Master of Science in Dementia Care: Light Therapy & Sleep Review
VerifiedAdded on 2023/06/11
|23
|5870
|463
Literature Review
AI Summary
This paper presents a systematic literature review investigating the effectiveness of light therapy in improving sleep quality among dementia patients. The review addresses the increasing prevalence of sleep disturbances in dementia and their negative impact on patients' quality of life and caregiver burden. The methodology involved a systematic search of databases like CINAHL Plus, MEDLINE Plus, Cochrane Library, and PubMed, guided by PRISMA checklist. The review included studies published between 2010 and 2017 that assessed light therapy as an intervention for dementia patients with sleep disturbances. The results of the review are discussed in relation to the existing literature, highlighting the potential benefits and limitations of light therapy for improving sleep duration and reducing nocturnal awakenings. The review concludes by emphasizing the need for further research to address the identified limitations and to inform future practice in dementia care, with a focus on non-pharmacological interventions for sleep management.

Running head: MASTER OF SCIENCE IN DEMENTIA CARE
Master of Science in dementia care
Name of the student:
Name of the University:
Author’s note
Master of Science in dementia care
Name of the student:
Name of the University:
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MASTER OF SCIENCE IN DEMENTIA CARE
Table of Contents
Introduction......................................................................................................................................1
Background and literature................................................................................................................2
Rationale of the present review.......................................................................................................5
Objective..........................................................................................................................................6
Methodology:...................................................................................................................................6
Results:..........................................................................................................................................10
Discussion:.....................................................................................................................................15
Conclusion:....................................................................................................................................17
Table of Contents
Introduction......................................................................................................................................1
Background and literature................................................................................................................2
Rationale of the present review.......................................................................................................5
Objective..........................................................................................................................................6
Methodology:...................................................................................................................................6
Results:..........................................................................................................................................10
Discussion:.....................................................................................................................................15
Conclusion:....................................................................................................................................17
2MASTER OF SCIENCE IN DEMENTIA CARE
Introduction
Dementia patients are at increased risk of suffering from circadian and sleep disturbances
that gradually get worse with age. Sleep disturbances have a direct negative impact in the quality
of life of the patients, also contributing to caregiver burden. Disrupted sleep has been linked with
increased confusion, agitation, increased risk of injury and falls. Given the impact of sleep
disturbances in patients, it is important to understand different interventional strategies that can
have a positive impact on the patient in relation to sleep quality and contribute to better quality
of life in patients. Light therapy has been indicated to be a potential non-pharmacological tool
that can improve sleep efficacy and consolidation. A systematic literature review was therefore
conducted that aimed at assessing the effectiveness of therapy in improving sleep quality in
dementia patients. The results of the project are presented in the present report. Such a review
summarizes the main results of the healthcare studies and provides evidence level on the
usefulness of the intervention. Recommendations are outlined on the basis of the results that
inform future practice.
The first section of the paper provides the background to the study along with a brief
literature review on the research topic. This section covers the problem being addressed,
previous research on the same topic, the shortcomings and problems of the research, the rationale
for the present study and the study objectives. The next section of the paper provides the details
of the project undertaken. The steps and methods undertaken for completing the project are
mentioned. The outcomes of the project are then highlighted. The following section is a
Introduction
Dementia patients are at increased risk of suffering from circadian and sleep disturbances
that gradually get worse with age. Sleep disturbances have a direct negative impact in the quality
of life of the patients, also contributing to caregiver burden. Disrupted sleep has been linked with
increased confusion, agitation, increased risk of injury and falls. Given the impact of sleep
disturbances in patients, it is important to understand different interventional strategies that can
have a positive impact on the patient in relation to sleep quality and contribute to better quality
of life in patients. Light therapy has been indicated to be a potential non-pharmacological tool
that can improve sleep efficacy and consolidation. A systematic literature review was therefore
conducted that aimed at assessing the effectiveness of therapy in improving sleep quality in
dementia patients. The results of the project are presented in the present report. Such a review
summarizes the main results of the healthcare studies and provides evidence level on the
usefulness of the intervention. Recommendations are outlined on the basis of the results that
inform future practice.
