Diabetes Wound Care and Treatment: A Report on Biofilm and Ulcers
VerifiedAdded on 2021/04/24
|15
|3567
|69
Report
AI Summary
This report investigates diabetes wound care, specifically addressing the challenges posed by diabetic foot ulcers (DFUs). It begins with an introduction to wound healing, the impact of diabetes on this process, and the associated risks of infection and delayed healing. The problem statement highlights the need for early detection of DFU complications, particularly focusing on the presence of biofilm as a potential precursor to infection. The research objectives aim to explore the utility of biofilm detection for early intervention and to evaluate effective treatment strategies. A literature review examines biofilm formation, its characteristics, and its impact on wound healing, as well as the pathogenesis of DFUs, including neuropathy, poor circulation, and elevated plantar pressures. The review also explores various treatment approaches, such as chitosan-based dressings, growth factors, and debridement techniques. The report outlines a research design and methodology, including a study involving diabetes patients with DFUs, utilizing gram staining, microscopy, and treatment with chitosan, growth factors, and debridement. Ethical considerations are also addressed. The study aims to determine if early detection of biofilm and prompt treatment can improve wound healing and reduce morbidity and mortality in diabetic patients.

Running head: Diabetes Wound Care and Treatment
Diabetes Wound Care and Treatment
Name of the Student
Name of the University
Author Note
Diabetes Wound Care and Treatment
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Diabetes wound care and treatment
Contents
Introduction:...............................................................................................................................2
Problem Statement:....................................................................................................................2
Research Objectives/Questions:.................................................................................................3
Literature Review:......................................................................................................................3
Biofilms:.................................................................................................................................3
Diabetic Foot Ulcer DFU:......................................................................................................5
Research Design and Methodology:..........................................................................................7
Ethical Considerations:..............................................................................................................9
Conclusion:................................................................................................................................9
Contents
Introduction:...............................................................................................................................2
Problem Statement:....................................................................................................................2
Research Objectives/Questions:.................................................................................................3
Literature Review:......................................................................................................................3
Biofilms:.................................................................................................................................3
Diabetic Foot Ulcer DFU:......................................................................................................5
Research Design and Methodology:..........................................................................................7
Ethical Considerations:..............................................................................................................9
Conclusion:................................................................................................................................9
2Diabetes wound care and treatment
Introduction:
Wound is any type of injury sustained on a living tissue due to a blow, cut or impact,
resulting in cuts or breakage of the skin. Minor wounds can naturally heal over time, however
for people suffering with diabetes, the wound can take a several weeks to heal, and often can
get infected. The normal wound healing process occurs in three stages, in the first stage an
immune reaction causes inflammation in the wound to prevent infection, in the second stage,
new cells are formed over the wound forming scab and in final stage a scar tissue develops
healing the wound. The wound healing process can get delayed or complicated because of
different health issues like: diabetes mellitus, rheumatoid arthritis, low levels of Human
Growth Hormone, Vascular disease and zinc deficiency. Each of these factors affects the
healing of wound differently. In diabetes, high levels of blood glucose can cause neuropathy
(damage to nerves) and reduces blood circulation, thereby preventing blood to reach the
areas affected by wounds or sores, thus affecting the normal healing process. Unhealed
wounds further increases risk of infections (fungal or bacterial) and even gangrene
(Ha.org.hk 2018; Mousley 2018).
Problem Statement:
Foot ulcers in diabetes care caused due to neuropathy, reduced blood circulation and
elevated plantar pressures, higher chances of morbidity, loss of limb and even mortality
(Kavitha et al. 2014). This highlights the necessity of early identification of the condition to
prevent its associated risks. Studies by Hurlow et al. (2015) have suggested that the evidence
of biofilm’s presence on slow healing wounds can be a precursor of an infection.
