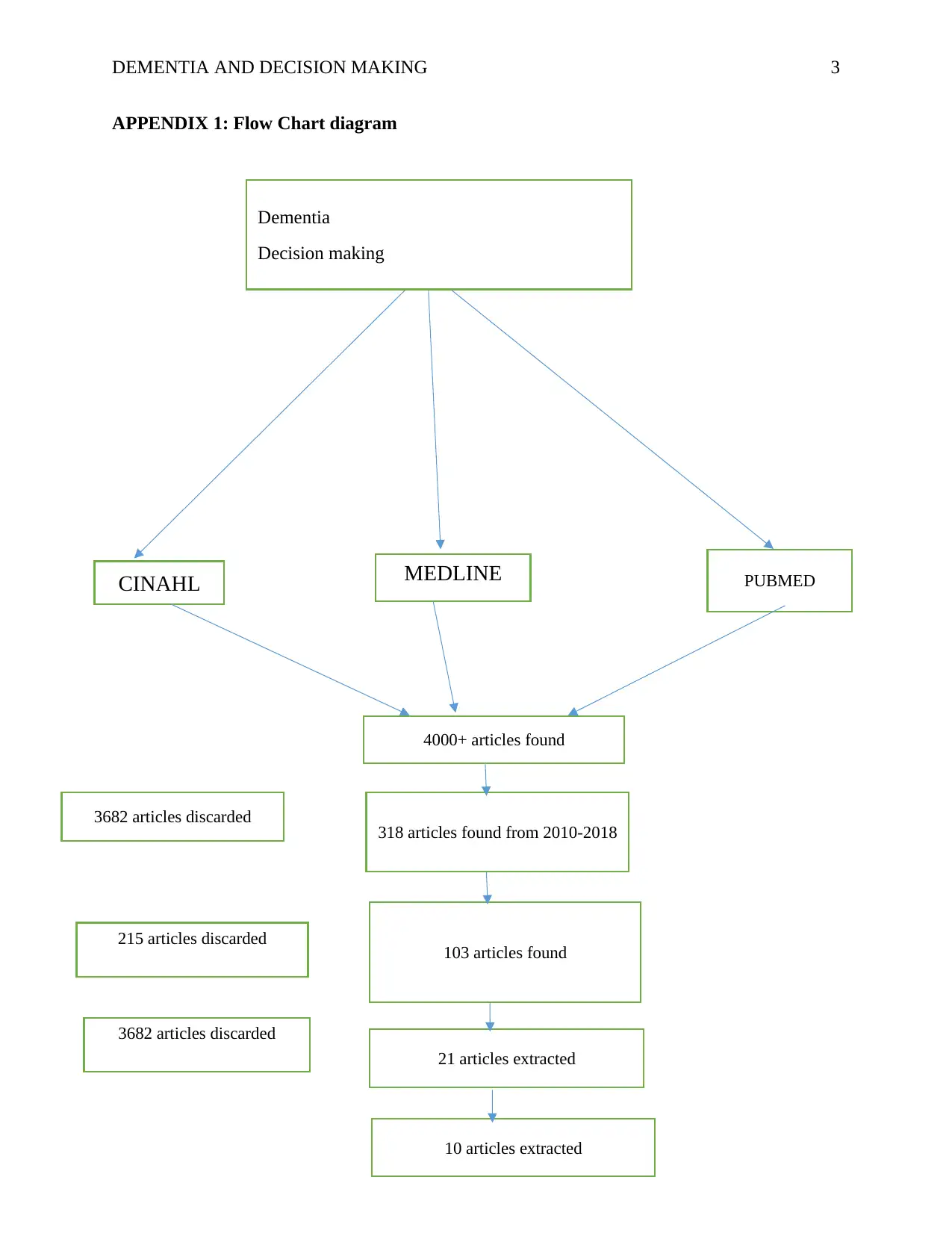
APPENDIX 1: Flow Chart diagram
MEDLINE
Dementia
Decision making
CINAHL MEDLINE PUBMED
4000+ articles found
318 articles found from 2010-2018
103 articles found
21 articles extracted
10 articles extracted
3682 articles discarded
215 articles discarded
3682 articles discarded
APPENDIX 1: Flow Chart diagram
MEDLINE
Dementia
Decision making
CINAHL MEDLINE PUBMED
4000+ articles found
318 articles found from 2010-2018
103 articles found
21 articles extracted
10 articles extracted
3682 articles discarded
215 articles discarded
3682 articles discarded
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
DEMENTIA AND DECISION MAKING 4
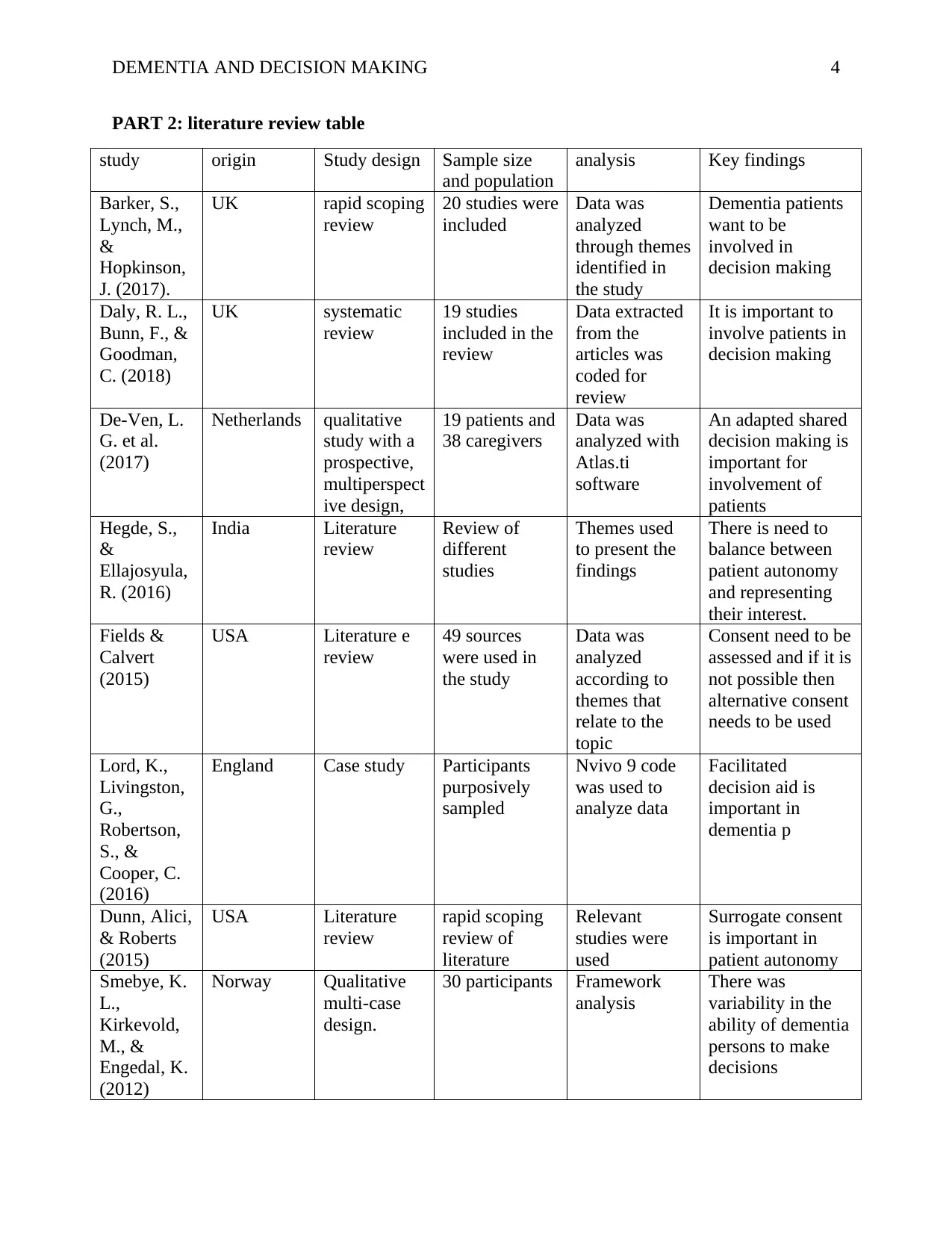
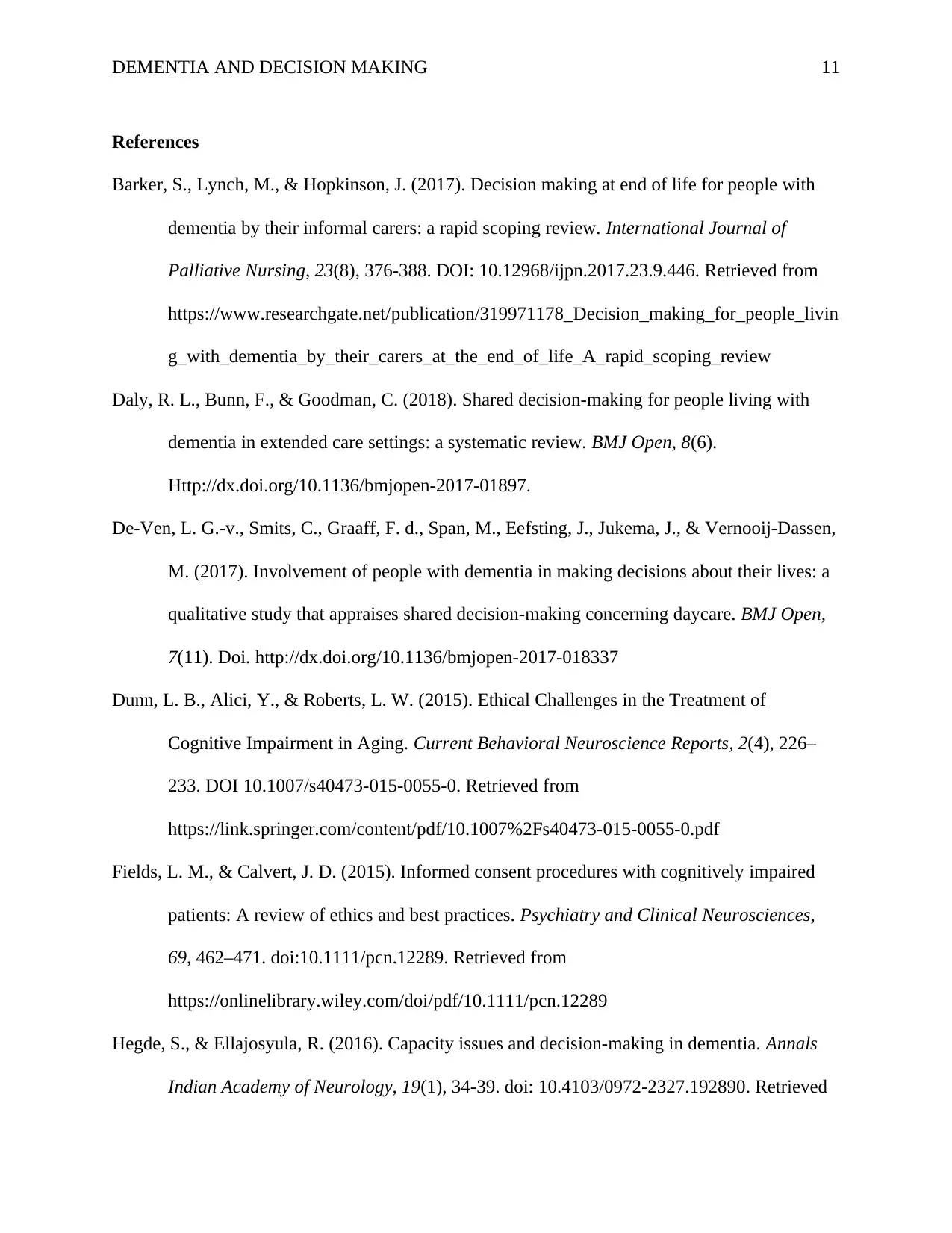
PART 2: literature review table
study origin Study design Sample size
and population
analysis Key findings
Barker, S.,
Lynch, M.,
&
Hopkinson,
J. (2017).
UK rapid scoping
review
20 studies were
included
Data was
analyzed
through themes
identified in
the study
Dementia patients
want to be
involved in
decision making
Daly, R. L.,
Bunn, F., &
Goodman,
C. (2018)
UK systematic
review
19 studies
included in the
review
Data extracted
from the
articles was
coded for
review
It is important to
involve patients in
decision making
De-Ven, L.
G. et al.
(2017)
Netherlands qualitative
study with a
prospective,
multiperspect
ive design,
19 patients and
