Analysis of Type 2 Diabetes in Children: Risk Factors & Solutions
VerifiedAdded on 2023/06/11
|10
|1724
|165
Report
AI Summary
This report examines the prevalence and causes of Type 2 Diabetes Mellitus (T2DM) among children in Australia, where approximately 31,000 individuals aged 10-24 are affected. The report highlights that indigenous Australian children have an eight-times higher occurrence rate compared to non-indigenous children. Key non-modifiable risk factors include genetic predisposition, exposure to maternal diabetes, and increased plasma insulin levels during puberty. Modifiable risk factors identified are childhood obesity, lack of physical activity, and unhealthy diets. The suggested solutions involve lifestyle modifications, such as increased physical activity and balanced diets, alongside pharmacological interventions like metformin and insulin treatment. The Australian government's initiatives, including the National Diabetes Services Schemes (NDSS), aim to raise awareness and provide subsidized medicines. The report concludes by recommending improved monitoring systems to capture unreported diabetes cases, especially among aboriginal populations, and better detection systems to differentiate between type 1 and type 2 diabetes, ensuring early and appropriate treatment.

Running head: DIABETES IN CHILDREN
Diabetes in Children
Name of the Student
Name of the University
Author Note
Diabetes in Children
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
DIABETES IN CHILDREN
Abstract
Approximately thirty one thousand people who are aged between 10 to 24 years suffer from
Type 2 Diabetes in Australia. The rate of occurrence of childhood and youth diabetes is
higher among the aboriginals. The non-modifiable risk factors associated with diabetes
include genetic predisposition, exposure to maternal diabetes and sudden increase in the
plasma insulin level during puberty. Modifiable risk factors which causes high incidence of
diabetes among children is childhood obesity, lack of physical activity and unhealthy diet. In
order to fight against childhood T2DM, proper lifestyle modifications and pharmacological
interventions must be taken into consideration. Government of Australia is working towards
the reduction in the rate of T2DM among children via launching National Diabetes Services
Schemes. However, government must further take initiatives towards early detection of
diabetes among children along with proper tabulation of the diabetes occurrence among the
youth via reducing the cases of unreported diabetes.
DIABETES IN CHILDREN
Abstract
Approximately thirty one thousand people who are aged between 10 to 24 years suffer from
Type 2 Diabetes in Australia. The rate of occurrence of childhood and youth diabetes is
higher among the aboriginals. The non-modifiable risk factors associated with diabetes
include genetic predisposition, exposure to maternal diabetes and sudden increase in the
plasma insulin level during puberty. Modifiable risk factors which causes high incidence of
diabetes among children is childhood obesity, lack of physical activity and unhealthy diet. In
order to fight against childhood T2DM, proper lifestyle modifications and pharmacological
interventions must be taken into consideration. Government of Australia is working towards
the reduction in the rate of T2DM among children via launching National Diabetes Services
Schemes. However, government must further take initiatives towards early detection of
diabetes among children along with proper tabulation of the diabetes occurrence among the
youth via reducing the cases of unreported diabetes.
