Exploring Diabetes Drugs for Treating Alzheimer's Disease (AD)
VerifiedAdded on 2023/04/24
|27
|9873
|135
Literature Review
AI Summary
This literature review examines the potential of repurposing type 2 diabetes drugs for the treatment of Alzheimer's disease (AD). It highlights the connection between diabetes and AD, primarily focusing on insulin resistance and deficiency as key links. The review discusses the epidemiology and etiology of AD, including the role of amyloid-beta plaques and neurofibrillary tangles. It also explores current standard of care therapies and novel experimental approaches for AD treatment. A significant portion of the review is dedicated to elucidating the link between type 2 diabetes drugs and their potential efficacy in treating AD, emphasizing the role of insulin resistance and the impact of drugs on amyloid-beta accumulation and tau protein phosphorylation. The review references various studies to support its claims and provides a comprehensive overview of the potential for repurposing diabetes drugs to combat Alzheimer's disease.

1
Title: Repurposing diabetes drugs as treatments for Alzheimer's Disease
Title: Repurposing diabetes drugs as treatments for Alzheimer's Disease
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Abstract
The research topic basically captures the association that exists between Alzheimer disease
and diabetes. Both of these conditions have an adverse impact on the health and well-being of
many people all around the globe. The research study primarily captures how certain anti-
diabetic drugs can be used for the purpose of treating AD in individuals. A thorough and
detailed insight has been provided onto both of the health conditions in order to show the link
that connects both of them. The key connection between diabetes and Alzheimer disease
arises due to insulin resistance and deficiency. The research study has been designed to
address how diabetic drugs can be used for the purpose of treating Alzheimer disease in
individuals.
Introduction
Type 2 diabetes and Alzheimer disease (AD) are considered as the two most common
diseases in the aging population. It has been estimated that around 5.4 million people in
United States suffer from AD and the risk of this disease increase with the age. According to
the study of Yarchoan & Arnold, (2014), one in the eight people above the age of 65 and
every one in two people above the age of 85 years suffer from AD. WHO has also recognised
the increasing complexity of the dementia and have also acknowledged that all countries
should consider dementia as a critical public health problem. AD is considered as the most
common form of dementia, in which people suffer from progressive deterioration of memory
along with other problems related to cognitive functioning (Lee & Krishnan, 2010). The
report of WHO has identified that “In Singapore, the number of people afflicted by the
condition is expected to rise from about 22,000 currently to about 53,000 in 2020 and
187,000 in 2050” (WHO, 2017, p. 2).
Similarly, the occurrence of type 2 diabetes among the population is also very high. Yarchoan
& Arnold, (2014) have identified that around 90% of the aging population of US suffer from
type 2 diabetes and similar statistics have been identified in other developing nations as well.
Therefore type 2 diabetes and AD are significant public health issues that affect the quality of
life of the individuals. Akter et al. (2011) has argued that there is a significant link between
diabetes and Alzheimer disease, as they result in many social and health related
consequences.
Abstract
The research topic basically captures the association that exists between Alzheimer disease
and diabetes. Both of these conditions have an adverse impact on the health and well-being of
many people all around the globe. The research study primarily captures how certain anti-
diabetic drugs can be used for the purpose of treating AD in individuals. A thorough and
detailed insight has been provided onto both of the health conditions in order to show the link
that connects both of them. The key connection between diabetes and Alzheimer disease
arises due to insulin resistance and deficiency. The research study has been designed to
address how diabetic drugs can be used for the purpose of treating Alzheimer disease in
individuals.
Introduction
Type 2 diabetes and Alzheimer disease (AD) are considered as the two most common
diseases in the aging population. It has been estimated that around 5.4 million people in
United States suffer from AD and the risk of this disease increase with the age. According to
the study of Yarchoan & Arnold, (2014), one in the eight people above the age of 65 and
every one in two people above the age of 85 years suffer from AD. WHO has also recognised
the increasing complexity of the dementia and have also acknowledged that all countries
should consider dementia as a critical public health problem. AD is considered as the most
common form of dementia, in which people suffer from progressive deterioration of memory
along with other problems related to cognitive functioning (Lee & Krishnan, 2010). The
report of WHO has identified that “In Singapore, the number of people afflicted by the
condition is expected to rise from about 22,000 currently to about 53,000 in 2020 and
187,000 in 2050” (WHO, 2017, p. 2).
Similarly, the occurrence of type 2 diabetes among the population is also very high. Yarchoan
& Arnold, (2014) have identified that around 90% of the aging population of US suffer from
type 2 diabetes and similar statistics have been identified in other developing nations as well.
Therefore type 2 diabetes and AD are significant public health issues that affect the quality of
life of the individuals. Akter et al. (2011) has argued that there is a significant link between
diabetes and Alzheimer disease, as they result in many social and health related
consequences.
3
Epidemiology of Alzheimer disease
According to the study of Reitz, Brayne, & Mayeux, (2011), more than 25 million people all
over the world suffer from dementia and the most common form of dementia is Alzheimer's
disease. In developed, as well as developing nations, Alzheimer's disease has significant
consequences and significantly affect the individuals, caregivers and healthcare providers.
According to the report of Alzheimer Disease Association Singapore, dementia is a
progressive intellectual decline and it has been identified that in the year 2018 around 50
million people around the world were affected by dementia. This number is also expected to
increase to 82 million 2030 and 152 million by 2050 (Alzheimer Disease Association, 2018).
According to this information around 82,000 people in the year 2018 will be affected by
dementia and this number can increase to 1000,000 in few years (Alzheimer Disease
Association, 2018). The financial strain caused by the disease worldwide is very high and had
cost around US$1 trillion. According to the study of Woo, Thompson, & Magadi (2017), in
Singapore, dementia has resulted in costing S$2.8 billion in the year 2015, which is estimated
to increase three time by 2030.
Qiu, Kivipelto, & von Strauss, (2009) have identified that most of the people suffering with
dementia around the world are mainly suffering from AD and there is an increase of 5 million
cases every year. The WiSE study conducted by Subramaniam et al. (2015), conducted a
comprehensive single phase, cross-sectional, epidemiological survey for understanding the
prevalence of dementia and Ad in Singapore. The study adopted the 10/66 protocol with the
Diagnostic and Statistical Manual of mental disorders -fourth edition (DSM-IV) for the
diagnosis of dementia among the population. According to the results of the study of), it was
identified that prevalence of 10/66 dementia is 10% in the older population (75 years and
above), while the prevalence of DSM-IV dementia was found to be 4.6%. The WiSE study
the likelihood of dementia increases with age. such as “for those aged 75–84 years was 4.3
times and for those 85 years and over, it was 18.4 times higher compared to that of elderly
aged 60–74 years” (Institute of Mental Health, 2015b, p. 1).
Etiology of Alzheimer’s Disease
Alzheimer’s Disease is considered as the most common form of dementia. This disease is
mainly characterised by the mitochondrial impairment, oxidative stress, synaptic dysfunction
and disruption of the blood brain barrier. This impairment are mainly caused by the abnormal
Epidemiology of Alzheimer disease
According to the study of Reitz, Brayne, & Mayeux, (2011), more than 25 million people all
over the world suffer from dementia and the most common form of dementia is Alzheimer's
disease. In developed, as well as developing nations, Alzheimer's disease has significant
consequences and significantly affect the individuals, caregivers and healthcare providers.
According to the report of Alzheimer Disease Association Singapore, dementia is a
progressive intellectual decline and it has been identified that in the year 2018 around 50
million people around the world were affected by dementia. This number is also expected to
increase to 82 million 2030 and 152 million by 2050 (Alzheimer Disease Association, 2018).
According to this information around 82,000 people in the year 2018 will be affected by
dementia and this number can increase to 1000,000 in few years (Alzheimer Disease
Association, 2018). The financial strain caused by the disease worldwide is very high and had
cost around US$1 trillion. According to the study of Woo, Thompson, & Magadi (2017), in
Singapore, dementia has resulted in costing S$2.8 billion in the year 2015, which is estimated
to increase three time by 2030.
Qiu, Kivipelto, & von Strauss, (2009) have identified that most of the people suffering with
dementia around the world are mainly suffering from AD and there is an increase of 5 million
cases every year. The WiSE study conducted by Subramaniam et al. (2015), conducted a
comprehensive single phase, cross-sectional, epidemiological survey for understanding the
prevalence of dementia and Ad in Singapore. The study adopted the 10/66 protocol with the
Diagnostic and Statistical Manual of mental disorders -fourth edition (DSM-IV) for the
diagnosis of dementia among the population. According to the results of the study of), it was
identified that prevalence of 10/66 dementia is 10% in the older population (75 years and
above), while the prevalence of DSM-IV dementia was found to be 4.6%. The WiSE study
the likelihood of dementia increases with age. such as “for those aged 75–84 years was 4.3
times and for those 85 years and over, it was 18.4 times higher compared to that of elderly
aged 60–74 years” (Institute of Mental Health, 2015b, p. 1).