38 caregivers
Data was
analyzed with
Atlas.ti
software
An adapted shared
decision making is
important for
involvement of
patients
Hegde, S.,
&
Ellajosyula,
R. (2016)
India Literature
review
Review of
different
studies
Themes used
to present the
findings
There is need to
balance between
patient autonomy
and representing
their interest.
Fields &
Calvert
(2015)
USA Literature e
review
49 sources
were used in
the study
Data was
analyzed
according to
themes that
relate to the
topic
Consent need to be
assessed and if it is
not possible then
alternative consent
needs to be used
Lord, K.,
Livingston,
G.,
Robertson,
S., &
Cooper, C.
(2016)
England Case study Participants
purposively
sampled
Nvivo 9 code
was used to
analyze data
Facilitated
decision aid is
important in
dementia p
Dunn, Alici,
& Roberts
(2015)
USA Literature
review
rapid scoping
review of
literature
Relevant
studies were
used
Surrogate consent
is important in
patient autonomy
Smebye, K.
L.,
Kirkevold,
M., &
Engedal, K.
(2012)
Norway Qualitative
multi-case
design.
30 participants Framework
analysis
There was
variability in the
ability of dementia
persons to make
decisions
PART 2: literature review table
study origin Study design Sample size
and population
analysis Key findings
Barker, S.,
Lynch, M.,
&
Hopkinson,
J. (2017).
UK rapid scoping
review
20 studies were
included
Data was
analyzed
through themes
identified in
the study
Dementia patients