The first section of the paper provides the background to the study along with a brief
literature review on the research topic. This section covers the problem being addressed,
previous research on the same topic, the shortcomings and problems of the research, the rationale
for the present study and the study objectives. The next section of the paper provides the details
of the project undertaken. The steps and methods undertaken for completing the project are
mentioned. The outcomes of the project are then highlighted. The following section is a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3MASTER OF SCIENCE IN DEMENTIA CARE
discussion of the overall project including project limitations and barriers and recommendations.
A summary is provided to draw together the previous sections of the project. A logical
conclusion brings in end to the report.
Background and literature
Dementia is the umbrella term encompassing varied conditions affecting thinking,
memory, behavior and ability to carry out daily activities of life in patients suffering from it.
Patients with dementia experience impairments in social and occupational functioning and
present distinct behavioral disturbances. Though dementia is common in adults, it is not an
inevitable part of the normal aging process. The most frequently occurring forms of dementia are
Alzheimer’s disease, vascular dementia, dementia with Lewy body, frontotemporal dementia and
mixed dementia. Rather than being considered as a subject for active attention dementia is often
ignored in terms of care provision. It is a leading cause of dependency and disability among
older patients (Harvey et al. 2018). Dementia is one of the leading causes of death in Australia.
As per the reports of Laver et al. (2016) dementia was the fourth most common cause of death in
Australia in the year 2011. Dementia accounted for 6 per cent of all deaths in the same year. It is
also to be noted that patients suffering from dementia are also at increased risk of dying due to
other illnesses. According to Nay et al. (2015) dementia brings about significant implications for
patient’s families, care givers and health care professionals. For them, dementia imposes stress
and economic burden.
Sleep disturbances are commonly found among dementia patients as a neurobehavioral
symptom, leading to negative impact on the daytime functioning of the patient. In addition, the
wellbeing of the caregiver is also directly influenced by the sleep pattern of the patients. The risk
discussion of the overall project including project limitations and barriers and recommendations.
A summary is provided to draw together the previous sections of the project. A logical
conclusion brings in end to the report.
Background and literature
Dementia is the umbrella term encompassing varied conditions affecting thinking,
memory, behavior and ability to carry out daily activities of life in patients suffering from it.
Patients with dementia experience impairments in social and occupational functioning and
present distinct behavioral disturbances. Though dementia is common in adults, it is not an
inevitable part of the normal aging process. The most frequently occurring forms of dementia are
Alzheimer’s disease, vascular dementia, dementia with Lewy body, frontotemporal dementia and
mixed dementia. Rather than being considered as a subject for active attention dementia is often
ignored in terms of care provision. It is a leading cause of dependency and disability among
older patients (Harvey et al. 2018). Dementia is one of the leading causes of death in Australia.
As per the reports of Laver et al. (2016) dementia was the fourth most common cause of death in
Australia in the year 2011. Dementia accounted for 6 per cent of all deaths in the same year. It is
also to be noted that patients suffering from dementia are also at increased risk of dying due to
other illnesses. According to Nay et al. (2015) dementia brings about significant implications for
patient’s families, care givers and health care professionals. For them, dementia imposes stress
and economic burden.
Sleep disturbances are commonly found among dementia patients as a neurobehavioral
symptom, leading to negative impact on the daytime functioning of the patient. In addition, the
wellbeing of the caregiver is also directly influenced by the sleep pattern of the patients. The risk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4MASTER OF SCIENCE IN DEMENTIA CARE
of falling asleep at the daytime and increased wakefulness at night contributes to such concerns.