2
DIABETES IN CHILDREN
Table of Contents
1. Introduction.........................................................................................................................3
2. Findings..............................................................................................................................3
2.1 Reason for T2DM in children..........................................................................................3
2.1.1 Non-modifiable risk factors......................................................................................3
2.1.2 Modifiable risk factors..............................................................................................4
2.2 Suggested solution.......................................................................................................4
3. Discussion...........................................................................................................................4
4. Conclusion..........................................................................................................................6
5. Recommendations...............................................................................................................6
6. References...........................................................................................................................8
DIABETES IN CHILDREN
Table of Contents
1. Introduction.........................................................................................................................3
2. Findings..............................................................................................................................3
2.1 Reason for T2DM in children..........................................................................................3
2.1.1 Non-modifiable risk factors......................................................................................3
2.1.2 Modifiable risk factors..............................................................................................4
2.2 Suggested solution.......................................................................................................4
3. Discussion...........................................................................................................................4
4. Conclusion..........................................................................................................................6
5. Recommendations...............................................................................................................6
6. References...........................................................................................................................8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
DIABETES IN CHILDREN
1. Introduction
Type 2 Diabetes Mellitus (T2DM) was initially considered as a disease of older
people however, according to the reports published by the Australian Institute of Health and
Welfare (2014), T2DM is also common among the children. The survey conducted by the
Australian Bureau of Statistics (ABS) showed that during June 2012, at 31,000 people who
are aged between 10 to 39 years, are diagnosed with type 2 diabetes. Of them 2,200 people
were aged in between 10 to 24 years and this constitutes of 0.3% of the total population. This
rate occurrence of type of diabetes is 8 times higher among the indigenous Australian
children (10 to 14) in comparison to the non-indigenous Australian children. The following
report aims to analyse the main underlying causes behind T2DM among the children,
governmental initiates in order to reduce the risk and subsequent recommendations to
improve the overall scenario further.
2. Findings
2.1 Reason for T2DM in children
2.1.1 Non-modifiable risk factors
According to the reports published by Kao and Sabin (2016), the early onset of T2DM
mainly occurs during adolescence and generally not before than that. During puberty, the
level of plasma insulin increase steadily from pre-pubertal baseline. It mainly reaches to its
peak during puberty and then gradually returns to pre-pubertal levels during the third decade
of life. Due to rise in the insulin level during puberty, there occurs decrease in insulin
sensitivity by 30% leading to the development of T2DM. Another non-modifiable risk factor
of T2DM among the children is exposure to maternal diabetes and genetic pre-disposition to
T2DM, ethnicity and family history of diabetes.
DIABETES IN CHILDREN
1. Introduction
Type 2 Diabetes Mellitus (T2DM) was initially considered as a disease of older
people however, according to the reports published by the Australian Institute of Health and
Welfare (2014), T2DM is also common among the children. The survey conducted by the
Australian Bureau of Statistics (ABS) showed that during June 2012, at 31,000 people who
are aged between 10 to 39 years, are diagnosed with type 2 diabetes. Of them 2,200 people
were aged in between 10 to 24 years and this constitutes of 0.3% of the total population. This
rate occurrence of type of diabetes is 8 times higher among the indigenous Australian
children (10 to 14) in comparison to the non-indigenous Australian children. The following
report aims to analyse the main underlying causes behind T2DM among the children,
governmental initiates in order to reduce the risk and subsequent recommendations to
improve the overall scenario further.
2. Findings
2.1 Reason for T2DM in children
2.1.1 Non-modifiable risk factors
According to the reports published by Kao and Sabin (2016), the early onset of T2DM
mainly occurs during adolescence and generally not before than that. During puberty, the
level of plasma insulin increase steadily from pre-pubertal baseline. It mainly reaches to its
peak during puberty and then gradually returns to pre-pubertal levels during the third decade
of life. Due to rise in the insulin level during puberty, there occurs decrease in insulin
sensitivity by 30% leading to the development of T2DM. Another non-modifiable risk factor
of T2DM among the children is exposure to maternal diabetes and genetic pre-disposition to
T2DM, ethnicity and family history of diabetes.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
DIABETES IN CHILDREN
2.1.2 Modifiable risk factors
Obesity is regarded as the one of the important modifiable risk factors behind the
development of T2DM among the youth (Smith & Ryckman, 2015). According to American
Diabetes Association (2015), 85% of the affected children are either obese or over-weight.
Another modifiable risk factor for diabetes mellitus in Australia is poor diet and lack of
physical inactivity and both of these further lead to gain in weight.