Etiology of Alzheimer’s Disease
Alzheimer’s Disease is considered as the most common form of dementia. This disease is
mainly characterised by the mitochondrial impairment, oxidative stress, synaptic dysfunction
and disruption of the blood brain barrier. This impairment are mainly caused by the abnormal
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
extracellular accumulation of amyloid-β peptide (Aβ) in the form of amyloid plaques and
aggregation of tau protein in intracellular neuro fibrillary tangles (NFTs) (Reitz, Brayne, &
Mayeux, 2011), which are considered as the hallmark of AD causing neuronal and synaptic
loss, increasing cognitive dysfunctions, loss of memory and normal body functions.
According to the study of Peric and Annaert, (2015), Ad could be of two types based on the
age of onset and pathological factors.
Another hypothesis is Tau protein deposition in the insoluble forms results in the loss of tau
function. This further results in instability of microtubule and promotes neurodegeneration.
Studies have identified that microtubule instability is a significant reason of AD (Kalra, and
Khan, 2015). Therefore, there are some significant causes of neurodegenerative disorder, that
may include genetic mutation, misfolding of protein, generation of the toxic molecules and
oxidative stress, mitochondrial dysfunction, neuro-inflammatory process and protein
degradation pathways. All of these causes are also associated with type 2 diabetes and its
pathological conditions.
Pathology of AD
Dementia is a disorder that is characterised by the deterioration of the cognitive functioning
and increasing behavioural problems. Alzheimer disease (AD) is considered as the most
common cause of Dementia. According to the study of Perry and Perry (2015) the pathology
of AD largely remains a mystery for most of the scholars and scientists. More focus has been
placed on brain, while the disease mainly takes place on cellular level. According to the study
of Reitz, Brayne, & Mayeux, (2011), the main pathological change that has been identified in
the AD brain tissue are that the level of both amyloid-β (Aβ) peptide is increased, which is
deposited extracellularly in diffuse and neuritic plaques. Also, hyperphosphory-lated tau (p-
tau), which is a microtubule assembly protein that mainly accumulated intercellularly as
neurofibrillary tangles (nFts) (Reitz, Brayne, & Mayeux, 2011).
Perry and Perry (2015) have also identified that molecular changes occurring due to aging in
the individuals led to altering the metabolism and biochemistry of individual pathways.
Addition to these pathologies, AD is also characterised by the widespread loss of synapses
and neurons. According to Ferrarelli (2018), Alzheimer’s disease (AD) is a complex
neurodegenerative disease, which is further characterised by the progressive loss of cognitive
functioning and dementia. Ferrarelli (2018) argued that “formation of plaques (focal
aggregates) of the protein amyloid-β (Aβ) in the brain is frequently observed in AD patients,
extracellular accumulation of amyloid-β peptide (Aβ) in the form of amyloid plaques and
aggregation of tau protein in intracellular neuro fibrillary tangles (NFTs) (Reitz, Brayne, &
Mayeux, 2011), which are considered as the hallmark of AD causing neuronal and synaptic
loss, increasing cognitive dysfunctions, loss of memory and normal body functions.
According to the study of Peric and Annaert, (2015), Ad could be of two types based on the
age of onset and pathological factors.
Another hypothesis is Tau protein deposition in the insoluble forms results in the loss of tau
function. This further results in instability of microtubule and promotes neurodegeneration.
Studies have identified that microtubule instability is a significant reason of AD (Kalra, and
Khan, 2015). Therefore, there are some significant causes of neurodegenerative disorder, that
may include genetic mutation, misfolding of protein, generation of the toxic molecules and
oxidative stress, mitochondrial dysfunction, neuro-inflammatory process and protein
degradation pathways. All of these causes are also associated with type 2 diabetes and its
pathological conditions.
Pathology of AD
Dementia is a disorder that is characterised by the deterioration of the cognitive functioning
and increasing behavioural problems. Alzheimer disease (AD) is considered as the most
common cause of Dementia. According to the study of Perry and Perry (2015) the pathology
of AD largely remains a mystery for most of the scholars and scientists. More focus has been
placed on brain, while the disease mainly takes place on cellular level. According to the study
of Reitz, Brayne, & Mayeux, (2011), the main pathological change that has been identified in
the AD brain tissue are that the level of both amyloid-β (Aβ) peptide is increased, which is
deposited extracellularly in diffuse and neuritic plaques. Also, hyperphosphory-lated tau (p-
tau), which is a microtubule assembly protein that mainly accumulated intercellularly as
neurofibrillary tangles (nFts) (Reitz, Brayne, & Mayeux, 2011).
Perry and Perry (2015) have also identified that molecular changes occurring due to aging in
the individuals led to altering the metabolism and biochemistry of individual pathways.
Addition to these pathologies, AD is also characterised by the widespread loss of synapses
and neurons. According to Ferrarelli (2018), Alzheimer’s disease (AD) is a complex
neurodegenerative disease, which is further characterised by the progressive loss of cognitive
functioning and dementia. Ferrarelli (2018) argued that “formation of plaques (focal
aggregates) of the protein amyloid-β (Aβ) in the brain is frequently observed in AD patients,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
as are acetylation and aggregation of the protein tau and loss of the prolyl isomerase Pin1”
(p. 1).
Standard of care / therapies for AD
Cholinesterase inhibitors is considered as the most significant part for the treatment of the
patients suffering with AD. For the treatment of mild to moderate AD, four drugs have been
approved including, donepezil, galantamine, rivastig-mine, and tacrine (Apostolova 2016).
This therapy is also considered as significant standard of care for the patients suffering with
AD. The ChEIs are considered as clinically beneficial in the double blinded, placebo control
trials. However, the recent reviews have informed that ChEIs including rivastigmine and
galantamine do not have much clinical benefits than donepezil. The recent studies have
shown that Acetylcholinesterase inhibitors (AChEIs) and memantine remain the only
important drugs that are used for the treatment of AD. It is also required that patient continue
these therapies for long terms for benefits, as the benefits can be seen on the severe level of
the illness as well (Bishara et al. 2015).
Novel experimental therapies for AD
According to the evidences, Alzheimer's disease (AD) is considered as a significant
healthcare problem in the developed and developing nations. The novel treatments and
pharmacotherapies are mainly based on the amyloidogenic hypothesis of AD, which informs
that beta amyloid (Aβ) peptide is mainly responsible for cognitive impairment in patients
with AD (Mahajan 2015). Therefore, the main goal of the novel treatment approaches is to
reduce the production of Aβ through the inhibition of β and γ secretase enzymes and to
enhance the mechanism of dissolution of the existing cerebral Aβ plaques (Folch et al. 2016).
The novel treatment strategies include cleavage of amyloid precursor protein (APP) by α-
secretase, which is also considered as the disease modifying strategy for AD (Mahajan 2015).
Link between T2D drugs and efficacy for AD
There are various studies that have provided the epidemiological evidences linking type 2
diabetes and its related conditions, like obesity, metabolic syndrome and hyperinsulinemia,
with Alzheimer’s disease (Beydoun et al. 2008; Li, Song, & Leng 2015). The main link of
type 2 diabetes and AD is associated with insulin resistance and deficiency. The first clue that
informs that how the brain may become insulin resistant in AD explains that Aβ oligomers
as are acetylation and aggregation of the protein tau and loss of the prolyl isomerase Pin1”
(p. 1).
Standard of care / therapies for AD
Cholinesterase inhibitors is considered as the most significant part for the treatment of the
patients suffering with AD. For the treatment of mild to moderate AD, four drugs have been
approved including, donepezil, galantamine, rivastig-mine, and tacrine (Apostolova 2016).
This therapy is also considered as significant standard of care for the patients suffering with
AD. The ChEIs are considered as clinically beneficial in the double blinded, placebo control
trials. However, the recent reviews have informed that ChEIs including rivastigmine and
galantamine do not have much clinical benefits than donepezil. The recent studies have
shown that Acetylcholinesterase inhibitors (AChEIs) and memantine remain the only
important drugs that are used for the treatment of AD. It is also required that patient continue
these therapies for long terms for benefits, as the benefits can be seen on the severe level of
the illness as well (Bishara et al. 2015).