Behavioral challenges arise in the form of agitation, arguments, violence, wandering and
increased falls (Wilfing 2015). Though risk of falling is an indirect impact, it holds much
significance since patient falls further bring in decline to the patient condition and add to the
burden on the care giver. Recovery of such dementia patients is challenging and takes more time
as compared to patients not suffering from dementia. Research highlights that the driving factors
for sleep disturbances are lack of social support, reduced circadian rhythm, eye problems as a
result of age, and limited exposure to sunlight (Sekiguchi, Iritani & Fujita 2017). Patients with
dementia spend 40% of their night time being awake and a considerable portion of the day
asleep.
As highlighted by Spira et al. (2014), the availability of dementia care together with
respite services is crucial for the maintenance of quality of life of patients that focuses on both
physical and mental health status. Recent and advanced treatment options have been continually
assessed for understanding whether they are capable of slowing the course of cognitive decline
and other health concerns. The primary aim is to enhance the quality of life of patients and
decrease the costs of institutional care. Despite growing research on the potential psychological
and pharmacological interventions across countries, their application to real life settings are
limited.
According to Ploeg and O'Connor (2014) normal circadian rhythm works by
synchronizing with the 24-hourcycle and it has been found that light is elementary for
maintaining this rhythm. Maintenance of normal circadian rhythm is supported when there is an
active exposure to 24-hour light/dark cycle. For elder dementia patients, the need of light
exposure is more for maintaining normal circadian rhythm. However, in patients who are
of falling asleep at the daytime and increased wakefulness at night contributes to such concerns.
Behavioral challenges arise in the form of agitation, arguments, violence, wandering and
increased falls (Wilfing 2015). Though risk of falling is an indirect impact, it holds much
significance since patient falls further bring in decline to the patient condition and add to the
burden on the care giver. Recovery of such dementia patients is challenging and takes more time
as compared to patients not suffering from dementia. Research highlights that the driving factors
for sleep disturbances are lack of social support, reduced circadian rhythm, eye problems as a
result of age, and limited exposure to sunlight (Sekiguchi, Iritani & Fujita 2017). Patients with
dementia spend 40% of their night time being awake and a considerable portion of the day
asleep.
As highlighted by Spira et al. (2014), the availability of dementia care together with
respite services is crucial for the maintenance of quality of life of patients that focuses on both
physical and mental health status. Recent and advanced treatment options have been continually
assessed for understanding whether they are capable of slowing the course of cognitive decline
and other health concerns. The primary aim is to enhance the quality of life of patients and
decrease the costs of institutional care. Despite growing research on the potential psychological
and pharmacological interventions across countries, their application to real life settings are
limited.
According to Ploeg and O'Connor (2014) normal circadian rhythm works by
synchronizing with the 24-hourcycle and it has been found that light is elementary for
maintaining this rhythm. Maintenance of normal circadian rhythm is supported when there is an
active exposure to 24-hour light/dark cycle. For elder dementia patients, the need of light
exposure is more for maintaining normal circadian rhythm. However, in patients who are
5MASTER OF SCIENCE IN DEMENTIA CARE
institutionalized, the scope of being exposed to sunlight is minimal. A rich pool of studies has
established the positive impact of bright light in dementia patients. Nevertheless, the outcomes of
the studies are not similar. The main findings of the paper indicate improved mood and sleep
patterns among patients (Most, Scheltens & Van Someren 2010).