2.2 Suggested solution
Among children and adolescents life style modifications are paramount for the treatment
of T2DM. Lifestyle modification includes vigorous physical activity (60 minutes per day)
which will help in maintaining healthy BMI along with reduction in extra body fat. Another
lifestyle modification include maintenance of balance diet which mainly encompass regular
meals filled with healthy snacks, decreased portion sizes, increase consumption of vegetables
and fruits and decreased consumption of high calorie beverages. However, only 10% of
children succeed to achieve their lifestyle modification aims and the main reason behind this
is peer pressure towards unhealthy eating, loss of follow-up and lack of proper knowledge
about balanced nutritional diet (Gao, Gao & Xue, 2016). Hence, apart from life modifications
pharmacological interventions are also important for better glycaemic control. The main
pharmacological interventions include metformin and insulin treatment. Alternative drugs
like thoazolidinediones and meglitinides though approved for adults T2DM treatment, are not
recommended for children (Tamborlane et al., 2016).
3. Discussion
Incidence of T2DM is increasing among the young individuals and is associated with
childhood obesity. Main interventions that are used to control prevalence and chronicity of
T2DM include lifestyle modifications and use of pharmaco-therapy (Kao & Sabin, 2016).
DIABETES IN CHILDREN
2.1.2 Modifiable risk factors
Obesity is regarded as the one of the important modifiable risk factors behind the
development of T2DM among the youth (Smith & Ryckman, 2015). According to American
Diabetes Association (2015), 85% of the affected children are either obese or over-weight.
Another modifiable risk factor for diabetes mellitus in Australia is poor diet and lack of
physical inactivity and both of these further lead to gain in weight.
2.2 Suggested solution
Among children and adolescents life style modifications are paramount for the treatment
of T2DM. Lifestyle modification includes vigorous physical activity (60 minutes per day)
which will help in maintaining healthy BMI along with reduction in extra body fat. Another
lifestyle modification include maintenance of balance diet which mainly encompass regular
meals filled with healthy snacks, decreased portion sizes, increase consumption of vegetables
and fruits and decreased consumption of high calorie beverages. However, only 10% of