Novel experimental therapies for AD
According to the evidences, Alzheimer's disease (AD) is considered as a significant
healthcare problem in the developed and developing nations. The novel treatments and
pharmacotherapies are mainly based on the amyloidogenic hypothesis of AD, which informs
that beta amyloid (Aβ) peptide is mainly responsible for cognitive impairment in patients
with AD (Mahajan 2015). Therefore, the main goal of the novel treatment approaches is to
reduce the production of Aβ through the inhibition of β and γ secretase enzymes and to
enhance the mechanism of dissolution of the existing cerebral Aβ plaques (Folch et al. 2016).
The novel treatment strategies include cleavage of amyloid precursor protein (APP) by α-
secretase, which is also considered as the disease modifying strategy for AD (Mahajan 2015).
Link between T2D drugs and efficacy for AD
There are various studies that have provided the epidemiological evidences linking type 2
diabetes and its related conditions, like obesity, metabolic syndrome and hyperinsulinemia,
with Alzheimer’s disease (Beydoun et al. 2008; Li, Song, & Leng 2015). The main link of
type 2 diabetes and AD is associated with insulin resistance and deficiency. The first clue that
informs that how the brain may become insulin resistant in AD explains that Aβ oligomers
6
get binds to hippocampal neurons and results in triggering the dendritic insulin receptor
substrates (IRs) from the plasma membrane (Zhao et al 2008), which was significantly
identified in the brain of the individual suffering from AD (Moloney et al. 2010).
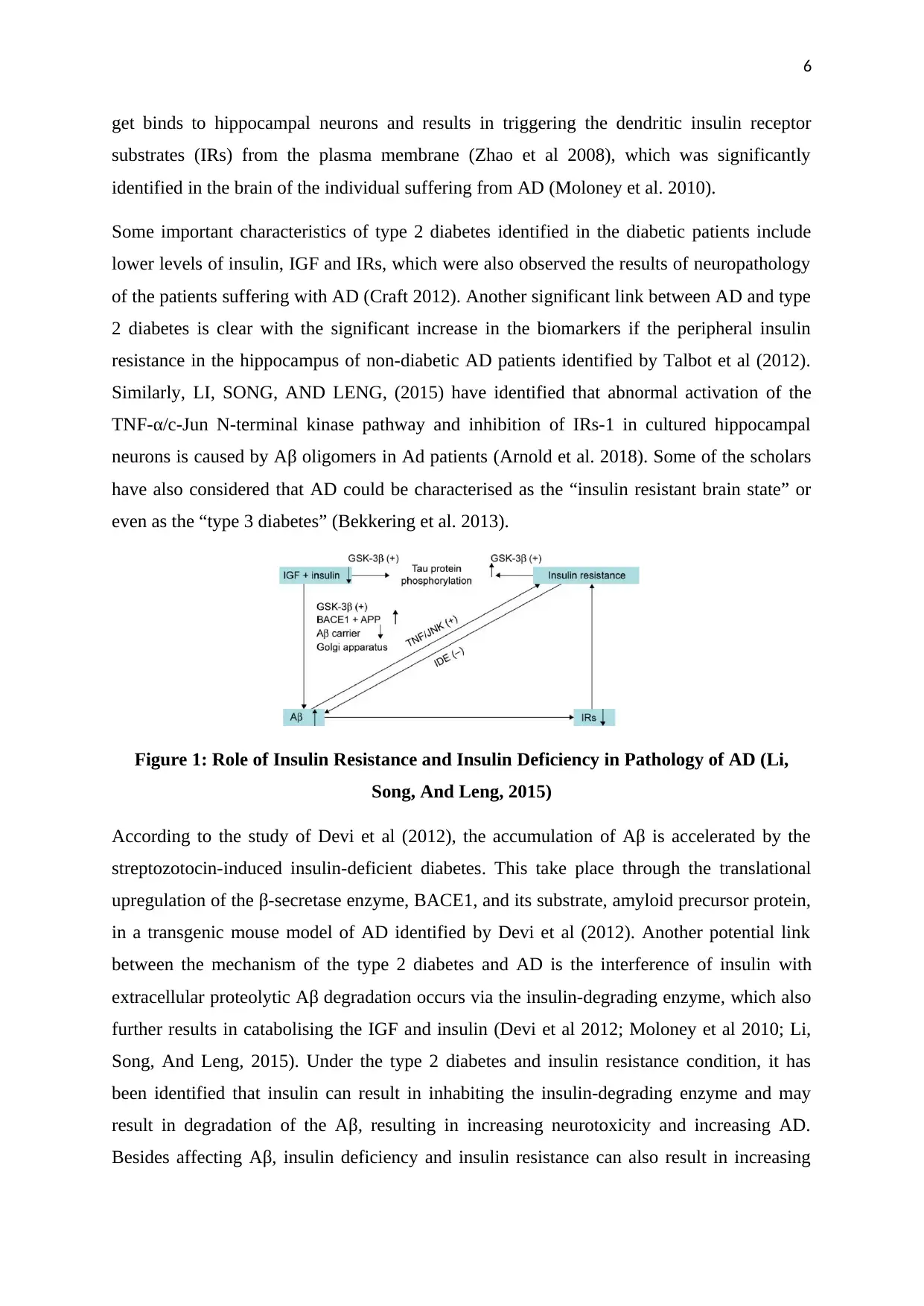
Some important characteristics of type 2 diabetes identified in the diabetic patients include
lower levels of insulin, IGF and IRs, which were also observed the results of neuropathology
of the patients suffering with AD (Craft 2012). Another significant link between AD and type
2 diabetes is clear with the significant increase in the biomarkers if the peripheral insulin
resistance in the hippocampus of non-diabetic AD patients identified by Talbot et al (2012).
Similarly, LI, SONG, AND LENG, (2015) have identified that abnormal activation of the
TNF-α/c-Jun N-terminal kinase pathway and inhibition of IRs-1 in cultured hippocampal
neurons is caused by Aβ oligomers in Ad patients (Arnold et al. 2018). Some of the scholars
have also considered that AD could be characterised as the “insulin resistant brain state” or
even as the “type 3 diabetes” (Bekkering et al. 2013).
Figure 1: Role of Insulin Resistance and Insulin Deficiency in Pathology of AD (Li,
Song, And Leng, 2015)
According to the study of Devi et al (2012), the accumulation of Aβ is accelerated by the
streptozotocin-induced insulin-deficient diabetes. This take place through the translational
upregulation of the β-secretase enzyme, BACE1, and its substrate, amyloid precursor protein,
in a transgenic mouse model of AD identified by Devi et al (2012). Another potential link
between the mechanism of the type 2 diabetes and AD is the interference of insulin with
extracellular proteolytic Aβ degradation occurs via the insulin-degrading enzyme, which also
further results in catabolising the IGF and insulin (Devi et al 2012; Moloney et al 2010; Li,
Song, And Leng, 2015). Under the type 2 diabetes and insulin resistance condition, it has
been identified that insulin can result in inhabiting the insulin-degrading enzyme and may
result in degradation of the Aβ, resulting in increasing neurotoxicity and increasing AD.
Besides affecting Aβ, insulin deficiency and insulin resistance can also result in increasing
get binds to hippocampal neurons and results in triggering the dendritic insulin receptor
substrates (IRs) from the plasma membrane (Zhao et al 2008), which was significantly
identified in the brain of the individual suffering from AD (Moloney et al. 2010).
Some important characteristics of type 2 diabetes identified in the diabetic patients include
lower levels of insulin, IGF and IRs, which were also observed the results of neuropathology
of the patients suffering with AD (Craft 2012). Another significant link between AD and type
2 diabetes is clear with the significant increase in the biomarkers if the peripheral insulin
resistance in the hippocampus of non-diabetic AD patients identified by Talbot et al (2012).
Similarly, LI, SONG, AND LENG, (2015) have identified that abnormal activation of the
TNF-α/c-Jun N-terminal kinase pathway and inhibition of IRs-1 in cultured hippocampal
neurons is caused by Aβ oligomers in Ad patients (Arnold et al. 2018). Some of the scholars
have also considered that AD could be characterised as the “insulin resistant brain state” or
even as the “type 3 diabetes” (Bekkering et al. 2013).