The researchers brought into limelight how light therapy might work for dementia
patients. The hypothalamic suprachiasmatic nucleus (SCN) has the function of being a circadian
pacemaker. This implied that there is a synchronization with the day and night cycle through
light. This synchronization is to be perceived as extremely sensitive. For dementia patients, there
is a considerable reduction in SCN since the activity and sensitivity is reduced. The ultimate
outcome is disturbed sleep patterns due to severe disruption in sleep. Such disturbances are
rerated to loss of vasopressin in SCN. Thus, exposure to light on a regular basis helps in
reactivating the SCN and stabilizing the 24-hour light dark cycle. The intervention has been
widely assessed for its benefits and effectiveness in dementia patients, mainly those who reside
in care facilities. The researchers highlighted how lighting characteristics affect circadian
rhythms. The neural machinery in the mammalian retina provides light information to both
the visual and circadian system. The quantity of polychromatic light required for activating
the circadian system is at least two orders of magnitude more than the amount that activates
the visual system. The circadian system is dependent on the timing of light exposure. The
higher exposure to light at the time of day the lower is the sensitivity of the circadian system to
light. Light information is known to travel from the retina to the SCN through the
retinohypothalamic tract (RHT). When there are considerable disturbances in the circadian
rhythms, older adults undergo poor sleeping pattern as the pathway is dysfunctional, leading
institutionalized, the scope of being exposed to sunlight is minimal. A rich pool of studies has
established the positive impact of bright light in dementia patients. Nevertheless, the outcomes of
the studies are not similar. The main findings of the paper indicate improved mood and sleep
patterns among patients (Most, Scheltens & Van Someren 2010).
The researchers brought into limelight how light therapy might work for dementia
patients. The hypothalamic suprachiasmatic nucleus (SCN) has the function of being a circadian
pacemaker. This implied that there is a synchronization with the day and night cycle through
light. This synchronization is to be perceived as extremely sensitive. For dementia patients, there
is a considerable reduction in SCN since the activity and sensitivity is reduced. The ultimate
outcome is disturbed sleep patterns due to severe disruption in sleep. Such disturbances are
rerated to loss of vasopressin in SCN. Thus, exposure to light on a regular basis helps in
reactivating the SCN and stabilizing the 24-hour light dark cycle. The intervention has been
widely assessed for its benefits and effectiveness in dementia patients, mainly those who reside
in care facilities. The researchers highlighted how lighting characteristics affect circadian
rhythms. The neural machinery in the mammalian retina provides light information to both
the visual and circadian system. The quantity of polychromatic light required for activating
the circadian system is at least two orders of magnitude more than the amount that activates
the visual system. The circadian system is dependent on the timing of light exposure. The
higher exposure to light at the time of day the lower is the sensitivity of the circadian system to
light. Light information is known to travel from the retina to the SCN through the
retinohypothalamic tract (RHT). When there are considerable disturbances in the circadian
rhythms, older adults undergo poor sleeping pattern as the pathway is dysfunctional, leading
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MASTER OF SCIENCE IN DEMENTIA CARE
to poor processing of light information, marked by low fidelity (Most, Scheltens & Van
Someren 2010).
.
Rationale of the present review
The importance of dementia care giving has been reported by healthcare professionals
across settings, who mainly point out the challenges faced in delivering care. Caregivers are
often subjected to increased amount of stress and physical exhaustion as a result of addressing
the varied needs of the patients. The strength of healthcare workforce caring for dementia
patients in Australia is noteworthy. Understanding the concerns faced by dementia caregivers is
therefore of prime importance.
Admission to care facilities as a result of sleep disturbance among dementia patients is
noted. This indicates that effective interventions are to be found out that can address sleep
disturbances and enhance quality of life. A number of studies have been undertaken in this
regard across different countries. However, there have been distinct limitations in such studies
(Forbes 2014). This is mainly attributed to the methodology used in such studies and limited
generalisability. Researchers have identified bias in those studies due to inclusion and exclusion
criteria. Primary studies on understanding effect of light exposure on dementia patients are
limited (Wilfling 2015). An urgent need of identify research literaturewith accurate methodology
in this respect forms the rationale for the present paper.
to poor processing of light information, marked by low fidelity (Most, Scheltens & Van
Someren 2010).
.
Rationale of the present review
The importance of dementia care giving has been reported by healthcare professionals
across settings, who mainly point out the challenges faced in delivering care. Caregivers are
often subjected to increased amount of stress and physical exhaustion as a result of addressing
the varied needs of the patients. The strength of healthcare workforce caring for dementia
patients in Australia is noteworthy. Understanding the concerns faced by dementia caregivers is
therefore of prime importance.