want to be
involved in
decision making
Daly, R. L.,
Bunn, F., &
Goodman,
C. (2018)
UK systematic
review
19 studies
included in the
review
Data extracted
from the
articles was
coded for
review
It is important to
involve patients in
decision making
De-Ven, L.
G. et al.
(2017)
Netherlands qualitative
study with a
prospective,
multiperspect
ive design,
19 patients and
38 caregivers
Data was
analyzed with
Atlas.ti
software
An adapted shared
decision making is
important for
involvement of
patients
Hegde, S.,
&
Ellajosyula,
R. (2016)
India Literature
review
Review of
different
studies
Themes used
to present the
findings
There is need to
balance between
patient autonomy
and representing
their interest.
Fields &
Calvert
(2015)
USA Literature e
review
49 sources
were used in
the study
Data was
analyzed
according to
themes that
relate to the
topic
Consent need to be
assessed and if it is
not possible then
alternative consent
needs to be used
Lord, K.,
Livingston,
G.,
Robertson,
S., &
Cooper, C.
(2016)
England Case study Participants
purposively
sampled
Nvivo 9 code
was used to
analyze data
Facilitated
decision aid is
important in
dementia p
Dunn, Alici,
& Roberts
(2015)
USA Literature
review
rapid scoping
review of
literature
Relevant
studies were
used
Surrogate consent
is important in
patient autonomy
Smebye, K.
L.,
Kirkevold,
M., &
Engedal, K.
(2012)
Norway Qualitative
multi-case
design.