Furthermore, biofim can have adverse effects on key healing processes like the
inflammatory response of immune system, formation of granular tissue and epithelialization
Introduction:
Wound is any type of injury sustained on a living tissue due to a blow, cut or impact,
resulting in cuts or breakage of the skin. Minor wounds can naturally heal over time, however
for people suffering with diabetes, the wound can take a several weeks to heal, and often can
get infected. The normal wound healing process occurs in three stages, in the first stage an
immune reaction causes inflammation in the wound to prevent infection, in the second stage,
new cells are formed over the wound forming scab and in final stage a scar tissue develops
healing the wound. The wound healing process can get delayed or complicated because of
different health issues like: diabetes mellitus, rheumatoid arthritis, low levels of Human
Growth Hormone, Vascular disease and zinc deficiency. Each of these factors affects the
healing of wound differently. In diabetes, high levels of blood glucose can cause neuropathy
(damage to nerves) and reduces blood circulation, thereby preventing blood to reach the
areas affected by wounds or sores, thus affecting the normal healing process. Unhealed
wounds further increases risk of infections (fungal or bacterial) and even gangrene
(Ha.org.hk 2018; Mousley 2018).
Problem Statement:
Foot ulcers in diabetes care caused due to neuropathy, reduced blood circulation and
elevated plantar pressures, higher chances of morbidity, loss of limb and even mortality
(Kavitha et al. 2014). This highlights the necessity of early identification of the condition to
prevent its associated risks. Studies by Hurlow et al. (2015) have suggested that the evidence
of biofilm’s presence on slow healing wounds can be a precursor of an infection.
Furthermore, biofim can have adverse effects on key healing processes like the
inflammatory response of immune system, formation of granular tissue and epithelialization
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Diabetes wound care and treatment
(Seth et al. 2012). This poses an important question “can biofilm be useful in the early
detection of infection in diabetic foot ulcers?”
Research Objectives/Questions:
The objective of the research is to study whether presence of biofilm can be used for
early slow healing foot ulcers in diabetic patients and what treatment/management strategies
can be used to minimize the risk of morbidity and mortality due to it.
Literature Review:
Through a systematic review of literature, several aspects were highlighted that
requires further studies to be done in the field of diabetic wound management. These aspects
are arranged thematically:
Biofilms:
Studies by Harlow et al. (2015) suggested that slow healing wounds often develop
biofilm, which can be a precursor of an infection. Biofilms can be understood as a well
structured microbial community existing in a polymeric matrix that is created by the
microbes (called extracellular polymeric substances EPS) stuck to a living or inert surface
(Flemming et al. 2015). Seth et al. (2012) also supported that biofilm bacteria are more
resistant to the immune reaction of the host as well as antiseptics and antibiotics, in
comparison to planktonic bacteria, which increases the risks of wound infection.
Furthermore, local inflammatory response to biofilm and microbial toxin can further cause
damage to the tissues, and the biofilm can spread by ‘seeding’ to adjacent surfaces to the
wound, forming new microbial colonies (Philips and Schultz 2012; Kaplan, Meyenhofer and
Fine 2003). Hurlow and Bowler (2012) added that poor moisture or poor control of exudates
in the environment can lead to the formation of a biofilm. Multispecies biofilm also have
(Seth et al. 2012). This poses an important question “can biofilm be useful in the early
detection of infection in diabetic foot ulcers?”
Research Objectives/Questions:
The objective of the research is to study whether presence of biofilm can be used for
early slow healing foot ulcers in diabetic patients and what treatment/management strategies
can be used to minimize the risk of morbidity and mortality due to it.
Literature Review:
Through a systematic review of literature, several aspects were highlighted that
requires further studies to be done in the field of diabetic wound management. These aspects
are arranged thematically:
Biofilms:
Studies by Harlow et al. (2015) suggested that slow healing wounds often develop
biofilm, which can be a precursor of an infection. Biofilms can be understood as a well
structured microbial community existing in a polymeric matrix that is created by the
microbes (called extracellular polymeric substances EPS) stuck to a living or inert surface
(Flemming et al. 2015). Seth et al. (2012) also supported that biofilm bacteria are more
resistant to the immune reaction of the host as well as antiseptics and antibiotics, in
comparison to planktonic bacteria, which increases the risks of wound infection.
Furthermore, local inflammatory response to biofilm and microbial toxin can further cause
damage to the tissues, and the biofilm can spread by ‘seeding’ to adjacent surfaces to the
wound, forming new microbial colonies (Philips and Schultz 2012; Kaplan, Meyenhofer and
Fine 2003). Hurlow and Bowler (2012) added that poor moisture or poor control of exudates
in the environment can lead to the formation of a biofilm. Multispecies biofilm also have
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Diabetes wound care and treatment
been found to be more pathogenic compared to single species biofilm (Seth et al. 2012). This
further implicates the necessity to identify the type of biodiversity while analyzing risk of
infection. Detecting biofim on wounds can allow healthcare providers to take precautionary
steps to avoid infection before the manifestation of its clinical signs like fever, suppuration,
erythema, edema, and pain in the wound, and conversely, presence of wounds that does not
heal despite treatment, can suggest the presence of biofilm (Hurlow et al. 2015).