Figure 1: Role of Insulin Resistance and Insulin Deficiency in Pathology of AD (Li,
Song, And Leng, 2015)
According to the study of Devi et al (2012), the accumulation of Aβ is accelerated by the
streptozotocin-induced insulin-deficient diabetes. This take place through the translational
upregulation of the β-secretase enzyme, BACE1, and its substrate, amyloid precursor protein,
in a transgenic mouse model of AD identified by Devi et al (2012). Another potential link
between the mechanism of the type 2 diabetes and AD is the interference of insulin with
extracellular proteolytic Aβ degradation occurs via the insulin-degrading enzyme, which also
further results in catabolising the IGF and insulin (Devi et al 2012; Moloney et al 2010; Li,
Song, And Leng, 2015). Under the type 2 diabetes and insulin resistance condition, it has
been identified that insulin can result in inhabiting the insulin-degrading enzyme and may
result in degradation of the Aβ, resulting in increasing neurotoxicity and increasing AD.
Besides affecting Aβ, insulin deficiency and insulin resistance can also result in increasing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
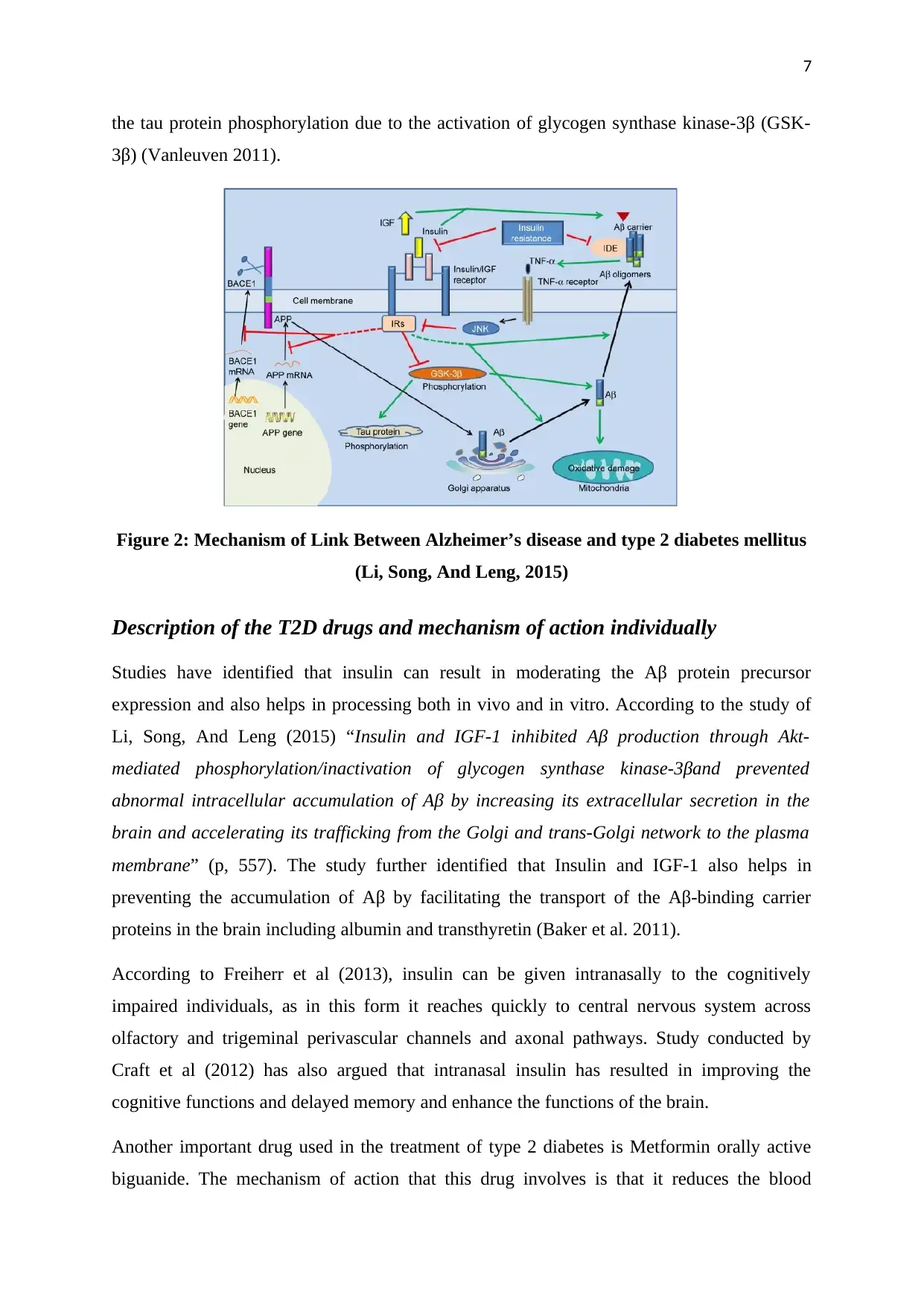
the tau protein phosphorylation due to the activation of glycogen synthase kinase-3β (GSK-
3β) (Vanleuven 2011).
Figure 2: Mechanism of Link Between Alzheimer’s disease and type 2 diabetes mellitus
(Li, Song, And Leng, 2015)
Description of the T2D drugs and mechanism of action individually
Studies have identified that insulin can result in moderating the Aβ protein precursor
expression and also helps in processing both in vivo and in vitro. According to the study of
Li, Song, And Leng (2015) “Insulin and IGF-1 inhibited Aβ production through Akt-
mediated phosphorylation/inactivation of glycogen synthase kinase-3βand prevented
abnormal intracellular accumulation of Aβ by increasing its extracellular secretion in the
brain and accelerating its trafficking from the Golgi and trans-Golgi network to the plasma
membrane” (p, 557). The study further identified that Insulin and IGF-1 also helps in
preventing the accumulation of Aβ by facilitating the transport of the Aβ-binding carrier
proteins in the brain including albumin and transthyretin (Baker et al. 2011).
According to Freiherr et al (2013), insulin can be given intranasally to the cognitively
impaired individuals, as in this form it reaches quickly to central nervous system across
olfactory and trigeminal perivascular channels and axonal pathways. Study conducted by
Craft et al (2012) has also argued that intranasal insulin has resulted in improving the
cognitive functions and delayed memory and enhance the functions of the brain.
Another important drug used in the treatment of type 2 diabetes is Metformin orally active
biguanide. The mechanism of action that this drug involves is that it reduces the blood
the tau protein phosphorylation due to the activation of glycogen synthase kinase-3β (GSK-
3β) (Vanleuven 2011).
Figure 2: Mechanism of Link Between Alzheimer’s disease and type 2 diabetes mellitus
(Li, Song, And Leng, 2015)
Description of the T2D drugs and mechanism of action individually
Studies have identified that insulin can result in moderating the Aβ protein precursor
expression and also helps in processing both in vivo and in vitro. According to the study of
Li, Song, And Leng (2015) “Insulin and IGF-1 inhibited Aβ production through Akt-
mediated phosphorylation/inactivation of glycogen synthase kinase-3βand prevented
abnormal intracellular accumulation of Aβ by increasing its extracellular secretion in the
brain and accelerating its trafficking from the Golgi and trans-Golgi network to the plasma
membrane” (p, 557). The study further identified that Insulin and IGF-1 also helps in
preventing the accumulation of Aβ by facilitating the transport of the Aβ-binding carrier
proteins in the brain including albumin and transthyretin (Baker et al. 2011).
According to Freiherr et al (2013), insulin can be given intranasally to the cognitively
impaired individuals, as in this form it reaches quickly to central nervous system across
olfactory and trigeminal perivascular channels and axonal pathways. Study conducted by
Craft et al (2012) has also argued that intranasal insulin has resulted in improving the
cognitive functions and delayed memory and enhance the functions of the brain.
Another important drug used in the treatment of type 2 diabetes is Metformin orally active
biguanide. The mechanism of action that this drug involves is that it reduces the blood
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
glucose levels by suppressing the hepatic glucose output increasing the intestinal use of
glucose, increasing insulin-mediated glucose disposal and decreasing the oxidation of fatty
acids (Femminella et al. 2017). Study conducted by Li, Song, and Leng (2015) has identified
that “It also reduces insulin levels, inflammation and thrombosis, and the risks of metabolic
syndrome and diabetes in persons without diabetes” (p. 554).
Studies have identified that inflammation and insulin resistance are significant in the
pathogenesis of AD. Therefore, Thiazolidinediones (peroxisome proliferator-activated
receptor-γ) (PPARγ) agonists and potent insulin sensitizers could be significant in treating
inflammation. Thiazolidinediones have anti-inflammatory properties and its mechanism
“involves stimulation of the action of PPARγ in response to changes in insulin, thereby
triggering a drop in serum glucose” (Li, Song, and Leng 2015, p. 555). The mechanism of
Thiazolidinediones encompasses the stimulation of the actions of PPARγ, which occurs in
response to insulin and brings a decrease in the level of serum glucose (Risner et al. 2006).