30 participants Framework
analysis
There was
variability in the
ability of dementia
persons to make
decisions
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
DEMENTIA AND DECISION MAKING 5
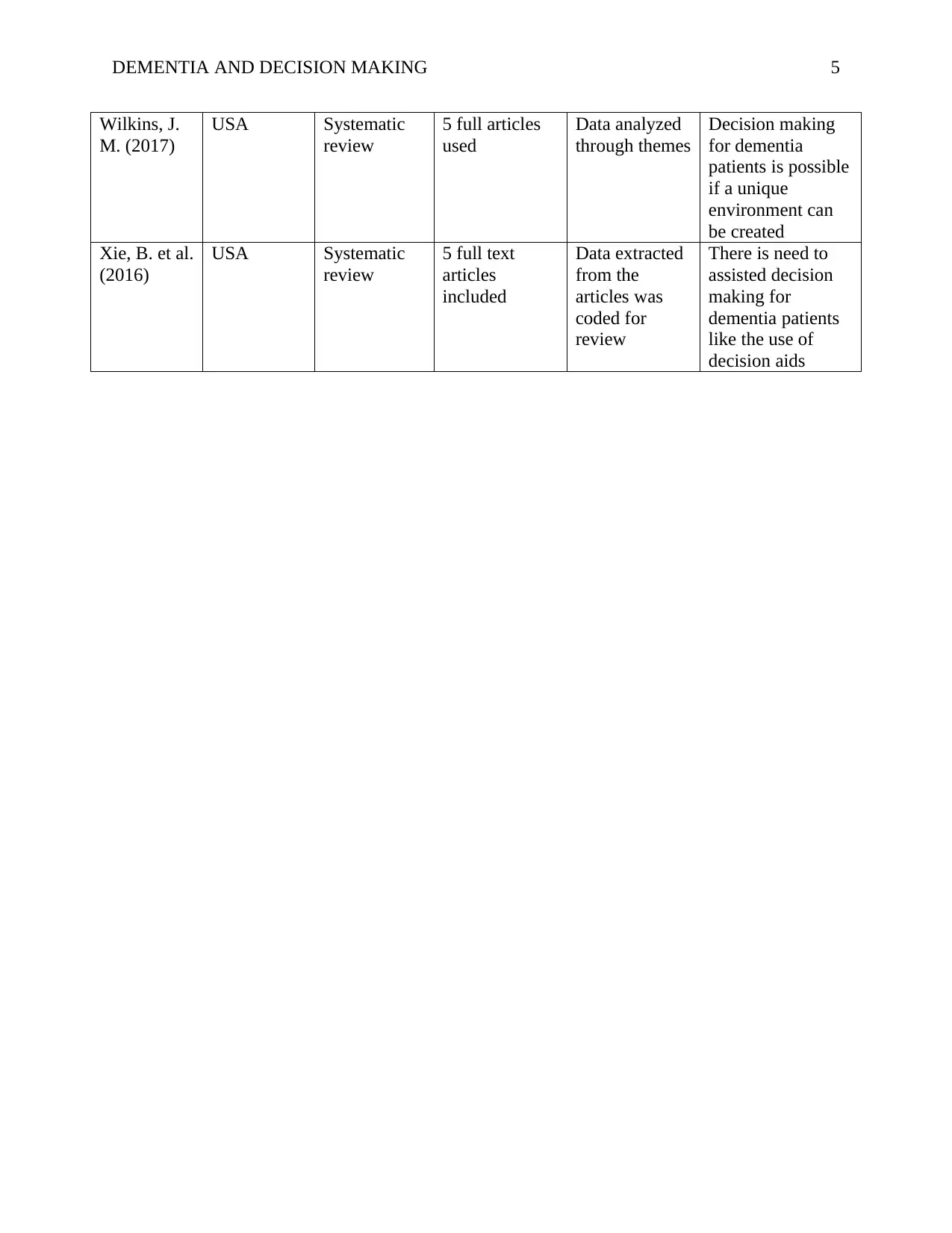
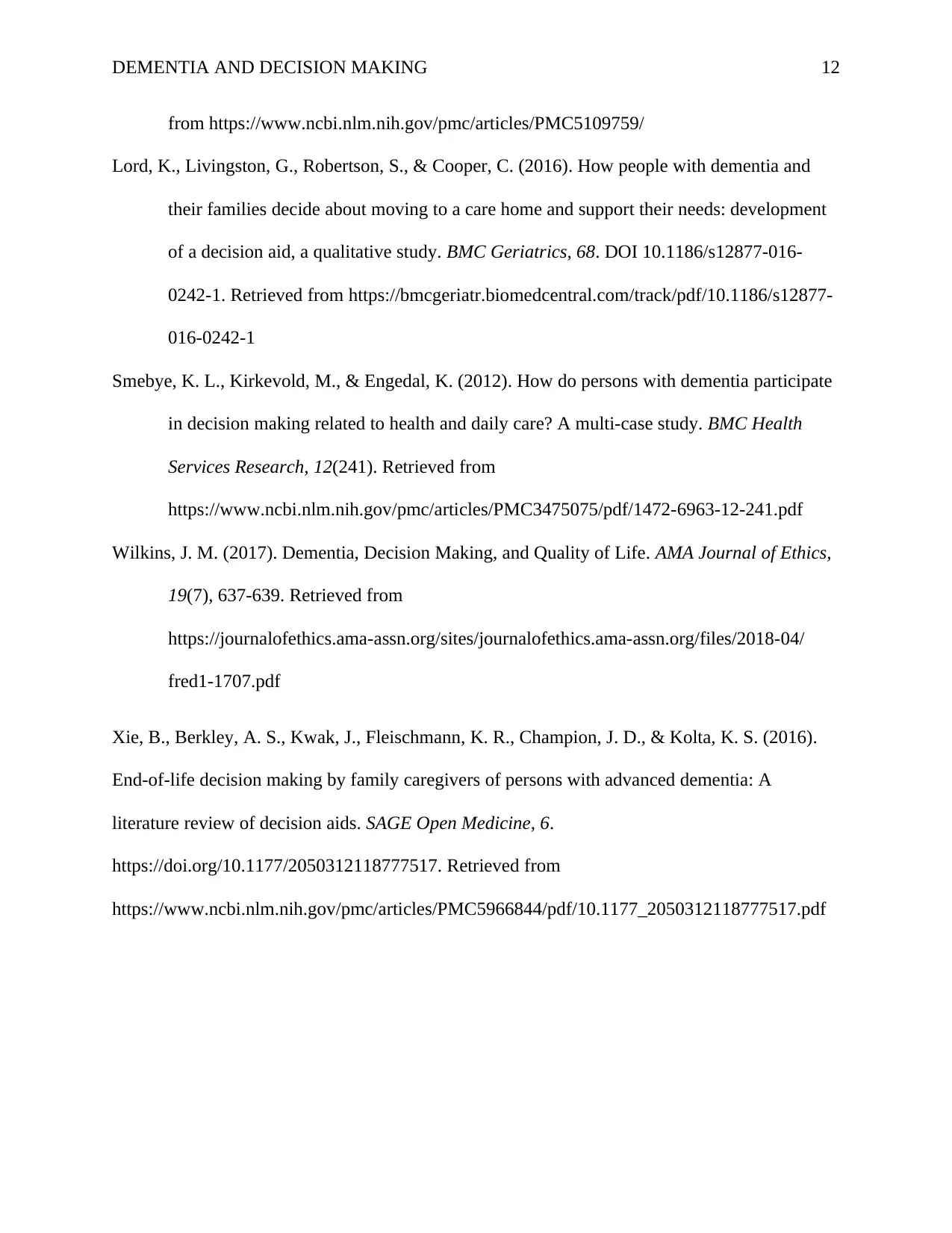
Wilkins, J.