children succeed to achieve their lifestyle modification aims and the main reason behind this
is peer pressure towards unhealthy eating, loss of follow-up and lack of proper knowledge
about balanced nutritional diet (Gao, Gao & Xue, 2016). Hence, apart from life modifications
pharmacological interventions are also important for better glycaemic control. The main
pharmacological interventions include metformin and insulin treatment. Alternative drugs
like thoazolidinediones and meglitinides though approved for adults T2DM treatment, are not
recommended for children (Tamborlane et al., 2016).
3. Discussion
Incidence of T2DM is increasing among the young individuals and is associated with
childhood obesity. Main interventions that are used to control prevalence and chronicity of
T2DM include lifestyle modifications and use of pharmaco-therapy (Kao & Sabin, 2016).
5
DIABETES IN CHILDREN
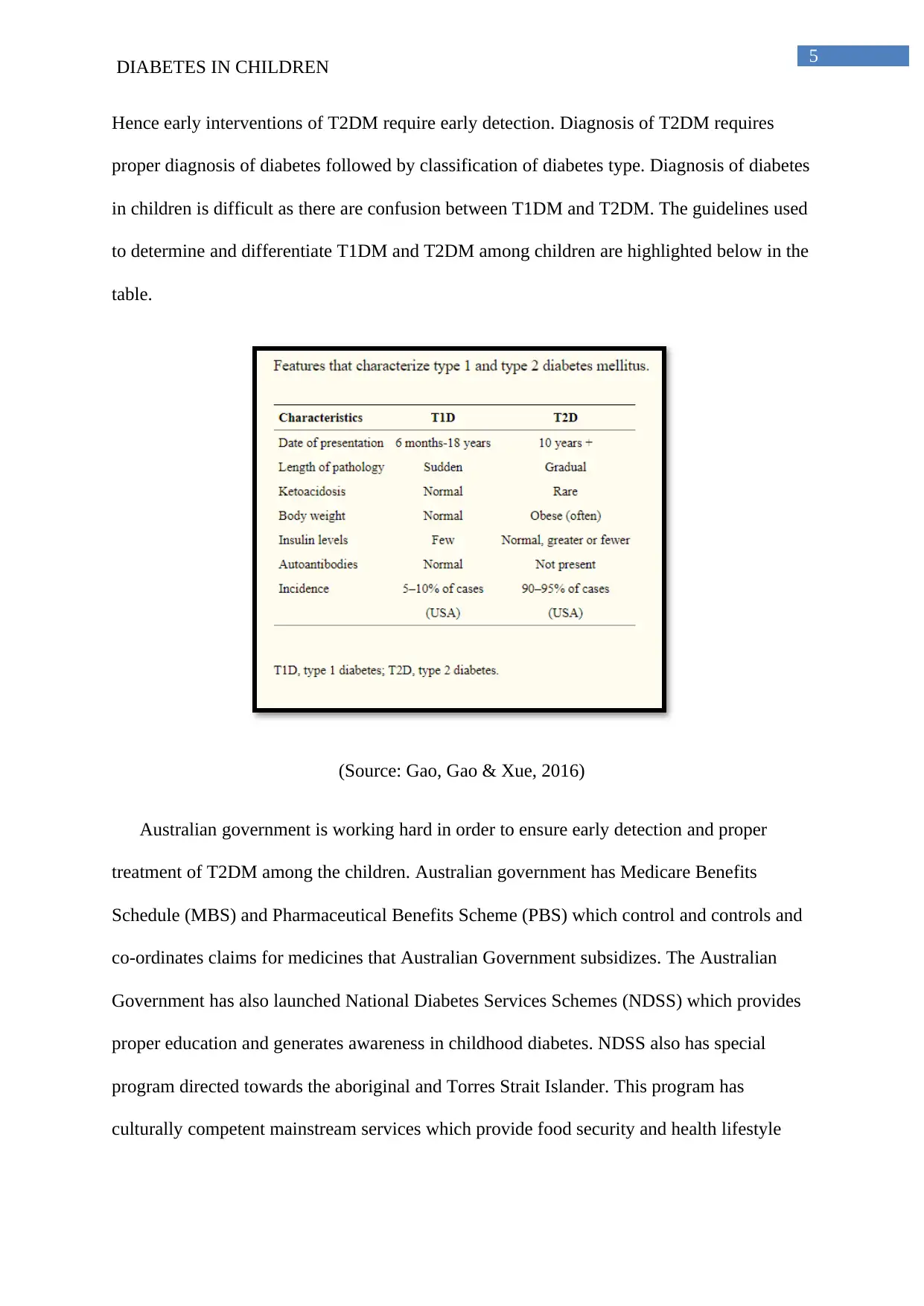
Hence early interventions of T2DM require early detection. Diagnosis of T2DM requires
proper diagnosis of diabetes followed by classification of diabetes type. Diagnosis of diabetes
in children is difficult as there are confusion between T1DM and T2DM. The guidelines used
to determine and differentiate T1DM and T2DM among children are highlighted below in the
table.
(Source: Gao, Gao & Xue, 2016)
Australian government is working hard in order to ensure early detection and proper
treatment of T2DM among the children. Australian government has Medicare Benefits
Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS) which control and controls and
co-ordinates claims for medicines that Australian Government subsidizes. The Australian
Government has also launched National Diabetes Services Schemes (NDSS) which provides
proper education and generates awareness in childhood diabetes. NDSS also has special
program directed towards the aboriginal and Torres Strait Islander. This program has
culturally competent mainstream services which provide food security and health lifestyle
DIABETES IN CHILDREN
Hence early interventions of T2DM require early detection. Diagnosis of T2DM requires
proper diagnosis of diabetes followed by classification of diabetes type. Diagnosis of diabetes
in children is difficult as there are confusion between T1DM and T2DM. The guidelines used
to determine and differentiate T1DM and T2DM among children are highlighted below in the
table.