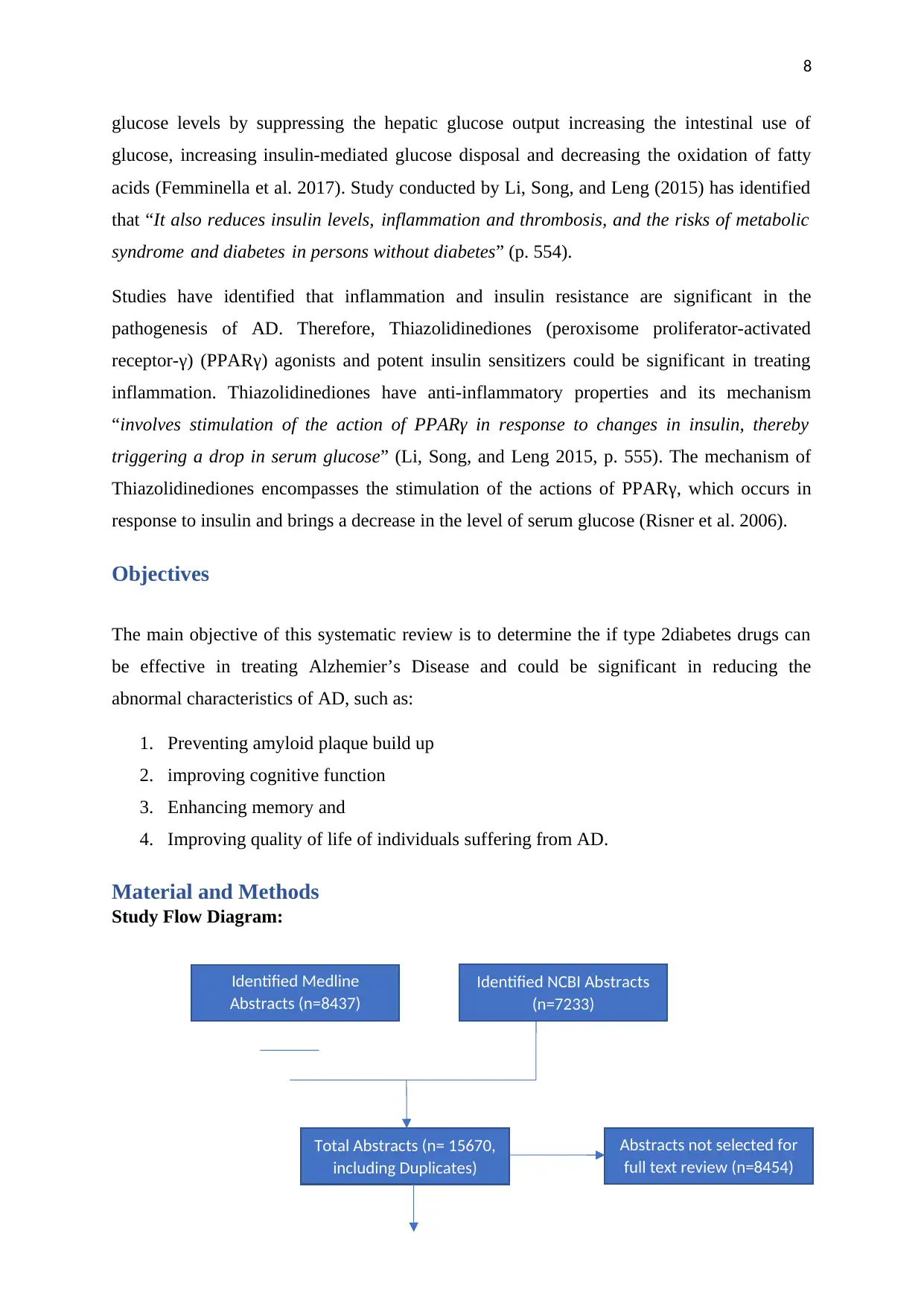
Objectives
The main objective of this systematic review is to determine the if type 2diabetes drugs can
be effective in treating Alzhemier’s Disease and could be significant in reducing the
abnormal characteristics of AD, such as:
1. Preventing amyloid plaque build up
2. improving cognitive function
3. Enhancing memory and
4. Improving quality of life of individuals suffering from AD.
Material and Methods
Study Flow Diagram:
Identified Medline
Abstracts (n=8437)
Identified NCBI Abstracts
(n=7233)
Abstracts not selected for
full text review (n=8454)
Total Abstracts (n= 15670,
including Duplicates)
glucose levels by suppressing the hepatic glucose output increasing the intestinal use of
glucose, increasing insulin-mediated glucose disposal and decreasing the oxidation of fatty
acids (Femminella et al. 2017). Study conducted by Li, Song, and Leng (2015) has identified
that “It also reduces insulin levels, inflammation and thrombosis, and the risks of metabolic
syndrome and diabetes in persons without diabetes” (p. 554).
Studies have identified that inflammation and insulin resistance are significant in the
pathogenesis of AD. Therefore, Thiazolidinediones (peroxisome proliferator-activated
receptor-γ) (PPARγ) agonists and potent insulin sensitizers could be significant in treating
inflammation. Thiazolidinediones have anti-inflammatory properties and its mechanism
“involves stimulation of the action of PPARγ in response to changes in insulin, thereby
triggering a drop in serum glucose” (Li, Song, and Leng 2015, p. 555). The mechanism of
Thiazolidinediones encompasses the stimulation of the actions of PPARγ, which occurs in
response to insulin and brings a decrease in the level of serum glucose (Risner et al. 2006).
Objectives
The main objective of this systematic review is to determine the if type 2diabetes drugs can
be effective in treating Alzhemier’s Disease and could be significant in reducing the
abnormal characteristics of AD, such as:
1. Preventing amyloid plaque build up
2. improving cognitive function
3. Enhancing memory and
4. Improving quality of life of individuals suffering from AD.
Material and Methods
Study Flow Diagram:
Identified Medline
Abstracts (n=8437)
Identified NCBI Abstracts
(n=7233)
Abstracts not selected for
full text review (n=8454)
Total Abstracts (n= 15670,
including Duplicates)
9
Inclusion and Exclusion Criteria: This systematic review of literature has included only
peer reviewed studies and published reports of health departments, health institutions and
government bodies for providing the correct statistics and data. Unpublished studies,
published thesis or dissertations, online articles etc are excluded from the research.
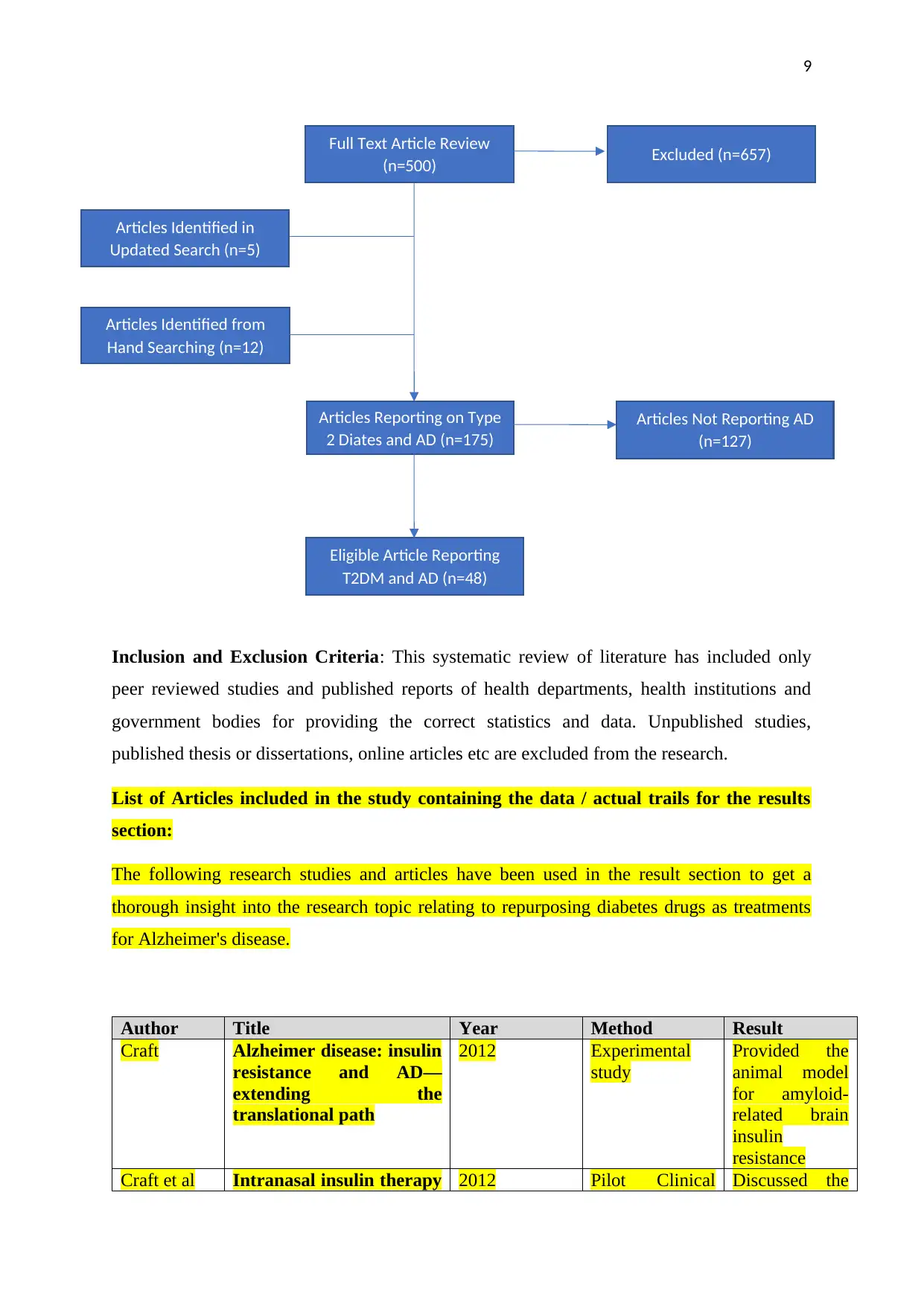
List of Articles included in the study containing the data / actual trails for the results
section:
The following research studies and articles have been used in the result section to get a
thorough insight into the research topic relating to repurposing diabetes drugs as treatments
for Alzheimer's disease.