M. (2017)
USA Systematic
review
5 full articles
used
Data analyzed
through themes
Decision making
for dementia
patients is possible
if a unique
environment can
be created
Xie, B. et al.
(2016)
USA Systematic
review
5 full text
articles
included
Data extracted
from the
articles was
coded for
review
There is need to
assisted decision
making for
dementia patients
like the use of
decision aids
Wilkins, J.
M. (2017)
USA Systematic
review
5 full articles
used
Data analyzed
through themes
Decision making
for dementia
patients is possible
if a unique
environment can
be created
Xie, B. et al.
(2016)
USA Systematic
review
5 full text
articles
included
Data extracted
from the
articles was
coded for
review
There is need to
assisted decision
making for
dementia patients
like the use of
decision aids
DEMENTIA AND DECISION MAKING 6
Part 3. Discussion section
The capacity to make one's decision is related to patient autonomy which is seen in the
functional assessment that is made by a clinician to determine the ability of the patient to make
decisions. A dementia diagnosis is not an automatic case that the person will be incapable of
making a decision (Daly, Bunn, & Goodman, 2018). Legislative challenges have been changing
slowly with the UN requiring the patients to have the best legal capacity to participate in decision
making. According to Hegde & Ellajosyula (2016), individual autonomy only exists if the patient
has the capacity for personal decisions and thus this can be assessed by a clinician to determine
personal ability. This means that the patient has to fulfil the above measures to be seen as having
the ability to make a decision. Several studies have been done on the role of dementia people in
decision making in issues about their lives. The patient benefits through the promotion of
dignity, integrity, and personhood as seen in different studies that have been done on the topic. In
the literature review, several studies were found on the topic with different arguments and
justification for the involvement of dementia patients in decision making.
Hegde & Ellajosyula (2016) argues that dementia only limits the cognitive ability of the
individual and it is not automatic that they will be unable to make decisions. Mild and moderate
dementia patients have the ability to assess information and derive meanings from their lives.
The clinician needs to carry out a comprehensive assessment to determine the patient’s decision
making ability. In cases where they are incapable of managing their own decisions, aided devices
can be used as decision guides. There are two levels of decision making that were reported in
most patients; decisions regarding daily activities that posed no harm and delegated decision
making. Delegated decision making entails identifying the person to assist in making major
Part 3. Discussion section
The capacity to make one's decision is related to patient autonomy which is seen in the
functional assessment that is made by a clinician to determine the ability of the patient to make
decisions. A dementia diagnosis is not an automatic case that the person will be incapable of
making a decision (Daly, Bunn, & Goodman, 2018). Legislative challenges have been changing
slowly with the UN requiring the patients to have the best legal capacity to participate in decision
making. According to Hegde & Ellajosyula (2016), individual autonomy only exists if the patient
has the capacity for personal decisions and thus this can be assessed by a clinician to determine
personal ability. This means that the patient has to fulfil the above measures to be seen as having
the ability to make a decision. Several studies have been done on the role of dementia people in
decision making in issues about their lives. The patient benefits through the promotion of
dignity, integrity, and personhood as seen in different studies that have been done on the topic. In
the literature review, several studies were found on the topic with different arguments and
justification for the involvement of dementia patients in decision making.
Hegde & Ellajosyula (2016) argues that dementia only limits the cognitive ability of the
individual and it is not automatic that they will be unable to make decisions. Mild and moderate
dementia patients have the ability to assess information and derive meanings from their lives.
The clinician needs to carry out a comprehensive assessment to determine the patient’s decision
making ability. In cases where they are incapable of managing their own decisions, aided devices
can be used as decision guides. There are two levels of decision making that were reported in
most patients; decisions regarding daily activities that posed no harm and delegated decision
making. Delegated decision making entails identifying the person to assist in making major
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
DEMENTIA AND DECISION MAKING 7
decisions. This is a conscious decision that is made as part patient’s capacity to understand the
inability to make the decision and request for assistance.
In Daly, Bunn, & Goodman (2018) study reported that despite the limited cognitive
ability to make their own decisions, dementia patients value being involved in decision making.