(Source: Gao, Gao & Xue, 2016)
Australian government is working hard in order to ensure early detection and proper
treatment of T2DM among the children. Australian government has Medicare Benefits
Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS) which control and controls and
co-ordinates claims for medicines that Australian Government subsidizes. The Australian
Government has also launched National Diabetes Services Schemes (NDSS) which provides
proper education and generates awareness in childhood diabetes. NDSS also has special
program directed towards the aboriginal and Torres Strait Islander. This program has
culturally competent mainstream services which provide food security and health lifestyle
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
DIABETES IN CHILDREN
choices among the aboriginal community (Australian Government Department of Health,
2015).
4. Conclusion
Thus from the above discussion it can be concluded that T2DM is common among the
Australian children and this occurrence rate is 8 times higher among the indigenous
Australian population. The analysis of the scientific journals and government websites led to
the elucidation that apart from the non-modifiable risk factors like genetic predisposition and
increase plasma insulin during puberty, few modifiable risk factors are also associated with
the development of T2DM among children. The main modifiable risk factors include
sedentary lifestyle, unhealthy diet that led to the development of obesity. So in order to fight
against obesity both lifestyle modification and pharmacological interventions must be
employed. The government of Australia has also taken initiatives in order to generate disease
awareness and proper availability of subsidized medicines for fighting against childhood
T2DM.
5. Recommendations
According to the reports published by Australian Institute of Health and Welfare (2014),
ability of Australian government to successfully monitor T2DM among the children and
youth has certain limitations like the counts of the people registered under the diabetes census
underestimate the original incidence and prevalence of diabetes. The main reason behind this
is undiagnosed cases of diabetes, especially among the aboriginal population remains un-
reported. So the government of Australia must come forward with proper funding and
structured database system in order to monitor the actual occurrence rate of diabetes among
the children and youth and this will in turn help them to frame better intervention strategies
and generating the supply of subsidised medicines. The government of Australia must also
DIABETES IN CHILDREN
choices among the aboriginal community (Australian Government Department of Health,
2015).
4. Conclusion
Thus from the above discussion it can be concluded that T2DM is common among the
Australian children and this occurrence rate is 8 times higher among the indigenous
Australian population. The analysis of the scientific journals and government websites led to
the elucidation that apart from the non-modifiable risk factors like genetic predisposition and
increase plasma insulin during puberty, few modifiable risk factors are also associated with
the development of T2DM among children. The main modifiable risk factors include
sedentary lifestyle, unhealthy diet that led to the development of obesity. So in order to fight
against obesity both lifestyle modification and pharmacological interventions must be
employed. The government of Australia has also taken initiatives in order to generate disease
awareness and proper availability of subsidized medicines for fighting against childhood
T2DM.
5. Recommendations
According to the reports published by Australian Institute of Health and Welfare (2014),
ability of Australian government to successfully monitor T2DM among the children and
youth has certain limitations like the counts of the people registered under the diabetes census
underestimate the original incidence and prevalence of diabetes. The main reason behind this
is undiagnosed cases of diabetes, especially among the aboriginal population remains un-
reported. So the government of Australia must come forward with proper funding and
structured database system in order to monitor the actual occurrence rate of diabetes among
the children and youth and this will in turn help them to frame better intervention strategies
and generating the supply of subsidised medicines. The government of Australia must also
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7
DIABETES IN CHILDREN
have proper detection system for type 1 and type 2 diabetes and proper detection will led to
early identification of the disease and thereby initiating early treatment (American Diabetes
Association, 2015).
DIABETES IN CHILDREN
have proper detection system for type 1 and type 2 diabetes and proper detection will led to
early identification of the disease and thereby initiating early treatment (American Diabetes
Association, 2015).
8
DIABETES IN CHILDREN
6. References
American Diabetes Association. (2015). 2. Classification and diagnosis of diabetes. Diabetes
care, 38(Supplement 1), S8-S16.
American Diabetes Association. (2015). Standards of medical care in diabetes—2015
abridged for primary care providers. Clinical diabetes: a publication of the American
Diabetes Association, 33(2), 97.