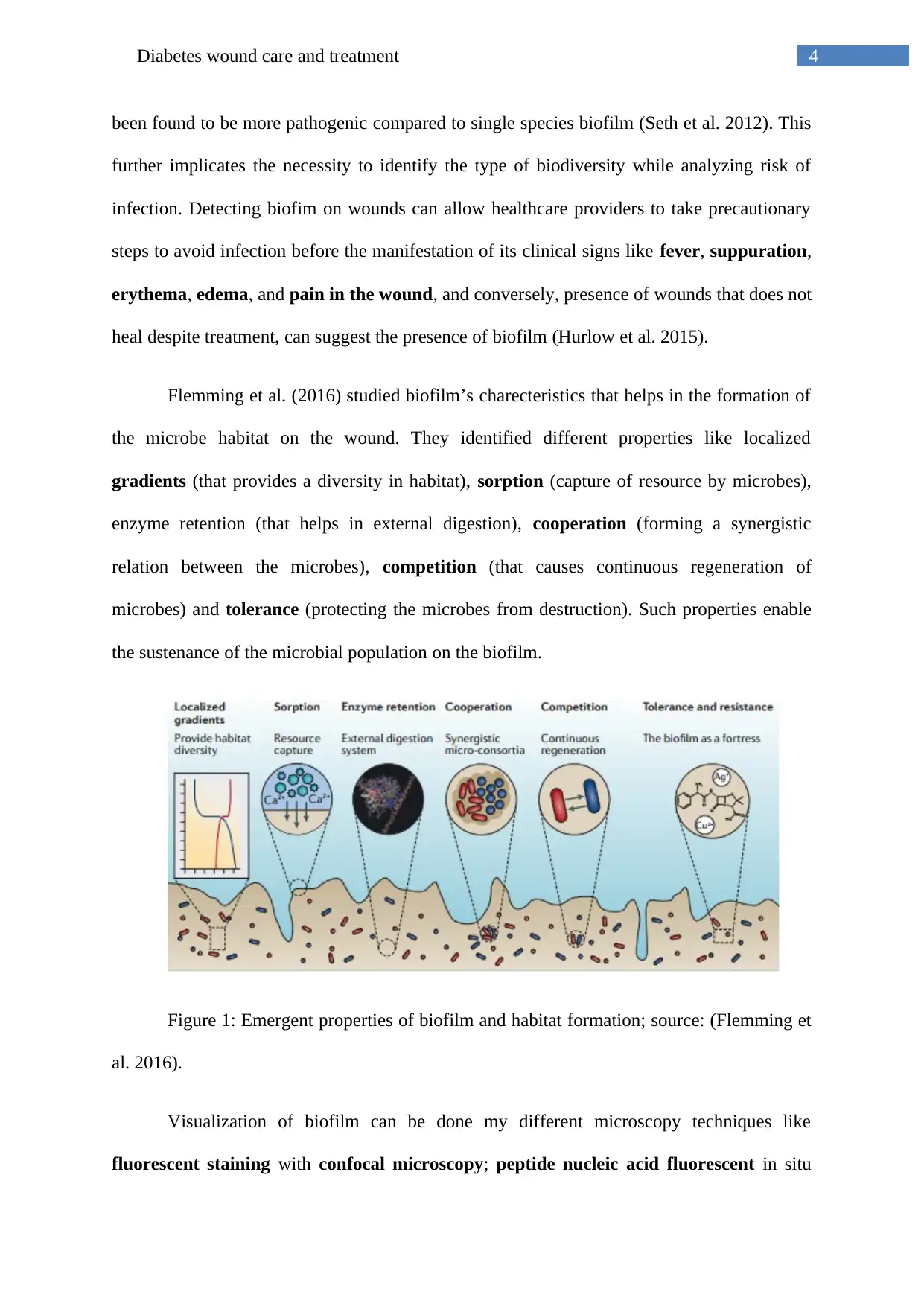
Flemming et al. (2016) studied biofilm’s charecteristics that helps in the formation of
the microbe habitat on the wound. They identified different properties like localized
gradients (that provides a diversity in habitat), sorption (capture of resource by microbes),
enzyme retention (that helps in external digestion), cooperation (forming a synergistic
relation between the microbes), competition (that causes continuous regeneration of
microbes) and tolerance (protecting the microbes from destruction). Such properties enable
the sustenance of the microbial population on the biofilm.