This is based on the UN convention of people with disabilities which requires them to be
involved in different decision-making levels. This study reported the concern of dementia
patients in cases where they were excluded in decision making. This was supported by Hegde &
Ellajosyula (2016) who reported that the participation dementia people participation increases
their quality of life and the decisions that were made. For Daly, Bunn, & Goodman (2018),
assisted decision making is important for cognitively impaired patients which is appreciated by
patients since it heightens self-esteem and reduces depression symptoms to maintain the daily
functioning of the patient. De-Ven, et al. (2017) study concluded that the sharing process needs
to be adapted to highlight the cognitive difficulties that the people face. Thus shared decision
making is reflected in increased capacity for personal obligation, the ability to manage a personal
life and even the participation in social activities.
In these studies, several themes have emerged on whether the patients need to be
involved in decision making or not. One of the themes that have been highlighted is the need for
informed consent through aided support. According to Fields & Calvert (2015), the cognitive
impairment caused by dementia makes most patients lack the full ability to make personal
decisions. This calls for the use of evidence-based approaches in determining the best way to
involve dementia patients. There are existing guidelines on how to involve such patients in
decision making as a way of respecting their autonomy and increasing their participation.
decisions. This is a conscious decision that is made as part patient’s capacity to understand the
inability to make the decision and request for assistance.
In Daly, Bunn, & Goodman (2018) study reported that despite the limited cognitive
ability to make their own decisions, dementia patients value being involved in decision making.
This is based on the UN convention of people with disabilities which requires them to be
involved in different decision-making levels. This study reported the concern of dementia
patients in cases where they were excluded in decision making. This was supported by Hegde &
Ellajosyula (2016) who reported that the participation dementia people participation increases
their quality of life and the decisions that were made. For Daly, Bunn, & Goodman (2018),
assisted decision making is important for cognitively impaired patients which is appreciated by
patients since it heightens self-esteem and reduces depression symptoms to maintain the daily
functioning of the patient. De-Ven, et al. (2017) study concluded that the sharing process needs
to be adapted to highlight the cognitive difficulties that the people face. Thus shared decision
making is reflected in increased capacity for personal obligation, the ability to manage a personal
life and even the participation in social activities.
In these studies, several themes have emerged on whether the patients need to be
involved in decision making or not. One of the themes that have been highlighted is the need for
informed consent through aided support. According to Fields & Calvert (2015), the cognitive
impairment caused by dementia makes most patients lack the full ability to make personal
decisions. This calls for the use of evidence-based approaches in determining the best way to
involve dementia patients. There are existing guidelines on how to involve such patients in
decision making as a way of respecting their autonomy and increasing their participation.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
DEMENTIA AND DECISION MAKING 8
Dunn, Alici, & Roberts (2015) study suggested that issues of patient inclusion have also
raised the issue of surrogate consent which is applies in patients with limited capacity to make
decisions. This allows them to frame the decision making role to honour patient wishes and
values to maintain the quality of life. However, there is a need to understand the vulnerabilities
that these people have which overlap from chronic illness, decision compromise, lack of
adequate infrastructure and clinical services. This creates the functioning challenges that make it
difficult for people to make their own decisions. Issues of ethical dilemmas have always been
pointed out in surrogate consent to highlight the need for promoting patient autonomy by all
means. Xie, et al. (2016) supports assisted decision making by arguing that there is a need to
tailor patient information that is used by the caregiver to make decisions rather than using pre-
researched information. This will enhance the focus on patient values and preferences to increase
the reliability of the decision in relation to the life of the patient. Wilkins (2017) added that the
decision of dementia and surrogate decisions is wide and varies from the long-term to short-term
decisions that have to be made about the patient.
One common theme that cuts across most of the studies is the burden of involving
dementia patients. According to Daly, Bunn, & Goodman (2016), Dunn, Alici, & Roberts (2015)
and Xie, et al. (2016), the cost implications for embedding share decision-making for dementia
people have not been adequately researched. This is because the interdependence of relationships
between the family/carer and the dementia people has not been established especially from the
fact that there is increased dissatisfaction of the patients with the options chosen for them. This is
highlights the need to understand the relationship that these people have with the patient in
achieving patient participation. This means that the family or carers can be enablers or blockers
of shared-decision making. This is all related to communication skills, personality and even
Dunn, Alici, & Roberts (2015) study suggested that issues of patient inclusion have also
raised the issue of surrogate consent which is applies in patients with limited capacity to make
decisions. This allows them to frame the decision making role to honour patient wishes and
values to maintain the quality of life. However, there is a need to understand the vulnerabilities
that these people have which overlap from chronic illness, decision compromise, lack of
adequate infrastructure and clinical services. This creates the functioning challenges that make it
difficult for people to make their own decisions. Issues of ethical dilemmas have always been
pointed out in surrogate consent to highlight the need for promoting patient autonomy by all
means. Xie, et al. (2016) supports assisted decision making by arguing that there is a need to
tailor patient information that is used by the caregiver to make decisions rather than using pre-
researched information. This will enhance the focus on patient values and preferences to increase
the reliability of the decision in relation to the life of the patient. Wilkins (2017) added that the
decision of dementia and surrogate decisions is wide and varies from the long-term to short-term
decisions that have to be made about the patient.
One common theme that cuts across most of the studies is the burden of involving
dementia patients. According to Daly, Bunn, & Goodman (2016), Dunn, Alici, & Roberts (2015)
and Xie, et al. (2016), the cost implications for embedding share decision-making for dementia
people have not been adequately researched. This is because the interdependence of relationships
between the family/carer and the dementia people has not been established especially from the
fact that there is increased dissatisfaction of the patients with the options chosen for them. This is
highlights the need to understand the relationship that these people have with the patient in
achieving patient participation. This means that the family or carers can be enablers or blockers
of shared-decision making. This is all related to communication skills, personality and even
DEMENTIA AND DECISION MAKING 9
routines of the workplace which define the nature of the relationships that the two develop
together.