Admission to care facilities as a result of sleep disturbance among dementia patients is
noted. This indicates that effective interventions are to be found out that can address sleep
disturbances and enhance quality of life. A number of studies have been undertaken in this
regard across different countries. However, there have been distinct limitations in such studies
(Forbes 2014). This is mainly attributed to the methodology used in such studies and limited
generalisability. Researchers have identified bias in those studies due to inclusion and exclusion
criteria. Primary studies on understanding effect of light exposure on dementia patients are
limited (Wilfling 2015). An urgent need of identify research literaturewith accurate methodology
in this respect forms the rationale for the present paper.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MASTER OF SCIENCE IN DEMENTIA CARE
Objective
The present systematic review had the objective of understanding the effectiveness of
light therapy in improving sleep quality among dementia patients. The research question
addressed was-
‘Is light therapy effective in improving sleep quality (duration of sleep) among the dementia
patients?”
Methodology:
Research design: Systematic review method guided by PRISMA checklist has been used as the
research design for the study. The PRISMA checklist is an appropriate framework that covers
items to be covered while writing a systematic review (Moher et al. 2015). Specific inclusion and
exclusion criteria guided the search process and relevant electronic databases were the main
resource to search for articles.
Inclusion and exclusion criteria:
The inclusion criteria for selection of articles are as follows:
Study design: As the main purpose of systematic review is to determine effectiveness of
light therapy in improving sleep quality among dementia patients, all primary research
articles based on qualitative and quantitative approach were included in the review.
Study participants: Those research articles were taken which had dementia patients
(such as people with vascular dementia, Lewy body dementia, Alzheimer’s disease and
frontotemporal dementia) as the participants for the study. Studies done with dementia
patient were included irrespective of severity of the condition.
Objective
The present systematic review had the objective of understanding the effectiveness of
light therapy in improving sleep quality among dementia patients. The research question
addressed was-
‘Is light therapy effective in improving sleep quality (duration of sleep) among the dementia
patients?”
Methodology:
Research design: Systematic review method guided by PRISMA checklist has been used as the
research design for the study. The PRISMA checklist is an appropriate framework that covers
items to be covered while writing a systematic review (Moher et al. 2015). Specific inclusion and
exclusion criteria guided the search process and relevant electronic databases were the main
resource to search for articles.
Inclusion and exclusion criteria:
The inclusion criteria for selection of articles are as follows:
Study design: As the main purpose of systematic review is to determine effectiveness of
light therapy in improving sleep quality among dementia patients, all primary research
articles based on qualitative and quantitative approach were included in the review.
Study participants: Those research articles were taken which had dementia patients
(such as people with vascular dementia, Lewy body dementia, Alzheimer’s disease and
frontotemporal dementia) as the participants for the study. Studies done with dementia
patient were included irrespective of severity of the condition.
8MASTER OF SCIENCE IN DEMENTIA CARE
Date of publication: Studies published within 7 years (from 2010 to 2017) were taken
for the review.
Type of intervention: For all selected research articles, light therapy should be used as
intervention for research. Studies with combination intervention such as light therapy
along with pharmacological interventions or artificial light were also included in the
review.
Research question: All research studies must address the research question for the study
and should have similar research objective.
Outcome variable: The main outcome variable for the study should include variables
that give indication about sleep quality and sleep efficiency such as duration of sleep,
nocturnal sleep time and number of night awakenings.
Language: Included research articles must be published in English language.
Search strategy:
Relevant articles related to the research questions were reviewed from online databases
like CINAHL Plus, MEDLINE Plus, Cochrane Library and PubMed. Google scholar was also
used as a search engine to identify additional articles relevant to the research question. Advanced
search for additional articles were also done from UOW online library. The search process by
refined by setting filters by choosing peer-reviewed full-text journal articles and using date filter
The research publication was limited to those published within 2010-2017 by modifying date
filter. The inclusion and exclusion criteria were applied to narrow down the search process.