Figure 1: Emergent properties of biofilm and habitat formation; source: (Flemming et
al. 2016).
Visualization of biofilm can be done my different microscopy techniques like
fluorescent staining with confocal microscopy; peptide nucleic acid fluorescent in situ
been found to be more pathogenic compared to single species biofilm (Seth et al. 2012). This
further implicates the necessity to identify the type of biodiversity while analyzing risk of
infection. Detecting biofim on wounds can allow healthcare providers to take precautionary
steps to avoid infection before the manifestation of its clinical signs like fever, suppuration,
erythema, edema, and pain in the wound, and conversely, presence of wounds that does not
heal despite treatment, can suggest the presence of biofilm (Hurlow et al. 2015).
Flemming et al. (2016) studied biofilm’s charecteristics that helps in the formation of
the microbe habitat on the wound. They identified different properties like localized
gradients (that provides a diversity in habitat), sorption (capture of resource by microbes),
enzyme retention (that helps in external digestion), cooperation (forming a synergistic
relation between the microbes), competition (that causes continuous regeneration of
microbes) and tolerance (protecting the microbes from destruction). Such properties enable
the sustenance of the microbial population on the biofilm.
Figure 1: Emergent properties of biofilm and habitat formation; source: (Flemming et
al. 2016).
Visualization of biofilm can be done my different microscopy techniques like
fluorescent staining with confocal microscopy; peptide nucleic acid fluorescent in situ
5Diabetes wound care and treatment
hybridization; scanning electron microscopy and light microscopy with gram staining
(Oates et al. 2014). Evidence of biofilm on clinical wounds can also be evidence by the
presence of excessive and increasing fluid exudates from wound, antibiotic resistance, and
repeated infection and wound recalcitrance. However, the study of literature showed a lack of
detailed studies done to link the biofilm’s presence on diabetic foot ulcers and the rapid
detection of biofilm on chronic wounds. Such knowledge can help to ascertain the importance
of biofilm in wound care practices.
Diabetic Foot Ulcer DFU:
Diabetic Foot ulcers are linked with diabetic neuropathy and nerve pain, and can
affect people suffering from both diabetes type 1 and 2. The foot ulcers can be caused due to
mild injuries to the foot, which subsequently fails to heal, and cause ulcers. The risk for this
condition can increase due to neuropathy, poor circulation of blood,
unmanaged/untreated/uncontrolled diabetes, poor fitting footwear, walking barefoot or
any activities that can increase the likelihood of sustaining even minor injury to the foot or
lower extremities (Diabetes.co.uk 2018). Estimates show that the propensity of diabetic
patients to develop foot ulcers can be 10%-25% (Dargaville et al. 2013). Due to the steep
increase in the global diagnosis of diabetes, it is necessary that the process of chronic wound
repair and tissue regeneration be studied in detail, which can help to develop understanding
of the process, and implement effective strategies for management and treatment. Dreifke,
Jayasuriya and Jayasuriya (2015) suggested that primary objective for healing of wound
involves timely closure of wound, prompt relief in pain, and aesthetically acceptable scar.
Hyperglycemia (or high blood glucose) can inhibit the formation of Extra Cellular
Matrix ECM through rising secretion of Tumor Necrosis Factor TNF alpha and Interleukins
IL-1beta. This is further complicated due to impaired migration of keratinocyte and function
hybridization; scanning electron microscopy and light microscopy with gram staining
(Oates et al. 2014). Evidence of biofilm on clinical wounds can also be evidence by the
presence of excessive and increasing fluid exudates from wound, antibiotic resistance, and
repeated infection and wound recalcitrance. However, the study of literature showed a lack of
detailed studies done to link the biofilm’s presence on diabetic foot ulcers and the rapid
detection of biofilm on chronic wounds. Such knowledge can help to ascertain the importance
of biofilm in wound care practices.