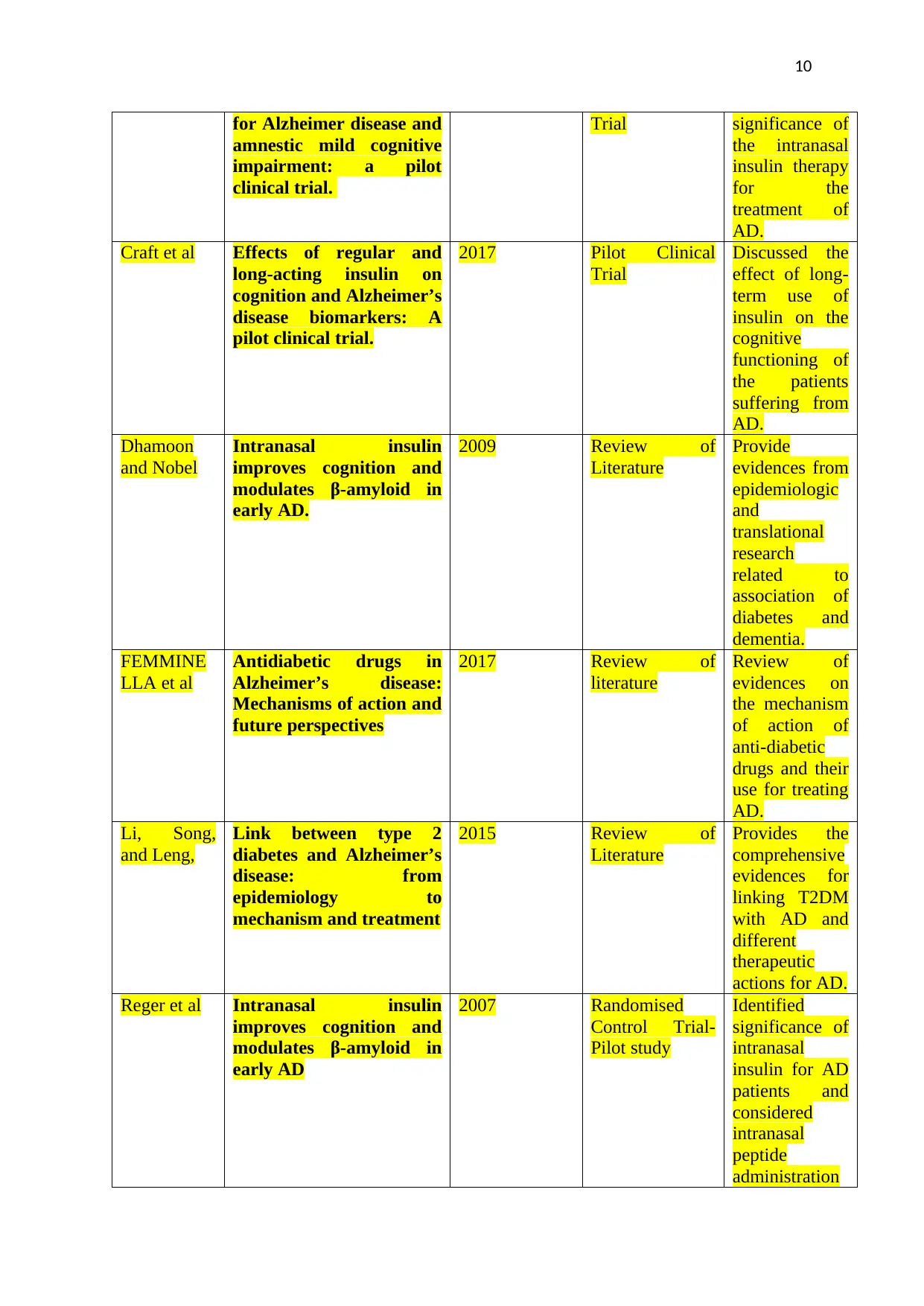
Author Title Year Method Result
Craft Alzheimer disease: insulin
resistance and AD—
extending the
translational path
2012 Experimental
study
Provided the
animal model
for amyloid-
related brain
insulin
resistance
Craft et al Intranasal insulin therapy 2012 Pilot Clinical Discussed the
Full Text Article Review
(n=500) Excluded (n=657)
Articles Reporting on Type
2 Diates and AD (n=175)
Articles Identified in
Updated Search (n=5)
Articles Identified from
Hand Searching (n=12)
Articles Not Reporting AD
(n=127)
Eligible Article Reporting
T2DM and AD (n=48)
Inclusion and Exclusion Criteria: This systematic review of literature has included only
peer reviewed studies and published reports of health departments, health institutions and
government bodies for providing the correct statistics and data. Unpublished studies,
published thesis or dissertations, online articles etc are excluded from the research.
List of Articles included in the study containing the data / actual trails for the results
section:
The following research studies and articles have been used in the result section to get a
thorough insight into the research topic relating to repurposing diabetes drugs as treatments
for Alzheimer's disease.
Author Title Year Method Result
Craft Alzheimer disease: insulin
resistance and AD—
extending the
translational path
2012 Experimental
study
Provided the
animal model
for amyloid-
related brain
insulin
resistance
Craft et al Intranasal insulin therapy 2012 Pilot Clinical Discussed the
Full Text Article Review
(n=500) Excluded (n=657)
Articles Reporting on Type
2 Diates and AD (n=175)
Articles Identified in
Updated Search (n=5)
Articles Identified from
Hand Searching (n=12)
Articles Not Reporting AD
(n=127)
Eligible Article Reporting
T2DM and AD (n=48)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
for Alzheimer disease and
amnestic mild cognitive
impairment: a pilot
clinical trial.
Trial significance of
the intranasal
insulin therapy
for the
treatment of
AD.
Craft et al Effects of regular and
long-acting insulin on
cognition and Alzheimer’s
disease biomarkers: A
pilot clinical trial.
2017 Pilot Clinical
Trial
Discussed the
effect of long-
term use of
insulin on the
cognitive
functioning of
the patients
suffering from
AD.
Dhamoon
and Nobel
Intranasal insulin
improves cognition and
modulates β-amyloid in
early AD.
2009 Review of
Literature
Provide
evidences from
epidemiologic
and
translational
research
related to
association of
diabetes and
dementia.
FEMMINE
LLA et al
Antidiabetic drugs in
Alzheimer’s disease:
Mechanisms of action and
future perspectives
2017 Review of
literature
Review of
evidences on
the mechanism
of action of
anti-diabetic
drugs and their
use for treating
AD.
Li, Song,
and Leng,
Link between type 2
diabetes and Alzheimer’s
disease: from
epidemiology to
mechanism and treatment
2015 Review of
Literature
Provides the
comprehensive
evidences for
linking T2DM
with AD and
different
therapeutic
actions for AD.