Australian Government Department of Health. (2015) Australian National Diabetes Strategy
2016–2020. Access date: 23rd June. 2018. Retrieved from:
http://www.health.gov.au/internet/main/publishing.nsf/content/3AF935DA210DA043
CA257EFB000D0C03/$File/Australian%20National%20Diabetes%20Strategy
%202016-2020.pdf
Australian Institute of Health and Welfare. (2014).Type 2 diabetes in Australia’s children and
young people: a working paper. Access date: 23rd June. 2018. Retrieved from:
https://www.aihw.gov.au/getmedia/bc5d50e5-8ca0-474d-be77-
f96234d9a532/15203.pdf.aspx?inline=true
Gao, Y. Q., Gao, M., & Xue, Y. (2016). Treatment of diabetes in children. Experimental and
therapeutic medicine, 11(4), 1168-1172. Doi: doi: 10.3892/etm.2016.3039
Kao, K., & Sabin, M. A. (2016). Type 2 diabetes mellitus in children and adolescents.
Australian Family Physician, 45(6), 401-406. Retrieved from
https://search.proquest.com/docview/1794902478?accountid=8194
DIABETES IN CHILDREN
6. References
American Diabetes Association. (2015). 2. Classification and diagnosis of diabetes. Diabetes
care, 38(Supplement 1), S8-S16.
American Diabetes Association. (2015). Standards of medical care in diabetes—2015
abridged for primary care providers. Clinical diabetes: a publication of the American
Diabetes Association, 33(2), 97.
Australian Government Department of Health. (2015) Australian National Diabetes Strategy
2016–2020. Access date: 23rd June. 2018. Retrieved from:
http://www.health.gov.au/internet/main/publishing.nsf/content/3AF935DA210DA043
CA257EFB000D0C03/$File/Australian%20National%20Diabetes%20Strategy
%202016-2020.pdf
Australian Institute of Health and Welfare. (2014).Type 2 diabetes in Australia’s children and
young people: a working paper. Access date: 23rd June. 2018. Retrieved from:
https://www.aihw.gov.au/getmedia/bc5d50e5-8ca0-474d-be77-
f96234d9a532/15203.pdf.aspx?inline=true
Gao, Y. Q., Gao, M., & Xue, Y. (2016). Treatment of diabetes in children. Experimental and
therapeutic medicine, 11(4), 1168-1172. Doi: doi: 10.3892/etm.2016.3039
Kao, K., & Sabin, M. A. (2016). Type 2 diabetes mellitus in children and adolescents.
Australian Family Physician, 45(6), 401-406. Retrieved from
https://search.proquest.com/docview/1794902478?accountid=8194
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
DIABETES IN CHILDREN
Smith, C. J., & Ryckman, K. K. (2015). Epigenetic and developmental influences on the risk
of obesity, diabetes, and metabolic syndrome. Diabetes, metabolic syndrome and
obesity: targets and therapy, 8, 295.
Tamborlane, W. V., Haymond, M. W., Dunger, D., Shankar, R., Gubitosi-Klug, R., Bethin,
K., ... & Portman, R. (2016). Expanding treatment options for youth with type 2
diabetes: current problems and proposed solutions: a white paper from the NICHD
Diabetes Working Group. Diabetes Care, 39(3), 323-329.
DIABETES IN CHILDREN
Smith, C. J., & Ryckman, K. K. (2015). Epigenetic and developmental influences on the risk
of obesity, diabetes, and metabolic syndrome. Diabetes, metabolic syndrome and
obesity: targets and therapy, 8, 295.
Tamborlane, W. V., Haymond, M. W., Dunger, D., Shankar, R., Gubitosi-Klug, R., Bethin,
K., ... & Portman, R. (2016). Expanding treatment options for youth with type 2
diabetes: current problems and proposed solutions: a white paper from the NICHD
Diabetes Working Group. Diabetes Care, 39(3), 323-329.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