Diabetic Foot Ulcer DFU:
Diabetic Foot ulcers are linked with diabetic neuropathy and nerve pain, and can
affect people suffering from both diabetes type 1 and 2. The foot ulcers can be caused due to
mild injuries to the foot, which subsequently fails to heal, and cause ulcers. The risk for this
condition can increase due to neuropathy, poor circulation of blood,
unmanaged/untreated/uncontrolled diabetes, poor fitting footwear, walking barefoot or
any activities that can increase the likelihood of sustaining even minor injury to the foot or
lower extremities (Diabetes.co.uk 2018). Estimates show that the propensity of diabetic
patients to develop foot ulcers can be 10%-25% (Dargaville et al. 2013). Due to the steep
increase in the global diagnosis of diabetes, it is necessary that the process of chronic wound
repair and tissue regeneration be studied in detail, which can help to develop understanding
of the process, and implement effective strategies for management and treatment. Dreifke,
Jayasuriya and Jayasuriya (2015) suggested that primary objective for healing of wound
involves timely closure of wound, prompt relief in pain, and aesthetically acceptable scar.
Hyperglycemia (or high blood glucose) can inhibit the formation of Extra Cellular
Matrix ECM through rising secretion of Tumor Necrosis Factor TNF alpha and Interleukins
IL-1beta. This is further complicated due to impaired migration of keratinocyte and function
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Diabetes wound care and treatment
of leukocyte can lead to infection. Additionally, depletion of inorganic phosphates in the
ulcerated area, leads to lowered levels of Adenosine Tri Phosphate (ATP) thereby adversely
affecting the immune response, further delaying/inhibiting the natural healing process (Lev-
Tov 2013).
Strategies like systemic glucose control, debridement of nonviable tissue and
maintaining proper perfusion of extremities are of immense importance for treating diabetic
ulcers (Dreifke, Jayasuriya and Jayasuriya 2015). Moura et al. (2014) suggested chitosan (a
linear copolymer extracted from the exoskeleton of crustaceans like crab or shrimps) based
dressings for healing diabetic wounds. They used the substance 5-methyl-pyrolidinone
chitosan (MPC) that supplies neurotensin (which is a neuropeptide that functions as
inflammatory modulator), and found that it can promote healing of wound. Studies done
using various forms of chitosan, like microparticles, membranes, hydrogel and scaffold to
analyze their wound healing effects (Park et al. 2009). Such strategy has shown to reduce
diabetic wounds in mice by 50% (Moura et al. 2014).
Studies by Yao et al. (2006) showed that treating patients suffering from diabetic foot
ulcers with Fibroblast Growth Factor-2 (FGF2) can increase wound closure by 68%, and in
3 weeks accelerated wound closure by 24% in comparison to a placebo group. This was
further supported through studies by Singla et al. (2014) that showed a significant
improvement in healing time and increase in closure of diabetic foot ulcers by the application
of tropical gens containing human epidermal growth factor (EGF).
Debridement (removal of damaged, dead or infected tissues) of diabetic wound has
been acknowledged to improve the healing potential of the surrounding healthy tissues.
Different types of debridement strategies have been suggested by many studies. Surgical
debridement where the necrotic or infected tissue is surgically removed is the quickest and
of leukocyte can lead to infection. Additionally, depletion of inorganic phosphates in the
ulcerated area, leads to lowered levels of Adenosine Tri Phosphate (ATP) thereby adversely
affecting the immune response, further delaying/inhibiting the natural healing process (Lev-
Tov 2013).
Strategies like systemic glucose control, debridement of nonviable tissue and
maintaining proper perfusion of extremities are of immense importance for treating diabetic
ulcers (Dreifke, Jayasuriya and Jayasuriya 2015). Moura et al. (2014) suggested chitosan (a
linear copolymer extracted from the exoskeleton of crustaceans like crab or shrimps) based
dressings for healing diabetic wounds. They used the substance 5-methyl-pyrolidinone
chitosan (MPC) that supplies neurotensin (which is a neuropeptide that functions as
inflammatory modulator), and found that it can promote healing of wound. Studies done
using various forms of chitosan, like microparticles, membranes, hydrogel and scaffold to
analyze their wound healing effects (Park et al. 2009). Such strategy has shown to reduce
diabetic wounds in mice by 50% (Moura et al. 2014).