Despite that, there are cases of patient non-involvement because of several reasons that
clinicians use to justify. Smebye, Kirkevold, & Engedal (2012) study reported that when
dementia progressed, patients develop the incapability of being involved in decision making. As
the condition becomes severe, the patient is left with little or no choices. Lord, Livingston,
Robertson, & Cooper (2016) study reported that in most cases when the condition has become
severe requiring the patient to be under a carer or the need to be assisted in making decisions.
This means that the role of the family and the carer is to reduce the risks that the patient can get
exposed to in case of personal decision making. Barker, Lynch, & Hopkinson (2017) study
reported that patient health is an important factor in influencing patient involvement. This means
that non-involvement can be regarded as the need to improve the life of the patient in high
cognitive impairment.
In addition to that Xie, et al. (2016) recommended that there is need to review the
existing information aids to improve their ability to assist the patient in making the decisions. In
their study, they reported that none of the decision aids that were found used any kind of
technology that reflects the information and communication technologies available in clinical
settings. Since most of the aids were delivered in a static print or audio/video formats, they are
invaluable to patients with unique values or preferences. Thus there is a need to tailor the
information aid interventions to reflect patient requirements. The use of advanced technology
websites or mobile applications can increase the ability of the patients to participate in the
decisisons.
routines of the workplace which define the nature of the relationships that the two develop
together.
Despite that, there are cases of patient non-involvement because of several reasons that
clinicians use to justify. Smebye, Kirkevold, & Engedal (2012) study reported that when
dementia progressed, patients develop the incapability of being involved in decision making. As
the condition becomes severe, the patient is left with little or no choices. Lord, Livingston,
Robertson, & Cooper (2016) study reported that in most cases when the condition has become
severe requiring the patient to be under a carer or the need to be assisted in making decisions.
This means that the role of the family and the carer is to reduce the risks that the patient can get
exposed to in case of personal decision making. Barker, Lynch, & Hopkinson (2017) study
reported that patient health is an important factor in influencing patient involvement. This means
that non-involvement can be regarded as the need to improve the life of the patient in high
cognitive impairment.
In addition to that Xie, et al. (2016) recommended that there is need to review the
existing information aids to improve their ability to assist the patient in making the decisions. In
their study, they reported that none of the decision aids that were found used any kind of
technology that reflects the information and communication technologies available in clinical
settings. Since most of the aids were delivered in a static print or audio/video formats, they are
invaluable to patients with unique values or preferences. Thus there is a need to tailor the
information aid interventions to reflect patient requirements. The use of advanced technology
websites or mobile applications can increase the ability of the patients to participate in the
decisisons.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
DEMENTIA AND DECISION MAKING 10
From the studies, it is evident that patient capacity varies from the stage of dementia.
This means that the healthcare professional needs to assess patient’s decision making capacity.
Despite the need to respect patient autonomy, there are limitations that determine whether the
decision can be made by the carer or not. In decisions that involve daily activities that can cause
no harm to the patient, autonomy. It is also evident that assisted decision making can be biased
and based on family or carer benefits rather than reflecting the needs of the patient. This requires
the use of a framework for negotiation to draw a line between the patient and carer needs. When
patients let the carers to make decisions for them, then it means that the person charged with that
responsibility is supposed to reflect the needs of the patient. Since dementia patients lack the full
cognitive capacity, then shared decision making and assisted decision making to remain
applicable for dementia patients based on their cognitive ability.
From the studies, it is evident that patient capacity varies from the stage of dementia.
This means that the healthcare professional needs to assess patient’s decision making capacity.
Despite the need to respect patient autonomy, there are limitations that determine whether the
decision can be made by the carer or not. In decisions that involve daily activities that can cause
no harm to the patient, autonomy. It is also evident that assisted decision making can be biased
and based on family or carer benefits rather than reflecting the needs of the patient. This requires
the use of a framework for negotiation to draw a line between the patient and carer needs. When
patients let the carers to make decisions for them, then it means that the person charged with that
responsibility is supposed to reflect the needs of the patient. Since dementia patients lack the full
cognitive capacity, then shared decision making and assisted decision making to remain
applicable for dementia patients based on their cognitive ability.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
DEMENTIA AND DECISION MAKING 11
References
Barker, S., Lynch, M., & Hopkinson, J. (2017). Decision making at end of life for people with
dementia by their informal carers: a rapid scoping review. International Journal of
Palliative Nursing, 23(8), 376-388. DOI: 10.12968/ijpn.2017.23.9.446. Retrieved from
https://www.researchgate.net/publication/319971178_Decision_making_for_people_livin
g_with_dementia_by_their_carers_at_the_end_of_life_A_rapid_scoping_review
Daly, R. L., Bunn, F., & Goodman, C. (2018). Shared decision-making for people living with
dementia in extended care settings: a systematic review. BMJ Open, 8(6).
Http://dx.doi.org/10.1136/bmjopen-2017-01897.