Reger et al Intranasal insulin
improves cognition and
modulates β-amyloid in
early AD
2007 Randomised
Control Trial-
Pilot study
Identified
significance of
intranasal
insulin for AD
patients and
considered
intranasal
peptide
administration
for Alzheimer disease and
amnestic mild cognitive
impairment: a pilot
clinical trial.
Trial significance of
the intranasal
insulin therapy
for the
treatment of
AD.
Craft et al Effects of regular and
long-acting insulin on
cognition and Alzheimer’s
disease biomarkers: A
pilot clinical trial.
2017 Pilot Clinical
Trial
Discussed the
effect of long-
term use of
insulin on the
cognitive
functioning of
the patients
suffering from
AD.
Dhamoon
and Nobel
Intranasal insulin
improves cognition and
modulates β-amyloid in
early AD.
2009 Review of
Literature
Provide
evidences from
epidemiologic
and
translational
research
related to
association of
diabetes and
dementia.
FEMMINE
LLA et al
Antidiabetic drugs in
Alzheimer’s disease:
Mechanisms of action and
future perspectives
2017 Review of
literature
Review of
evidences on
the mechanism
of action of
anti-diabetic
drugs and their
use for treating
AD.
Li, Song,
and Leng,
Link between type 2
diabetes and Alzheimer’s
disease: from
epidemiology to
mechanism and treatment
2015 Review of
Literature
Provides the
comprehensive
evidences for
linking T2DM
with AD and
different
therapeutic
actions for AD.
Reger et al Intranasal insulin
improves cognition and
modulates β-amyloid in
early AD
2007 Randomised
Control Trial-
Pilot study
Identified
significance of
intranasal
insulin for AD
patients and
considered
intranasal
peptide
administration
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
as novel
treatment for
degenerative
diseases.
Koenig et al
Effects of the Insulin
Sensitizer Metformin in
Alzheimer’s Disease: Pilot
Data from a Randomized
Placebo-Controlled
Crossover Study
2017 Randomized
Placebo-
Controlled
Crossover Study
The metformin
drug can
enhance the
executive
functioning of
an individual
with AD
Risner et al Efficacy of rosiglitazone
in a genetically defined
population with mild-to-
moderate Alzheimer's
disease
2006 Randomised
control trial
Identified the
significance of
rosiglitazone
for treating
AD.
Results
Link Between Type 2 Diabetes and Alzheimer’s Disease
Studies have identified that type 2 diabetes and Alzheimer’s Disease have similar
pathological components. This is the reason that some scholars have called Ad as the type 3
diabetes. Evidences have also informed that type 2 diabetes is significantly associated with
increased risk of cognitive impairments. Both diseases have become the significant public
health concern all over the world, as very large number of aging populations around the
world, suffers from type 2 diabetes and AD. Diabetes affect the neurons and brain synaptic.
In Ad also the patients suffer from the loss of brain functions, decreased cognitive
functioning, loss of memory and inability in carrying out activities of daily life. The results of
this systematic review of literature informs that determining and identifying the link between
type 2 diabetes and AD can significantly help in developing the treatment strategies and
interventions that could address the similar pathological complexities of both diseases.
In type 2 diabetes, patients suffer from high blood sugar levels, which are caused by insulin
resistance and due to which body becomes unresponsive to insulin hormone. Although,
studies have identified that acute administration of insulin may improve the memory
domains. However, the studies have also identified that delayed memory process could also
as novel
treatment for
degenerative
diseases.
Koenig et al
Effects of the Insulin
Sensitizer Metformin in
Alzheimer’s Disease: Pilot
Data from a Randomized
Placebo-Controlled
Crossover Study
2017 Randomized
Placebo-
Controlled
Crossover Study
The metformin
drug can
enhance the
executive
functioning of
an individual
with AD
Risner et al Efficacy of rosiglitazone
in a genetically defined
population with mild-to-
moderate Alzheimer's
disease
2006 Randomised
control trial
Identified the
significance of
rosiglitazone
for treating
AD.
Results
Link Between Type 2 Diabetes and Alzheimer’s Disease
Studies have identified that type 2 diabetes and Alzheimer’s Disease have similar
pathological components. This is the reason that some scholars have called Ad as the type 3
diabetes. Evidences have also informed that type 2 diabetes is significantly associated with
increased risk of cognitive impairments. Both diseases have become the significant public
health concern all over the world, as very large number of aging populations around the
world, suffers from type 2 diabetes and AD. Diabetes affect the neurons and brain synaptic.
In Ad also the patients suffer from the loss of brain functions, decreased cognitive
functioning, loss of memory and inability in carrying out activities of daily life. The results of
this systematic review of literature informs that determining and identifying the link between
type 2 diabetes and AD can significantly help in developing the treatment strategies and
interventions that could address the similar pathological complexities of both diseases.
In type 2 diabetes, patients suffer from high blood sugar levels, which are caused by insulin
resistance and due to which body becomes unresponsive to insulin hormone. Although,
studies have identified that acute administration of insulin may improve the memory
domains. However, the studies have also identified that delayed memory process could also
12
occur due to chronic administration of insulin. Insulin signalling is an important brain
function that helps in taking up of glucose and results in producing the insulin degrading
enzyme (IDE) in order to reduce the glucose level from the body. IDE plays a significant role
in degradation of both insulin as well as amyloid beta (Aβ) protein. Therefore,
hyperinsulinemia could result in causing the competitive inhibition for IDE-dependent
Aβ degradation and can result in increasing the production of Aβ and can lead to Aβ plaque
accumulation. Therefore, the result of the studies displays a strong link between type 2
diabetes and AD.
Evidences informed that in diabetes, the alteration in the insulin signalling occurs that results
in reducing the IDE production and further resulting in reducing the degradation of Aβ and
therefore, this mechanism results in abnormal accumulation of Aβ in brain causing plaques
that result in affecting the cognitive functions, memory and loss of ability to carry out
activities of daily life. Increasing the insulin signalling has been identified as an important
approach that can help in reducing Aβ accumulation in Hippocampus and Cortex. Aβ
clearance is significant for preventing plaque accumulation, therefore, insulin has been found
to be significant in enhancing Aβ clearance. The deposition or the accumulation of Aβ can be
significantly increased by impaired insulin signalling caused by AD. Therefore, there is a
significant and important link between type 2 diabetes and AD, which may require the special
approach and strategies for the treatment of AD.