Date of publication: Studies published within 7 years (from 2010 to 2017) were taken
for the review.
Type of intervention: For all selected research articles, light therapy should be used as
intervention for research. Studies with combination intervention such as light therapy
along with pharmacological interventions or artificial light were also included in the
review.
Research question: All research studies must address the research question for the study
and should have similar research objective.
Outcome variable: The main outcome variable for the study should include variables
that give indication about sleep quality and sleep efficiency such as duration of sleep,
nocturnal sleep time and number of night awakenings.
Language: Included research articles must be published in English language.
Search strategy:
Relevant articles related to the research questions were reviewed from online databases
like CINAHL Plus, MEDLINE Plus, Cochrane Library and PubMed. Google scholar was also
used as a search engine to identify additional articles relevant to the research question. Advanced
search for additional articles were also done from UOW online library. The search process by
refined by setting filters by choosing peer-reviewed full-text journal articles and using date filter
The research publication was limited to those published within 2010-2017 by modifying date
filter. The inclusion and exclusion criteria were applied to narrow down the search process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MASTER OF SCIENCE IN DEMENTIA CARE
The primary search terms for selection of articles included dementia, light therapy, sleep
disturbance/disorder, interventions, Alzheimer’s disease, morning light, cognitive impairment.
Boolean operators like AND or OR was also used to combine terms similar in meaning.
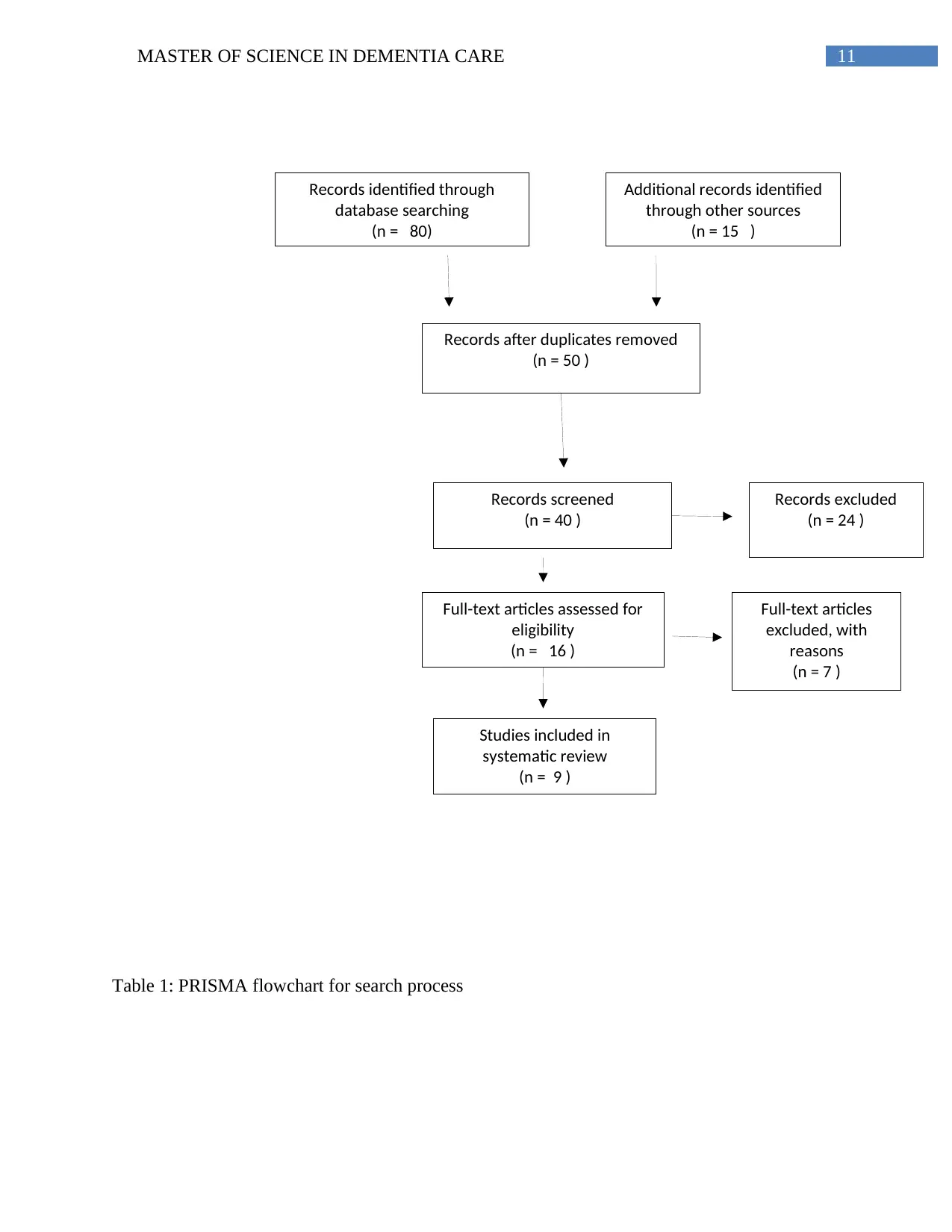
Data abstraction: A PRISMA flow diagram was used to summarize the research process and
number of articles included or excluded for the review. The PRISMA flow diagram can give idea
about number of articles identified from database search, articles screened by title and abstract
and number of final articles included for the studies (Booth, Sutton and Papaioannou 2016).
After final selection of articles for the review, all the articles were extracted by making a table on
author, year of publication, details of intervention, study finding and implications of research.
Use of specific method to extract data is necessary as it helps in better interpretation of
systematic review results and provides good overview about the contribution of each included