Studies by Yao et al. (2006) showed that treating patients suffering from diabetic foot
ulcers with Fibroblast Growth Factor-2 (FGF2) can increase wound closure by 68%, and in
3 weeks accelerated wound closure by 24% in comparison to a placebo group. This was
further supported through studies by Singla et al. (2014) that showed a significant
improvement in healing time and increase in closure of diabetic foot ulcers by the application
of tropical gens containing human epidermal growth factor (EGF).
Debridement (removal of damaged, dead or infected tissues) of diabetic wound has
been acknowledged to improve the healing potential of the surrounding healthy tissues.
Different types of debridement strategies have been suggested by many studies. Surgical
debridement where the necrotic or infected tissue is surgically removed is the quickest and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Diabetes wound care and treatment
most efficient method (Driver 2014). In autolytic debridement, an occlusive dressing is
applied on the wound that allows tissue fluids containing macrophages, enzymes and
neutrophils to accumulate which can then eliminate the microbes and digest the necrotic
tissues in a moist wound healing environment (Sibbald et al. 2000). Mechanical debridement
requires the elimination of necrotic tissue by wound dressing that is regularly changed,
without causing any damage to the adjacent healthy tissues. Scrubbing of the wounds also
helps the elimination of devitalized tissue and wound exudates, however such a process can
also cause bleeding and pain due to trauma to wound (Rolstad and Ovington 2017).
Enzymatic debridement involves enzymes like collagenase, papain and fibrinolysin, and can
be used when surgical process is not an option (Ramundo and Gray 2008). Maggot
debridement involves maggots of Lucilia sericata, raised in sterile environment, placed on
the wound and then wrapped using secondary dressing. Consequently the maggot larvae
feeds on the dead tissue and secrete antimicrobial substances that ultimately show infection
and foster healing and closure of wound.
This implicates the importance to study further how the application of chitosan,
growth factors and debridement of diabetic foot ulcers can reduce associated complications,
morbidity risks and accelerate the processes of healing ad closure of wound.
Research Design and Methodology:
The study will involve diabetes patients, who have been diagnosed with foot ulcer
(DFU). The study will analyze each patient using gram staining and light microscopy and
scanning electron microscopy to finds signs of biofilm and to classify its type, and then put
on a treatment module that comprises of chitosan dressing and application of Growth Factors,
and debridement (if needed) for 2 weeks. After the treatment, the patients will be analyzed
again for foot ulcer. The study will be compared to a trial group consisting of patients with
most efficient method (Driver 2014). In autolytic debridement, an occlusive dressing is
applied on the wound that allows tissue fluids containing macrophages, enzymes and
neutrophils to accumulate which can then eliminate the microbes and digest the necrotic
tissues in a moist wound healing environment (Sibbald et al. 2000). Mechanical debridement
requires the elimination of necrotic tissue by wound dressing that is regularly changed,
without causing any damage to the adjacent healthy tissues. Scrubbing of the wounds also
helps the elimination of devitalized tissue and wound exudates, however such a process can
also cause bleeding and pain due to trauma to wound (Rolstad and Ovington 2017).
Enzymatic debridement involves enzymes like collagenase, papain and fibrinolysin, and can
be used when surgical process is not an option (Ramundo and Gray 2008). Maggot
debridement involves maggots of Lucilia sericata, raised in sterile environment, placed on
the wound and then wrapped using secondary dressing. Consequently the maggot larvae
feeds on the dead tissue and secrete antimicrobial substances that ultimately show infection
and foster healing and closure of wound.
This implicates the importance to study further how the application of chitosan,
growth factors and debridement of diabetic foot ulcers can reduce associated complications,
morbidity risks and accelerate the processes of healing ad closure of wound.
Research Design and Methodology:
The study will involve diabetes patients, who have been diagnosed with foot ulcer
(DFU). The study will analyze each patient using gram staining and light microscopy and
scanning electron microscopy to finds signs of biofilm and to classify its type, and then put
on a treatment module that comprises of chitosan dressing and application of Growth Factors,
and debridement (if needed) for 2 weeks. After the treatment, the patients will be analyzed
again for foot ulcer. The study will be compared to a trial group consisting of patients with
8Diabetes wound care and treatment
signs of biofilm, but given a different form of treatment or patients who refused treatment
after diagnosis.
The selected research process will be a primary research, and research philosophy
will be ‘positivism’ as it allows objectivity in the study, and gain factual information from
the observation. The research design will be ‘conclusive’ and the type of conclusive research
design used will be “causal” as it aims to ascertain whether early detection of DFU using
biofilm and early treatment can enhance wound healing and closure (that is studying the
effect of early detection and treatment for DFU).