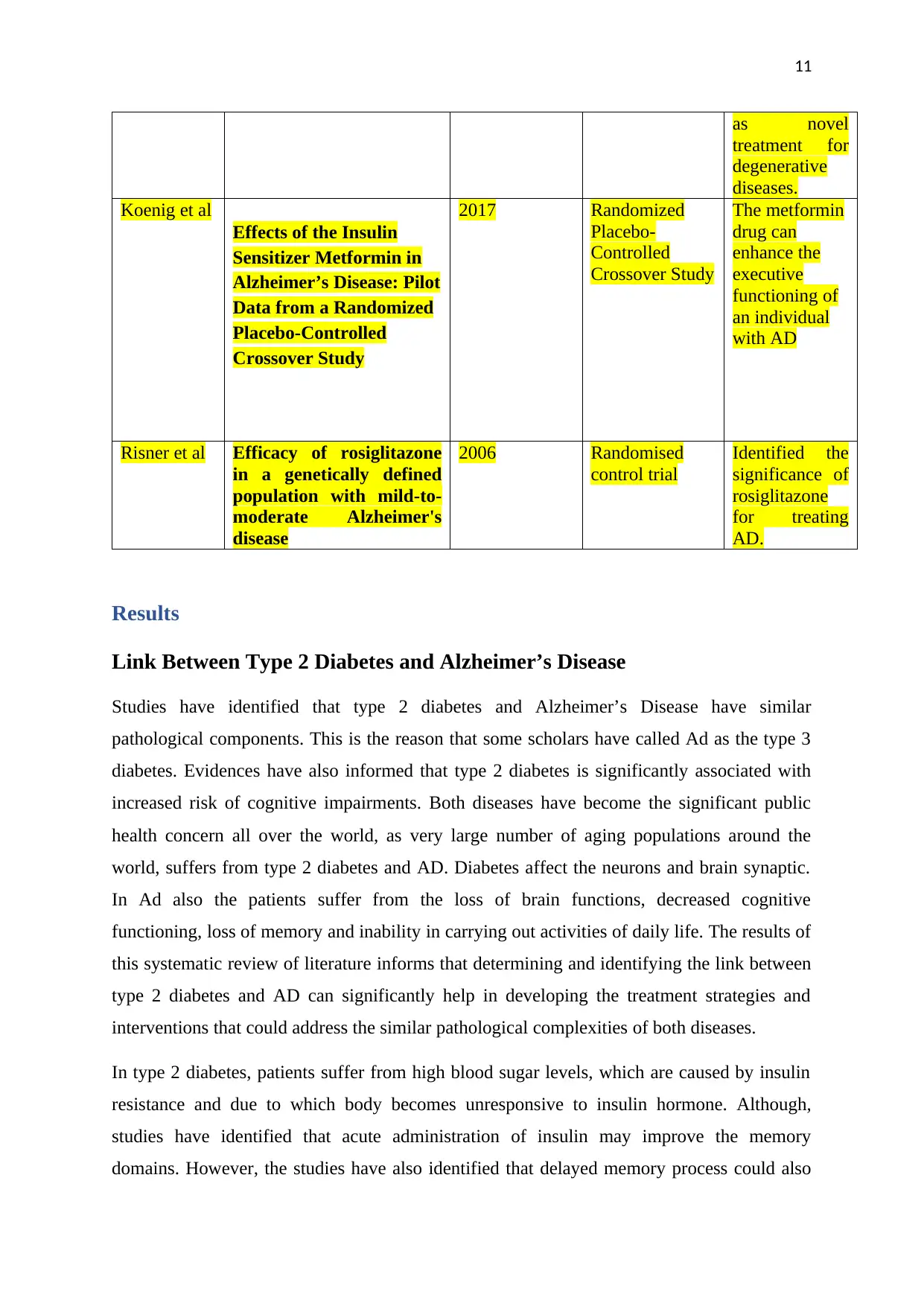
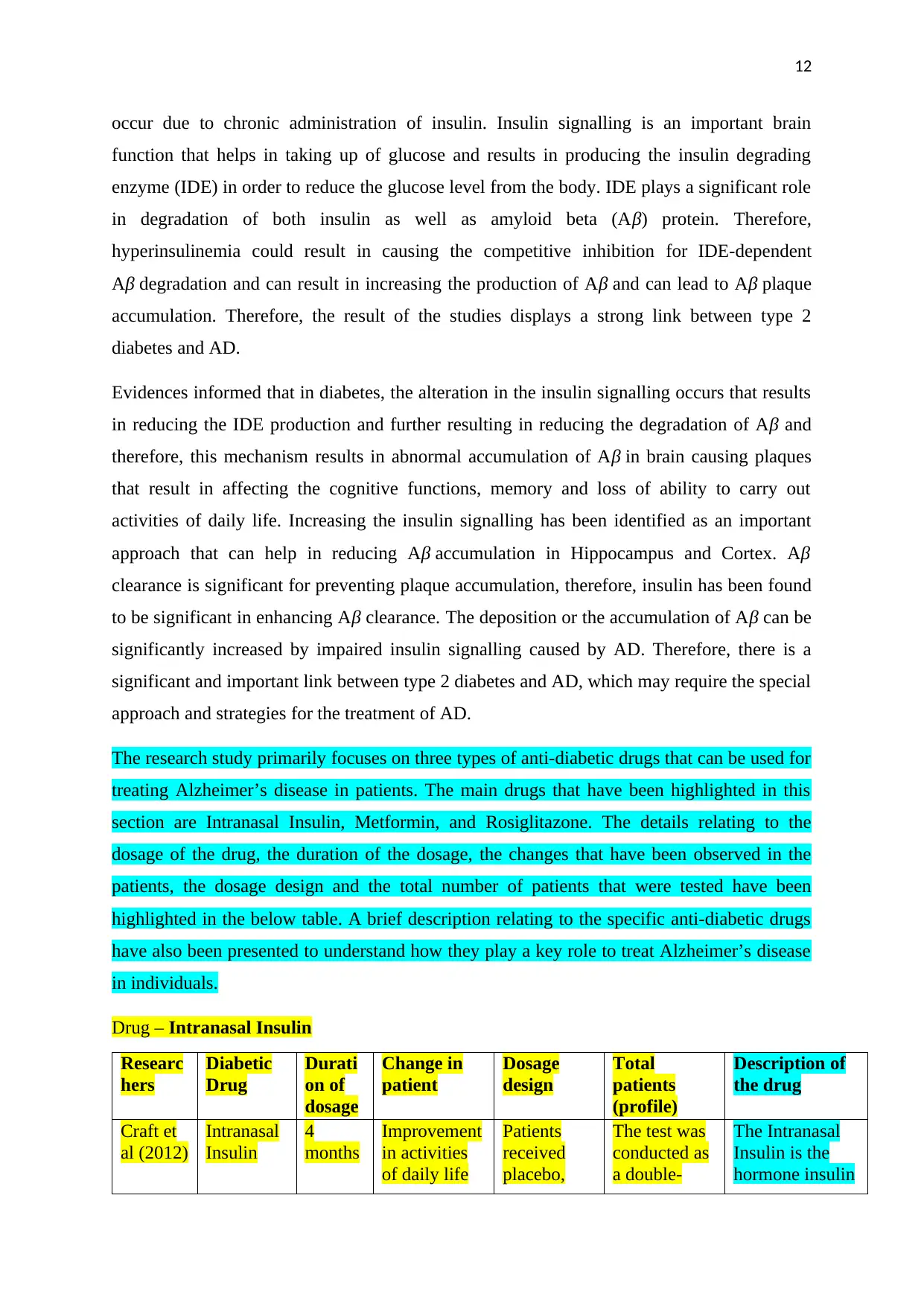
The research study primarily focuses on three types of anti-diabetic drugs that can be used for
treating Alzheimer’s disease in patients. The main drugs that have been highlighted in this
section are Intranasal Insulin, Metformin, and Rosiglitazone. The details relating to the
dosage of the drug, the duration of the dosage, the changes that have been observed in the
patients, the dosage design and the total number of patients that were tested have been
highlighted in the below table. A brief description relating to the specific anti-diabetic drugs
have also been presented to understand how they play a key role to treat Alzheimer’s disease
in individuals.
Drug – Intranasal Insulin
Researc
hers
Diabetic
Drug
Durati
on of
dosage
Change in
patient
Dosage
design
Total
patients
(profile)
Description of
the drug
Craft et
al (2012)
Intranasal
Insulin
4
months
Improvement
in activities
of daily life
Patients
received
placebo,
The test was
conducted as
a double-
The Intranasal
Insulin is the
hormone insulin
occur due to chronic administration of insulin. Insulin signalling is an important brain
function that helps in taking up of glucose and results in producing the insulin degrading
enzyme (IDE) in order to reduce the glucose level from the body. IDE plays a significant role
in degradation of both insulin as well as amyloid beta (Aβ) protein. Therefore,
hyperinsulinemia could result in causing the competitive inhibition for IDE-dependent
Aβ degradation and can result in increasing the production of Aβ and can lead to Aβ plaque
accumulation. Therefore, the result of the studies displays a strong link between type 2
diabetes and AD.
Evidences informed that in diabetes, the alteration in the insulin signalling occurs that results
in reducing the IDE production and further resulting in reducing the degradation of Aβ and
therefore, this mechanism results in abnormal accumulation of Aβ in brain causing plaques
that result in affecting the cognitive functions, memory and loss of ability to carry out
activities of daily life. Increasing the insulin signalling has been identified as an important
approach that can help in reducing Aβ accumulation in Hippocampus and Cortex. Aβ
clearance is significant for preventing plaque accumulation, therefore, insulin has been found
to be significant in enhancing Aβ clearance. The deposition or the accumulation of Aβ can be
significantly increased by impaired insulin signalling caused by AD. Therefore, there is a
significant and important link between type 2 diabetes and AD, which may require the special
approach and strategies for the treatment of AD.
The research study primarily focuses on three types of anti-diabetic drugs that can be used for
treating Alzheimer’s disease in patients. The main drugs that have been highlighted in this
section are Intranasal Insulin, Metformin, and Rosiglitazone. The details relating to the
dosage of the drug, the duration of the dosage, the changes that have been observed in the
patients, the dosage design and the total number of patients that were tested have been
highlighted in the below table. A brief description relating to the specific anti-diabetic drugs
have also been presented to understand how they play a key role to treat Alzheimer’s disease
in individuals.
Drug – Intranasal Insulin
Researc
hers
Diabetic
Drug
Durati
on of
dosage
Change in
patient
Dosage
design
Total
patients
(profile)
Description of
the drug
Craft et
al (2012)
Intranasal
Insulin
4
months
Improvement
in activities
of daily life
Patients
received
placebo,
The test was
conducted as
a double-
The Intranasal
Insulin is the
hormone insulin
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 27
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