studies in addressing the research question (Jonnalagadda, Goyal and Huffman 2015).
Data analysis: The analysis of research articles were done first by the reviewing title and
abstract of journal articles. The data analysis process was done by two reviewers to maintain
reliability of study and prevent influence of selection bias on study outcome. This approach also
eliminated sources of bias. After the selection of research articles based on review of title and
abstract, the second phase of analysis included review of full text article to collect findings
related to the effect of intervention, strength of methodology and application of study findings.
The reference list of articles was also reviewed to find other articles that address the research
question. Article which does not met inclusion criteria were excluded during the first phase of
data analysis.
The primary search terms for selection of articles included dementia, light therapy, sleep
disturbance/disorder, interventions, Alzheimer’s disease, morning light, cognitive impairment.
Boolean operators like AND or OR was also used to combine terms similar in meaning.
Data abstraction: A PRISMA flow diagram was used to summarize the research process and
number of articles included or excluded for the review. The PRISMA flow diagram can give idea
about number of articles identified from database search, articles screened by title and abstract
and number of final articles included for the studies (Booth, Sutton and Papaioannou 2016).
After final selection of articles for the review, all the articles were extracted by making a table on
author, year of publication, details of intervention, study finding and implications of research.
Use of specific method to extract data is necessary as it helps in better interpretation of
systematic review results and provides good overview about the contribution of each included
studies in addressing the research question (Jonnalagadda, Goyal and Huffman 2015).
Data analysis: The analysis of research articles were done first by the reviewing title and
abstract of journal articles. The data analysis process was done by two reviewers to maintain
reliability of study and prevent influence of selection bias on study outcome. This approach also
eliminated sources of bias. After the selection of research articles based on review of title and
abstract, the second phase of analysis included review of full text article to collect findings
related to the effect of intervention, strength of methodology and application of study findings.