The sample will be drawn from patients diagnosed with diabetes and foot ulcers (in
the UK) but have not started treatment for the same. The study will exclude patients of foot
ulcers from other causes (other than diabetes) to eliminate interferences in the etiologies of
different conditions. Sample size: the sample can include anywhere between 20 to 30 patients
(depending on the final sampling process), and will be selected through non-probability
(purposive) sampling.
This can be useful to analyze whether early identification of infections in diabetic foot
ulcers can be done by looking for signs of biofilm on diabetic patients, and whether the
selected management/treatment strategies can enhance or accelerate the healing and closure
of wound. Data collection method will be quantitative, and collect the following data:
Presence of Biofilm (yes/no)
Type of biofilm (single species/multi species)
Wound healing time after treatment (in days)
Wound closing time after treatment (in days)
signs of biofilm, but given a different form of treatment or patients who refused treatment
after diagnosis.
The selected research process will be a primary research, and research philosophy
will be ‘positivism’ as it allows objectivity in the study, and gain factual information from
the observation. The research design will be ‘conclusive’ and the type of conclusive research
design used will be “causal” as it aims to ascertain whether early detection of DFU using
biofilm and early treatment can enhance wound healing and closure (that is studying the
effect of early detection and treatment for DFU).
The sample will be drawn from patients diagnosed with diabetes and foot ulcers (in
the UK) but have not started treatment for the same. The study will exclude patients of foot
ulcers from other causes (other than diabetes) to eliminate interferences in the etiologies of
different conditions. Sample size: the sample can include anywhere between 20 to 30 patients
(depending on the final sampling process), and will be selected through non-probability
(purposive) sampling.
This can be useful to analyze whether early identification of infections in diabetic foot
ulcers can be done by looking for signs of biofilm on diabetic patients, and whether the
selected management/treatment strategies can enhance or accelerate the healing and closure
of wound. Data collection method will be quantitative, and collect the following data:
Presence of Biofilm (yes/no)
Type of biofilm (single species/multi species)
Wound healing time after treatment (in days)
Wound closing time after treatment (in days)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Diabetes wound care and treatment
The collected data will be subjected to correlation analysis to relate the early detection
of biofilm and faster recovery due to treatment with chitosan, growth factor and debridement.
Ethical Considerations:
To ensure compliance to ethical standards and principles, the following ethical considerations
shall prevail throughout the study:
a) Participation of the patient in the study will be completely voluntary
b) All participants will be briefed before and after the study, informing them about the
reason for the study and the overall flow of the study or treatment
c) Any personally identified information will be kept confidential and private, and shall
not be published or shared.
d) All clinical and diagnostic data will be represented intact, without any manipulation
e) Permission will be taken from the local ethics board/committee before starting the
research.
Conclusion:
Diabetic foot ulcer can increase risks of morbidity and even mortality in diabetic
patients, and considering the rise in the cases of diabetes globally, it is important to learn
strategies that can enable early detection and prevention of DFU and its co morbidities. Also
precautionary strategies (prevention of diabetes) can be the most efficient; more studies needs
to be done that can link the importance of biofilm specifically for DFU. Since biofilm have
been identified as a prequel to infection, detection of biofilm on foot ulcer can be a strong
suggestion for treatment measures. The study will aim to analyze how early detection coupled
with prompt intervention can reduce the risks associated with DFU and allow speedy
The collected data will be subjected to correlation analysis to relate the early detection
of biofilm and faster recovery due to treatment with chitosan, growth factor and debridement.
Ethical Considerations:
To ensure compliance to ethical standards and principles, the following ethical considerations
shall prevail throughout the study:
a) Participation of the patient in the study will be completely voluntary
b) All participants will be briefed before and after the study, informing them about the
reason for the study and the overall flow of the study or treatment
c) Any personally identified information will be kept confidential and private, and shall
not be published or shared.
d) All clinical and diagnostic data will be represented intact, without any manipulation
e) Permission will be taken from the local ethics board/committee before starting the
research.