De-Ven, L. G.-v., Smits, C., Graaff, F. d., Span, M., Eefsting, J., Jukema, J., & Vernooij-Dassen,
M. (2017). Involvement of people with dementia in making decisions about their lives: a
qualitative study that appraises shared decision-making concerning daycare. BMJ Open,
7(11). Doi. http://dx.doi.org/10.1136/bmjopen-2017-018337
Dunn, L. B., Alici, Y., & Roberts, L. W. (2015). Ethical Challenges in the Treatment of
Cognitive Impairment in Aging. Current Behavioral Neuroscience Reports, 2(4), 226–
233. DOI 10.1007/s40473-015-0055-0. Retrieved from
https://link.springer.com/content/pdf/10.1007%2Fs40473-015-0055-0.pdf
Fields, L. M., & Calvert, J. D. (2015). Informed consent procedures with cognitively impaired
patients: A review of ethics and best practices. Psychiatry and Clinical Neurosciences,
69, 462–471. doi:10.1111/pcn.12289. Retrieved from
https://onlinelibrary.wiley.com/doi/pdf/10.1111/pcn.12289
Hegde, S., & Ellajosyula, R. (2016). Capacity issues and decision-making in dementia. Annals
Indian Academy of Neurology, 19(1), 34-39. doi: 10.4103/0972-2327.192890. Retrieved
References
Barker, S., Lynch, M., & Hopkinson, J. (2017). Decision making at end of life for people with
dementia by their informal carers: a rapid scoping review. International Journal of
Palliative Nursing, 23(8), 376-388. DOI: 10.12968/ijpn.2017.23.9.446. Retrieved from
https://www.researchgate.net/publication/319971178_Decision_making_for_people_livin
g_with_dementia_by_their_carers_at_the_end_of_life_A_rapid_scoping_review
Daly, R. L., Bunn, F., & Goodman, C. (2018). Shared decision-making for people living with
dementia in extended care settings: a systematic review. BMJ Open, 8(6).
Http://dx.doi.org/10.1136/bmjopen-2017-01897.
De-Ven, L. G.-v., Smits, C., Graaff, F. d., Span, M., Eefsting, J., Jukema, J., & Vernooij-Dassen,
M. (2017). Involvement of people with dementia in making decisions about their lives: a
qualitative study that appraises shared decision-making concerning daycare. BMJ Open,
7(11). Doi. http://dx.doi.org/10.1136/bmjopen-2017-018337
Dunn, L. B., Alici, Y., & Roberts, L. W. (2015). Ethical Challenges in the Treatment of
Cognitive Impairment in Aging. Current Behavioral Neuroscience Reports, 2(4), 226–
233. DOI 10.1007/s40473-015-0055-0. Retrieved from
https://link.springer.com/content/pdf/10.1007%2Fs40473-015-0055-0.pdf
Fields, L. M., & Calvert, J. D. (2015). Informed consent procedures with cognitively impaired
patients: A review of ethics and best practices. Psychiatry and Clinical Neurosciences,
69, 462–471. doi:10.1111/pcn.12289. Retrieved from
https://onlinelibrary.wiley.com/doi/pdf/10.1111/pcn.12289
Hegde, S., & Ellajosyula, R. (2016). Capacity issues and decision-making in dementia. Annals
Indian Academy of Neurology, 19(1), 34-39. doi: 10.4103/0972-2327.192890. Retrieved
DEMENTIA AND DECISION MAKING 12
from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5109759/
Lord, K., Livingston, G., Robertson, S., & Cooper, C. (2016). How people with dementia and
their families decide about moving to a care home and support their needs: development
of a decision aid, a qualitative study. BMC Geriatrics, 68. DOI 10.1186/s12877-016-
0242-1. Retrieved from https://bmcgeriatr.biomedcentral.com/track/pdf/10.1186/s12877-
016-0242-1
Smebye, K. L., Kirkevold, M., & Engedal, K. (2012). How do persons with dementia participate
in decision making related to health and daily care? A multi-case study. BMC Health
Services Research, 12(241). Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475075/pdf/1472-6963-12-241.pdf
Wilkins, J. M. (2017). Dementia, Decision Making, and Quality of Life. AMA Journal of Ethics,
19(7), 637-639. Retrieved from
https://journalofethics.ama-assn.org/sites/journalofethics.ama-assn.org/files/2018-04/
fred1-1707.pdf
Xie, B., Berkley, A. S., Kwak, J., Fleischmann, K. R., Champion, J. D., & Kolta, K. S. (2016).
End-of-life decision making by family caregivers of persons with advanced dementia: A
literature review of decision aids. SAGE Open Medicine, 6.
https://doi.org/10.1177/2050312118777517. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5966844/pdf/10.1177_2050312118777517.pdf
from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5109759/
Lord, K., Livingston, G., Robertson, S., & Cooper, C. (2016). How people with dementia and
their families decide about moving to a care home and support their needs: development
of a decision aid, a qualitative study. BMC Geriatrics, 68. DOI 10.1186/s12877-016-
0242-1. Retrieved from https://bmcgeriatr.biomedcentral.com/track/pdf/10.1186/s12877-
016-0242-1
Smebye, K. L., Kirkevold, M., & Engedal, K. (2012). How do persons with dementia participate
in decision making related to health and daily care? A multi-case study. BMC Health
Services Research, 12(241). Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475075/pdf/1472-6963-12-241.pdf
Wilkins, J. M. (2017). Dementia, Decision Making, and Quality of Life. AMA Journal of Ethics,
19(7), 637-639. Retrieved from
https://journalofethics.ama-assn.org/sites/journalofethics.ama-assn.org/files/2018-04/
fred1-1707.pdf
Xie, B., Berkley, A. S., Kwak, J., Fleischmann, K. R., Champion, J. D., & Kolta, K. S. (2016).
End-of-life decision making by family caregivers of persons with advanced dementia: A
literature review of decision aids. SAGE Open Medicine, 6.
https://doi.org/10.1177/2050312118777517. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5966844/pdf/10.1177_2050312118777517.pdf
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