The reference list of articles was also reviewed to find other articles that address the research
question. Article which does not met inclusion criteria were excluded during the first phase of
data analysis.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10MASTER OF SCIENCE IN DEMENTIA CARE
Appraisal of research articles: The appraisal of the research article was done by the use of
Cochrane Risk of Bias Assessment tool. The advantage of the tool is that help to identify
methodological rigour in the study by identifying risk of different kinds of bias in studies. The
tool helps to categorize research articles on the basis of selection bias, performance bias,
detection bias, attrition bias and reporting bias. It covers six domains to give an overview about
types of bias observed in studies. This includes random sequence generation, blinding
participants, blinding of outcome analysis, incomplete outcome data, selective reporting and
other source of bias. The advantage of using relevant and evidence based quality assessment tool
in systematic review is that it supports research to assess the validity and credibility of research
based on methodological rigour and complete reporting of study findings (Ahmed, Sutton and
Riley, 2012).
The research findings have presented in the form of thematic analysis and reporting of the
review is in relevance with the PRISMA guideline. The advantage of using thematic analysis in
systematic review is that it helps to integrate the findings of multiple studies. Thematic synthesis
is done by the development of descriptive themes and analytical themes. The descriptive themes
gives clear idea about findings of the primary research studies and the analytical themes lead to
generation of new interpretive constructs and hypotheses.
Results:
The initial search process in different databases after entering search terms returned 80
studies for analysis. However, after removal of duplicate, 50 articles were screened for suitability
on the basis of inclusion and exclusion criteria. The summary of the search process and the final
number of articles obtained for systematic has been provided in Flowchart below.
Appraisal of research articles: The appraisal of the research article was done by the use of
Cochrane Risk of Bias Assessment tool. The advantage of the tool is that help to identify
methodological rigour in the study by identifying risk of different kinds of bias in studies. The
tool helps to categorize research articles on the basis of selection bias, performance bias,
detection bias, attrition bias and reporting bias. It covers six domains to give an overview about
types of bias observed in studies. This includes random sequence generation, blinding
participants, blinding of outcome analysis, incomplete outcome data, selective reporting and
other source of bias. The advantage of using relevant and evidence based quality assessment tool
in systematic review is that it supports research to assess the validity and credibility of research
based on methodological rigour and complete reporting of study findings (Ahmed, Sutton and
Riley, 2012).
The research findings have presented in the form of thematic analysis and reporting of the
review is in relevance with the PRISMA guideline. The advantage of using thematic analysis in
systematic review is that it helps to integrate the findings of multiple studies. Thematic synthesis
is done by the development of descriptive themes and analytical themes. The descriptive themes
gives clear idea about findings of the primary research studies and the analytical themes lead to
generation of new interpretive constructs and hypotheses.
Results:
The initial search process in different databases after entering search terms returned 80
studies for analysis. However, after removal of duplicate, 50 articles were screened for suitability
on the basis of inclusion and exclusion criteria. The summary of the search process and the final
number of articles obtained for systematic has been provided in Flowchart below.
11MASTER OF SCIENCE IN DEMENTIA CARE
Records identified through
database searching
(n = 80)
Additional records identified
through other sources
(n = 15 )
Records after duplicates removed
(n = 50 )
Records screened
(n = 40 )
Records excluded
(n = 24 )
Full-text articles assessed for
eligibility
(n = 16 )
Studies included in
systematic review
(n = 9 )
Full-text articles
excluded, with
reasons
(n = 7 )
Table 1: PRISMA flowchart for search process
Records identified through
database searching
(n = 80)
Additional records identified
through other sources
(n = 15 )
Records after duplicates removed
(n = 50 )
Records screened
(n = 40 )
Records excluded
(n = 24 )
Full-text articles assessed for
eligibility
(n = 16 )
Studies included in
systematic review
(n = 9 )
Full-text articles
excluded, with
reasons
(n = 7 )
Table 1: PRISMA flowchart for search process
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