Conclusion:
Diabetic foot ulcer can increase risks of morbidity and even mortality in diabetic
patients, and considering the rise in the cases of diabetes globally, it is important to learn
strategies that can enable early detection and prevention of DFU and its co morbidities. Also
precautionary strategies (prevention of diabetes) can be the most efficient; more studies needs
to be done that can link the importance of biofilm specifically for DFU. Since biofilm have
been identified as a prequel to infection, detection of biofilm on foot ulcer can be a strong
suggestion for treatment measures. The study will aim to analyze how early detection coupled
with prompt intervention can reduce the risks associated with DFU and allow speedy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10Diabetes wound care and treatment
recovery. The final results of the study can then be then used to compare results from other
studies to support its veracity.
recovery. The final results of the study can then be then used to compare results from other
studies to support its veracity.
11Diabetes wound care and treatment
References:
Dargaville, T.R., Farrugia, B.L., Broadbent, J.A., Pace, S., Upton, Z. and Voelcker, N.H.,
2013. Sensors and imaging for wound healing: a review. Biosensors and Bioelectronics, 41,
pp.30-42.
Diabetes.co.uk, 2018. Diabetes and Foot Ulcers. [online] Diabetes.co.uk. Available at:
https://www.diabetes.co.uk/diabetes-complications/diabetic-foot-ulcers.html [Accessed 23
Feb. 2018].
Dreifke, M., Jayasuriya, A. and Jayasuriya, A., 2015. Current wound healing procedures and
potential care. Materials Science and Engineering: C, 48, pp.651-662.
Driver, V.R., 2014. Treating the macro and micro wound environment of the diabetic patient:
managing the whole patient, not the hole in the patient. In Foot and Ankle Quarterly—The
Seminar Journal (Vol. 16, pp. 47-56).
Flemming, H.C., Wingender, J., Szewzyk, U., Steinberg, P., Rice, S.A. and Kjelleberg, S.,
2016. Biofilms: an emergent form of bacterial life. Nature Reviews Microbiology, 14(9),
p.563.
Ha.org.hk., 2018. Cite a Website - Cite This For Me. [online] Ha.org.hk. Available at:
http://www.ha.org.hk/haho/ho/ap/AP17-18Eng.pdf [Accessed 22 Feb. 2018].
Hurlow, J. and Bowler, P.G., 2012. Potential implications of biofilm in chronic wounds: a
case series. journal of wound care, 21(3), pp.109-119.
Hurlow, J., Couch, K., Laforet, K., Bolton, L., Metcalf, D. and Bowler, P., 2015. Clinical
Biofilms: A Challenging Frontier in Wound Care. Advances in Wound Care, 4(5), pp.295-
301.
References:
Dargaville, T.R., Farrugia, B.L., Broadbent, J.A., Pace, S., Upton, Z. and Voelcker, N.H.,
2013. Sensors and imaging for wound healing: a review. Biosensors and Bioelectronics, 41,
pp.30-42.
Diabetes.co.uk, 2018. Diabetes and Foot Ulcers. [online] Diabetes.co.uk. Available at:
https://www.diabetes.co.uk/diabetes-complications/diabetic-foot-ulcers.html [Accessed 23
Feb. 2018].
Dreifke, M., Jayasuriya, A. and Jayasuriya, A., 2015. Current wound healing procedures and
potential care. Materials Science and Engineering: C, 48, pp.651-662.
Driver, V.R., 2014. Treating the macro and micro wound environment of the diabetic patient:
managing the whole patient, not the hole in the patient. In Foot and Ankle Quarterly—The
Seminar Journal (Vol. 16, pp. 47-56).
Flemming, H.C., Wingender, J., Szewzyk, U., Steinberg, P., Rice, S.A. and Kjelleberg, S.,
2016. Biofilms: an emergent form of bacterial life. Nature Reviews Microbiology, 14(9),
p.563.
Ha.org.hk., 2018. Cite a Website - Cite This For Me. [online] Ha.org.hk. Available at:
http://www.ha.org.hk/haho/ho/ap/AP17-18Eng.pdf [Accessed 22 Feb. 2018].
Hurlow, J. and Bowler, P.G., 2012. Potential implications of biofilm in chronic wounds: a
case series. journal of wound care, 21(3), pp.109-119.
Hurlow, J., Couch, K., Laforet, K., Bolton, L., Metcalf, D. and Bowler, P., 2015. Clinical
Biofilms: A Challenging Frontier in Wound Care. Advances in Wound Care, 4(5), pp.295-
301.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





